Abstract
Study Objectives
Neighborhood disadvantage has been linked to poor sleep. However, the extant research has primarily focused on self-reported assessments of sleep and neighborhood characteristics. The current study examines the association between objective and perceived neighborhood characteristics and actigraphy-assessed sleep duration, efficiency, and wakefulness after sleep onset (WASO) in an urban sample of African American adults.
Methods
We examined data from predominantly African American adults (n = 788, mean age 55 years; 77% female) living in two low-income neighborhoods. Perceived neighborhood characteristics included safety, social cohesion, and satisfaction with one’s neighborhood as a place to live. Objective neighborhood conditions included walkability, disorder, street lighting, and crime levels. Sleep duration, efficiency, and WASO were measured via 7 days of wrist-worn actigraphy. Analyses estimated each of the sleep outcomes as a function of perceived and objective neighborhood characteristics. Individual-level sociodemographics, body mass index, and psychological distress were included as covariates.
Results
Greater perceived safety was associated with higher sleep efficiency and shorter WASO. Higher levels of crime were associated with poorer sleep efficiency and longer WASO, but these associations were only evident in one of the neighborhoods. Several interactions emerged suggesting that the association between neighborhood characteristics and sleep outcomes differed by neighborhood.
Conclusions
Both how residents perceive their neighborhood safety and their exposure to objectively measured crime have implications for sleep continuity. These findings suggest that neighborhood conditions may contribute to disparities in sleep health.
Keywords: actigraphy, neighborhood disadvantage, disparities, sleep, socioeconomic status, crime
Statement of Significance.
Living in a socioeconomically disadvantaged neighborhood may contribute to pervasive disparities in sleep and other morbidities. This study is among the first to examine objective and perceived assessments of neighborhood conditions in relation to objectively measured sleep in a high-risk sample of predominantly low-income, African American residents. Higher crime and lower perceived safety were associated with poorer sleep efficiency and longer WASO. Disturbed sleep may be an important pathway linking neighborhood characteristics and adverse health outcomes.
Introduction
Neighborhood characteristics are increasingly recognized as important risk factors for a host of physical and mental health morbidities [1, 2]. Residing in neighborhoods with higher levels of adverse characteristics such as crime and disorder or lower levels of socioeconomic status, social cohesion, walkability, and/or access to healthy foods has been associated with cardiometabolic risk factors including higher body mass index (BMI) [3, 4], diabetes [5], and hypertension [6, 7]. However, the mechanisms underlying these associations are not fully understood.
A parallel line of research has identified short, disrupted, irregular, and/or poor quality sleep as important risk factors for numerous health conditions, including obesity, cardiometabolic dysregulation, physical limitations, poorer immune functioning, and poor self-reported health [8–11]. Thus, sleep represents an important potential mechanism through which neighborhood environments may influence physical and mental health [12–15].
An emergent area of research has examined associations between the conditions of one’s neighborhood of residence and either sleep quality or duration [13, 16–19]. In general, disadvantaged neighborhood conditions (e.g. higher levels of crime and/or noise; lower levels of social cohesion, and/or walkability) are associated with shorter sleep duration and poorer sleep quality [12–14, 20–23]. Importantly, most prior work in this area has focused exclusively on perceived indicators of neighborhood conditions. Perceptions of neighborhood conditions are important indicators of an individual’s stress appraisal related to their neighborhood environments [24], and some studies suggest that perceived neighborhood conditions are even more strongly associated with health outcomes than observed characteristics [25–27]. Despite these important contributions, such reports are subject to a number of reporting biases, which is particularly problematic for studies that also rely on the subjective reporting of sleep; an individual’s tendency toward positive or negative valence could influence perceptions of both sleep and their neighborhood environment [28]. In fact, most prior studies of neighborhood-sleep associations have also relied on subjective, self-reported assessments of sleep [12, 14, 18]. Of the few studies that have included objective measures of sleep, via wrist-worn actigraphy methods, the findings have been somewhat mixed depending on the sleep outcome, perhaps due to differences in the age of the sample as well as the methodology to assess sleep and neighborhood conditions [16, 19]. For example, in one study of children in Alabama, higher levels of neighborhood economic deprivation were associated with shorter sleep duration and poorer sleep efficiency [16]. In a study of older adults from the Multi-Ethnic Study of Atherosclerosis (MESA) study, higher levels of social cohesion and safety were associated with longer sleep duration and earlier sleep midpoint, whereas neighborhood social factors were not associated with indicators of sleep continuity, including sleep efficiency or sleep fragmentation [19]. In the Sueño ancillary study of the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), lower levels of perceived safety were associated with greater risk of sleeping less than 6 hr per night (based on actigraphy), after covariate adjustment [29].
Finally, relatively little research has focused on neighborhood-sleep associations within low-income African American populations. Such research is important for two major reasons. First, African Americans face relatively greater risk for sleep problems, including short sleep duration, more fragmented sleep, and worse sleep quality, relative to non-Hispanic Whites [30–34]. Second, African Americans are disproportionately likely to live in disadvantaged neighborhoods compared with non-Hispanic Whites [35]. Furthermore, some evidence suggests that sleep-health associations consistently identified among non-Hispanic Whites (e.g. associations of sleep duration and BMI) [36] may be less consistent in African Americans [37].
The current analyses make several unique contributions to the existing literature: (1) examining associations of multiple perceived and objective indicators of neighborhood characteristics; (2) analyzing associations of these characteristics with actigraphy-assessed sleep duration, as well as two important indicators of sleep continuity, sleep efficiency, and wakefulness after sleep onset (WASO); and (3) exploring these associations in a sample of low-income African Americans in two comparable urban neighborhoods.
We hypothesized that lower levels of perceived neighborhood social cohesion, safety, and satisfaction, as well as more negative objectively measured neighborhood characteristics (i.e. higher crime rates, greater neighborhood disorder, and increased exposure to street lighting) would be associated with poorer sleep efficiency, longer WASO, and shorter sleep duration, after adjustment for other known risk factors for sleep disturbances, including individual-level SES, psychological distress, and BMI.
Methods
Study population and participants
The PHRESH Sleep study (PHRESHZzz) is part of a set of studies that build upon the original study of Pittsburgh Hill/Homewood Eating, Shopping, and Health (PHRESH), which recruited a random sample of households in two low-income, predominantly African American neighborhoods in Pittsburgh, Pennsylvania. One neighborhood (the Hill District) has and continues to undergo substantially more neighborhood economic revitalization, including housing and greenspace improvements and renovation, compared with the other neighborhood (Homewood). PHRESHZzz is designed to investigate how changes in the neighborhood environment may influence sleep and other health behaviors. This study uses baseline data collected in Spring 2013, which was collected prior to major greenspace and housing renovations. Data collection included neighborhood-level built and social characteristics, and detailed individual-level data, collected during an in-home interview. All study protocols were approved by RAND’s Institutional Review Board.
Actigraphy-based sleep outcomes
We used the Actigraph GT3x+, which has been validated to measure sleep/wake rhythms relative to both polysomnography and Actiwatch [38–41]. Participants were asked to wear the accelerometer on their wrist continuously for 7 consecutive days. Based on prior research suggesting the minimum number of nights required to establish reliable sleep-wake patterns via actigraphy, participants with <4 nights of data were excluded from the analyses (N = 210). The average number of nights of actigraphy for the analytic sample was 5.96, SD = 0.52, range = 4.00−7.00. Data were separated into sleep and wake periods using data on bedtimes and waketimes from daily sleep diaries, and further verified by visual inspection of the actigraphy tracings. Sleep data were then scored using the Cole–Kripke algorithm [42] to determine sleep and wake periods, and to derive the primary sleep outcomes (i.e. sleep efficiency, WASO, and duration). Sleep outcomes were averaged across all nights during each assessment period to provide an assessment of habitual sleep patterns across all available nights of data.
Sleep efficiency represents the total duration of objectively measured sleep divided by the total time in bed, as reported in sleep diaries and visual inspection of actigraphy records, with higher values indicating better sleep continuity. Sleep efficiency was analyzed as a continuous measure.
WASO was defined as the total number of minutes scored as wake (based on movement) after sleep onset based upon the Cole–Kripke algorithm. WASO was analyzed as a continuous variable, with higher values indicating longer WASO.
Sleep duration is the total amount of time spent sleeping during the participant’s time in bed, assessed by actigraphy. Based on prior literature demonstrating that both short [43] and long [44] sleep durations are associated with adverse health outcomes, secondary analyses analyzed total sleep time using three categories: <7 hr (N = 605); 7 to 9 hr (N = 159), inclusive; and >9 hr (N = 24). Notably, given the small number of “long sleepers” in this sample (only 3% of sample), the analyses comparing the reference (7–9 hr) and >9 hr group are exploratory.
Perceived neighborhood-level exposures
We included three measures of perceived neighborhood characteristics: social cohesion, perceived safety, and neighborhood satisfaction.
Social cohesion was assessed with a validated, five-item Likert-scale, ranging from 1 (strongly agree) to 5 (strongly disagree) [45]. Participants were asked how strongly they agree or disagree with various statements (e.g. “People around here are willing to help their neighbors”; “This is a close-knit neighborhood”) (Cronbach’s α = 0.84) [45]. Higher scores indicate greater social cohesion.
Perceived safety was measured by averaging four items rated on five-point Likert scales, ranging from 1 (strongly agree) to 5 (strongly disagree), with higher scores indicating greater perceived safety [46]. Participants were asked how strongly they agree or disagree with various statements (e.g. “You feel safe walking in your neighborhood during the day,” “You feel safe walking in your neighborhood at night,” “Your neighborhood is safe from crime,” “Violence is a problem in your neighborhood” (reverse-coded) (Cronbach’s α = 0.71).
Neighborhood satisfaction was assessed by a single-item rated on a five-point Likert scale, asking participants, “All things considered, would you say you are very satisfied, satisfied, dissatisfied, very dissatisfied or neutral - neither satisfied nor dissatisfied with your neighborhood as a place to live?” [47]. Higher scores indicate greater neighborhood satisfaction.
Objective neighborhood-level exposures
In both neighborhoods, trained data collectors conducted audits on 613 street segments. Segments (both sides of a street between two cross streets) were randomly selected from both neighborhoods, with an oversampling of segments where there was anticipated change. Data collectors walked the length of each segment to complete the audits, adapted from the Bridging the Gap Street Segment Tool [48, 49]. We audited a 25 per cent sample of street segments within a quarter mile of the participant’s residence [50]. Aspects of neighborhoods that were hypothesized to be relevant for sleep were selected for construction of derived variables.
Specifically, we created several scores that capture objectively-measured aspects of neighborhood disorder, street lighting, and walkability. The disorder score is the sum of following items present in the street: lack of aesthetics (e.g. art), litter, vacant housing, bars on windows, broken windows, and the data collector reporting that they did not feel safe walking on the segment. Cronbach’s α for objective neighborhood disorder is 0.77. Higher scores indicate greater disorder. The street lighting score is based on the dichotomous variable where 1 indicates any lighting on either side of the street and 0 indicates no lighting. A higher score represents a greater proportion of street segments with any street lighting. Based on prior research linking greater neighborhood disorder [13] or greater exposure to street lighting [51] with sleep disturbances, we hypothesized that these objective measures of disorder and lighting would be associated with shorter sleep duration, poorer sleep efficiency, and longer WASO.
We derived the walkability index [49] from neighborhood street segment observations in both neighborhoods. The walkability index was designed based on the social-ecological model and evidence that sidewalks and other street characteristics were associated with physical activity/walking [52–54]. Specifically, the walkability index was composed of the following items: traffic signs at the intersection (4 points) pedestrian crossings (2 points), sidewalks (10 points), lighting (2 points), transit (2 points), and mixed use (2 points). For each street segment, we summed the items and used the weighted average across the street segments (Cronbach’s α = 0.55) and the scale ranges from 0 to 22, with higher scores indicating greater walkability [49]. Consistent with limited prior research demonstrating a link between less walkable neighborhood environments and increased risk for sleep disturbance, we predicted that lower walkability would be associated with poorer sleep efficiency, longer WASO, and shorter sleep duration.
To create participant-level exposures we created a weighted average of the street segment-level measures, using the sampled segments within a quarter mile of a participant’s home with weights proportional to the length of each segment. Segments with a missing value on a measure were omitted from the participant’s buffer-level calculation for that measure.
Neighborhood-level crime exposures
Using incident-level crime data provided by the City of Pittsburgh police department and ArcGIS 10.2 software, we calculated street network distances from each household to each approximate crime location. We were able to geocode 95 per cent of the incidents using the address information from the raw data. For each household, we summed the total number of 2012 crimes that occurred within a 1 km network distance, to arrive at the household buffer for crime in 2012. The 1 km distance was chosen because this has been used in prior neighborhoods research [55, 56] and because this is considered “walking distance” (or within 10 min by walking). We predicted that higher levels of crime would be associated with poorer sleep efficiency, longer WASO, and shorter sleep duration.
Individual-level covariates
Variables that are known to be associated with sleep disturbances and/or neighborhood disadvantage were selected a priori and included as covariates. In particular, sociodemographics including age, gender, education (categorized into less than high school [referent], high school diploma, and some college/bachelor’s degree), marital/cohabitation status (married or living with a partner versus living alone), household annual income, length of time in neighborhood, and presence of children in the home were collected via interview. In addition, given known associations between sleep disturbances and symptoms of depression and anxiety [57], we statistically controlled for a general measure of psychological distress, using the validated Kessler 6 instrument (Cronbach’s α = 0.86), to evaluate the independent associations between neighborhood characteristics and sleep outcomes [58]. BMI was calculated from interviewer-measured height (without shoes) and weight as weight in kg divided by height in m2. To account for unmeasured differences across neighborhoods that could confound associations between neighborhood characteristics and sleep, we also adjusted for neighborhood, using a binary indicator of Hill District versus Homewood. We did not include race/ethnicity as a covariate because 96 per cent of the sample self-identified as Black or African American.
Analytic sample
Of the 1051 participants who were part of the study cohort in 2013, we excluded residents who no longer lived in one of the two study neighborhoods (Hill District, Homewood; n = 48), participants with <4 nights of actigraphy-measured sleep due to missing accelerometry data or incomplete sleep logs (n = 210), or who were missing covariates (n = 5). Therefore, the sample size for analysis with perceived neighborhood-level exposures was 788. For analyses with objective neighborhood-level measures, we excluded those missing street segment data from street audits (n = 65) for a sample size of 723. Finally, for analyses including neighborhood-level crime exposures, we excluded those missing crime data (n = 13) for a sample size of 775 adults. Those excluded due to missing/invalid data were on average 2 years younger than the analytic sample (p = 0.04). The analytic sample did not differ significantly from the excluded sample on any other study variables.
Statistical analyses
We performed descriptive analyses and multivariable models using SAS software, Version 9.4 (SAS Institute Inc., Cary, NC, USA). We calculated means and standard deviations (continuous variables) and percentages (categorical variables) of individual-level and neighborhood-level variables. For each neighborhood-level exposure, we ran separate main effect models predicting sleep outcomes. All models included age, gender, education, marital/cohabitation status, household annual income, presence of children in the home, length of residence in neighborhood, BMI, psychological distress, and neighborhood indicator (Hill District versus Homewood) as covariates. To assess whether associations between neighborhood-level exposures and sleep differed by neighborhood, we tested interactions between an indicator of neighborhood and each neighborhood-level exposure. We also conducted secondary analyses using multinomial logistic regression models to examine the association between neighborhood characteristics and the categorical definition of sleep duration. Also, we ran sensitivity analyses by excluding the small number of non-Black/African American participants. As results were virtually the same with and without the Black/African American participants, only models from the full sample (including non-black/non-African American participants) are presented herein.
Results
Sample characteristics
Descriptive statistics stratified by neighborhood and for the full sample are presented in Table 1. By design, 68 per cent (N = 535) of the sample was from the Hill District (intervention neighborhood), and the remaining 32 per cent (N = 253) resided in the Homewood neighborhood (Table 1). Women constituted 77 per cent of the sample. Annual household incomes averaged $20 900. Approximately 20.9 per cent of the sample was married or cohabiting, and 27.8 per cent of participants had children in the home. Participants were 55.2 years old on average, with an average BMI of 31.1 kg/m2. Sleep efficiency averaged 80.9 per cent. WASO averaged 77.5 min. Total sleep time averaged 6.0 hr. There were no differences between the two neighborhoods in individual-level sociodemographic characteristics, psychological distress, BMI, sleep duration (continuous or categorical), social cohesion, or crime levels. However, there were significant neighborhood differences in length of residence in neighborhood, sleep efficiency, WASO, neighborhood safety, satisfaction, disorder, street lighting and walkability. Therefore, all models included the neighborhood indicator*neighborhood characteristic interaction term.
Table 1.
Study characteristics for the total analytical sample and stratified by neighborhood
| Mean (SD) or per cent | |||
|---|---|---|---|
| Total (n = 788) | Intervention neighborhood (n = 535) | Control neighborhood (n = 253) | |
| Female | 77.0% | 78.1% | 74.7% |
| Mean age (years) | 55.2 (16.3) | 55.3 (16.5) | 55.2 (15.9) |
| Education | |||
| Less than high school | 13.3% | 14.0% | 11.9% |
| High school | 42.8% | 42.8% | 42.7% |
| Some college | 30.3% | 30.7% | 29.6% |
| College | 13.6% | 12.5% | 15.8% |
| Annual household income in US$1000s | 20.9 (19.2) | 21.2 (19.4) | 20.2 (19.0) |
| Married or living with partner | 20.9% | 19.6% | 23.7% |
| Household with children | 27.8% | 26.5% | 30.4% |
| Mean no. of years lived in neighborhood*** | 31.6 (23.0) | 35.4 (23.6) | 23.7 (19.5) |
| Psychological distress | 4.3 (4.6) | 4.2 (4.5) | 4.6 (4.8) |
| Mean BMI (kg/m2) | 31.1 (7.4) | 30.8 (7.2) | 31.8 (8.0) |
| Mean minutes sleep duration | 361.1 (84.8) | 363.8 (84.1) | 355.5 (86.2) |
| Mean sleep efficiency(%)** | 80.9 (9.6) | 81.7 (8.8) | 79.2 (11.1) |
| Mean minutes of WASO* | 77.5 (43.0) | 74.9 (40.6) | 83.0 (47.2) |
| Subjective neighborhood measures | |||
| Social cohesion | 3.1 (0.8) | 3.1 (0.8) | 3.0 (0.8) |
| Neighborhood safety*** | 2.9 (0.8) | 3.0 (0.8) | 2.6 (0.7) |
| Neighborhood satisfaction*** | 3.4 (1.2) | 3.6 (1.1) | 3.1 (1.2) |
| Objective neighborhood measures† | |||
| Neighborhood disorder*** | 4.7 (0.9) | 4.3 (0.7) | 5.4 (0.7) |
| Street Lighting (% of street segments)*** | 97.1 (5.0) | 97.6 (3.0) | 96.1 (7.6) |
| Walkability index*** | 8.1 (1.7) | 8.3 (1.8) | 7.6 (1.5) |
| Pittsburgh Police Dept. Data‡ | |||
| Total crime | 22.5 (18.9) | 21.7 (19.6) | 24.2 (17.4) |
*p ≤ 0.05; **p ≤ 0.001; ***p ≤ 0.0001.
†Sample sizes for the street segment audit data are total, n = 723; Hill District, n = 486; and Homewood, n = 237.
‡Sample sizes for crime data are total, n = 775; Hill District, n = 525; and Homewood, n = 250.
Neighborhood characteristics and sleep efficiency
In regression analyses (Table 2), higher levels of perceived neighborhood safety were associated with greater sleep efficiency (B = 1.14, p < 0.05). None of the other perceived neighborhood characteristics were associated with sleep efficiency, nor were there any significant interactions with neighborhood.
Table 2.
Results of linear regression models predicting sleep duration, efficiency, and WASO from subjective and objective neighborhood characteristics
| Sleep efficiency (%) | Wakefulness after sleep onset (min) | Total sleep time (min) | ||
|---|---|---|---|---|
| n | B (SE) | B (SE) | B (SE) | |
| Perceived neighborhood characteristics | ||||
| Social cohesion | 783 | 0.61 (0.54) | −2.10 (2.44) | 7.58 (4.83) |
| Social cohesion*neighborhood | 783 | −0.82 (0.88) | 4.91 (3.98) | −1.09 (7.87) |
| Safety | 788 | 1.14 (0.55)* | −5.64 (2.47)* | 2.26 (4.94) |
| Safety*neighborhood | 788 | −0.86 (0.98) | 4.43 (4.39) | −10.46 (8.79) |
| Satisfaction | 788 | 0.49 (0.37) | −2.09 (1.64) | 1.53 (3.28) |
| Satisfaction*neighborhood | 788 | −0.45 (0.62) | 2.46 (2.76) | 2.23 (5.52) |
| Objective neighborhood characteristics | ||||
| Disorder | 723 | −0.08 (0.59) | 1.45 (2.61) | 0.05 (5.29) |
| Disorder*neighborhood | 723 | −1.56 (1.08) | 8.95 (4.84)# | 1.11 (9.79) |
| Street lighting | 723 | 1.96 (14.32) | 7.23 (64.09) | 135.06 (128.89) |
| Street lighting*neighborhood | 723 | 5.83 (16.44) | −31.21 (73.58) | −50.35 (147.97) |
| Walkability | 723 | 0.37 (0.25) | −1.42 (1.11) | 3.80 (2.24)# |
| Walkability*neighborhood | 723 | −0.95 (0.48)* | 3.43 (2.14) | −7.76 (4.30)# |
| Pittsburgh Police Dept. Data | ||||
| Total crime | 775 | −0.06 (0.02)** | 0.23 (0.10)* | −0.26 (0.19) |
| Crime*neighborhood | 775 | 0.10 (0.04)* | −0.40 (0.18)* | 0.36 (0.36) |
Each of the neighborhood characteristics is entered into separate models. Each model includes the following covariates: neighborhood, age, male, married, income, education, any children in home, years lived in neighborhood, psychological distress, and BMI. For each model, the neighborhood interactions reflect the values for the control neighborhood. The intervention neighborhood is the reference category. Bold values indicate statistically significant results.
**p < 0.01; *p ≤ 0.05; #p < 0.10.
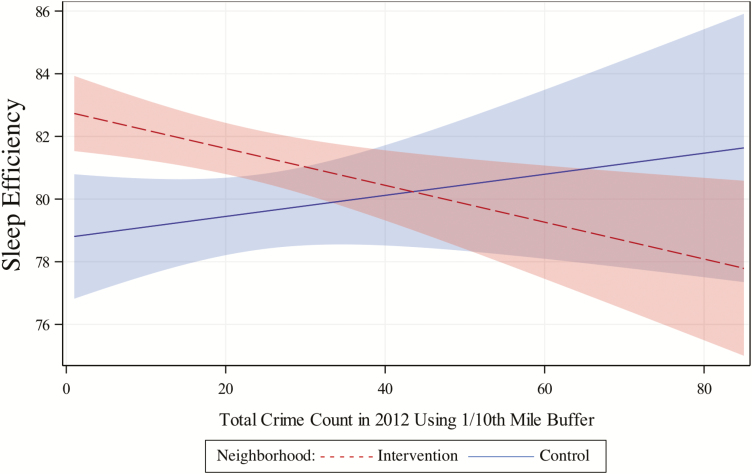
In terms of objective neighborhood characteristics, higher crime rates were associated with lower sleep efficiency (B = −0.06, p < 0.01). There was also a significant neighborhood*crime interaction for sleep efficiency (B = 0.09, p < 0.05). As shown in Figure 1, the association of crime with sleep efficiency was only evident in the Hill District. There were no other significant main effects of objective neighborhood characteristics on sleep efficiency; however, there was a significant cross-over interaction between neighborhood and walkability, indicating differential (though both non-significant) associations between walkability and sleep efficiency according to neighborhood.
Figure 1.
Predicted values for sleep efficiency according to total crime counts for each neighborhood.
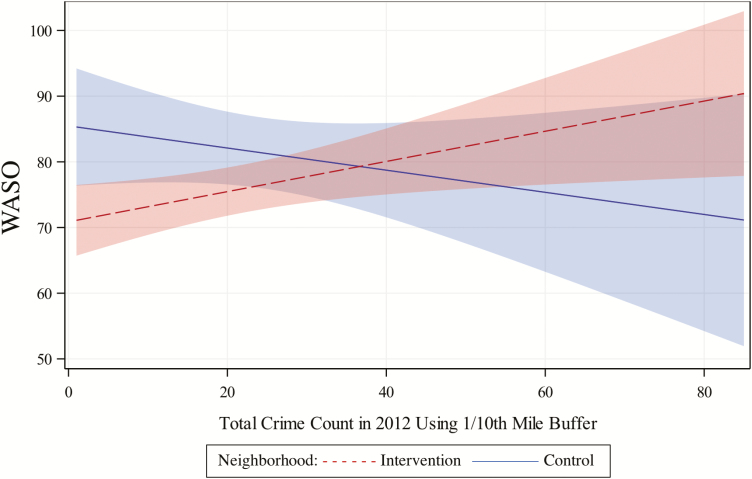
Neighborhood characteristics and WASO
Similar to the sleep efficiency results, greater perceived neighborhood safety was associated with shorter WASO (B = −5.64, p < 0.05); however, none of the other perceived neighborhood measures were associated with WASO (Table 2). As with sleep efficiency, there was a significant neighborhood*crime interaction for WASO (B = −0.40, p < 0.05) such that the association of crime with WASO was only evident in the intervention neighborhood (i.e. Hill District; Figure 2). There was also a marginal interaction between neighborhood disorder and neighborhood, such that greater disorder was associated with greater WASO, but only in the comparison neighborhood.
Figure 2.
Predicted values for WASO according to total crime counts for each neighborhood.
Neighborhood characteristics and sleep duration
As shown in Table 2, there was a marginal main effect of walkability and a marginal interaction between walkability and neighborhood on sleep duration, suggesting a positive association between more walkable neighborhoods and longer sleep duration, but only in the intervention neighborhood. None of the other perceived and objective neighborhood characteristics included in these analyses were significantly associated with either the continuous or categorical measure of sleep duration.
Discussion
The current findings are among the first to examine the association between perceived and objective indicators of neighborhood conditions and objectively measured sleep efficiency, WASO, and duration in a large, urban sample of predominantly African American residents from two socioeconomically disadvantaged neighborhoods. Results demonstrated significant, cross-sectional associations between greater objectively measured crime and poorer sleep efficiency and longer WASO. Notably, however, and consistent with other studies of neighborhood effects, the magnitude of these effects was small. In addition, there was a significant interaction between neighborhood indicator and crime such that the association between crime and sleep efficiency or WASO was only evident in the Hill District (the intervention neighborhood), despite that the two communities did not differ in crime levels at baseline. There was also a significant interaction between walkability and neighborhood on sleep efficiency, as well as marginally significant interactions between neighborhood and walkability for sleep duration, and neighborhood and disorder for WASO, suggesting a different pattern of associations between the two neighborhoods. With the exception of neighborhood disorder, findings were generally stronger and consistent with hypothesized associations in the intervention neighborhood (i.e., the Hill District). Importantly, this ongoing study is designed as a natural experiment to examine how changes in neighborhood conditions, spurred by considerable economic investment, primarily in the Hill District and to a much lesser extent in Homewood, will relate to changes in sleep and other downstream health consequences. It is not clear why the association between crime and sleep efficiency and WASO was not evident in Homewood, though it may be due to unmeasured neighborhood conditions that differentiate the neighborhoods (e.g. differences in media coverage of crime) and/or limited power due to the smaller sample in Homewood. Alternatively, one might speculate that Hill District residents were more sensitive to the effects of crime on their sleep because they had higher levels of perceived safety when compared with Homewood residents.
With regard to sleep duration, other than the marginally significant interaction between walkability and neighborhood, we did not find any other significant associations between other neighborhood characteristics and the continuous or categorical measure of sleep duration. The lack of significant associations between neighborhood conditions and sleep duration is generally consistent with the extant literature, as prior studies have similarly reported null results for actigraphy-assessed sleep duration [15, 17, 59], although there are exceptions [19]. Discrepancies across studies may reflect differences in the sample characteristics as well as differences in how neighborhood characteristics were evaluated. Importantly, indicators of disrupted sleep continuity (e.g. poorer efficiency and longer WASO), as well as short and long sleep duration are robustly linked with health outcomes, including cardiovascular disease morbidity and mortality [60, 61]. Some caution is warranted in interpretation of the multinomial regression results presented herein, as only 3 per cent of the sample was categorized as long sleepers (>9 hr of sleep, on average). Thus, we were limited in our ability to investigate the degree to which neighborhood conditions associate with longer than normal sleep durations, and the small sample size may also have limited the power to detect statistical significance and precision of point estimates in the multinomial regression models.
Consistent with prior work [18, 19, 52], including our own previous publication in this sample which focused on subjective sleep quality [62], we found that greater perceived safety was associated with better sleep efficiency and shorter WASO, even after adjusting for sociodemographic characteristics, BMI, and psychological distress. We did not, however, find significant associations between other perceived neighborhood measures including social cohesion or neighborhood satisfaction and any of the sleep outcomes, after adjustment for covariates. This is in contrast to prior work, which has generally found associations between perceived neighborhood measures and subjective sleep outcomes. Importantly, by utilizing perceived and objective indicators of neighborhood conditions and objective measures of sleep, the current study overcomes potential biases including common method variance and negative affect bias that may be inherent in the prior literature which has predominantly focused on self-reported neighborhood conditions and sleep. Finally, the overall small magnitude of the effects of neighborhood conditions on sleep both within our study and across studies may contribute to inconsistencies.
Given these findings, it is important to consider the potential pathways that may account for the observed associations. Our findings are consistent with research and theory suggesting that a sense of environmental safety and security should contribute to better sleep, at least in part, by reducing physiological and negative emotional arousal, which are antithetical to sleep [12, 13, 63]. Importantly, the fact that findings persisted even after adjustment for psychological distress suggests that the association between neighborhood disadvantage and disrupted sleep continuity is not exclusively due to psychological distress. We also found that aspects of the physical environment, namely, walkability and disorder were associated sleep outcomes, but effects were dependent on the neighborhood (as indicated by interaction terms). We did not find significant associations between street lighting and sleep outcomes; however, this may be due in part, to the limited variability in this measure, derived from street segment audits. Nevertheless, it is important for future work to examine aspects of the physical and social environment in relation to sleep, as there may be competing pathways that differentiate the effects of a given characteristic on sleep. For instance, from a social environment perspective, one might hypothesize that greater exposure to street lighting could enhance feelings of safety and security, thereby improving sleep. However, from a physical environment perspective, exposure to street lighting may disrupt sleep continuity and duration, potentially contributing to circadian disruption or perhaps in areas with greater lighting, residents are more likely to stay out at night. There are several other direct pathways through which neighborhood conditions may influence sleep, including direct effects via noise or other environmental pollutants; however, the study did not measure these constructs.
These findings must be interpreted within the context of several study limitations. First, because the data are cross-sectional, we cannot infer causality. We hope to address this limitation in the context of our ongoing study which will examine how changes in neighborhood conditions associate with changes in sleep. Second, although we statistically adjusted for many potential confounders of the association, including individual-level sociodemographic characteristics, psychological distress, and BMI, we did not control for other key confounders, particularly sleep disorders such as sleep apnea. Given that the sample is comprised of predominantly African American, overweight women, a population at high risk for sleep apnea [64], such an explanation is plausible. Although we controlled for BMI which is a robust risk factor for apnea, associations between neighborhood conditions and sleep outcomes may be due to the confounding of sleep apnea or some other unmeasured variable(s). As mentioned, although we included a number of potentially relevant objective neighborhood measures, we did not include others that may be particularly salient for sleep, including environmental pollutants and noise levels [31]. Finally, although the use of actigraphy is a strength of our study relative to sole reliance on self-reported assessments of sleep, actigraphy also has limitations and provides an imperfect, albeit validated, behavioral measure of sleep. Furthermore, we did not distinguish between weekday and weekend sleep patterns, which may have introduced heterogeneity; however, such distinctions are somewhat arbitrary in a population with nonstandard work hours and/or not working. Finally, residential selection into neighborhoods could bias results, as unobserved characteristics (e.g. health consciousness) may underlie an individual’s residential location and may also influence their sleep.
These limitations notwithstanding our study makes several unique contributions to the literature, including the inclusion of a variety of perceived and objective neighborhood conditions, as well as key objectively determined dimensions of sleep (duration, efficiency, and WASO) that are linked with morbidity and mortality. Finally, our study makes an important contribution to the literature and is relevant to public policy, as we address these questions in a high-risk and understudied population of urban, African American residents living in socioeconomically disadvantaged neighborhoods.
Neighborhood disadvantage is an important social determinant of health and health disparities, including sleep health. African Americans are disproportionately more likely to live in disadvantaged neighborhoods, even after accounting for individual-level socioeconomic status and are at increased risk for a number of sleep problems and disorders, including short sleep duration, poor sleep efficiency and quality, and increased risk for sleep apnea. Public health professionals and policy makers may consider neighborhood disorder, exposure to street lighting, crime levels, and perception of safety as key, modifiable, neighborhood factors that could contribute to the disproportionate burden of poor sleep health among African Americans and those living in socioeconomically disadvantaged neighborhoods.
Acknowledgments
The authors express sincere appreciation and gratitude to La’Vette Wagner, study field coordinator, the data collection staff, our project coordinator, Jennifer Sloan, and our research assistant, Alvin Nugroho. The authors thank our community partners, including Hill House Association, Operation Better Block, and Homewood Children’s Village and most importantly our participants, who make this work possible.
Funding
Funding was provided by the National Heart Lung Blood Institute (Grant No. R01 HL122460 and HL131531) and the National Cancer Institute (Grant No. R01CA164137).
Conflict of interest statement. Dr. Buysse has the following conflicts of interest (COIs) to disclose in the past 12 months: Consultant for BeHealth and Emmi Solutions; participated in CME program sponsored by CME Institute; and received licensing fees for the PSQI. These COIs are not relevant to the work herein. None of the other authors have financial or nonfinancial COIs to disclose relevant to the work under review.
References
- 1. Diez Roux AV, et al. . Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. [DOI] [PubMed] [Google Scholar]
- 2. White K, et al. . Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health Place. 2011;17(2):438–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Burdette HL, et al. . Neighborhood safety, collective efficacy, and obesity in women with young children. Obesity (Silver Spring). 2006;14(3):518–525. [DOI] [PubMed] [Google Scholar]
- 4. Fish JS, et al. . Association of perceived neighborhood safety with [corrected] body mass index. Am J Public Health. 2010;100(11):2296–2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Auchincloss AH, et al. . Neighborhood resources for physical activity and healthy foods and incidence of type 2 diabetes mellitus: the Multi-Ethnic study of Atherosclerosis. Arch Intern Med. 2009;169(18):1698–1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Morenoff JD, et al. . Understanding social disparities in hypertension prevalence, awareness, treatment, and control: the role of neighborhood context. Soc Sci Med. 2007;65(9):1853–1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mujahid MS, et al. . Neighborhood characteristics and hypertension. Epidemiology. 2008;19(4):590–598. [DOI] [PubMed] [Google Scholar]
- 8. Gallicchio L, et al. . Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18(2):148–158. [DOI] [PubMed] [Google Scholar]
- 9. Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol. 2015;66: 143–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jennings JR, et al. . Self-reported sleep quality is associated with the metabolic syndrome. Sleep. 2007;30(2):219–223. [DOI] [PubMed] [Google Scholar]
- 11. Nock NL, et al. . Empirical evidence for “syndrome Z”: a hierarchical 5-factor model of the metabolic syndrome incorporating sleep disturbance measures. Sleep. 2009;32(5):615–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hale L, et al. . Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Prev Med. 2010;51(3-4):275–278. [DOI] [PubMed] [Google Scholar]
- 13. Hale L, et al. . Perceived neighborhood quality, sleep quality, and health status: evidence from the Survey of the Health of Wisconsin. Soc Sci Med. 2013;79:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hill TD, et al. . Neighborhood disorder, sleep quality, and psychological distress: testing a model of structural amplification. Health Place. 2009;15(4):1006–1013. [DOI] [PubMed] [Google Scholar]
- 15. Johnson DA, et al. . The association of neighborhood characteristics with sleep duration and daytime sleepiness. Sleep Health. 2015;1(3):148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bagley EJ, et al. . Neighborhood economic deprivation and social fragmentation: associations with children’s sleep. Behav Sleep Med. 2016;14:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Desantis AS, et al. . Associations of neighborhood characteristics with sleep timing and quality: the Multi-Ethnic Study of Atherosclerosis. Sleep. 2013;36(10):1543–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hill TD, et al. . Perceived neighborhood safety and sleep quality: a global analysis of six countries. Sleep Med. 2016;18:56–60. [DOI] [PubMed] [Google Scholar]
- 19. Johnson DA, et al. . The neighborhood social environment and objective measures of sleep in the multi-ethnic study of atherosclerosis. Sleep. 2017;40(1). doi:10.1093/sleep/zsw016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Brouillette RT, et al. . Childhood sleep apnea and neighborhood disadvantage. J Pediatr. 2011;158(5):789–795.e1. [DOI] [PubMed] [Google Scholar]
- 21. Chambers EC, et al. . Sleep and the housing and neighborhood environment of urban Latino adults living in low-income housing: the Ahome study. Behav Sleep Med. 2016;14(2):169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Simonelli G, et al. . The impact of home safety on sleep in a Latin American country. Sleep Health. 2015;1(2):98–103. [DOI] [PubMed] [Google Scholar]
- 23.Singh GK, Kenney MK. Rising prevalence and neighborhood, social, and behavioral determinants of sleep problems in US children and adolescents, 2003–2012. Sleep Disord. 2013;2013:394320. doi:10.1155/2013/394320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ross CE, et al. . Disorder and decay: the concept and measurement of perceived neighborhood disorder. Urban Aff Rev. 1999;34(3):412–432. [Google Scholar]
- 25. Sampson RJ, et al. . Seeing disorder: neighborhood stigma and the social construction of “broken windows”. Soc Psychol Q. 2004;67(4):319–342. [Google Scholar]
- 26. Weden MM, et al. . Subjective and objective neighborhood characteristics and adult health. Soc Sci Med. 2008;66(6):1256–1270. [DOI] [PubMed] [Google Scholar]
- 27. Wen M, et al. . Objective and perceived neighborhood environment, individual SES and psychosocial factors, and self-rated health: an analysis of older adults in Cook County, Illinois. Soc Sci Med. 2006;63(10):2575–2590. [DOI] [PubMed] [Google Scholar]
- 28. Lauderdale DS, et al. . Sleep duration: how well do self-reports reflect objective measures? The CARDIA Sleep Study. Epidemiology. 2008;19(6):838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Simonelli G, et al. . Neighborhood factors as predictors of poor sleep in the Sueno ancillary study of the Hispanic community health study/study of Latinos. Sleep. 2016;40(1):zsw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Adenekan B, et al. . Sleep in America: role of racial/ethnic differences. Sleep Med Rev. 2013;17(4):255–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Baldwin CM, et al. . Sleep disturbances, quality of life, and ethnicity: the Sleep Heart Health Study. J Clin Sleep Med. 2010;6(2):176–183. [PMC free article] [PubMed] [Google Scholar]
- 32. Chen X, et al. . Racial/ethnic differences in sleep disturbances: the multi-ethnic study of atherosclerosis (MESA). Sleep. 2015;38(6):877–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hall MH, et al. . Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep. 2009;32(1):73–82. [PMC free article] [PubMed] [Google Scholar]
- 34. Olafiranye O, et al. . Obstructive sleep apnea and cardiovascular disease in blacks: a call to action from the Association of Black Cardiologists. Am Heart J. 2013;165(4):468–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pattillo M. Black middle-class neighborhoods. Annu Rev Sociol. 2005;31(1):305–329. [Google Scholar]
- 36. Cappuccio FP, et al. . Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Reither EN, et al. . Ethnic variation in the association between sleep and body mass among US adolescents. Int J Obes (Lond). 2014;38(7):944–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cellini N, et al. . Direct comparison of two actigraphy devices with polysomnographically recorded naps in healthy young adults. Chronobiol Int. 2013;30(5):691–698. [DOI] [PubMed] [Google Scholar]
- 39. Cellini N, et al. . Free-living cross-comparison of two wearable monitors for sleep and physical activity in healthy young adults. Physiol Behav. 2016;157:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rosenberger ME, et al. . Twenty-four hours of sleep, sedentary behavior, and physical activity with nine wearable devices. Med Sci Sports Exerc. 2016;48(3):457–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zinkhan M, et al. . Agreement of different methods for assessing sleep characteristics: a comparison of two actigraphs, wrist and hip placement, and self-report with polysomnography. Sleep Med. 2014;15(9):1107–1114. [DOI] [PubMed] [Google Scholar]
- 42. Cole RJ, et al. . Automatic sleep/wake identification from wrist activity. Sleep. 1992;15(5):461–469. [DOI] [PubMed] [Google Scholar]
- 43. Itani O, et al. . Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. 2017;32:246–256. [DOI] [PubMed] [Google Scholar]
- 44. Jike M, et al. . Long sleep duration and health outcomes: a systematic review, meta-analysis and meta-regression. Sleep Med Rev. 2018;39:25–36. [DOI] [PubMed] [Google Scholar]
- 45. Sampson RJ, et al. . Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. [DOI] [PubMed] [Google Scholar]
- 46. Mujahid MS, et al. . Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. 2007;165(8):858–867. [DOI] [PubMed] [Google Scholar]
- 47. Pebley AR, et al. . The Los Angeles Family and Neighborhood Survey. Santa Monica, CA: RAND Corporation; 2004. [Google Scholar]
- 48. Kelly CM, et al. . The association of sidewalk walkability and physical disorder with area-level race and poverty. J Epidemiol Community Health. 2007;61(11):978–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Slater SJ, et al. . Walkable communities and adolescent weight. Am J Prev Med. 2013;44(2):164–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. McMillan TE, et al. . Neighborhood sampling: how many streets must an auditor walk? Int J Behav Nutr Phys Act. 2010;7:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Chepesiuk R. Missing the dark: health effects of light pollution. Environ Health Perspect. 2009;117(1):A20–A27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Duncan DT, et al. . Perceived neighborhood safety is associated with poor sleep health among gay, bisexual, and other men who have sex with men in Paris, France. J Urban Health. 2017;94(3):399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Dunton GF, et al. . Physical environmental correlates of childhood obesity: a systematic review. Obes Rev. 2009;10(4):393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Smith KR, et al. . Effects of neighborhood walkability on healthy weight: assessing selection and causal influences. Soc Sci Res. 2011;40(5):1445–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Boone-Heinonen J, et al. . The neighborhood energy balance equation: does neighborhood food retail environment + physical activity environment = obesity? The CARDIA study. PLoS One. 2013;8(12):e85141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Rundle AG, et al. . Using GPS data to study neighborhood walkability and physical activity. Am J Prev Med. 2016;50(3):e65–e72. [DOI] [PubMed] [Google Scholar]
- 57. Alvaro PK, et al. . A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kessler RC, et al. . Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. [DOI] [PubMed] [Google Scholar]
- 59. Fuller-Rowell TE, et al. . Racial disparities in sleep: the role of neighborhood disadvantage. Sleep Med. 2016;27-28:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Dew MA, et al. . Healthy older adults’ sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med. 2003;65(1):63–73. [DOI] [PubMed] [Google Scholar]
- 61. Knutson KL. Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab. 2010;24(5):731–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. DeSantis A, et al. . Is the association between neighborhood characteristics and sleep quality mediated by psychological distress? An analysis of perceived and objective measures of 2 Pittsburgh neighborhoods. Sleep Health. 2016;2(4):277–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Troxel WM, et al. . Examination of neighborhood disadvantage and sleep in a multi-ethnic cohort of adolescents. Health Place. 2017;45:39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Durrence HH, et al. . The sleep of African Americans: a comparative review. Behav Sleep Med. 2006;4(1):29–44. [DOI] [PubMed] [Google Scholar]