Abstract
Spinal epidural abscesses (SEA) can be challenging to diagnose and may result in serious adverse outcomes sometimes leading to neurologic compromise, sepsis, and even death. While SEA may lead to litigation for healthcare providers, little is known about the medicolegal factors predicting case outcome of SEA related litigation cases. Three large medicolegal databases (VerdictSearch, Westlaw, and LexisNexis) were queried for SEA-related malpractice cases. Plaintiff (patient) age, sex, previous infection history and clinical outcomes such as residual paraplegia/quadriplegia, and delay in diagnosis or treatment were examined. The relationship between these variables and the proportion of plaintiff rulings and size of indemnity payments were assessed. Of the 135 cases that met inclusion criteria, 29 (21.5%) settled, 59 (43.7%) resulted in a defendant ruling, and 47 (34.8%) resulted in a plaintiff ruling. Mean award for plaintiff rulings was $4,291,400 (95% CI, $5,860,129 to $2,722,671), which was significantly larger than mean awards for cases that settled out of court, $2,324,170 (95% CI, $3,206,124 to $1,442,217) (P<0.05). The proportion of plaintiff verdicts and size of monetary awards were not significantly related to age or sex of the patient. A previously known infection was not significantly associated with the proportion of plaintiff verdicts or indemnity payments (P>0.05). In contrast, plaintiff verdicts were more common for patients who became paraplegic or quadriplegic (P<0.02) and were associated with significantly higher monetary awards (P<0.05) relative to patients without paralysis. Plaintiff verdicts were also more common when cases had an associated delay in diagnosis (P=0.008) or delay in treatment (P<0.001). Internists were the most commonly sued physician named in 20 (14.8%) suits, followed by anesthesiologists in 13 (9.6%) suits, emergency medicine physicians in 12 (8.9%) suits, family medicine physicians in 9 (6.7%) suits, neurosurgeons and orthopedic surgeons in 6 (4.4%) suits each, and multiple providers in 2 (1.5%) suits. The remaining lawsuits were against a hospital or another specialty not previously listed This investigation examined legal claims associated with SEA and found that the likelihood of a plaintiff verdict was significantly related to patient outcome (paralysis) and physician factors (delay in diagnosis or treatment compared). Additionally, paralyzed plaintiffs receive higher award payouts. Non-operative physicians, who are often responsible for initial diagnosis, were more frequently named in malpractice suits than surgeons. Increased awareness of the medicolegal implications of SEA can better prevent delays in diagnosis and treatment, and thus, alleged negligence-based lawsuits.
Key words: Spinal epidural abscess, malpractice litigation
Introduction
Spinal epidural abscess (SEA) is a lifethreatening infectious condition in which purulent material accumulates in the epidural space. The condition is challenging to diagnose and may result in serious adverse outcomes sometimes leading to neurologic compromise, sepsis, and even death. SEA presents with a high degree of individual variability. The classic triad of neurologic deficit, spinal pain, and fever may not be found on initial patient presentation, and delays in diagnosis can increase the risk of severe neurologic deficit.1 Reliance on the classic triad of SEA is not sufficient to consistently diagnose SEA in a timely manner and can lead to litigation risk.
Previous studies have addressed the medicolegal aspects of SEA. In 2013, French et al. examined 19 cases of SEA (or spinal epidural hematoma) and found that delay in treatment resulted in unfavorable verdicts for providers.2 In 2017, DePasse et al. observed that a delay in diagnosis, a delay in treatment, and increased severity of neurologic injury resulted in a higher proportion of plaintiff (patient) verdicts and higher indemnity payments in a single legal database.3 The aim of this study was to more discretely examine risk factors for SEA litigation. In addition to delay in diagnosis, delay in treatment, and increased severity of neurologic injury, we hypothesized that the route of infection and the specific profession of the physician named in the lawsuit are related to plaintiff verdicts and higher indemnity payments.
Materials and Methods
VerdictSearch (ALM Media Properties, LLC, New York, NY), Westlaw (Thomson Reuters Corporation, New York, NY), and LexisNexis (RELX Group, Dayton, Ohio) are online, publicly available legal research databases. The databases were queried for all medical malpractice litigation cases regarding SEA. Only cases in which court decisions were made based on the medical merits of the arguments were included in this study; cases involving statutory interpretation and legal precedence were excluded. Furthermore, cases in which SEA was a characteristic of the case, and not the primary subject of arguments, were excluded.
The VerdictSearch database was queried for the term epidural abscess. Results were filtered to the malpractice subcategory, and cases involving brain abscesses were excluded. The Westlaw database was queried for the term epidural abscess. Results were filtered to the jury verdicts and settlements subcategory for all federal and state cases between 1986-2016. Finally, the LexisNexis database was queried for the term epidural abscess. Results were filtered to the all federal and state courts subcategory between 1986-2016.
Data was abstracted to include the age and sex of the patient, whether the plaintiff had a known infection prior to diagnosis, the mechanism of infection (assessed as direct and non-direct inoculation), the severity of neurologic complications (assessed from less severe pain, weakness, and numbness to more severe permanent paraplegia and quadriplegia), the presence of a delay in diagnosis or treatment, the presence of the classic triad of SEA symptoms, the specialty of the provider and the state in which the claim was filed. The outcome of the lawsuit was recorded (as patient, physician or settlement verdicts) along with the indemnity payment. Exclusion criteria included cases with missing information, cases not relevant to spinal epidural abscess, or duplicates of cases in the databases.
This study used Chi-Square tests with Microsoft Excel (Microsoft Corporation, Redmond WA) to assess the association of SEA litigation risk factors with the proportion of cases that settled and the proportion of cases that resulted in plaintiff verdicts. Furthermore, effects of the assessed risk factors on indemnity payments were evaluated using Student’s t-tests. Statistical significance was set at P<0.05.
Results
Databases characteristics
In total, 67 VerdictSearch cases, 154 Westlaw cases and 127 LexisNexis cases were assessed. Of the 67 VerdictSearch cases assessed, 9 cases were excluded for insufficient information, leaving a total of 58 cases for analysis. Of the 154 Westlaw cases assessed, 20 were excluded for insufficient information, 36 were excluded for overlapping with VerdictSearch cases, and 21 were excluded for being repeat cases within Westlaw. A total of 77 Westlaw cases remained for analysis. Of the 127 LexisNexis cases assessed, 103 cases were excluded for insufficient information, 5 overlapped with VerdictSearch cases, 8 overlapped with Westlaw cases, and 11 were repeated cases within LexisNexis. Thus, 13 LexisNexis cases remained for analysis, and a grand total of 135 cases met inclusion criteria for this study (Table 1).
Table 1.
Databases characteristics.
| Westlaw (154) | VerdictSearch (67) | LexisNexis (127) | |
|---|---|---|---|
| Overlapped with Westlaw | - | 36 | 8 (retained with overlap) |
| Overlapped with VerdictSearch | 36 (removed) | - | 5 (retained with overlap) |
| Overlapped with LexisNexis | 8 | 5 | - |
| Insufficient Information (all removed) | 20 | 9 | 103 |
| Repeated case within same database (all removed) | 21 | 0 | 11 |
| Remaining cases for analysis | 77 | 58 | 13 |
Demographics and case characteristics
The mean age of the plaintiff was 47.7±14.8 years, with 57 (42.2%) female plaintiffs and 78 (57.8%) male plaintiffs. In the 53 (39.3%) cases in which the plaintiff was under 50 years of age, there was no difference in either the proportion of settlements versus court cases (P>0.48) or the proportion of plaintiff verdicts versus defendant verdicts (P>0.09) when compared to cases in which the plaintiff was over 50. Similarly, for the 78 cases with male plaintiffs, there was no difference in either proportion when compared to cases with female plaintiffs (P>0.34, P>0.06). Neither age (P>0.63) nor gender (P>0.14) were significantly related to the size of the indemnity payments (Table 2).
Table 2.
Malpractice suit case characteristics.
| Variable | No. cases |
|---|---|
| Mean age | 47.7±14.8 yrs |
| Sex | |
| Females | 57 (42.2%) |
| Males | 78 (57.8%) |
| Known infection prior to diagnosis | |
| Known infection | 33 |
| Unknown infection | 66 |
| Mechanism of infection | |
| Spinal injection | 18 |
| IV drug use | 9 |
| Other | 5 |
| Neurologic complications | |
| Less severe | |
| (weakness, pain, numbness) | 47 |
| More severe | |
| (paraplegia, quadriplegia) | 76 |
| Death | 6 |
| Delay in diagnosis | 107 (79.3%) |
| Delay in treatment | 25 (18.5%) |
| Profession sued | |
| Hospital | 35 |
| Internist | 20 |
| Anesthesiologist | 13 |
| Emergency medicine | 12 |
| Family medicine | 9 |
| Neurosurgeon | 6 |
| Orthopedic surgeon | 6 |
| Radiologist | 5 |
| Multiple professions | 2 |
| Other | 27 |
Litigation outcomes
Of the 135 cases, 29 (21.5%) settled and 106 (78.5%) went to trial. Of those that proceeded to trial, 59 (55.7%) resulted in a defendant ruling and 47 (43.3%) resulted in a plaintiff ruling. Overall, 34.8% of all cases resulted in a verdict for the plaintiff.
The mean award for plaintiff rulings was $4,291,400 (95% CI, $5,860,129 to $2,722,671), which was significantly larger than mean awards for cases that settled out of court, $2,324,170 (95% CI, $3,206,124 to $1,442,217) (P<0.05). Geographic distributions of SEA lawsuits nationwide (Figure 1), as well as the U.S. regional frequency of SEA lawsuits with mean indemnity payments (Table 3) were analyzed by U.S. Divisions. Divisions are based on the U.S. Census Bureau’s most recent guidelines.
Figure 1.
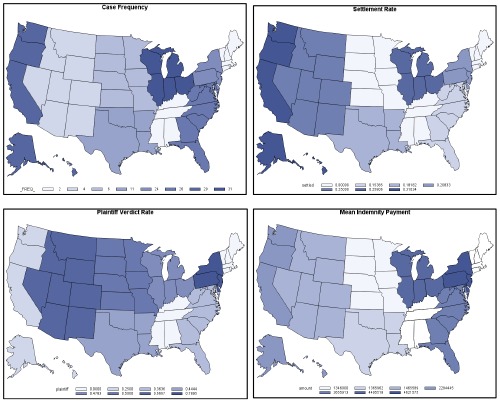
Map of SEA cases and case characteristics across the U.S.
Table 3.
Malpractice suit cases per U.S. region and division.
| U.S. Division | Case Frequency | Mean Award ($) | Standard Deviation ($) | Minimum ($) | Maximum (S) | |
|---|---|---|---|---|---|---|
| REGION 1 | Division 1 (CT, ME, MA, NH, RI, VT) | 2 (All Defendant Verdicts) | 0 | 0 | 0 | 0 |
| Division 2 (DE, NJ, NY, PA) | 24 | 4,864,815 | 6,494,838 | 200,000 | 22,903,000 | |
| REGION 2 | Division 3 (IL, IN, MI, OH, WI) | 31 | 4,495,518 | 3,453,306 | 185,000 | 12,350,000 |
| Division 4 (IA, KS, MN, MO, NE, ND, SD) | 6 | 1,346,000 | 680,843 | 750,000 | 2,088,000 | |
| REGION 3 | Division 5 (FL, GA, MD, NC, SC, VA, DC, WV) | 26 | 3,655,913 | 5,174,403 | 452,918 | 19,252,039 |
| Division 6 (AL, KY, MS, TN) | 2 (All Defendant Verdicts) | 0 | 0 | 0 | 0 | |
| Division 7 (AR, LA, OK, TX) | 11 | 1,365,962 | 924,922 | 100,000 | 2,425,774 | |
| REGION 4 | Division 8 (AZ, CO, ID, MT, NV, NM, UT, WY) | 4 | 1,465,589 | 2,066,219 | 4,551 | 2,926,627 |
| Division 9 (AK, CA, HI, OR, WA) | 29 | 2,284,445 | 2,700,309 | 100,000 | 9,420,840 |
Profession sued
Multiple physician specialties were named in lawsuits including internists in 20 (14.8%) suits, followed by anesthesiologists in 13 (9.6%) suits, emergency medicine physicians in 12 (8.9%) suits, family medicine physicians in 9 (6.7%) suits, neurosurgeons and orthopedic surgeons in 6 (4.4%) suits each, and multiple providers in 2 (1.5%) suits (including a radiologist, infectious disease specialist and neurologist in one suit, and two neurologists and an orthopedic surgeon in the other) (Table 2). The remaining lawsuits involved hospitals, prison health services, Veterans Health Administration, and one lawsuit each in which the defendant was an obstetrician, general surgeon, infectious disease specialist, pediatrician, and urogynecologist.
Patients involved in suits against the most commonly sued professions (internists, emergency medicine physicians, and anesthesiologists) were more likely to have a favorable legal outcome (P<0.02) and were more likely to win verdicts when taken to court (P<0.05) when compared to all other professions sued. We detected no difference in the likelihood to settle (P>0.2) or in indemnity payment (P>0.8) when comparing these professions.
Known infection and mechanism of infection
In 33 (24.4%) cases, there was a known source of infection prior to diagnosis of SEA. There was no difference in proportion of settlements, proportion of plaintiff verdicts, or indemnity payments (P>0.86, P>0.57 and P>0.32, respectively) when compared to 66 (48.9x%) cases with no known infection. 18 (13.3%) patients had a recent history of epidural injection, 9 (6.7%) patients had a known history of IV drug use (IVDU) and 5 (3.7%) had a recent epidural catheter placement. Compared to all non-direct inoculation cases, in these 32 (23.7%) cases with alleged direct inoculation etiologies (i.e., invasive spine injections, catheter placement or IVDU), there was no significant difference in proportion of settlements, plaintiff verdicts or indemnity payments (P>0.36, P>0.35 and P>0.56 respectively).
Neurologic complications
Neurologic sequelae of SEA included less severe neurologic injury (including pain, weakness or numbness) in 47 (34.8%) patients, severe injury (including paraplegia or quadriplegia) in 76 (56.3%) patients and death in 6 (4.4%) patients. All cases involving the death of the plaintiff reported plaintiffs previously suffering from quadriplegia. Though there was no difference in the proportion of settlements in cases with severely injured plaintiffs (P=0.64); these plaintiffs were more likely to receive a plaintiff verdict if the case went to trial compared to cases with less severely injured plaintiffs (P=0.02) (Table 4). Furthermore, severely injured plaintiffs received mean awards of $7,949,505, which were significantly larger than mean awards ($1,120,373) for plaintiffs without devastating neurologic sequelae (P<0.05).
Table 4.
Outcomes for plaintiffs with less severe and plaintiffs with more severe neurologic complications.
| Settlement | Court case | Plaintiff verdict | Defense verdict | |
|---|---|---|---|---|
| More severe | 19 | 57 | 32* | 25 |
| Less severe | 10 | 37 | 12 | 25 |
*P<0.05.
Further investigation in this study found no difference between the proportion of settled cases to court cases for paraplegics and quadriplegics (P>0.51), nor was a there a difference in payments awards when comparing these two levels of severe neurologic sequelae (P>0.21). No difference in indemnity payment was found between paraplegics and quadriplegics (P>0.25).
Delay in diagnosis or treatment
A delay in diagnosis was alleged in 107 (79.3%) cases, and a delay in treatment was alleged in 25 (18.5%) cases. A delay in diagnosis was more likely to result in a plaintiff verdict if the case went to court (P<0.0002) (Table 5). However, we found no significant difference in the likelihood to settle between cases with a delayed diagnosis and cases with no delay in diagnosis (P>0.13). No difference in payment was detected when compared to no delayed in diagnosis (P>0.93).
Table 5.
Outcomes for cases with and without delayed diagnosis.
| Settlement | Court case | Plaintiff verdict | Defense verdict | |
|---|---|---|---|---|
| Delay in diagnosis | 25 | 82 | 42** | 40 |
| No delay | 4 | 24 | 5 | 19 |
**P<0.001.
Similarly, in the 25 cases (18.5%) in which there was alleged delay in treatment after the diagnosis of SEA had been made, plaintiffs were more likely to win (P=0.0007) (Table 6). There was one case with a physician verdict when an alleged delay in treatment and the case went to trial. Delay in treatment did not affect the proportion of cases that settled (P=0.16). No difference in monetary award was detected when compared to no delay in treatment (P>0.32).
Table 6.
Outcomes for cases with and without delayed treatment.
| Settlement | Court case | Plaintiff verdict | Defense verdict | |
|---|---|---|---|---|
| Delay in treatment | 8 | 17 | 15** | 2 |
| No delay | 21 | 89 | 32 | 57 |
**P<0.001.
Discussion
While SEA is an uncommon condition, its incidence is rising given the increase in prevalence of patients at risk (including patients with diabetes mellitus, intravenous drugs users, infection with HIV, degenerative bone disease and trauma), heightened awareness of SEA, and increased use of sensitive imaging techniques.4-8 SEA presents a high risk for malpractice litigation, however, only two previous studies have specifically examined the medicolegal outcomes of SEA. This study utilized three extensive, validated databases to assess the factors of SEA malpractice litigation over a larger sample size and greater timeframe than previously performed studies.
Our study found that a subgroup of medical practitioners (internists, emergency medicine physicians, and anesthesiologists) are most likely to be sued for cases of SEA. Plaintiffs in these suits are more likely to have a favorable outcome, including either settling or winning in court.
Internists were the most commonly sued profession often for delaying diagnosis due to failing to consult neurologic or orthopedic services, recognizing SEA as a potential cause of symptoms, or ordering imaging in a timely manner. Emergency medicine physicians, the third most commonly sued profession, often allegedly failed to do an appropriately timed workup of SEA (including necessary radiologic imaging). When patients present multiple times in a short interval (i.e., within 12-36 hours) with worsening complaints or neurologic deficits, clinical/imaging evaluations for SEA is warranted, as early recognition of SEA can minimize neurologic morbidity.9 As internists and emergency medicine physicians are most likely to provide the first clinical assessment of SEA patients, a heightened awareness of the high variability in clinical presentation of SEA may help to avoid delays in diagnosis and treatment, and thus, costly litigation.1
Anesthesiologists were the second most commonly sued individual profession, likely because infections are a known and not fully preventable complication of invasive spinal procedures. Yet, of the 13 cases in which anesthesiologists were named in the suit, 10 were defendant verdicts, while one plaintiff verdict was a delay in treatment. When compared to the other most commonly sued professions (internists and emergency medicine physicians), anesthesiologists are at a relatively lower risk of losing legal cases. Despite being difficult to prove, a breach in sterile technique was alleged in the other two plaintiff verdicts. Nevertheless, careful screening mechanisms are necessary for those giving injections when patients present with symptoms which may represent infection of the epidural space.
In total, 35 (25.9%) of the 135 cases involved hospitals. While a very small proportion of these cases had prorated negligence indemnity payments for specific defendants, the vast majority were suits against hospitals as a whole. Any indication of SEA warrants multiple providers’ involvement in the case (from the initial suspicion of SEA to imaging and treatment). Best care practices should properly reflect multi-specialty involvement.
This study found no association between the route of infection and outcomes. Knowledge of a patients’ medical history, social background and risk of SEA may not be as helpful relative to more sensitive indicators and clinical features. Furthermore, outcomes were not affected by the incremental increase in severity of injury (paraplegia versus quadriplegia), but rather by whether or not a severe injury occurred. This suggests that physicians should ambitiously aim to avoid any delay in diagnosis, since the severity of neurologic sequelae is often difficult to predict immediately prior to the onset of more indicative SEA symptoms. Such high interindividual variability questions whether the classic triad used by frontline clinicians to make an initial clinical assessment is reliable in reaching the diagnosis of SEA in a timely manner. Nevertheless, the other findings in this study are largely consistent with those of DePasse et al.: delayed diagnosis, delayed treatment and neurologic complications result in more plaintiff wins, while age, sex and pre-existing known infection do not affect outcomes.
Consistent with DePasse et al., our study demonstrates an association between neurological outcome and case outcome. Paralyzed plaintiffs were both more likely to win verdicts and receive higher monetary awards. However, there were no differences in outcomes between quadriplegic and paraplegic plaintiffs. This suggests that legal outcomes are determined broadly by the severity of neurologic deficit but indemnity payments may not be based on the specific level of spinal injury.
This study is the largest of its kind that examines SEA litigation. The methods reflect a careful procedure for capturing relevant, categorical data within the medicolegal databases. Nevertheless, this study has limitations, which include the limited amount of extractable information from the legal databases. Cases often have missing information pertinent to making claims about current standard of care practices. Due to the fact that the databases are not created for health care professionals, clinical detail is limited and often excludes important information on patient risk factors, affected spinal levels and specific SEA pathogens. Nevertheless, VerdictSearch, Westlaw, and LexiNexis have proved useful in previous studies to evaluate legal claims.10-12 Future studies should more precisely correlate risk factors for SEA litigation with deficiencies in current diagnostic practices to avoid costly litigation and better serve patients.
Conclusions
This investigation identified factors associated with plaintiff verdicts and indemnity payments across three medicolegal databases for cases associated with spinal epidural abscess. Delays in diagnosis and neurologic deficits are significantly associated with medicolegal outcomes. Primary care providers, often responsible for the initial diagnosis of SEA were the most commonly sued physicians. Educational initiatives and quality care improvement projects for primary care providers should focus on avoiding delays in diagnosis which may mitigate patient risk and prevent costly litigation.
References
- 1.Rosc-Bereza K, Arkuszewski M, Ciach- Wysocka E, Boczarska-Jedynak M. Spinal epidural abscess: common symptoms of an emergency condition. A case report. Neuroradiol J 2013;26:464-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.French KL, Daniels EW, Ahn UM, Ahn NU. Medicolegal cases for spinal epidural hematoma and spinal epidural abscess. Orthopedics 2013;36:48-53. [DOI] [PubMed] [Google Scholar]
- 3.DePasse JM, Ruttiman R, Eltorai AEM, et al. Assessment of malpractice claims due to spinal epidural abscess. J Neurosurg Spine 2017:1-8. [DOI] [PubMed] [Google Scholar]
- 4.Bond A, Manian FA. Spinal epidural abscess: a review with special emphasis on earlier diagnosis. Biomed Res Int 2016;2016:1614328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sendi P, Bregenzer T, Zimmerli W. Spinal epidural abscess in clinical practice. QJM 2008;101:1-12. [DOI] [PubMed] [Google Scholar]
- 6.Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev 2000;23:175-204; discussion 5. [DOI] [PubMed] [Google Scholar]
- 7.Pradilla G, Ardila GP, Hsu W, Rigamonti D. Epidural abscesses of the CNS. Lancet Neurol 2009;8:292-300. [DOI] [PubMed] [Google Scholar]
- 8.Darouiche RO. Spinal Epidural Abscess. N Engl J Med 2006;355:2012-20. [DOI] [PubMed] [Google Scholar]
- 9.Khursheed N, Dar S, Ramzan A, et al. Spinal epidural abscess: report on 27 cases. Surg Neurol Int 2017;8:240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Epstein NE. A review of medicolegal malpractice suits involving cervical spine: what can we learn or change? J Spinal Disord Tech 2011;24:15-9. [DOI] [PubMed] [Google Scholar]
- 11.Epstein NE. It is easier to confuse a jury than convince a judge: the crisis in medical malpractice. Spine (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]


