Abstract
Background
The potential therapeutic values of Korean Red Ginseng extract (KRGE) in autoimmune disorders of nervous system have not been fully investigated.
Methods
We used an acute experimental autoimmune encephalomyelitis animal model of multiple sclerosis and determined the effects and mechanism of KRGE on spinal myelination.
Results
Pretreatment with KRGE (100 mg/kg, orally) for 10 days before immunization with myelin basic protein (MBP)68–82 peptide exerted a protective effect against demyelination in the spinal cord, with inhibited recruitment and activation of immune cells including microglia, decreased mRNA expression of detrimental inflammatory mediators (interleukin-6, interferon-γ, and cyclooxygenase-2), but increased mRNA expression of protective inflammatory mediators (insulin-like growth factor β1, transforming growth factor β, and vascular endothelial growth factor-1). These results were associated with significant downregulation of p38 mitogen-activated protein kinase and nuclear factor-κB signaling pathways in microglia/macrophages, T cells, and astrocytes.
Conclusion
Our findings suggest that KRGE alleviates spinal demyelination in acute experimental autoimmune encephalomyelitis through inhibiting the activation of the p38 mitogen-activated protein kinase/nuclear factor-κB signaling pathway. Therefore, KRGE might be used as a new therapeutic for autoimmune disorders such as multiple sclerosis, although further investigation is needed.
Keywords: demyelination, experimental autoimmune encephalomyelitis, Korean Red Ginseng, nuclear factor-κB, p-38 mitogen-activated protein kinase
1. Introduction
Multiple sclerosis (MS), a chronic, inflammatory, and demyelinating disease of the central nervous system (CNS), is affecting thousands of people worldwide [1], [2]. Although many possible mechanisms have been suggested for the pathogenesis of MS, it is currently accepted that infiltration of immune cells including autoreactive T cells [especially interferon (IFN)-γ-producing T cells [T helper 1 (Th1)] and interleukin (IL)-17-producing Th17 subsets] into the CNS through the blood–brain barrier is the direct cause of demyelination [3]. These activated immune cells can secrete inflammatory mediators that contribute to inflammation and demyelination in the brain and spinal cord [1], [2]. Mitogen-activated protein kinase (MAPK) signaling pathways are involved in direct cellular responses to a diverse array of stimuli such as mitogens, osmotic stress, heat shock, and proinflammatory cytokines [4]. Specifically, pharmacological inhibition of p38 MAPK can selectively ameliorate experimental autoimmune encephalomyelitis (EAE), indicating that p38 MAPK might be associated with the onset of EAE [5]. As an upstream signal in the inflammation pathway, phosphorylated (p) p38 MAPK can mediate activation of the nuclear factor (NF)-κB signaling pathway [6]. The NF-κB pathway is highly relevant to autoimmunity. Targeting the NF-κB pathway may be an effective approach in treating immune-mediated diseases [7]. Microarray analysis of genes from brain tissue of patients with MS has revealed a positive relationship between MS and the NF-κB pathway [8], [9]. NF-κB-deficient mice are reported to be significantly resistant to EAE [10]. Nevertheless, the role of p38 MAPK and NF-κB signaling pathways in the pathogenesis of MS remains unclear.
The international standard to treat MS is by using corticosteroids including Dexamethasone, Methylprednisolone, Solumedrol, and Prednisone either orally or via intravenous administration. These medications are usually prescribed for short term (during a relapse). They are not recommended for long-term use in MS because of adverse effects such as reduced natural immune response [11], [12], [13]. Currently, disease-modification therapy represents a promising new approach to treat MS. However, principal MS medications such as Avonex (IFN-β-1a), Betaseron (IFN-β-1b), Copaxone (glatiramer acetate), and Gilenya (fingolimod) may produce significant adverse effects such as mood disorders, loose fat around the area of the injection, chest pain, and depression [11], [12], [13]. Therefore, efficient and safe drugs are urgently needed for the treatment of MS.
Currently, traditional herbal medicines have been gradually gaining popularity to enhance normal physical condition and treat disease because they have various active constituents [14]. Panax ginseng Meyer, a representative herbal medicine, has been called the elixir of life for its mysterious medicinal effects in Eastern Asia including Korea, China, and Japan for > 2,000 years. It has been widely used as a restorative therapy or tonic rather than as a cure for a particular illness [15], [16]. According to existing studies, total ginseng extract and its main ingredients such as ginsenosides, polysaccharides, and gintonin have beneficial effects for neurological and immunological disorders possibly through regulating the MAPK/NF-κB signaling pathway and mediating inflammation [15], [17], [18]. The aqueous extract of North American ginseng can significantly decrease clinical signs of EAE via inhibiting inflammatory mediators such as the levels of circulating tumor necrosis factor-α and CNS immunoreactive inducible nitric oxide (iNOS) [19]. An acidic polysaccharide of P. ginseng can ameliorate the progression of EAE by promoting the generation of immunosuppressive regulatory T (Treg) cells through activating transcription factor forkhead box (Fox)p3 [20]. Ginsenoside Rd can effectively ameliorate the clinical severity of EAE through reducing the permeability of the blood–brain barrier and promoting Th2 shift both in vivo and in vitro [21]. Recently, we have reported that Korean Red Ginseng (KRG; steamed root of P. ginseng) and ginsenoside-Rb1/Rg1 can alleviate EAE by suppressing Th1 and Th17 cells and upregulating Treg cells [22]. These reports suggest that ginseng has potential to be used in multitarget approaches to treat MS/EAE. These reports also increase the possibility that ginseng might exert a protective effect on EAE via regulating yet undemonstrated different signaling pathways. Here, we demonstrated that Korean Red Ginseng extract (KRGE) could protect spinal demyelination in acute EAE model through downregulating the p38 MAPK/NF-κB signaling pathway.
2. Materials and methods
2.1. Animals and ethical approval
Ten-week-old female Lewis rats (Japan SLC Inc., Hamamatsu, Japan) were kept at a constant temperature of 23 ± 3°C with a 12-h light–dark cycle (lights on 08:00 to 20:00 h), and fed food and water ad libitum. The animals were allowed to habituate to the housing facilities for 1 week before the experiments. All experimental procedures were reviewed and approved by the Institutional Animal Care and Use Committee of Kyung Hee University. In this process, proper randomization of laboratory animals and handling of data were performed in a blinded manner in accordance with recent recommendations from a National Institutes of Health Workshop on preclinical models of neurological diseases [23].
2.2. KRGE preparation
KRGE (Hong Sam Jung Plus; Lot No. H2006(3)-3065) was obtained from Korea Ginseng Corporation, Daejeon, Korea. KRGE was prepared from roots of 6-year-old fresh P. ginseng as previously described [24]. Briefly, KRG was made by steaming fresh ginseng roots at 90–100°C for 3 h followed by drying at 50–80°C. KRGE was prepared from KRG water extract after three 8-h cycles of extraction in circulating hot water (85–90°C). KRGE contained major ginsenosides Rb1 (7.44 mg/g), Rb2 (2.59 mg/g), Rc (3.04 mg/g), Rd (0.91 mg/g), Re (1.86 mg/g), Rf (1.24 mg/g), Rg1 (1.79 mg/g), Rg2s (1.24 mg/g), Rg3s (1.39 mg/g), and Rh1 (1.01 mg/g), and other minor ginsenosides.
2.3. Experimental groups, EAE induction, clinical evaluation, and KRGE treatment
Rats were divided into the following four groups: (1) Sham [saline, subcutaneous (s.c.) + saline, per oral (p.o.)]; (2) MBP [300 μg myelin basic protein peptide (MBP68–82), s.c. + saline, p.o.]; (3) MBP + KRGE [300 μg MBP68–82, s.c. + 100 mg/kg KRGE, p.o.]; and (4) KRGE [saline, s.c. + 100 mg/kg KRGE, p.o.]. EAE was induced as described previously [22], [25] with an emulsion containing 300 μg MBP68–82 peptide (Sigma–Aldrich, St. Louis, MO, USA) in complete Freund's adjuvant (Difco, Detroit, MI, USA) and 250 ng pertussis toxin (List Biologic, Campbell, CA, USA). Rats in the sham group were treated with saline alone instead of MBP68-82 peptide, pertussis toxin, or KRGE. In a previous study [22], 100 mg/kg KRGE was found to be the most effective dose (25 mg/kg/d, 50 mg/kg/d, and 100 mg/kg/d) treatments in MBP-induced EAE. Therefore, we treated rats once daily at a dose of 100 mg/kg KRGE. Clinical signs were evaluated daily using the clinical scoring scale as described previously [22].
2.4. Histopathological assessment of spinal cords
To evaluate histopathological changes, spinal sections were prepared as described previously [22], [25], [26]. Briefly, rats from each group were sacrificed at the peak of clinical score (13–14 d after immunization) and perfused intracardially with cold 4% paraformaldehyde in 0.1M phosphate buffer (pH 7.4). Spinal cords were removed, cryoprotected in 30% sucrose solution, and sectioned into 30-μm thickness using a cryostat microtome. To evaluate cellular infiltration, hematoxylin and eosin staining was performed as described previously [22], [25], [26].
2.5. Immunohistochemical evaluation
Frozen spinal sections from each group (n = 5 per group) were prepared at the peak of clinical score (13–14 d after immunization) as described previously [22]. Immunohistochemical staining was accomplished as previously described [22], [25], [26]. Briefly, anti-ionized calcium binding adaptor molecule-1 (Iba-1) antibody (1:2,000; Wako, Osaka, Japan) was used as primary antiserum and rabbit IgG (1:200; Vector Laboratories, Burlingame, CA, USA) was used as secondary antiserum. ABC kit (Vector Laboratories) was used for staining detection. Immunofluorescent staining was accomplished as described previously [26], [27]. Briefly, frozen spinal sections (n = 3 per spinal cord) were incubated with the following primary antibodies: rabbit anti-MBP (1: 500; Sigma–Aldrich), rabbit anti-p-p38 MAPK, p-IκBa, NF-κB/65, CD11b, glial fibrillary acidic protein (GFAP; 1: 500; Santa Cruz Biotechnology, Santa Cruz, CA, USA), and mouse anti-CD4 (1:500; BD Biosciences, San Jose, CA, USA) antibodies and secondary antibodies include Cyanine 3- and fluorescein-isothiocyanate-conjugated mouse/rabbit IgG antibody (1:200; Jackson ImmunoResearch, West Grove, PA, USA). To quantify the level of demyelination, all images from three sections per spinal cord in each group were captured using confocal imaging system (LSM 5 PASCAL; Carl Zeiss, Oberkochen, Germany). The integrated pixel density was measured using NIH Image J program (http://rsbweb.nih.gov/ij/). The level of demyelination was determined by dividing the total white matter area by the total demyelinated area.
2.6. Western blot analysis
Rats (n = 5 per group) were sacrificed at the peak of neurological impairment and their lumbar spinal cords were removed with lysis buffer (50mM Tris–HCl, pH 7.5, 150mM NaCl, 1% Triton X-100, 10% glycerol, and protease inhibitor mixture). Whole cell extract was prepared as described previously [22], [25], [26]. Nuclear and cytoplasmic extracts were separated as described previously by Dignam et al. [28]. Polyvinylidene difluoride membranes with transferred proteins were incubated with anti-p-extracellular signal-regulated kinase (ERK), p-C-Jun N-terminal kinase (JNK), and p-p38 (1:1,000; Cell Signaling Technology, Danvers, MA, USA) and rabbit anti- p-IκBɑ and NF-κB/65 (1:1,000; Santa Cruz Biotechnology) antibodies, followed by incubation with horseradish-peroxidase-conjugated secondary antibody to detection with enhanced chemiluminescence (Amersham Pharmacia Biotechnology, Piscataway, NJ, USA) and exposure to X-ray film. For normalization of antibody signal, the membranes were stripped and re-probed with antibodies for total ERK, JNK, p38, actin, glyceraldehyde 3-phosphate dehydrogenase (1:2,000; Cell Signaling Technology) and histone (1:1,000; Abcam, Cambridge, MA, USA). After western blotting was performed several times, the density of each band was converted to numerical values using the Photoshop CS2 program (Adobe, San Jose, CA, USA), subtracting background values from an area of film immediately adjacent to the stained band.
2.7. Real-time polymerase chain reaction
To determine the mRNA levels of inflammatory cytokines [interleukin (IL)-6 and IFN-γ], cyclooxegenase-2 (COX-2), and growth factors [insulin-like growth factor (IGF)-1, transforming growth factor (TGF-β), and vascular endothelial growth factor (VEGF)-1] at peak time of neurological impairment, the rats used for real-time polymerase chain reaction (PCR) analysis (n = 5 per group) were anesthetized, and each lumbar spinal cord was removed and deep frozen. Real-time PCR was performed using SYBR Green PCR Master Mix (Applied Biosystems, Foster City, CA, USA) as previously described [29]. Sequences of oligonucleotide primers are listed in Table 1. Expression levels of each gene were normalized to that of glyceraldehyde 3-phosphate dehydrogenase. All real-time-PCR experiments were performed at least three times.
Table 1.
PCR primer sequence for PCR analysis
| Primer | Forward Sequence (5'→3') | Reverse Sequence (5'→3') |
|---|---|---|
| Rat COX-2 | GCA TTC TTT GCC CAG CAC TTC ACT | TTT AAG TCC ACT CCA TGG CCC AGT |
| Rat GAPDH | AGG TCA TCC CAG AGC TGA ACG | CAC CCT GTT GCT GTA GCC GTA T |
| Rat IFN-γ | GAA AGC CTA GAA AGT CTG AAT AAC | GCA GCG ACT CCT TTT CCG CTT CCT |
| Rat IGF-1 | ATT GTG GAT GAG TGT TGC TTC | ATT GAT ATT TGG CAG GTG TTC C |
| Rat IL-6 | CAA GAG ACT TCC AGC CAG TTG C | TGG CCG AGT AGA CCT CAT AGT GAC C |
| Rat TGF-β | CTT CAG CTC CAC AGA GAA GAA CTG C | CAC GAT CAT GTT GGA CAA CTG CTC C |
| Rat VEGF-1 | CAG AGA TTC AAT TCA GTG GCC | GAG CAG GTC AGG TTC ACA GG |
2.8. Statistical analysis
Statistical analysis was performed using SPSS for Windows version 21.0 (SPSS Inc., Chicago, IL, USA). Multiple comparisons were made using one-way analysis of variance with Tukey post hoc test. All data are presented as mean ± standard error and statistical difference was accepted at the 5% level unless otherwise indicated.
3. Results
3.1. Effect of KRGE on demyelination and cellular infiltration in spinal cord of EAE rats
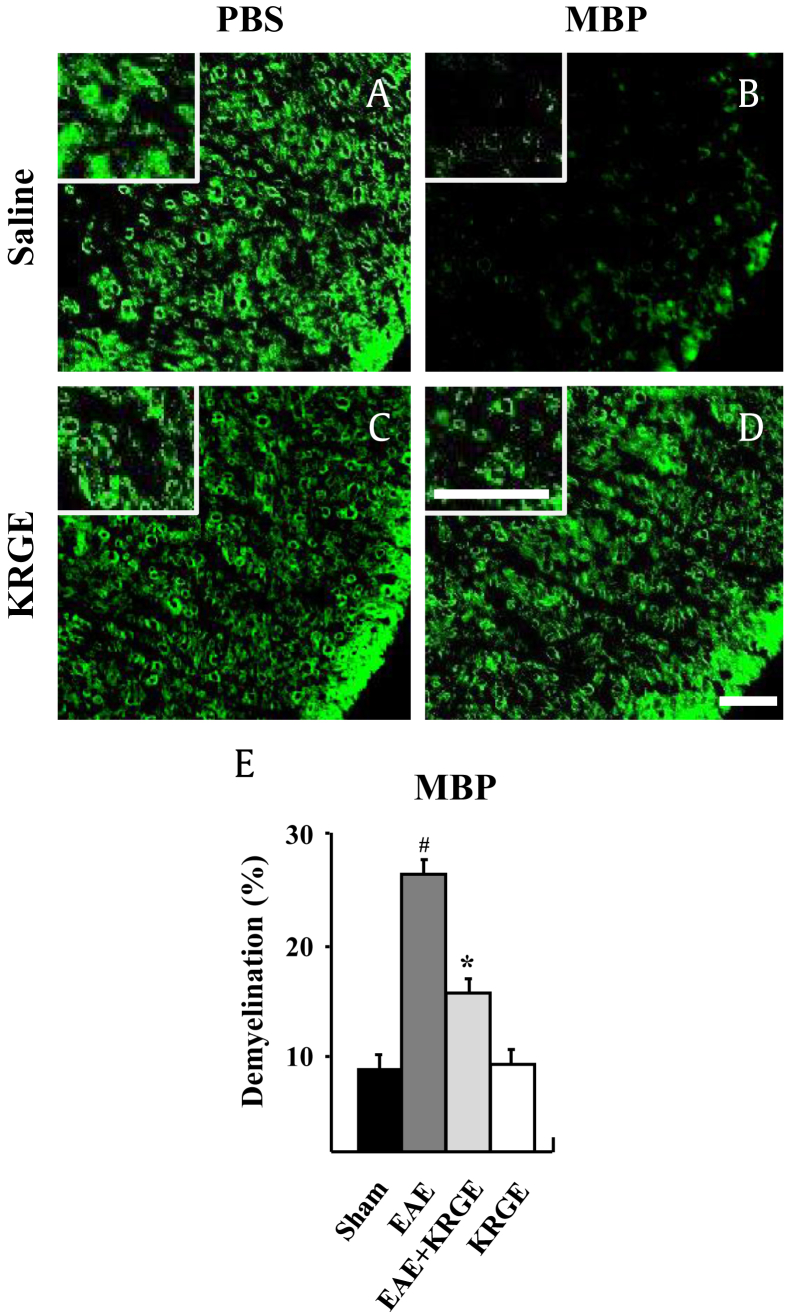
Previously, we have reported that KRGE could alleviate neurological symptoms and spinal demyelination based on staining with luxol fast blue in EAE rats [22]. Such effect is achieved by suppressing the differentiation/infiltration of Th1 and Th17 cells and upregulating the differentiation/infiltration of Treg cells [22]. In that study, the protective effect of KRGE on the both items is the best at 13–14 d (at peak of neurological symptoms) after EAE induction [22]. Thus, in the current study, we used the same time schedule (13–14 d after EAE induction) to further investigate the molecular mechanisms involved in the protective effect of KRGE on spinal demyelination in acute EAE. First, we determined whether KRGE could maintain the integrity of myelin in EAE rats. As shown in Fig. 1, immunofluorescent labeling of MBP (a marker for myelin) displayed an intact myelin-sheath-like ring in the white matter of the spinal cord in both the sham group and KRGE group (Figs. 1A, 1C). However, the immunofluorescence intensity in the spinal cord of the EAE group (Fig. 1B) was significantly lower than that of the sham or the KRGE group. The reduction in immunofluorescence intensity was blocked in the EAE + KRGE group (Fig. 1D). The level of demyelination was semiautomatically quantified (Fig. 1E). These results suggest that KRGE has protective effect against spinal demyelination in acute EAE.
Fig. 1.
KRGE reduces demyelination in the spinal cords of EAE rats. (A–D) Representative photographs showing the levels of demyelination by immunofluorescence staining using MBP antiserum. (E) Quantified graph of A–D. Analysis of variance test; #p < 0.01 versus sham group; *p < 0.01 versus EAE group. Bars, 50 μm. EAE, experimental autoimmune encephalomyelitis; KRGE = Korean Red Ginseng extract; MBP, myelin basic protein; PBS, phosphate-buffered saline.
3.2. Effects of KRGE on activation and infiltration of inflammatory/immune cells in the spinal cord of EAE rats
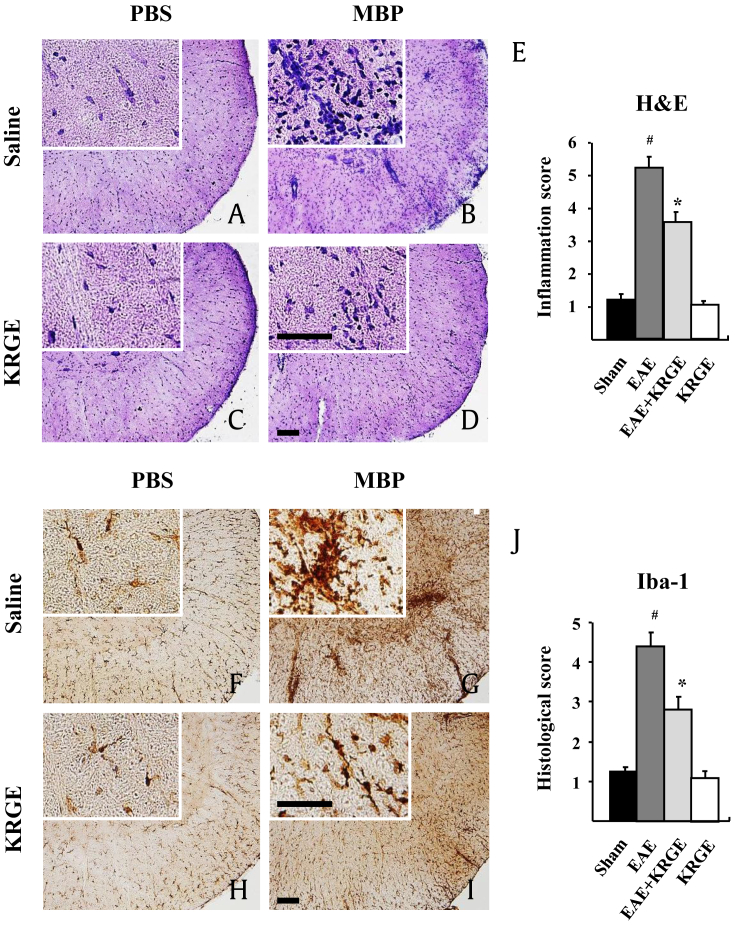
It is well known that inflammatory/immune cells infiltrate damaged lesions during the course of neurological diseases such as MS [30], [31]. Therefore, we tested the regulating effect of KRGE on cellular infiltration into the spinal cord of EAE rats by hematoxylin and eosin staining. As shown in Fig. 2, cellular infiltration in the white matter of the spinal cord of rats in the EAE group was increased (Figs. 2B, 2E) compared to that of mice in the sham or KRGE group (Figs. 2A, 2C, 2E). However, cellular infiltration in the white matter of the spinal cord of rats from the EAE + KRGE group was lower than that of the EAE group (Figs. 2C, 2E). Since inflammatory/immune cells may include resident microglia (the major intrinsic immunocompetent phagocytic cells in the CNS) and peripheral immune cells such as blood-derived macrophages and T cells [30], [31], we investigated the effect of KGRE on the distribution of microglia and macrophages in the spinal cord. In the white matter of the spinal cord of the sham and KRGE groups, Iba-1 (a marker for microglia/macrophage lineage cells) immunoreactive cells showed small cell bodies with thin processes (Figs. 2F, 2H, 2J), indicating resting form [24]. However, in the white matter of the spinal cord of the EAE group, Iba-1-immunoreactive cells showed enlarged cell bodies with short and thick processes with increased number (Figs. 2G, 2J), indicating activated form [22], [24], [25], [26], [32], [33]. Interestingly, Iba-1 immunoreactivity was significantly reduced in the spinal cord of the EAE + KRGE group compared to that of the EAE group (Figs. 2I, 2J). Our findings indicate that KRGE can help prevent spinal demyelination via inhibiting activation/infiltration of microglia and macrophages.
Fig. 2.
KRGE alleviates immune cell infiltrations in the spinal cords of EAE rats. (A–E) Representative photographs showing the level of inflammatory/cellular and microglia/macrophages infiltration by hematoxylin and eosin staining. (F–J) Representative photographs after immunohistochemistry staining using Iba-1 antiserum. Insets display high magnification micrographs of areas marked with squares. (E and J) Quantified graphs of A–D (E) and E–H (J). Analysis of variance test; #p < 0.01 versus sham group; *p < 0.01 versus EAE group. Bars, 100 μm. EAE, experimental autoimmune encephalomyelitis; H&E, hematoxylin and eosin, KRGE, Korean Red Ginseng extract; MBP, myelin basic protein; PBS, phosphate-buffered saline.
3.3. Effects of KRGE on expression of inflammatory mediators in the spinal cord of EAE rats
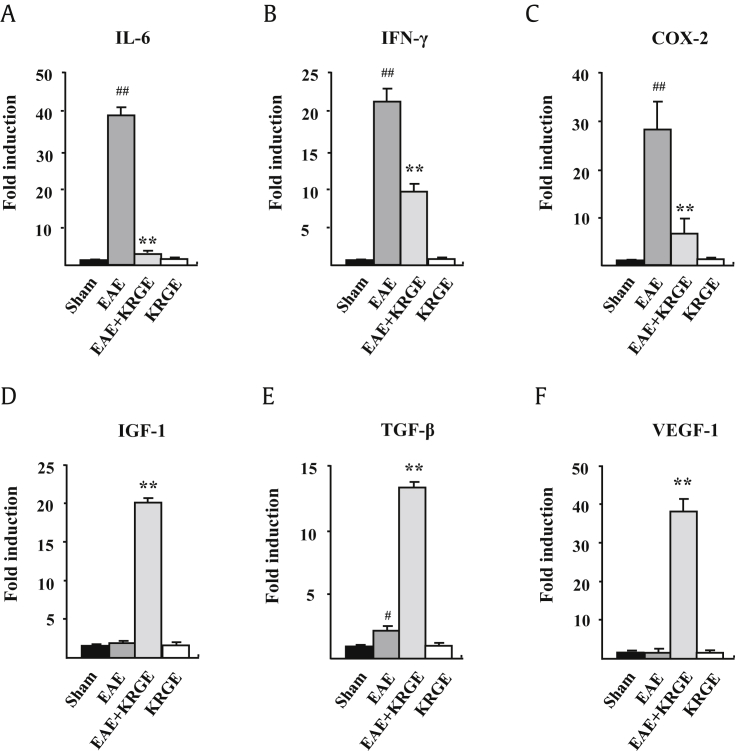
Activated and infiltrated immune cells may produce neurotoxic or neurotrophic mediators involved in the etiology of immunological and inflammatory diseases [34]. Therefore, we examined the effect of KRGE on mRNA expression levels of representative inflammatory mediators in spinal cords of EAE rats at 13–14 d after immunization. Real-time PCR results revealed that there was little or no mRNA expression changes of representative inflammatory cytokines (IL-6 and IFN-γ), COX-2, or growth factors (IGF-1, TGF-β, and VEGF-1) in the spinal cords between the sham and KRGE group (Fig. 3). However, the mRNA expression levels of IL-6, IFN-γ, and COX-2 were significantly increased in the spinal cord of rats in the EAE group compared to those in the sham or KRGE group. However, the mRNA expression levels of IL-6, IFN-γ, and COX-2 in the spinal cord of rats in the EAE group were significantly lower than those in the EAE + KRGE group (Figs. 3A–3C). In contrast, the mRNA expression levels of IGF-1 and VEGF-1, except TGF-β, were not significantly increased in the spinal cord of rats in the EAE group compared to those in the sham or KRGE group, although the expression levels of TGF-β1, VEGF, and IGF-1 were significantly increased in the EAE + KRGE group compared to those in the EAE group (Figs. 3D–3F). The results indicated that KRGE could suppress demyelination in spinal cords of EAE rats through inhibiting the expression of neurotoxic factors and upregulating the expression of neuroprotective factors.
Fig. 3.
KRGE regulates the mRNA levels of inflammatory mediators in the spinal cord of EAE rats. (A–F) Real-time polymerase chain reaction results for mRNA levels of IL-6 (A), IFN-γ (B), COX-2 (C), IGF-β1 (D), TGF-β (E), and VEGF-1 (F) the spinal cord of EAE rats. Analysis of variance test; #p < 0.01 versus sham group; *p < 0.01 versus EAE group. COX, cyclo-oxygenase; EAE, experimental autoimmune encephalomyelitis; IFN, interferon; IGF, insulin-like growth factor; IL, interleukin; KRGE, Korean Red Ginseng extract; TGF, transforming growth factor; VEGF, vascular endothelial growth factor.
3.4. Effect of KRGE on MAPKs and NF-κB signaling pathways in the spinal cords of EAE rats
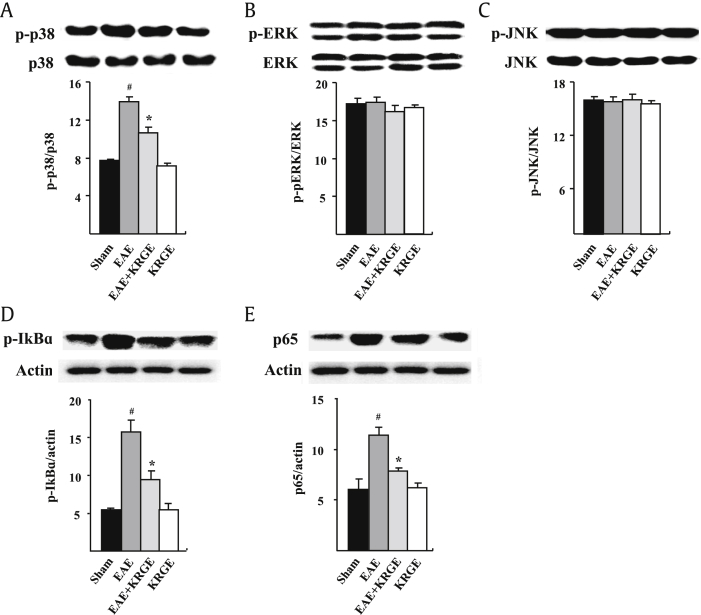
MAPKs and NF-κB signaling pathways are key mediators of inducible transcription in the immune system as upstream signaling pathways in inflammatory reactions [10], [35]. Therefore, we investigated the effect of KRGE on MAPKs and NF-κB signaling pathways in the spinal cords of EAE rats at 13–14 d after immunization. Western blot analysis revealed that the expression levels of p-p38 MAPK, p-IκBα, and NF-κB/p65 were significantly upregulated in the spinal cords of EAE rats compared to those in the sham or KRGE group. However, the protein levels of p-p38 MAPK, p-IκBα, and NF-κB/p65 in the spinal cords of rats in the EAE + KRGE group were significantly lower than those in the EAE group (Figs. 4A, 4D, 4E). However, the activation of JNK or ERK was not significantly affected by immunization or KRGE pretreatment (Figs. 4B, 4C). Our findings suggest that pretreatment of KRGE might reduce spinal demyelination by inhibiting the phosphorylation of p38 MAPK and NF-κB signaling pathways, but not JNK and ERK pathways.
Fig. 4.
KRGE inhibits activation of p38 MAPK and NF-κB signaling pathways in the spinal cords of EAE rats. Western blot analysis and quantitative results for the protein levels of p-p38 (A), p-ERK (B) and p-JNK (C), p-IκBα (D), and NF-κB/p65 (E) in the spinal cord of EAE rats. Analysis of variance test; #p < 0.01 versus sham group; *p < 0.01 versus EAE group. EAE, experimental autoimmune encephalomyelitis; ERK, extracellular signal-regulated kinase; JNK, c-Jun N-terminal kinase; KRGE, Korean Red Ginseng extract; MAPK, mitogen-activated protein kinase; NF-κB, nuclear factor-κB.
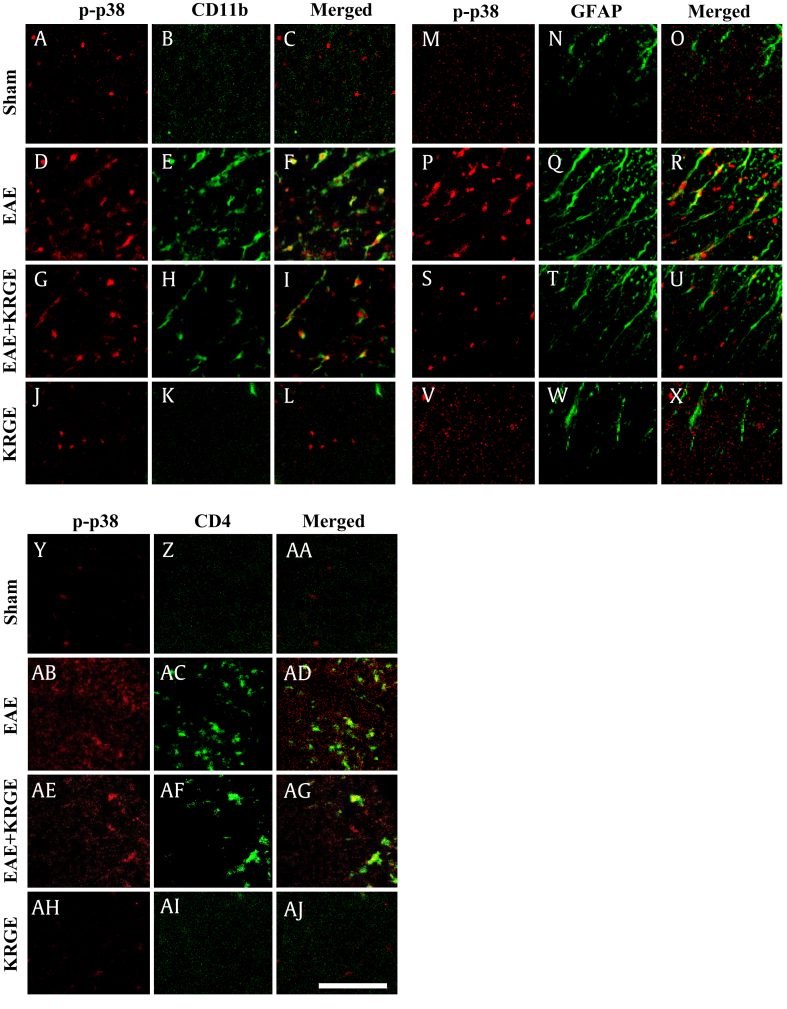
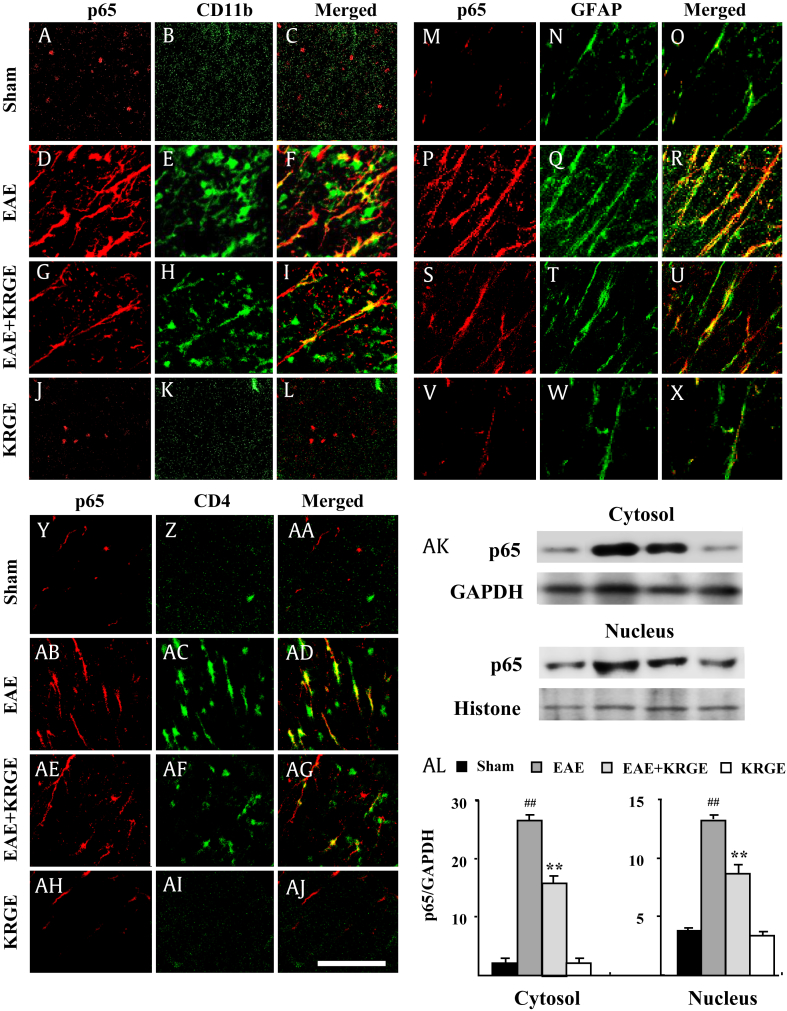
3.5. Effects of KRGE on distribution of p-38 MAPKs and NF-κB/p65 in spinal cords
The activation patterns of p38 MAPK and NF-κB are kaleidoscopically dependent on cell types during developmental stages of neurological disorders [10], [35]. Thus, we investigated whether the activation of p38 MAPK and NF-κB pathways was associated with a specific cell type in the spinal cords of EAE rats. As shown in Fig. 5, the expression level of p-p38 MAPK in nucleus-like structures of CD11b-immunoreactive cells in the spinal white matter of rats in the EAE group was higher compared to that in the sham or KRG group. However, the expression level of p-p38 MAPK in the EAE + KRGE group was lower than in the EAE group (Figs. 5A–5L). The expression of p-p38 MAPK was also observed in nucleus-like structures of GFAP-immunoreactive cells and CD4-immunoreactive cells T cells in the spinal cords of EAE rats. However, their intensities of immunofluorescent were lower than those in the EAE + KRGE group (Figs. 5M–5AJ). These alterations in the expression of p-p38 MAPK based on immunofluorescence staining were in agreement with the results on the expression of p-p38 MAPK protein by western blot analysis (Fig. 4A). The expression level of NF-κB/p65 was similar to that of p-p38 MAPK. That is, the expression of NF-κB/p65 was upregulated in CD11b-, GFAP-, and CD4-immunoreactive cells in the spinal white matter of rats in the EAE group compared to that in the sham group. However, it was markedly lower in the EAE + KRGE group than that in the EAE group (Fig. 6). Unlike nuclear expression of p-p38 MAPK, cellular distribution of NF-κB/p65 was unclear in cytosol and/or nucleus (Fig. 6). Therefore, the expression level of NF-κB/p65 was measured in isolated cytosol and nuclei. Alteration in the expression level of NF-κB/p65 was found both in the cytosol and nuclei (Figs. 5AK, 5AL). Because NeuN-immunofluorescent cells were not observed in the white mater of spinal cords of any of the groups, p-p38 MAPK or NF-κB/p65-immunoreactive cells were not merged with neurons (data not shown). Taken together, the activation of p38 MAPK and NF-κB pathways might be involved in the protective effect of KRGE against spinal demyelination via inhibiting increases of microglia/macrophages, astrocyte, and T cells in the spinal cords of EAE rats.
Fig. 5.
KRGE blocks the activation and distribution of p-p38 MAPK in the spinal cords of EAE rats. Spinal cord sections were subjected to double immunofluorescence staining to determine immunofluorescence intensities of p-p38 protein in CD11b- (A–L), GFAP- (M–X), and CD4-immunoreactive cells (Y–AJ) in the white matter of spinal cords of EAE rats. Bar, 100 μm. EAE, experimental autoimmune encephalomyelitis; GFAP, glial fibrillary acidic protein; KRGE, Korean Red Ginseng extract; MAPK, mitogen-activated protein kinase.
Fig. 6.
KRGE blocks activation and distribution of NF-κB/p65 in the spinal cords of EAE rats. (A–AJ) Spinal cord sections were subjected to double immunofluorescence staining to determine immunofluorescence intensities of NF-κB/p65 protein in CD11b- (A–L), GFAP- (M–X), and CD4-immunoreactive cells (Y–AJ) in the white matter of the spinal cord of EAE rats. Bar, 100 μm. (AK and AL) Western blot analysis (AK) and quantified results (AL) for protein levels of NF-κB/p65 in the cytosol and nucleus obtained from the spinal cord of EAE rats. Analysis of variance test; ##p < 0.05 versus sham group; **p < 0.05 versus EAE group. EAE, experimental autoimmune encephalomyelitis; GAPDH, glyceraldehyde 3-phosphate dehydrogenase; GFAP, glial fibrillary acidic protein; KRGE, Korean Red Ginseng extract; NF-κB, nuclear factor-κB.
4. Discussion
MS is an autoimmune and inflammatory demyelinating disease of the CNS. The cause of MS remains unknown. It is widely regarded that pathogenic Th cells and aberrant expression of cytokines are vital to its pathogenesis [36]. The results of the present study demonstrated that KRGE pretreatment could alleviate demyelination by reducing inflammatory cells infiltration, diminishing the expression levels of proinflammatory mediators (IL-6, IFN-γ, and COX-2), enhancing the expression levels of growth factors (IGF-1, TGFβ, and VEGF-1), and decreasing the activation of the p38 MAPK/NF-κB signaling pathway in the spinal cords of EAE rats. Our findings indicate that KRGE pretreatment can be used to protect against spinal demyelination induced by EAE. Such protective effect of KRGE might be associated with downregulation of the p38 MAPK/NF-κB signaling pathway.
In demyelinated lesions of MS patients and EAE animal models, activated and infiltrated immune cells (microglia, macrophages, T cells, etc.) may produce mediators beneficial to normal structures but detrimental to degenerative structures [36], [37]. Thus, regulating the activation and migration of these immune cells might be an attractive therapeutic approach for MS patients and EAE animal models [36], [37]. For instance, Minocycline, a broad-spectrum tetracycline antibiotic, may delay the onset and progression of disease and prevents inflammation and demyelination in relapsing–remitting EAE by inhibiting microglial activation and expression of proinflammatory cytokines/chemokines [38]. Total ginseng extract, KRGE, or ginsenosides such as Rb1, Rg1, Rh3, and Re may exert neuroprotective effect in neurological disorders including Alzheimer's disease and Parkinson's disease through inhibiting the migration/infiltration of immune cells and the expression of proinflammatory cytokines/chemokines [15]. Our previous study has demonstrated that KRGE can prevent the development of Huntington's disease-like symptoms and striatal cell death in 3-nitropropionic acid (NPA)-induced striatal toxic mouse model by attenuating the activation and infiltration of microglia and reducing the mRNA levels of tumor necrosis factor-α, IL-1β, IL-6, and iNOS [24]. These results suggest that KRGE might be able to inhibit the activation/infiltration of immune cells (microglia, T cells, macrophages, etc) and regulate the production of inflammatory mediators around/within demyelinating lesion in EAE through other mechanisms.
Recently, we have demonstrated that KRGE can alleviate EAE by suppressing Th1 and Th17 cells and upregulating regulatory T cells [22]. In acute EAE rats, pretreatment with KRGE significantly reduced the population of CD4+/IFN-γ+, and CD4+/IL-17+ T cells in the spinal cord, corresponding to downregulated mRNA expression of IFN-γ, IL-17, and IL-23 in the spinal cord [22]. In contrast, KRGE pretreatment increased the population of CD4+/Foxp3+ T cells in the spinal cord of these rats, corresponding to upregulated mRNA expression of Foxp3 in the spinal cord [22]. Nevertheless, the critical role of KRGE in demyelination and its associated immune cells and immune mediators remain unclear. In the present study, KRGE pretreatment inhibited the activation/infiltration of Iba-1-immunoreactive cells (microglia and macrophages), decreased mRNA expression of IL-6, IFN-γ, and COX-2, and increased the mRNA expression levels of growth factors (IGF-1, TGF-β, and VEGF-1), and reduced demyelination in the spinal cords of EAE rats. The decrease in expression of IL-6, IFN-γ, and COX-2 is in accordance with results of previous reports [26], [39]. IGF-1, TGF-β, and VEGF-1 are growth factors known to be expressed in most neurodegenerative diseases [40], [41], [42]. However, they are not widely studied in MS or EAE. IGF-1 can reduce immune cell responses in acute nondemyelinative EAE [40]. It also stimulates Treg cells and suppresses EAE [41]. TGF-β is a potent regulatory cytokine with diverse effects on hemopoietic cells. Defects in TGF-β expression and its signaling in T cells are correlated with the onset of EAE [43]. VEGF-1 is involved in the recruitment of monocytic macrophages and glial reactions during EAE [42]. Ginsenosides (Rg5, Rd, and Rb1) can regulate the expression of IGF-1 in streptozotocin-induced memory impaired rats [44] and the expression of TGF-β in liver fibrosis around hepatic stellate cells [45]. These reports support that KRGE has protective effects on an experimental model of MS through regulating the activities of IGF-1, TGF-β, and VEGF-1. However, the detail mechanisms remain to be further elucidated.
MAPKs (p38, JNK, and ERK 1/2) and NF-κB signaling pathways are involved in the activation of immune system during inflammatory neurodegeneration. Specifically, the activation of p38 MAPK in CD4+ T cells controls IL-17 production and induces the development and progression of both chronic and relapsing–remitting forms of EAE [7], [10], [35]. In addition, regulation of p38 MAPK activity specifically in T cells is sufficient to modulate EAE severity [35]. KRGE can attenuate neuronal death corresponding to reduction of microglial activation by inhibiting phosphorylation of p38 MAPK pathway in 3-NPA-induced striatal toxicity model [24]. Interestingly, intrathecal administration of SB203580 (a p38 inhibitor) has increased the survival rate in a 3-NPA-induced Huntington's disease model [24]. These results suggest that activation of p38 MAPK is critical to immune cell function during the development and progression of neuronal damage. However, the function and distribution of p38 MAPK depending on cell types in neurodegenerative disorders such as demyelination are not well known. In the present study, the expression of p-p38 MAPK was increased in the spinal cords (specifically in microglia, astrocytes, and T cells of white matter of spinal cords) at the peak of behavioral impairment (13–14 d after immunization) in EAE rats, whereas KRGE pretreatment inhibited the increase of its expression, corresponding to reduced demyelination. In agreement with the findings of this study, pretreatment with bee venom acupuncture at Zusanli (ST36) acupoints has been reported to suppress activation of the p38 MAPK pathway in the spinal cord of acute EAE rats [25]. In one study, p-p38 immunoreactivity was observed in macrophages, astrocytes, and T cells in spinal lesions during peak stage of EAE [46]. Inhibiting p38-MAPK activation can reduce chemokine CC ligand (CCL)2/CCL5-induced T-cell migration in EAE, coinciding with reduced CNS inflammation and demyelination [47]. A significant increase in the number of p-p38 immunoreactive cells has been predominantly found in the microglia of ipsilateral L4–5 spinal dorsal horn after incision, while intrathecal pretreatment of FR167653 (a specific p38 inhibitor) can attenuate the incision-induced mechanical allodynia [48]. Collectively, these findings suggest that KRGE can regulate the activation of p38 MAPK and offer protection against demyelination.
The expression levels of p-ERK and p-JNK are reported to be significantly increased in the spinal cords (astrocyte, T cells, and macrophages) of rats with EAE at peak stage compared to those in the controls. However, their expression levels are decreased slightly in the recovery stage of acute EAE [46]. Microglial chemotaxis is mediated by chemokine CXC receptor 7 through ERK1/2 activation during EAE [49]. Chemokine CXC receptor 7 neutralizing treatment can ameliorate the clinical severity of EAE with reduced ERK1/2 phosphorylation, but not JNK and p38 MAPKs [49]. Triterpenes inhibit ERK phosphorylation and reduce the proliferative response, phagocytic properties, and synthesis of proinflammatory mediators induced by the addition of inflammatory stimuli to microglia [50]. Treatment with an ERK inhibitor attenuates acute EAE, associated with significant suppression of autoantigen-specific Th17 and Th1 responses [51]. Overexpression of Sprouty4 or pharmacological inhibition of ERK upregulates IL-1 receptor 1 expression in primary T cells [52]. In the present study, phosphorylation levels of ERK and JNK were not significantly changed by immunization or KRGE pretreatment (Fig. 4). Because the differential expression of three MAPKs was discerned in an animal model of neurological diseases including MS, the exact function of MAPKs in immune cells during neural inflammation remains unclear. Taken together, these results suggest that KRGE can regulate inflammatory neurodegeneration through activation of p38 MAPK, and not p-ERK or p-JNK MAPKs, during CNS autoimmunity. The functional role of MAPKs including ERK, JNK, and p38 in microglia/macrophages, astrocytes, and T cells needs further study in EAE model of human autoimmune diseases.
As a downstream cascade of p38 MAPK in inflammation, the NF-κB signaling pathway is essentially involved in the pathogenicity of autoimmune diseases such as MS [10]. Microarray analysis of genes of MS brain tissue has revealed a positive correlation between MS and NF-κB [8], [9]. It has been reported that mice lacking NF-κB are significantly protected from EAE [10]. The activation of RelA (p65) of NF-κB and IκB dissociation has a distinct role in EAE progression by altering IκB phosphorylation and/or degradation [53]. In the present study, KRGE pretreatment blocked the activation of NF-κB and IκBα in the spinal cord of rats with EAE (Fig. 6). Additionally, NF-κB expression level was increased in microglia, astrocytes, or T cells of EAE spinal cord (white matter) by immunofluorescence staining. However, its expression level was decreased by KRGE pretreatment (Fig. 6). These results are consistent with previous reports [54] showing that NF-κB immunoreactivity is primarily detected in the cytoplasm (inactive form of NF-κB) of neurons and glial cells in the white matter of sham animals. However, immunoreactivity of NF-κB is mainly observed in the nucleus (active form of NF-κB) of neurons in the gray matter and presumptive glial cells in the white matter after spinal cord injury [54]. Taken together, these findings indicate that KRGE pretreatment might be able to diminish the development and progression of EAE by blocking the activation of the NF-κB signaling pathway in the spinal cord, although the details of the distribution and mechanism of NF-κB signal pathway need further studies.
5. Conclusions
The present study and our previous study [22] show that KRGE pretreatment can alleviate behavioral severity or demyelination in EAE rats through regulating the migration and infiltration of immune cells such as resting microglia, macrophages, and T cells associated with reduced activation of the p38 MAPK and NF-κB pathways. Given the known functions of KRGE in neural function and immune activity, regulating the function and distribution of p38 MAPK and NF-κB pathways might be essential to the effect of KRGE in preventing demyelination in MS and EAE.
Acknowledgments
This research was supported by a grant from the Korean Society of Ginseng and the Korea Ginseng Cooperation (2013–2014) and by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology, Republic of Korea (NRF-2014R1A2A1A11051240). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of interest
None of the authors of this manuscript have any conflict of interest to declare.
References
- 1.Dendrou C.A., Fugger L., Friese M.A. Immunopathology of multiple sclerosis. Nat Rev. 2015;15:545–558. doi: 10.1038/nri3871. [DOI] [PubMed] [Google Scholar]
- 2.Hoglund R.A., Maghazachi A.A. Multiple sclerosis and the role of immune cells. World J Exp Med. 2014;4:27–37. doi: 10.5493/wjem.v4.i3.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Volpe E., Battistini L., Borsellino G. Advances in T helper 17 cell biology: pathogenic role and potential therapy in multiple sclerosis. Mediators Inflamm. 2015;2015:475158. doi: 10.1155/2015/475158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pearson G., Robinson F., Beers Gibson T., Xu B.E., Karandikar M., Berman K., Cobb M.H. Mitogen-activated protein (MAP) kinase pathways: regulation and physiological functions. Endocrine Rev. 2001;22:153–183. doi: 10.1210/edrv.22.2.0428. [DOI] [PubMed] [Google Scholar]
- 5.Krementsov D.N., Noubade R., Dragon J.A., Otsu K., Rincon M., Teuscher C. Sex-specific control of central nervous system autoimmunity by p38 mitogen-activated protein kinase signaling in myeloid cells. Ann Neurol. 2014;75:50–66. doi: 10.1002/ana.24020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karunakaran S., Ravindranath V. Activation of p38 MAPK in the substantia nigra leads to nuclear translocation of NF-kappaB in MPTP-treated mice: implication in Parkinson's disease. J Neurochem. 2009;109:1791–1799. doi: 10.1111/j.1471-4159.2009.06112.x. [DOI] [PubMed] [Google Scholar]
- 7.Mc Guire C., Prinz M., Beyaert R., van Loo G. Nuclear factor kappa B (NF-kappaB) in multiple sclerosis pathology. Trends Mol Med. 2013;19:604–613. doi: 10.1016/j.molmed.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 8.Lock C., Hermans G., Pedotti R., Brendolan A., Schadt E., Garren H., Langer-Gould A., Strober S., Cannella B., Allard J. Gene-microarray analysis of multiple sclerosis lesions yields new targets validated in autoimmune encephalomyelitis. Nat Med. 2002;8:500–508. doi: 10.1038/nm0502-500. [DOI] [PubMed] [Google Scholar]
- 9.Mycko M.P., Papoian R., Boschert U., Raine C.S., Selmaj K.W. cDNA microarray analysis in multiple sclerosis lesions: detection of genes associated with disease activity. Brain. 2003;126:1048–1057. doi: 10.1093/brain/awg107. [DOI] [PubMed] [Google Scholar]
- 10.Hilliard B., Samoilova E.B., Liu T.S., Rostami A., Chen Y. Experimental autoimmune encephalomyelitis in NF-kappa B-deficient mice:roles of NF-kappa B in the activation and differentiation of autoreactive T cells. J Immunol. 1999;163:2937–2943. [PubMed] [Google Scholar]
- 11.Levin M.C., Jackson W.C. Developing a therapeutic plan for treating MS: evidence for new treatments. J Clin Psychiatry. 2014;75:e34. doi: 10.4088/JCP.12100nr8c. [DOI] [PubMed] [Google Scholar]
- 12.Thompson A.J., Toosy A.T., Ciccarelli O. Pharmacological management of symptoms in multiple sclerosis: current approaches and future directions. Lancet. 2010;9:1182–1199. doi: 10.1016/S1474-4422(10)70249-0. [DOI] [PubMed] [Google Scholar]
- 13.Jeffery D.R. Recent advances in treating multiple sclerosis: efficacy, risks and place in therapy. Ther Adv Chron Dis. 2013;4:45–51. doi: 10.1177/2040622312466279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu S., Yi L.Z., Liang Y.Z. Traditional Chinese medicine and separation science. J Separation Sci. 2008;31:2113–2137. doi: 10.1002/jssc.200800134. [DOI] [PubMed] [Google Scholar]
- 15.Cho I. Effects of Panax ginseng in neurodegenerative diseases. J Ginseng Res. 2012;36:342–353. doi: 10.5142/jgr.2012.36.4.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee S.M., Bae B.S., Park H.W., Ahn N.G., Cho B.G., Cho Y.L., Kwak Y.S. Characterization of Korean Red Ginseng (Panax ginseng Meyer): history, preparation method, and chemical composition. J Ginseng Res. 2015;39:384–391. doi: 10.1016/j.jgr.2015.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saba E., Jeon B.R., Jeong D.H., Lee K., Goo Y.K., Kwak D., Kim S., Roh S.S., Kim S.D., Nah S.Y. A novel Korean Red Ginseng compound gintonin inhibited inflammation by MAPK and NF-kappaB pathways and recovered the levels of mir-34a and mir-93 in RAW 264.7 cells. Evid Based Complement Alternat Med. 2015;2015:624132. doi: 10.1155/2015/624132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim H.J., Kim P., Shin C.Y. A comprehensive review of the therapeutic and pharmacological effects of ginseng and ginsenosides in central nervous system. J Ginseng Res. 2013;37:8–29. doi: 10.5142/jgr.2013.37.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bowie L.E., Roscoe W.A., Lui E.M., Smith R., Karlik S.J. Effects of an aqueous extract of North American ginseng on MOG (35-55)-induced EAE in mice. Can J Physiol Pharmacol. 2012;90:933–939. doi: 10.1139/y2012-092. [DOI] [PubMed] [Google Scholar]
- 20.Hwang I., Ahn G., Park E., Ha D., Song J.Y., Jee Y. An acidic polysaccharide of Panax ginseng ameliorates experimental autoimmune encephalomyelitis and induces regulatory T cells. Immunol Lett. 2011;138:169–178. doi: 10.1016/j.imlet.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 21.Zhu D., Liu M., Yang Y., Ma L., Jiang Y., Zhou L., Huang Q., Pi R., Chen X. Ginsenoside Rd ameliorates experimental autoimmune encephalomyelitis in C57BL/6 mice. J Neurosci Res. 2014;92:1217–1226. doi: 10.1002/jnr.23397. [DOI] [PubMed] [Google Scholar]
- 22.Lee M.J., Jang M., Choi J., Chang B.S., Kim D.Y., Kim S.H., Kwak Y.S., Oh S., Lee J.H., Chang B.J. Korean Red Ginseng and ginsenoside-Rb1/-Rg1 alleviate experimental autoimmune encephalomyelitis by suppressing Th1 and Th17 cells and upregulating regulatory T cells. Mol Neurobiol. 2016;53:1977–2002. doi: 10.1007/s12035-015-9131-4. [DOI] [PubMed] [Google Scholar]
- 23.Landis S.C., Amara S.G., Asadullah K., Austin C.P., Blumenstein R., Bradley E.W., Crystal R.G., Darnell R.B., Ferrante R.J., Fillit H. A call for transparent reporting to optimize the predictive value of preclinical research. Nature. 2012;490:187–191. doi: 10.1038/nature11556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jang M., Lee M.J., Kim C.S., Cho I.H. Korean Red Ginseng extract attenuates 3-nitropropionic acid-induced Huntington’s-like symptoms. Evid Based Complement Alternat Med. 2013;2013:237207. doi: 10.1155/2013/237207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee M.J., Jang M., Choi J., Lee G., Min H.J., Chung W.S., Kim J.I., Jee Y., Chae Y., Kim S.H. Bee venom acupuncture alleviates experimental autoimmune encephalomyelitis by upregulating regulatory T cells and suppressing Th1 and Th17 responses. Mol Neurobiol. 2016;53:1419–1445. doi: 10.1007/s12035-014-9012-2. [DOI] [PubMed] [Google Scholar]
- 26.Lee M.J., Bing S.J., Choi J., Jang M., Lee G., Lee H., Chang B.S., Jee Y., Lee S.J., Cho I.H. IKKbeta-mediated inflammatory myeloid cell activation exacerbates experimental autoimmune encephalomyelitis by potentiating Th1/Th17 cell activation and compromising blood brain barrier. Mol Neurodegen. 2016;11:54. doi: 10.1186/s13024-016-0116-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Piao Z.G., Cho I.H., Park C.K., Hong J.P., Choi S.Y., Lee S.J., Lee S., Park K., Kim J.S., Oh S.B. Activation of glia and microglial p38 MAPK in medullary dorsal horn contributes to tactile hypersensitivity following trigeminal sensory nerve injury. Pain. 2006;121:219–231. doi: 10.1016/j.pain.2005.12.023. [DOI] [PubMed] [Google Scholar]
- 28.Dignam J.D., Lebovitz R.M., Roeder R.G. Accurate transcription initiation by RNA polymerase II in a soluble extract from isolated mammalian nuclei. Nuc Acid Res. 1983;11:1475–1489. doi: 10.1093/nar/11.5.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cho I.H., Hong J., Suh E.C., Kim J.H., Lee H., Lee J.E., Lee S., Kim C.H., Kim D.W., Jo E.K. Role of microglial IKKbeta in kainic acid-induced hippocampal neuronal cell death. Brain. 2008;131:3019–3033. doi: 10.1093/brain/awn230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lopes Pinheiro M.A., Kooij G., Mizee M.R., Kamermans A., Enzmann G., Lyck R., Schwaninger M., Engelhardt B., de Vries H.E. Immune cell trafficking across the barriers of the central nervous system in multiple sclerosis and stroke. Biochim Biophys Acta. 2016;1862:461–471. doi: 10.1016/j.bbadis.2015.10.018. [DOI] [PubMed] [Google Scholar]
- 31.Kipp M., van der Valk P., Amor S. Pathology of multiple sclerosis. CNS Neurol Disord Drug Target. 2012;11:506–517. doi: 10.2174/187152712801661248. [DOI] [PubMed] [Google Scholar]
- 32.Jang M., Lee M.J., Cho I.H. Ethyl pyruvate ameliorates 3-nitropropionic acid-induced striatal toxicity through anti-neuronal cell death and anti-inflammatory mechanisms. Brain Behav Immun. 2014;38:151–165. doi: 10.1016/j.bbi.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 33.Jang M., Cho I.H. Sulforaphane ameliorates 3-nitropropionic acid-induced striatal toxicity by activating the Keap1-Nrf2-ARE pathway and inhibiting the MAPKs and NF-kappaB pathways. Mol Neurobiol. 2016;53:2619–2635. doi: 10.1007/s12035-015-9230-2. [DOI] [PubMed] [Google Scholar]
- 34.Kennedy K.J., Strieter R.M., Kunkel S.L., Lukacs N.W., Karpus W.J. Acute and relapsing experimental autoimmune encephalomyelitis are regulated by differential expression of the CC chemokines macrophage inflammatory protein-1alpha and monocyte chemotactic protein-1. J Neuroimmunol. 1998;92:98–108. doi: 10.1016/s0165-5728(98)00187-8. [DOI] [PubMed] [Google Scholar]
- 35.Noubade R., Krementsov D.N., Del Rio R., Thornton T., Nagaleekar V., Saligrama N., Spitzack A., Spach K., Sabio G., Davis R.J. Activation of p38 MAPK in CD4 T cells controls IL-17 production and autoimmune encephalomyelitis. Blood. 2011;118:3290–3300. doi: 10.1182/blood-2011-02-336552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lassmann H., van Horssen J. The molecular basis of neurodegeneration in multiple sclerosis. FEBS Lett. 2011;585:3715–3723. doi: 10.1016/j.febslet.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 37.Lobsiger C.S., Cleveland D.W. Glial cells as intrinsic components of non-cell-autonomous neurodegenerative disease. Nat Neurosci. 2007;10:1355–1360. doi: 10.1038/nn1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen X., Ma X., Jiang Y., Pi R., Liu Y., Ma L. The prospects of minocycline in multiple sclerosis. J Neuroimmunol. 2011;235:1–8. doi: 10.1016/j.jneuroim.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 39.Choi J.H., Lee M.J., Jang M., Kim E.J., Shim I., Kim H.J., Lee S., Lee S.W., Kim Y.O., Cho I.H. An oriental medicine, Hyungbangpaedok-San attenuates motor paralysis in an experimental model of multiple sclerosis by regulating the T cell response. PLoS One. 2015;10:e0138592. doi: 10.1371/journal.pone.0138592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu X., Linnington C., Webster H.D., Lassmann S., Yao D.L., Hudson L.D., Wekerle H., Kreutzberg G.W. Insulin-like growth factor-I treatment reduces immune cell responses in acute non-demyelinative experimental autoimmune encephalomyelitis. J Neurosci Res. 1997;47:531–538. doi: 10.1002/(sici)1097-4547(19970301)47:5<531::aid-jnr8>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 41.Bilbao D., Luciani L., Johannesson B., Piszczek A., Rosenthal N. Insulin-like growth factor-1 stimulates regulatory T cells and suppresses autoimmune disease. EMBO Mol Med. 2014;6:1423–1435. doi: 10.15252/emmm.201303376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Park J.M., Shin Y.J., Cho J.M., Choi J.Y., Jeun S.S., Cha J.H., Lee M.Y. Upregulation of vascular endothelial growth factor receptor-3 in the spinal cord of Lewis rats with experimental autoimmune encephalomyelitis. J Histochem Cytochem. 2013;61:31–44. doi: 10.1369/0022155412462975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mirshafiey A., Mohsenzadegan M. TGF-beta as a promising option in the treatment of multiple sclerosis. Neuropharmacology. 2009;56:929–936. doi: 10.1016/j.neuropharm.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 44.Chu S., Gu J., Feng L., Liu J., Zhang M., Jia X., Liu M., Yao D. Ginsenoside Rg5 improves cognitive dysfunction and beta-amyloid deposition in STZ-induced memory impaired rats via attenuating neuroinflammatory responses. Int Immunopharmacol. 2014;19:317–326. doi: 10.1016/j.intimp.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 45.Lo Y.T., Tsai Y.H., Wu S.J., Chen J.R., Chao J.C. Ginsenoside Rb1 inhibits cell activation and liver fibrosis in rat hepatic stellate cells. J Medicinal Food. 2011;14:1135–1143. doi: 10.1089/jmf.2010.1485. [DOI] [PubMed] [Google Scholar]
- 46.Shin T., Ahn M., Jung K., Heo S., Kim D., Jee Y., Lim Y.K., Yeo E.J. Activation of mitogen-activated protein kinases in experimental autoimmune encephalomyelitis. J Neuroimmunol. 2003;140:118–125. doi: 10.1016/s0165-5728(03)00174-7. [DOI] [PubMed] [Google Scholar]
- 47.Cheng W., Zhao Q., Xi Y., Li C., Xu Y., Wang L., Niu X., Wang Z., Chen G. IFN-beta inhibits T cells accumulation in the central nervous system by reducing the expression and activity of chemokines in experimental autoimmune encephalomyelitis. Mol Immunol. 2015;64:152–162. doi: 10.1016/j.molimm.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 48.Wen Y.R., Suter M.R., Ji R.R., Yeh G.C., Wu Y.S., Wang K.C., Kohno T., Sun W.Z., Wang C.C. Activation of p38 mitogen-activated protein kinase in spinal microglia contributes to incision-induced mechanical allodynia. Anesthesiology. 2009;110:155–165. doi: 10.1097/ALN.0b013e318190bc16. [DOI] [PubMed] [Google Scholar]
- 49.Bao J., Zhu J., Luo S., Cheng Y., Zhou S. CXCR7 suppression modulates microglial chemotaxis to ameliorate experimentally-induced autoimmune encephalomyelitis. Biochem Biophys Res Comm. 2016;469:1–7. doi: 10.1016/j.bbrc.2015.11.059. [DOI] [PubMed] [Google Scholar]
- 50.Martin R., Hernandez M., Cordova C., Nieto M.L. Natural triterpenes modulate immune-inflammatory markers of experimental autoimmune encephalomyelitis: therapeutic implications for multiple sclerosis. Br J Pharmacol. 2012;166:1708–1723. doi: 10.1111/j.1476-5381.2012.01869.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brereton C.F., Sutton C.E., Lalor S.J., Lavelle E.C., Mills K.H. Inhibition of ERK MAPK suppresses IL-23- and IL-1-driven IL-17 production and attenuates autoimmune disease. J Immunol. 2009;183:1715–1723. doi: 10.4049/jimmunol.0803851. [DOI] [PubMed] [Google Scholar]
- 52.Fukaya T., Someya K., Hibino S., Okada M., Yamane H., Taniguchi K., Yoshimura A. Loss of Sprouty4 in T cells ameliorates experimental autoimmune encephalomyelitis in mice by negatively regulating IL-1beta receptor expression. Biochem Biophys Res Comm. 2014;447:471–478. doi: 10.1016/j.bbrc.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 53.Hwang I., Ha D., Ahn G., Park E., Joo H., Jee Y. Experimental autoimmune encephalomyelitis: association with mutual regulation of RelA (p65)/NF-kappaB and phospho-IkappaB in the CNS. Biochem Biophys Res Comm. 2011;411:464–470. doi: 10.1016/j.bbrc.2011.06.195. [DOI] [PubMed] [Google Scholar]
- 54.Yune T.Y., Lee S.M., Kim S.J., Park H.K., Oh Y.J., Kim Y.C., Markelonis G.J., Oh T.H. Manganese superoxide dismutase induced by TNF-beta is regulated transcriptionally by NF-kappaB after spinal cord injury in rats. J Neurotrauma. 2004;21:1778–1794. doi: 10.1089/neu.2004.21.1778. [DOI] [PubMed] [Google Scholar]