Abstract
Background
Er: YAG lasers (ERLs) show suitable characteristics for scaling and root planing, but previous studies have drawn conflicting conclusions. This meta-analysis aimed to systematically appraise the available evidence concerning the effectiveness of ERLs as an adjunct to scaling and root planing (SRP) for non-surgical periodontal treatment.
Material/Methods
Randomized controlled trials (RCTs) comparing ERLs+SRP with SRP alone for the treatment of chronic periodontitis were searched in 9 electronic biomedical databases up to January 2018. The weighted mean differences (WMDs) and 95% confidence intervals (CIs) were counted for probing depth (PD) reduction, clinical attachment level (CAL) gain, and visual analog scale (VAS) score. Heterogeneity was evaluated with the I2 statistic for interstudy comparisons and the χ2-based Q statistic for intra-study comparisons. Sensitivity analysis was conducted by switching to a random or fixed effect model based on the heterogeneity. Publication bias was measured by Begg’s test.
Results
Ten related RCTs met the inclusion criteria. There were statistically significant differences in the assessed clinical parameters at the three-month follow-up: PD reduction (WMD=0.32, 95%CI range from 0.14 to 0.51, p<0.001; p=0.003, I2=69.7%); CAL gain (WMD=0.31, 95%CI range from 0.22 to 0.40, p<0.001; p=0.209, I2=28.8%); and VAS scores (WMD=−1.38, 95%CI range from −2.45 to −0.31, p<0.001; p=0.182, I2=44%). There were no significant differences at the six- and twelve-month follow-ups. Sensitivity analysis revealed that the results were consistent. No evidence of publication bias was detected.
Conclusions
This systematic analysis demonstrated that ERLs+SRP provides additional short-term effectiveness and that patients experience less pain compared to SRP. There were no significant differences at the medium-term and long-term follow-ups. Long-term well-designed RCTs are required.
MeSH Keywords: Chronic Periodontitis; Dental Scaling; Lasers, Solid-State
Background
Chronic periodontitis (CP) is an infectious disease caused by microorganisms, which can lead to progressive destruction of the periodontal tissues and early tooth loss [1]. The typical clinical symptoms are attachment loss, formation of periodontal pockets, and bone absorption. Bacteria and their metabolites on plaque are an initial factor in the pathogenesis [2]. With a rough and poly-porous surface, dental calculus provides superior conditions for bacteria to colonize, proliferate, and cause disease [3]; thus, the primary objective of initial periodontal treatment is to eliminate bacteria and calculus on the root surface and maintain a biologically harmonious root surface [4,5].
Scaling and root planing (SRP), performed by hand or with ultrasonic devices, is a basic and essential procedure for CP treatment in first-stage periodontal therapy. Considerable evidence supports the view that hand-held instruments and ultrasonic devices have similar clinical effectiveness [6,7]. Both approaches have advantages and disadvantages. Hand-held instruments provide a better sense of touch for dentists to determine if the root surface is rough, but they require more time, physical effort, and special professional training. In comparison, ultrasonic devices have advantages of efficiency and less operator fatigue, but they have the risks of damaging the root surfaces, leaving aerosol contamination and generating vibrations that may lead to dental fear and discomfort [8]. Hand-held instruments and ultrasonic devices both have difficulties in accessing the anatomical variations, such as root concavities, root furcations, grooves, and the distal surfaces of molars [9].
Various types of lasers have been applied in periodontal treatments. Among all laser therapies, the use of Er: YAG lasers (ERLs) is most suitable for periodontal treatment [10, 11] because it is capable of achieving both soft- and hard-tissue ablation [12]. While Nd: YAG lasers, CO2 lasers, and diode lasers are suitable for removing soft tissue [12], if they are used for hard tissue removal, thermal adverse effects can lead to cracks on the root surfaces [13–15]. ERLs have an ideal wavelength of 2.94 um, which is close to the maximum absorption coefficient of water and hydroxyapatite. When ERLs are used to irradiating, the absorption of the energy by water and hydrous organic components rapidly builds up the evaporation of water, resulting in internal pressure and microexplosions in the calculus [16]. ERLs can be applied to remove subgingival calculus that traditional mechanical hand instruments cannot reach and to eliminate smear layers of infected cementum without thermal adverse effects [17–19]. Furthermore, ERLs possess bactericidal and endotoxic effects [20–22] and have the potential to accelerate cell proliferation and reattachment to the root surfaces [23–26]. Er,Cr: YSGG lasers are also applied in periodontal treatment as an adjunct to non-surgical periodontal treatment [27,28]. However, its wavelength is different from that of ERLs, so the present meta-analysis focusing on ERLs aimed to provide a precise systematic evaluation of the effectiveness of ERLs as an adjunct to SRP to guide clinical use in periodontal treatment.
Material and Methods
This meta-analysis was designed in advance, and followed the guidelines of the QUOROM statement [29] and the PRISMA statement [30].
PICOS question
A clinical questionnaire [31] was established by the participants, intervention, comparison, outcomes, and study design (PICOS) in this meta-analysis.
P: Chronic periodontal patients who needed non-surgical treatment.
I: ERLs as an adjunctive therapy to SRP.
C: SRP conducted with manual curettes and/or ultrasonic devices.
O: Clinical effectiveness and patients’ perceptions.
S: Randomized controlled trials (RCTs).
Search strategy
The following important biomedical electronic databases were searched for relevant publications until January 31, 2018: PubMed, the Cochrane Controlled Clinical Trial Register (CCCTR), Medline, EMBase, Science Direct, OVID, ISI Web of Knowledge, China National Knowledge Internet (CNKI), and the Chinese BioMedical Literature Database (CBM).
Search strategies were permuted and combined by medical subheadings (MeSH) and keywords as the following phrases:
(“Periodontitis” [MeSH] OR “Chronic Periodontitis” [MeSH] OR “Periodontal Diseases” [MeSH]) AND (“Lasers, Solid-State” [MeSH] OR “Erbium” [MeSH] OR “Lasers” [MeSH] OR “Laser Therapy” [MeSH] OR “erbium yttrium aluminum garnet”) AND (“periodontal non-surgical treatment” OR “periodontal non-surgical therapy” OR “scaling root planing” OR “dental scaling” OR “periodontal treatment” OR “periodontal therapy” OR “Dental Scaling”[MeSH] OR “Root Planing” [MeSH]) AND (“periodontal pocket*” OR “pocket depth” OR “plaque index” OR “dental plaque” OR “dental calculus” OR “attachment loss” OR “clinical attachment level” OR “Periodontal Pocket”[MeSH] OR “Periodontal Attachment Loss”[MeSH]).
search strategy in PubMed was
#1 “Lasers, Solid-State” [MeSH] OR “Erbium” [MeSH] OR “Lasers” [MeSH].
#2 “scaling root planing” OR “Dental Scaling” [MeSH] OR “Root Planing” [MeSH].
#3 “Periodontitis” [MeSH] OR “Chronic Periodontitis” [MeSH].
#4 randomized controlled trials.
#5 #1AND#2AND#3AND#4.
Furthermore, the references of selected full-text articles and related reviews were scrutinized to obtain potentially relevant studies. Only published articles in Chinese and English languages were included. No restriction was applied concerning the publication year.
All searched articles from different databases were entered into NoteExpress. Sifting was performed independently by 2 researchers to minimize the potential bias among researchers. Preliminary selection was achieved by screening titles and abstracts and secondary selection was conducted by screening full-text articles. Disagreements on the inclusion or exclusion of the retrieved papers were resolved by discussion.
Inclusion criteria
A1: Randomized clinical trials
A2: General CP patients who needed non-surgical periodontal treatment
A3: ERLs adjunctive to traditional SRP by hand or/and ultrasonic devices compared with SRP alone
A4: Clinical parameters
Exclusion criteria
B1: Studies not designed as a randomized clinical trial
B2: Patients who were aged ≤15 years old, who had other types of periodontitis, who had systematic diseases, who took antibiotics or medications that could alter the investigated clinical effect, who received periodontal therapy in the past 6 months, or who were pregnant
B3: Surgical therapy or maintenance therapy
B4: The WMD value of the curative effect indicator data and the 95%CI data cannot be extracted, converted or used
Study characteristics
The following information was collected for each included publication: study design, number of patients, the devices used in the test and control groups, and clinical effectiveness with the follow-up period. Discrepancies were solved by discussions. Data were independently extracted from included full-text publications by 2 researchers.
Quality assessment
A methodological quality evaluation of all included RCTs was conducted independently by 2 researchers using the Jadad score scale [32]. The evaluation standard consisted of random sequence generation, randomized concealment, blinding, and loss to follow-up. The first 3 standards were scored as appropriate (2 scores), unclear (1 score), or inappropriate (0 score) and the fourth standard was scored described (1 score) or no (0 score). Total scores ranging from 1 to 4 were rated as low quality, and total scores ranging from 5 to 7 were rated as high quality.
Statistical analysis
Heterogeneity was evaluated by a Q test. Significant heterogeneity was indicated by p<0.1. A random-effects model was selected to calculate the weighted mean differences (WMDs) and their 95%CIs when heterogeneity was high (p<0.1); otherwise, a fixed-effects model was applied [33]. For WMD, p<0.01 was considered statistically significant.
Sensitivity analysis was conducted by switching effect models. The presence of publication bias was investigated for each outcome of interest by Begg’s test for quantitative analysis [34]. Publication bias existed at p value<0.1. All statistical analyses were conducted using Stata 11 Intercooled (Stata Corporation, College Station, TX, USA).
Results
Search results
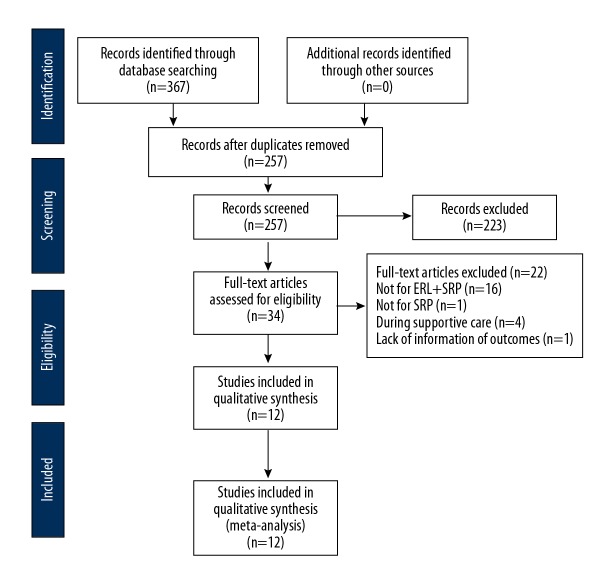
As shown in Figure 1, there were 367 related studies, from which 110 duplicate articles were identified and deleted. Based on viewing of titles and abstracts, 223 papers were excluded; after screening the full text, 22 articles were excluded. Finally, 12 articles (10 RCTs) entered the quality assessment and data extraction stage. The characteristics of the eligible studies are shown in Table 1. A total of 307 patients participated, and 301 patients finished the 10 pooled studies.
Figure 1.
Flow chart of search results.
Table 1.
Characteristic of included studies.
| Study | Design | Patients | Test group | Control group | Outcomes |
|---|---|---|---|---|---|
| Ming [35] | Split mouth | 18 patients | Ultrasonic+ ERLs | Ultrasonic | 6 months PD, CAL |
| Fengzhou [36] | Split mouth | 30 patients | Ultrasonic+ Manual+ ERLs | Ultrasonic+ manual | 1, 3 months PD |
| Weiyan [37] | Parallel arm | 82 patients | Manual+ Ultrasonic+ ERLs | Manual+ ultrasonic devices | VAS |
| Kaiyue [38] | Split mouth | 11 patients | Manual+ Ultrasonic+ ERLs | Ultrasonic+ manual | 3 months PD, CAL |
| Shuxia [39] | Parallel arm | 40 patients | Ultrasonic+ ERLs | Ultrasonic | 1.5, 3 months CAL |
| Lopes [40,41] | Split mouth quadrant | 21–19 patients | Manual+ ERLs | Manual | 1, 3, 6, 12 months PD, CAL |
| Rotundo [42] | Split mouth quadrant | 27-26patients | Manual+ Ultrasonic+ ERLs | Ultrasonic+ manual | 3, 6 months PD, CAL, VAS |
| Yilmaz [43] | Parallel arm | 18 patients | SRP+ ERLs | SRP | 3 months PD, CAL |
| Yilmaz [44] | Parallel arm | 20 patients | SRP+ ERLs | SRP | 3 months PD, CAL |
| Sanz-Sánchez [45,46] | Parallel arm | 40–37 patients | Ultrasonic+ ERLs | Ultrasonic | 3, 6, 12 months PD, CAL |
Risk of bias within studies
Analysis of the methodological quality of the included RCTs revealed that 6 studies had a low risk of bias [38,40–46] and the other 4 were at high risk of bias [35–37,39]. The results of the Jadad scale quality analysis are presented in Table 2.
Table 2.
Quality assessment of studies.
| Study | Random generation | Allocation concealment | Blinded method | Lost of follow-up | Score |
|---|---|---|---|---|---|
| Ming 2015 [35] | Random | Unclear | Unclear | Not mentioned | 3 |
| Fengzhou 2016 [36] | Toss a coin | Unclear | Unclear | Not mentioned | 4 |
| LuoWeiyan 2017 [37] | Random number table | Unclear | Unclear | Not mentioned | 4 |
| Kaiyue 2017 [38] | Computer | Unclear | Examiner blinded | Not mentioned | 5 |
| Shuxia 2017 [39] | Random | Unclear | Examiner blinded | Not mentioned | 4 |
| Lopes 2008 [40], 2010 [41] | Computer | Sealed envelopes | Examiner blinded | Described | 7 |
| Rotundo 2010 [42] | Computer | Unclear | Examiner blinded | Described | 6 |
| Yilmaz 2012 [43] | Computer | Unclear | Examiner blinded | Not mentioned | 5 |
| Yilmaz 2013 [44] | Computer | Unclear | Examiner blinded | Not mentioned | 5 |
| Sanz-Sánchez 2015 [45], 2016 [46] | Computer | Sealed envelopes | Examiner blinded | Described | 7 |
Meta-analysis results
The outcomes of interest were changes in probing depth (PD), clinical attachment level (CAL) measured separately from baseline to 3-, 6-, and 12-month follow-ups, and visual analog scale (VAS) scores immediately after treatment.
PD reduction
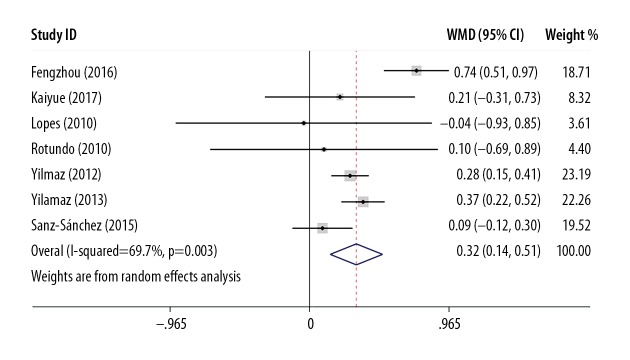
A significant difference in PD reduction in favor of ERLs+SRP compared to SRP was observed at the 3-month follow-up, as shown in Figure 2 (WMD=0.33, 95%CI range 0.25 to 0.41, p<0.001), with heterogeneity (χ2=19.83, p=0.003, I2=69.7%). As high heterogeneity was detected, the study by Li Fengzhou [36] was excluded because its methodological quality was low. The heterogeneity was substantially decreased (χ2=5.27, p=0.39, I2=5.1%), and the result was consistent (WMD=0.27, 95%CI range 0.18 to 0.36, p<0.001).
Figure 2.
Funnel plot of PD reduction at 3-month follow-up.
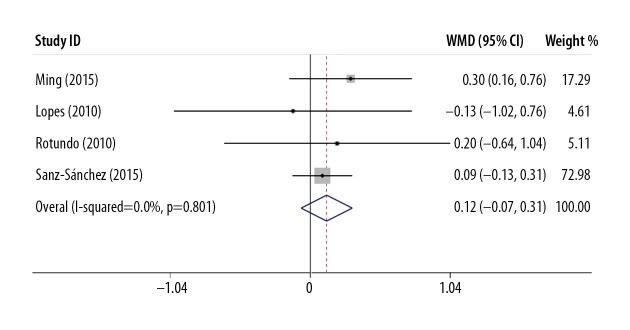
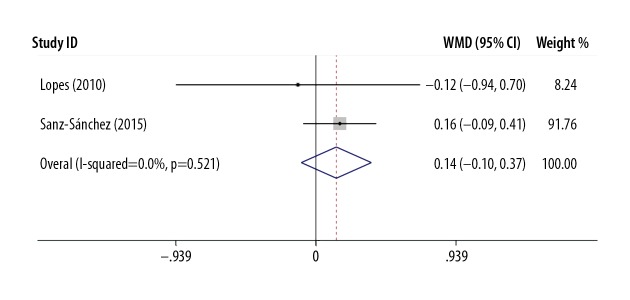
No significant difference in PD reduction was observed in favor of ERLs+SRP compared to SRP at the 6-month follow-up, as shown in Figure 3 (WMD=0.12, 95%CI range −0.07 to 0.31, p=0.21) without heterogeneity (χ2=1.00, p=0.80, I2=0%); the data for the 12-month follow-up are shown in Figure 4 (WMD=0.14, 95%CI range −0.10 to 0.37, p=0.25), with no heterogeneity (χ2=0.41, p=0.52, I2=0%).
Figure 3.
Funnel plot of PD reduction at 6-month follow-up.
Figure 4.
Funnel plot of PD reduction at 12-month follow-up.
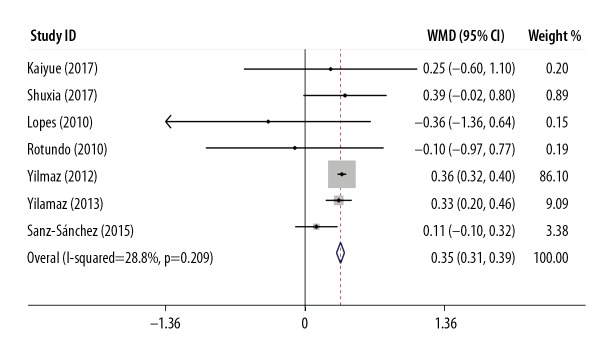
CAL gain
Significant differences in the 3-month outcomes were observed (WMD=0.35, 95%CI range 0.31 to 0.39, p<0.001), with low heterogeneity (χ2=8.42, p=0.209, I2=28.8%). Forest plots for the CAL gain at the 3-month follow-up are shown in Figure 5.
Figure 5.
Funnel plot of CAL gain at 3-month follow-up.
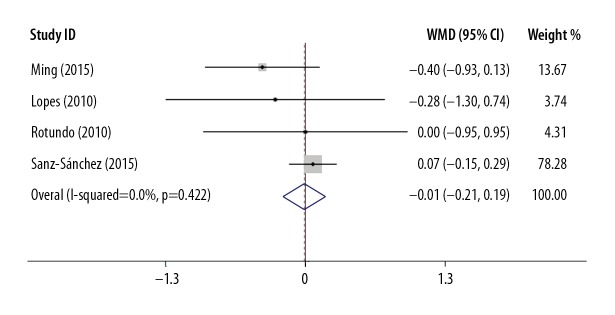
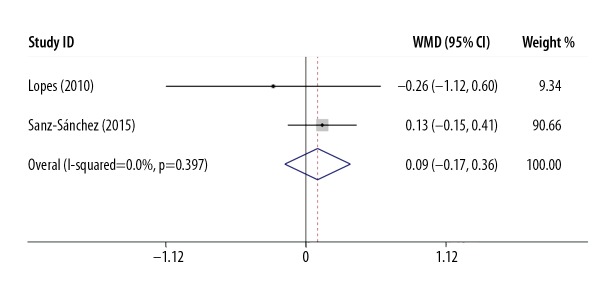
No significant difference in CAL gain was observed between ERLs+SRP and SRP, as shown in Figure 6, at the 6-month follow-up (WMD=−0.01, 95%CI range −0.21 to 0.19, p=0.92) without heterogeneity (χ2=2.81, p=0.422, I2=0%); the 12-month follow-up is shown in Figure 7 (WMD=0.09, 95%CI range −0.17 to 0.36, p=0.49) without heterogeneity (χ2=0.72, p=0.397, I2=0%).
Figure 6.
Funnel plot of CAL gain at 6-month follow-up.
Figure 7.
Funnel plot of CAL gain at 12-month follow-up.
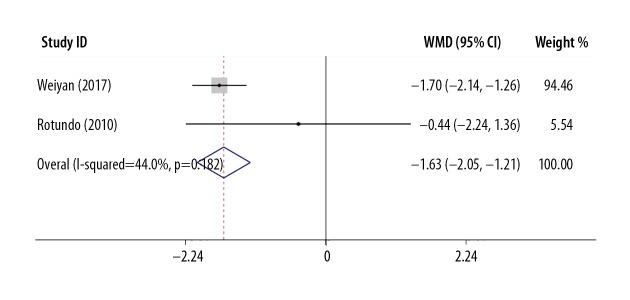
VAS
A significant difference was observed in favor of ERLs+SRP compared to SRP (WMD=−1.63, 95%CI range −2.05 to −0.21, p<0.001) with moderate heterogeneity (χ2=1.78, p=0.182, I2=44%). Forest plots for VAS are shown in Figure 8.
Figure 8.
Funnel plot of VAS immediately after treatment.
Sensitivity analysis
Sensitivity analysis was conducted by switching the effect model for all investigated parameters at all follow-up periods. All results remained consistent, indicating that the results were stable.
Publication bias
Publication bias was investigated by Begg’s test for quantitative analysis, in terms of PD reduction, p=1.000; and in terms of the CAL gain p=0.23. All p values were greater than 0.1 and indicated the absence of publication bias.
Discussion
Superior to the previous study
This meta-analysis systematically evaluated available clinical evidence concerning ERLs as an adjunct to SRP, published up to January 2018, with 307 pooled patients from 10 RCTs, and quantitatively assessed 3 clinical parameters that were evaluated separately according to follow-up period. Additionally, sensitivity analysis was performed and publication bias was assessed. These advantages increase the reliability and stability of the results over those of the previous study [47]; thus, this meta-analysis is the most comprehensive evaluation to date of the clinical effectiveness of ERLs+SRP.
Summary of the main findings
The notable findings of this meta-analysis indicated that significant differences were observed at the short-term (3-month) follow-up in favor of ERLs+SRP in terms of PD reduction and CAL gain, with moderate or low heterogeneity, respectively. The main source of heterogeneity appears to originate from the study by Li Fengzhou [36], for which the methodological quality was low. After excluding that study, the heterogeneity substantially decreased, and the results remained consistent. The medium-term and long-term follow-up of clinical parameters of PD and CAL changes showed no differences. These results could be interpreted partially as showing that ERLs can remove smear layers, can accelerate periodontal ligament fibroblasts and blood cell adherence to the root surface, and can eliminate endotoxins and bacteria [48]. Although the medium- and long-term clinical effects were closely related to initial treatment, treatment effectiveness diminished over time and was affected by confounding factors such as the frequency of maintenance care, dietary habits, the patients’ oral hygiene habits, systemic disorders, and the host immune response [49].
In terms of patients’ perceptions during treatment, ERLs+SRP had an advantage over SRP as measured by VA,S with moderate heterogeneity. This result was in accordance with a clinical trial that applied 2 methods to measure patients’ pain perceptions during supportive care [50]. ERLs were characterized by no vibration and little sound, patients may perceive less fear and nervousness, and thus experience less pain. In addition, the mechanism may have potential relevance because ERLs were capable of melting exposed fresh dentinal tubules and cementum caused by SRP [51].
The parameters investigated in this meta-analysis are crucial for periodontal treatment. PD and CAL are the most frequently used and the most informative parameters for estimating the severity of inflammation as well as the response to treatment during periodontal therapy [52]. The VAS is used to measure patients’ perception of pain. Pain experienced during treatment should be discussed, not only due to the treatment itself, but also due to dental fear caused by pain, which may result in missing appointments and affect the effectiveness of periodontal treatment [49].
Quality of evidence
The studies included in this meta-analysis were low in methodological quality, presuming a limitation in methodology. The most frequently unsatisfied methodological criterion was the absence of allocation concealment, as only 2 studies used the correct method. In 8 RCTs, blinding methods were adapted for outcome examiners (but not for patients and doctors) for the differences in devices and procedures between the test and control groups, and the blinding methods of other studies were unclear. Five of the 10 RCTs [37,39,43–46] used the correct parallel randomization, while 5 of the 10 RCTs [35,36,38,40–42] used a split-mouths design, which has the potential disadvantage of within-patient bias for carry-across effects [53].
The heterogeneity could be caused by differences among the included studies, such as different inclusion criteria for CP patients, the combined use of calculus detection systems, ERLs parameter settings, the inclusion of smokers, and study design method.
Sensitivity analysis was conducted, and consistent results were achieved. Analysis of publication bias was performed. The trim-and-fill analysis assumed no missing studies. Begg’s test revealed no publication bias. Therefore, the possibility of publication bias can be excluded.
Limitations
Limitation of the evidence
Lasers, unlike other instruments, have no defined and accepted protocols for standard usage in periodontal treatment [54–56], and the studies included in this meta-analysis used different power parameter settings. There were also different inclusion criteria for long-term periodontal patients among the included studies. Smoking is a risk factor for CP [57]; 2 RCTs [42,45,46] involved both smokers and non-smokers, and although an intergroup balance was achieved at baseline, the outcomes affected by this confounding factor were unknown. Some of the included studies were small in terms of sample size, which may have led to a problem with low statistical power. Some included studies tested different numbers of sites on different numbers of teeth, with different tooth positions. These confounding factors discussed above may have increased the interstudy heterogeneity. Evidence focused on long-term clinical outcomes is still lacking. The expense of lasers is a main barrier to broader use, but no evidence has addressed their cost-effectiveness. Adverse events were evaluated in only 1 study, by Rotundo [42]. Two periodontal abscesses were observed in the ERLs+SRP group, while no periodontal abscesses were found in the SRP group. There was no additional discussion about this issue.
Limitation of the meta-analysis
Articles published only in English and Chinese were selected for this systematic review. These choices might have led to bias in the results of important studies published in languages other than English and Chinese.
Implications for clinical practice
The results of this meta-analysis suggest that ERLs as an adjunct to SRP could provide better short-term clinical effectiveness than SRP alone. However, these benefits were not stable after a long follow-up period. Therefore, dentists should comprehensively balance the cost and benefits for patients and the convenience the clinicians may experience. Although the benefit achieved was not outstanding, patients with moderate or advanced periodontal disease would benefit from this improvement, because it takes long-term repeated supportive periodontal care, and this benefit might be superimposed. Based on the hemostasis characteristics of ERLs [12], patients with hypertensive diseases and hemagglutination inhibition, such as hematological disorders, diabetes, and hepatic disease, would likely benefit from this new instrument.
Implications for research
As discussed above, the following recommendations have been made. First, parallel-arm controlled, large sample-size, long-term clinical trials are needed in future studies, and clinical trials should be of high methodological quality, like the CONSORT statement [58]. Second, to achieve the best efficacy and safety, studies on clinical practice protocols for achieving safe use, such as power settings, pulse durations, and repetition rates, are needed. Third, evidence is needed to address the choice for patients and doctors concerning cost-effect analysis, and patients’ perceptions of pain, as well as doctor training and ability to operate the lasers.
Conclusions
ERLs as an adjunct to SRP may have additional benefits in the short-term, as patients experience less pain compared to SRP. There were no significant differences in clinical effectiveness at the medium- and long-term follow-ups. Long-term, well-designed RCTs are required in the future.
Footnotes
Conflicts of interest
None.
Source of support: Departmental sources
References
- 1.Kinane DF. Causation and pathogenesis of periodontal disease. Periodontology 2000. 2001;25:8–20. doi: 10.1034/j.1600-0757.2001.22250102.x. [DOI] [PubMed] [Google Scholar]
- 2.Cekici A, Kantarci A, Hasturk H, Van Dyke TE. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontology 2000. 2014;64(1):57–80. doi: 10.1111/prd.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White DJ. Dental calculus: Recent insights into occurrence, formation, prevention, removal and oral health effects of supragingival and subgingival deposits. Eur J Oral Sci. 1997;105(5 Pt 2):508–22. doi: 10.1111/j.1600-0722.1997.tb00238.x. [DOI] [PubMed] [Google Scholar]
- 4.Dentino A, Lee S, Mailhot J, Hefti AF. Principles of periodontology. Periodontology 2000. 2013;61:16–53. doi: 10.1111/j.1600-0757.2011.00397.x. [DOI] [PubMed] [Google Scholar]
- 5.Slots J. Periodontology: Past, present, perspectives. Periodontology 2000. 2013;62:7–19. doi: 10.1111/prd.12011. [DOI] [PubMed] [Google Scholar]
- 6.Tunkel J, Heinecke A, Flemmig TF. A systematic review of efficacy of machine-driven and manual subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol. 2002;29(Suppl 3):72–81. doi: 10.1034/j.1600-051x.29.s3.4.x. discussion 90–91. [DOI] [PubMed] [Google Scholar]
- 7.Walmsley AD, Lea SC, Landini G, Moses AJ. Advances in power driven pocket/root instrumentation. J Clin Periodontol. 2008;35(8 Suppl):22–28. doi: 10.1111/j.1600-051X.2008.01258.x. [DOI] [PubMed] [Google Scholar]
- 8.Oda S, Nitta H, Setoguchi T, et al. Current concepts and advances in manual and power-driven instrumentation. Periodontology 2000. 2004;36:45–58. doi: 10.1111/j.1600-0757.2004.03674.x. [DOI] [PubMed] [Google Scholar]
- 9.Crespi R, Barone A, Covani U. Histologic evaluation of three methods of periodontal root surface treatment in humans. J Periodontol. 2005;76(3):476–81. doi: 10.1902/jop.2005.76.3.476. [DOI] [PubMed] [Google Scholar]
- 10.Aoki A, Ando Y, Watanabe H, Ishikawa I. In vitro studies on laser scaling of subgingival calculus with an erbium: YAG laser. J Periodontol. 1994;65(12):1097–106. doi: 10.1902/jop.1994.65.12.1097. [DOI] [PubMed] [Google Scholar]
- 11.Aoki A, Miura M, Akiyama F, et al. In vitro evaluation of Er: YAG laser scaling of subgingival calculus in comparison with ultrasonic scaling. J Periodontal Res. 2000;35(5):266–77. doi: 10.1034/j.1600-0765.2000.035005266.x. [DOI] [PubMed] [Google Scholar]
- 12.Gaspirc B, Skaleric U. Morphology, chemical structure and diffusion processes of root surface after Er: YAG and Nd: YAG laser irradiation. J Clin Periodontol. 2001;28(6):508–16. doi: 10.1034/j.1600-051x.2001.028006508.x. [DOI] [PubMed] [Google Scholar]
- 13.Yaneva B, Firkova E, Karaslavova E, Romanos GE. Bactericidal effects of using a fiber-less Er: YAG laser system for treatment of moderate chronic periodontitis: Preliminary results. Quintessence Int. 2014;45(6):489–97. doi: 10.3290/j.qi.a31803. [DOI] [PubMed] [Google Scholar]
- 14.Ando Y, Aoki A, Watanabe H, Ishikawa I. Bactericidal effect of erbium YAG laser on periodontopathic bacteria. Lasers Surg Med. 1996;19(2):190–200. doi: 10.1002/(SICI)1096-9101(1996)19:2<190::AID-LSM11>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 15.Folwaczny M, Mehl A, Aggstaller H, Hickel R. Antimicrobial effects of 2.94 microm Er: YAG laser radiation on root surfaces: An in vitro study. J Clin Periodontol. 2002;29(1):73–78. doi: 10.1034/j.1600-051x.2002.290111.x. [DOI] [PubMed] [Google Scholar]
- 16.Ogita M, Tsuchida S, Aoki A, et al. Increased cell proliferation and differential protein expression induced by low-level Er: YAG laser irradiation in human gingival fibroblasts: Proteomic analysis. Lasers Med Sci. 2015;30(7):1855–66. doi: 10.1007/s10103-014-1691-4. [DOI] [PubMed] [Google Scholar]
- 17.Belal MH, Watanabe H. Comparative study on morphologic changes and cell attachment of periodontitis-affected root surfaces following conditioning with CO2 and Er: YAG laser irradiations. Photomed Laser Surg. 2014;32(10):553–60. doi: 10.1089/pho.2014.3769. [DOI] [PubMed] [Google Scholar]
- 18.Oliveira GJ, Theodoro LH, Marcantonio JE, et al. Effect of Er, Cr: YSGG and Er: YAG laser irradiation on the adhesion of blood components on the root surface and on root morphology. Braz Oral Res. 2012;26(3):256–62. doi: 10.1590/s1806-83242012000300012. [DOI] [PubMed] [Google Scholar]
- 19.Crespi R, Romanos GE, Cassinelli C, Gherlone E. Effects of Er: YAG laser and ultrasonic treatment on fibroblast attachment to root surfaces: An in vitro study. J Periodontol. 2006;77(7):1217–22. doi: 10.1902/jop.2006.050416. [DOI] [PubMed] [Google Scholar]
- 20.Aoki A, Sasaki KM, Watanabe H, Ishikawa I. Lasers in nonsurgical periodontal therapy. Periodontology 2000. 2004;36:59–97. doi: 10.1111/j.1600-0757.2004.03679.x. [DOI] [PubMed] [Google Scholar]
- 21.Israel M, Cobb CM, Rossmann JA, Spencer P. The effects of CO2, Nd: YAG and Er: YAG lasers with and without surface coolant on tooth root surfaces. An in vitro study. J Clin Periodontol. 1997;24(9 Pt 1):595–602. doi: 10.1111/j.1600-051x.1997.tb00235.x. [DOI] [PubMed] [Google Scholar]
- 22.Theodoro LH, Haypek P, Bachmann L, et al. Effect of ER: YAG and diode laser irradiation on the root surface: Morphological and thermal analysis. J Periodontol. 2003;74(6):838–43. doi: 10.1902/jop.2003.74.6.838. [DOI] [PubMed] [Google Scholar]
- 23.Schwarz F, Sculean A, Berakdar M, et al. In vivo and in vitro effects of an Er: YAG laser, a GaAlAs diode laser, and scaling and root planing on periodontally diseased root surfaces: A comparative histologic study. Lasers Surg Med. 2003;32(5):359–66. doi: 10.1002/lsm.10179. [DOI] [PubMed] [Google Scholar]
- 24.Schwarz F, Aoki A, Becker J, Sculean A. Laser application in non-surgical periodontal therapy: A systematic review. J Clin Periodontol. 2008;358:29–44. doi: 10.1111/j.1600-051X.2008.01259.x. [DOI] [PubMed] [Google Scholar]
- 25.Passanezi E, Damante CA, de Rezende ML, Greghi SL. Lasers in periodontal therapy. Periodontol 2000. 2015;67(1):268–91. doi: 10.1111/prd.12067. [DOI] [PubMed] [Google Scholar]
- 26.Ishikawa I, Aoki A, Takasaki AA. Potential applications of Erbium: YAG laser in periodontics. J Period Res. 2004;39(4):275–85. doi: 10.1111/j.1600-0765.2004.00738.x. [DOI] [PubMed] [Google Scholar]
- 27.Kelbauskiene S, Baseviciene N, Goharkhay K, et al. One-year clinical results of Er,Cr: YSGG laser application in addition to scaling and root planing in patients with early to moderate periodontitis. Lasers Med Sci. 2011;26(4):445–52. doi: 10.1007/s10103-010-0799-4. [DOI] [PubMed] [Google Scholar]
- 28.Dereci O, Hatipoglu M, Sindel A, et al. The efficacy of Er,Cr: YSGG laser supported periodontal therapy on the reduction of peridodontal disease related oral malodor: A randomized clinical study. Head Face Med. 2016;12(1):20. doi: 10.1186/s13005-016-0116-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moher D, Cook DJ, Eastwood S, et al. Improving the quality of reports of meta-analyses of randomised controlled trials: The QUOROM statement. Onkologie. 2000;23(6):597–602. doi: 10.1159/000055014. [DOI] [PubMed] [Google Scholar]
- 30.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ. 2015;349:g7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 31.Schlosser RW, Koul R, Costello J. Asking well-built questions for evidence-based practice in augmentative and alternative communication. J Commun Disord. 2007;40(3):225–38. doi: 10.1016/j.jcomdis.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 32.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 33.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101. [PubMed] [Google Scholar]
- 35.Ming C. [The clinical effect of erbium laser assisted treatment of chronic periodontitis]. Modern Medicine Journal of China. 2015;11:59–61. [in Chinese] [Google Scholar]
- 36.Zhou LF, Fan X. [A short-term clinical effect observation of Er: YAG laser assisted treatment of chronic periodontitis]. Journal of Prevention and Treatment for Stomatological Diseases. 2016;(03):170–73. [in Chinese] [Google Scholar]
- 37.Weiyan L, Yuyue H, Zhijuan Z, et al. [Study On the clinical effect of Er: YAG laser assisted ultrasound therapy instrument in periodontitis patients]. Nursing Practice and Research. 2017;(11):10–12. [in Chinese] [Google Scholar]
- 38.Kaiyue W, Chunjiao X, Yutan C, et al. [Detection of Dickkopf-1 and alkaline phosphatase activity in gingival crevicular fluid from chronic periodontitis with Er: YAG laser as an adjunctive treatment]. Shanghai Journal of Stomatology. 2017;(03):285–89. [in Chinese] [PubMed] [Google Scholar]
- 39.Shuxia S, Shaojun Z, Na L, Peizhen S. [Short term clinical effect of Er: YAG laser for chronic periodontitis]. Shandong Medical Journal. 2017;(10):98–99. [in Chinese] [Google Scholar]
- 40.Lopes BM, Marcantonio RA, Thompson GM, et al. Short-term clinical and immunologic effects of scaling and root planing with Er: YAG laser in chronic periodontitis. J Periodontol. 2008;79(7):1158–67. doi: 10.1902/jop.2008.070600. [DOI] [PubMed] [Google Scholar]
- 41.Lopes BMV, Theodoro LH, Melo RF, et al. Clinical and microbiologic follow-up evaluations after non-surgical periodontal treatment with erbium: YAG laser and scaling and root planing. J Periodontol. 2010;81(5):682–91. doi: 10.1902/jop.2010.090300. [DOI] [PubMed] [Google Scholar]
- 42.Rotundo R, Nieri M, Cairo F, et al. Lack of adjunctive benefit of Er: YAG laser in non-surgical periodontal treatment: A randomized split-mouth clinical trial. J Clin Periodontol. 2010;37(6):526–33. doi: 10.1111/j.1600-051X.2010.01560.x. [DOI] [PubMed] [Google Scholar]
- 43.Yilmaz S, Kut B, Gursoy H, et al. Er: YAG laser versus systemic metronidazole as an adjunct to nonsurgical periodontal therapy: A clinical and microbiological study. Photomed Laser Surg. 2012;30(6):325–30. doi: 10.1089/pho.2010.2762. [DOI] [PubMed] [Google Scholar]
- 44.Yılmaz S, Algan S, Gursoy H, et al. Evaluation of the clinical and antimicrobial effects of the Er: YAG laser or topical gaseous ozone as adjuncts to initial periodontal therapy. Photomed Laser Surg. 2013;31(6):293–98. doi: 10.1089/pho.2012.3379. [DOI] [PubMed] [Google Scholar]
- 45.Sanz-Sanchez I, Ortiz-Vigon A, Matos R, et al. Clinical efficacy of subgingival debridement with adjunctive erbium: Yttrium-aluminum-garnet laser treatment in patients with chronic periodontitis: A randomized clinical trial. J Periodontol. 2015;86(4):527–35. doi: 10.1902/jop.2014.140258. [DOI] [PubMed] [Google Scholar]
- 46.Sanz-Sanchez I, Ortiz-Vigon A, Herrera D, Sanz M. Microbiological effects and recolonization patterns after adjunctive subgingival debridement with Er: YAG laser. Clin Oral Investig. 2016;20(6):1253–61. doi: 10.1007/s00784-015-1617-y. [DOI] [PubMed] [Google Scholar]
- 47.Zhao Y, Yin Y, Tao L, et al. Er: YAG laser versus scaling and root planing as alternative or adjuvant for chronic periodontitis treatment: A systematic review. J Clin Periodontol. 2014;41(11):1069–79. doi: 10.1111/jcpe.12304. [DOI] [PubMed] [Google Scholar]
- 48.Lavu V, Sundaram S, Sabarish R, Rao SR. Root surface bio-modification with erbium lasers- a myth or a reality? Open Dent J. 2015;9:79–86. doi: 10.2174/1874210601509010079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Axelsson P, Lindhe J. The significance of maintenance care in the treatment of periodontal disease. J Clin Periodontol. 1981;8(4):281–94. doi: 10.1111/j.1600-051x.1981.tb02039.x. [DOI] [PubMed] [Google Scholar]
- 50.Braun A, Jepsen S, Deimling D, Ratka-Kruger P. Subjective intensity of pain during supportive periodontal treatment using a sonic scaler or an Er: YAG laser. J Clin Periodontol. 2010;37(4):340–45. doi: 10.1111/j.1600-051X.2010.01536.x. [DOI] [PubMed] [Google Scholar]
- 51.Belal MH, Yassin A. A comparative evaluation of CO2 and erbium-doped yttrium aluminium garnet laser therapy in the management of dentin hypersensitivity and assessment of mineral content. J Periodontal Implant Sci. 2014;44(5):227–34. doi: 10.5051/jpis.2014.44.5.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Caton J, Greenstein G, Polson AM. Depth of periodontal probe penetration related to clinical and histologic signs of gingival inflammation. J Periodontol. 1981;52(10):626–29. doi: 10.1902/jop.1981.52.10.626. [DOI] [PubMed] [Google Scholar]
- 53.Hujoel PP, DeRouen TA. Validity issues in split-mouth trials. J Clin Periodontol. 1992;19(9 Pt 1):625–27. doi: 10.1111/j.1600-051x.1992.tb01709.x. [DOI] [PubMed] [Google Scholar]
- 54.Folwaczny M, Mehl A, Haffner C, et al. Root substance removal with Er: YAG laser radiation at different parameters using a new delivery system. J Periodontol. 2000;71(2):147–55. doi: 10.1902/jop.2000.71.2.147. [DOI] [PubMed] [Google Scholar]
- 55.Folwaczny M, Thiele L, Mehl A, Hickel R. The effect of working tip angulation on root substance removal using Er: YAG laser radiation: An in vitro study. J Clin Periodontol. 2001;28(3):220–26. doi: 10.1034/j.1600-051x.2001.028003220.x. [DOI] [PubMed] [Google Scholar]
- 56.Crespi R, Romanos GE, Barone A, et al. Er: YAG laser in defocused mode for scaling of periodontally involved root surfaces: An in vitro pilot study. J Periodontol. 2005;76(5):686–90. doi: 10.1902/jop.2005.76.5.686. [DOI] [PubMed] [Google Scholar]
- 57.Johnson GK, Guthmiller JM. The impact of cigarette smoking on periodontal disease and treatment. Periodontol 2000. 2007;44:178–94. doi: 10.1111/j.1600-0757.2007.00212.x. [DOI] [PubMed] [Google Scholar]
- 58.Moher D, Schulz KF, Altman DG. The CONSORT statement: Revised recommendations for improving the quality of reports of parallel-group randomized trials. J Am Podiatr Med Assoc. 2001;91(8):437–42. doi: 10.7547/87507315-91-8-437. [DOI] [PubMed] [Google Scholar]