Abstract
We report the case of a patient with a spinal extradural arteriovenous fistula (AVF) associated with Cowden syndrome (CS) that was successfully treated by endovascular surgery. CS is an autosomal dominant disorder associated with diverse symptoms caused by a deleterious mutation in the phosphatase and tensin homolog (PTEN) gene. A 67-year-old woman was diagnosed with CS based on her medical history of multiple cancers for which she underwent abdominal surgery, macrocephaly, Lhermitte-Duclos disease, and facial papules. Her genetic testing demonstrated a PTEN mutation. She presented with progressive paraparesis and her MRI of the thoracolumbar spine showed the spinal cord edema along with flow voids. A spinal angiogram demonstrated a spinal extradural AVF with the perimedullary drainage. The AVF was successfully treated by endovascular surgery. The PTEN mutation can accelerate angiogenesis; thus, vascular anomalies are one of the diagnostic criteria of CS. However, only two cases of vascular anomalies involving the spinal cord in patients with CS have been reported previously. As the present case, both cases had a history of abdominal or retroperitoneal cancer. The PTEN mutation accompanied with abdominal surgery might have caused this vascular anomaly as the consequences of venous congestion around the thoracolumbar spine. A spinal extradural AVF should be considered in patients with CS who present with myelopathy, especially when the patient has a history of abdominal or retroperitoneal surgery. Regarding the treatment strategy, endovascular surgery should be considered because surgical insult could prompt secondary vascular anomalies resulting from neovascularization due to the PTEN mutation.
Keywords: central nervous system vascular anomalies, Cowden syndrome, Cowden disease, dural arteriovenous fistula, PTEN hamartoma tumor syndrome
Introduction
Cowden syndrome (CS) is a rare autosomal dominant disorder associated with multiple hamartomas and a high risk of the development of malignant tumors. The physical characteristics of the disorder are macrocephaly and pathognomonic mucocutaneous lesion, including trichilemmomas and papillomatous papules. Approximately 80% of patients with CS have a phosphatase and tensin homolog (PTEN) mutation.1) When a PTEN mutation is identified by genetic analysis, the patient is diagnosed with PTEN hamartoma tumor syndrome (PHTS). PHTS includes CS, Bannayan–Riley–Ruvalcaba syndrome (BRRS), Proteus syndrome, and Proteus-like syndrome.2)
Vascular anomalies, including arteriovenous malformations and cavernous malformations, have also been reported as symptoms of PHTS, particularly in patients with CS and BRRS.3) However, vascular anomalies involving the spinal cord are extremely rare. Herein, we report a case of a thoracolumbar spinal extradural arteriovenous fistula (AVF) in a patient with CS that was successfully treated by endovascular surgery.
Case Report
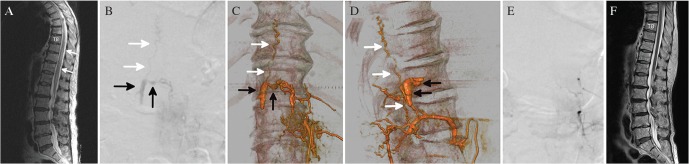
A 67-year-old woman presented with a chief complaint of progressive motor weakness of the lower extremities for the past 4 days and was referred to our emergency department. She had a medical history of macrocephaly, Lhermitte-Duclos disease in the left cerebellar hemisphere, and face trichilemmomas. Furthermore, she had also undergone surgery for breast cancer and advanced cecal cancer. Therefore, she had been clinically diagnosed with CS according to the National Comprehensive Cancer Network diagnostic criteria with direct sequencing of PTEN by polymerase chain reaction (PCR) revealing a missense mutation: p.G129V in exon 5. The neurologic examination demonstrated grade 1 spastic paraparesis in manual muscle testing (MMT) with sensory disturbances at the level of the seventh thoracic dermatome bilaterally. She had urinary incontinence upon admission. MRI of the thoracolumbar spine showed edema extending from T8 to the conus medullaris with flow voids along the dorsal side of the thoracic cord (Fig. 1A). A spinal angiogram (Artis zee BA Twin, Siemens, Munich, Germany) demonstrated a spinal extradural AVF with the perimedullary drainage. The fistula was supplied by the dorsal somatic branches from the bilateral L1 and left L2 segmental arteries, and they drained into the perimedullary vein via the right-sided epidural venous pouch (Figs. 1B–D). She underwent two-staged endovascular embolization. A microcatheter was successfully placed up to the distal part of the right L1 lumbar artery, and the shunt point as well as the venous pouch was completely embolized with 25% n-butyl-2-cyanoacrylate (Fig. 1E). Her symptoms gradually improved so that the motor examination of her lower extremities demonstrated grade 3 in MMT 30 days after the treatment. One year later, the fistula was not recanalized, and she was able to walk with a walker. An MRI of the thoracolumbar spine revealed resolution of the thoracic cord edema (Fig. 1F).
Fig. 1.
(A) A T2-weighted MRI of the thoracolumbar level showing intramedullary hyperintensity (white arrows) extending from T8 to the conus medullaris with some dorsal perimedullary flow voids. (B) Spinal DSA, the left L2 injection, showing a spinal extradural AVF with an extradural venous pouch (black arrows) that drained into the perimedullary vein (white arrows). (C) A 3D rotational DSA, the left L2 injection, anterio-posterior view, showing the ventral venous pouch (black arrows) was connected to the perimedullary vein (white arrows). (D) 3D-rotational DSA, left L2 injection, lateral view, showing the relationship between the vascular and bony structures. (E) Spinal DSA, left L2 injection, showing the fistula and perimedullary vein were completely obliterated. (F) Spinal MRI T2-weighted images, 1 year after embolization, showing the resolution of the thoracic cord edema. MRI: magnetic resonance imaging, DSA: digital subtraction angiography, 3D: three-dimensional.
Discussion
The International Consortium diagnostic criteria for CS were created in 1996 based on clinical experience and case reports from the literature.4) According to the initial diagnostic criteria, vascular anomalies were not included. While case reports regarding PHTS have increased, PHTS turned out to represent vascular anomalies. Since the diagnostic criteria for PHTS was revised in 2013, vascular anomalies have been included as the minor criteria.3) However, vascular anomalies of PHTS usually occur in the soft tissues and skin.5) We reported the case of a spinal extradural AVF in a patient with CS with a missense mutation: p.G129V in exon 5. As summarized in Table 1, only three cases of vascular anomaly involving the spinal cord in patients with CS have been reported previously.6,7) Various PTEN mutations were shown in these cases. In our case, a PCR-direct sequencing of PTEN revealed a missense mutation: p.G129V in exon 5. This mutation is classified into variant of uncertain significance in the diagnosis of FALCO biosystems (Kyoto, Japan). Missense mutations are usually hard to identify as either deleterious or as an uncertain significant variant. Yet, this mutation has been reported previously as deleterious,8) and an in silico analysis demonstrated that the mutation likely negatively impacted the protein (polyphen2, SIFT, and Align-GVGD). In addition, since exon 5 of the PTEN gene encodes the functional domain of the protein, mutations in this region may affect its phosphatase function.9) Although the PTEN gene is one of the most commonly mutated tumor suppressor genes in patients with cancer, PTEN mutations are also known to accelerate angiogenesis. The loss of PTEN functioning leads to overexpression of angiogenic factors such as vascular endothelial growth factor (VEGF).10) Therefore, the mutation was considered to elicit vascular anomalies with angiogenesis.
Table 1.
Reported cases of spinal dural or extradural AVF in a patient with Cowden syndrome
| Author | Age/Sex | AVF location | Fistula level | PTEN mutation/Locations | Past medical history | Symptoms and signs | Treatment | Outcome | Follow-up period |
|---|---|---|---|---|---|---|---|---|---|
| Wu et al.6) | 65/M | Spinal dural AVF | L3 | c.37A>T/Exon 1 | Prostate cancer | Lower limb weakness, dysesthesia, urinary retention | TAE | GR | 4 months |
| Barreras et al.7) | 57/F | Spinal extradural AVF | L2, L4 | Positive/Intron 3 | Nephrectomy | Lower extremities weakness, numbness | TAE | MD | 2 years |
| Present case | 67/F | Spinal extradural AVF | L1, L2 | p.G129V/Exon 5 | Ileocecal resection | Paraplegia | TAE | MD | 1 year |
AVF: arteriovenous fistula, F: female, GR: good recover, M: male, MD: moderate disability, TAE: transarterial embolization.
There was another factor of developing spinal extradural AVF in the present case. We speculated that spinal extradural AVFs tend to develop in patients with CS because of the venous congestion caused by abdominal surgery for associated malignant tumors. All reported cases had a history of cancers in the abdominal or retroperitoneal cavity accompanied with an extradural AVF at the lumber level. Murakami et al. described seven cases of a spinal extradural AVF with a history of surgery.11) Most secondary spinal extradural AVFs occurred after laminectomy. Meanwhile, there were two cases of spinal extradural AVFs following prostatectomy and resection of the abdominal aortic aneurysm. Thus, abdominal or retroperitoneal surgery might cause venous congestion around thoracolumbar spine, resulting in vascular anomalies particularly in patients with CS.
In terms of treatment strategy, Rangel-Castilla et al. classified spinal extradural AVFs into three types, of which type A was defined spinal extradural AVFs with the intradural venous drainage.12) The therapeutic goal for type A spinal extradural AVF is occlusion of the intradural perimedullary vein and the epidural venous pouch. In our case, we performed the endovascular surgery for the following reasons. First, the extradural AVF composed of a single perimedullary drainer. Second, considering the genetic background of excessive angiogenesis, such as the PTEN mutation, direct surgery might have caused secondary vascular anomalies by the surgical insult itself. Sadahiro et al. reported a case of secondary dural AVF that developed in the cerebellar surface, together with the thickened dura mater containing abnormal vessels after brainstem cavernous angioma surgery in a patient with CS. Immunohistochemical findings of the removed dura mater revealed that the abnormal vessels were diffusely positive for VEGF, which might have resulted in neovascularization of the dura mater.13) This fact may support our therapeutic strategy.
As mentioned above, patients with CS usually had surgical histories as a consequence of accompanied malignant cancers. A spinal extradural AVF could occur in patients with CS because of the abdominal venous congestion by surgical insults and the possibility of excessive neovascularization due to PTEN mutations. If type A spinal extradural AVF is found in patients with CS, endovascular surgery might have an advantage so as to avoid surgical insults.
Footnotes
Conflicts of Interest Disclosure
The authors have no conflicts of interest to declare.
References
- 1).Marsh DJ, Kum JB, Lunetta KL, et al. : PTEN mutation spectrum and genotype-phenotype correlations in Bannayan-Riley-Ruvalcaba syndrome suggest a single entity with Cowden syndrome. Hum Mol Genet 8: 1461–1472, 1999 [DOI] [PubMed] [Google Scholar]
- 2).Merks JH, de Vries LS, Zhou XP, et al. : PTEN hamartoma tumour syndrome: variability of an entity. J Med Genet 40: e111, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Pilarski R, Burt R, Kohlman W, Pho L, Shannon KM, Swisher E: Cowden syndrome and the PTEN hamartoma tumor syndrome: systematic review and revised diagnostic criteria. J Natl Cancer Inst 105: 1607–1616, 2013 [DOI] [PubMed] [Google Scholar]
- 4).Nelen MR, Padberg GW, Peeters EA, et al. : Localization of the gene for Cowden disease to chromosome 10q22-23. Nat Genet 13: 114–116, 1996 [DOI] [PubMed] [Google Scholar]
- 5).Tan WH, Baris HN, Burrows PE, et al. : The spectrum of vascular anomalies in patients with PTEN mutations: implications for diagnosis and management. J Med Genet 44: 594–602, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Wu TY, Willoughby E, Hutchinson DO, et al. : Congestive myeloradiculopathy in a patient with Cowden syndrome. J Clin Neurosci 22: 431–433, 2015 [DOI] [PubMed] [Google Scholar]
- 7).Barreras P, Gailloud P, Pardo CA: A longitudinally extensive myelopathy associated with multiple spinal arteriovenous fistulas in a patient with Cowden syndrome: a case report. Spine J 18: e1–e5, 2018 [DOI] [PubMed] [Google Scholar]
- 8).Pilarski R, Stephens JA, Noss R, Fisher JL, Prior TW: Predicting PTEN mutations: an evaluation of Cowden syndrome and Bannayan-Riley-Ruvalcaba syndrome clinical features. J Med Genet 48: 505–512, 2011 [DOI] [PubMed] [Google Scholar]
- 9).Konopka B, Paszko Z, Janiec-Jankowska A, Goluda M: Assessment of the quality and frequency of mutations occurrence in PTEN gene in endometrial carcinomas and hyperplasias. Cancer Lett 178: 43–51, 2002 [DOI] [PubMed] [Google Scholar]
- 10).Castellino RC, Muh CR, Durden DL: PI-3 kinase-PTEN signaling node: an intercept point for the control of angiogenesis. Curr Pharm Des 15: 380–388, 2009 [DOI] [PubMed] [Google Scholar]
- 11).Murakami T, Nakagawa I, Wada T, Kichikawa K, Nakase H: Lumbar spinal epidural arteriovenous fistula with perimedullary venous drainage after endoscopic lumbar surgery. Interv Neuroradiol 21: 249–254, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).Rangel-Castilla L, Holman PJ, Krishna C, Trask TW, Klucznik RP, Diaz OM: Spinal extradural arteriovenous fistulas: a clinical and radiological description of different types and their novel treatment with Onyx. J Neurosurg Spine 15: 541–549, 2011 [DOI] [PubMed] [Google Scholar]
- 13).Sadahiro H, Ishihara H, Goto H, et al. : Postoperative dural arteriovenous fistula in a patient with Cowden disease: a case report. J Stroke Cerebrovasc Dis 23: 572–575, 2014 [DOI] [PubMed] [Google Scholar]