Abstract
Objectives. To describe trends in rates of pelvic inflammatory disease (PID) encounters among American Indian/Alaska Native (AI/AN) women aged 15 to 44 years in the United States receiving care within the Indian Health Service (IHS).
Methods. We analyzed IHS discharge data sets for PID encounters during 2001 to 2015 with International Classification of Diseases, Ninth Revision, Clinical Modification, diagnosis codes. We calculated rates of PID encounters per 100 000 women overall and stratified by age group, region, and health care setting. We used regression to identify trends in the total, annual, and average annual percent changes in the rate of PID encounters.
Results. There were 44 042 PID encounters during 2001 to 2015 (rate = 825 per 100 000). The highest rates were among women aged 20 to 24 years (1104) and from the Alaska region (1556). Rates significantly decreased overall (2001: 1084; 2015: 512; P < .001) and within all age groups and health care settings. There was variability in Alaska, with large increases during 2001 to 2010 followed by large decreases during 2010 to 2015.
Conclusions. We observed decreasing trends in PID encounters among AI/AN women aged 15 to 44 years during 2001 to 2015, with the exception of increases in the Alaska region.
Pelvic inflammatory disease (PID), a condition characterized by inflammation of the female upper genital tract, can result from untreated sexually transmitted infections (STIs). Pelvic inflammatory disease may be asymptomatic or subclinical, but can also result in mild to severe symptoms. It is estimated that untreated cervical chlamydial and gonococcal infections can progress to clinical PID in 10% to 15% of infected women.1,2 Early diagnosis and treatment of PID is important to prevent long-term reproductive sequelae, such as ectopic pregnancy and infertility.3 Screening for and early treatment of STIs, such as chlamydia, is critical to prevent PID.4–6
National estimates indicate that approximately 2.5 million women of reproductive age have received a PID diagnosis in their lifetime.7 However, PID is not nationally notifiable, and surveillance data available to monitor PID rates are limited. This is partially attributable to the difficulties surrounding the diagnosis of PID.8 Limited national data indicate a decrease in PID hospitalizations, ambulatory visits, and emergency department visits, and a shift over many years from inpatient to outpatient care.9–11 Although racial disparities among PID cases have been reported, published estimates of PID among American Indian/Alaska Native (AI/AN) individuals are not available.7,12,13
American Indians/Alaska Natives have long experienced disparities in both chronic and infectious diseases. With regard to STIs, AI/AN women are disproportionally affected, with rates of chlamydia and gonorrhea 4.1 times and 6.1 times the rate among non-Hispanic White women, respectively.14 This disparity varies geographically, with AI/AN women in Alaska demonstrating the highest rates of chlamydia and gonorrhea compared with women in other parts of the United States.13,15 Furthermore, racial misclassification (e.g., AI/AN individuals are often coded as White in state-based, notifiable disease surveillance data) likely results in an underreporting of STI rates among AI/AN individuals.16
The Indian Health Service (IHS) is an agency within the Department of Health and Human Services responsible for providing health care to eligible AI/AN individuals. Indian Health Service federal, tribal, and urban clinics provide health services to approximately 2.2 million AI/AN persons belonging to 573 federally recognized tribes in 37 states.17,18 The persons receiving care within the IHS are a subset of the approximately 5.2 million national AI/AN population and are provided care mostly in rural and frontier areas.19 Despite the large AI/AN population and the well-documented disparities, the funding appropriation for IHS has consistently been less than 50% of the estimated level of need. This directly contributes to a lower expenditure for health services per capita compared with other federal health programs such as Medicaid, Medicare, and the Veterans Health Administration.20,21
The IHS collects and manages electronic health data for the patients it supports and serves. In addition to informing clinical management, these data are routinely monitored to assess disease burden and trends in disease within the AI/AN population over time.17 The purpose of this study was to analyze discharge data within the IHS National Patient Information Reporting System to determine trends in the rates of acute PID encounters among AI/AN women. Women aged 15 to 44 years receiving care at IHS facilities in the United States during fiscal years 2001 through 2015 were included. Given that rates of reported STI cases vary by region, we also aimed to understand any geographic variation and to describe the rates of inpatient, outpatient, and emergency department encounters with an acute PID diagnosis.13,14
METHODS
We analyzed information on inpatient, outpatient, and emergency department visits (hereafter termed “encounters”) for AI/AN women from the IHS Direct and Contract Health Service Inpatient Discharge and Outpatient data sets during 2001 to 2015. Annual data were reported in federal fiscal year intervals; for example, 2015 data included records from October 1, 2014, through September 30, 2015. The IHS divides the United States into 12 distinct geographic areas for administrative purposes. Following methodology from previous studies using IHS clinical data, the 12 IHS areas were collapsed into 7 standard administrative regions to limit attribution of study findings to individual tribes while still permitting analysis of regional variations.22,23 The IHS regions (Figure A, available as a supplement to the online version of this article at http://www.ajph.org) incorporate the following administrative areas: East (Nashville), Northern Plains East (Bemidji), Northern Plains West (Great Plains, Billings), Alaska, Southern Plains (Oklahoma), Southwest (Albuquerque, Navajo, Phoenix–Tucson), and West (California, Portland). We excluded the West region from the inpatient and emergency department discharge data sets because of the lack of IHS- or tribally operated hospitals and emergency departments and the incompleteness of information on contract health services. We included all 7 regions in the outpatient data sets.
Case Definition
We selected encounters for acute PID (hereafter PID), defined as any acute infection of the upper female genitourinary tract or inflammatory diseases of the reproductive tract, among AI/AN women aged 15 to 44 years during 2001 to 2015 by using the following International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: 098.10, 098.16, 098.17, 098.19, 098.86, 099.56, 614.0, 614.2, 614.3, 614.5, 614.8, 614.9, 615.0, and 615.9 (Table A, available as a supplement to the online version of this article at http://www.ajph.org).10,24–27 We included inpatient, outpatient, and emergency department encounters if a PID diagnosis code was in any 1 of 15 diagnoses available in the record for the encounter. It is possible for a person to be represented more than once if they had more than 1 PID encounter in the study period. We evaluated additional ICD-9-CM codes accompanying those used to define a PID encounter to further substantiate ICD-9-CM codes for PID (Table B, available as a supplement to the online version of this article at http://www.ajph.org).
Covariates of Interest
We examined annual and average annual rates of PID encounters stratified by age group, region, type of health care setting, and concurrent STI diagnoses. Ages were grouped into 5-year categories: 15 to 19, 20 to 24, 25 to 29, 30 to 34, 35 to 39, and 40 to 44 years. We conducted regional assessments as described previously. We classified type of health care setting as inpatient, outpatient, and emergency department. Concurrent STI diagnoses included diagnosis codes for chlamydia, gonorrhea, or both on the same record as the PID encounter. We defined chlamydia by using ICD-9-CM codes 078.88, 079.88, 079.98, 099.41, and 099.5 through 099.59 in any of 15 diagnoses; we similarly defined gonorrhea by using ICD-9-CM codes 098.0 through 098.8.
Statistical Analysis
We calculated the annual and average annual rates of PID encounters as the number of PID encounters divided by the corresponding IHS user population. The annual IHS user population was defined as all registered AI/AN persons who received IHS-funded health care at least once within the preceding 3 years (i.e., for 2001, the user had at least 1 visit for fiscal years 1999, 2000, and 2001).17,28 We calculated rates and their associated 95% confidence intervals (CIs) per 100 000 women for the overall study period, by year, as well as stratified by age group, region, and health care setting. We calculated average annual rates with the number of encounters during 2001 to 2015 as the numerator and the summation of the annual IHS user populations during 2001 to 2015 as the denominator. In addition, we calculated the annual and average annual rates of encounters with both PID and concurrent STI diagnosis codes. We examined the distribution of age group and region within each health care setting and calculated the proportion with a concurrent STI diagnosis within each setting. We used Poisson regression to compare average annual rates between age groups and regions and to analyze the overall trend across the study period by age group and region. We conducted analyses with SAS statistical software (version 9.3; SAS Institute Inc, Cary, NC).
We calculated the total percent change in the annual rate of PID encounters during 2001 to 2015 as the difference in the rate of PID encounters between 2001 and 2015, divided by the rate of PID encounters in 2001. We estimated the annual percent change (APC) and average annual percent change (AAPC) by using Joinpoint software version 4.5.0.1 (National Cancer Institute, Bethesda, MD). This statistical software used trend data to identify log-linear models with the fewest inflection points. We calculated the APC as the log-linear slope of the trend segment between inflection points. We calculated the AAPC as the weighted average of the individual APCs over the entire study period, with the weights equal to the length of the APC intervals between inflection points. When no inflection points existed in a Joinpoint model, the AAPC was equivalent to the APC and we presented the APC; however, when 1 or more inflection points existed, we presented the AAPC to provide a summary measure of trends over the study period. We estimated the total percent change, APC, and AAPC (where applicable) overall and by age group, region, health care setting, and concurrent STI diagnosis. We determined statistical significance for all analyses as P < .05.
RESULTS
The number of AI/AN women aged 15 to 44 years in the IHS user population increased from 324 480 in 2001 to 380 049 in 2015. During this time, there were 44 042 inpatient, outpatient, and emergency department PID encounters in this population (Table 1). The overall average annual rate of PID encounters among this population was 825 (95% CI = 818, 833) per 100 000 AI/AN women with the highest rate observed among those aged 20 to 24 years (rate = 1104 per 100 000; 95% CI = 1085, 1124; P < .001); the lowest rate was among those aged 40 to 44 years (rate = 538 per 100 000; 95% CI = 521, 555; P < .001). Regionally, the highest rate was observed in Alaska (rate = 1556 per 100 000; 95% CI = 1521, 1593; P < .001) with rates almost double the overall rate, while the highest number of PID encounters was in the Southwest region (15 618), reflecting the large number of AI/AN accessing IHS services in this region. The average annual rate of having a concurrent chlamydia, gonorrhea, or chlamydia and gonorrhea diagnosis during the same encounter as a PID diagnosis was 59 (95% CI = 57, 61), 15 (95% CI = 14, 16), and 4 (95% CI = 4, 5) per 100 000, respectively.
TABLE 1—
Number and Average Annual Rate of Encounters With Acute Pelvic Inflammatory Disease (PID) Diagnosis Among American Indian/Alaska Native (AI/AN) Women Aged 15 to 44 Years by Selected Characteristics: United States, Indian Health Service (IHS), 2001–2015
| No. of PID Encounters | Rate/100 000 (95% CI) | |
| Total | 44 042 | 825 (818, 833) |
| Age group, y | ||
| 15–19 | 6 939 | 645 (630, 660) |
| 20–24 | 12 014 | 1 104 (1 085, 1 124) |
| 25–29 | 9 542 | 1 018 (998, 1 038) |
| 30–34 | 6 626 | 828 (809, 848) |
| 35–39 | 5 098 | 705 (686, 725) |
| 40–44 | 3 823 | 538 (521, 555) |
| Region | ||
| Alaska | 7 187 | 1 556 (1 521, 1 593) |
| East | 1 234 | 783 (740, 828) |
| Northern Plains East | 1 629 | 476 (453, 499) |
| Northern Plains West | 5 988 | 879 (857, 901) |
| Southern Plains | 8 527 | 724 (709, 739) |
| Southwest | 15 618 | 837 (824, 850) |
| Westa | 3 859 | 595 (577, 615) |
| Concurrent STI diagnosis | ||
| Chlamydiab | 3 156 | 59 (57, 61) |
| Gonorrheab | 789 | 15 (14, 16) |
| Chlamydia and gonorrheab | 238 | 4 (4, 5) |
Note. CI = confidence interval; STI = sexually transmitted infection. PID was defined by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 098.10, 098.16, 098.17, 098.19, 098.86, 099.56, 614.0, 614.2, 614.3, 614.5, 614.8, 614.9, 615.0, and 615.9 in any of 15 diagnosis slots.24 An encounter was defined as any inpatient, outpatient, or emergency department visit. Average annual rate was calculated per 100 000 AI/AN women aged 15 to 44 y, where the number of encounters in the study period 2001 to 2015 was the numerator and the summation of the annual IHS user populations across the study period 2001 to 2015 was the denominator.
Data from the West region only reflected outpatient encounters because of the lack of IHS inpatient or emergency department facilities in the region and incomplete regional contract care information.
Concurrent STI diagnosis was defined as a codiagnosis with chlamydia or gonorrhea on the same visit as the PID diagnosis. Chlamydia was defined by ICD-9-CM codes 078.88, 079.88, 079.98, 099.41, and 099.5–099.59 in any of 15 diagnosis slots; gonorrhea was defined by ICD-9-CM codes 098.0–098.8 in any of 15 diagnosis slots.24
Health Care Setting
Comparing average annual rates of PID encounters in our study period across health care settings (Table 2), the highest overall rate of encounters occurred in the outpatient setting (642 per 100 000 AI/AN women; 95% CI = 635, 649) and was more than 10 times the rate of PID encounters in the inpatient setting (63 per 100 000; 95% CI = 61, 66). In each of the settings, the highest rates were among the group aged 20 to 24 years (inpatient: 84 per 100 000 [95% CI = 79, 90]; outpatient: 837 per 100 000 [95% CI = 820, 854]; emergency department: 219 per 100 000 [95% CI = 210, 229]), and the lowest rates were among the group aged 40 to 44 years (inpatient: 48 per 100 000 [95% CI = 42, 54]; outpatient: 432 per 100 000 [95% CI = 417, 447]; emergency department: 73 per 100 000 [95% CI = 67, 80]). Regionally, the Northern Plains East region had the lowest rate in each of the hospital settings (inpatient: 13 per 100 000 [95% CI = 9, 17]; outpatient: 450 per 100 000 [95% CI = 428, 473]; emergency department: 13 per 100 000 [95% CI = 10, 18]). The East region had the highest rate of PID encounters in the emergency department during 2001 to 2015, while Alaska had the highest rate of PID encounters in the inpatient and outpatient setting (Table 2). Within Alaska, the rate of outpatient PID encounters was almost 10 times the rate of inpatient or emergency department PID encounters (inpatient: 136 per 100 000 [95% CI = 126, 147]; outpatient: 1273 per 100 000 [95% CI = 1241, 1306]; emergency department: 148 per 100 000 [95% CI = 137, 159]). The highest rate of PID encounters with a concurrent STI diagnosis was observed in the outpatient setting (chlamydia: 52 per 100 000 [95% CI = 51, 54]; gonorrhea: 11 per 100 000 [95% CI = 10, 12]; both chlamydia and gonorrhea: 3 per 100 000 [95% CI = 3, 4]).
TABLE 2—
Number, Percentage, and Average Annual Rate of Encounters With a Pelvic Inflammatory Disease (PID) Diagnosis by Health Care Setting and Selected Characteristics Among American Indian/Alaska Native (AI/AN) Women Aged 15 to 44 Years: United States, Indian Health Service (IHS), 2001–2015
| Inpatient |
Outpatient |
Emergency Department |
||||
| No. (%) | Rate (95% CI) | No. (%) | Rate (95% CI) | No. (%) | Rate (95% CI) | |
| Total | 2 970 | 63 (61, 66) | 34 257 | 642 (635, 649) | 6 815 | 145 (142, 149) |
| Age group, y | ||||||
| 15–19 | 544 (18) | 58 (53, 63) | 5 184 (15) | 482 (469, 495) | 1 211 (18) | 129 (122, 136) |
| 20–24 | 807 (27) | 84 (79, 90) | 9 105 (27) | 837 (820, 854) | 2 102 (31) | 219 (210, 229) |
| 25–29 | 547 (18) | 66 (61, 72) | 7 544 (22) | 805 (787, 823) | 1 451 (21) | 176 (167, 185) |
| 30–34 | 416 (14) | 59 (54, 65) | 5 268 (15) | 658 (641, 676) | 942 (14) | 134 (125, 143) |
| 35–39 | 359 (12) | 56 (51, 63) | 4 087 (12) | 565 (548, 583) | 652 (10) | 103 (95, 111) |
| 40–44 | 297 (10) | 48 (42, 54) | 3 069 (9) | 432 (417, 447) | 457 (7) | 73 (67, 80) |
| Region | ||||||
| Alaska | 628 (21) | 136 (126, 147) | 5 877 (17) | 1 273 (1 241, 1 306) | 682 (10) | 148 (137, 159) |
| East | 70 (2) | 44 (35, 56) | 876 (3) | 556 (520, 594) | 288 (4) | 183 (162, 205) |
| Northern Plains East | 44 (1) | 13 (9, 17) | 1 540 (4) | 450 (428, 473) | 45 (1) | 13 (10, 18) |
| Northern Plains West | 476 (16) | 70 (64, 76) | 4 634 (14) | 680 (661, 700) | 878 (13) | 129 (121, 138) |
| Southern Plains | 435 (15) | 37 (34, 41) | 6 446 (19) | 547 (534, 561) | 1 646 (24) | 140 (133, 147) |
| Southwest | 1 317 (44) | 71 (67, 75) | 11 025 (32) | 591 (580, 602) | 3 276 (48) | 176 (170, 182) |
| Westa | . . . | . . . | 3 859 (11) | 595 (577, 615) | . . . | . . . |
| Concurrent STI diagnosis | ||||||
| Chlamydiab | 222 (7) | 5 (4, 5) | 2 798 (8) | 52 (51, 54) | 136 (2) | 3 (2, 3) |
| Gonorrheab | 126 (4) | 3 (2, 3) | 581 (2) | 11 (10, 12) | 82 (1) | 2 (1, 2) |
| Chlamydia and gonorrheab | 31 (1) | 1 (0, 1) | 184 (1) | 3 (3, 4) | 23 (0) | 0 (0, 1) |
Note. CI = confidence interval; STI = sexually transmitted infection. PID was defined by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 098.10, 098.16, 098.17, 098.19, 098.86, 099.56, 614.0, 614.2, 614.3, 614.5, 614.8, 614.9, 615.0, and 615.9 in any of 15 diagnosis slots.24 Average annual rate was calculated per 100 000 AI/AN women aged 15 to 44 years, where the number of encounters in the study period 2001 to 2015 was the numerator and the summation of the annual IHS user populations across the study period 2001 to 2015 was the denominator.
Although there were outpatient visits in each of the 7 regions listed, inpatient and emergency department encounters were not captured in the West because of lack of IHS inpatient or emergency department facilities and incomplete contract care information. For this reason, the IHS users in the West were not included in the denominator when we calculated inpatient or emergency department rates.
Concurrent STI diagnoses were defined as a codiagnosis with chlamydia or gonorrhea on the same visit as the PID diagnosis. Chlamydia was defined by ICD-9-CM codes 078.88, 079.88, 079.98, 099.41, and 099.5–099.59 in any of 15 diagnosis slots; gonorrhea was defined by ICD-9-CM codes 098.0–098.8 in any of 15 diagnosis slots.24
Trends in Pelvic Inflammatory Disease Encounters
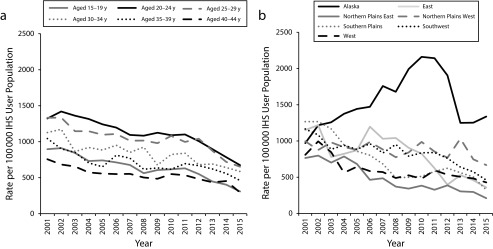
Overall, the annual rate of PID encounters decreased from 1084 (95% CI = 1048, 1120) per 100 000 AI/AN women in 2001 to 512 (95% CI = 490, 536) in 2015, representing a 52.7% total decline and an AAPC of −5.0% (95% CI = −7.0%, −2.9%; Table 3). The highest rate of PID encounters was among women aged 20 to 24 years and those living in the Alaska region nearly every year of the study period, while the lowest rate was among those aged 40 to 44 years and those living in the Northern Plains East region nearly every year of the study period (Figures 1a and 1b).
TABLE 3—
Trends in the Annual Rate of Encounters With a Pelvic Inflammatory Disease (PID) Diagnosis Among American Indian/Alaska Native (AI/AN) Women Aged 15 to 44 Years by Selected Characteristics: United States, Indian Health Service (IHS), Fiscal Years 2001–2015
| % Change in Rate of PID Encounters, (2001, 2015) | Inflection Year(s) | Trend Segment | Annual Percent Change (95% CI) | Average Annual Percent Change (95% CI) | |
| Total | −52.7 | 2008 | 2001–2008 | −4.4 (−5.7, −3.2) | −5.0 (−7.0, −2.9) |
| 2011 | 2008–2011 | 2.0 (−8.3, 13.5) | |||
| 2011–2015 | −10.8 (−14.1, −7.4) | ||||
| Age group, y | |||||
| 15–19 | −65.6 | 2008 | 2001–2008 | −6.0 (−7.6, −4.4) | −7.3 (−10.0, −4.5) |
| 2011 | 2008–2011 | 1.6 (−12.0, 17.4) | |||
| 2011–2015 | −15.4 (−20.2, −10.4) | ||||
| 20–24 | −49.0 | 2012 | 2001–2012 | −2.8 (−3.6, −1.9) | −5.0 (−6.5, −3.5) |
| 2012–2015 | −12.6 (−19.2, −5.5) | ||||
| 25–29 | −51.0 | 2007 | 2001–2007 | −4.4 (−6.8, −1.9) | −5.1 (−7.3, −3.0) |
| 2012 | 2007–2012 | 0.2 (−4.5, 5.2) | |||
| 2012–2015 | −14.8 (−21.7, −7.3) | ||||
| 30–34 | −48.0 | . . . | . . . | −3.9 (−5.1, −2.8) | |
| 35–39 | −55.8 | . . . | . . . | −3.9 (−5.2, −2.6) | |
| 40–44 | −61.2 | . . . | . . . | −4.0 (−5.2, −2.8) | |
| Region | |||||
| Alaska | 37.9 | 2010 | 2001–2010 | 8.6 (5.5, 11.8) | 1.1 (−1.4, 3.8) |
| 2010–2015 | −11.0 (−16.4, −5.3) | ||||
| East | −68.8 | 2008 | 2001–2008 | −0.4 (−6.9, 6.5) | −7.3 (−11.5, −2.9) |
| 2008–2015 | −13.7 (−20.5, −6.3) | ||||
| Northern Plains East | −72.4 | . . . | . . . | −8.5 (−10.2, −6.8) | |
| Northern Plains West | −33.0 | . . . | . . . | −1.3 (−2.7, 0.1) | |
| Southern Plains | −74.4 | 2009 | 2001–2009 | −11.8 (−14.3, −9.1) | −9.5 (−14.7, −4.0) |
| 2013 | 2009–2013 | 4.7 (−10.6, 22.6) | |||
| 2013–2015 | −25.0 (−48.1, 8.3) | ||||
| Southwest | −60.5 | 2003 | 2001–2003 | −11.3 (−26.1, 6.6) | −6.2 (−9.0, −3.2) |
| 2011 | 2003–2011 | −1.2 (−3.9, 1.5) | |||
| 2011–2015 | −13.0 (−19.4, −6.1) | ||||
| Westa | −46.9 | . . . | . . . | −4.6 (−6.3, −2.9) | |
| Type of carea | |||||
| Inpatient | −63.9 | 2011 | 2001–2011 | −2.4 (−4.1, −0.7) | −6.9 (−9.3, −4.5) |
| 2011–2015 | −17.3 (−24.6, −9.3) | ||||
| Outpatient | −52.1 | 2008 | 2001–2008 | −4.9 (−6.6, −3.1) | −4.8 (−7.5, −2.0) |
| 2011 | 2008–2011 | 3.7 (−10.0, 19.5) | |||
| 2011–2015 | −10.5 (−14.8, −6.0) | ||||
| Emergency department | −49.7 | . . . | . . . | −4.6 (−5.8, −3.3) | |
| Concurrent STI diagnosisb | |||||
| Chlamydia | 157.5 | 2010 | 2001–2010 | 22.5 (17.3, 27.9) | 6.1 (2.5, 9.8) |
| 2010–2015 | −18.1 (−24.2, −11.5) | ||||
| Gonorrhea | 91.5 | . . . | . . . | 5.5 (2.1, 9.0) | |
| Chlamydia and gonorrheac | . . . | 2010 | 2004–2010 | 32.2 (15.1, 51.9) | 16.3 (1.1, 33.7) |
| 2013 | 2010–2013 | −20.1 (−54.7, 40.8) | |||
| 2013–2015 | 38.8 (−18.9, 137.6) |
Note. CI = confidence interval; STI = sexually transmitted infection. PID was defined by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 098.10, 098.16, 098.17, 098.19, 098.86, 099.56, 614.0, 614.2, 614.3, 614.5, 614.8, 614.9, 615.0, and 615.9 in any of 15 diagnosis slots.24 An encounter was defined as any inpatient, outpatient, or emergency department visit. Annual rate was calculated per 100 000 AI/AN women aged 15 to 44 years, where the number of encounters in the study period 2001 to 2015 was the numerator and the summation of the annual IHS user populations across the study period 2001 to 2015 was the denominator.
Although there were outpatient visits in each of the 7 regions listed, inpatient and emergency department encounters were not captured in the West because of lack of IHS inpatient or emergency department facilities and incomplete contract care information. For this reason, the IHS users in the West were not included in the denominator when we calculated inpatient or emergency department rates.
Concurrent STI diagnoses were defined as a codiagnosis with chlamydia or gonorrhea on the same encounter as the PID diagnosis. Chlamydia was defined by ICD-9-CM codes 078.88, 079.88, 079.98, 099.41, and 099.5–099.59 in any of 15 diagnosis slots; gonorrhea was defined by ICD-9-CM codes 098.0–098.8 in any of 15 diagnosis slots.24
Because of a low number of PID encounters with a concurrent diagnosis of both chlamydia and gonorrhea in 2001, 2002, and 2003, the trend analysis was performed during 2004 through 2015.
FIGURE 1—
Trends and Significance for Annual Ratesa of Encounters With a Pelvic Inflammatory Disease (PID) Diagnosisb Among American Indian/Alaska Native (AI/AN) Women Aged 15 to 44 Years by (A) Age Group and (B) Region: United States, Indian Health Service (IHS), Fiscal Years 2001 Through 2015
Note. Except for the line for Alaska in part b, all lines indicate a statistically significant trend test at P < .05.
aAnnual rate is calculated per 100 000 AI/AN women aged 15 to 44 years for the corresponding IHS use population for each stratified group.
bPelvic inflammatory disease is defined by codes 098.10, 098.16, 098.17, 098.19, 098.86, 099.56, 614.0, 614.2, 614.3, 614.5, 614.8, 614.9, 615.0, and 615.9 in any of 15 diagnosis slots. Encounter is defined as any inpatient, outpatient, or emergency department visit.
There was a significant decrease in the annual rate of PID encounters during 2001 through 2015 among all age groups (P < .001; Figure 1a). The largest decrease in PID encounters during 2001 to 2015 was among women aged 15 to 19 years (total: −65.6%; AAPC: −7.3; 95% CI = −10.0%, −4.5%), compared with all older age groups (Table 3). All regions except Alaska experienced a significant decline in the annual rate of PID encounters during the study period (P < .001 for all regions except the Northern Plains West where P = .03; Figure 1b). The largest decrease in the annual rate of PID encounters was among women living in the Southern Plains region (total: −74.4%; AAPC = −9.5; 95% CI = −14.7%, −4.0%; Table 3). The annual PID encounter rate in the Alaska region remained stable during the study period (total: 37.9%; AAPC = 1.1%; 95% CI = −1.4%, 3.8%). Despite this overall stability, there was an inflection point in the Alaska region in 2010, with large increases observed during 2001 to 2010 (APC = 8.6%; 95% CI = 5.5%, 11.8%) followed by even larger decreases during 2010 to 2015 (APC = −11.0%; 95% CI = −16.4%, −5.3%). The rate of PID encounters in Alaska was 2.6 times the IHS national average in 2015 (data not shown).
The annual rate of PID encounters also decreased in all health care settings (Table 3). The largest decrease in the rate of PID encounters during 2001 to 2015 was among women receiving inpatient care (total: −63.9%; AAPC = −6.9%; 95% CI = −9.3%, −4.5%), while lower decreases in the rate of PID encounters were observed in the outpatient setting (total: −52.1%; AAPC= −4.8%; 95% CI = −7.5%, −2.0%) and emergency department setting (total: −49.7%; APC= −4.6%; 95% CI = −5.8%, −3.3%).
Factoring in the presence of a concurrent STI diagnosis, there were substantial increases in the annual rate of PID encounters during 2001 to 2015 among those with a concurrent chlamydia and gonorrhea diagnosis (Table 3). The increases were more pronounced in those with a concurrent chlamydia diagnosis, with a total percent increase of 157.5% (AAPC = 6.1%; 95% CI = 2.5%, 9.8%). Despite this overall increase, there was an inflection point in this group in 2010, with large increases observed during 2001 to 2010 (APC = 22.5%; 95% CI = 17.3%, 27.9%) followed by equally large decreases during 2010 to 2015 (APC = −18.1%; 95% CI = −24.2%, −11.5%).
DISCUSSION
Our study demonstrated decreasing trends of PID encounters across all age groups and health care settings among AI/AN women receiving care supported by the IHS during 2001 to 2015. A previous study using data from the Healthcare Cost Utilization Project evaluating trends in diagnoses of acute PID in a nationally representative sample of emergency departments found similar decreases in emergency department visits with a PID diagnosis during 2006 through 2013 but excluded other health care settings. Similar to our study, ICD-9-CM codes were used for case identification; however, analyses by race/ethnicity were not possible because of the lack of race/ethnicity in the Healthcare Utilization Project data.11 This is the first study to examine trends in PID encounters in AI/AN women and was only possible using a unique and comprehensive health care data set that captures data from all health care hospitalizations, outpatient visits, and emergency department visits for AI/AN people cared for within a system of federal, tribal, and urban clinics. Because AI/AN people only represent about 2% of the US population and are typically underrepresented within national data sets, estimates of PID among AI/AN women cannot be reliably determined with other data sources.19
We found higher annual PID encounter rates among women with concurrent STI diagnoses. Although our study measured the presence of concurrent STI diagnoses with a PID diagnosis, we could not estimate how many of the PID diagnoses could be attributed to current or previous chlamydial or gonococcal infections. Estimates regarding the population attributable fraction of PID to chlamydial or gonococcal infections vary, although they are both frequently isolated bacteria from patients with PID.29–32
Rates were highest among women living in the Alaska region. Data from the Alaska Department of Health and Social Services show a significant increase of reported gonorrhea cases in Alaska during 2008 to 2010. Many of these reported cases of gonorrhea were coinfected with chlamydia.33,34 Because of these increases, the Alaska Department of Health and Social Services requested assistance in 2010 from the Centers for Disease Control and Prevention (CDC) in the form of an Epi-Aid, which is the mechanism by which CDC investigates urgent public health problems. Collaborating with state and tribal health officials, the Epi-Aid investigated possible prevention and control strategies and found that patients and providers in Alaska were willing to use expedited partner therapy, the practice of providing medications to infected patients to give to their sexual partners.34 Following the investigation, the Alaska Department of Health recommended expedited partner therapy, and in the following years, gonorrhea case rates in Alaska decreased.34 The Epi-Aid assisted in increasing awareness of and screening for STIs, implementation and legalization of expedited partner therapy in the state of Alaska, and ultimately lowering STI rates and possibly STI sequelae, such as PID.
Our results show that, similar to rates of reported gonorrhea, rates of PID encounters increased in Alaska during 2001 to 2010, followed by a dramatic decrease during 2010 to 2015. Though no causal relationship can be assumed between rates of gonorrhea and rate of PID encounters, an ecologic link may exist. As AI/AN people can (and do) seek care outside of tribal clinics, resulting in data from IHS not exactly overlapping data for the entire state of Alaska, we evaluated trends in chlamydia and gonorrhea encounters in IHS facilities during the study period and found similar trends to those identified for PID.
The highest decreases in PID encounters observed in this study in the inpatient compared with outpatient and emergency department setting coincides with the increased treatment of PID in the outpatient setting in recent years. Recommendations changed in the late 1990s regarding the appropriate treatment location for PID on the basis of evidence from a randomized controlled trial indicating no difference in outcomes to PID whether randomized to inpatient or outpatient treatment.35 Since that time, there has been a transition from PID being treated in inpatient settings to increased treatment in outpatient settings, a phenomenon that is supported by the results of this study.
Limitations
Our study is subject to several limitations. First, our study was based on encounter and not patient-level data, allowing the possibility for a person to be represented more than once if she had more than 1 encounter for PID during the study period. As patients with multiple STI events or a previous PID diagnosis are more likely to be diagnosed with a subsequent episode of PID, these results should be interpreted cautiously when compared with other studies describing PID or STIs with patient-level data. Also, PID is often incorrectly diagnosed because of the inherent diagnostic difficulties surrounding it, which requires providers to make a clinical diagnosis on the basis of nonspecific signs and symptoms.8 However, there is no reason to expect that the trend of inaccurate diagnoses among providers would have changed over time. Given consistent inaccurate diagnoses throughout all years of the study, the observed trends would not have been impacted.
Second, the use of ICD-9-CM codes has been shown to have a modest positive predictive value for identifying PID, potentially underestimating the true rates of PID encounters.25 Also, we did not validate the ICD-9-CM codes used to identify PID encounters. Coding, diagnostic, and treatment practices may vary by region and over time, although the selected ICD-9-CM codes and findings were consistent with those from other studies.10,25–27 To corroborate the ICD-9-CM codes used to identify PID encounters, we evaluated other codes assigned to the same encounter and found a majority were consistent with a diagnosis of PID (Table B, available as a supplement to the online version of this article at http://www.ajph.org). In addition, given that ICD-9-CM codes are assigned to an encounter before the receipt of laboratory results to confirm (or rule out) an infection with chlamydia or gonorrhea, the results regarding a concurrent infection should be interpreted cautiously.
Third, because the West region does not have IHS-operated hospitals and emergency departments, we were unable to evaluate the burden of inpatient and emergency department PID encounters in this region, which could affect calculated rates and interpretation. However, we have no reason to believe that the West region would have different inpatient or emergency department findings than the other regions; observed decreases in outpatient PID encounters are similar to other regions.
Finally, because our data source is limited to encounters among patients accessing the IHS federal, tribal, and urban facilities, our results might not be generalizable to AI/AN patients outside the IHS system.
Public Health Implications
To our knowledge, this is the first study to examine trends in rates of PID encounters among AI/AN women, a population disproportionally affected by STIs. The results of our study coincide with other national estimates for decreasing trends of PID and offers insight into the utility of discharge data sets in the surveillance and examination of PID trends. Prevention of PID relies heavily on screening programs to prevent and control STIs. Efforts to increase STI screening are under way at IHS, and interventions including electronic health record reminders, provider education, and standing orders are being evaluated. These strategies could help to decrease rates of STIs and, subsequently, PID and other reproductive sequelae, as well. Outside the IHS system, enhancing community awareness on the long-term effects of STIs, decreasing stigma, and improving access to care and services is also critical. Future analyses will aim to further understand the contribution of STIs in AI/AN women to the subsequent development of PID and to evaluate long-term reproductive consequences, such as infertility and ectopic pregnancy. Future efforts will also aim to incorporate patient identifiers to evaluate the number of AI/AN women impacted by PID.
HUMAN PARTICIPANT PROTECTION
This study was determined to be public health practice and nonresearch and was exempt from institutional review board review.
REFERENCES
- 1.Westrom L, Eschenbach D. Pelvic inflammatory disease. In: Holmes KK, Sparling PF, Stamm WE, editors. Sexually Transmitted Diseases. 4th ed. New York, NY: McGraw-Hill; 2008. pp. 783–809. [Google Scholar]
- 2.Weström L, Joesoef R, Reynolds G, Hagdu A, Thompson SE. Pelvic inflammatory disease and fertility. A cohort study of 1,844 women with laparoscopically verified disease and 657 control women with normal laparoscopic results. Sex Transm Dis. 1992;19(4):185–192. [PubMed] [Google Scholar]
- 3.Haggerty CL, Gottlieb SL, Taylor BD, Low N, Xu F, Ness RB. Risk of sequelae after Chlamydia trachomatis genital infection in women. J Infect Dis. 2010;201(suppl 2):S134–S155. doi: 10.1086/652395. [DOI] [PubMed] [Google Scholar]
- 4.Oakeshott P, Kerry S, Aghaizu A et al. Randomised controlled trial of screening for Chlamydia trachomatis to prevent pelvic inflammatory disease: the POPI (Prevention of Pelvic Infection) trial. BMJ. 2010;340:c1642. doi: 10.1136/bmj.c1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scholes D, Stergachis A, Heidrich FE, Andrilla H, Holmes KK, Stamm WE. Prevention of pelvic inflammatory disease by screening for cervical chlamydial infection. N Engl J Med. 1996;334(21):1362–1366. doi: 10.1056/NEJM199605233342103. [DOI] [PubMed] [Google Scholar]
- 6.LeFevre ML. Screening for chlamydia and gonorrhea: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161(12):902–910. doi: 10.7326/M14-1981. [DOI] [PubMed] [Google Scholar]
- 7.Kreisel K, Torrone E, Bernstein K, Hong J, Gorwitz R. Prevalence of pelvic inflammatory disease in sexually experienced women of reproductive age—United States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2017;66(3):80–83. doi: 10.15585/mmwr.mm6603a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Pelvic inflammatory disease (PID): CDC Fact Sheet. 2016. Available at: http://www.cdc.gov/std/pid/STDFact-PID.htm. Accessed September 26, 2017.
- 9.Sutton MY, Sternberg M, Zaidi A, St Louis ME, Markowitz LE. Trends in pelvic inflammatory disease hospital discharges and ambulatory visits, United States, 1985–2001. Sex Transm Dis. 2005;32(12):778–784. doi: 10.1097/01.olq.0000175375.60973.cb. [DOI] [PubMed] [Google Scholar]
- 10.Bohm MK, Newman L, Satterwhite CL, Tao G, Weinstock HS. Pelvic inflammatory disease among privately insured women, United States, 2001–2005. Sex Transm Dis. 2010;37(3):131–136. doi: 10.1097/OLQ.0b013e3181bf576f. [DOI] [PubMed] [Google Scholar]
- 11.Kreisel K, Flagg EW, Torrone E. Trends in pelvic inflammatory disease emergency department visits, United States, 2006–2013. Am J Obstet Gynecol. 2018;218(1):117.e1–117.e10. doi: 10.1016/j.ajog.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Leichliter JS, Chandra A, Aral SO. Correlates of self-reported pelvic inflammatory disease treatment in sexually experienced reproductive-aged women in the United States, 1995 and 2006–2010. Sex Transm Dis. 2013;40(5):413–418. doi: 10.1097/OLQ.0b013e318285ce46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walker FJ, Llata E, Doshani M et al. HIV, chlamydia, gonorrhea, and primary and secondary syphilis among American Indians and Alaska Natives within Indian Health Service areas in the United States, 2007–2010. J Community Health. 2015;40(3):484–492. doi: 10.1007/s10900-014-9961-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2016. Atlanta, GA: US Department of Health and Human Services; 2017. [Google Scholar]
- 15.Centers for Disease Control and Prevention and Indian Health Service. Indian Health Surveillance report—sexually transmitted diseases 2011. Atlanta, GA: US Department of Health and Human Services; 2014. [Google Scholar]
- 16.Thoroughman DA, Frederickson D, Cameron HD, Shelby LK, Cheek JE. Racial misclassification of American Indians in Oklahoma state surveillance data for sexually transmitted diseases. Am J Epidemiol. 2002;155(12):1137–1141. doi: 10.1093/aje/155.12.1137. [DOI] [PubMed] [Google Scholar]
- 17.Indian Health Service. Trends in Indian Health, 2014 Edition. Available at: https://www.ihs.gov/dps/includes/themes/responsive2017/display_objects/documents/Trends2014Book508.pdf. Accessed May 9, 2018.
- 18. Indian Health Service. IHS profile. Available at: https://www.ihs.gov/newsroom/factsheets/ihsprofile. Accessed May 9, 2018.
- 19.US Census Bureau. The American Indian and Alaska Native population: 2010. 2010 Census Briefs. Available at: https://www.census.gov/prod/cen2010/briefs/c2010br-10.pdf. Accessed May 9, 2018.
- 20.Indian Health Service. 2017. IHS expenditures per capita and other federal health care expenditures per capita. Available at: https://www.ihs.gov/ihcif/includes/themes/responsive2017/display_objects/documents/2018/2017_IHS_Expenditures.pdf. Accessed May 9, 2018.
- 21.Indian Health Service. FY 2017 Indian Health Service level of need funded (LNF) calculation: resources needed, resources available, and LNF scores summarized by IHS area. Available at: https://www.ihs.gov/ihcif/includes/themes/responsive2017/display_objects/documents/2018/FY_2017_LevelofNeedFunded_(LNF)_Table.pdf. Accessed May 9, 2018.
- 22.Gordon PH, Mehal JM, Holman RC, Rowland LP, Rowland AS, Cheek JE. Incidence of amyotrophic lateral sclerosis among American Indians and Alaska Natives. JAMA Neurol. 2013;70(4):476–480. doi: 10.1001/jamaneurol.2013.929. [DOI] [PubMed] [Google Scholar]
- 23.Mehal JM, Holman RC, Vora NM, Blanton J, Gordon PH, Cheek JE. Encephalitis-associated hospitalizations among American Indians and Alaska Natives. Am J Trop Med Hyg. 2014;90(4):755–759. doi: 10.4269/ajtmh.13-0420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.International Classification of Diseases, Ninth Revision, Clinical Modification. Hyattsville, MD: National Center for Health Statistics; 1980. [Google Scholar]
- 25.Satterwhite CL, Yu O, Raebel MA et al. Detection of pelvic inflammatory disease: development of an automated case-finding algorithm using administrative data. Infect Dis Obstet Gynecol. 2011;2011:428351. doi: 10.1155/2011/428351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Owusu-Edusei K, Bohm MK, Chesson HW, Kent CK. Chlamydia screening and pelvic inflammatory disease: insights from exploratory time-series analyses. Am J Prev Med. 2010;38(6):652–657. doi: 10.1016/j.amepre.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 27.Goyal M, Hersh A, Luan X, Localio R, Trent M, Zaoutis T. National trends in pelvic inflammatory disease among adolescents in the emergency department. J Adolesc Health. 2013;53(2):249–252. doi: 10.1016/j.jadohealth.2013.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Indian Health Service. National Patient Information Reporting System: National Data Warehouse. NPIRS Basic Business Rules. Available at: https://www.ihs.gov/NDW/documents/WUPS/NPIRS_Basic_Business_Rules.pdf. Accessed May 9, 2018.
- 29.Kristensen GB, Bollerup A, Lind K et al. Infections with Neisseria gonorrhoeae and Chlamydia trachomatis in women with acute salpingitis. Genitourin Med. 1985;61(3):179–184. doi: 10.1136/sti.61.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Møller BR, Mardh P-A, Ahrons S, Nussler E. Infection with Chlamydia trachomatis, Mycoplasma hominis, and Neisseria gonorrhoeae in patients with acute pelvic inflammatory disease. Sex Transm Dis. 1981;8(3):198–202. [PubMed] [Google Scholar]
- 31.Eschenbach DA, Buchanan TM, Pollock HM et al. Polymicrobial etiology of acute pelvic inflammatory disease. N Engl J Med. 1975;293(4):166–171. doi: 10.1056/NEJM197507242930403. [DOI] [PubMed] [Google Scholar]
- 32.Sweet RL, Draper D, Schachter J, James J, Hadley W, Brooks G. Microbiology and pathogenesis of acute salpingitis as determined by laparoscopy: what is the appropriate site to sample? Am J Obstet Gynecol. 1980;138(7 pt 2):985–989. doi: 10.1016/0002-9378(80)91093-5. [DOI] [PubMed] [Google Scholar]
- 33. State of Alaska. Statewide increase in gonococcal infection—Alaska, 2009. Anchorage, AK: Department of Health and Social Services, Division of Public Health; 2010.
- 34. State of Alaska. An assessment of expedited partner therapy for enhanced gonorrhea and chlamydia control in Alaska. Anchorage, AK: Department of Health and Social Services, Division of Public Health; 2011.
- 35.Ness RB, Trautmann G, Richter HE et al. Effectiveness of treatment strategies of some women with pelvic inflammatory disease: a randomized trial. Obstet Gynecol. 2005;106(3):573–580. doi: 10.1097/01.AOG.0000175193.37531.6e. [DOI] [PubMed] [Google Scholar]