Abstract
Background:
The Hospital Readmission Reduction Program (HRRP) disproportionately penalizes hospitals serving minority communities. The National Academy of Science, Engineering, and Medicine has recommended that the Centers for Medicare and Medicaid Services (CMS) consider adjusting for social risk factors in their risk adjustment methodology. This study examines the association between the racial and ethnic composition of a hospital market and the impact of other social risk factors on the probability of a hospital being penalized under the HRRP.
Methods:
This study analyzes data from CMS, the American Hospital Association (AHA) and the American Community Survey (ACS) for 3,168 hospitals from 2013 to 2017. We used logistic regression models to estimate the association between the penalty status under HRRP and the racial and ethnic composition of a hospital market, and explored whether this association was moderated by other social risk factors.
Results:
Our results indicate that the probability of being penalized increases with the percentage of Black and Asian residents in the hospital service area (HSA) and decreased with the percentage of Hispanic residents in the HSA. This association was reduced and became statistically insignificant when we controlled for other social risk factors. The strongest predictors of penalty status were the hospital’s share of Medicaid patients and the percent of persons without a high school diploma in the HSA.
Conclusions:
By incorporating relevant social risk factors in the reimbursement methodology, CMS could mitigate the negative effects of HRRP on hospitals serving minority communities.
Keywords: HRRP, readmission, penalized hospital, social risk factors, racial composition
Introduction
There is growing concern that Medicare value-based payment programs disproportionately penalize hospitals that serve disadvantaged communities. These programs tie reimbursement to the quality of care and penalize hospitals for high rates of poor healthcare outcomes. However, patients from disadvantaged communities may have poorer healthcare outcomes for reason that are beyond the hospital’s control. Social risk factors such poverty, low educational attainment, social isolation, and neighborhood disadvantage can hinder patients’ ability to heal and recover from illness.1 Some health researchers and policymakers assert that Medicare’s value-based payment programs unfairly penalize certain hospitals because the current risk adjustment methodologies that measure quality of care do not adequately account for the influence of social risk factors.2–6 Studies have found that hospitals serving low-income patients were more likely to be penalized.7 Several studies have found that hospitals that care for low-income patients are more than twice as likely to be penalized compared to hospitals that care for higher-income patients.2,5,8,9 Because of this disparity in the likelihood of being penalized, these Medicare payment programs may ultimately reduce health care resources available to residents of disadvantaged communities.6 Given that low income communities are often predominantly minority communities, value-based payment programs may have the unintended consequence of increasing racial and ethnic disparities in healthcare.
There is evidence that social risk factors – such as education, income, race/ethnicity, and employment – have an impact on health and health outcomes.1,7 In 2014, Congress passed the Improving Medicare Post-Acute Care Transformation (IMPACT) Act which required that the Office of the Assistant Secretary for Planning and Evaluation (ASPE) study the association between social risk factors and performance under existing federal payment systems and make recommendations based on their findings.7,10 The ASPE report examined the associations between healthcare outcomes and several social risk factors, such as dual enrollment in Medicare and Medicaid, residence in a low-income area, Hispanic ethnicity, Black race, and residence in a rural area. The report concluded that beneficiaries with such social risk factors had worse outcomes on several quality measures regardless of provider, and providers that served a disproportionate number of beneficiaries with these social risk factors tended to perform worse on quality of care measures – even after adjusting for beneficiary characteristics.7,10 The National Quality Forum (NQF) has recommended the inclusion of social risk factors in risk adjustment under certain conditions and the National Academies of Science, Engineering, and Medicine (NASEM) has reported on how the Centers for Medicare and Medicaid Services (CMS) could incorporate social risk factors in their reimbursement methodologies. 1,11 The NASEM report lists four primary reasons why it is important to account for social risk factors in Medicare payment programs: to reduce disparities in access, quality, and health outcomes; to improve quality and efficient care delivery for all patients; to promote fair and accurate reporting; and to compensate providers in a fair way.1,6
Section 3025 of the Affordable Care Act established the Hospital Readmissions Reduction Program (HRRP), which requires CMS to reduce payments to Inpatient Prospective Payment System (IPPS) hospitals with excess readmissions, beginning with discharges after October 1, 2012.12 Hospital penalty under HRRP is calculated using excess readmission ratios (ERRs) – a ratio of predicted-to-expected readmissions – for six program measures.13 An ERR greater than 1 is an indication that the hospital performed worse than the average performance of all hospitals.13 Using a “payment adjustment factor formula,” payment reductions were capped at 1% for FY 2013, 2% for FY 2014, and 3% for FY 2015 and beyond.13 As a result, hospitals were penalized $280 million in 2013, $227 million in 2014 and $420 in 2016.14,15 Initially, the program focused on patients admitted for acute myocardial infarction (AMI), heart failure (HF) and pneumonia. In the FY 2015, CMS expanded the applicable conditions to include patients admitted for: an acute exacerbation of chronic obstructive pulmonary disease (COPD); and elective total hip arthroplasty (THA) and total knee arthroplasty (TKA). In FY 2016, CMS included additional pneumonia diagnoses, i.e., patients with aspiration pneumonia and sepsis patients coded with pneumonia present on admission (not including severe sepsis). In FY 2017, CMS further expanded the program to include patients admitted for coronary artery bypass graft (CABG) surgery. The excess readmission calculation is based on actual readmission data from 2 to 5 years prior to the fiscal year of reference. 13
In this study, we focus on racial and ethnic composition of the hospital’s marketplace because we are interested in whether the HRRP has a negative impact on hospitals serving minority communities. We estimate the association between racial and ethnic composition of a hospital’s marketplace and its likelihood of being penalized under HRRP. We address two hypotheses: (1) the racial and ethnic composition of a hospital’s market area predicts which hospitals were penalized under HRRP, and (2) accounting for social risk factors and hospital characteristics can moderate the association between the racial and ethnic composition of a hospital’s market and the likelihood of being penalized. Adjusting the reimbursement methodology explicitly for the racial and ethnic composition of a hospital’s market may be politically problematic, therefore it is important to identify other social risk factors that moderate the association between minority communities and the likelihood of hospitals __ that serve racial and ethnic populations __ being penalized. The problem with such an approach is that it elicits notions of redlining and labeling minority patients as inherently high risk, which could be viewed as discrimination or reverse discrimination (i.e., hospitals are paid more for a minority patient than a comparable white patient).
This study contributes to the literature on the impact of HRRP in two important ways. Several previous studies have demonstrated that hospitals serving minority patients are disproportionately penalized by the HRRP, however, these studies16,17 often have limited race/ethnicity categories to Whites and Blacks. This study examines Whites, Blacks, Hispanics, Asians and persons of “other race”. In addition, studies18–20 examining hospital readmissions often define minority groups based on the racial composition of the Medicare population while this analysis examines the racial/ethnic composition of communities - providing insight into the impact of the HRRP program access to care for all patient including non-Medicare patients.
Conceptual Framework
The NASEM has provided a conceptual framework for the relationship between social risk factors and health outcomes, such as hospital readmission rates.1 This model identifies social risks and explains how they are related to health care outcomes including hospital readmissions rates.1 Social risk factors include five major domains: (1) social economic position; (2) racial, ethnic and cultural context; (3) gender; (4) social relationships; and (5) residential and community context.
Although variations in hospital quality may contribute to readmission rates, there is evidence that social risk factors, such as socioeconomic status and race may contribute to an increased risk of readmission for selected diagnosis.21 Several studies have found that patients living in high poverty neighborhoods were more likely to be readmitted than patients living in lower poverty neighborhoods.18,22–24 This suggests that despite controlling for differences in hospital practices, social risk factors such as race and socioeconomic status may impact hospital readmission rates.18,25 Failure to take social risk factors into account in the HRRP risk adjustment may lead to the penalization of hospitals that disproportionally serve populations with a greater burden of social risk factors.
Research Methods and Data
We used data published by CMS on HRRP from 2013 to 2017 to compute each hospital’s penalty status. This data was merged with data from the American Hospitals Association 2013–2015 Annual Survey of Hospitals to obtain measures of hospital characteristics, (i.e., beds, full-time equivalent employees (FTE) per adjusted admission, ownership status, teaching status, urban-rural location, and provisions of high-tech index, and community oriented services).
We used Hospital Cost Report data to compute the percentage of Medicare and Medicaid patients at each hospital. We obtained each hospital’s case-mix index from CMS. The Dartmouth Atlas of Health Care defines hospital service areas (HSA) with a crosswalk from zip codes to HSAs. For each HSA, we computed the following: the percent of residents who were White, Black, Asian, Hispanic and “other race” (defined as percent of Native American, Alaska Native and multiracial); the percent of residents 25 years and older without a high school diploma or general education diploma (GED); the percent of residents with limited English proficiency, the percent of residents living alone, and the poverty rate using data from the American Community Survey five-years survey 2011–2014. The NASEM report recommends controlling for neighborhood characteristics, and examining communities at the HSA level is one way to summarize the neighborhood characteristics of the patients being served.1
Finally, we merged data with MMCO Statistical & Analytic Reports to include dual eligible Medicare and Medicaid beneficiaries. Maryland hospitals were excluded because they do not participate in the CMS inpatient prospective payment system. We required hospitals have complete data for all five years, and our final sample included 3,168 hospitals per year.
Analysis
We used bivariate and multivariate analyses to determine if hospital penalty status is associated with the percentage of minority residents in the HSA. We also used unpaired t-test to compare penalized versus non-penalized hospitals. The base model includes only percentages of residents in the HSA who are Asian, Black, Hispanic and other race. The final model also includes hospital characteristics, HSA-level social risk factors and state level fixed effects. The analysis adjusts for factors such as hospital size, ownership type, and teaching categories in order to compare hospitals to their peers based on hospital characteristics – not just in absolute terms. This approach is suggested by the NASEM report that recommends adjusting for risk factors by peer groups.1 We estimated the models using GLM specifying a binomial distribution and logit link function. We weighted each observation by its squared adjusted admissions to correct for heteroscedasticity associated with size. All the models were estimated using STATA 14 and RStudio was used to map the data. We report the predicted probabilities and marginal effects for each independent variable instead of odds ratios because two thirds of the hospitals were penalized under the HRRP. The models were estimated separately for each year because HRRP payment penalties and the number of conditions included in the penalty calculation increased from 2013 to 2017.
Results
Table 1 compares penalized and non-penalized hospitals by the racial and ethnic composition of the hospital service area, hospital characteristics, and social risk factors in 2013 and 2017. Compared to non-penalized hospitals, hospitals in HSAs with higher proportions of Black, Asian and “other race” residents were more likely to be penalized in 2013 and 2017, and hospitals in HSAs with a high proportion of White residents were less likely to be penalized in 2013. In both years, penalized hospitals were larger on average, more likely to be teaching hospitals, served a higher proportion of Medicaid patients, provided more high tech and community oriented services and had lower average case-mix. In 2017, hospitals in urban or rural areas were more likely to be penalized. In 2013, hospitals were more likely to be penalized if they were serving communities with a higher proportion of: adult residents without a high school diploma or GED, individuals with limited English proficiency, residents living below the federal poverty level or if they were serving communities with a lower proportion of adult residents with a 4-year college degree. These patterns of associations did not change in 2017 although the associations were not statistically significant for the HSA characteristics of limited English proficiency and living below the federal poverty level.
Table 1:
Comparing Penalized and Non-Penalized Hospitals, 2013 and 2017
| Hospital Penalized Status | ||||||
|---|---|---|---|---|---|---|
| 2013 | 2017 | |||||
| Penalized | Non-Penalized | Penalized | Non-Penalized | |||
| Control Variables | Mean/SD | Mean/SD | p-value | Mean/SD | Mean/SD | p-value |
| Racial Composition at Hospital Service Areas (HSAs) | ||||||
| Percent Non-White (HSA level) | 0.307 | 0.269 | 0.000*** | 0.297 | 0.285 | 0.252 |
| (0.226) | (0.210) | (0.221) | (0.222) | |||
| Percent White | 0.693 | 0.731 | 0.000*** | 0.703 | 0.715 | 0.252 |
| (0.226) | (0.210) | (0.221) | (0.222) | |||
| Percent Black | 0.115 | 0.077 | 0.000*** | 0.108 | 0.080 | 0.000*** |
| (0.136) | (0.111) | (0.132) | (0.117) | |||
| Percent Hispanic | 0.125 | 0.122 | 0.597 | 0.123 | 0.130 | 0.288 |
| (0.160) | (0.151) | (0.156) | (0.163) | |||
| Percent Asian | 0.034 | 0.027 | 0.000*** | 0.033 | 0.028 | 0.031* |
| (0.059) | (0.050) | (0.057) | (0.053) | |||
| Percent Other Race | 0.033 | 0.043 | 0.001*** | 0.033 | 0.047 | 0.002** |
| (0.065) | (0.089) | (0.063) | (0.108) | |||
| Hospital Characteristics | ||||||
| Hospital Size | ||||||
| Total Hospital Beds | 237.200 | 173.800 | 0.000*** | 235.100 | 135.800 | 0.000*** |
| (218.000) | (189.400) | (217.000) | (160.500) | |||
| Adjusted admission | 20,829 | 15,919 | 0.000*** | 20,818 | 12,355 | 0.000*** |
| (18,478) | (16,163) | (18,244) | (14,404) | |||
| FTE per Adjusted Admission | 18.210 | 17.670 | 0.129 | 18.160 | 17.480 | 0.216 |
| (7.012) | (10.560) | (6.734) | (13.160) | |||
| Ownership type | ||||||
| Non-for-profit (=1; if Yes) | 0.615 | 0.592 | 0.223 | 0.624 | 0.536 | 0.000*** |
| (0.487) | (0.492) | (0.484) | (0.499) | |||
| For Profit (=1; if Yes) | 0.231 | 0.250 | 0.241 | 0.226 | 0.284 | 0.003** |
| (0.421) | (0.433) | (0.418) | (0.451) | |||
| Public (=1; if Yes) | 0.155 | 0.158 | 0.795 | 0.150 | 0.179 | 0.087 |
| (0.362) | (0.365) | (0.357) | (0.384) | |||
| Teaching Categories (Non-Teaching (Ref.)) | ||||||
| Non-Teaching (≤0.25) | 0.561 | 0.716 | 0.000*** | 0.588 | 0.721 | 0.000*** |
| (0.496) | (0.451) | (0.492) | (0.449) | |||
| Minor-Teaching (≤0.25) | 0.341 | 0.254 | 0.000*** | 0.328 | 0.244 | 0.000*** |
| (0.474) | (0.436) | (0.470) | (0.430) | |||
| Major Teaching (>0.25) | 0.098 | 0.030 | 0.000*** | 0.084 | 0.036 | 0.000*** |
| (0.297) | (0.170) | (0.278) | (0.185) | |||
| Percentage of Discharges | ||||||
| Medicaid | 0.130 | 0.115 | 0.000*** | 0.129 | 0.112 | 0.002** |
| (0.110) | (0.117) | (0.108) | (0.127) | |||
| Medicare | 0.360 | 0.349 | 0.040* | 0.357 | 0.351 | 0.419 |
| (0.124) | (0.143) | (0.120) | (0.168) | |||
| Location (=1; if Urban) | ||||||
| Urban | 0.904 | 0.922 | 0.080 | 0.916 | 0.884 | 0.021* |
| (0.295) | (0.269) | (0.277) | (0.321) | |||
| Rural | 0.097 | 0.078 | 0.080 | 0.084 | 0.116 | 0.021* |
| (0.295) | (0.269) | (0.277) | (0.321) | |||
| Other (After imputing Missing) | ||||||
| Hi-Tech Services Index | 9.901 | 8.922 | 0.000*** | 9.967 | 7.933 | 0.000*** |
| (4.536) | (4.698) | (4.536) | (4.577) | |||
| Hospital Community Index | 5.541 | 5.038 | 0.000*** | 5.500 | 4.840 | 0.000*** |
| (1.737) | (2.066) | (1.781) | (2.120) | |||
| Case Mix Index | 1.467 | 1.566 | 0.000*** | 1.493 | 1.534 | 0.034* |
| (0.276) | (0.399) | (0.282) | (0.465) | |||
| Social Risk Factor Variables (2011–2014) | ||||||
| Education | ||||||
| Percent 25yrs/older -No diploma | 0.152 | 0.138 | 0.000*** | 0.149 | 0.143 | 0.057 |
| (0.073) | (0.067) | (0.071) | (0.071) | |||
| Percent 25yrs/older-High School | 0.315 | 0.311 | 0.213 | 0.316 | 0.306 | 0.006** |
| (0.088) | (0.087) | (0.088) | (0.085) | |||
| Percent 25yrs/older −4 years College & more | 0.531 | 0.550 | 0.000*** | 0.534 | 0.551 | 0.002** |
| (0.126) | (0.116) | (0.124) | (0.118) | |||
| Demographic | ||||||
| Limited English proficiency | 0.064 | 0.053 | 0.000*** | 0.061 | 0.057 | 0.199 |
| (0.078) | (0.063) | (0.075) | (0.069) | |||
| Living alone | 0.112 | 0.110 | 0.052 | 0.111 | 0.112 | 0.405 |
| (0.035) | (0.033) | (0.034) | (0.035) | |||
| Economic | ||||||
| Percent Persons 65+ Below Poverty | 0.096 | 0.086 | 0.000*** | 0.093 | 0.090 | 0.045* |
| (0.041) | (0.036) | (0.040) | (0.040) | |||
| Ratio of Dual (Medicare –Medicaid Enrolles) to POP 65+ | 0.271 | 0.242 | 0.000*** | 0.264 | 0.248 | 0.000*** |
| (0.110) | (0.0957) | (0.107) | (0.103) | |||
| Number of Dual (Medicare –Medicaid Enrolles) | 32,698.5 | 21,191.7 | 0.000*** | 29,753.8 | 24,773.4 | 0.112 |
| (74,722.1) | (59,125.4) | (70,310.2) | (68,650.4) | |||
| N | 2,094 | 1,074 | 3,168 | 2,549 | 619 | 3,168 |
SOURCES: Authors’ Analysis from the; Hospital Cost report-2014, AHA Annual Survey of Hospitals −2014, ACS-2011–2014, CMI2014, HHS-2014–2015; arf.hrsa.gov and Readmissions Reduction Program Medicare-2013–2017 & CMS-MMCO-2013–2015
Notes:
Parentheses present the Std. Dev.
Bonferroni correction (a = 0.05; 2013~0.0024 & 2017~0.0025) employed to determine the statistical differences in means between penalized and non-penalized hospitals.
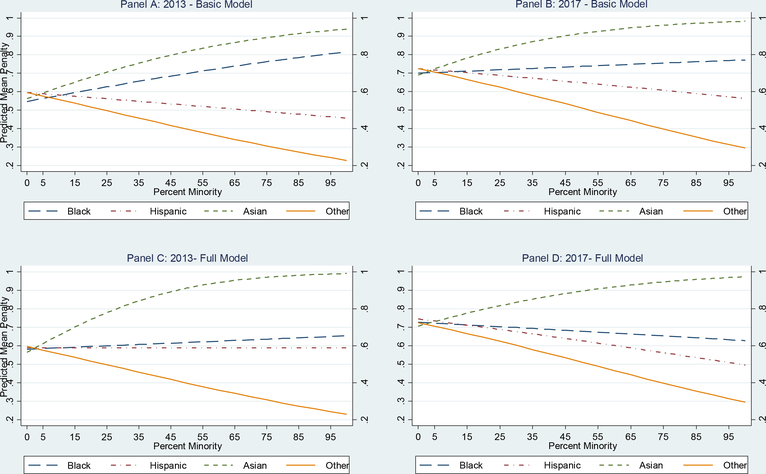
The association between the likelihood of being penalized and the proportion of minorities in the HSA varied by racial and ethnic group. Figure 1 reports the unadjusted (basic model) and adjusted (full model) association between the likelihood of a hospital in a HSA being penalized and the proportion of minorities in the HSA for each racial and ethnic group ranging from 0 to 100. In the basic model for both 2013 and 2017, as the percentage of Blacks and Asians residing in the HSA increased, the likelihood of a hospital in that HSA being penalized also increased. As the proportion of Black or Asian residents in the HSA increased from 5 to 95 percent, the likelihood of a hospital in the HSA being penalized increased from 0.56 to 0.81 (for percent Black residents) and 0.59 to 0.93 (for percent Asian residents) in 2013, and from 0.70 to 0.77 (for percent Black residents) and 0.72 to 0.98 (for percent Asian residents) in 2017. In the basic models for 2013 and 2017, the percent of Hispanic and other race residents in the HSA had a different association with the likelihood of being penalized. As the percent of Hispanic and other race residents in the HSA increased from 5 to 95 percent, the likelihood of being penalized declined from 0.59 to 0.46 (for percent Hispanic residents) and 0.58 to 0.24 (for percent other race residents) in 2013 and from 0.72 to 0.57 (for percent Hispanic residents) and 0.71 to 0.31 (for present other race residents) in 2017.
Figure 1.
The Association between Percent of Minority Residents in the HSA and the Likelihood of Being Penalized, 2013 and 2017
Note: This is the predicted probability of being penalized from GLM logistic models, changing the percent of minority’s resident at HSA level from 0–100. The dependent variable is penalized status and independent variables are percent of each minority groups.
As the proportion of Black or Asian residents in the HSA increased from 5 to 95 percent in the full model for 2013, the likelihood of a hospital in the HSA being penalized increased from 0.59 to 0.65 (for percent Black residents) and from 0.61 to 0.99 (for percent Asian residents) in 2013.However,in contrast to the basic model, in the multivariate analyses - when socioeconomic variables such as poverty or education status are included-the significant effect disappears for the Black population. This suggest that these socioeconomic factors mediate the effect of Black race, a finding that has been noted in prior research.26
As the proportion of Hispanic residents increases in this model, we see almost no change in the likelihood of hospital penalty - as the proportion of Hispanic residents increases from 5 to 95 percent, the likelihood of a hospital being penalized remained at 0.59. However, an increase in the proportion of the other race category is negatively associated with a likelihood of hospital penalty – as the proportion of other race residents increases from 5 percent to 95 percent, the likelihood decreases from 0.58 to 0.24. In panel D we see the likelihood of a hospital in the HSA being penalized decreased from 0.72 to 0.63 (for percent Black residents) and increased from 0.73 to 0.97 (for percent Asian residents). For the full model in 2017 as the percent of Hispanic and other race residents in the HSA increased from 5 to 95 percent, the likelihood of being penalized declined from 0.73 to 0.51 (for percent Hispanic residents) and 0.71 to 0.31 (for percent other race residents).
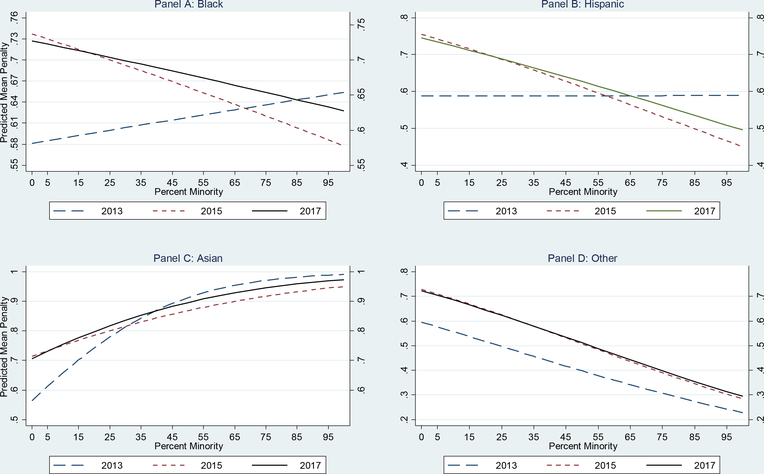
The four panels in Figure 2 display the association between the likelihood of a hospital being penalized and the increase in percent of minority residents in the HSA in 2013, 2015 and 2017 using the full GLM logistic model. Panel A in Figure 2 shows that the likelihood of a hospital in an HSA being penalized increased as the percent of the Black residents increased in 2013, but decreased in years 2015 and 2017. Panel B displays a similar decreasing trend in years 2015 and 2017 for the Hispanic population, but in 2013 as the proportion of Hispanic residents increased there was almost no change in the likelihood of a hospital being penalized.
Figure 2:
Association between Percent Minority Group Residents at HSA level and the Likelihood of Being Penalized, by Racial/Ethnic Group for 2013, 2015 and 2017
Note: This is the predicted probability of being penalized from GLM logistic full models, changing the percent of minority’s resident at HSA level from 0–100. The dependent variable is penalized status and independent variables are percent of each minority groups.
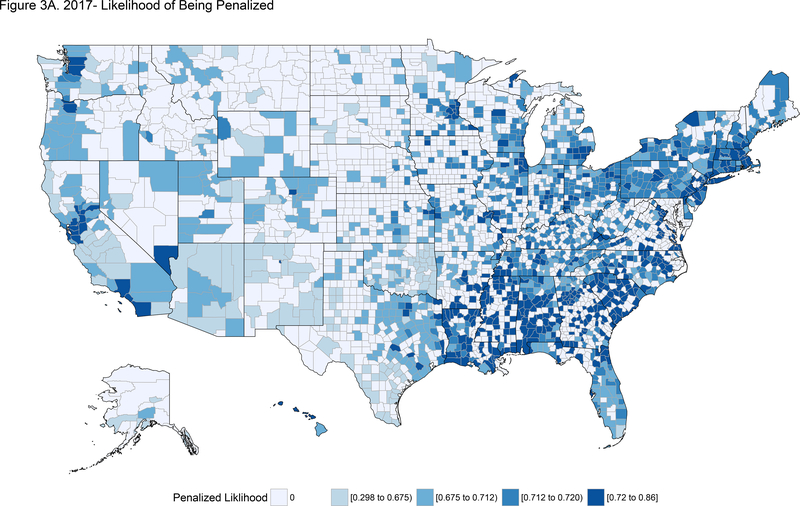
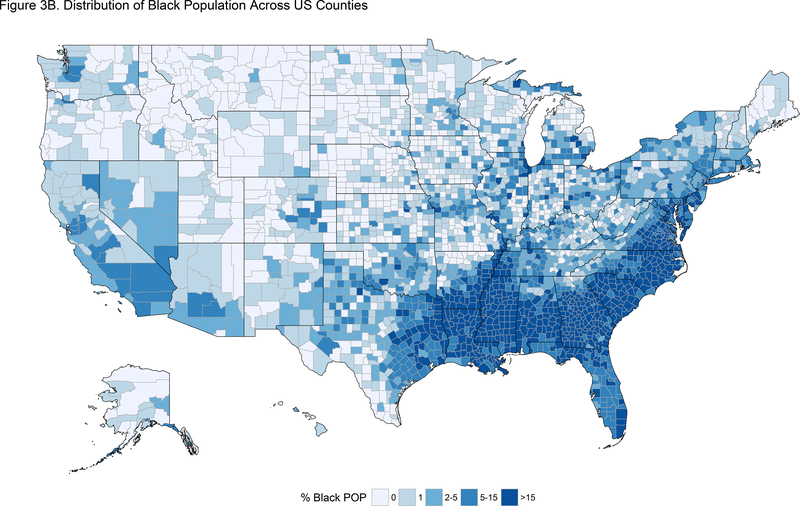
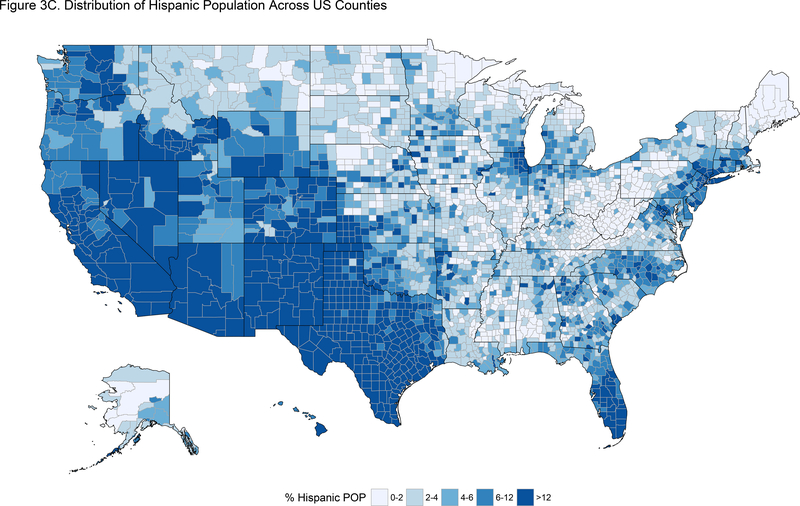
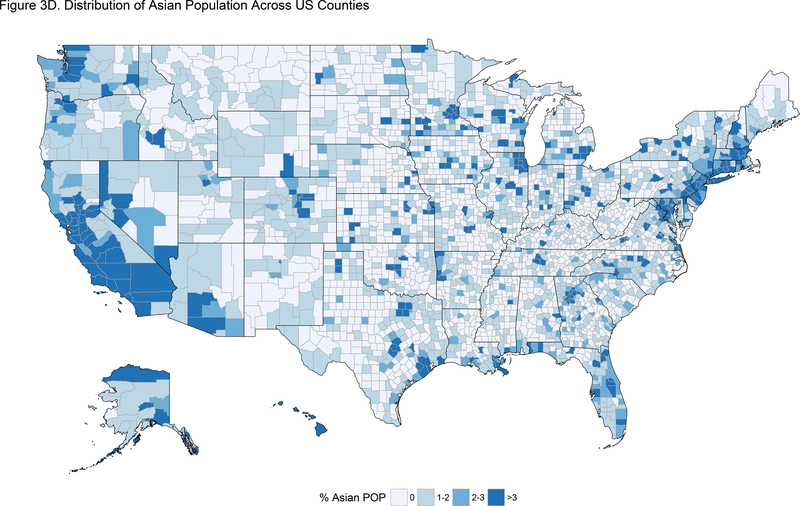
The four maps in Figure 3 display the association between the likelihood of a hospital being penalized in 2017 and percent of minority residents at the county level including Black, Hispanic and Asian populations. As presented in Figure 3A, hospitals located in counties in Northeast, Southeast and West Coast were more likely to be penalized in 2017. This corresponds to counties with the highest percentages of Black and Asian residents (See Figure 3B and 3D.) However, hospitals located in the Southwest were least likely to be penalized, corresponding to counties with highest percentages of Hispanic population (See Figure 3C.) The geographic association for Black and Hispanics residents and the likelihood of being penalized is fairly clear. However, the association between Asian residents and the likelihood of being penalized is not as straightforward. This is probably due to diversity within Asians which include subgroups with vastly different economic status, educational attainment, health insurance coverage and English proficiency.
Figure 3.
Comparing Distribution of Percent Minority Group Residents (Black, Hispanic and Asian) at County level and the Likelihood of Being Penalized, 2017
In Table 2, we display the marginal effects for each independent variable in the full model, which includes race/ethnicity, hospital characteristics, and social risk factor variables for the years 2013 and 2017. We find that after controlling for hospital characteristics and other social risk factors, there is still an association between the percent Hispanic and Asian in an HSA and the likelihood of a hospital being penalized in 2013, and an association between the percent Hispanic, percent Asian and percent other race in an HSA and the likelihood of a hospital being penalized in 2017. Table 2 also shows that larger hospitals and minor teaching hospitals were more likely to be penalized, as were hospitals with more Medicaid and Medicare patients. Hospitals with more hi-tech services and community oriented services were more likely to be penalized under the HRRP during both years. Urban hospitals were less likely to be penalized in 2013 and hospitals with a higher case mix index were less likely to be penalized in 2013 and 2017. We also found that hospitals in HSAs with a high proportion of adults with no high school diploma were more likely to be penalized in both years. However, surprisingly, hospitals in HSAs with a higher proportion of persons living below the federal poverty level were less likely to be penalized for both years. Hospitals serving communities with a greater proportion of people living alone were less likely to be penalized in 2017. Lastly, in 2013 we found that hospitals in HSAs with a higher proportion of dual eligible individuals - those enrolled in both Medicare and Medicaid - were more likely to be penalized. Similar results were found when we estimated the models using modified Poisson regression.
Table 2:
The Marginal Effect of Hospital Characteristics on HRRP Penalty, 2013 and 2017
| 2013 | 2017 | |||
|---|---|---|---|---|
| Control Variables | dy/dx | St. Err | dy/dx | St. Err |
| Racial Composition at Hospital Service Areas (HSAs); Ref, White | ||||
| Percent Black | 0.0531 | (0.0785) | −0.101 | (0.0672) |
| Percent Hispanic | 0.0283 | (0.1373) | −0.2155* | (0.1051) |
| Percent Asian | 0.9423*** | (0.2840) | 0.5256* | (0.2353) |
| Percent Other Race | −0.1382 | (0.0960) | −0.2268** | (0.0759) |
| Hospital Characteristics | ||||
| Hospital Size | ||||
| Total Hospital Beds | 0.0003*** | (0.0001) | 0.0006*** | (0.0001) |
| FTE per Adjusted Admission | 0.0125*** | (0.0012) | 0.0133*** | (0.0011) |
| Ownership type | ||||
| For Profit (=1; if Yes) | −0.0089 | (0.0203) | 0.012 | (0.0183) |
| Public (=1; if Yes) | −0.0860*** | (0.0231) | −0.0655*** | (0.0190) |
| Teaching Categories (Non-Teaching (Ref.)) | ||||
| Minor-Teaching (≤0.25) | 0.1050*** | (0.0196) | 0.0428* | (0.0184) |
| Major Teaching (>0.25) | 0.2885*** | (0.0603) | 0.0157 | (0.0503) |
| Percentage of Discharges | ||||
| Medicaid | 0.2554** | (0.0833) | 0.3648*** | (0.0733) |
| Medicare | 0.1621** | (0.0597) | 0.1081* | (0.0503) |
| Location (=1; if Urban) | ||||
| Urban | −0.0625* | (0.0263) | 0.0103 | (0.0211) |
| Other variables | ||||
| Hi-Tech Services Index | 0.0098*** | (0.0029) | 0.0150*** | (0.0025) |
| Hospital Community Index | 0.0199*** | (0.0050) | 0.0140** | (0.0043) |
| Case Mix Index | −0.2226*** | (0.0269) | −0.1104*** | (0.0220) |
| Social Risk Factor Variables | ||||
| Education | ||||
| Percent 25yrs/older -No Diploma | 0.5026** | (0.1723) | 0.4370** | (0.1570) |
| Demographic | ||||
| Limited English proficiency | −0.1923 | (0.3488) | 0.1363 | (0.2747) |
| Living alone | 0.0402 | (0.2543) | −0.4985* | (0.1961) |
| Economics | ||||
| Percent Persons 65+ Below Poverty | −0.1852 | (0.2429) | 0.3516 | (0.2105) |
| Number of Dual (Medicare –Medicaid Enrollees)/1000 | 0.0005** | (0.0002) | 0.0001 | (0.0001) |
| N | 3,161 | 3,161 | ||
SOURCES: Authors’ Analysis from the: Hospital Cost report-2014, AHA Annual Survey of Hospitals −2014, ACS-2011–2014, CMI2014, HHS-2014–2015; arf.hrsa.gov and Readmissions Reduction Program Medicare-2013–2017, CMS-MMCO-2013–2015
p<0.05
p<0.01
p<0.001
Notes:
Based on GLM logistic regression, marginal effects evaluated at the mean of predictor variables, with std. err. in parentheses.
We estimated separate models for each year.
We included all States and DC except Maryland.
Models included state fix effect with reference of California.
The tertiary-high tech services index listed the specialty services the hospital provided from a list of 27 items: Shaped beam radiation system, burn care, computed-tomography (CT) scanner, adult cardiac surgery, electron beam computed tomography (EBCT), extracorporeal shock waved lithotripter (ESWL), full-field digital mammography, heart transplant, image-guided radiation therapy, intensity-modulated radiation therapy (IMRT), kidney transplant, liver transplant, lung transplant, magnetic resonance imaging (MRI), multislice spiral computed tomography < 64 slice, neonatal intensive care, bone marrow transplant services, other transplant, positron emission tomography/CT (PET/CT), positron emission tomography (PET), proton beam therapy, robotic surgery, single photon emission computerized tomography (SPECT), stereotactic radiosurgery, tissue transplant, certified trauma center and ultrasound hospitals.
Community index is the sum of 11 community services provided by hospitals such as community outreach, health fair, community health education, health screenings, immunization program, indigent care clinic, linguistic/translation services, meals on wheels, mobile health services, teen outreach services, and rural health clinic hospitals.
Discussion
This study examines the association between the racial and ethnic composition of a HSA and a hospital’s likelihood of being penalized under the HRRP. There is growing concern that the lack of risk adjustment for social risk factors in value-based payment programs, such as the HRRP, may lead to disproportionate penalties for minority-serving hospitals and hospitals that primarily treat low-income patients.8,27–30 A recent national survey of hospital leaders found that the most commonly endorsed critique of the HRRP was that the program does not adjust for social risk factors – more than 75% of hospital leaders reported this lack of adjustment as a critical issue.4 Several previous studies have found that safety net hospitals are more likely to be penalized under the HRRP.5,8,31
Our study shows that a hospital’s likelihood of being penalized increased as the share of Black and Asian residents increased in the hospital’s HSA, yet this was not true for the percent of Hispanic residents. This may in part be due to the “Hispanic paradox” – the idea that although Hispanics have lower socioeconomic status and higher rates of being uninsured, they have lower overall mortality rates and longer life expectancy compared to both Blacks and Whites.32 Hospitals in HSAs with higher proportions of Hispanic residents may be more culturally competent and may implement policies and procedures that better serve the Hispanic population. An additional explanation may be that because as a group Hispanics have higher rates of being uninsured, they therefore have lower rates of readmissions.33 A study examining the relationship among the insurance status, race and the likelihood of readmission found that lower readmission rates could result from a lack of health insurance and poor access to health care, especially among minority populations.33 The lack of health insurance coverage may also explain the negative association between likelihood of being penalized and the proportion of population that are defined as “other race”. This category includes Native American, Alaska Native and multiracial and there is evidence that Native Americans and Alaska Native populations have high rates of uninsurance and significant barriers to obtaining care.34
The finding regarding the increase in the likelihood of penalty for the Asian population may be due to a number of factors. The Asian population is the fastest growing racial group in the United States, and historical aggregation of subgroups has distorted the understanding of disease burden and mortality patterns among this population.35–37 Some studies have found that compared to non-Hispanic Whites, the proportionate mortality burden of hypertensive heart diseases and cerebrovascular disease is higher among the Asian-American population.36 In addition, there is evidence that certain subgroups of the Asian population may have a higher risk of readmissions compared to Whites and this in part may be due to language barriers and poor medical adherence.37–39 In this study, HSAs with a high proportion of the Asian residents are more likely to have higher excess readmissions for HF and AMI between 2013–2017. It is possible that HSAs with large Asian populations have a large proportion of certain Asian subgroups, and that the associated likelihood of high readmissions is due to the health outcomes of those subpopulations. Regarding the findings for the Black communities, several studies have shown that compared to White Medicare beneficiaries, Black Medicare patients are more likely to be readmitted.19,40,41
The large positive association between a hospital’s penalty status and the share of hospital discharges covered by Medicaid suggests that it is important to provide Medicaid beneficiaries with appropriate wrap around services (e.g. care coordination) to reduce the likelihood of readmissions. Medicaid beneficiaries may not receive adequate post-discharge services because of Medicaid’s low reimbursement for non-hospital follow-up services.42,43 In addition, efforts could be made to link discharged Medicaid beneficiaries with social services and community-based agencies that address social determinants of health, such as housing, employment, and food security. However, social services departments and community-based organizations have limited funds and large populations to serve and therefore may not be able to serve Medicaid beneficiaries who have been discharged without additional resources.44,45 The association between penalized hospitals and the provision of community oriented and high tech services functions as a risk adjuster due to the fact that hospitals that provide these services may attract patients with a higher risk profile which is otherwise not captured in the model.
Information about the dual eligible population was included as an adjustment in the model as there is evidence that it is an indicator of worse outcomes and greater resource use because it reflects the lower incomes of Medicaid recipients.6 In fact, the ASPE Report to Congress cited dual enrollment status as the most powerful predictor of poor health outcomes.7,10
The association we find between low educational attainment and the likelihood of a hospital being penalized supports the NASEM conclusion that health literacy is an important determinant of health care outcomes.1 In addition, previous studies provide evidence to support the relationship between educational attainment and health literacy.46–49 Interventions that address health literacy may help reduce avoidable hospital readmission.
Limitations
One limitation of this study is that it includes the racial and ethnic composition of a hospital’s HSA as opposed to the hospital itself. This was done in part because this is a national study (our analysis includes all states except for Maryland) and data on the racial and ethnic composition of HSAs was available for every state, whereas data for the racial and ethnic composition of hospital patients is only available for a subset of states. To validate our approach, we conducted a sensitivity analysis comparing the percent of racial and ethnic minorities in the HSAs to the percent of racial and ethnic minorities discharged in hospitals in 11 states in 2013. We found the correlation between the racial/ethnic composition of the HSA compared to the hospital was 80%. In addition, we chose to use racial/ethnic composition of the HSAs minimize the possible endogeneity between the racial and ethnic composition of the hospitals’ patients and the likelihood of being penalized. Hospitals are able to influence the racial and ethnic composition of their patient population, they may decide not to avoid serving certain patients with certain social risk factors. This study is interested in impact on access to care, therefore if hospitals in certain HSAs are disproportionately penalized then geographic access to care all of the residents within those communities may be affected. Also, using the HSA allows us to consider hospitals from the entire nation and all payer groups not just Medicare. All-payer administrative data with race and ethnic information are only available for a subset of states. Medicare data while available nationally only has the racial and ethnic composition of Medicare beneficiaries which contains disproportionately more Black and White patients and fewer Hispanic, Asian and other race patients.
Conclusions
This study focuses on the association between the racial and ethnic composition of the HSA and a hospital’s likelihood of being penalized. Incorporating social risk factors in reimbursement methodology of Medicare’s HRRP may reduce the impact of the program on hospitals serving minority communities. However, even with risk adjustment, hospitals that serve a larger percentage of Medicare and Medicaid patients and are in HSAs with a large proportion of residents with low educational attainment are at greater risk of being penalized.
Acknowledgments
This research was support by a grant number P60MD00214 from NIMHD
Footnotes
The authors have no conflicts of interest to report.
Contributor Information
Darrell J Gaskin, Johns Hopkins Bloomberg School of Public Health, William C. and Nancy F. Richardson Professor in Health Policy, Department of Health Policy and Management, Director of the Johns, Hopkins Center for Health Disparities Solutions, 624 North Broadway Ave, Hampton, House, Suite #441, Baltimore, Maryland, 21205, United States, dgaskin1@jhu.edu.
Hossein Zare, Johns Hopkins Bloomberg School of Public Health, Department of Health Policy and Management, Johns Hopkins Center for Health Disparities Solutions, University of Maryland University College, Health Services Management, 624 North Broadway Ave, Hampton House, Room #310, Baltimore, Maryland, 21205, United States., Phone: +1 410-614-7246, hzare1@jhu.edu.
Roza Vazin, Johns Hopkins Bloomberg School of Public Health, Department of Health Policy and Management, 624 North Broadway Ave, Hampton House, Room #307, Baltimore, Maryland, 21205, United States., rvazin1@jhu.edu.
DeJa Love, CareFirst BlueCross BlueShield, dejamlove@gmail.com.
Donald Steinwachs, Johns Hopkins Bloomberg School of Public Health, Department of Health Policy and Management, 624 North Broadway Ave, Hampton House, Baltimore, Maryland, 21205, United States., dsteinwachs@jhu.edu.
References
- 1.National Academies of Sciences, Engineering and Medicine. Accounting for Social Risk Factors in Medicare Payment: Identifying Social Risk Factors. Washington D.C: National Academies Press. doi: 10.17226/23635. https://www.nap.edu/read/23635/. Accessed March 13, 2018. [DOI] [Google Scholar]
- 2.Fuller RL, Atkinson G, Hughes JS. Indications of biased risk adjustment in the hospital readmission reduction program. J Ambul Care Manage 2015;38:39–47. [DOI] [PubMed] [Google Scholar]
- 3.DuGoff E, Bishop S, Rawal P. Hospital Readmission Reduction Program Reignites Debate Over Risk Adjusting Quality Measurse. Health Affairs Blog https://www.healthaffairsorg/do/101377/hblog20140814040725/full/ Updated August 14 2014 Accessed March 13, 2018.
- 4.Joynt KE, Figueroa JE, Oray J, Jha AK. Opinions on the Hospital Readmission Reduction Program: results of a national survey of hospital leaders. Am J Manag Care 2016;22:e287–94. [PMC free article] [PubMed] [Google Scholar]
- 5.Boozary AS, Manchin J 3rd, Wicker RF. The Medicare Hospital Readmissions Reduction Program: Time for Reform. JAMA 2015;314:347–8. [DOI] [PubMed] [Google Scholar]
- 6.Buntin MB, Ayanian JZ. Social Risk Factors and Equity in Medicare Payment. N Engl J Med 2017;376:507–10. [DOI] [PubMed] [Google Scholar]
- 7.Department of Health and Human Services, Office of the Assistant Secretary of Planning and Evaluation. Report to Congress: Social Risk Factors and Performance under Medicare’s Value-based Payment Programs. https://aspe.hhs.gov/system/files/pdf/253971/ASPESESRTCfull.pdf. Updated December 2016 Accesses March 13 2018.
- 8.Gilman M, Adams EK, Hockenberry JM, Wilson IB, Milstein AS, Becker ER. California safety-net hospitals likely to be penalized by ACA value, readmission, and meaningful-use programs. Health Aff (Millwood) 2014;33:1314–22. [DOI] [PubMed] [Google Scholar]
- 9.McHugh M, Kang R, Hasnain-Wynia R. Understanding the safety net: inpatient quality of care varies based on how one defines safety-net hospitals. Med Care Res Rev 2009;66:590–605. [DOI] [PubMed] [Google Scholar]
- 10.Joynt KE, De Lew N, Sheingold SH, Conway PH, Goodrich K, Epstein AM. Should Medicare Value-Based Purchasing Take Social Risk into Account? N Engl J Med 2017;376:510–3. [DOI] [PubMed] [Google Scholar]
- 11.Fiscella K, Burstin HR, Nerenz DR. Quality measures and sociodemographic risk factors: to adjust or not to adjust. Jama 2014;312:2615–6. [DOI] [PubMed] [Google Scholar]
- 12.Counsel OotL. Complication of patinet Protection and Affordable Care Act, Patient Protection and Affordable Act (Health related Portion of the Health Care and Education Reconcilation Act of 2010) Part 2: National Stratehy to Improve Health Care Quality, Sections 3011 and 3502,. U.S. House of representatives: Office of the Legislative Counsel, USA; 2010. [Google Scholar]
- 13.CMS. Readmissions Reduction Program (HRRP). Department of Health and Human Services, Centers for Medicare & Medicaid Services; at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html Updated April 28, 2018 Accessed June 18, 2018. [Google Scholar]
- 14.CMS. Federal register, Vol 77, No. 170 (August, 2012). Department of Health and Human Services, Centers for Medicare & Medicaid Services; https://www.gpo.gov/fdsys/pkg/FR-2012-08-31/pdf/2012-19079.pdf. Updated August 31, 2012 Accessed March 13, 2018. [Google Scholar]
- 15.CMS. Federal register, Vol 80, No. 158. Pages 49325–49886 (August, 2015). Department of Health and Human Services, Centers for Medicare & Medicaid Services; https://www.gpo.gov/fdsys/pkg/FR-2015-08-17/pdf/2015-19049.pdf. Updated August 17, 2015 Accessed March 13, 2018.26292371 [Google Scholar]
- 16.Figueroa JF, Zheng J, Orav EJ, Epstein AM, Jha AK. Medicare Program Associated With Narrowing Hospital Readmission Disparities Between Black And White Patients. Health Aff (Millwood) 2018;37:654–61. [DOI] [PubMed] [Google Scholar]
- 17.Mellor J, Daly M, Smith M. Does It Pay to Penalize Hospitals for Excess Readmissions? Intended and Unintended Consequences of Medicare’s Hospital Readmissions Reductions Program. Health Econ 2017;26:1037–51. [DOI] [PubMed] [Google Scholar]
- 18.Hu J, Gonsahn MD, Nerenz DR. Socioeconomic status and readmissions: evidence from an urban teaching hospital. Health Aff (Millwood) 2014;33:778–85. [DOI] [PubMed] [Google Scholar]
- 19.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA 2011;305:675–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGarry BE, Blankley AA, Li Y. The Impact of the Medicare Hospital Readmission Reduction Program in New York State. Med Care 2016;54:162–71. [DOI] [PubMed] [Google Scholar]
- 21.Casillas CB. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program. Washington DC: Henry J Kaiser Family Foundation 2016. [Google Scholar]
- 22.Kind AJ, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med 2014;161:765–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herrin J, St Andre J, Kenward K, Joshi MS, Audet AM, Hines SC. Community factors and hospital readmission rates. Health Serv Res 2015;50:20–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes 2011;4:53–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McHugh MD, Carthon JM, Kang XL. Medicare readmissions policies and racial and ethnic health disparities: a cautionary tale. Policy Polit Nurs Pract 2010;11:309–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bikdeli B, Wayda B, Bao H, et al. Place of residence and outcomes of patients with heart failure: analysis from the telemonitoring to improve heart failure outcomes trial. Circulation: Cardiovascular Quality and Outcomes 2014;7:749–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. Jama 2011;306:1688–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Calvillo–King L, Arnold D, Eubank KJ, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. Journal of general internal medicine 2013;28:269–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilman M, Hockenberry JM, Adams EK, Milstein AS, Wilson IB, Becker ER. The Financial Effect of Value-Based Purchasing and the Hospital Readmissions Reduction Program on Safety-Net Hospitals in 2014: A Cohort Study. Ann Intern Med 2015;163:427–36. [DOI] [PubMed] [Google Scholar]
- 30.Glance LG, Kellermann AL, Osler TM, Li Y, Li W, Dick AW. Impact of Risk Adjustment for Socioeconomic Status on Risk-adjusted Surgical Readmission Rates. Ann Surg 2016;263:698–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA 2013;309:342–3. [DOI] [PubMed] [Google Scholar]
- 32.McCarthy M CDC report confirms “Hispanic paradox”. BMJ 2015;350:h2467. [DOI] [PubMed] [Google Scholar]
- 33.Basu J, Hanchate A, Bierman A. Racial/Ethnic Disparities in Readmissions in US Hospitals: The Role of Insurance Coverage. Inquiry 2018;55:46958018774180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Artiga S, Arguello R, Duckett P Health Coverage and Care for American Indians and Alaska Natives. https://www.kff.org/disparities-policy/issue-brief/health-coverage-and-care-for-american-indians-and-alaska-natives/. Updated October 2013 Accessed July 25, 2018.
- 35.Brown AUS Hispanic and Asian populations growing, but for different reasons. http://www.pewresearch.org/fact-tank/2014/06/26/u-s-hispanic-and-asian-populations-growing-but-for-different-reasons/. Updated July 17, 2014 Accessed March 13, 2018.
- 36.Jose PO, Frank AT, Kapphahn KI, et al. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol 2014;64:2486–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sentell T, Ahn HJ, Miyamura J, Taira DA. Thirty-Day Inpatient Readmissions for Asian American and Pacific Islander Subgroups Compared With Whites. Med Care Res Rev 2018;75:100–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nakagawa K, Ahn HJ, Taira DA, Miyamura J, Sentell TL. Ethnic Comparison of 30-Day Potentially Preventable Readmissions After Stroke in Hawaii. Stroke 2016;47:2611–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Karliner LS, Kim SE, Meltzer DO, Auerbach AD . Influence of language barriers on outcomes of hospital care for general medicine inpatients. J Hosp Med 2010;5:276–82. [DOI] [PubMed] [Google Scholar]
- 40.Tsai TC, Orav EJ, Joynt KE. Disparities in surgical 30-day readmission rates for Medicare beneficiaries by race and site of care. Ann Surg 2014;259:1086–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Girotti ME, Shih T, Revels S, Dimick JB. Racial disparities in readmissions and site of care for major surgery. J Am Coll Surg 2014;218:423–30. [DOI] [PubMed] [Google Scholar]
- 42.DeLia D, Tong J, Gaboda D, Casalino LP. Post-discharge follow-up visits and hospital utilization by Medicare patients, 2007–2010. Medicare & medicaid research review 2014;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Polsky D, Richards M, Basseyn S, et al. Appointment availability after increases in Medicaid payments for primary care. New England Journal of Medicine 2015;372:537–45. [DOI] [PubMed] [Google Scholar]
- 44.Bradley E, Taylor L, Bradley H. The American health care paradox: Why spending more is getting us less: PublicAffairs; 2013.
- 45.Medicaid and Medicare Home Health Payments for. Skilled Nursing and Home Health Aide Services. Department of Health and Humman Services, Washington: https://oig.hhs.gov/oei/reports/oei-07-06-00641.pdf. Updated February 5, 2009 Accessed March 13, 2018. [Google Scholar]
- 46.Cho YI, Lee S-YD, Arozullah AM, Crittenden KS. Effects of health literacy on health status and health service utilization amongst the elderly. Social science & medicine 2008;66:1809–16. [DOI] [PubMed] [Google Scholar]
- 47.Bennett IM, Chen J, Soroui JS, White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. The Annals of Family Medicine 2009;7:204–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Logan RA, Wong WF, Villaire M, et al. Health literacy: A necessary element for achieving health equity. National Academy of Medicine; 2015. [Google Scholar]
- 49.Buchmueller TC, Orzol S, Shore-Sheppard LD. The effect of Medicaid payment rates on access to dental care among children. American Journal of Health Economics 2015. [Google Scholar]