Abstract
Sorafenib, a multikinase inhibitor with antiproliferative, antiangiogenic, and proapoptotic properties, constitutes the only effective first-line drug approved for the treatment of advanced hepatocellular carcinoma (HCC). Despite its capacity to increase survival in HCC patients, its success is quite low in the long term owing to the development of resistant cells through several mechanisms. Among these mechanisms, the antiangiogenic effects of sustained sorafenib treatment induce a reduction of microvessel density, promoting intratumoral hypoxia and hypoxia-inducible factors (HIFs)-mediated cellular responses that favor the selection of resistant cells adapted to the hypoxic microenvironment. Clinical data have demonstrated that overexpressed HIF-1α and HIF-2α in HCC patients are reliable markers of a poor prognosis. Thus, the combination of current sorafenib treatment with gene therapy or inhibitors against HIFs have been documented as promising approaches to overcome sorafenib resistance both in vitro and in vivo. Because the depletion of one HIF-α subunit elevates the expression of the other HIF-α isoform through a compensatory loop, targeting both HIF-1α and HIF-2α would be a more interesting strategy than therapies that discriminate among HIF-α isoforms. In conclusion, there is a marked correlation between the hypoxic microenvironment and sorafenib resistance, suggesting that targeting HIFs is a promising way to increase the efficiency of treatment.
Liver cancer: overcoming treatment resistance
Targeting hypoxia-inducible factors (HIFs), regulatory proteins induced by low oxygen levels, could increase the effectiveness of sorafenib, the only systemic therapy approved for advanced liver cancer. Long-term treatment with sorafenib starves tumors of oxygen, which can lead to the proliferation of cancer cells that are able to survive low oxygen levels. HIFs regulate genes involved in this adaptation and HIF levels are increased in sorafenib-resistant cells. José Mauriz at the University of León, Spain, and colleagues review recent studies on the effects of HIF inhibition on sorafenib efficacy. They conclude that HIF-1α and HIF-2α are predictive markers of sorafenib resistance and that using inhibitors of both these factors as an add-on therapy could improve patient survival. This strategy may be applicable to other types of cancer in which reduced oxygen conditions lead to drug resistance.
Introduction
Hepatocellular carcinoma (HCC) represents the second and the sixth cause of cancer-related death worldwide in men and women, respectively, and its incidence is increasing in regions with historically low rates such as Oceania, Western Europe and Northern America1. Unfortunately, most cases are diagnosed in advanced stages, when there are no amenable curative therapies, and the unique palliative drug approved by the Food and Drug Administration (FDA) as the first-line chemotherapy is sorafenib (BAY 43–9006, Nexavar®; Bayer HealthCare Pharmaceuticals Inc.; Leverkusen, Germany)2,3.
Sorafenib is a multikinase inhibitor that blocks tumor cell proliferation by inhibiting serine/threonine kinase isoforms of Raf, Raf-1, and B-Raf, leading to the inhibition of mitogen-activated protein kinase/extracellular signal-regulated kinase (ERK) signaling pathways, decreased expression of cyclin D1 and cell cycle arrest4–6. Sorafenib exhibits antiangiogenic activity by targeting the tyrosine kinase receptors hepatocyte factor receptor (c-Kit), FMS-like tyrosine kinase (FLT-3), vascular endothelial growth factor receptors 2 and 3 (VEGFR-2, VEGFR-3), and platelet-derived growth factor receptor4,7,8. In addition, sorafenib promotes apoptosis by inhibiting eIF4E phosphorylation and subsequent downregulation of the antiapoptotic factor Mcl-1 translation4,7 or through a progressive increase in endoplasmic reticulum stress associated with a shift from autophagy to apoptosis9.
Sorafenib approval was founded on the results of the Sorafenib Hepatocellular Carcinoma Assessment Randomized Protocol (SHARP) trial, in which it was shown to be effective and safe. SHARP was an international, multicenter, randomized, double-blind, placebo-controlled trial in 602 patients with unresectable HCC. This trial demonstrated that sorafenib could improve patient survival; however, the response rates were very low (from 7.9 months in the placebo group to 10.7 with sorafenib; hazard ratio: 0.69 (95% CI: 0.55, 0.87), p = 0.00058). In addition to its clinical benefits, sorafenib is usually well tolerated, with fatigue, weight loss, rash/desquamation, alopecia, palmar-plantar erythrodysesthesia, diarrhea, anorexia, nausea, and abdominal pain being the more common adverse reactions10. These results were supported by a phase III randomized, double-blind, placebo-controlled trial in 271 patients of the Asia-Pacific region11 and by the Global Investigation of therapeutic DEcisions in HCC and Of its treatment with sorafeNib (GIDEON), which included a heterogeneous population of 1571 unresectable HCC patients12. In recent years, various clinical studies have also indicated that sorafenib has antitumor effects not only in HCC but also in other cancer types, including thyroid cancer, myeloid leukemia, mesothelioma, renal cell carcinoma, and prostate cancer13–17.
Although sorafenib can prolong survival in HCC patients, its efficacy is short owing to the development of resistant cells. Although some patients are initially resistant to sorafenib because of HCC heterogeneity, in most cases, the resistance is acquired because of long-term exposure to the drug. Several mechanisms are implicated in the reduction of tumor cell sensitivity to sorafenib, such as loops of the phosphatidylinositol-3-kinase (PI3K)/protein kinase B (Akt) and janus tyrosine kinase (JAK)/signal transducer and activator of transcription (STAT) pathways, epithelial–mesenchymal transition (EMT) or hypoxia-inducible response5,8,18,19. Here, we consider the role of the hypoxic microenvironment in sorafenib resistance.
Hypoxia and HIFs in HCC
The tumor microenvironment is closely involved in tumor development8. Changes in the oxygen supply that occur during inflammation, metabolic disorders, steatohepatitis, viral hepatitis, and carcinogenesis are sufficient to promote a hypoxic response. However, despite the variable oxygen tensions, hypoxic responses are not observed in normal healthy liver20. Hypoxia is a common property of solid tumors, such as HCC, which appears because of faulty vascularization and intense metabolic activity, related to radio- and chemoresistance, selection of more invasive clones and poor clinical outcomes8,20,21. The adaptive response to hypoxia entails a set of “prosurvival” changes regulated by hypoxia-inducible factors (HIFs) and is involved in tumor development and progression22,23.
HIFs are transcription factors that regulate a wide range of genes involved in proliferation, glucose metabolism, angiogenesis, tumor invasion, and metastasis; all processes focused on cell adaptation to the lack of oxygen20,23. HIFs are heterodimeric complexes comprising a HIF-α subunit regulated through oxygen-dependent proteasomal degradation and a HIF-β subunit constitutively expressed24. Three isoforms of the HIF-α subunit (HIF-1α, HIF-2α, and HIF-3α) have been described, and the overexpression of HIF-1α and HIF-2α has been detected in different liver diseases, including nonalcoholic fatty liver disease, alcoholic liver disease, radiation-induced liver injury, and HCC23.
HIF-1α and HIF-2α share a similar protein structure and mutual targets, but they regulate independent patterns of downstream gene induction; although HIF-1α is ubiquitously expressed, HIF-2α is only expressed by definite cell types, including hepatocytes25,26. The cellular levels of HIF-α subunits depend on the balance between its oxygen-dependent degradation and oxygen-independent synthesis21,24. Under normoxia (normal oxygen supply), HIF-α is constitutively degraded and kept at low basal activity24. Prolyl hydroxylases (PHDs) hydroxylate proline residues using oxygen as cofactor and allow the interaction between HIF-α and the von Hippel-Lindau (VHL) tumor suppressor protein. Successively, the ubiquitin E3 ligase protein recognizes VHL, resulting in the ubiquitination of HIF-α and its imminent proteasomal degradation21,23. Furthermore, factor inhibiting HIF hydroxylates asparagine residues of HIF-α, disturbing the interaction between HIF and the transcriptional coactivators CREB-binding protein and p300 in the promoter regions24. Conversely, under hypoxia conditions (low oxygen supply), hydroxylation, and proteasomal degradation of HIF-α weaken owing to the lack of oxygen, so that HIF-α is stabilized and translocated into the nucleus, where it heterodimerizes with HIF-β and binds to hypoxia-response elements in the promoters of its targets genes involved in tumor progression and therapy resistance20,24.
During the long-term periods of hypoxia, a HIF-1α-dependent feedback loop increases PHDs expression, leading to the reactivation of HIF-1α hydroxylation and proteasomal degradation. Hence, HIF-1α appears to play the main role in the response to acute hypoxia, whereas the HIF-2α levels may increase over time, driving the response to chronic hypoxia20,26. In addition, the depletion of one HIF-α subunit elevates the levels of the other HIF-α isoforms by a compensatory loop, and it is known that the switch from HIF-1α to HIF-2α confers to the tumor a more aggressive phenotype26.
It was demonstrated that both HIF-1α and HIF-2α are upregulated in HCC and are considered markers of poor prognosis. However, studies have also reported that overexpression of HIF-2α could play a tumor suppressor role in HCC depending on the cellular context27.
HIFs and sorafenib resistance
Lack of oxygen is common in solid tumors such as HCC and drives vascular endothelial growth factor (VEGF) production and angiogenesis through HIF-1α activation28. Thus, the antiangiogenic actions of sorafenib are derived from blockade of the HIF-1α/VEGF pathway29–31. Sorafenib inhibits hypoxia-induced HIF-1α protein synthesis, leading to decreased VEGF expression and lower tumor vascularization both in different HCC cell lines29,31 and HCC xenograft mice29. A study by Xu et al.30 reported that this drug could reduce HIF-1α and VEGF expression and microvessel density, augmenting the time to recurrence when it is used as a coadjuvant to radiofrequency ablation.
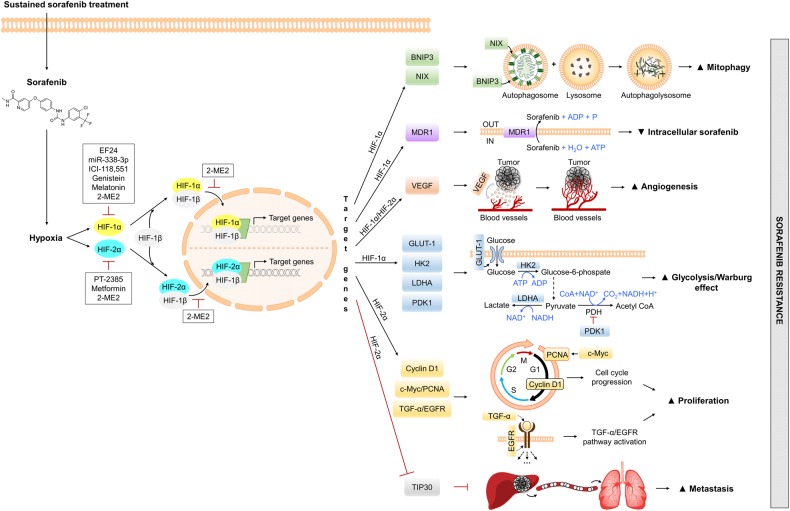
Nonetheless, there is a gripping correlation between acquired sorafenib resistance and the hypoxic microenvironment because the antiangiogenic activity of sustained sorafenib treatment leads to tumor starvation and succeeding intratumoral hypoxia, favoring the selection of resistant cell clones adapted to the deficit of oxygen and nutrients32–34. This situation limits sorafenib efficiency (Fig. 1)32.
Fig. 1. Hypoxia-related mechanisms of sorafenib resistance and targeting strategies against HIFs.
Sustained sorafenib treatment enhances hypoxia-inducible factors 1α or 2α, which promote the transcription of a wide range of genes involved in mitophagy, proliferation, glucose metabolism, angiogenesis, tumor invasion, and metastasis, leading to sorafenib resistance. This resistance can be overcome by different small molecules or drugs that inhibit HIFs. ADP, adenosine diphosphate; ATP, adenosine triphosphate; BNIP3, B-cell lymphoma-2 (BCL2)/adenovirus E1B 19 kDa-interacting protein 3; c-Myc, Myc proto-oncogene protein; CoA, coenzyme A; EGFR, phospho-epidermal growth factor receptor; GLUT-1, glucose transporter 1; HIF, hypoxia-inducible factor; HK2, hexokinase 2; LDHA, lactate dehydrogenase A; MDR1, multidrug resistance protein 1; NAD+, nicotinamide adenine dinucleotide (oxidized form); NADH, nicotinamide adenine dinucleotide (reduced form); NIX, BNIP3-like protein X; P, phosphate; PCNA, proliferating cell nuclear antigen; PDH, pyruvate dehydrogenase; PDK1, pyruvate dehydrogenase kinase isoform 1; TGF-α, transforming growth factor α; TIP30, oxidoreductase HTATIP2; VEGF, vascular endothelial growth factor
It was reported that hypoxia confers sorafenib resistance in myeloid leukemia, renal, or gastric cancer cells35–38 and is responsible for the acquired resistance to different anticancer drugs in HCC cells, including doxorubicin, etoposide, cisplatin, SN38, and 5-fluorouracil39–43. In fact, Liang et al.32 reported that the continued administration of sorafenib in HCC subcutaneous mouse tumor models increases the protein levels and transcriptional activity of HIF-1α. Likewise, HCC tissues obtained from sorafenib-resistant patients display increased intratumor hypoxia and expression of HIF-1α compared with sorafenib-sensitive or untreated HCCs32. Sorafenib resistance is associated with the increased expression of the multidrug resistance protein 1 (MDR1), glucose transporter 1 (GLUT-1), and VEGF because of HIF-1α protein stabilization32,44. In addition, galectin-1, a protein involved in modulating cell–cell and cell–matrix interactions, was reported to be a downstream target of the Akt/mTOR/HIF-1α pathway and was defined as a predictive marker of sorafenib resistance45. β-2 Adrenergic receptor (ADRB2) signaling modulates autophagy negatively by disturbing the beclin1/phosphatidylinositol-3-kinase VPS3/autophagy-related protein 14 complex in an Akt-dependent manner, promoting the stabilization of HIF-1α, reprogramming glucose metabolism of HCC cells, and leading to the acquisition of sorafenib resistance46. This role of glycolysis in sorafenib resistance was supported by a report where HIF-1α activation endorses cell survival by amplifying the expression of glycolytic enzymes—for instance, GLUT-1 and hexokinase 2 (HK2)—to accelerate the glycolytic rate47. Mitophagy, a specific form of autophagy, is activated under hypoxic conditions in HCC cells by the upregulation of the mitophagy targets of HIF-1α, B-cell lymphoma-2/adenovirus E1B 19 kDa-interacting protein 3 (BNIP3) and BNIP3-like protein X (NIX). It was described that mitophagy exerts a cytoprotective role on tumor cells; however, unfortunately, sorafenib treatment cannot abolish this process33.
In addition, given the feedback mechanism between the HIF-1α and HIF-2α subunits, it can be thought that sorafenib treatment may upregulate HIF-2α through the inhibition of HIF-1α, promoting sorafenib resistance and a more aggressive tumor growth25,26,34. It was verified that sorafenib upregulates HIF-2α through the hypoxic response switch from HIF-1α inhibition, contributing to the resistance of hypoxic HCC cells by activating the HIF-2α/transforming growth factor (TGF)-α/epidermal growth factor receptor (EGFR) pathway26 and increasing the expression of VEGF and cyclin D125. Another study found that sorafenib treatment enhances HIF-2α accumulation, contributing to androgen receptor (AR) reduction, which is related to HCC progression and metastasis48. Moreover, Liu et al.34 reported a feedback mechanism and described that the HIF-2α increase positively regulates β-catenin/Myc proto-oncogene protein (c-Myc) expression and that c-Myc directly upregulates proliferating cell nuclear antigen (PCNA) expression under hypoxic conditions in HCC cells, thus increasing the proliferation involved in sorafenib resistance. Zhu et al.49 also supported that HIF-2α is involved in the process by which hypoxia protects HCC cells against sorafenib. Hepatopoietin Cn (HPPCn) is a growth factor isolated from hepatic stimulator substance that promotes sorafenib resistance by elevating HIF-2α levels through the promotion of cell growth and metastasis in HCC. In addition, Akt-mediated sentrin-specific protease 1 (SENP1) upregulation accounts for HPPCn-induced HIF-2α accumulation under a hypoxic microenvironment. Another study confirmed that the overexpression of HIF-2α by sorafenib promotes HCC invasion and metastasis via the downregulation of oxidoreductase HTATIP2 (TIP30)50.
These studies endorse the existing relationship between the high expression of HIFs and the resistance phenomenon to sorafenib, suggesting that hypoxia significantly affects sorafenib therapy and that a promising way to overcome resistance is to target these factors (Table 1).
Table 1.
Hypoxia and sorafenib resistance in HCC
| Cell lines/animal models/human samples | Effects on HIF after sorafenib treatment | Global effects | References |
|---|---|---|---|
| HCCs from patients HepG2, Huh7, PLC-5, Hep3B, and SK-Hep-1 cells BALB/c mice inoculated with Hep3B or Huh7 and orthotopic Huh7 hepatic tumors |
↑ HIF-1α | ↑ GLUT-1, MDR1, and VEGF Activation of NF-κB | 32 |
| Human HCC samples HepG2, SMMC-7721, BEK-7402, Hep3B, and Huh7 cells BALB/c nude mice subcutaneous model with HepG2 cells |
↑ HIF-1α | ↑ GLUT-1, MDR1, and VEGF | 44 |
| Sorafenib-resistant Huh7 cells (Huh7R) Tumor xenograft model by subcutaneously injecting Huh7 and Huh7R cells in BALB/c nude mice |
↑ HIF-1α | ↑ Galectin-1 | 45 |
| HCC samples HepG2, SMMC-7721, MHCC-LM3, and CSQT-2 cells DEN-induced HCC in C57BL/6 mice Mouse xenograft model derived from SMMC-7721 cells |
↑ HIF-1α | ↑ GLUT-1, HK2, PDK1, LDHA, and VEGF | 46 |
| HCC-LM3 and Bel-7402 cells BALB/c nu/nu injected with HCC-LM3 cells |
↑ HIF-1α | ↑ GLUT-1 and HK2 | 47 |
| HepG2 and Huh7 cells BALB/c mice with Huh7 subcutaneously injected |
↓ HIF-1α ↑ HIF-2α |
Activation of TGF-α/EGFR | 26 |
| HepG2 and Huh7 cells BALB/c mice with Huh7 subcutaneously injected |
↓ HIF-1α ↑ HIF-2α |
↑ VEGF and cyclin D1 ↓ LDHA |
25 |
| HepG2, Huh7, and SK-Hep-1 cells Mice HCC nodules Orthotopic HCC mouse models with SK-Hep-1 cells |
↑ HIF-2α | ↑ AR | 25 |
| HepG2, Huh7, Bel-7402, and SMMC-7402 cells BALB/c mice subcutaneously inoculated with HepG2 |
↓ HIF-1α ↑ HIF-2α |
↑ β-catenin/c-Myc/PCNA | 34 |
| HCC cells | ↑ HIF-2α | – | 49 |
| MHCC97H cells BALB/c mice subcutaneously injected with MHCC97H cells |
↑ HIF-2α | ↓ TIP30 | 50 |
AR androgen receptor, c-Myc Myc proto-oncogene protein, DEN diethylnitrosamine, EGFR epidermal growth factor receptor, GLUT-1 glucose transporter 1, HCC hepatocellular carcinoma, HIF hypoxia-inducible factor, HK2 hexokinase 2, LDHA lactate dehydrogenase A, MDR1 multidrug resistance protein 1, PCNA proliferating cell nuclear antigen, PDK1 pyruvate dehydrogenase kinase isoform 1, TGF-α transforming growth factor α, TIP30 oxidoreductase HTATIP2, VEGF vascular endothelial growth factor
Targeting HIFs to overcome sorafenib resistance
Given the pathological role of HIFs in liver disease, particularly in HCC, inhibition of HIFs is being explored as an effective treatment strategy. Furthermore, because of the participation of HIFs in the development of resistance to chemotherapeutic drugs in HCC, HIF inhibitors can be administered in combination with current therapies (Table 2)23.
Table 2.
Therapeutic approaches against HIFs to overcome sorafenib resistance in HCC
| Models | Strategies to target hypoxia markers | Effects on hypoxia markers | Global effects | References |
|---|---|---|---|---|
| HepG2, Huh7, PLC-5, Hep3B, and SK-Hep-1 cells BALB/c mice inoculated with Hep3B or Huh7 and orthotopic Huh7 hepatic tumors |
EF24 plus sorafenib | VHL-dependent HIF-1α protein degradation | ↓ DNA-binding activity of NF-κB ↓ VEGF, GLUT-1 ↓ Migration, invasion, and metastasis ↑ Apoptosis |
32 |
| HepG2, SMMC-7721, BEK-7402, Hep3B, and Huh7 cells BALB/c nude mice subcutaneous model with HepG2 cells |
Overexpression of miR-338-3p plus sorafenib treatment | HIF-1α mRNA inhibition | ↓ MDR1 ↓ Tumor growth ↑ Apoptosis |
44 |
| HepG2, SMMC-7721, MHCC-LM3, and CSQT-2 cells Mouse xenograft model derived from SMMC-7721 cells |
ICI-118,551 plus sorafenib | Autophagic degradation of HIF-1α protein | ↓ Glucose metabolism and proliferation ↑ Autophagic cell death |
46 |
| HCC-LM3 and Bel-7402 cells BALB/c nu/nu injected with HCC-LM3 cells |
Genistein plus sorafenib | HIF-1α mRNA downregulation | ↓ GLUT-1 and HK2 ↓ Glycolysis and induce apoptosis |
47 |
| Hep3B cells | Melatonin and sorafenib combination | HIF-1α protein downregulation | ↓ BNIP3 and NIX ↓ Cytoprotective hypoxia-induced mitophagy |
33 |
| HepG2 and Huh7 cells BALB/c mice with Huh7 subcutaneously injected |
HIF-2α siRNA plus sorafenib | Knockdown of HIF-2α by RNA interference | ↓ HIF-2α, TGF-α, p-EGFR, p-STAT3, p-Akt, p-ERK, cyclin D1, and VEGF ↓ HCC tumors growth ↑ Apoptosis |
26 |
| HepG2, Huh7, and SK-Hep-1 cells Orthotopic HCC mouse models with SK-Hep-1 cells |
PT-2385 plus sorafenib | HIF-2α protein downregulation | ↑AR ↓ p-STAT3, p-Akt, p-ERK, B-Raf, and Raf-1 ↓ Invasion |
48 |
| HCC cells | HIF-2α shRNA plus sorafenib | Knockdown of HIF-2α by RNAinterference |
↓ Tumor growth and metastasis | 49 |
| HepG2, Huh7, Bel-7402, and SMMC-7402 cells BALB/c mice subcutaneously inoculated with HepG2 |
HIF-2α shRNA or siRNA plus sorafenib | Knockdown of HIF-2α by RNA interference | ↓ β-catenin/c-Myc/PCNA ↓ Proliferation and tumor growth |
34 |
| MHCC97H cells BALB/c mice subcutaneously injected with MHCC97H cells |
Metformin plus sorafenib | HIF-2α protein inhibition | ↑ TIP30 ↓ Proliferation, EMT, postoperative recurrence, and lung metastasis ↑ Apoptosis |
50 |
| HepG2 and Huh7 cells BALB/c mice with Huh7 subcutaneously injected |
2-ME2 plus sorafenib | Inhibition of nuclear translocation and expression of HIF-1α and HIF-2α proteins | ↓ VEGF, LDHA, and cyclin D1 ↓ Proliferation and angiogenesis ↑ Apoptosis |
25 |
2-ME2 2-methoxyestradiol, ADRB2 β-2 adrenergic receptor, AR androgen receptor, B-Raf serine/threonine-protein kinase, BNIP3 B-cell lymphoma-2 (BCL2)/adenovirus E1B 19 kDa-interacting protein 3, c-Myc Myc proto-oncogene protein, EMT epithelial–mesenchymal transition, GLUT-1 glucose transporter 1, HCC hepatocellular carcinoma, HIF hypoxia-inducible factor, HK2 hexokinase 2, LDHA lactate dehydrogenase A, MDR1 multidrug resistance protein 1, NIX BNIP3-like protein X, p-Akt phospho-protein kinase B, p-EGFR phospho-epidermal growth factor receptor, p-ERK phospho-extracellular signal-regulated kinases, p-STAT3 phospho-signal transducer and activator of transcription 3, PCNA proliferating cell nuclear antigen, Raf-1 Raf proto-oncogene serine/threonine-protein kinase, TGF-α transforming growth factor α, TIP30 oxidoreductase HTATIP2, VEGF vascular endothelial growth factor, VHL von Hippel-Lindau
Different studies showed that sustained sorafenib therapy leads to increased intratumor hypoxia, which has been associated with reduced sorafenib sensitivity through HIF stabilization in HCC, and reported that targeting HIF-1α can improve sorafenib efficacy. Liang et al.32 suggested that hypoxia induced by continued sorafenib treatment causes sorafenib resistance in HCC through HIF-1α and nuclear factor kappa B (NF-κB) activation. The combination of sorafenib and EF24, a curcumin analog, can overcome hypoxia-mediated sorafenib resistance by encouraging the proteasomal degradation of HIF-1α in a VHL-dependent manner in HCC cells, leading to the suppression of its target genes MDR1, GLUT-1, and VEGF and activity of NF-κB. The combination of EF24 and sorafenib also exhibited synergistic properties against tumor growth in subcutaneous and orthotopic hepatic tumor models32. In addition, the overexpression of miR-338-3p, which is strikingly downregulated in HCC patient samples and HCC cell lines, reduces cell viability and stimulates cell apoptosis by directly binding to the 3´-UTR of HIF-1α. Moreover, transfection of miR-338-3p can surpass sorafenib resistance mediated by hypoxia, acting synergistically against HCC tumor growth in an HCC subcutaneous nude mice tumor model by inhibiting HIF-1α44. ADRB2 signaling plays an essential role in maintaining the proliferation and survival of HCC cells through the stabilization of HIF-1α mediated by the downregulation of the autophagy process, leading to the reprogramming of glucose metabolism of HCC cells and acquisition of sorafenib resistance. Thus, the inhibition of ADRB2 signaling by the adrenoreceptor antagonist ICI-118,551 or knockdown of ADRB2 expression improved autophagy, which induced HIF-1α destabilization and upgraded the antitumor activity of sorafenib46.
The use of natural compounds has also shown positive effects in the improvement of sorafenib treatment. Genistein, a natural isoflavone, enhanced the antitumor effects of sorafenib in sorafenib-resistant HCC cells and an HCC xenograft mouse model by downregulating HIF-1α, therefore inactivating GLUT-1 and HK2 to suppress glycolysis and sensitize aerobic glycolytic HCC cells to the mitochondrial apoptosis47. Similarly, melatonin, a natural hormone, can downregulate HIF-1α protein synthesis through the inhibition of the mammalian target of rapamycin complex 1/ribosomal protein S6 kinase beta-1/ribosomal protein S6 pathway. Moreover, sorafenib and melatonin coadministration reduced the expression of HIF-1α-mitophagy targets BNIP3 and NIX, blocking the cytoprotective mitophagy induced by the hypoxic microenvironment33.
Nonetheless, other studies have focused their attention on the hypoxic response switch from HIF-1α- to HIF-2α-dependent pathways supported by sorafenib and succeeding the upregulation of HIF-2α, which subscribes to the insensitivity of hypoxic HCC cells to the drug25. Zhao et al.26 proposed that sorafenib-induced HIF-2α upregulation contributes to the resistance of hypoxic HCC cells by activating the TGF-α/EGFR pathway. The employment of gefitinib, a specific EGFR inhibitor, allows blockade of the TGF-α/EGFR pathway, downregulating the activation of STAT3, Akt, and ERK, and, in combination with sorafenib, can reduce the proliferation and induce the apoptosis of HCC cells under hypoxia. Likewise, transfection of HIF-2α siRNA decreased the expression of TGF-α, VEGF, and cyclin D1, and repressed the activation of EGFR, inhibiting the proliferation and promoting the apoptosis of HCC cells in vitro; HIF-2α siRNA also synergized with sorafenib to suppress the growth of HCC tumors in vivo26. Furthermore, sorafenib-induced or hypoxia-induced HIF-2α transcriptionally suppresses AR by binding to an HRE of the AR promoter. In vitro and in vivo studies have suggested that PT-2385, a specific HIF-2α inhibitor, improves sorafenib effectiveness by inhibiting HIF-2α, increasing AR and suppressing the downstream activation of STAT3, Akt, and ERK pathways48.
Another study also supported that HIF-2α contributes to sorafenib resistance in HCC. On this occasion, desumoylation of HIF-2α by SENP1 was reported to be implicated in HPPCn-enhanced sorafenib resistance under hypoxic conditions in HCC. The growth factor HPPCn increases HIF-2α levels, which promote cell growth and metastasis; thus, the combination of lentivirus-mediated HIF-2α shRNA and sorafenib presented synergistically effects to prevent tumor growth49. A study by Liu et al.34 showed that HIF-2α is involved in sorafenib resistance by regulating cell proliferation via the β-catenin/c-Myc-dependent pathway under hypoxic conditions. Thus, the combination of HIF-2α shRNA and sorafenib treatment exhibited an additive positive effect on inhibiting proliferation in HCC cells and in HepG2 xenograft mouse tumors, a finding mainly attributed to the decreased expression of PCNA that is directly regulated by c-Myc34.
It was also found that the overexpression of HIF-2α by sorafenib decreased the expression of TIP30, an oxidoreductase required for tumor suppression, stimulating the process of EMT and the subsequent promotion of HCC invasion and metastasis. Metformin (the first-line medication for the treatment of type II diabetes) has been tested in addition to sorafenib, showing inhibited expression of HIF-2α but upregulation of TIP30 at the protein levels, recovering the sensitivity of hypoxic HCC cells to sorafenib therapy in vitro. In addition, the combination of sorafenib with metformin revealed meaningful inhibition of the recurrence and metastasis of primary liver cancer in an orthotopic xenograft mouse model following surgical resection by modulating the expression of HIF-2α and TIP3050.
Unlike therapies that differentiate among HIF-α isoforms, targeting both HIF-1α and HIF-2α signaling would be more prejudicial to tumor cell survival than strategies directed only against one of them20. A study by Ma et al.25 employed 2-methoxyestradiol (2-ME2), a natural metabolite of estradiol. 2-ME2 repressed the nuclear translocation of HIF-1α and HIF-2α proteins and significantly weakened the expression levels of both HIF-1α and HIF-2α as well as their downstream targets VEGF, lactate dehydrogenase A, and cyclin D1, enhancing the sorafenib sensitivity of hypoxic HCC cells. Furthermore, 2-ME2 synergized with sorafenib to inhibit the proliferation and induction of apoptosis of HCC cells in vitro and in vivo and to inhibit tumor angiogenesis25.
Conclusions and future perspectives
Sorafenib, a multitarget tyrosine kinase inhibitor, is the only effective first-line drug for the treatment of advanced HCC patients. Sorafenib resistance in HCC is a fact; nonetheless, the mechanisms that explain this resistance are complex and remain unclear. The genetic heterogeneity of HCC could explain the appearance of primary resistance. Thus, the identification of predictive biomarkers related to primary resistance to sorafenib will be very rewarding. Sorafenib targets several kinase pathways; thus, it can also simultaneously or consecutively activate additional switches and compensatory pathways—for instance, PI3K/Akt and JAK/STAT pathways, EMT, and tumor hypoxia—leading to acquired resistance.
Recent evidence has supported that hypoxia plays a key role in HCC development and therapy. In fact, clinical data have proven that hypoxia markers HIF-1α and HIF-2α are trustworthy indicators of the poor prognosis of HCC patients; even so, the role of HIF-2α depends on the cellular context.
The antiangiogenic effects of long-term sorafenib treatment promote decreased microvessel density and enhanced tumor hypoxia, which lead to HIF-mediated cellular responses triggering adaptive mechanisms to the hypoxic microenvironment. Not surprisingly, HIFs have been recognized as potential targets for HCC therapy. The use of gene therapy to target HIFs or the addition of HIF inhibitors to current therapies has improved their effectiveness. Particularly, in cancers such as HCC, in which there is a recognized overexpression of HIFs, existing drugs such as sorafenib or other antiangiogenic and vascular targeting molecules promote the activity of HIFs. Additional studies are necessary to select optimal therapeutic agents targeted against HIFs for enhanced clinical outcomes, considering the response switch between HIF-1α and HIF-2α.
Different clinical trials have examined the effect of targeting hypoxia in HCC. A recently completed phase I study evaluated the intravenous infusion effect of the HIF-1α mRNA antagonist RO7070179 in HCC patients failing to respond to systemic therapy (clinicaltrials.gov Identifier: NCT02564614). Other trials have focused on the use of hypoxia-activated prodrugs (HAPs), molecules that specifically target the hypoxic fractions of tumors. Thus, two early phase I/II trials analyzed different HAPs, TH-302 or PR104, in combination with sorafenib, in patients with advanced HCC that cannot be removed by surgery (clinicaltrials.gov Identifier: NCT01497444 and NCT00862082). A phase I study to be completed in December 2020 aims to establish the prime dose and tolerability of an HAP, tirapazamine, combined with embolization in HCC (clinicaltrials.gov Identifier: NCT02174549).
In addition to inhibiting hypoxia-induced signaling, improving HCC oxygenation could be an interesting approach to overcome sorafenib resistance. Indeed, some studies have analyzed the potential usefulness of a synthetic tetrameric hemoglobin, YQ23, which can target hypoxia to improve HCC therapy by its facilitation of oxygen delivery51–53.
Several drugs have been proposed as second-line treatment for advanced HCC after the failure of sorafenib therapy, and some of them are under evaluation in clinical trials3,5. Presently, only the tyrosine kinase inhibitor regorafenib (Stivarga®; Bayer HealthCare Pharmaceuticals Inc.; Leverkusen, Germany)54 and the human immunoglobulin G4 monoclonal antibody nivolumab (Opdivo®; Bristol-Myers Squibb Co.; NY, USA)55 have been approved by the FDA for HCC previously treated with sorafenib.
Further investigations focused on the elucidation of mechanisms involved in sorafenib resistance would allow for better understanding and help to propose more effective strategies to increase the efficacy of treatment.
Acknowledgements
CIBERehd is funded by Instituto de Salud Carlos III, Spain. CMB is supported by the Asociación Española Contra el Cáncer (AECC)-Junta Provincial de León. FF by the Ministry of Education of Spain (Becas FPU: FPU16/05277).
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These senior authors contributed equally: Javier González-Gallego, José L. Mauriz
References
- 1.Torre LA, et al. Global Cancer Statistics, 2012. CA Cancer J. Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Quintieri L, Selmy M, Indraccolo S. Metabolic effects of antiangiogenic drugs in tumors: therapeutic implications. Biochem. Pharmacol. 2014;89:162–170. doi: 10.1016/j.bcp.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 3.Connell LC, Harding JJ, Abou-Alfa GK. Advanced hepatocellular cancer: the current state of future research. Curr. Treat. Options Oncol. 2016;17:43. doi: 10.1007/s11864-016-0415-3. [DOI] [PubMed] [Google Scholar]
- 4.Liu L, et al. Sorafenib blocks the RAF/MEK/ERK pathway, inhibits tumor angiogenesis, and induces tumor cell apoptosis in hepatocellular carcinoma model PLC/PRF/5. Cancer Res. 2006;66:11851–11858. doi: 10.1158/0008-5472.CAN-06-1377. [DOI] [PubMed] [Google Scholar]
- 5.Zhai B, Sun XY. Mechanisms of resistance to sorafenib and the corresponding strategies in hepatocellular carcinoma. World J. Hepatol. 2013;5:345–352. doi: 10.4254/wjh.v5.i7.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prieto-Domínguez N, et al. Modulation of autophagy by sorafenib: effects on treatment response. Front. Pharmacol. 2016;7:1–16. doi: 10.3389/fphar.2016.00151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gauthier A, Ho M. The role of sorafenib in the treatment of advanced hepatocellular carcinoma: an update. Hepatol. Res. 2013;43:147–154. doi: 10.1111/j.1872-034X.2012.01113.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu Y, Zheng B, Wang H, Chen L. New knowledge of the mechanisms of sorafenib resistance in liver cancer. Acta Pharmacol. Sin. 2017;38:614–622. doi: 10.1038/aps.2017.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rodríguez-Hernández M. A., et al. Molecular characterization of autophagic and apoptotic signaling induced by sorafenib in liver cancer cells. J. Cell Physiol. (in press) 10.1002/jcp.26855 [DOI] [PubMed]
- 10.Llovet JM, et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 2008;359:378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 11.Cheng AL, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10:25–34. doi: 10.1016/S1470-2045(08)70285-7. [DOI] [PubMed] [Google Scholar]
- 12.Lencioni R, et al. GIDEON (Global Investigation of therapeutic DEcisions in hepatocellular carcinoma and of its treatment with sorafeNib): second interim analysis. Int. J. Clin. Pract. 2014;68:609–617. doi: 10.1111/ijcp.12352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schneider TC, et al. Long-term analysis of the efficacy and tolerability of sorafenib in advanced radio-iodine refractory differentiated thyroid carcinoma: final results of a phase II trial. Eur. J. Endocrinol. 2012;167:643–650. doi: 10.1530/EJE-12-0405. [DOI] [PubMed] [Google Scholar]
- 14.Papa S, et al. Phase 2 study of sorafenib in malignant mesothelioma previously treated with platinum-containing chemotherapy. J. Thorac. Oncol. 2013;8:783–787. doi: 10.1097/JTO.0b013e31828c2b26. [DOI] [PubMed] [Google Scholar]
- 15.Meyer A, et al. Role of sorafenib in overcoming resistance of chemotherapy-failure castration-resistant prostate cancer. Clin. Genitourin. Cancer. 2014;12:100–105. doi: 10.1016/j.clgc.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 16.Röllig C, et al. Addition of sorafenib versus placebo to standard therapy in patients aged 60 years or younger with newly diagnosed acute myeloid leukaemia (SORAML): a multicentre, phase 2, randomised controlled trial. Lancet Oncol. 2015;16:1691–1699. doi: 10.1016/S1470-2045(15)00362-9. [DOI] [PubMed] [Google Scholar]
- 17.Joshi A, et al. Efficacy and safety of sorafenib in advanced renal cell cancer and validation of Heng criteria. Indian J. Cancer. 2016;53:423–428. doi: 10.4103/0019-509X.180861. [DOI] [PubMed] [Google Scholar]
- 18.Nishida N, Kitano M, Sakurai T, Kudo M. Molecular mechanism and prediction of sorafenib chemoresistance in human hepatocellular carcinoma. Dig. Dis. 2015;33:771–779. doi: 10.1159/000439102. [DOI] [PubMed] [Google Scholar]
- 19.Niu L, et al. New insights into sorafenib resistance in hepatocellular carcinoma: responsible mechanisms and promising strategies. Biochim Biophys. Acta Rev. Cancer. 2017;1868:564–570. doi: 10.1016/j.bbcan.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 20.Wilson GK, Tennant DA, McKeating JA. Hypoxia inducible factors in liver disease and hepatocellular carcinoma: Current understanding and future directions. J. Hepatol. 2014;61:1397–1406. doi: 10.1016/j.jhep.2014.08.025. [DOI] [PubMed] [Google Scholar]
- 21.Lin D, Wu J. Hypoxia inducible factor in hepatocellular carcinoma: a therapeutic target. World J. Gastroenterol. 2015;21:12171–12178. doi: 10.3748/wjg.v21.i42.12171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luo D, Wang Z, Wu J, Jiang C, Wu J. The role of hypoxia-inducible factor-1 in hepatocellular carcinoma. Biomed. Res. Int. 2014;2014:409272. doi: 10.1155/2014/409272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ju C, Colgan SP, Eltzschig HK. Hypoxia-inducible factors as molecular targets for liver diseases. J. Mol. Med. 2016;94:613–627. doi: 10.1007/s00109-016-1408-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen C, et al. Hypoxia inducible factors in hepatocellular carcinoma. Oncotarget. 2017;5:46691–46703. doi: 10.18632/oncotarget.17358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ma L, et al. 2-Methoxyestradiol synergizes with sorafenib to suppress hepatocellular carcinoma by simultaneously dysregulating hypoxia-inducible factor-1 and -2. Cancer Lett. 2014;355:96–105. doi: 10.1016/j.canlet.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 26.Zhao D, et al. Upregulation of HIF-2α induced by sorafenib contributes to the resistance by activating the TGF-α/EGFR pathway in hepatocellular carcinoma cells. Cell Signal. 2014;26:1030–1039. doi: 10.1016/j.cellsig.2014.01.026. [DOI] [PubMed] [Google Scholar]
- 27.Xiong XX, Qiu XY, Hu DX, Chen XQ. Advances in hypoxia-mediated mechanisms in hepatocellular carcinoma. Mol. Pharmacol. 2017;92:246–255. doi: 10.1124/mol.116.107706. [DOI] [PubMed] [Google Scholar]
- 28.Carbajo-Pescador S, et al. Inhibition of VEGF expression through blockade of Hif1α and STAT3 signalling mediates the anti-angiogenic effect of melatonin in HepG2 liver cancer cells. Br. J. Cancer. 2013;109:83–91. doi: 10.1038/bjc.2013.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu LP, Ho RLK, Chen GG, Lai PBS. Sorafenib inhibits hypoxia-inducible factor-1α synthesis: Implications for antiangiogenic activity in hepatocellular carcinoma. Clin. Cancer Res. 2012;18:5662–5671. doi: 10.1158/1078-0432.CCR-12-0552. [DOI] [PubMed] [Google Scholar]
- 30.Xu M, et al. Sorafenib suppresses the rapid progress of hepatocellular carcinoma after insufficient radiofrequency ablation therapy: an experiment in vivo. Acta Radiol. 2013;54:199–204. doi: 10.1258/ar.2012.120249. [DOI] [PubMed] [Google Scholar]
- 31.Xu M, et al. Sorafenib blocks the HIF-1α/VEGFA pathway, inhibits tumor invasion, and induces apoptosis in hepatoma cells. DNA Cell Biol. 2014;33:275–281. doi: 10.1089/dna.2013.2184. [DOI] [PubMed] [Google Scholar]
- 32.Liang Y, et al. Hypoxia-mediated sorafenib resistance can be overcome by EF24 through Von Hippel-Lindau tumor suppressor-dependent HIF-1α inhibition in hepatocellular carcinoma. Hepatology. 2013;57:1847–1857. doi: 10.1002/hep.26224. [DOI] [PubMed] [Google Scholar]
- 33.Prieto-Domínguez N, et al. Melatonin enhances sorafenib actions in human hepatocarcinoma cells by inhibiting mTORC1/p70S6K/HIF-1α and hypoxia-mediated mitophagy. Oncotarget. 2017;8:91402–91414. doi: 10.18632/oncotarget.20592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu F, et al. Targeting hypoxia-inducible factor-2α enhances sorafenib antitumor activity via β-catenin/C-Myc-dependent pathways in hepatocellular carcinoma. Oncol. Lett. 2015;10:778–784. doi: 10.3892/ol.2015.3315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Van Oosterwijk JG, et al. Hypoxia-induced upregulation of BMX kinase mediates therapeutic resistance in acute myeloid leukemia. J. Clin. Invest. 2018;128:369–380. doi: 10.1172/JCI91893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao CX, Luo CL, Wu XH. Hypoxia promotes 786-O cells invasiveness and resistance to sorafenib via HIF-2α/COX-2. Med. Oncol. 2015;32:419. doi: 10.1007/s12032-014-0419-4. [DOI] [PubMed] [Google Scholar]
- 37.Bielecka ZF, et al. Hypoxic 3D in vitro culture models reveal distinct resistance processes to TKIs in renal cancer cells. Cell Biosci. 2017;7:1–18. doi: 10.1186/s13578-017-0197-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen Y, Sun L, Guo D, Wu Z, Chen W. Co-delivery of hypoxia inducible factor-1α small interfering RNA and 5-fluorouracil to overcome drug resistance in gastric cancer SGC-7901 cells. J. Gene Med. 2017;19:e2998. doi: 10.1002/jgm.2998. [DOI] [PubMed] [Google Scholar]
- 39.Jung EU, et al. Hypoxia and retinoic acid-inducible NDRG1 expression is responsible for doxorubicin and retinoic acid resistance in hepatocellular carcinoma cells. Cancer Lett. 2010;298:9–15. doi: 10.1016/j.canlet.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 40.Daskalow K, et al. Role of hypoxia-inducible transcription factor 1α for progression and chemosensitivity of murine hepatocellular carcinoma. J. Mol. Med. 2010;88:817–827. doi: 10.1007/s00109-010-0623-4. [DOI] [PubMed] [Google Scholar]
- 41.Tak E, et al. Human carbonyl reductase 1 upregulated by hypoxia renders resistance to apoptosis in hepatocellular carcinoma cells. J. Hepatol. 2011;54:328–339. doi: 10.1016/j.jhep.2010.06.045. [DOI] [PubMed] [Google Scholar]
- 42.Dai XY, et al. Nuclear translocation and activation of YAP by hypoxia contributes to the chemoresistance of SN38 in hepatocellular carcinoma cells. Oncotarget. 2016;7:6933–6947. doi: 10.18632/oncotarget.6903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li JQ, Wu X, Gan L, Yang XL, Miao ZH. Hypoxia induces universal but differential drug resistance and impairs anticancer mechanisms of 5-fluorouracil in hepatoma cells. Acta Pharmacol. Sin. 2017;38:1642–1654. doi: 10.1038/aps.2017.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xu H, et al. MiR-338-3p inhibits hepatocarcinoma cells and sensitizes these cells to sorafenib by targeting hypoxia-induced factor 1α. PLoS. ONE. 2014;9:e115565. doi: 10.1371/journal.pone.0115565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yeh CC, et al. Integrated stable isotope labeling by amino acids in cell culture (SILAC) and isobaric tags for relative and absolute quantitation (iTRAQ) quantitative proteomic analysis identifies galectin-1 as a potential biomarker for predicting sorafenib resistance in liver cancer. Mol. Cell Proteom. 2015;14:1527–1545. doi: 10.1074/mcp.M114.046417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu FQ, et al. ADRB2 signaling promotes HCC progression and sorafenib resistance by inhibiting autophagic degradation of HIF1α. J. Hepatol. 2016;65:314–324. doi: 10.1016/j.jhep.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 47.Li S, et al. Genistein suppresses aerobic glycolysis and induces hepatocellular carcinoma cell death. Br. J. Cancer. 2017;117:1518–1528. doi: 10.1038/bjc.2017.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xu J, et al. Increasing AR by HIF-2α inhibitor (PT-2385) overcomes the side-effects of sorafenib by suppressing hepatocellular carcinoma invasion via alteration of pSTAT3, pAKT and pERK signals. Cell Death Dis. 2017;8:e3095. doi: 10.1038/cddis.2017.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhu B, et al. Desumoylation of hypoxia inducible factor (HIF)-2α by SENP1 is involved in HPPCn-enhanced sorafenib resistance under hypoxia in hepatocellular carcinoma. J. Hepatol. 2014;60:S83–S84. doi: 10.1016/S0168-8278(14)60214-2. [DOI] [Google Scholar]
- 50.You A, et al. Metformin sensitizes sorafenib to inhibit postoperative recurrence and metastasis of hepatocellular carcinoma in orthotopic mouse models. J. Hematol. Oncol. 2016;9:1–9. doi: 10.1186/s13045-016-0253-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li CX, et al. A novel oxygen carrier “YQ23” suppresses the liver tumor metastasis by decreasing circulating endothelial progenitor cells and regulatory T cells. BMC Cancer. 2014;14:293. doi: 10.1186/1471-2407-14-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee NP, et al. Oxygen carrier YQ23 can enhance the chemotherapeutic drug responses of chemoresistant esophageal tumor xenografts. Cancer Chemother. Pharmacol. 2015;76:1199–1207. doi: 10.1007/s00280-015-2897-2. [DOI] [PubMed] [Google Scholar]
- 53.Qi X, Wong BL, Lau SH, Ng KT, Kwok SY. A hemoglobin-based oxygen carrier sensitized cisplatin based chemotherapy in hepatocellular carcinoma. Oncotarget. 2017;8:85311–85325. doi: 10.18632/oncotarget.19672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bruix J, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389:56–66. doi: 10.1016/S0140-6736(16)32453-9. [DOI] [PubMed] [Google Scholar]
- 55.El-Khoueiry AB, et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492–2502. doi: 10.1016/S0140-6736(17)31046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]