Abstract
Study Objectives
To identify weekly sleep trajectories (sleep pattern changing by day over a course of week) of specific characteristics and examine the associations between trajectory classes and obesity and hypertension.
Methods
A total of 2043 participants (mean age 46.9, 65.5% female) completed at least 7 days of actigraphy aged 18–64 from the Sueño ancillary study of the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Weekly sleep trajectories for three daily level measures (wake after sleep onset [WASO], daytime napping duration, and intranight instability index) were identified using latent class growth models. The outcomes were obesity and hypertension.
Results
Using the trajectory with low-stable WASO as reference, the trajectory classes with increasing and high-concave patterns had significantly higher odds for obesity (OR 3.64 [1.23–10.84]) and hypertension (OR 5.25 [1.33, 20.82]), respectively. Compared with individuals with a low-stable napping duration trajectory, those with the high-concave pattern class were associated with hypertension (OR 2.27 [1.10–4.67]), and the association was mediated in part by obesity (OR 1.11 [1.00–1.22]). Individuals in the high intranight instability index trajectory had significantly larger likelihood for both obesity (OR 1.90 [1.26–2.86]) and hypertension (OR 1.86 [1.13–3.06]) compared with those in the low intranight instability index trajectory.
Conclusions
Weekly trajectories varied for WASO, daytime napping duration, and intranight instability index. The trajectories with relatively larger values for these three measures were associated with greater risk for obesity and hypertension. These findings suggest that a stable pattern with relatively small weekly and nightly variability may be beneficial for cardiovascular health.
Keywords: sleep trajectory, obesity, hypertension, wake after sleep onset, napping duration, actigraphy
Statement of Significance
Existing studies investigating associations between sleep and cardiovascular disease (CVD) risk factors rely on data in which sleep measures are summarized over multiple days. Using a longitudinal latent growth modeling approach, we observed heterogeneity in interday night-to-night sleep patterns and found that sleep patterns with large weekly and/or nighty variability were associated with prevalent hypertension and obesity. These findings highlight the importance of temporal sleep beyond average measures. Future longitudinal studies assessing weekly sleep trajectories with CVD risk incidence are needed to provide insights into causal associations.
Introduction
Sleep greatly influences people’s daily functioning and physical and mental health. Many studies have observed an association between sleep quantity and quality with cardiovascular disease (CVD) risk [1–3]. Major CVD diseases are leading causes of mortality among US Hispanic/Latino individuals, and prevalence of hypertension and obesity varies markedly across Hispanic/Latino background groups [4]. For these reasons, there is a strong interest in understanding the association between sleep measures and CVD risk factors in the diverse Hispanic/Latino population [5, 6].
Patel et al. found both high variability in night-to-night sleep duration and increased daytime napping duration to be strongly associated with obesity, independent of mean nightly sleep duration [7]. In addition, Knutson et al. found that later sleep timing was significantly associated with higher estimated insulin resistance in both those with and without diabetes [8]. These findings suggest that characteristics of sleep beyond mean sleep duration may play a role in weight homeostasis and metabolic function, highlighting the complex relationship between sleep and metabolism. However, most prior studies have used summarized sleep measures over several days, which are unable to provide a complete description of sleep patterns, i.e. amount, quality, and regularity of sleep. For example, using standard deviation to summarize multinight sleep duration is not able to elucidate night-to-night patterns of variation. Despite the recent derivation of sleep trajectories from longitudinal data, which can vary within and between individuals, the sleep pattern changing by day over a course of week (weekly sleep trajectories) has not been investigated [9–11].
Actigraphy-derived multinight data are an emerging tool, which not only provides detailed observations for each night but also allows for assessment of multinight variations. Since those daily level activity measures in literature are designed to describe 24 hr circadian rhythms (e.g. intraday variability score) and not specific to sleep [12, 13], we derive a new measure from each day’s actigraphy activity during nightly sleep and named, “intranight instability index.” We further investigate whether this measure is indicative of nightly sleep patterns associated with hypertension or obesity.
The objective of this study is to utilize a longitudinal latent growth modeling approach to identify weekly sleep trajectories to describe temporal sleep patterns across a week. We hypothesized that the weekly sleep trajectory classes are associated with obesity and hypertension independent of sleep duration. The investigation of associations between weekly sleep trajectories derived from objective repeated measures data and CVD risk factors including examination of possible mediators might reveal new insights not evident from traditional summary sleep measures.
Methods
The Sueño study
The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) is a multicenter epidemiological study of 16415 self-identified Hispanic/Latino adults at four field centers (Bronx, NY; Chicago, IL; Miami, FL; and San Diego, CA) [14, 15]. Study participants aged 18–74 underwent an extensive clinical exam and assessments to determine baseline risk factors between 2008 and 2011. The Sueño sleep ancillary study recruited 2252 individuals aged 18–64 from December 2010 to December 2013 who were within 30 months of their baseline HCHS/SOL examination. Participants were excluded if they reported a history of narcolepsy, severe obstructive sleep apnea, or were found to have severe obstructive sleep apnea on home sleep testing. Further details of this cohort have been previously described [16]. All Sueño participants were asked to wear an Actiwatch Spectrum (Philips Respironics, Murrysville, PA) device on their nondominant wrist and not remove the device for the duration of the study. In this paper, we consider only 2043 individuals who had at least 7 days actigraphy sleep data. The actigraphy method utilized by Sueño study follows the general guidelines in literature [17].
Variables
Five conventional nightly sleep measures, wake after sleep onset (WASO), sleep duration, sleep latency (duration between time in bed and sleep onset), sleep midpoint (clock time of the epoch that is exactly midway in the sleep interval), and number of wake bouts (number of continuous periods of wake, at least 30 s long, during sleep interval) were summarized at the daily sleep interval level. Actigraphs were programmed to collect activity and ambient light data in 30 s epochs. A validated Sueño algorithm was used to set main rest intervals (interval starts from the first epoch scored as sleep and ends in the last epoch scored as sleep) based on four inputs: event markers, sleep diary, white light intensity, and activity in order of importance, respectively [16]. Once rest intervals were defined, the Actiware 5.59 algorithm was applied to generate sleep/wake status for each epoch. The 7 day sequence for weekly trajectory was from Monday to Sunday defined by sleep end time. For instance, if the sleep interval end time is between Monday 0:00 and 24:00, the day is referenced as Monday. This weekday reference of a sleep interval reflects the sleep start time in previous day, e.g. if sleep ends on Monday morning, the sleep start time is usually on Sunday.
Two conventional nap measures are considered: daytime napping duration and number of naps. Napping time was defined as minutes scored as sleep in blocks of at least 5 min occurring outside of the main sleep interval. The weekday reference for nap measures is based on nap ending time.
For this study, there were two CVD risk factors defined as the primary response variables: obesity and hypertension at the in-person Sueño visit. Obesity was defined as body mass index (BMI: weight/height2) of greater than or equal to 30 kg/m2. Hypertension was defined as a self-reported physician diagnosis of high blood pressure that was not isolated to a pregnancy.
Intranight instability index
We proposed a new summary measure named intranight instability index (mean of activity count in a sleep interval divided by standard deviation of activity count in the same interval) to describe the nightly sleep pattern. Our theoretical derivation indicated that intranight instability index increases with the increasing of mean activity or the decreasing of percentage of epochs with zero activity count. This was evidenced by the strong data correlation between intranight instability index and mean activity (corr = 0.91, p < 0.001), and between intranight instability index and percentage of epochs with zero activity count (corr = −0.84, p < 0.001) during sleep. In addition, the magnitude of intranight instability index had a concordance with the magnitude of four commonly used sleep measures, which implies that larger intranight instability index is indicative of longer onset latency and WASO, less sleep efficiency (percentage of time spent asleep within sleep interval), and larger fragmentation index. These suggested intranight instability index as a marker of nightly sleep quality. See Supplementary Material for details.
Statistical methods
The reported values in the tables were weighted to adjust for HCHS/SOL sampling weights to account for the complex survey design. All analyses were conducted using SAS software, version 9.4. Latent class growth models (LCGM) are semiparametric techniques used to identify distinct subgroups of individuals following a similar pattern of change over time on a given variable [18]. They were used to identify groups who shared similar underlying trajectories over a week for relevant sleep measures in this study. LCGM univariate models (each model includes only one sleep measure as a response variable) were estimated using SAS Proc Traj, an add-on SAS procedure based on a semiparametric group–based modeling strategy [19, 20]. We do not consider multivariate models that simultaneously evaluate more than one sleep measure due to the problem of convergence when using Proc Traj. To account for uncertainty in trajectory group memberships assigned from posterior probability, 20 datasets with imputed membership were generated. Logistic regression analyses were applied to estimate the associations between sleep pattern groups and obesity and hypertension for each dataset, and the SAS MIANALYZE procedure was used to combine the results. See Supplementary Material for details on the estimation.
We also examined whether one of the two risk factors is a mediator for the association between the other risk factor and sleep trajectories in all models [21]. The results indicated that the association between hypertension and napping duration trajectories is partially explained by a mediator, obesity. A mediation analysis modifying the method by Valeri and VanderWeele was followed to appropriately account for the HCHS/SOL complex sampling design [22].
Results
Wake after sleep onset
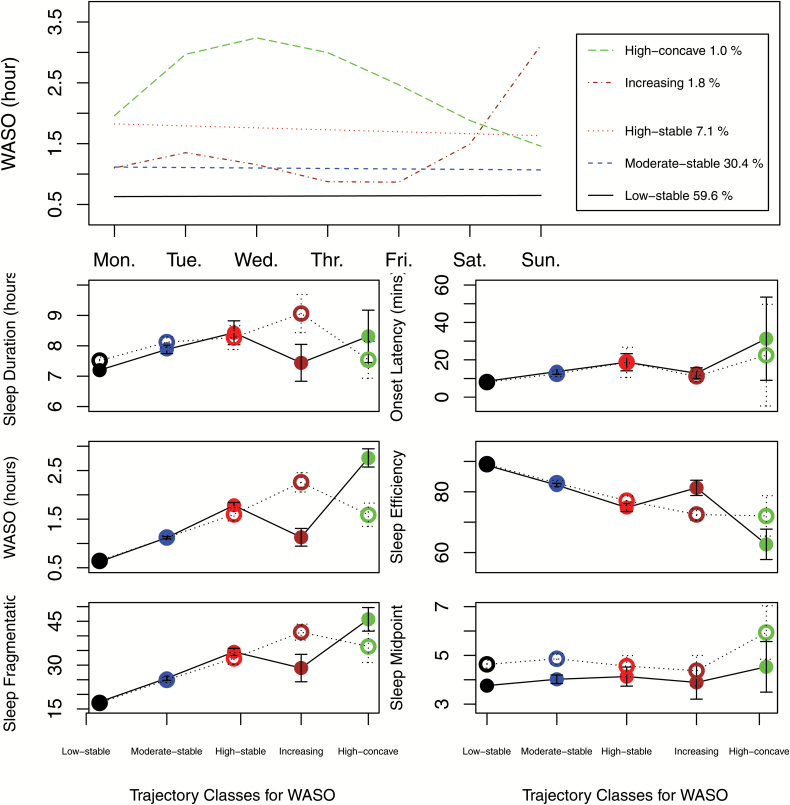
Five identified trajectories for WASO are shown in the top plot in Figure 1: low-stable: 59.6 per cent of participants had an approximate 0.6 hr stable WASO; moderate-stable: 30.4 per cent of participants had a stable WASO slightly larger than 1 hr; high-stable: 7.1 per cent of participants had stable WASO between 1.5 and 2 hr; increasing: 1.8 per cent of participants had WASO around 1 hr on weekdays and increased up to 3 hr in weekends; and high-concave: 1 per cent of participants had large WASO ranging from 1.5 to 3.5 hr with a concave curvature pattern.
Figure 1.
Weekly trajectory classes identified for the WASO (hr), and average of six sleep measures by weekday vs. weekends depending on trajectory classes. Solid circle with solid line: weekday average with 95% CI; open circle with dotted line: weekend average with 95% CI.
The associations between trajectory classes and outcomes are shown in Table 1. Using the low-stable class as reference, individuals in the increasing class had significantly higher odds for obesity (OR 3.64 [1.23–10.84]); individuals in the high-concave and high-stable classes had significantly higher odds (OR 5.25 [1.33–20.82]) and nearly significant higher odds (OR 1.92 [0.92–4.01]) for hypertension, respectively.
Table 1.
Associations between response variables and trajectory classes for WASO and intranight instability index
| Obesity | Hypertension | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | ||||||
| OR (95% CI) |
P | OR (95% CI) |
P | OR (95% CI) |
P | OR (95% CI) |
P | ||
| Trajectory class for WASO | Ref: Low-stable | ||||||||
| Moderate-stable | 1.00 (0.71,1.39) |
0.980 | 1.13 (0.80,1.59) |
0.499 | 1.04 (0.69,1.57) |
0.832 | 1.10 (0.72,1.70) |
0.652 | |
| High-stable | 0.99 (0.56,1.75) |
0.978 | 1.25 (0.68,2.29) |
0.472 | 1.74 (0.83,3.67) |
0.143 | 1.92 (0.92,4.01) |
0.082 | |
| Increasing | 3.20 (1.11,9.22) |
0.031 | 3.64 (1.23,10.84) |
0.020 | 1.30 (0.44,3.81) |
0.630 | 1.35 (0.45,4.04) |
0.595 | |
| High-concave | 0.83 (0.29,2.43) |
0.741 | 1.00 (0.36,2.74) |
0.998 | 4.83 (1.29,18.07) |
0.019 | 5.25 (1.33,20.82) |
0.018 | |
| Trajectory class for intranight instability index | Ref: Low | ||||||||
| Moderate | 1.27 (0.92,1.75) |
0.146 | 1.30 (0.95,1.80) |
0.105 | 1.01 (0.72,1.41) |
0.972 | 1.01 (0.72,1.41) |
0.954 | |
| High | 1.78 (1.19,2.67) |
0.005 | 1.90 (1.26,2.86) |
0.002 | 1.84 (1.11,3.05) |
0.017 | 1.86 (1.13,3.06) |
0.015 | |
| Highly variable | 1.36 (0.67,2.74) |
0.398 | 1.31 (0.64,2.69) |
0.454 | 1.88 (0.86,4.10) |
0.114 | 1.85 (0.84,4.07) |
0.125 | |
Obesity: BMI at Sueño ≥ 30; Hypertension: self-report of a physician diagnosis of high blood pressure, and hypertension not concurrent with pregnancy at Sueño.
Model 1: adjusted for age, gender, race, site, and employment (part-time and shift, part-time and nonshift, full-time and shift, and full-time and nonshift); Model 2: adjustment in model 1 + average sleep duration.
Daytime napping duration
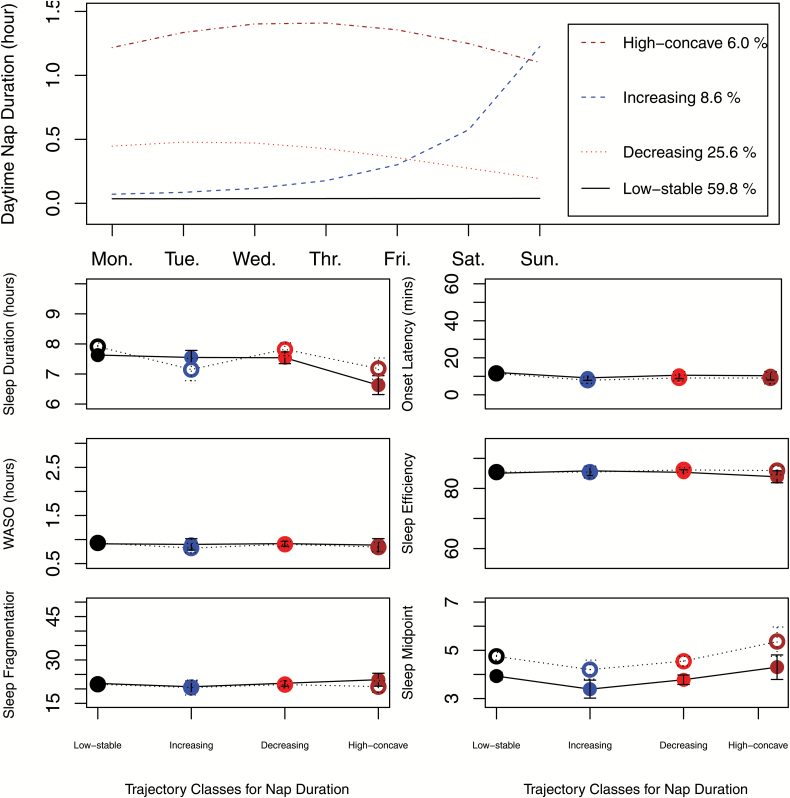
The top plot in Figure 2 shows four identified trajectories for the daytime napping duration in hours: low-stable: 59.8 per cent of participants consistently had almost very little napping; decreasing: 25.6 per cent of participants had a decreasing trend from weekday towards weekend; increasing: 8.6 per cent of participants had an increasing pattern from weekdays towards weekend; high-concave: 6.0 per cent of participants had more than 1 hr napping duration with a concave pattern.
Figure 2.
Weekly trajectory classes identified for the daytime napping duration (hr), and average of six sleep measures by weekday vs. weekends depending on trajectory classes. solid circle with solid line: weekday average with 95% CI; open circle with dotted line: weekend average with 95% CI.
The results for modeling the association between hypertension and napping duration trajectories considering obesity as a mediator are shown in Table 2. Compared with the low-stable class, the association between hypertension and the high-concave pattern class was significant (OR 2.27 [1.10–4.67]), and this association was mediated in part through obesity (OR 1.11 [1.00–1.22], p value = 0.054). The direct association was significant (OR 2.06 [1.00–4.21], p value = 0.049) and stronger than indirect association through obesity.
Table 2.
Associations between hypertension and trajectory classes for daytime napping duration with obesity as a mediator
| Response variable: hypertension; mediator: obesity | ||||||
|---|---|---|---|---|---|---|
| Trajectories for daytime nap duration (Ref: Low-stable) | Direct association | Indirect association | Total association | |||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Increasing | 0.86 (0.48,1.56) | 0.629 | 1.02 (0.93,1.13) | 0.642 | 0.88 (0.48 1.62) | 0.689 |
| Decreasing | 1.30 (0.91, 1.85) | 0.148 | 0.98 (0.92, 1.04) | 0.529 | 1.27 (0.89, 1.83) | 0.187 |
| High-concave | 2.06 (1.00, 4.21) | 0.049 | 1.11 (1.00, 1.22) | 0.054 | 2.27 (1.10, 4.67) | 0.026 |
Hypertension: self-report of a physician diagnosis of high blood pressure, and hypertension not concurrent with pregnancy at Sueño; Obesity: BMI at Sueño ≥ 30.
Model 1: adjusted for age, gender, race, site, and employment (part-time and shift, part-time and nonshift, full-time and shift, full-time and nonshift); Model 2: adjustment in model 1 + average sleep duration.
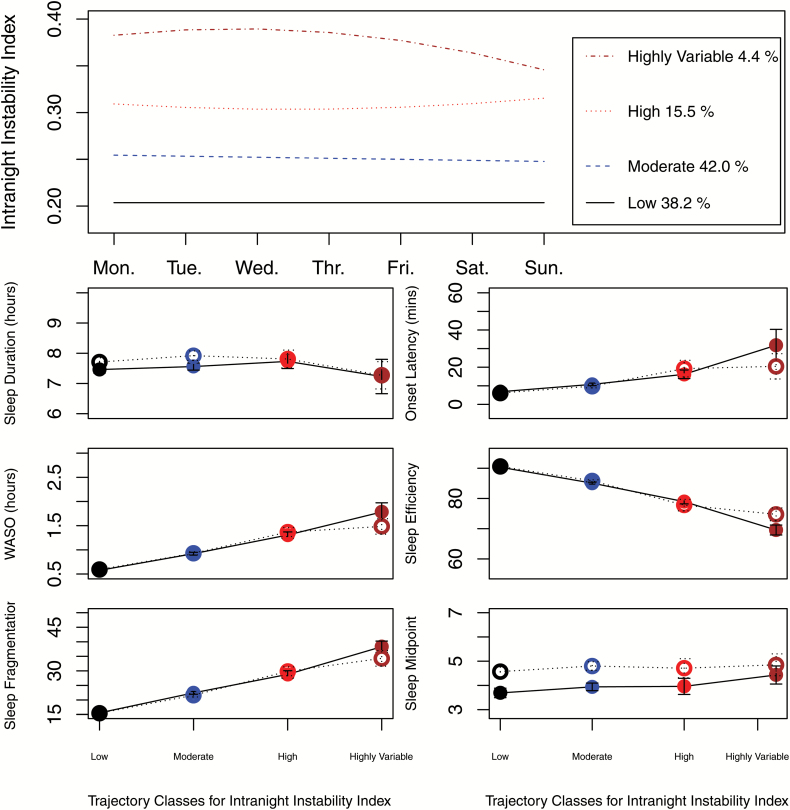
Intranight instability index
As shown in Figure 3, there are four identified trajectories for intranight instability index. low: 38.2 per cent of participants had stable pattern with approximate 0.2 index; moderate: 42.0 per cent of participants had stable index about 0.25; high: 15.5 per cent of participants had index around 0.3 with slight increasing trend; and highly variable: 4.4 per cent of participants had a decreasing trend with large value of index above 0.35. It can been seen from subplots in Figure 3 that there were no significant differences for duration and time across different trajectory groups, but the differences exist for sleep quality (linear patterns for sleep onset latency, WASO, sleep efficiency, and sleep fragmentation index). It implies that intranight instability index is indicative of sleep quality more than duration. As shown in Table 1, compared with the low intranight instability index class, individuals in high class had significant higher odds for both obesity (OR 1.90 [1.26–2.86]) and hypertension (OR 1.86 [1.13–3.06]).
Figure 3.
Weekly trajectory classes identified for intranight instability index and average of six sleep measures by weekday vs. weekends depending on trajectory classes. Solid circle with solid line: weekday average with 95% CI; open circle with dotted line: weekend average with 95% CI.
Trajectories by employment status
The distributions of trajectory classes were significantly different across three categories of employment status: unemployed, nonshift workers, and shift workers. The “shiftwork” variable was obtained from an occupational questionnaire administered on the day that actigraphy was begun. This questionnaire collected a variety of data related to work status, including commute time, number of jobs worked, and shift classification (afternoon shift, night shift, split shift, irregular shift/on call, and rotating shift), the latter used to define whether changing shifts was characteristic of current job (Supplementary Table 7). Compared with shift workers and unemployed individuals, nonshift workers had significantly higher proportion in trajectory classes with less variability (with lower WASO, shorter napping duration, or smaller intranight instability index). See Supplemental Table 5 for details.
Five other sleep measures
We also identified weekly trajectories for sleep duration, number of daytime naps, sleep onset latency, sleep midpoint, and number of wake bouts during sleep interval. However, these trajectories were not informative because the patterns were either relatively flat (reflecting mean values across the week) or not associated with obesity or hypertension. For example, the three identified weekly trajectories for sleep duration had parallel patterns being flat on weekdays and slightly increased on weekend. They can be represented as average sleep durations clustered around 5.8, 7.6, and 9.4 hr. Similar patterns were also observed for sleep midpoint. The varied trajectories for sleep onset latency were associated with neither obesity nor hypertension.
Discussion
Using LCGM, we identified heterogeneous weekly sleep trajectories and investigate their associations with obesity and hypertension. The existing studies investigating associations between sleep and CVD risk factors rely on data in which the sleep measures are summarized over multiple days. To the best of our knowledge, we are among the first to model the nonlinear patterns of daily sleep over a week and to study their association with obesity and hypertension using a novel longitudinal data analysis technique. In conclusion, the trajectories for WASO with relatively large weekly variability or longer duration were associated with an increased risk of obesity and hypertension. Daytime napping duration of more than 1 hr reflects poor nightly sleep and was associated with a higher risk of hypertension, and this association was mediated in part by obesity. The intranight instability index is indicative of nightly sleep quality. Larger values of intranight instability index were associated with increased risk of obesity and hypertension.
These heterogeneous patterns and associated CVD health implications were not evident from the traditional summary measures. For example, although the association between average WASO and obesity was not significant (OR 1.13 [0.98–1.30]), we identified the increasing trajectory for WASO with significant odds for obesity (OR 3.64 [1.23–10.84]). As another example, the contrary patterns between increasing and decreasing trajectories for napping duration are not differentiable in terms of average napping duration (increasing: 25.5 min; decreasing: 23.9 min). These highlight the importance of temporal sleep beyond average measures.
Weekday-to-weekend differences in sleep seems to be the main factor driving the large inter-day variability for various sleep trajectories. Social jetlag (circadian dyssynchrony in sleep timing induced by work/school schedule) has been shown to be associated with poor health independent of sleep duration in several studies [23, 24]. The weekday/weekend differences in sleep mid-time were similar across various trajectory groups, which implies that social jetlag was not a significant confounder in our analysis. It appears that compensation for weekday sleep deficiencies is only beneficial when weekend sleep is not compromised in terms of both duration and quality. For instance, the participants in the increasing group for WASO had longer weekend sleep durations but worse sleep quality, and they had higher odds for obesity; the participants having better weekend sleep quality but shorter duration in the high-concave class for WASO were found to have a higher likelihood of hypertension.
Findings for napping duration trajectories support previous reports that short 10–30 min habitual napping is beneficial, and more than 1 hr daytime napping may be associated with CVD risk factors [25–27]. Moreover, our approach was strengthened by examining nightly sleep related to napping trajectory classes. It implies that the daytime nap is beneficial only when the nightly sleep deficiency is compromised in terms of both duration and quality. Individuals, who supplemented slightly shorter nightly sleep on weekdays (e.g. decreasing napping trajectory) or on weekends (e.g. increasing napping trajectory) by napping, were not at increased odds for obesity or hypertension. On the other hand, the daytime nap following relatively shorter nightly sleep was associated with a higher risk of obesity and hypertension in the high-concave napping trajectory class.
Our proposed nightly sleep measure, intranight instability index, combines information regarding mean activity with the percentage of epochs with zero activity count during sleep. This strengthens the ability of the index to predict metabolic outcomes. In terms of statistical significance and magnitude of odds ratio, Supplementary Table 2 shows that the intranight instability index was associated with both obesity and hypertension more strongly than most other single traditional measures. There were two exceptions: the OR was higher for WASO than for the intranight instability index for hypertension, and longer sleep duration was more strongly protective than did the intranight instability index representing a risk for obesity. Larger intranight instability index values indicate lower sleep quality and were associated with increased risk of obesity and hypertension. The effects for the highly variable intranight instability index trajectory were not significant and might be a result of lack of power. Supplementary Material provides additional details regarding the justification of intranight instability index.
The distribution of employment status by sleep trajectories shows that the highly variable sleep classes were not simply due to a high prevalence of shift workers since the distribution of sleep patterns was not significantly different between unemployed individuals and shift workers (Supplementary Table 5). This might be explained by findings in some studies that the unemployed individuals have lower sleep quality and shorter sleep duration [28–30]. Those employed individuals in the increasing group for WASO might experience high job stress due to long work hours (about 7.5 hr in average more than those in other groups) and therefore slept longer on weekends. The increasing and high-concave groups for WASO also had higher prevalence of ever having shift work in current job (increasing: 57.7 per cent; high concave: 78.0 per cent), and longer commute times (home-to-work: increasing [0.46], high concave [0.53]; work-to-home: increasing [0.86], high concave [0.53] in hours) comparing with those of other classes. It is challenging to maintain an ideal sleep since people today face various stresses associated with fast life pace. An individual may try to maintain a stable nightly sleep pattern and to include short daytime nap or weekend catch-up sleep when nightly sleep is not enough. Our findings suggest that sleep compensation may not be beneficial if the nightly sleep deficiency is more severe (e.g. the high concave class for both WASO and daytime napping duration).
There are several limitations of our work that should be noted. In this study, the sleep intervals of Sueño actigraphy data were set using a standardized scoring algorithm. That was found to be highly reproducible in generating sleep variables with no significant differences in reproducibility across important subgroups and activity data [16]. However, the gold standard of sleep assessment, polysomnography, was not performed concurrently with actigraphy in the Sueño study. The measures derived from actigraphy data might not represent true sleep well with some errors, which results in biases in analysis. A reasonable assumption is that an individual’s sleep habit would not change significantly over a short time period [10, 31]. This supports our estimates of general weekly sleep behavior. Whenever data are available, analyses based on sleep over weeks, months, and even years will be more informative and powerful in assessing sleep changes over time. It is known that different devices and scoring algorithms produce different counts for the same activity [32]. Therefore, the extent to which the methods describe here are generalizable to other devices or other methods of summarizing accelerometry is unclear at this time, and future studies will be required to validate the use of the intranight instability index in a broader range of settings. Finally, this was a cross-sectional study, that is, outcomes are observed at the time when sleep is measured. Longitudinal studies are needed to evaluate the association of sleep trajectories with CVD risk incidence.
We examine the complex associations of sleep with obesity and hypertension based on a more complete metric including nightly sleep, daytime naps, and sleep quality. Our findings suggest that beneficial sleep from a cardiovascular standpoint should have a stable pattern with relatively small weekly and nightly variability.
Supplementary Material
Supplementary material is available at SLEEP online.
Funding
The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Center on Minority Health and Health Disparities, the National Institute of Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements. The Sueño ancillary study was supported by NHLBI HL098297.
Conflict of interest statement. None declared.
References
- 1. Haba-Rubio J, et al. . Objective sleep structure and cardiovascular risk factors in the general population: the HypnoLaus Study. Sleep. 2015;38(3):391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ford ES, et al. . Associations between self-reported sleep duration and sleeping disorder with concentrations of fasting and 2-h glucose, insulin, and glycosylated hemoglobin among adults without diagnosed diabetes. J Diabetes. 2014;6(4):338–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lecube A, et al. . Characterization of sleep breathing pattern in patients with Type 2 Diabetes: Sweet Sleep Study. PLoS One. 2015;10(3):doi: 10.1371/journal.pone.0119073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Daviglus ML, et al. . Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Patel SR, et al. . Social and health correlates of sleep duration in a US Hispanic Population: Results from the Hispanic Community Health Study/Study of Latinos. Sleep. 2015;38(10):1515–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cespedes EM, et al. . Joint associations of insomnia and sleep duration with prevalent diabetes: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL). J Diabetes. 2016;8(3):387–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Patel SR, et al. ; Osteoporotic Fractures in Men (MrOS); Study of Osteoporotic Fractures (SOF) Research Groups The association between sleep patterns and obesity in older adults. Int J Obes (Lond). 2014;38(9):1159–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Knutson KL, et al. . Association between sleep timing, obesity, diabetes: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) cohort study. SLEEP. 2017;40(4): doi: 10.1093/sleep/zsx014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wong K, et al. . The trajectories of sleep disturbances in Rett syndrome. J Sleep Res. 2015;24(2):223–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gilmour H, et al. . Longitudinal trajectories of sleep duration in the general population. Health Rep. 2013;24(11):14–20. [PubMed] [Google Scholar]
- 11. Chiu HY, et al. . Trajectories of sleep changes during the acute phase of traumatic brain injury: a 7-day actigraphy study. J Formos Med Assoc. 2013;112(9):545–553. [DOI] [PubMed] [Google Scholar]
- 12. vanSomeren EJW, et al. . Circadian rest-activity rhythm disturbance in Alzheimer’s disease. Biol Psychiatry. 1996;40(4):259–270. [DOI] [PubMed] [Google Scholar]
- 13. Zuurbier LA, et al. . Fragmentation and stability of circadian activity rhythms predict mortality: the Rotterdam study. Am J Epidemiol. 2015;181(1):54–63. [DOI] [PubMed] [Google Scholar]
- 14. Sorlie PD, et al. . Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20(8):629–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lavange LM, et al. . Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20(8):642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Patel SR, et al. . Reproducibility of a standardized actigraphy scoring algorithm for sleep in a US Hispanic/Latino population. Sleep. 2015;38(9):1497–1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ancoli-Israel S, et al. . The SBSM guide to actigraphy monitoring: clinical and research applications. Behav Sleep Med. 2015;13Suppl 1:S4–S38. [DOI] [PubMed] [Google Scholar]
- 18. Nagin D. Group-Based Modeling of Development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 19. Jones BL, et al. . A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods & Res. 2001;29(3):374–393. [Google Scholar]
- 20. Nagin DS, et al. . Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–138. [DOI] [PubMed] [Google Scholar]
- 21. Baron RM, et al. . The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. [DOI] [PubMed] [Google Scholar]
- 22. Valeri LVT. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS Macros. Psychol Methods. 2013;18(2):137–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Roenneberg T, et al. . Social jetlag and obesity. Curr Biol. 2012;22(10):939–943. [DOI] [PubMed] [Google Scholar]
- 24. Wittmann M, et al. . Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;23(1-2):497–509. [DOI] [PubMed] [Google Scholar]
- 25. Cao Z, et al. . The effects of midday nap duration on the risk of hypertension in a middle-aged and older Chinese population: a preliminary evidence from the Tongji-Dongfeng Cohort Study, China. J Hypertens. 2014;32(10):1993–8; discussion 1998. [DOI] [PubMed] [Google Scholar]
- 26. Hayashi M, et al. . The effects of a 20-min nap before post-lunch dip. Psychiatry Clin Neurosci. 1998;52(2):203–204. [DOI] [PubMed] [Google Scholar]
- 27. Tietzel AJ, et al. . The recuperative value of brief and ultra-brief naps on alertness and cognitive performance. J Sleep Res. 2002;11(3):213–218. [DOI] [PubMed] [Google Scholar]
- 28. Hyyppä MT, et al. . Quality of sleep during economic recession in Finland: a longitudinal cohort study. Soc Sci Med. 1997;45(5):731–738. [DOI] [PubMed] [Google Scholar]
- 29. Perales FPS. Losing ground, losing sleep: local economic conditions, economic vulnerability, and sleep. Soc Sci Res. 2017;62:189–203. [DOI] [PubMed] [Google Scholar]
- 30. Soltani M, et al. . Sleepless nights: the effect of socioeconomic status, physical activity, and lifestyle factors on sleep quality in a large cohort of Australian women. Arch Womens Ment Health. 2012;15(4):237–247. [DOI] [PubMed] [Google Scholar]
- 31. Ohayon MM, et al. . Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27(7):1255–1273. [DOI] [PubMed] [Google Scholar]
- 32. Ancoli-Israel S, et al. . The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26(3):342–392. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.