The scourge of tuberculosis has afflicted mankind for thousands of years. Today, although often regarded as a disease of the past, tuberculosis is still globally the number one cause of death among infectious diseases, ranking above HIV/AIDS (1). Few also appreciate that drug-resistant tuberculosis accounts for a sizable proportion of the problem of antimicrobial resistance (AMR); it has been estimated that it accounts for a quarter of AMR-associated deaths (2). Throughout the 20th century large declines in tuberculosis incidence have been observed, as a result of socioeconomic development and the application of effective drug treatments and comprehensive control efforts. However, this has not benefitted all countries, nor has it been enough to eliminate tuberculosis as a global public health threat. The emergence of multidrug- and extensively drug-resistant forms of tuberculosis (MDR-TB and XDR-TB), and of global challenges like war, migration, deprivation, inequality and social upheaval, collectively threaten to reverse the progress made in fighting tuberculosis.
In 1993 the World Health Organization (WHO) declared tuberculosis a global health emergency, and brought forward specific control strategies accompanied by ambitious goals: the DOTS strategy (until 2005), the Stop TB strategy (2006–2015) and the End TB strategy (2016–2035) which was endorsed by WHO member states in 2014. End TB has set the most ambitious goals yet: a 90% reduction in tuberculosis incidence and 95% reduction in tuberculosis deaths by 2035 compared with 2015. To achieve these, it promotes political commitment and government stewardship as a pillar of the overall strategy. In that, it certainly appears successful; the first global ministerial conference on tuberculosis was held November 2017 in Moscow, Russia, and produced the “Moscow Declaration to End TB” (3). This meeting is to be followed by another first, a session for heads of state to discuss tuberculosis at the UN General Assembly in September 2018.
Ahead of this seminal event, WHO recently published a comprehensive review on the current status of the global tuberculosis epidemic (1). What do we learn from this interesting article? First the good news; important progress has been made, with global tuberculosis incidence and mortality declining between 2000 and 2016. The current (2015–2016) annual rate of decline was 1.9% for incidence and 4% for mortality (for all tuberculosis deaths, including those among HIV-positive persons). The number of tuberculosis patients that are being diagnosed and treated is on the rise, including patients with drug-resistant forms. There are multiple new diagnostic tests in various stages of development or already in use, including rapid tests for drug-resistance such as the Xpert MTB/RIF and line probe assays. Most importantly, ten completely new drugs for tuberculosis are currently being tested in phase I, II or III trials; this includes two drugs, bedaquiline and delamanid, that have been already provisionally approved for use in MDR-TB. Bedaquiline and delamanid provide two new and sorely needed treatment options for these patients, and represent the first new anti-TB medicines in almost half a century. Multiple candidate vaccines for tuberculosis are also in development.
All is hardly well though. In order to achieve the ambitious targets set, the current rate of decline in global tuberculosis incidence needs to accelerate significantly to 4–5% per year in 2020, and 10% in 2025. Currently only few countries and regions show declines of more than 4% per year, and mostly in Europe, rather than in the countries with the highest tuberculosis burden. Achieving the 2025 target will be very difficult without new drug therapies, new diagnostics, but most of all intensified organized tuberculosis control efforts. However, the world is already failing at the very first step; WHO estimates that only 61% of the 10.4 million new tuberculosis cases per year are getting diagnosed and started on treatment, falling to just 22% for drug-resistant tuberculosis. Thus, too many patients with tuberculosis do not get a chance to receive the care they need. Even for those who do start treatment, the global treatment success rate has been 83% overall (for all cases), falling to just 54% for drug-resistant tuberculosis and 30% for XDR-TB, according to the latest WHO data (1). The large majority of eligible MDR-TB patients have not been able to receive bedaquiline and delamanid (4), which could be lifesaving for them; the main reasons for this is the current insufficient knowledge about how best to use these new drugs in combination with other standard treatments, the need for close monitoring and reporting of adverse events, and the high price of the drugs, which makes them unaffordable for many patients.
Besides the large gaps in diagnosis, notification and treatment, a significant funding gap exists for tuberculosis prevention and care in low- and middle-income countries: an estimated $6.9 billion against the $9.2 billion required in 2017 and $12 billion for 2020 (1). But what really threatens to blow up the economics of tuberculosis care, is the emergence of drug-resistant tuberculosis; whereas the standard 6-month course for drug-sensitive tuberculosis (isoniazid, rifampicin, ethambutol and pyrazinamide) costs as little as $40, a treatment course for MDR-TB can last 2 years and cost up to $5,000. Even a WHO-recommended seven-drug standard short (9–12 months) course for MDR-TB costs $1,000 per eligible patient. An estimated 490,000 new MDR-TB cases occurred in 2016, half of whom in three countries: India, China and Russia. Especially in Russia and the countries of the former Soviet Union, drug-resistant tuberculosis represents a high (over 15%) proportion of all tuberculosis cases, and thus poses a particular challenge.
Countering the threat of drug resistance, and achieving the steeper declines in tuberculosis incidence envisaged for the period after 2025, is next to impossible without new developments in treatments, diagnostics, and especially a new and effective vaccine that can prevent active disease in people with latent tuberculosis infection. For this reason, tuberculosis research is of primary importance. A total of $4.6 billion was invested into tuberculosis research between 2009 and 2016, of which a lion’s share of $1.8 billion was provided by the USA, with much smaller contributions from other countries. Recent political developments, however, put these research funds increasingly in jeopardy (5). Even at the current levels of funding, the $0.7 billion invested in 2016 is far under the annual requirement of $2 billion estimated by WHO. Therefore, although some progress has occurred, there is still a very long way to go.
In light of this situation, it is clear that more political commitment to fighting tuberculosis is required in all countries. The upcoming UN General Assembly session is a good opportunity to show such commitment, but this needs to be backed up by concrete action and measurable targets in the short term too, rather than only in the long term. Tuberculosis prevention, testing and treatment need to be scaled up as part of a comprehensive control program, particularly in high-burden countries, in order to close the detection, notification and treatment gaps. It is disgraceful, to say the least, that 4 out of 10 incident cases of tuberculosis still go undiagnosed and unreported, not to mention the gaps in drug sensitivity testing of cases. Scaling up tuberculosis control programmes require not just financial and material resources, but also investment in people; the world needs many more tuberculosis “warriors” to fight the disease in the field alongside patients (6). Action is needed now, and timetables for action need to focus more on the short term, in order to capture the attention span of the world’s governments and render them accountable for achieving results. Lofty promises and goals for ending tuberculosis in some distant future will not mean anything unless concrete steps are taken in the present.
In addition, the world needs to invest far more on tuberculosis research. It is unacceptable that just 0.25% of global research expenditure goes to tuberculosis (7), even though it is among the top ten causes of death worldwide (1). The world needs improved diagnostics, both for active disease, for latent infection and for drug sensitivity testing; the holy grail would be a point-of-care test for tuberculosis, which would significantly facilitate case detection and treatment especially in low-resource settings. New and affordable treatments are needed, particularly for drug-resistant tuberculosis. Effort should be made both to accelerate progress of existing compounds through the drug pipeline (8), and bring new compounds to the table. Significantly more research is also needed to establish the best way to use new tuberculosis drugs, determine their safety profile, and establish effective combination regimens for each category of patients; otherwise, potentially lifesaving drugs will remain unavailable for the majority of the patients who could benefit from them. Finally, more operational research is essential to address topics such as optimal access to and delivery of tuberculosis care, addressing the joint epidemic with HIV, tuberculosis in special populations such as international migrants, measurement of disease burden, etc. Funding for tuberculosis research should be protected and reinforced across the board; especially high-income countries beside the United States should increase their relative contribution, to demonstrate their commitment and set a good example for others to follow.
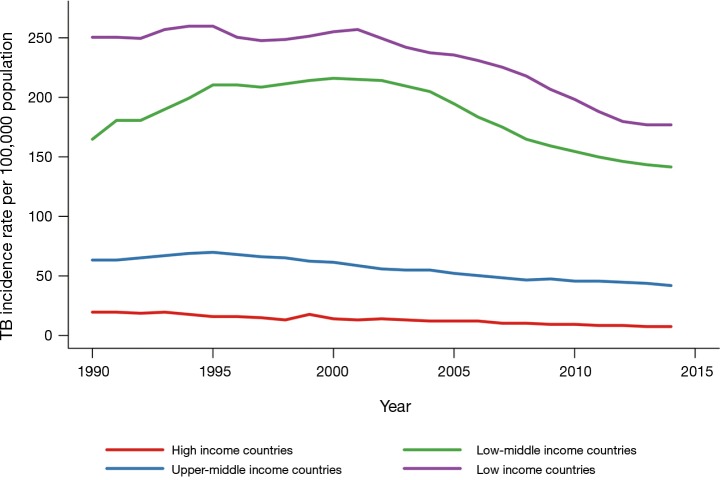
Ultimately though, one should not forget that tuberculosis is first and foremost a disease of poverty, deprivation and inequality (9). There is a clear gradient between economy and tuberculosis incidence, with high-income countries having several times lower incidence than low-income countries (Figure 1). Social and economic determinants have been observed to affect tuberculosis incidence trends even more than indices of tuberculosis control (11). Global migration means that no country is immune from this disease (10), and in several high-income countries foreign-born persons already comprise the majority of reported tuberculosis cases (12). For the developed world, fighting tuberculosis at home means fighting it abroad to a large extent, especially given that screening migrants is complicated and its yield low (13). Innovations in diagnosis and treatment, or the potential discovery of an effective vaccine, will mean nothing if the resources to apply these worldwide are not available. Besides health expenditure, at least a minimum of spending in social protection and development remains essential in fighting tuberculosis (14). As a result, tuberculosis is a socio-political problem at least as much as a medical one, therefore solving it will depend on political pressure and political will at least as much as on science (15).
Figure 1.
Median tuberculosis incidence rate (per 100,000 persons per year) per country group by level of economic development (high-, upper-middle-, low-middle- and low-income countries). Reproduced from Pescarini et al. (10).
Acknowledgements
None.
Provenance: This is an invited Editorial commissioned by the Section Editor Xu-Guang Guo (Division of Clinical Microbiology, Department of Clinical Laboratory Medicine, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Floyd K, Glaziou P, Zumla A, et al. The global tuberculosis epidemic and progress in care, prevention, and research: an overview in year 3 of the End TB era. Lancet Respir Med 2018;6:299-314. 10.1016/S2213-2600(18)30057-2 [DOI] [PubMed] [Google Scholar]
- 2.Review on Antimicrobial Resistance. Tackling drug-resistant infections globally: final report and recommendations. 2016.
- 3.World Health Organization. Moscow declaration to end TB. In: First WHO Ministerial Conference to Ending TB in the Sustainable Development Era: A Multisectoral Response, 2017. [Google Scholar]
- 4.Médecins Sans Frontières, Stop TB Partnership. Out of Step 2017. TB Policies in 29 Countries. A survey of prevention, testing and treatment policies and practices. Available online: https://www.msfaccess.org/outofstep2017
- 5.Frick M. Funding for tuberculosis research-an urgent crisis of political will, human rights, and global solidarity. Int J Infect Dis 2017;56:21-4. 10.1016/j.ijid.2016.11.412 [DOI] [PubMed] [Google Scholar]
- 6.India’s “tuberculosis warrior.” BBC News. Available online: https://www.bbc.com/news/world-asia-india-43456442
- 7.Moses H, 3rd, Matheson DH, Cairns-Smith S, et al. The anatomy of medical research: US and international comparisons. JAMA 2015;313:174-89. 10.1001/jama.2014.15939 [DOI] [PubMed] [Google Scholar]
- 8.Clinical Pipeline Available online: https://www.newtbdrugs.org/pipeline/clinical
- 9.Noppert GA, Wilson ML, Clarke P, et al. Race and nativity are major determinants of tuberculosis in the U.S.: evidence of health disparities in tuberculosis incidence in Michigan, 2004-2012. BMC Public Health 2017;17:538. 10.1186/s12889-017-4461-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pescarini JM, Rodrigues LC, Gomes MG, et al. Migration to middle-income countries and tuberculosis-global policies for global economies. Global Health 2017;13:15. 10.1186/s12992-017-0236-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dye C, Lönnroth K, Jaramillo E, et al. Trends in tuberculosis incidence and their determinants in 134 countries. Bull World Health Organ 2009;87:683-91. 10.2471/BLT.08.058453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pareek M, Greenaway C, Noori T, et al. The impact of migration on tuberculosis epidemiology and control in high-income countries: a review. BMC Med 2016;14:48. 10.1186/s12916-016-0595-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dobler CC, Fox GJ, Douglas P, et al. Screening for tuberculosis in migrants and visitors from high-incidence settings: present and future perspectives. Eur Respir J 2018;52. doi: . 10.1183/13993003.00591-2018 [DOI] [PubMed] [Google Scholar]
- 14.Siroka A, Ponce NA, Lönnroth K. Association between spending on social protection and tuberculosis burden: a global analysis. Lancet Infect Dis 2016;16:473-9. 10.1016/S1473-3099(15)00401-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coker R. Lessons from New York’s tuberculosis epidemic. Tuberculosis is a political as much as a medical problem-and so are the solutions. BMJ 1998;317:616. 10.1136/bmj.317.7159.616 [DOI] [PMC free article] [PubMed] [Google Scholar]