Abstract
Objective:
Disparities in mental health care exist between regional and demographic groups. While screening is recommended as part of a correctional mental health strategy, little work has been done to explore whether it can narrow regional and demographic disparities in access to care. We compared treatment access rates by sex, race, age, and region in relation to screening results.
Methods:
We conducted a retrospective cohort study using administrative data. All 7965 admissions to the prison system were followed for a median of 14 months.
Results:
Males and non-Indigenous minority racial groups had lower rates of treatment regardless of screening results; they were less likely both to self-report needs and to receive treatment if these needs were reported. Regional differences revealed higher treatment rates in Atlantic Canada and Ontario, as well as higher rates of inmates self-reporting needs on screening who did not receive treatment in the Atlantic, Québec, and Pacific regions. There were minimal differences between inmates of different age groups.
Conclusions:
Findings suggest potential resource gaps and/or differences in the performance of screening to detect mental health needs across demographic and regional groups. Screening did not narrow, and may have widened, differences between groups.
Keywords: prisons, mass screening, mental disorders, mental health services, health care disparities
Abstract
Objectif:
Les disparités dans les soins de santé mentale existent entre groupes régionaux et démographiques. Bien que le dépistage soit recommandé dans le cadre d’une stratégie correctionnelle de santé mentale, on a peu exploré s’il peut réduire les disparités régionales et démographiques de l’accès aux soins. Nous avons comparé les taux d’accès au traitement selon le sexe, la race, l’âge et la région en relation avec les résultats du dépistage.
Méthodes:
Nous avons mené une étude de cohorte rétrospective à l’aide de données administratives. Toutes les 7 965 admissions dans le système carcéral ont été suivies pour une moyenne de 14 mois.
Résultats:
Les groupes d’hommes et de minorité raciale non autochtone avaient des taux plus faibles de traitement sans égard aux résultats du dépistage; ils étaient moins susceptibles d’autodéclarer des besoins et de recevoir un traitement si ces besoins étaient déclarés. Les différences régionales révélaient des taux de traitement plus élevés dans le Canada atlantique et l’Ontario, ainsi que des taux plus élevés de détenus autodéclarant des besoins au dépistage qui ne recevaient pas de traitement dans les régions de l’Atlantique, du Québec, et du Pacifique. Les différences entre détenus de différents groupe d’âge étaent minimes.
Conclusions:
Les résultats suggèrent des lacunes potentielles des ressources et/ou des différences de rendement du dépistage pour détecter les besoins de santé mentale dans les groupes démographiques et régionaux. Le dépistage n’a pas réduit les différences entre les groupes mais peut les avoir élargies.
Approximately 12% to 14% of inmates experience current psychotic, bipolar, or major depressive disorder.1,2 While many inmates with mental illness were treated in the community,3–7 between 50% and 75% are untreated during incarceration.8–10 Groups who have lower rates of accessing community services such as males, ethnic/racial minorities, and younger individuals are overrepresented in prisons. Interprovincial differences in access to community services also exist in Canada. In 2002, 9% to 10% of survey respondents reported past-year treatment in most provinces (territories were excluded), although rates were approximately 7% in Newfoundland and Prince Edward Island and roughly 11% in Nova Scotia, Manitoba, and British Columbia.11 Age-standardized mental health hospital discharge rates in 2014 were approximately 600 per 100,000 population in Ontario, Québec, and Prairie provinces and 700 to 800 per 100,000 in British Columbia and Atlantic provinces.12 There has been little investigation into whether preexisting disparities continue within prisons13,14 or of the performance of screening tools for subgroups.15 The small body of work in this area reports less treatment among Indigenous16,17 and minority racial or ethnic groups,18–20 men,9,20,21 and younger offenders.20 Common screening tools may also perform worse for racial or ethnic minorities and women.15,22,23
Screening presumes that needs are unrecognized by the individual and/or the health system. However, attitudinal barriers (e.g., preference to self-manage, perceived ineffectiveness of services, or lack of perceived need) are the most common reason that people do not seek services.24–26 Structural barriers (e.g., availability, cost, and knowledge of services) are generally less common, although they are more common in the United States compared with countries with public health systems such as Canada and the Netherlands,27 Atlantic Canada and the territories26 compared with the rest of Canada, and among those who are younger or of minority race.24 Screening is more likely to address structural as opposed to attitudinal barriers, as attitudinal barriers may lead to underreporting symptoms and/or refusing treatment. While most research on barriers has been conducted in the community, inmates report similar barriers other than cost.17,19,28,29 However, barriers may vary at different points in incarceration. For example, newly admitted inmates at intake units (as opposed to regular prison wings) reported higher rates of preferring to care for themselves, unawareness of how to access services, and worries about how other inmates and staff would perceive them.29
Our prior work30 found that screening in Canadian prisons performs at sensitivity (75%) and specificity (71%) that are comparable to the best-studied tools for use with prisoners.15,31 However, while 79% of inmates with mental illness had contact with a mental health professional, only 46% received sustained treatment,32 a figure that is comparable to access rates internationally.8–10 This may be caused in part by lower sensitivity of screening among those who did not self-report receiving treatment immediately prior to their incarceration and for racial minorities30; sex, age, and regional differences were not considered. Barriers to care discussed previously may also explain why roughly one-third of those with clinical contact did not remain in treatment.
To address some of these unanswered questions about screening within Canadian prisons, we examined demographic and regional differences in mental health treatment access prior to and following mental health screening.
Methods
Sample
We conducted a retrospective cohort study of all 7965 admissions to the Canadian prison system (i.e., individuals convicted of a criminal offence and sentenced to 2 years or longer of incarceration). Inclusion criteria were new admissions between the implementation date of screening (varied between November 2012 and June 2013) and September 2014. Median follow-up was 14 months (range, 0.03 to 28.2), ending at first release from prison (27.6%), death (0.2%), or March 2015 (72.2%), whichever came first. The sample was primarily male (93.6%), with an average age of 35.7 years (SD = 12.3). The majority (58.7%) of inmates self-reported white/Caucasian race, 23.4% reported Indigenous ancestry, 8.5% African/black race, and 9.4% reported another minority race.
Measures
Mental Health Screening
Consenting inmates complete computerized mental health screening between 3 and 14 days after admission to an intake prison. Three items capture self-reported diagnosis, psychotropic medication, and hospitalization in the month prior to incarceration: endorsement of any of these 3 items is considered a recent mental health history. Two standardized measures are also included to capture self-harm risk and potential mental illness. The Depression Hopelessness Suicide Screening Form (DHS)33 is a 39-item questionnaire. Increased self-harm risk is indicated by endorsement of 1 of 5 items capturing a recent (i.e., past 2 years) or multiple prior suicide attempts, history of self-harm, or current thoughts of or a plan to self-harm.34 A total score, as well as depression and hopelessness subscale scores, is calculated based on the number of endorsed items. A total score of 8 or higher, 7 or higher on the depression subscale (17 items), or 2 or higher on the hopelessness scale (10 items) is considered elevated distress warranting further assessment.35 The Brief Symptom Inventory (BSI)36 is a 53-item self-report measure. Nine subscale scores (depression, anxiety, phobia, psychoticism, interpersonal sensitivity, paranoia, hostility, somatization, and obsessive-compulsive) and a global severity index are calculated as the average item response. A respondent scoring above a T-score of 63 (using general adult population norms) on the Global Severity Index or on 2 of the 9 subscales is considered a possible case.36 Screening also measures intellectual functioning,37 attention-deficit hyperactivity disorder,38 and self-reported lifetime mental health needs; these do not factor into the scoring model but are used to inform recommendations for correctional programming and/or to help interpret ambiguous screening results.
During the study period, inmates were classified as either flagged, unclassified (requiring clinical judgment based on a minimum of a file review in addition to reviewing test results), or screened out using an iterative classification tree.39 However, as part of a recent consultation with front-line screening staff (manuscript in preparation), many staff reported finding the prior model difficult to understand and reliance on certain information (namely, recent mental health histories and self-harm risk) to override recommendations of the model. Our prior work32 developed a simpler model that arrived at similar decisions for most (82%) offenders. This model classified inmates into mutually exclusive groups of those who reported (1) a recent history, (2) increased self-harm risk (on the DHS), (3) elevated distress on both the BSI and DHS, and (4) none of the prior needs (i.e., screened negative). This model is being implemented in Canadian prisons. Furthermore, since it can help estimate the yield of screening versus continuity of care for known cases and is more generalizable to other settings, we apply it in the current study. Supplementary analyses showed similar findings to the primary analyses in terms of the pattern of findings (see the online supplement).
Mental Health Service Use
Clinical contacts in regular prisons were documented by staff in the Mental Health Tracking System (a system used for corporate reporting that has since been replaced by an electronic medical record). Because treatment end dates were not systematically recorded, an inmate was considered to be receiving treatment if they had at least 1 contact with a mental health professional for counseling, medication review, or crisis intervention within the past 30 days. Second, each of the 5 regions has a regional treatment center that provides 24-hour inpatient mental health care for acute and serious mental illness. We extracted admission and discharge dates for treatment center admissions from the prison’s electronic case management system’s transfer log; the entire duration of a treatment center admission was counted as time in treatment. To account for unequal follow-up times, we adopted the definition from past work that inmates who spent 10% or more of their time in treatment received treatment that is equivalent to most prior definitions of minimally adequate treatment or guidelines.32
Analysis
We calculated the proportions of offenders who accessed treatment by screening results. We refer to inmates who received treatment but who were not screened or who reported a recent history prior to incarceration as clinically detectable. Those who reported self-harm risk factors or elevated distress (without a recent history) and received treatment reflect the yield of screening. Those who self-reported either a recent history, self-harm risk, or distress but did not receive treatment reflect the costs of screening (i.e., false-positives) or undertreated needs. Finally, some inmates were provided treatment despite screening negative; the meaning of these cases is ambiguous (e.g., they could be false-negatives, incident illness, and/or overtreated).
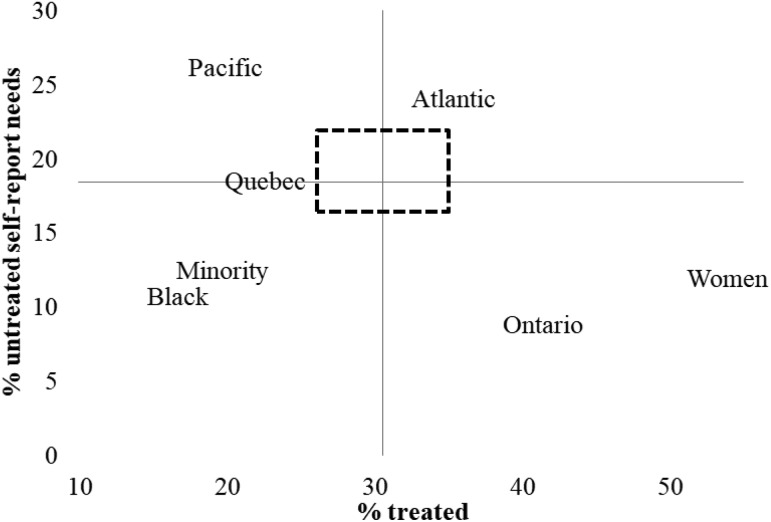
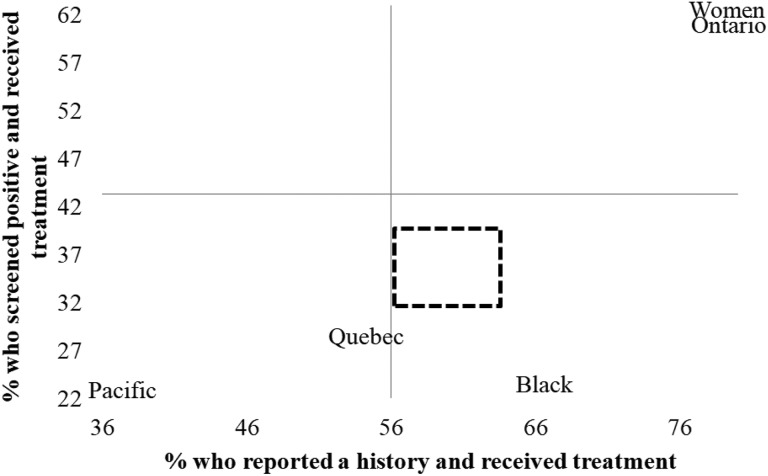
For concision, we rely primarily on graphical presentation of results in Figures 1 and 2, which integrate the various statistical findings. Figure 1 shows the relationship between the total percentage of inmates who received treatment versus the proportion of inmates who self-reported needs but were untreated. Figure 2 shows the treatment rates of inmates who self-reported either a history (on the x-axis) or self-harm risk or distress (combined on the y-axis) in relation to the estimated positive predictive value (PPV) of these self-reported items/tests.
Figure 1.
Percentage who received treatment versus those who self-reported needs but did not receive treatment. All groups not displayed in the figure fall within the dashed rectangle. Differences for these groups in the adjusted models (Table 2 and 3) were not statistically significant.
Figure 2.
Observed treatment rates for those self-reporting a recent history or needs on screening versus the expected rate (i.e., positive predictive value) shown by the axes. All groups not displayed in the figure fall within the dashed rectangle. Differences for these groups in the adjusted models (Table 3) were not statistically significant.
We refer to supporting statistics from Tables 1 through 3 to explain these figures. Table 1 shows the distribution of treatment and screening results, stratified by sex, race, region, and age. Chi-square tests were used to assess for differences in the distribution of treatment access in relation to screening results.
Table 1.
Distribution (%) of treatment access and screening results.a
| Treated | Untreated | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | n | Not screened | Recent history | Self-harm risk | Distress alone | Screen negative | Not screened | Recent history | Self-harm risk | Distress alone | Screen negative | |
| Total | 7965 | 5.4 | 12.5 | 2.5 | 3.4 | 6.8 | 12.0 | 8.2 | 3.7 | 6.5 | 39.1 | |
| Sex, χ2(9) = 198.6, P < 0.001 | ||||||||||||
| Men | 7455 | 5.1 | 11.5 | 2.3 | 3.4 | 6.7 | 11.8 | 8.3 | 3.7 | 6.8 | 40.4 | |
| Women | 510 | 10.0 | 27.1 | 4.3 | 3.9 | 8.6 | 14.5 | 7.1 | 2.8 | 2.2 | 19.6 | |
| Race, χ2(27) = 458.2, P < 0.001 | ||||||||||||
| White | 4676 | 5.1 | 14.2 | 2.5 | 3.6 | 7.3 | 8.4 | 9.3 | 3.4 | 6.5 | 34.9 | |
| Indigenous | 1860 | 7.1 | 13.3 | 3.4 | 3.9 | 7.0 | 15.1 | 9.1 | 5.9 | 6.2 | 51.5 | |
| Black | 677 | 4.3 | 6.2 | 0.6 | 1.8 | 3.8 | 18.2 | 3.1 | 1.2 | 6.5 | 34.5 | |
| Other | 752 | 4.4 | 4.9 | 1.6 | 2.9 | 5.9 | 21.0 | 3.3 | 1.7 | 7.5 | 33.2 | |
| Region, χ2(36) = 678.9, P < 0.001 | ||||||||||||
| Atlantic | 885 | 3.2 | 20.7 | 3.3 | 3.7 | 4.5 | 5.7 | 13.3 | 2.9 | 7.8 | 34.9 | |
| Quebec | 2193 | 3.7 | 7.8 | 2.4 | 2.4 | 6.4 | 7.3 | 6.6 | 4.2 | 7.8 | 51.5 | |
| Ontario | 1570 | 8.2 | 18.2 | 1.7 | 5.0 | 8.5 | 15.2 | 4.6 | 1.0 | 3.3 | 34.5 | |
| Prairie | 2550 | 6.5 | 11.1 | 2.9 | 3.8 | 7.9 | 14.8 | 7.9 | 5.0 | 6.8 | 33.2 | |
| Pacific | 767 | 4.0 | 9.1 | 1.7 | 1.6 | 3.5 | 16.6 | 15.3 | 4.0 | 6.9 | 37.3 | |
| Age, χ2(27) = 48.6, P = 0.007 | ||||||||||||
| 18-24 | 1614 | 4.7 | 12.5 | 2.7 | 3.2 | 6.6 | 12.6 | 8.4 | 3.8 | 7.7 | 37.9 | |
| 25-39 | 3638 | 5.7 | 13.2 | 2.5 | 3.4 | 6.6 | 12.0 | 8.9 | 3.5 | 6.1 | 38.2 | |
| 40-54 | 2020 | 5.6 | 12.7 | 2.4 | 3.6 | 6.6 | 12.3 | 7.6 | 3.6 | 6.2 | 39.4 | |
| 55+ | 693 | 5.2 | 7.9 | 1.7 | 3.9 | 8.7 | 9.7 | 6.1 | 4.6 | 6.9 | 45.3 | |
aBolded figures indicate groups in which the proportion differed from the total population by (1) 25% lower in relative terms, (2) 50% higher in relative terms, or (3) 5% absolute difference in either direction.
Table 2.
Adjusted predictors (relative risk) of treatment access in relation to screening results.a
| Total | Clinical/history-taking detection | Screening yield | Screen negative | |
|---|---|---|---|---|
| Men | REF | REF | REF | REF |
| Women | 1.72 [1.57, 1.88] | 2.04 [1.80, 2.31] | 2.05 [1.53, 2.75] | 2.02 [1.52, 2.70] |
| White | REF | REF | REF | REF |
| Indigenous | 1.03 [0.95, 1.12] | 1.03 [0.92, 1.15] | 1.29 [1.05, 1.60] | 1.09 [0.90, 1.34] |
| Black | 0.41 [0.34, 0.49] | 0.41 [0.32, 0.52] | 0.27 [0.16, 0.45] | 0.35 [0.24, 0.53] |
| Other | 0.55 [0.48, 0.64] | 0.43 [0.34, 0.54] | 0.62 [0.43, 0.88] | 0.62 [0.46, 0.85] |
| Atlantic | REF | REF | REF | REF |
| Quebec | 0.64 [0.57, 0.72] | 0.49 [0.41, 0.58] | 0.52 [0.39, 0.70] | 1.07 [0.77, 1.50] |
| Ontario | 1.35 [1.22, 1.51] | 1.30 [1.13, 1.50] | 1.21 [0.90, 1.63] | 2.22 [1.58, 3.12] |
| Prairie | 0.89 [0.80, 0.99] | 0.72 [0.62, 0.83] | 0.83 [0.63, 1.11] | 1.72 [1.24, 2.39] |
| Pacific | 0.55 [0.47, 0.65] | 0.54 [0.44, 0.67] | 0.43 [0.28, 0.68] | 0.79 [0.50, 1.26] |
| 18-24 | REF | REF | REF | REF |
| 25-39 | 1.05 [0.96, 1.14] | 1.09 [0.96, 1.23] | 1.07 [0.85, 1.34] | 1.02 [0.83, 1.26] |
| 40-54 | 1.04 [0.94, 1.15] | 1.06 [0.92, 1.22] | 1.10 [0.85, 1.41] | 1.01 [0.79, 1.29] |
| 55+ | 0.92 [0.80, 1.06] | 0.77 [0.61, 0.95] | 0.88 [0.61, 1.27] | 1.08 [0.80, 1.46] |
aAdjusted for all variables shown in the table and for the length of follow-up time. Models are fit separately for each screening result category, where individuals identified at prior steps are excluded when fitting the model. Bolded figures represent statistically significant findings at an alpha of .05.
Table 3.
Adjusted predictors (relative risk) of being untreated following self-reported needs on screening.a
| History | Self-harm risk or distress | |
|---|---|---|
| Men | REF | REF |
| Women | 0.50 [0.37, 0.68] | 0.64 [0.46, 0.89] |
| White | REF | REF |
| Indigenous | 0.97 [0.85, 1.11] | 0.98 [0.89, 1.09] |
| Black | 0.99 [0.71, 1.38] | 1.41 [1.23, 1.61] |
| Other | 0.97 [0.72, 1.31] | 1.15 [0.99, 1.33] |
| Atlantic | REF | REF |
| Quebec | 1.20 [1.00, 1.45] | 1.17 [1.02, 1.35] |
| Ontario | 0.51 [0.40, 0.66] | 0.63 [0.50, 0.79] |
| Prairie | 1.07 [0.89, 1.27] | 1.06 [0.92, 1.23] |
| Pacific | 1.74 [1.46, 2.08] | 1.28 [1.08, 1.51] |
| 18-24 | REF | REF |
| 25-39 | 1.02 [0.88, 1.18] | 0.93 [0.84, 1.03] |
| 40-54 | 0.95 [0.80, 1.14] | 0.93 [0.83, 1.05] |
| 55+ | 1.10 [0.86, 1.41] | 0.98 [0.84, 1.15] |
aAdjusted for all variables shown in the table, and for the length of follow-up time. Models are fit separately for each screening result, and included only those who reported the need. Bolded figures represent statistically significant findings at an alpha of .05.
To estimate independent associations between the variables under study and treatment access, we fit Poisson regression models with robust variance to calculate adjusted relative risks. This approach is recommended given that odds ratios overestimate associations when outcomes are common (i.e., >10%).40 We entered follow-up time in the model to account for unequal follow-up. Table 2 explores treatment access. The first model estimated the relative differences of clinically detectable cases. The second and third models excluded those who reported a history or who were not screened to focus on impacts of screening. The second model estimated the relative yield of screening (combining the self-harm and distress items due to small numbers in each group), and the final model estimated the relative risk of receiving treatment despite screening negative (i.e., of obtaining a false-negative result or developing incident needs). Table 3 focused on unmet needs and false-positives (i.e., costs or implementation challenges of screening). We fit separate models to distinguish a lack of continuity of (self-reported) care as a clinically detectable need from those who reported self-harm risk or distress without a recent history (i.e., focused on potential false-positives or lack of follow-up to screening).
Ethics
Approval was obtained from the Ottawa Health Science Network Research Ethics Board (protocol number 20150240-01 H); the project was also approved by Correctional Service of Canada.
Results
As seen in Table 1, 30.6% of offenders received treatment. Of these, 17.9% were clinically identifiable (i.e., 5.4% were not screened and 12.5% reported a recent history). Screening yielded a maximum of 5.9% of inmates accessing treatment (i.e., 2.5% reported self-harm risk and 3.4% reported distress). The final 6.8% of treated inmates screened negative. A further 18.4% of inmates self-reported either a history (8.2%), self-harm risk (3.7%), or distress alone (6.5%) but did not receive treatment. In total, 51.1% of inmates had either a negative screening result (39.1%) or were not screened (12.0%) and were untreated.
The upper left-hand quadrant of Figure 1 indicates low treatment rates and higher rates of potential unmet needs. There were 15.3% of inmates in the Pacific region who were untreated inmates but self-reported a recent history and 10.9% who reported a distress or self-harm (Table 1); as seen in Table 3, these rates were 1.74 (95% confidence interval [CI], 1.46 to 2.08) and 1.28 (95% CI, 1.08 to 1.51) times higher than in the Atlantic region (see also Figure 2). To a lesser degree, higher rates of unmet needs may also exist in the Québec (i.e., inmates were roughly 1.2 times more likely to be untreated following self-reported needs; see Table 3) and Atlantic regions (i.e., 13.3% of all offenders reported a recent history but did not receive treatment; see Table 1).
The bottom right-hand quadrant of Figure 1 displays subgroups (i.e., Ontario region and women) who may be overtreated. Figure 2 shows that for these groups, roughly 20% more inmates who self-reported either a history, self-harm risk, or distress received treatment than expected based on the PPV. Women were 1.72 to 2.05 times more likely to receive treatment (Table 2) in the adjusted model. Not only are these differences in access attributable to preexisting differences (e.g., 27.1% of women vs. 11.5% of men received treatment and self-reported a recent history; Table 1), but women were also 36% to 50% less likely to be untreated if they self-reported a recent history (relative risk [RR] = 0.50; 95% CI, 0.37 to 0.68), or were screen detected (RR = 0.64; 95% CI, 0.46 to 0.89). A similar pattern is seen in Ontario, although with occasionally weaker relationships.
Racial or ethnic differences are more complex. Nonwhite inmates were more likely to not complete screening (i.e., 22%-25% were not screened, compared with 13.5% of white inmates; Table 1). While similar proportions of white and Indigenous inmates received treatment (RR = 1.03; 95% CI, 0.95 to 1.12), there was a slightly higher yield of screening for Indigenous offenders (7.3% vs. 6.1% of white offenders; RR = 1.29; 95% CI, 1.05 to 1.60). Black and other minority inmates had treatment rates that were roughly half those of white inmates. While these groups appear in the bottom left-hand quadrant of Figure 1 (suggesting lower need that is mostly met), Figure 2 reveals disparities in terms of responding to potential needs of black inmates and other minority inmates. Black inmates who reported a history had treatment rates slightly higher than the PPV of the history-taking questions (consistent with other groups; RR for untreated inmates with a recent history = 0.99; 95% CI, 0.71 to 1.38). However, those who self-reported self-harm risk or distress were 1.41 (95% CI, 1.23 to 1.61) times more likely to be untreated (see Table 3). The pattern was similar—although weaker—for other minority inmates, who were 1.15 (95% CI, 0.99 to 1.33) times more likely to be untreated if they self-reported self-harm risk or distress.
Age differences were minimal, as the only significant difference was a smaller proportion (7.9%) of older offenders who received treatment in prison and self-reported a recent history (RR = 0.77; 95% CI, 0.61 to 0.95).
Discussion
We observed disparate rates of continuity of care and impacts of screening between the sexes, regions, and racial groups. In many cases, preexisting differences from the community increased following screening, as seen by higher rates of reported needs and, in some cases, higher rates of follow-up treatment. For example, there were roughly twice as many clinically detectable cases among women and inmates in the Atlantic or Ontario regions. Since fewer inmates remain to be detected through screening, we would have expected a lower yield of screening. Yet there was also a greater yield of screening among women and in the Ontario and Atlantic regions.
The magnitude and impacts of regional differences warrant further consideration. Specific to Canadian prisons, determining the appropriate level of treatment in response to positive screens and resource requirements to achieve this level of care requires further study. If groups with fewer clinically detectable cases reflected greater undetected need in the community, higher rates of self-harm risk and self-reported distress at intake to prison would be expected. Conversely, as in the Pacific region, which has one of the higher rates of community mental hospital discharges in Canada12 but among the lowest yields of clinically detectable cases, unmet need may be reflected in higher rates of inmates self-reporting needs who did not receive treatment in prison. Where these patterns are not observed, there may be a difference in prevalence of illness. For example, given that high prevalence of mental illness was previously reported in Québec provincial jails (i.e., those sentenced to shorter sentences),41 and the prevalence of mental illness in the community is similar in Québec to the rest of Canada,42 other explanations warrant further exploration for the lower proportion of clinically detectable cases. One potential explanation is the higher use of not criminally responsible verdicts in Québec,43 which could result in people with mental illness who commit serious crimes that would result in a longer prison sentence being diverted to forensic hospitals. While these questions related to resource allocation and trajectories through health and social services require answers to improve responses to persons with mental illness, answering them extends beyond the data at hand.
Culturally-informed or responsive care principles emphasize that to reduce disparities, policy and practice must acknowledge differences in how individuals understand mental health and report symptoms.44 Lower screening completion rates among nonwhite inmates warrant attention. While reasons for noncompletion were not collected, these include inmate refusal and not attending screening. Alegria and colleagues45 note that inappropriate matching of treatment to patient preferences, language, culture, and other characteristics and prior experiences of inadequate care may lead to higher rates of refusing or not completing treatment and missing appointments among minority groups. As one recommendation to eliminate racial and ethnic disparities in mental health care, they suggest campaigns to address stigma and trust issues as well as providing specific information on accessing services.45
In the community, black and Asian individuals were between 61% and 84% less likely to seek treatment than Caucasians (Indigenous and Latin Americans had non–statistically significant higher rates of accessing care),46 which is consistent with a lower rate of clinically detectable cases in our study. Given that fewer black and other minority inmates reported self-harm risk or distress and received treatment, screening does not appear to narrow differences in access rates. We lacked diagnostic assessments to explore whether our findings reflect true prevalence differences or differential performance of screening. While others have observed that individuals of an ethnic or racial minority are more likely to have a complex pathway to mental health care, including the police or other parts of the justice system (which could result in a higher prevalence),47–49 a lower prevalence of mental illness among minority inmates (13%) than white (25%) or Aboriginal (23%) inmates was previously reported.30
We did not observe other hypothesized ethnic disparities. For example, similar treatment access by white and Indigenous inmates is inconsistent with findings indicating lower treatment rates by Indigenous persons in New Zealand prisons.16 We also observed similar rates of service use by inmates of minority race who report a recent mental health history, which suggests that continuity of care in Canadian prisons is provided equally regardless of race or ethnicity. By contrast, Sayers and colleagues13 found that African American and Asian inmates who were treated in the community were 4% and 10% less likely, respectively, to be treated in prison.
Sayers and colleagues’13 finding that the absolute rate of continuity of care was 4% lower among females also differed from ours, in which women were roughly twice as likely to receive treatment. Sayers and colleagues conducted their work in one of the largest U.S. jails with a population between 2000 and 2400 inmates, where women are a minority of the population (13%). In Canadian prisons, women are incarcerated in separate facilities, with rated capacities ranging from 99 to 215.50 The ratio of mental health staff to inmates may be greater than in most other prison settings (including Correctional Service of Canada’s men’s institutions), and there may be a greater focus on gender-informed correctional care51 (including mental health needs). As noted previously, while much of the difference in access between men and women predates incarceration, there were also higher rates of treatment provided to women when matched to men reporting similar needs on screening. On the other hand, American studies that focus on treatment rates for the entire population (i.e., not simply continuity of care) report similar findings, namely, that women have higher rates of treatment use in prison.20,21
While we addressed the understudied question about differences in access to treatment in relation to screening, we lacked measures of severity of need that would have allowed us to accurately distinguish, for example, false-positive screening results from unmet needs and true-negatives from missed cases. We were also unable to assess whether the intensity of service provided was appropriately matched to the needs of the individual, although this question extends beyond the impact of screening to consider the clinical work to develop and monitor a treatment plan. Finally, while comparing treatment rates to the PPVs of screening can estimate observed versus expected treatment rates, differences in prevalence would result in inaccurate estimates of under- or overtreatment because of the inverse relationship between prevalence and PPV.52
Despite these limitations, our work provides a framework that can be used to evaluate the real-world impact of implementing screening. Given the costs and logistic challenges of obtaining gold standard measures to validate screening tools and the need to estimate the actual impacts of screening, further work using administrative data may help address current knowledge and implementation gaps. Increased understanding of regional and demographic differences in detection and treatment of mental illness in community and correctional settings may identify good practices and gaps along the continuum of health and justice services that may reduce inequities and overrepresentation of persons with mental illness in the criminal justice system.
Supplemental Material
Online_supplement for Mental Health Screening and Differences in Access to Care among Prisoners by Michael S. Martin, Anne G. Crocker, Beth K. Potter, George A. Wells, Rebecca M. Grace, and Ian Colman in The Canadian Journal of Psychiatry
Acknowledgments
Dr. Martin was supported by a Vanier Canada Graduate Scholarship. Dr. Colman is supported by the Canada Research Chairs program. This research was supported by the Correctional Service of Canada (CSC), who provided access to data. However, CSC had no role in the conduct of the study. The views expressed are those of the authors and do not necessarily reflect the views of the department or the Government of Canada.
Footnotes
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Martin is an employee of the prison service. He was on unpaid education leave at the time of this work. Ms. Grace has previously worked on contract for the prison service. The remaining authors have no interests to declare.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ian Colman  http://orcid.org/0000-0001-5924-0277
http://orcid.org/0000-0001-5924-0277
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Fazel S, Seewald K. Severe mental illness in 33,588 prisoners worldwide: systematic review and meta-regression analysis. Br J Psychiatry. 2012;200(5):364–373. [DOI] [PubMed] [Google Scholar]
- 2. Beaudette JN, Stewart LA. National prevalence of mental disorders among incoming Canadian male offenders. Can J Psychiatry. 2016;61(10):624–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Martin MS, Potter BK, Crocker AG, Wells GA, Colman I. Yield and efficiency of mental health screening: a comparison of screening protocols at intake to prison. PLos One. 2016;11(5):e0154106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Way BB, Sawyer DA, Lilly SN, Moffitt C, Stapholz BJ. Characteristics of inmates who received a diagnosis of serious mental illness upon entry to New York State prison. Psychiatr Serv. 2008;59(11):1335–1337. [DOI] [PubMed] [Google Scholar]
- 5. Fisher WH, Packer IK, Banks SM, Smith D, Simon LJ, Roy-Bujnowski K. Self-reported psychiatric hospitalization histories of jail detainees with mental disorders: comparison with a non-incarcerated national sample. J Behav Health Serv Res. 2002;29(4):458–465. [DOI] [PubMed] [Google Scholar]
- 6. Mundt AP, Kastner S, Mir J, Priebe S. Did female prisoners with mental disorders receive psychiatric treatment before imprisonment? BMC Psychiatry. 2015;15:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bebbington P, Jakobowitz S, McKenzie N, et al. Assessing needs for psychiatric treatment in prisoners: 1. Prevalence of disorder. Soc Psychiatry Psychiatr Epidemiol. 2017;52(2):221–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Teplin LA. Detecting disorder: the treatment of mental illness among jail detainees. J Consult Clin Psychol. 1990;58(2):233–236. [DOI] [PubMed] [Google Scholar]
- 9. Jakobowitz S, Bebbington P, McKenzie N, et al. Assessing needs for psychiatric treatment in prisoners: 2. Met and unmet need. Soc Psychiatry Psychiatr Epidemiol. 2017;52(2):231–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Senior J, Birmingham L, Harty MA, et al. Identification and management of prisoners with severe psychiatric illness by specialist mental health services. Psychol Med. 2012;43(7):1511–1520. [DOI] [PubMed] [Google Scholar]
- 11. Vasiliadis HM, Lesage A, Boyer R. Service use for mental health reasons: cross-provincial differences in rates, determinants, and equity of access. Can J Psychiatry. 2005;50(10):614–619. [DOI] [PubMed] [Google Scholar]
- 12. Canadian Institute for Health Information. HMHDB hospital mental health services in Canada. Quick stats. 2016. [accessed 2016 Nov 11] https://www.cihi.ca/en/quick-stats.
- 13. Sayers SK, Domino ME, Cuddeback GS, Barrett NJ, Morrissey JP. Connecting mentally ill detainees in large urban jails with community care. Psychiatr Q. 2016;88(2):323–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Youman K, Drapalski A, Stuewig J, Bagley K, Tangney J. Race differences in psychopathology and disparities in treatment seeking: community and jail-based treatment-seeking patterns. Psychol Serv. 2010;7(1):11–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Martin MS, Colman I, Simpson AI, McKenzie K. Mental health screening tools in correctional institutions: a systematic review. BMC Psychiatry. 2013;13:275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Simpson AI, Brinded PM, Fairley N, Laidlaw TM, Malcolm F. Does ethnicity affect need for mental health service among New Zealand prisoners? Aust N Z J Psychiatry. 2003;37(6):728–734. [DOI] [PubMed] [Google Scholar]
- 17. Skogstad P, Deane FP, Spicer J. Barriers to helpseeking among New Zealand prison inmates. J Offender Rehabil. 2005;42(2):1–24. [Google Scholar]
- 18. Prins SJ, Osher FC, Steadman HJ, Robbins PC, Case B. Exploring racial disparities in the brief jail mental health screen. Crim Justice Behav. 2012;39(5):635–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Faust E, Magaletta PR. Factors predicting levels of female inmates’ use of psychological services. Psychol Serv. 2010;7(1):1–10. [Google Scholar]
- 20. Kaba F, Solimo A, Graves J, et al. Disparities in mental health referral and diagnosis in the New York city jail mental health service. Am J Public Health. 2015;105(9):1911–1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Drapalski AL, Youman K, Stuewig J, Tangey J. Gender differences in jail inmates’ symptoms of mental illness, treatment history and treatment seeking. Crim Behav Ment Health. 2009;19(3):193–206. [DOI] [PubMed] [Google Scholar]
- 22. Kubiak SP, Beeble ML, Bybee D. Using the K6 to assess the mental health of jailed women. J Offender Rehabil. 2009;48(4):296–313. [Google Scholar]
- 23. Ober C, Dingle K, Clavarino A, Najman JM, Alati R, Heffernan EB. Validating a screening tool for mental health and substance use risk in an Indigenous prison population. Drug Alcohol Rev. 2013;32(6):611–617. [DOI] [PubMed] [Google Scholar]
- 24. Mojtabai R, Olfson M, Sampson NA, et al. Barriers to mental health treatment: results from the National Comorbidity Survey Replication. Psychol Med. 2011;41(8):1751–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Andrade LH, Alonso J, Mneimneh Z, et al. Barriers to mental health treatment: results from the WHO world mental health surveys. Psychol Med. 2014;44(6):1303–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Afifi TO, Cox BJ, Sareen J. Perceived need and help-seeking for mental health problems among Canadian provinces and territories. Can J Community Ment Health. 2005;24(1):51–61. [DOI] [PubMed] [Google Scholar]
- 27. Sareen J, Jagdeo A, Cox BJ, et al. Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatr Serv. 2007;58(3):357–364. [DOI] [PubMed] [Google Scholar]
- 28. Morgan RD, Steffan JS, Shaw LB, Wilson S. Needs for and barriers to correctional mental health services: inmate perceptions. Psychiatr Serv. 2007;58(9):1181–1186. [DOI] [PubMed] [Google Scholar]
- 29. Morgan RD, Rozycki AT, Wilson S. Inmate perceptions of mental health services. Professional Psychology: Research and Practice. 2004;35(4):389–396. [Google Scholar]
- 30. Martin MS, Wells GA, Crocker AG, Potter BK, Colman I. Decision curve analysis as a framework to estimate the potential value of screening or other decision making aids. Int J Methods Psychiatr Res. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. National Institute for Health and Care Excellence. Mental health of adults in contact with the criminal justice system. London (UK): National Institute for Health and Clinical Excellence; 2017. [PubMed] [Google Scholar]
- 32. Martin MS, Potter BK, Crocker AG, Wells GA, Grace RM, Colman I. Mental health treatment patterns following screening at intake to prison. J Consult Clin Psychol. 2017;86(1):15–23. [DOI] [PubMed] [Google Scholar]
- 33. Mills JF, Kroner DG. A new instrument to screen for depression, hopelessness, and suicide in incarcerated offenders. Psychol Serv. 2004;1(1):83–91. [Google Scholar]
- 34. Martin MS, Dorken SK, Simpson AI, McKenzie K, Colman I. The predictive validity of the depression hopelessness suicide screening form for self-injurious or suicidal behaviour among prisoners. J Forensic Psychiatr Psychol. 2014;25(6):733–747. [Google Scholar]
- 35. Mills JF, Kroner DG. Depression, hopelessness and suicide screening form: user guide. Kingston (ON): Author; 2003. [Google Scholar]
- 36. Derogatis LR. Brief Symptom Inventory: administration, scoring, and procedures manual. 4th ed Minneapolis (MN): National Computer Systems; 1993. [Google Scholar]
- 37. Naglieri JA, Bardos AN. GAMA (General Ability Measure for Adults) manual. Toronto (ON): NCS Pearson; 1997. [Google Scholar]
- 38. Kessler RC, Adler L, Ames M, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35(2):245–256. [DOI] [PubMed] [Google Scholar]
- 39. Martin MS, Wamboldt AD, O’Connor SL, Fortier J, Simpson AI. A comparison of scoring models for computerised mental health screening for federal prison inmates. Crim Behav Ment Health. 2013;23(1):6–17. [DOI] [PubMed] [Google Scholar]
- 40. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]
- 41. Lafortune D. Prevalence and screening of mental disorders in short-term correctional facilities. Int J Law Psychiatry. 2010;33(2):94–100. [DOI] [PubMed] [Google Scholar]
- 42. Thompson AH. Variations in the prevalence of psychiatric disorders and social problems across Canadian provinces. Can J Psychiatry. 2005;50(10):637–642. [DOI] [PubMed] [Google Scholar]
- 43. Crocker AG, Nicholls TL, Seto MC, Côté G, Charette Y, Caulet M. The national trajectory project of individuals found not criminally responsible on account of mental disorder in canada. Part 1: context and methods. Can J Psychiatry. 2015;60(3):98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Substance Abuse and Mental Health Services Administration. Improving cultural competence. Rockville (MD): Substance Abuse and Mental Health Services Administration; 2014. [PubMed] [Google Scholar]
- 45. Alegria M, Alvarez K, Ishikawa RZ, DiMarzio K, McPeck S. Removing obstacles to eliminating racial and ethnic disparities in behavioral health care. Health Aff (Millwood). 2016;35(6):991–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Gadalla TM. Ethnicity and seeking treatment for depression: a Canadian national study. Can Ethnic Studies. 2010;41-42(3-1):233–245. [Google Scholar]
- 47. Bhui K, Ullrich S, Kallis C, Coid JW. Criminal justice pathways to psychiatric care for psychosis. Br J Psychiatry. 2015;207(6):523–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bhui K, Stansfeld S, Hull S, Priebe S, Mole F, Feder G. Ethnic variations in pathways to and use of specialist mental health services in the UK: systematic review. Br J Psychiatry. 2003;182(2):105–116. [DOI] [PubMed] [Google Scholar]
- 49. Flora N, Barbaree H, Simpson AIF, Noh S, McKenzie K. Pathways to forensic mental health care in Toronto: a comparison of European, African-Caribbean, and other ethnoracial groups in Toronto. Can J Psychiatry. 2012;57(7):414–421. [DOI] [PubMed] [Google Scholar]
- 50. Correctional Service of Canada. Institutional profiles. [accessed 2018 Feb 21] http://www.csc-scc.gc.ca/institutions/index-eng.shtml.
- 51. de Vogel V, Nicholls TL. Gender matters: an introduction to the special issues on women and girls. Int J Forensic Ment Health. 2016;15(1):1–25. [Google Scholar]
- 52. Glaros AG, Kline RB. Understanding the accuracy of tests with cutting scores: the sensitivity, specificity, and predictive value model. J Clin Psychol. 1988;44(6):1013–1023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online_supplement for Mental Health Screening and Differences in Access to Care among Prisoners by Michael S. Martin, Anne G. Crocker, Beth K. Potter, George A. Wells, Rebecca M. Grace, and Ian Colman in The Canadian Journal of Psychiatry