Abstract
Objective:
To assess whether neighbourhood deprivation is associated with exposure to an antidepressant drug treatment (ADT) and its quality among individuals diagnosed with unipolar depression and insured by the Quebec public drug plan.
Method:
We conducted an administrative database cohort study of adults covered by the Quebec public drug plan who were diagnosed with a new episode of unipolar depression. We assessed material and social deprivation using an area-based index. We considered exposure to an ADT as having ≥1 claim for an ADT within the 365 days following depression diagnosis. Among those exposed to ADT, ADT quality was assessed with 3 indicators: first-line recommended ADT, persistence with the ADT, and compliance with the ADT. Generalized linear models were used to estimate adjusted prevalence ratios (aPR) and 95% confidence intervals (95% CI).
Results:
Of 100,432 individuals with unipolar depression, 65,436 (65%) were exposed to an ADT in the year following the diagnosis. Individuals living in the most materially deprived areas were slightly more likely to be exposed to an ADT than those living in the least deprived areas (aPR, 1.04; 95% CI, 1.03 to 1.06). The likelihoods of being exposed to a first-line ADT, persisting for the minimum recommended duration and complying with the ADT were independent of the deprivation levels.
Conclusions:
Neighbourhood deprivation was not associated with ADT quality among individuals insured by the Quebec public drug plan. It might be partly attributable to the public drug plan whose goal is to provide equitable access to prescription drugs regardless of income.
Keywords: depression, antidepressant agents, socioeconomic factors, residence characteristics, drug prescriptions, medication adherence, cohort studies, administrative databases
Abstract
Objectif :
Évaluer si la défavorisation du quartier de résidence est associée à l’exposition à un traitement médicamenteux antidépresseur (TMA) et à sa qualité parmi les personnes ayant reçu un diagnostic de dépression unipolaire et assurées par le régime public d’assurance médicaments du Québec.
Méthode :
À l’aide de bases de données administratives, nous avons mené une étude de cohorte incluant les adultes couverts par le régime public d’assurance médicaments du Québec ayant reçu un diagnostic de nouvel épisode de dépression unipolaire. Nous avons évalué le niveau de défavorisation matérielle et sociale du quartier de résidence à l’aide de l’indice développé par Pampalon et collègues. Nous avons défini l’exposition à un TMA comme avoir ≥ 1 réclamation pour un antidépresseur au cours des 365 jours suivant le diagnostic de dépression. Parmi les personnes exposées au TMA, la qualité du TMA a été évaluée par trois indicateurs : avoir un TMA recommandé en première intention selon les lignes directrices, la persistance avec le TMA pour la durée minimale recommandée et l’observance au TMA. Des modèles linéaires généralisés ont servi à estimer les rapports de prévalences ajustés (RPa) et les intervalles de confiance à 95 % (IC 95 %).
Résultats :
Parmi les 100 432 personnes souffrant de dépression unipolaire, 65 436 (65 %) ont été exposées à un TMA dans l’année suivant le diagnostic. Les personnes vivant dans les quartiers les plus défavorisés matériellement étaient légèrement plus susceptibles d’être exposées à un TMA que celles vivant dans les quartiers les moins défavorisés (RPa 1,04; IC 95 % 1,03 à 1,06). L'exposition à un TMA de première intention, la persistance pour la durée minimale recommandée et l'observance au TMA n'étaient pas associées au niveau de défavorisation.
Conclusions :
La défavorisation du quartier de résidence n’est pas associée à la qualité du TMA chez les personnes assurées par le régime public d’assurance médicaments du Québec. Ces résultats peuvent être attribuables en partie au régime public d’assurance médicaments dont le but est d’offrir un accès équitable aux médicaments prescrits sans égard au revenu.
In 2012, the proportion of individuals who had a major depressive episode was 4.7% and 4.4% in Canada and in Quebec, respectively, proportions similar to those observed in 2002.1,2 Depression is an important public health issue because of its negative impact on several aspects of the patient’s life,3,4 the associated increased suicide risk,3,5,6 and the direct and indirect costs that depression generates.7 Treatments for depression include the prescription of an antidepressant drug treatment (ADT) and psychotherapy.3
The prescription of ADT by providers and its use by patients are influenced by several factors,8–14 including indicators of deprivation. According to Townsend,15 there are 2 dimensions of deprivation: material, which involves the deprivation of goods and convenience, and social, which refers to relationships within the family and the community. For material deprivation, in some studies conducted in the general population, it has been observed that individuals with lower socioeconomic status (SES) or living in more deprived neighbourhoods were more likely than others to be exposed to an ADT,16–19 whereas the opposite has been reported in other studies.20–22 Among individuals with depression, some indicators of lower SES were also associated with a greater likelihood of ADT exposure23 or the opposite,24 and no association was found in a Canadian study using area-based deprivation indexes.25 To our knowledge, very few studies have considered ADT exposure and its use by patients with regards to indicators related to the social dimension of deprivation. However, it has been reported that patients with a mental illness having higher social support are more likely to seek general medical services26 and, in some studies, that marital status is associated with ADT adherence.27
Social inequalities regarding exposure to ADT and its quality may vary from one health care setting to another depending on the cost and terms of access to drug treatment. In the province of Quebec, all citizens are covered by a drug insurance plan. Quebecers whose employers do not offer a drug insurance group plan, those 65 years and older, and those receiving a guaranteed income supplement (GIS) or welfare are covered by the public drug insurance plan (Régime public d’assurance médicaments [RPAM]) administered by the Régie de l’assurance-maladie du Québec (RAMQ). The financial contribution requested from beneficiaries varies according to whether they receive partial or maximum GIS or welfare. For example, the maximum monthly contribution varies from $88.83 for those who do not receive a GIS or welfare to $0 for those who receive between 94% and 100% of the GIS or receive welfare.28
One of the objectives of the RPAM is to provide equitable access to prescription drugs to all beneficiaries, regardless of income.29 However, the association between deprivation and exposure to ADT and its quality was never evaluated in this context. We thus conducted a study among adults covered by the RPAM who were diagnosed with a new episode of unipolar depression, to assess the association between neighbourhood material and social deprivation and 1) exposure to an ADT during the first year after the diagnosis of depression, 2) exposure to a guideline-recommended first-line antidepressant, 3) persistence with the ADT for the 240-day recommended minimum treatment duration, and 4) compliance with the ADT.
Method
Study Design and Data Source
We conducted a cohort study of individuals aged 18 years or more who were insured by the RPAM who were diagnosed with a new episode of unipolar depression. The following RAMQ databases were used: 1) the demographic database, including information on the beneficiaries (sex, age, welfare or GIS status, and residency area); 2) the physician claims database, including information on ambulatory visits (date and diagnosis); 3) the drug claims database, including information on all prescriptions claimed (drug identity, dispensing date, number of days supply, and prescriber’s specialty); and 4) the hospitalization database, including information on hospitalizations (date, primary diagnosis, and secondary diagnoses). For each individual, RAMQ provided the material and social neighbourhood deprivation levels based on the dissemination area (DA) of residence on the date of the depression diagnosis.
Study Population
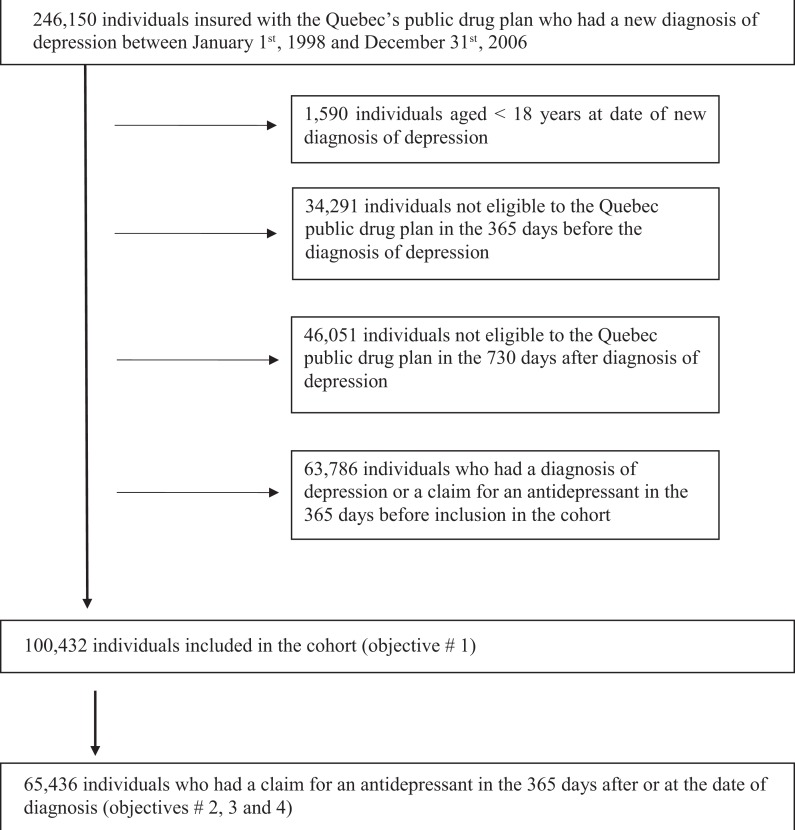
We included individuals who, between 1 January 1998 and 31 December 2006, had an in-patient diagnosis of unipolar depression (International Classification of Diseases-9 [ICD-9] codes 300.4, 311; or ICD-10 codes F32, F33, F34.1). We also included individuals with an ambulatory diagnosis of unipolar depression if this diagnosis was followed by at least one other diagnosis of unipolar depression (either in-patient or ambulatory) within the following 365 days. A similar procedure has also been done in the past to increase the specificity of case selection.25,30,31 Individuals were considered to have been diagnosed for a new episode of depression on the date of the first encountered depression diagnosis. To include only individuals who had a new episode of depression, we excluded those who had a diagnosis code for depression or had claimed an antidepressant in the 365-day look-back period prior to the date of diagnosis. We also excluded individuals not insured by the RPAM for the entire 365-day and 730-day periods preceding and following the depression diagnosis, respectively.
Variables
Material and Social Deprivation Index
We used the neighbourhood deprivation index developed by Pampalon and Raymond.32 No individual socioeconomic data are available in Quebec administrative databases, and this index was developed and integrated in numerous administrative databases such as those of the RAMQ to allow for the exploration of social inequalities.33 Based on the Canadian census data, this index is assigned to each DA. The DA is the smallest area for which it is possible to obtain census data (400-700 individuals), and each DA corresponds to a postal code. This deprivation index has 2 separate dimensions: material and social. Each DA material dimension is calculated using the following neighbourhood indicators: the proportion of persons without a high school degree, the ratio of employed persons to the total population, and the average personal income. The indicators used to calculate the social dimension are as follows: the proportion of persons separated, divorced, or widowed; the proportion of people living alone; and the proportion of single-parent families. Each DA is classified according to its score for the material and social dimensions, from the least deprived to the most deprived. The DAs are then separated into quintiles. A level of deprivation ranging from 1 (least deprived) to 5 (most deprived) is attributed to each DA for both the material and the social dimensions. This deprivation index is widely used,34–36 and evidence supports its temporal stability and predictive validity.32,33 This index also correlates with SES measured at an individual level.33
Exposure and Quality of Antidepressant Drug Treatment
We considered all individuals having 1 or more claims for any antidepressant in the 365 days following the date of the depression diagnosis as exposed to an ADT. We assessed the quality of the ADT among the exposed individuals using 3 quality indicators defined based on the Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines published in 2001, 2009, and 2016.3,37–41 For the quality indicators we used, recommendations remained the same across these different editions. We considered individuals as exposed to a first-line recommended ADT if the antidepressant claimed was among those recommended as first-line agents in the guidelines.39–41 If more than 1 antidepressant was initiated, individuals were not considered exposed to a first-line ADT. Next, persistence with treatment—which entails taking the medication for the recommended length of time42–45—was measured using the treatment anniversary method.42 According to the CANMAT guidelines, the treatment duration for an episode of depression includes an acute phase of 8 to 12 weeks (56-84 days) and a maintenance phase of 6 to 24 months (183-730 days).3,37–41 We then considered individuals as persistent with treatment if they were still on ADT 240 days after initiation. Individuals were categorized as persistent if the most recent dispensing of the drug before the 240th anniversary day of treatment initiation included a supply of antidepressants that was sufficient enough to be covered on that 240th day. To allow for a reasonable refill gap, individuals who had a supply of antidepressants sufficient to be covered between the 195th and 240th day were also considered as persistent. Compliance with the ADT—which entails taking the medication in accordance with the prescribed dosage, timing, and frequency42–44—was measured among persistent individuals using the proportion of days covered.42 Individuals who were supplied antidepressants to cover at least 80% of the days in the 240-day period following ADT initiation were considered compliant.
Covariables
Many variables were considered as potential confounders, depending of the outcome of interest: sex; age at depression diagnosis (10-year categories); calendar year of the depression diagnosis to control for the fact that subjects were included in the study over a period of 8 years; specialty of the physician who prescribed the initial ADT (general practitioner, psychiatrist, or other), since specialty could be related to ADT prescription; and the initial type of ADT regimen (monotherapy or combined therapy), because this could be related to persistence and compliance. We also adjusted for residency area, as defined by Statistics Canada (Montreal metropolitan region area, other metropolitan areas [>100,000 inhabitants], towns of 10,000-100,000 inhabitants, and rural and small-town areas [<10,000 inhabitants])46 as recommended by the developers of the deprivation index because deprivation levels are more variable in DA covering small cities and rural areas than those in urban areas.33,47
Statistical Analyses
We assessed the effects of the material and social deprivation levels on exposure to the ADT and on each of the quality indicators by calculating the prevalence ratios (PR) and their 95% confidence intervals (95% CI) using a generalized linear model with a Poisson working model.48 Model-robust variances were computed with sandwich estimators to account for the larger variance of Poisson variables compared with the binomial variables.49 We first evaluated the effect of material and social deprivation independently. We then adjusted the PRs for sex, age, residency area, and calendar year at diagnosis of depression. For all analyses related to the quality of the ADT, we adjusted for the initial ADT regimen and for the specialty of the physician who prescribed it. For the analyses pertaining to persistence and compliance, whether the antidepressant was a first-line recommended treatment or not was added to the models. For adjusted models, when the effect of material deprivation was assessed, the model was adjusted for social deprivation and conversely. We tested the final models for collinearity using variance inflation factor tests.50,51
Since the deprivation index is an area-based index, we tested the sensitivity of our results using the sole SES indicator measured at an individual level available in the RPAM database instead of the neighbourhood deprivation index. This indicator describes the status of the individuals covered by the RPAM as follows: receiving GIS (partial or maximum), receiving welfare, or not receiving these types of financial support. Compared with the material and social dimensions of the deprivation index, the RPAM beneficiary status does not capture a large range of socioeconomic variations and does not take into account social deprivation, but it allows identification of individuals with the most precarious socioeconomic situations.
The Commission d’accès à l’information du Québec authorized access to the data. This study was approved by the ethics boards of the Centre Hospitalier Universitaire (CHU) de Québec–Université Laval and the CHU de Sherbrooke.
Results
A total of 100,432 individuals were included in the cohort (Figure 1). Their characteristics are presented in Table 1. Regarding material deprivation, 14,760 (14.7%) individuals were living in the least deprived areas, while 24,427 (24.3%) were living in the most deprived areas. For social deprivation, 14,107 (14.0%) individuals were living in the least deprived areas, and 27,637 (27.5%) individuals were living in the most deprived areas.
Figure 1.
Selection of study population.
Table 1.
Characteristics of the 100,432 individuals with a new diagnosis of depression and the 65,436 of those individuals who claimed an antidepressant in the 365 days after diagnosisa.
| Characteristics | Individuals with new diagnosis of depression | Individuals with new diagnosis of depression who claimed an antidepressant |
|---|---|---|
| Sociodemographic characteristics | ||
| Sex | ||
| Female | 65,440 (65.2) | 44,254 (67.6) |
| Male | 34,992 (34.8) | 21,182 (32.4) |
| Age at diagnosis | ||
| 18-24 years | 7258 (7.2) | 4397 (6.7) |
| 25-34 years | 15,380 (15.3) | 9315 (14.2) |
| 35-44 years | 19,282 (19.2) | 12,110 (18.5) |
| 45-54 years | 16,646 (16.6) | 10,780 (16.5) |
| 55-64 years | 12,958 (12.9) | 8756 (13.4) |
| 65-74 years | 16,007 (15.9) | 11,024 (16.9) |
| ≥75 years | 12,901 (12.9) | 9054 (13.8) |
| Mean (SD) | 50.9 (18.5) | 51.9 (18.5) |
| Residency area at diagnosis of depression | ||
| Montreal Census Metropolitan area | 46,975 (46.8) | 28,389 (43.4) |
| Other Metropolitan Census areas (>100,000 inhabitants) | 18,397 (18.3) | 12,470 (19.1) |
| Agglomerations of 10,000-100,000 inhabitants | 12,304 (12.2) | 8509 (13.0) |
| Small towns and rural areas (<10,000 inhabitants) | 21,750 (21.7) | 15,461 (23.6) |
| Not available | 1006 (1.0) | 607 (0.9) |
| Guaranteed income supplement (GIS) | ||
| No | 60,077 (59.8) | 39,447 (60.3) |
| Partial | 12,677 (12.6) | 8939 (13.7) |
| Maximum | 27,678 (27.6) | 17,050 (26.0) |
| Deprivation level—material | ||
| Quintile 1 | 14,760 (14.7) | 9086 (13.9) |
| Quintile 2 | 16,192 (16.1) | 10,308 (15.8) |
| Quintile 3 | 19,078 (19.0) | 12,563 (19.2) |
| Quintile 4 | 21,836 (21.8) | 14,408 (22.0) |
| Quintile 5 | 24,427 (24.3) | 16,451 (25.1) |
| Missing | 4139 (4.1) | 2620 (4.0) |
| Deprivation level—social | ||
| Quintile 1 | 14,107 (14.0) | 9555 (14.6) |
| Quintile 2 | 15,738 (15.7) | 10,711 (16.4) |
| Quintile 3 | 17,372 (17.3) | 11,521 (17.6) |
| Quintile 4 | 21,439 (21.4) | 13,725 (21.0) |
| Quintile 5 | 27,637 (27.5) | 17,304 (26.4) |
| Missing | 4139 (4.1) | 2620 (4.0) |
| Medical and treatment characteristics | ||
| Specialty of physician who made the diagnosis | ||
| General practitioner | 78,676 (78.3) | 55,354 (84.6) |
| Psychiatrist | 13,983 (13.9) | 5853 (8.9) |
| Other or not available | 7773 (7.8) | 4229 (6.5) |
| Specialty of physician who prescribed the initial antidepressant | ||
| General practitioner | N/A | 55,797 (85.3) |
| Psychiatrist | N/A | 7104 (10.8) |
| Other or not available | N/A | 2535 (3.9) |
| Therapeutic scheme at antidepressant initiation | ||
| Monotherapy | N/A | 58,448 (89.3) |
| Polytherapy | N/A | 6988 (10.7) |
N/A = not applicable.
aValues are expressed as n (%) except for the mean (SD) of age.
A total of 65,436 individuals (65.2%) were exposed to an ADT in the 365 days after the depression diagnosis. Their characteristics are presented in Table 1. Individuals living in the most materially deprived areas were slightly more likely to be exposed to an ADT compared with those living in the least materially deprived areas (adjusted PR [aPR], 1.04; 95% CI, 1.03 to 1.06) (Table 2). By contrast, individuals living in the most socially deprived areas were slightly less likely to be exposed to an ADT (aPR, 0.96; 95% CI, 0.94 to 0.97).
Table 2.
Likelihood of being exposed to an antidepressant in the 365 days after the depression diagnosis and, among exposed individuals, likelihood to be exposed to a first-line guideline-recommended antidepressant, according to material and social neighbourhood deprivation levels.
| Exposure to an antidepressant in the 365 days after diagnosis in the 100,432 study individualsd | Exposure to a first-line guideline-recommended antidepressant among the 65,436 individuals exposed to an antidepressante | |||||
|---|---|---|---|---|---|---|
| Deprivation level | %a | Crude PR (95% CI) | Adjustedb PR (95% CI) | %a | Crude PR (95% CI) | Adjustedc PR (95% CI) |
| Material | ||||||
| Quintile 1 | 61.6 | 1.00 | 1.00 | 88.4 | 1.00 | 1.00 |
| Quintile 2 | 63.7 | 1.03 (1.02-1.05) | 1.02 (1.00-1.04) | 88.9 | 1.01 (1.00-1.02) | 1.00 (0.99-1.01) |
| Quintile 3 | 65.9 | 1.07 (1.05-1.09) | 1.04 (1.02-1.06) | 89.5 | 1.01 (1.00-1.02) | 1.00 (0.99-1.01) |
| Quintile 4 | 66.0 | 1.07 (1.06-1.09) | 1.04 (1.02-1.05) | 88.9 | 1.01 (1.00-1.01) | 0.99 (0.98-1.00) |
| Quintile 5 | 67.4 | 1.09 (1.08-1.11) | 1.04 (1.03-1.06) | 88.9 | 1.01 (1.00-1.01) | 0.99 (0.98-1.00) |
| Social | ||||||
| Quintile 1 | 67.7 | 1.00 | 1.00 | 89.7 | 1.00 | 1.00 |
| Quintile 2 | 68.1 | 1.00 (0.99-1.02) | 1.00 (0.99-1.02) | 89.7 | 1.00 (0.99-1.01) | 1.00 (0.99-1.01) |
| Quintile 3 | 66.3 | 0.98 (0.96-0.99) | 0.98 (0.97-1.00) | 89.2 | 0.99 (0.99-1.00) | 1.00 (0.99-1.01) |
| Quintile 4 | 64.0 | 0.95 (0.93-0.96) | 0.97 (0.95- 0.98) | 89.0 | 0.99 (0.98-1.00) | 1.00 (0.99-1.01) |
| Quintile 5 | 62.6 | 0.92 (0.91-0.94) | 0.96 (0.94-0.97) | 87.8 | 0.98 (0.97-0.99) | 0.99 (0.98-1.00) |
CI = confidence interval; PR = prevalence ratio.
aPercentages of exposed individuals in each quintile.
bAdjusted models for exposure to an antidepressant in the 365 days after depression diagnosis included sex, age, residency area, and year of diagnosis. The model assessing the effect of material deprivation was adjusted for social deprivation, whereas the model assessing the effect of social deprivation was adjusted for material deprivation.
cAdjusted models for exposure to a first-line guideline-recommended antidepressant included sex, age, residency area, year of diagnosis, and specialty of physician who prescribed the initial antidepressant. The model assessing the effect of material deprivation was adjusted for social deprivation, whereas the model assessing the effect of social deprivation was adjusted for material deprivation.
dInformation on deprivation level not available for 4139 individuals.
eInformation on deprivation level not available for 2620 individuals.
Among the 65,436 individuals exposed to an ADT, 58,187 (88.9%) were exposed to a first-line guideline-recommended antidepressant (Table 2). The level of material and social deprivation was not statistically associated with the likelihood of being exposed to a first-line guideline-recommended ADT. Among the 65,436 individuals who initiated an ADT, 35,344 (54.0%) persisted with the ADT for the recommended minimum duration, and among them, 26,304 (74.4%) were compliant. Neither the level of material nor social neighbourhood deprivation was associated with persistence and compliance (Table 3).
Table 3.
Likelihood of persistence with antidepressant drug treatment (ADT) 240 days after initiation and, among persistent individuals, likelihood of compliance with ADT, according to material and social neighbourhood deprivation levels.
| Persistence with ADT 240 days after initiation (n = 65,436)c | Compliance with ADT (≥80% of days covered) among the 35,344 individuals who were persistentd | |||||
|---|---|---|---|---|---|---|
| Deprivation level | %a | Crude PR (95% CI) | Adjustedb PR (95% CI) | %a | Crude PR (95% CI) | Adjustedb PR (95% CI) |
| Material | ||||||
| Quintile 1 | 54.6 | 1.00 | 1.00 | 74.5 | 1.00 | 1.00 |
| Quintile 2 | 55.2 | 1.01 (0.99-1.04) | 1.01 (0.98-1.03) | 75.0 | 1.01 (0.98-1.03) | 1.00 (0.98-1.02) |
| Quintile 3 | 54.4 | 1.00 (0.97-1.02) | 1.00 (0.97-1.02) | 74.4 | 1.00 (0.98-1.02) | 0.99 (0.97-1.01) |
| Quintile 4 | 52.9 | 0.97 (0.95-0.99) | 0.97 (0.95-1.00) | 73.9 | 0.99 (0.97-1.01) | 0.98 (0.96-1.00) |
| Quintile 5 | 53.4 | 0.98 (0.96-1.00) | 0.98 (0.96-1.01) | 74.0 | 0.99 (0.97–1.01) | 0.98 (0.96-1.00) |
| Social | ||||||
| Quintile 1 | 55.3 | 1.00 | 1.00 | 75.7 | 1.00 | 1.00 |
| Quintile 2 | 54.4 | 0.98 (0.96-1.01) | 0.99 (0.96-1.01) | 74.7 | 0.99 (0.97-1.01) | 0.98 (0.96-1.00) |
| Quintile 3 | 53.9 | 0.98 (0.95-1.00) | 0.98 (0.95-1.00) | 75.0 | 0.99 (0.97-1.01) | 0.99 (0.97-1.00) |
| Quintile 4 | 53.7 | 0.97 (0.95-1.00) | 0.98 (0.96-1.01) | 73.8 | 0.98 (0.96-1.00) | 0.98 (0.96-1.00) |
| Quintile 5 | 53.2 | 0.96 (0.94-0.98) | 0.99 (0.96–1.01) | 73.2 | 0.97 (0.95-0.99) | 0.98 (0.96-1.00) |
aPercentages of exposed individuals in each quintile.
bAdjusted models included sex, age, residency area, year of diagnosis, specialty of physician who prescribed the initial antidepressant, therapeutic scheme at initiation (monotherapy/polytherapy), and first-line guideline-recommended antidepressant (yes/no). The model assessing the effect of material deprivation was adjusted for social deprivation, whereas the model assessing the effect of social deprivation was adjusted for material deprivation.
cInformation on deprivation level not available for 2620 individuals.
dInformation on deprivation level not available for 1462 individuals.
When we used SES at the individual level using the RPAM beneficiary status instead of the neighbourhood deprivation index, aPRs remained similar: that is, close to 1.00 (aPRs ranging from 0.96 to 1.02). However, individuals receiving maximum GIS or welfare (i.e., those expected to be the most materially deprived) were slightly less likely to be exposed to an ADT (aPR, 0.96; 95% CI, 0.95 to 0.97) and to receive a first-line guideline-recommended ADT (aPR, 0.97; 95% CI, 0.97 to 0.98) compared with those not receiving GIS.
Discussion
We did not observe socioeconomic inequalities regarding ADT among individuals covered by the RPAM and diagnosed with a new episode of depression when we used a neighbourhood deprivation index. The likelihood of being exposed to a first-line antidepressant, to persist for the recommended duration, and to comply with the ADT was independent of the material and social neighbourhood deprivation levels. Our results suggest that individuals living in the most materially deprived areas were slightly more likely to be exposed to an ADT than those living in the least deprived areas.
To our knowledge, this study is the first to explore the association between neighbourhood deprivation and ADT exposure and quality among individuals treated for depression in a Canadian setting. In a prior database study of individuals with prevalent mood disorders including bipolar depression, it was observed that variation in exposure to antidepressants was minimal across different levels of neighbourhood deprivation.25 For individuals diagnosed with a new episode of unipolar depression, we observed a 4% increase in the likelihood of exposure to an ADT for those living in the most materially deprived areas as opposed to those living in the least materially deprived ones. This result was not expected. The clinical relevance of this slight increase is unknown. This result is similar to that observed in a study conducted among 4493 Australians where the use of ADT, which is subsidised in this country for the most deprived individuals, was higher among those with lower SES measured at an individual level.23 Based on these results and others showing that lower SES was also associated with higher use of other subsidised care (e.g., general practitioner consultations) but inversely associated with use of nonsubsidised complementary medicines, the authors concluded that the more prevalent use of ADT among the most deprived individuals may be due to the social safety net. The same explanation may apply to our context where the most deprived individuals are those who pay the least for their medication due to the public drug plan copayment modalities. This result may also be the consequence of the lower cost for drug therapy compared with the cost of psychotherapy, another guideline-recommended treatment for mild to moderate depression. However, we were not able to assess whether psychotherapy was the case because in the Province of Quebec, therapies from psychologists are not covered by the public health plan and thus are not captured in the RAMQ databases. Further research is needed to explore whether the slightly increased likelihood of exposure to ADT for individuals living in the most materially deprived areas can be explained by a lesser likelihood of exposure to psychotherapy.
Our results also suggest that selection of the antidepressant prescribed to and initiated by patients is not guided by socioeconomic factors. Indeed, 89% of the individuals exposed to an ADT used a recommended first-line ADT, which was very similar to the 88% observed in a population-based study conducted in Denmark, where the drug plan was public.52 In the Danish study, such an exposure was not associated with indicators of socioeconomic status measured at the individual level.18 However, in a study conducted in France among the general population,53 where all individuals are also publicly insured for prescription drugs, it was observed that individuals with a very low income (those who do not incur out-of-pocket costs) were more likely than others to receive a tricyclic ADT, a class of antidepressants that is not recommended as a first-line treatment for depression. The discrepancy between our results and those observed in the latter study suggests that factors other than those related to the drug plan may play a role.
Our results are in line with those of other studies in which the proportion of individuals persisting and/or complying with ADT was low.52–59 Indeed, only 40% of individuals who initiated an ADT were both persistent and compliant. This proportion is lower than what has been observed in the province of Quebec for the treatment of chronic diseases such as schizophrenia (∼50%)60,61 and diabetes (62%).62 This result suggests that strategies to optimize adherence to the ADT should be prioritized, particularly in the primary care settings, where ADT is mainly prescribed.
Neither persistence nor compliance with ADT was associated with material and social neighbourhood deprivation in our study. Moreover, in a study conducted in the United States among 177,469 adults with depression, other authors observed that patient neighbourhood incomes were not a significant predictor of early discontinuation defined as not claiming an antidepressant in the 180 days after initiation.10 This is in line with a study of individuals with schizophrenia who were also insured by the RPAM, in which the proportion of those exposed to antipsychotics for at least 80% of the days during the expected 2-year treatment was not different between individuals living in the most deprived areas and those living in the least deprived ones.63 On the contrary, in a Danish study that included individuals insured by a public drug plan, individuals with lower SES were more likely to discontinue their ADT in the 6 months after its prescription—defined as not claiming the ADT in the 6 months after its first prescription.52 Some of the differences observed across studies10,52,54–58 might be explained by differences in the measure of deprivation used (i.e., individual vs. neighbourhood), in the drug insurance systems, and in how persistence, compliance, and deprivation are defined.
Our study has strengths. First, it is a population-based study since all individuals who were diagnosed with a new episode of depression and insured by the RPAM were included in the study. Second, we used measures of neighbourhood deprivation that separately took into account both dimensions of deprivation—material and social. Third, to assess the quality of ADT, we built 3 indicators based on guidelines for depression.3,37–41 Fourth, to our knowledge, this is the first study of the association between neighbourhood deprivation and ADT adherence that distinguishes between persistence and compliance, which are 2 distinct components of adherence behaviour that may not be necessarily influenced by the same determinants.42,44
This study also has limitations. Because the deprivation index is based on the area of residency, it may not reflect the exact deprivation level of some individuals. However, this index was developed using census data for the smallest geographical area for which it was possible to obtain these data and that contained a relatively homogenous population of residents.33 In addition, except for the slight differences reported above, our results were not sensitive to changes in the method for measuring SES (individual vs. geographically based deprivation index). The slight differences observed indicate that research taking into account both individual socioeconomic factors and the neighbourhood environment is still needed to deepen our understanding of the mechanisms linking deprivation and exposure to ADT. Furthermore, some limitations were inherent to the use of administrative data. For example, the RAMQ databases did not include clinical information, such as the severity of the depression, that could have helped to better characterize the quality of ADT. The RAMQ databases contained only the prescriptions that were dispensed by the pharmacists. Therefore, it was not possible to determine whether the lack of exposure to ADT was due to suboptimal prescribing or to primary nonadherence. In a study conducted in the United States using e-prescribing and pharmacy dispensing data, 29.5% of new antidepressant prescriptions were not filled.64 In addition, since we did not have information on the treatment duration planned by the prescribing physician, it was not possible to determine whether early discontinuation was due to a suboptimal duration of treatment determined by the physician or to the patient’s decision. Moreover, we had to assume that antidepressants claimed were indeed taken by the individuals. Therefore, we may have overestimated the proportion of individuals who were persistent and compliant with ADT. Finally, we used a dataset covering the period between 1998 and 2006. It is unknown to what extent the situation described during those years would still apply today. However, the RPAM access and copayment modalities have not changed since, and the annual prevalence of major depressive episodes in Canada has remained unchanged in the last decade.1 Recommendations regarding guideline-recommended first-line antidepressants and the minimum duration of treatment have also remained unchanged across the Canadian guidelines published in 2001, 2009, and 2016.3,37–41
Conclusions
Among individuals covered by the RPAM, we did not observe socioeconomic inequalities regarding exposure to an ADT and its quality using neighbourhood deprivation. These results suggest that the provincial drug plan might be achieving its goal of providing equal access to prescription drugs independently of income, at least among those covered by the RPAM. Finally, these results underline that suboptimal persistence and compliance are important challenges in this population.
Supplementary Material
Acknowledgments
The authors thank Josiane Courteau, PhD, for data management and Éric Demers, MSc, for his assistance with the statistical analyses.
Footnotes
Contributors: Jocelyne Moisan, Alain Vanasse, Alain Lesage, Marie-Josée Fleury, and Jean-Pierre Grégoire contributed to the acquisition of the data. Sophie Lauzier, Hichem Kadachi, and Jean-Pierre Grégoire contributed to the design and analyses. Sophie Lauzier, Hichem Kadachi, and Jean-Pierre Grégoire prepared the manuscript. All authors contributed to the interpretation of the results, critically revised the manuscript, and provided final approval of the manuscript submitted for publication.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: S. Lauzier received salary support from the Chair on Adherence to Treatments, Université Laval, during the study period. The Chair on Adherence to Treatments was funded through unrestricted grants from AstraZeneca Canada, Merck Canada, Pfizer Canada, Sanofi Canada, and the Prends soin de toi Program. H. Kadachi received a scholarship from the Chair on adherence to treatments, Université Laval, and from the Fonds pour l’enseignement et la recherche, Faculty of Pharmacy, Université Laval.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by an unrestricted grant from the Prends soin de toi Program (a peer-reviewed multistakeholder [AstraZeneca, Lilly, Lundbeck, and Merck] research funding program in mental health). S. Lauzier received a career research award from Fonds de recherche du Québec–Santé in partnership with the Institut national d’excellence en santé et en services sociaux (INESSS).
References
- 1. Patten SB, Williams JV, Lavorato DH, et al. Major depression in Canada: what has changed over the past 10 years? Can J Psychiatry. 2016;61(2):80–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baraldi A, Joubert K, Bordeleau M. Portrait statistique de la santé mentale Québécois. Résultats de L’enquête Sur La Santé Dans Les Collectivités Canadiennes—Santé Mentale 2012. Québec: Institut de la Statistique du Québec; 2015. [Google Scholar]
- 3. Lam RW, McIntosh D, Wang J, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder, section 1: disease burden and principles of care. Can J Psychiatry. 2016;61(9):510–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10(11):e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Patten SB, Williams JV, Lavorato DH, et al. Descriptive epidemiology of major depressive disorder in Canada in 2012. Can J Psychiatry. 2015;60(1):23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Holma KM, Melartin TK, Haukka J, et al. Incidence and predictors of suicide attempts in DSM-IV major depressive disorder: a five-year prospective study. Am J Psychiatry. 2010;167(7):801–808. [DOI] [PubMed] [Google Scholar]
- 7. Greenberg PE, Fournier AA, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76(2):155–162. [DOI] [PubMed] [Google Scholar]
- 8. Lin HC, Erickson SR, Balkrishnan R. Physician prescribing patterns of innovative antidepressants in the United States: the case of MDD patients 1993-2007. Int J Psychiatry Med. 2011;42(4):353–368. [DOI] [PubMed] [Google Scholar]
- 9. Lawrence RE, Rasinski KA, Yoon JD, et al. Physician race and treatment preferences for depression, anxiety, and medically unexplained symptoms. Ethn Health. 2015;20(4):354–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rossom RC, Shortreed S, Coleman KJ, et al. Antidepressant adherence across diverse populations and healthcare settings. Depress Anxiety. 2016;33(8):765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bushnell GA, Sturmer T, White A, et al. Predicting persistence to antidepressant treatment in administrative claims data: considering the influence of refill delays and prior persistence on other medications. J Affect Disord. 2016;196:138–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jaffray M, Cardy AH, Reid IC, et al. Why do patients discontinue antidepressant therapy early? A qualitative study. Eur J Gen Pract. 2014;20(3):167–173. [DOI] [PubMed] [Google Scholar]
- 13. Aikens JE, Nease DE, Jr, Nau DP, et al. Adherence to maintenance-phase antidepressant medication as a function of patient beliefs about medication. Ann Fam Med. 2005;3(1):23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rivero-Santana A, Perestelo-Perez L, Perez-Ramos J, et al. Sociodemographic and clinical predictors of compliance with antidepressants for depressive disorders: systematic review of observational studies. Patient Prefer Adherence. 2013;7:151–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Townsend P. Deprivation. J Soc Pol. 1987;16:125–146. [Google Scholar]
- 16. von Soest T, Bramness JG, Pedersen W, et al. The relationship between socio-economic status and antidepressant prescription: a longitudinal survey and register study of young adults. Epidemiol Psychiatr Sci. 2012;21(1):87–95. [DOI] [PubMed] [Google Scholar]
- 17. Raymond CB, Morgan SG, Caetano PA. Antidepressant utilization in British Columbia from 1996 to 2004: increasing prevalence but not incidence. Psychiatr Serv. 2007;58(1):79–84. [DOI] [PubMed] [Google Scholar]
- 18. Hansen DG, Sondergaard J, Vach W, et al. Socio-economic inequalities in first-time use of antidepressants: a population-based study. Eur J Clin Pharmacol. 2004;60(1):51–55. [DOI] [PubMed] [Google Scholar]
- 19. Crump C, Sundquist K, Sundquist J, et al. Neighborhood deprivation and psychiatric medication prescription: a Swedish national multilevel study. Ann Epidemiol. 2011;21(4):231–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bocquier A, Cortaredona S, Verdoux H, et al. Social inequalities in new antidepressant treatment: a study at the individual and neighborhood levels. Ann Epidemiol. 2013;23(3):99–105. [DOI] [PubMed] [Google Scholar]
- 21. Kivimaki M, Gunnell D, Lawlor DA, et al. Social inequalities in antidepressant treatment and mortality: a longitudinal register study. Psychol Med. 2007;37(3):373–382. [DOI] [PubMed] [Google Scholar]
- 22. Andersen I, Thielen K, Nygaard E, et al. Social inequality in the prevalence of depressive disorders. J Epidemiol Community Health. 2009;63(7):575–581. [DOI] [PubMed] [Google Scholar]
- 23. Butterworth P, Olesen SC, Leach LS. Socioeconomic differences in antidepressant use in the PATH Through Life Study: evidence of health inequalities, prescribing bias, or an effective social safety net? J Affect Disord. 2013;149(1-3):75–83. [DOI] [PubMed] [Google Scholar]
- 24. Young AS, Klap R, Sherbourne CD, et al. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58(1):55–61. [DOI] [PubMed] [Google Scholar]
- 25. Vanasse A, Courteau J, Lesage A, et al. [Health inequities in mood disorders based on material and social deprivation in dwelling sectors]. Can J Psychiatry. 2012;57(12):772–781. [DOI] [PubMed] [Google Scholar]
- 26. Maulik PK, Eaton WW, Bradshaw CP. The role of social network and support in mental health service use: findings from the Baltimore ECA study. Psychiatr Serv. 2009;60(9):1222–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bull SA, Hu XH, Hunkeler EM, et al. Discontinuation of use and switching of antidepressants: influence of patient-physician communication. JAMA. 2002;288(11):1403–1409. [DOI] [PubMed] [Google Scholar]
- 28.Amount to pay for prescription drugs, author. http://www.ramq.gouv.qc.ca/en/citizens/prescription-drug-insurance/Pages/amount-to-pay-prescription-drugs.aspx [cited 2017 July 14]. Available from:
- 29.Québec prescription drug insurance, author. http://www.ramq.gouv.qc.ca/en/citizens/prescription-drug-insurance/Pages/prescription-drug-insurance.aspx [cited 2017 July 14]. Available from:
- 30. Alaghehbandan R, Macdonald D, Barrett B, et al. Using administrative databases in the surveillance of depressive disorders—case definitions. Popul Health Manag. 2012;15(6):372–380. [DOI] [PubMed] [Google Scholar]
- 31. Spettell CM, Wall TC, Allison J, et al. Identifying physician-recognized depression from administrative data: consequences for quality measurement. Health Serv Res. 2003;38(4):1081–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pampalon R, Raymond G. Un Indice de Défavorisation Pour la Planification de la Santé et du Bien-Être au Québec. Québec: Institut National de Santé Publique du Québec; 2000. [Google Scholar]
- 33. Pampalon R, Hamel D, Gamache P, et al. Validation of a deprivation index for public health: a complex exercise illustrated by the Quebec index. Chronic Dis Inj Can. 2014;34(1):12–22. [PubMed] [Google Scholar]
- 34. Pampalon R, Martinez J, Hamel D. Does living in rural areas make a difference for health in Quebec? Health Place. 2006;12(4):421–435. [DOI] [PubMed] [Google Scholar]
- 35. Hamel D, Pampalon R. Traumatismes et Défavorisation au Québec. Québec: Institut National de Santé Publique du Québec; 2002. [Google Scholar]
- 36. Pampalon R, Raymond G. Indice de défavorisation matérielle et sociale: son application au secteur de la santé et du bien-être. Santé, Société et Solidarité. 2003;2(1):191–208. [Google Scholar]
- 37. Patten SB, Kennedy SH, Lam RW, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults, I: classification, burden and principles of management. J Affect Disord. 2009;117(Suppl 1):S5–S14. [DOI] [PubMed] [Google Scholar]
- 38. Reesal RT, Lam RW, Group CDW. Clinical guidelines for the treatment of depressive disorders, II: principles of management. Can J Psychiatry. 2001;46(Suppl 1):21S–28S. [PubMed] [Google Scholar]
- 39. Kennedy SH, Lam RW, Cohen NL, et al. Clinical guidelines for the treatment of depressive disorders, IV: medications and other biological treatments. Can J Psychiatry. 2001;46(Suppl 1):38S–58S. [PubMed] [Google Scholar]
- 40. Kennedy SH, Lam RW, McIntyre RS, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder, section 3: pharmacological treatments. Can J Psychiatry. 2016;61(9):540–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lam RW, Kennedy SH, Grigoriadis S, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults, III: pharmacotherapy. J Affect Disord. 2009;117(Suppl 1):S26–S43. [DOI] [PubMed] [Google Scholar]
- 42. Grégoire JP, Moisan J. Assessment of adherence to drug treatment in database research In: Almarsdottir AB, Andersen M, Benko R, et al., eds. Drug Utilization Research: Methods and Applications. Chichester (UK): John Wiley & Sons, Ltd; 2016. [Google Scholar]
- 43. Wahl C, Gregoire JP, Teo K, et al. Concordance, compliance and adherence in healthcare: closing gaps and improving outcomes. Healthc Q. 2005;8(1):65–70. [DOI] [PubMed] [Google Scholar]
- 44. Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–47. [DOI] [PubMed] [Google Scholar]
- 46.Statistical Area Classification (SAC), author http://www12.statcan.gc.ca/census-recensement/2011/ref/dict/geo045-eng.cfm [cited 2017 July 14]. Available from:
- 47. Pampalon R, Hamel D, Gamache P, et al. A deprivation index for health planning in Canada. Chronic Dis Can. 2009;29(4):178–191. [PubMed] [Google Scholar]
- 48. Lumley T, Kronmal R, Ma S. Relative risks regression in medical research: models, contrasts, estimators and algorithms. UW Biostatistics Working Paper Series. 2006;293:1–24. [Google Scholar]
- 49. Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200. [DOI] [PubMed] [Google Scholar]
- 50. Kleinbaum DG, Nizam A, Muller KE. Applied Regression Analysis and Other Multivariable Methods. Belmont (CA): Duxbury Press; 2008. [Google Scholar]
- 51. Marquardt DW. Generalized inverses, ridge regression biased linear estimation and non-linear estimation. Technometrics. 1970;12:591–612. [Google Scholar]
- 52. Hansen DG, Vach W, Rosholm JU, et al. Early discontinuation of antidepressants in general practice: association with patient and prescriber characteristics. Fam Pract. 2004;21(6):623–629. [DOI] [PubMed] [Google Scholar]
- 53. Bocquier A, Cortaredona S, Verdoux H, et al. Social inequalities in early antidepressant discontinuation. Psychiatr Serv. 2014;65(5):618–625. [DOI] [PubMed] [Google Scholar]
- 54. Sundell KA, Waern M, Petzold M, et al. Socio-economic determinants of early discontinuation of anti-depressant treatment in young adults. Eur J Public Health. 2013;23(3):433–440. [DOI] [PubMed] [Google Scholar]
- 55. Akincigil A, Bowblis JR, Levin C, et al. Adherence to antidepressant treatment among privately insured patients diagnosed with depression. Med Care. 2007;45(4):363–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Olfson M, Marcus SC, Tedeschi M, et al. Continuity of antidepressant treatment for adults with depression in the United States. Am J Psychiatry. 2006;163(1):101–108. [DOI] [PubMed] [Google Scholar]
- 57. Demyttenaere K. Risk factors and predictors of compliance in depression. Eur Neuropsychopharmacol. 2003;13(Suppl 3):S69–S75. [DOI] [PubMed] [Google Scholar]
- 58. Jeon-Slaughter H. Economic factors in of patients’ nonadherence to antidepressant treatment. Soc Psychiatry Psychiatr Epidemiol. 2012;47(12):1985–1998. [DOI] [PubMed] [Google Scholar]
- 59. Assayag J, Forget A, Kettani FZ, et al. The impact of the type of insurance plan on adherence and persistence with antidepressants: a matched cohort study. Can J Psychiatry. 2013;58(4):233–239. [DOI] [PubMed] [Google Scholar]
- 60. Zongo FE, Moisan J, Gregoire JP, et al. Association between community pharmacy loyalty and persistence and implementation of antipsychotic treatment among individuals with schizophrenia. Res Social Adm Pharm. 2016;14(1):53–61. [DOI] [PubMed] [Google Scholar]
- 61. Cooper D, Moisan J, Gregoire JP. Adherence to atypical antipsychotic treatment among newly treated patients: a population-based study in schizophrenia. J Clin Psychiatry. 2007;68(6):818–825. [DOI] [PubMed] [Google Scholar]
- 62. Guenette L, Moisan J, Breton MC, et al. Difficulty adhering to antidiabetic treatment: factors associated with persistence and compliance. Diabetes Metab. 2013;39(3):250–257. [DOI] [PubMed] [Google Scholar]
- 63. Brouwers FM, Courteau J, Gregoire JP, et al. The adequacy of pharmaceutical treatment of schizophrenia in Quebec varies with age, but is not influenced by sex or neighbourhood deprivation. Can J Psychiatry. 2013;58(8):456–465. [DOI] [PubMed] [Google Scholar]
- 64. Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25(4):284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.