Abstract
Background and Purpose
Patients with moyamoya vasculopathy (MMV) may experience cognitive impairment, but its reported frequency, severity, and nature vary. In a systematic review and metaanalysis, we aimed to assess the presence, severity, and nature of cognitive impairments in children and adults with MMV.
Methods
We followed the MOOSE guidelines for meta-analysis and systematic reviews of observational studies. We searched Ovid Medline and Embase for studies published between January 1, 1969 and October 4, 2016. Independent reviewers extracted data for mean intelligence quotient (IQ) and standardized z-scores for cognitive tests, and determined percentages of children and adults with cognitive deficits, before and after conservative or surgical treatment. We explored associations between summary measures of study characteristics and cognitive impairments by linear regression analysis.
Results
We included 17 studies (11 studies reporting on 281 children, six on 153 adults). In children, the median percentage with impaired cognition was 30% (range, 13% to 67%); median IQ was 98 (range, 71 to 107). Median z-score was –0.39 for memory, and –0.43 for processing speed. In adults, the median percentage with impaired cognition was 31% (range, 0% to 69%); median IQ was 95 (range, 94 to 99). Median z-scores of cognitive domains were between –0.9 and –0.4, with multiple domains being affected. We could not identify determinants of cognitive impairment.
Conclusions
A large proportion of children and adults with MMV have cognitive impairment, with modest to large deficits across various cognitive domains. Further studies should investigate determinants of cognitive deficits and deterioration, and the influence of revascularization treatment on cognitive functioning.
Keywords: Moyamoya disease, Intelligence, Child, Adult, Neuropsychological tests, Review
Introduction
Moyamoya vasculopathy (MMV) is a cerebrovascular disorder of largely unknown etiology characterized by progressive stenosis or occlusion of the supraclinoid internal carotid arteries and their proximal branches [1,2]. Patients may present with transient ischemic attacks (TIAs) and ischemic stroke but also with headache, movement disorders, and seizures [1,3]. MMV can also lead to cognitive impairment [4]. Cognitive functions may not only be affected by overt or silent brain infarcts or hemorrhages but also by chronic hypoperfusion, as cognitive impairment has been diagnosed in adults with MMV without stroke [5]. Early age of onset and longer disease duration have been associated with the occurrence of cognitive impairment [6]. Many patients with MMV undergo surgical revascularization to improve cerebral blood flow (CBF) and prevent future ischemic stroke [2], but prospective studies on the effect of surgical treatment on cognition are lacking. A previously published descriptive review has provided an overview on cognition in moyamoya disease (MMD) suggesting that the impact of MMV on cognition is more pronounced in children than in adults [7]. In the present study we systematically collected and meta-analyzed available quantitative information on the presence, severity and nature of cognitive impairment in children and adults with MMV and its determinants, in particular cerebral perfusion. Furthermore, we aimed to determine the effect of surgical intervention on cognition.
Methods
For the conduction of this systematic review we followed the meta-analysis of observational studies in epidemiology (MOOSE) guidelines [8].
Search strategy and selection criteria
We searched Ovid Medline and Embase for publications of studies describing cognitive function in patients with MMV published between January 1, 1969 (the year the disorder was given its name) and October 4, 2016 (see online Supplementary for Syntax). No limits were set for languages; native speakers translated papers that were written in other languages than English, German, or French. Titles and abstracts were scanned and papers were included on the basis of full text by two authors independently (A.K. and C.J.M.K.); disagreement was resolved by consensus. Additional studies were included from the reference lists of included studies. We included studies reporting cognitive or intellectual functioning in children and adults that allowed analysis of quantitative data on group level (i.e., intelligence quotient [IQ] scores) of at least five patients. If authors reported neuropsychological assessment without providing raw neuropsychological data, we contacted them for additional data. In case of (suspected) overlap between study cohorts, we included the study with the largest sample size with information on the proportion of patients with impaired cognition. In case individual patient data were provided, we excluded patients without quantitative cognitive data.
Data extraction
Three authors (A.K. all papers; C.J.M.K. and E.B. half of the studies each) independently extracted data from selected papers. Disagreements were solved by consensus. Of the authors from 13 publications who were approached for additional data, one provided baseline characteristics and scores of neuropsychological tests [9], five could not provide additional information, and seven authors did not respond. The risk of bias was evaluated by one author (A.K.) using the Newcastle-Ottawa scale adapted for cross-sectional studies (see online Supplementary for the Risk Assessment) [10].
We collected the following study characteristics: study design; midyear of study; in- and exclusion criteria; number of patients with MMD or moyamoya syndrome (MMS, known associated disease) [1]; mean age and duration of symptoms (at time of diagnosis; presentation; neuropsychological assessment, operation, inclusion or not specified); proportion of females; ethnicity (Asian, Caucasian, Hispanic, African, and Afro-American, according to the definition provided by the authors, or—if not provided—by country of publication); site of clinical stroke or TIA (uni- or bilateral); application of diagnostic criteria for MMV [1]; site of vasculopathy; and site of (silent) stroke on imaging; and results of CBF and cerebrovascular reserve (CVR) studies. We divided presenting symptoms into four categories depending on the information provided by the authors: (1) ischemic stroke only; (2) TIA(s) only; (3) hemorrhage; or (4) other symptoms. We collected information on the level of education and occupation. In studies that provided longitudinal assessment of cognitive functioning, data were also collected for the second time-point, including the type of revascularization in surgically treated patients.
From the neuropsychological assessments we extracted the following data: mean full-scale intelligent quotient (FSIQ), developmental quotient (DQ) (pooled with FSIQ as IQ); verbal intelligent quotient (VIQ); performance intelligent quotient (PIQ); raw or standardized z-scores of cognitive tests; and the proportion of patients with cognitive impairment overall and per cognitive domain (Supplementary Table 1 summarizes the specific neuropsychological tests applied by each study). For studies that did not provide the proportion of patients with cognitive impairment, we calculated the proportion based on published normative data if possible. For DQ (a ratio calculated by dividing the mental developmental age with the chronological age) we appointed to have the same norm sample as (FS)IQ, unless otherwise specified [11]. Cognitive test results derived from neuropsychological evaluation were grouped into six predefined cognitive domains according to standard neuropsychological practice specified in Lezak: intelligence, memory, processing speed, attention and executive functions, visual perception and construction, and language (Supplementary Table 2) [12]. In studies that provided results of multiple cognitive tests investigating the same domain, we determined the mean score and, if possible, calculated the mean z-scores and standard deviations (SDs) for the domain. A z-score is a standardized score which entails the number of SDs that an individual test result differs from the mean score in healthy controls, thereby indicating the relative location of a measurement within its distribution [13].
Data analysis
To assess the presence of cognitive impairment, we determined the median proportion of patients with cognitive impairment. Cognitive impairment was defined according to the authors’ criteria, or as a cognitive score (overall, or on a specific domain, or on at least two tests) deviating more than 1.5 SD from the population mean, or IQ <85. To assess the severity of the impairment, we calculated the median cognitive scores of the various cognitive tests. To determine whether mean age, ethnicity, sex, mean duration of symptoms, and presenting symptoms were determinants of cognitive impairment, we performed linear regression analysis weighted by the inverse standard error of the proportion of patients with impaired cognition. Due to lack of data, this could not be performed for other patients’ characteristics. We qualitatively determined the reported association between frontal CBF and CVR and cognitive impairment as reported by the authors.
In studies that provided longitudinal assessment of cognitive function, we determined whether cognitive functions improved, deteriorated or remained stable over time. For intelligence, we used a cut-off point of more than 10 points differences of IQ scores at follow-up. For cognitive domains, change over time was categorized according to the criteria provided by the authors.
Results
After screening 299 studies (66 studies were screened on full text), we included 17 studies reporting cognitive function in a total of 434 patients (Figure 1). Eleven studies reported on 281 children and six studies on 153 adults. Tables 1 and 2 and Supplementary Tables 3 and 4 summccs and neuropsychological test results [4,6,9,14-27]. Four studies reported on cerebral hemodynamic measures in relation to cognitive functions [4,9,17,21]. Nine studies reported longitudinal assessment of cognitive function over time, eight of which provided data after surgical treatment in children; one after conservative treatment in adults (Table 2 and Supplementary Table 5) [4,15-20,22,23]. Study quality varied between three and six out of seven: three studies had a total score of 3 [4,21,22]; five studies a score of 4 [16,18-20,23]; five studies a score of 5 [6,9,17,25,27]; and four studies a score of 6.14,15,24,26 The most important reasons for studies having a risk of bias were: sample size <30 patients (65%) and no information on whether patients were included consecutively (87%) (Supplementary Table 6).
Figure 1.
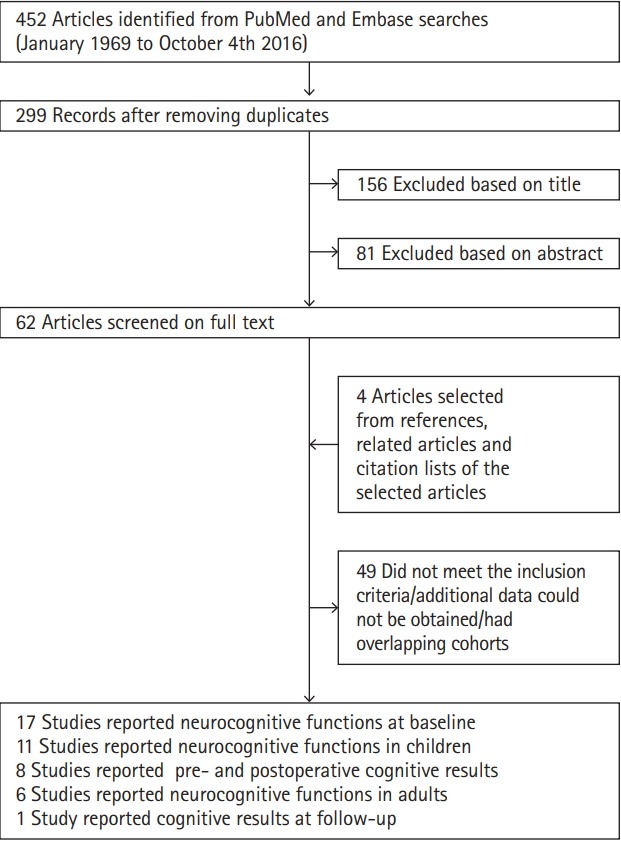
Flowchart.
Table 1.
Basic characteristics of studies and neuropsychological results in children and adults with moyamoya vasculopathy
| Study | No. | Age (yr) | Presenting symptoms (%) | Duration (mo) | Cognitive impairment overall (%) | FSIQ impaired (%) | VIQ impaired (%) | PIQ impaired (%) | Memory impaired (%) | Procspeed impaired (%) | Att/EF impaired (%) | Visper/const impaired (%) | Language impaired (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hsu et al. (2014) [6]* | 13 | 13.9±6.3 (6–17)† | TIA 100 | 17±15.9 (1–48)† | 39 | 0 | 17 | 0 | 15 | 8 | 8 | 18 | - |
| Williams et al. (2012) [14]* | 30 | 10.1±4† | Infarction 50 | 35.0±49 (2–204)† | - | - | - | - | - | - | - | - | - |
| Lee et al. (2011) [15]* | 65 | 9.1 (4–17)† | - | - | - | - | - | - | - | - | - | - | - |
| Imaizumi et al. (1999) [16]* | 38 | 6.5±3.3 (1–13)‡ | Infarction 26 | 16.2±16.1 (160)‡ | - | - | - | - | - | - | - | - | - |
| TIA 63 | |||||||||||||
| Other 11 | |||||||||||||
| Ohtaki et al. (1998) [17]* | 8§ | 7.1±2.0 (5–11)‖ | Minor completed stroke 12.5 | 18.9±19.7 (2–60)‖ | 13 | 13 | - | - | - | - | - | - | - |
| Hemorrhage 12.5 | |||||||||||||
| TIA 75 | |||||||||||||
| Matsushima et al. (1997) [18]* | 20 | 9.6±3.4‖ | Infarction 30 | - | 15 | - | - | - | - | - | - | - | - |
| TIA 70 | |||||||||||||
| Matsushima et al. (1991) [19]* | 50¶ | 9.4±4.3 (2–21)‖ | Movement disorder 80 | 55.8±50.7 (0–188)‖ | 50 | - | - | - | - | - | - | - | - |
| Seizures 6 | |||||||||||||
| Headache 10 | |||||||||||||
| Involuntary movements 4 | |||||||||||||
| Sato et al. (1990) [20]* | 12** | 5.9±2.3 (1–10)† | Ischemia 50 | 12.6±10.6 (1–31)† | 67 | - | 57 | 56 | - | - | - | - | - |
| TIA 50% | |||||||||||||
| Tagawa et al. (1989) [21]* | 10†† | 10.2±3.2 (6−15)† | Infarction 10 | 57.8±50.5 (13−155)† | 30 | 30 | - | - | - | - | - | - | - |
| TIA 90 | |||||||||||||
| Ibayashi et al. (1985) [22]* | 15 | 9.2±3.3 (5−16)‡‡ | Completed stroke 53 | 48.3±44.3 (19–136)‡‡ | - | - | - | - | - | - | - | - | - |
| TIA 47 | |||||||||||||
| Ishii et al. (1984) [4]* | 20 | 9.9±3.1 (5–16)‡‡ | Completed stroke 60 | - | 22 | 22 | 21 | 26 | - | - | - | - | - |
| TIA 40 | |||||||||||||
| Lei et al. (2017) [26]§§ | 26 | 40.2±9.4‡‡ | Minor stroke 27 | - | - | - | - | - | - | - | - | - | - |
| TIA 54 | |||||||||||||
| Headache 19 | |||||||||||||
| Kazumata et al. (2015) [27]§§ | 23 | 40.9±9.5 (21–58)‡‡ | TIA 43 | - | 30 | 8 | 4 | 17 | 35 | 33 | 30 | 22 | 39 |
| Asymptomatic 57 | |||||||||||||
| Su et al. (2013) [23]§§ | 26 | 43.7±8.6 (26–59)‡‡ | Hemorrhage 100 | 1.2† | 0 | - | - | - | - | - | - | - | - |
| Calviere et al. (2012) [9]§§ | 13 | 36.6±12.9‡‡ | Ischemic stroke 62 | 36.1‖‖ | 54 | - | - | - | 54 | 23 | 54 | 23 | 31 |
| Hemorrhage 8 | |||||||||||||
| Other 30 | |||||||||||||
| Festa et al. (2010) [25]§§ | 29 | 39.9±11.2 (20–65)‖‖ | Ischemic stroke 72 | - | 69 | - | - | - | 39 | 21¶¶ | 19*** | 29 | 20 |
| TIA 17 | |||||||||||||
| Hemorrhage 3 | |||||||||||||
| Other 8 | |||||||||||||
| Karzmark et al. (2008) [24]§§ | 36 | 36.6±9.9† | - | - | 31 | 19 | 25 | 25 | 7 | 39 | 43 | 23 | 40 |
Values are presented as mean±standard deviation (range) or mean±standard deviation.
FSIQ, full-scale intelligent quotient; VIQ, verbal intelligence quotient; PIQ, performal intelligence quotient; Procspeed, processing speed; Att, attention; EF, executive function; Visper/const, visual perception/construction; TIA, transient ischemic attack.
Studies reporting results in children;
At neuropsychological assessment;
At diagnosis;
Excluding 2 patients (1 scaled out, 1 not investigated);
At operation;
Study included 65 patients with preoperative data in 50 patients;
Study included 13 patients from which 12 had preoperative data;
Study included 21 patients from which 10 had preoperative data;
Not specified;
Studies reporting results in adults;
At presentation;
n=19;
n=16.
Table 2.
Longitudinal neuropsychological test performances
| Study | FU period (mo) | Impairment overall (A/B) (%)* | Improved (%) | Stable (%) | Deteriorated (%) |
|---|---|---|---|---|---|
| Lee et al. (2011) [15] † | 19‡ (5-46) | - | - | - | - |
| Imaizumi et al. (1999) [16] † | >120§ | - | - | - | - |
| Ohtaki et al. (1998) [17] † | 85.2±32.59‖ (23-110) | 13/13 | 12 | 63 | 25 |
| Matsushima et al. (1997) [18] † | 113‡ | 15/20 | - | - | - |
| Matsushima et al. (1991) [19] † | 26.2±14.7‡ (7-58) | 50/49 | 27 | 49 | 24 |
| Sato et al. (1990) [20] † | 44.4±26.3¶ (4-99) | 67/58 | PIQ 11 | PIQ 78 | PIQ 11 |
| VIQ 29 | VIQ 57 | VIQ 14 | |||
| DQ 0 | DQ 100 | DQ 0 | |||
| Ibayashi et al. (1985) [22] † | 6.5±4.9‡ (1-17) | - | FSIQ 47 | - | - |
| VIQ 20 | |||||
| PIQ 60 | |||||
| Ishii et al. (1984) [4] † | 6–68‡ | 22/- | FSIQ 53 | FSIQ 40 | FSIQ 6 |
| VIQ 13 | VIQ 73 | VIQ 13 | |||
| PIQ 67 | PIQ 20 | PIQ 13 | |||
| Su et al. (2013) [23]** | 24‖ | 0/100 | 0 | 0 | 100 |
Values are presented as median (range), mean±standard deviation (range), or range.
FU, follow-up; PIQ, performal intelligence quotient; VIQ, verbal intelligence quotient; DQ, developmental quotient; FSIQ, full-scale intelligent quotient.
A/B, prior neuropsychological test result/longitudinal neuropsychological test result;
Studies reporting results in children;
FU period defined as time of operation to NPA;
FU period defined as time from onset of disease to neurospychological assessment;
FU period defined as time of NPA to NPA;
FU period unspecified;
Studies reporting results in adults.
Children
In the 11 studies reporting on children, median age of the study cohorts was 9.4 years (range, 5.9 to 13.9); the median percentage females 55% (range, 33% to 75%; 10 studies, 268 patients). All studies except one [14] described Asian cohorts of which nine were Japanese. Two studies described the criteria they used for the diagnosis of MMV: confirmation by angiographic evidence of moyamoya collaterals and stenosis in one study [14] and according to Sato et al. [20] in the other. One paper reported the inclusion of patients with MMS (n=20) [14]. Presenting symptoms were reported in 10 studies (216 children). The median proportion of children presenting with ischemic stroke was 31% (range, 0% to 60%; nine studies, 166 patients), and with TIA only 69% (range, 40% to 100%; nine studies, 166 patients) [4,6,14,16-18,20-22]. Presentation with hemorrhage was rare (one patient in 166 children in nine studies). One study (50 patients) did not report symptoms that could be classified according to our predefined categories [19].
The median duration of symptoms was 27.0 months (range, 12.6 to 57.8). We found no information on school performance or the presence of depression among the pediatric studies.
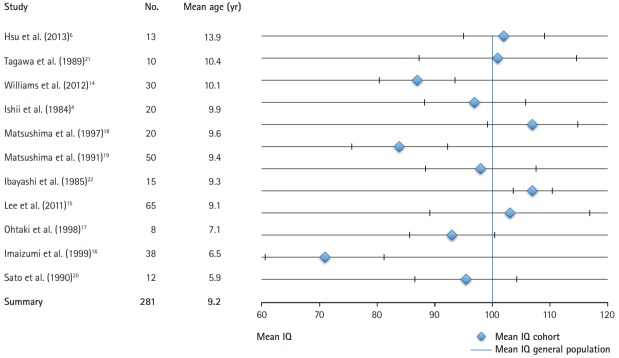
Cognitive impairment
The median proportion of children with cognitive impairment overall was 30% (range, 13% to 67%; seven studies, 133 patients) (Figure 2) with a median IQ score of 101 (range, 71 to 107) [4,6,17-21]. In the included 11 studies, the median IQ score was 98 (range, 71 to 107) [4,6,14-22], median VIQ score was 97 (range, 77 to 108; seven studies, 170 children) [4,6,14,15,18,20,22], and median PIQ score was 100 (range, 89 to 109; six studies, 163 children) [4,6,14,15,18,22]. Three studies reported on specific cognitive domains [6,14,15]. Memory was affected in 15% of patients (one study, 13 patients) [6]. Eight percent of the patients had impairment in processing speed and attention and executive functions, and 18% in the visual perception and construction domain (one study, 13 patients) [6]. The median z-score for memory was –0.39 (range, –0.85 to 0.45; three studies, 108 children) [6,14,15] and for processing speed –0.43 (range, –0.86 to 0.00; two studies, 43 children) [6,14]. One study (13 patients) assessed additional domains with mean z-scores of 0.50 for attention and executive function; and –0.53 for visual perception and construction [6].
Figure 2.
Mean intelligence quotient (IQ) with 95% confidence interval (CI) in children (11 studies, 281 children) ordered by mean age (mean summary IQ, 95.5; 95% CI, 86.7 to 104.2). The blue vertical line represents the mean IQ in the average population.
We found no association between mean age (B=–0.014; 95% confidence interval [CI], –0.112 to 0.083; P=0.723); type of presenting symptom (for infarction [B=–0.002; 95% CI, –0.017 to 0.013; P=0.672] and for TIA [B=–0.002; 95% CI, –0.013 to 0.017; P=0.672); mean duration of symptoms (B=0.000; 95% CI, –0.016 to 0.016; P=0.945); and proportion of females (B=–0.005; 95% CI, –0.025 to 0.014; P=0.508), and the proportion of patients with cognitive impairment (Supplementary Table 7) [4,6,18,20,21].
Cerebral blood flow
Three studies investigated the relation between CBF (xenon-enhanced computed tomography [CT] [4] or single photon emission CT [SPECT]) [17] and IQ scores [21]. In one study, patients with a lower IQ showed a tendency for a more marked depression of mean CBF than those with a normal IQ (quantitative analysis not provided) [4]. Another study reported a marked depression of CBF (qualitatively determined) in the frontal lobes in seven out of nine patients, all having normal IQ scores [17]. The third study reported no relation between abnormal patterns of CBF and IQ [21].
Longitudinal results
Eight studies (199 patients) evaluated the effect of revascularization surgery on cognitive performances after a median follow-up period of 35.3 months (range, 6.5 to 113) [4,15-20,22]. All eight studies reported IQ and one also assessed memory. Indirect revascularization was performed in 90.5% of the patients, direct in 0.5% and combined in 9%. The median proportion of children with impaired intelligence pre-operatively was 33% (range, 13% to 67%; four studies, 88 children) and at followup after revascularization 35% (range, 13% to 58%; four studies, 81 children) [17-20]. In the other four studies proportions of children with impaired IQs were not reported post-operatively.
Median scores at follow-up were: for IQ 97 (range, 68 to 108; six studies, 161 children) with a pre-operative median IQ score in these studies of 101 (range, 71 to 107; 170 children); for VIQ 97 (range, 82 to 106; four studies, 107 children) with a pre-operative median VIQ score of 101 (range, 77 to 108; 107 children); and for PIQ 102 (range, 100 to 109; three studies, 100 children) with a pre-operative median PIQ score of 100 (range, 97 to 109; 100 children).
Based on available individual patient data, improvement in IQ (≥10 points) was observed in a median proportion of 27% of patients (range, 5.5% to 53%; five studies, 91 children) [4,17,19,20,22], no change in 56% (range, 40% to 89%; four studies, 76 children) and deterioration in 15% (range, 5.5% to 25%; four studies, 76 children). Improvement in VIQ was seen in 20% (range, 13% to 29%; three studies, 37 children) [4,20,22], no change in 65% (57% and 73%; two studies, 22 children) and deterioration in 13.5% (13% and 14%; two studies, 22 children). PIQ scores improved in 63.5% (60% and 67%; two studies, 30 patients), remained stable in 20% (one study, 15 patients) and deteriorated in 13% (one study, 15 patients) [4,22]. Memory function improved after surgery (pre-operative z-score 0.45; after surgery 0.77) [15]. One study in which 18 out of the 38 patients were operated on (five combined, 13 indirect) reported no improvement of IQ after revascularization (no quantitative data available) [16].
Adults
In the six studies reporting on adults, median age was 40.1 years (range, 36.6 to 43.7) and the median percentage of females 63% (range, 46% to 74%) [9,23-27]. Of a total of 153 patients, 87 were Asian (57%), 56 Caucasian (37%), and 10 had another ethnicity (7%). The median proportion of adults presenting with ischemic stroke was 27% (range, 0% to 72%; five studies, 117 patients), TIA only 17% (range, 0% to 54%; five studies, 117 patients), hemorrhage 3% (range, 0% to 100%; five studies, 117 patients), and 19% (range, 0% to 57%; five studies, 117 patients) had other symptoms [9,23,25-27]. The median duration of symptoms at assessment or inclusion was 18.6 months (1.2 and 36.1 months; two studies).
Cognitive impairment
The median proportion of patients with cognitive impairment was 31% (range, 0% to 69%; five studies, 127 patients) [9,23-25,27]. In the four studies investigating cognition by means of a neuropsychological test battery, the median proportion with impaired cognition on one or more of the reported domains was 42.5% (range, 30% to 69%) [9,24,25,27]. The median IQ score was 95 (range, 94 to 99; three studies, 88 patients) [24,25,27]; median VIQ score was 94 and median PIQ score 93 (two studies, 59 patients).
Four studies (101 patients) reported on specific cognitive domains [9,24,25,27]. The median proportion of patients with impaired memory was 37% (range, 7% to 54%), impaired processing speed 28% (range, 21% to 39%), impaired attention and executive functions 37% (range, 19% to 54%), impaired visual perception and construction 23% (range, 22% to 29%), and impaired language 35% (range, 20% to 40%) [9,24,25,27]. The median z-scores (three studies, 78 patients) were: for memory –0.4 (range, –1.1 to –0.2), for processing speed –0.9 (range, –1.7 to –0.8), for attention and executive function –0.9 (range, –0.95 to –0.4), for visual perception and construction –0.4 (range, –0.5 to –0.2), and for language –0.6 (range, –0.8 to –0.15). One study of patients with an intraventricular hemorrhage (IVH) showed a mean score within the normal range (27.4±1.2 [range, 26 to 29]) on the Montreal Cognitive Assessment (MoCA) [23].
We found no association between mean age (B=–0.044; 95% CI, –0.184 to 0.096; P=0.387) or proportion of females (B=0.011; 95% CI, –0.031 to 0.053; P=0.460) and cognitive impairment (Supplementary Table 7). Analysis of the association of type of presenting symptom and cognitive impairment was not possible, because of lack of data categorized according to our predefined classification.
The mean duration of education was 12.1±3.1 years (three studies, 91 patients) [24-26]. In a series of 26 patients from one study, nine finished college or a higher-level education, five primary school or less, and 12 middle school [23]. Another study of 36 patients reported that 25 participated in a full-time job, five were unemployed and five were homemakers; one patient had retired [24].
Cerebral blood flow studies
One study reported a correlation of the apparent diffusion coefficient (ADC) in normal appearing frontal white matter on diffusion weighted imaging with CVR on perfusion magnetic resonance imaging and executive functions (Spearman coefficient, –0.46; P=0.01) [9]. Elevation of ADC was significantly correlated with executive dysfunction (area under the curve for cognitive impairment, 0.85; 95% CI, 0.59 to 1.16; P=0.032).
Longitudinal results
In the study assessing cognitive impairment in patients with solely IVH, all patients had normal MoCA scores at baseline (mean MoCA score 27.4±1.2 [range, 26 to 39]) and mild cognitive impairments after a mean follow-up of 24 months (mean MoCA score 18.7±1.3 [range, 16 to 21]) without treatment [23].
Discussion
Our systematic review shows that around 30% of children and of adults have cognitive impairment. When assessed on a group level, median IQ scores are within the normal range in both children and adults. Information on specific domains of cognitive function is limited, with relatively modest impairments in memory and processing speed observed in children, and modest to large impairments across various cognitive domains in adults.
Since there was not a large discrepancy between VIQ and PIQ, total IQ scores provide a reliable insight in cognitive functioning in children. Longitudinal results in children showed that IQ scores on a group level remained within normal limits over time. In adults, longitudinal studies of neuropsychological assessments other than with a screening test have not been performed.
In a previous review, the authors concluded that cognition is affected more frequently in children than in adults, reporting intelligence to be impaired in children, and executive functions in adults [7]. However, our systematic review and meta-analysis show that in adults the proportion of patients with impairment of cognitive function is as large as in children. In comparison with this aforementioned review, we included five additional studies on children [6,14,15,21,22] and four recent studies on adults [9,23,26,27]; and excluded studies without quantitative data. Although the highest median percentage of impaired function was found in the domain attention and executive functions, we found similar proportions of patients with impairment for the other cognitive domains. In children, other domains than intelligence were investigated in only three studies. Patients with a normal intelligence may show selective cognitive impairment in other cognitive domains. Therefore, extensive neuropsychological evaluation is of great importance, also in children who generally show a diffusely impaired cognitive profile in case of cognitive deterioration because their brain is still developing.
It remains uncertain if the neurocognitive profile of patients with MMS differs from that in patients with MMD, since the presence of associated diseases was reported in only one study, which did not demonstrate a difference between these groups [14].
We did not find an association between the predefined determinants and the proportion of patients with cognitive impairment, probably due to the limited data available. Some of the included studies suggested that age at onset [4,6,22] and longer duration of disease were [6] associated with cognitive dysfunction, however we could not confirm these associations in our metaanalysis. Previous studies were small including 13 to 20 patients and observed associations may have been due to chance. Information on the determinants of cognitive impairment and its course is scarce. The relation between cerebral perfusion and cognition in children remains unclear, whereas in adults, a single study suggested a relation between diminished perfusion in the frontal matter and executive dysfunction. Several studies have suggested that (frontal) hypoperfusion, white matter disease and infarction are associated with cognitive disturbances [28-31]. It remains unclear whether MMV directly affects cognition by chronic hypoperfusion, or that cognitive impairment is mainly the result of stroke. The observed impaired cognition in patients without stroke supports the hypothesis that chronic hypoperfusion is a contributing factor to cognitive impairment in patients with MMV [5,6]. One study reported that executive dysfunction was associated with stroke and white matter lesions and not with CVR; however, patients with higher baseline CBF had better cognitive functioning [32]. Improvement in intelligence and cerebral perfusion in children has been observed after revascularization surgery [4,17], and for this reason frontal revascularization procedures are performed more often [2,17,33]. Whether prevention of cognitive decline should be an indication for revascularization surgery in patients with MMV remains unclear. Although our review shows that a fair number of patients improved or remained stable after revascularization, the quantity of the included data is too limited to draw final conclusions.
Although we were able to collect a reasonable amount of data on cognitive function in patients with MMV, the review was limited by the relatively low number of patients described in the individual studies. Information bias could not be avoided, given the large heterogeneity of the reported cognitive tests. Since little information on patients’ characteristics was available, results could be influenced by selection bias and we could not control for confounding factors like the presence of silent infarction on imaging. Finally, we were not able to perform meta-analysis of the relation between CBF and cognition and of the effect of revascularization due to the low number and heterogeneity of studies. Our review also has strengths. We were able to quantify cognitive impairments in MMV. In addition, we were able to eliminate the risk of selection bias due to language since we did not include language restrictions. Despite these methodological shortcomings, our results give valuable insight in the presence, severity and nature of cognitive functions in MMV before and after revascularization, since we quantified cognitive impairments in MMV.
Conclusions
Large prospective studies with a standardized neuropsychological test battery are needed to determine the severity of cognitive impairment and the domains affected. Information on school level and performance, and on work status is also of importance, since it reflects function rather than deficits [34]. It remains to be established whether cognitive outcome can be improved by revascularization surgery.
Acknowledgments
We thank Dr. M. Poon (Buckinghamshire, England), S. Diederen and R. Hendriks (Utrecht, the Netherlands) for supporting the translation of the Chinese and Japanese papers.
This work was supported by the Dutch Brain Foundation (2012(1)-179); the Christine Bader Fund Irene Children’s Hospital); the Tutein Nolthenius Oldenhof Fund, the Johanna Children Fund and Friends of the Wilhelmina Children’s Hospital.
Dr. Catharina J. M. Klijn is supported by a Clinical Established Investigator grant from the Dutch Heart Foundation (grant number 2012T077) and an Aspasia grant from ZonMw (grant number 015008048).
Footnotes
Disclosure
The authors have no financial conflicts of interest.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2018.01550.
Applied cognitive instruments/tests for each study
Predefined cognitive domains according to standard neuropsychological practice specified in Lezak[20]
Characteristics of studies assessing cognitive functions in children and adults with moyamoya vasculopathy
Neuropsychological test performances
Longitudinal neuropsychological test performances
Critical appraisal of the included studies
Linear regression analysis
Supplementary for Syntax
Supplementary for the Risk Assessment
References
- 1.Scott RM, Smith ER. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009;360:1226–1237. doi: 10.1056/NEJMra0804622. [DOI] [PubMed] [Google Scholar]
- 2.Kronenburg A, Braun KP, van der Zwan A, Klijn CJ. Recent advances in moyamoya disease: pathophysiology and treatment. Curr Neurol Neurosci Rep. 2014;14:423. doi: 10.1007/s11910-013-0423-7. [DOI] [PubMed] [Google Scholar]
- 3.Kleinloog R, Regli L, Rinkel GJ, Klijn CJ. Regional differences in incidence and patient characteristics of moyamoya disease: a systematic review. J Neurol Neurosurg Psychiatry. 2012;83:531–536. doi: 10.1136/jnnp-2011-301387. [DOI] [PubMed] [Google Scholar]
- 4.Ishii R, Takeuchi S, Ibayashi K, Tanaka R. Intelligence in children with moyamoya disease: evaluation after surgical treatments with special reference to changes in cerebral blood flow. Stroke. 1984;15:873–877. doi: 10.1161/01.str.15.5.873. [DOI] [PubMed] [Google Scholar]
- 5.Karzmark P, Zeifert PD, Bell-Stephens TE, Steinberg GK, Dorfman LJ. Neurocognitive impairment in adults with moyamoya disease without stroke. Neurosurgery. 2012;70:634–638. doi: 10.1227/NEU.0b013e3182320d1a. [DOI] [PubMed] [Google Scholar]
- 6.Hsu YH, Kuo MF, Hua MS, Yang CC. Selective neuropsychological impairments and related clinical factors in children with moyamoya disease of the transient ischemic attack type. Childs Nerv Syst. 2014;30:441–447. doi: 10.1007/s00381-013-2271-9. [DOI] [PubMed] [Google Scholar]
- 7.Weinberg DG, Rahme RJ, Aoun SG, Batjer HH, Bendok BR. Moyamoya disease: functional and neurocognitive outcomes in the pediatric and adult populations. Neurosurg Focus. 2011;30:E21. doi: 10.3171/2011.3.FOCUS1150. [DOI] [PubMed] [Google Scholar]
- 8.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 9.Calviere L, Ssi Yan Kai G, Catalaa I, Marlats F, Bonneville F, Larrue V. Executive dysfunction in adults with moyamoya disease is associated with increased diffusion in frontal white matter. J Neurol Neurosurg Psychiatry. 2012;83:591–593. doi: 10.1136/jnnp-2011-301388. [DOI] [PubMed] [Google Scholar]
- 10.Herzog R, Álvarez-Pasquin MJ, Díaz C, Del Barrio JL, Estrada JM, Gil Á. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kurita H, Osada H, Shimizu K, Tachimori H. Validity of DQ as an estimate of IQ in children with autistic disorder. Psychiatry Clin Neurosci. 2003;57:231–233. doi: 10.1046/j.1440-1819.2003.01106.x. [DOI] [PubMed] [Google Scholar]
- 12.Lezak M, Howieson D, Bigler E, Tranel D. Neuropsychological Assessment. 5th ed. New York, NY: Oxford University Press; 2012. [Google Scholar]
- 13.Bowerman BL, O’Connell RT, Hand ML. Business Statistics in Practice. 2nd New York, NY: McGraw Hill Higher Education; 2001. [Google Scholar]
- 14.Williams TS, Westmacott R, Dlamini N, Granite L, Dirks P, Askalan R, et al. Intellectual ability and executive function in pediatric moyamoya vasculopathy. Dev Med Child Neurol. 2012;54:30–37. doi: 10.1111/j.1469-8749.2011.04144.x. [DOI] [PubMed] [Google Scholar]
- 15.Lee JY, Phi JH, Wang KC, Cho BK, Shin MS, Kim SK. Neurocognitive profiles of children with moyamoya disease before and after surgical intervention. Cerebrovasc Dis. 2011;31:230–237. doi: 10.1159/000321901. [DOI] [PubMed] [Google Scholar]
- 16.Imaizumi C, Imaizumi T, Osawa M, Fukuyama Y, Takeshita M. Serial intelligence test scores in pediatric moyamoya disease. Neuropediatrics. 1999;30:294–299. doi: 10.1055/s-2007-973508. [DOI] [PubMed] [Google Scholar]
- 17.Ohtaki M, Uede T, Morimoto S, Nonaka T, Tanabe S, Hashi K. Intellectual functions and regional cerebral haemodynamics after extensive omental transplantation spread over both frontal lobes in childhood moyamoya disease. Acta Neurochir (Wien) 1998;140:1043–1053. doi: 10.1007/s007010050213. [DOI] [PubMed] [Google Scholar]
- 18.Matsushima Y, Aoyagi M, Nariai T, Takada Y, Hirakawa K. Long-term intelligence outcome of post-encephalo-duro-arterio-synangiosis childhood moyamoya patients. Clin Neurol Neurosurg. 1997;99 Suppl 2:S147–S150. doi: 10.1016/s0303-8467(97)00055-3. [DOI] [PubMed] [Google Scholar]
- 19.Matsushima Y, Aoyagi M, Koumo Y, Takasato Y, Yamaguchi T, Masaoka H, et al. Effects of encephalo-duro-arterio-synangiosis on childhood moyamoya patients: swift disappearance of ischemic attacks and maintenance of mental capacity. Neurol Med Chir (Tokyo) 1991;31:708–714. doi: 10.2176/nmc.31.708. [DOI] [PubMed] [Google Scholar]
- 20.Sato H, Sato N, Tamaki N, Matsumoto S. Chronic low-perfusion state in children with moyamoya disease following revascularization. Childs Nerv Syst. 1990;6:166–171. doi: 10.1007/BF00308495. [DOI] [PubMed] [Google Scholar]
- 21.Tagawa T, Itagaki Y, Mimaki T, Tanaka J, Ito N, Suzuki Y, et al. Intelligence and regional cerebral blood flow in children with Moyamoya disease. No To Hattatsu. 1989;21:9–13. [PubMed] [Google Scholar]
- 22.Ibayashi K, Takeuchi S, Ishii R, Tanaka R, Tsuruoka H. Intelligence and memory function of juvenile patients with moyamoya disease. With reference to the effect of surgical treatment. Nerv Syst Child. 1985;10:155–161. [Google Scholar]
- 23.Su SH, Hai J, Zhang L, Yu F, Wu YF. Assessment of cognitive function in adult patients with hemorrhagic moyamoya disease who received no surgical revascularization. Eur J Neurol. 2013;20:1081–1087. doi: 10.1111/ene.12138. [DOI] [PubMed] [Google Scholar]
- 24.Karzmark P, Zeifert PD, Tan S, Dorfman LJ, Bell-Stephens TE, Steinberg GK. Effect of moyamoya disease on neuropsychological functioning in adults. Neurosurgery. 2008;62:1048–1051. doi: 10.1227/01.neu.0000325866.29634.4c. [DOI] [PubMed] [Google Scholar]
- 25.Festa JR, Schwarz LR, Pliskin N, Cullum CM, Lacritz L, Charbel FT, et al. Neurocognitive dysfunction in adult moyamoya disease. J Neurol. 2010;257:806–815. doi: 10.1007/s00415-009-5424-8. [DOI] [PubMed] [Google Scholar]
- 26.Lei Y, Su J, Jiang H, Guo Q, Ni W, Yang H, et al. Aberrant regional homogeneity of resting-state executive control, default mode, and salience networks in adult patients with moyamoya disease. Brain Imaging Behav. 2017;11:176–184. doi: 10.1007/s11682-016-9518-5. [DOI] [PubMed] [Google Scholar]
- 27.Kazumata K, Tha KK, Narita H, Kusumi I, Shichinohe H, Ito M, et al. Chronic ischemia alters brain microstructural integrity and cognitive performance in adult moyamoya disease. Stroke. 2015;46:354–360. doi: 10.1161/STROKEAHA.114.007407. [DOI] [PubMed] [Google Scholar]
- 28.Karasawa J, Touho H, Ohnishi H, Miyamoto S, Kikuchi H. Long-term follow-up study after extracranial-intracranial bypass surgery for anterior circulation ischemia in childhood moyamoya disease. J Neurosurg. 1992;77:84–89. doi: 10.3171/jns.1992.77.1.0084. [DOI] [PubMed] [Google Scholar]
- 29.Kuroda S, Houkin K, Ishikawa T, Nakayama N, Ikeda J, Ishii N, et al. Determinants of intellectual outcome after surgical revascularization in pediatric moyamoya disease: a multivariate analysis. Childs Nerv Syst. 2004;20:302–308. doi: 10.1007/s00381-004-0924-4. [DOI] [PubMed] [Google Scholar]
- 30.Calviere L, Catalaa I, Marlats F, Viguier A, Bonneville F, Cognard C, et al. Correlation between cognitive impairment and cerebral hemodynamic disturbances on perfusion magnetic resonance imaging in European adults with moyamoya disease. Clinical article. J Neurosurg. 2010;113:753–759. doi: 10.3171/2010.4.JNS091808. [DOI] [PubMed] [Google Scholar]
- 31.Hosoda C, Nariai T, Ishiwata K, Ishii K, Matsushima Y, Ohno K. Correlation between focal brain metabolism and higher brain function in patients with moyamoya disease. Int J Stroke. 2010;5:367–373. doi: 10.1111/j.1747-4949.2010.00461.x. [DOI] [PubMed] [Google Scholar]
- 32.Mogensen MA, Karzmark P, Zeifert PD, Rosenberg J, Marks M, Steinberg GK, et al. Neuroradiologic correlates of cognitive impairment in adult moyamoya disease. AJNR Am J Neuroradiol. 2012;33:721–725. doi: 10.3174/ajnr.A2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kronenburg A, Esposito G, Fierstra J, Braun KP, Regli L. Combined bypass technique for contemporary revascularization of unilateral MCA and bilateral frontal territories in moyamoya vasculopathy. Acta Neurochir Suppl. 2014;119:65–70. doi: 10.1007/978-3-319-02411-0_11. [DOI] [PubMed] [Google Scholar]
- 34.Bulder MM, Hellmann PM, van Nieuwenhuizen O, Kappelle LJ, Klijn CJ, Braun KP. Measuring outcome after arterial ischemic stroke in childhood with two different instruments. Cerebrovasc Dis. 2011;32:463–470. doi: 10.1159/000332087. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Applied cognitive instruments/tests for each study
Predefined cognitive domains according to standard neuropsychological practice specified in Lezak[20]
Characteristics of studies assessing cognitive functions in children and adults with moyamoya vasculopathy
Neuropsychological test performances
Longitudinal neuropsychological test performances
Critical appraisal of the included studies
Linear regression analysis
Supplementary for Syntax
Supplementary for the Risk Assessment