Abstract
Purpose:
Recent data suggest great variability in costs for surgical hospitalization for spinal surgery. However, the magnitude of expenditures attributable to complications is unknown. The purpose of this study is to describe cost of care associated with surgical and medical complications after cervical spine surgery.
Materials and Methods:
A retrospective cohort study utilizing the National Inpatient Sample years 2002–2014 was conducted. A weighted sample of 901,508 adults undergoing elective cervical fusion for degenerative indications was extracted using diagnostic and procedure codes. Twelve categories of major complications were identified, and patient/hospital variables were evaluated as predictors of the overall reimbursed cost using multivariate regression. Mean differences (B) and 95% confidence intervals were reported.
Results:
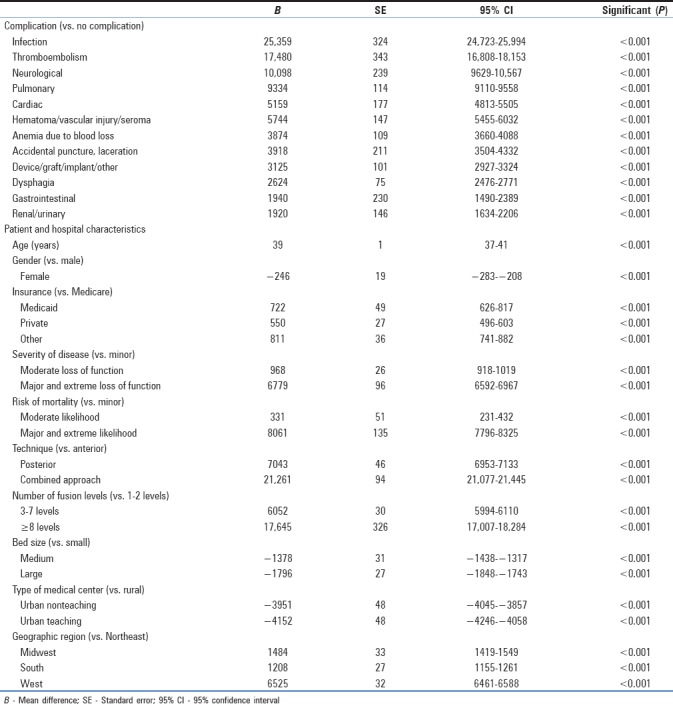
The mean age was 52.2 ± 11.4 years, with 5.2% of patients experiencing a complication. Mean overall increase in inflation-adjusted cost associated with complication was $16,435 ± 10,358, varying significantly by type of complication, surgical approach, and number of levels fused. The most common complications and their attributed costs were dysphagia (1.6%, B = $2624 [2476–2771], P < 0.001), pulmonary complications (1.0%, B = $9334 [9110–9558], P < 0.001), and device-related complications (0.9%, B = $3125 [2927–3324], P < 0.001). The costliest complications were infection (0.1%, B = $25359 [24723–25994], P < 0.001), thromboembolism (0.1%, B = $17480 [16808–18153], P < 0.001), and neurological complications (0.2%, B = $10098 [9629–10567], P < 0.001).
Conclusions:
Although complications are rare after elective cervical fusion, they are associated with dramatically increase costs of care as high as $25,359 in the setting of postoperative infection. Improved understanding of the economic magnitude of complications may help guide efforts in reducing health care spending and improving perioperative care.
Keywords: Cervical fusion, degenerative spine disease, health economics, inpatient complications, reimbursement
INTRODUCTION
Spine surgery to treat degenerative diseases in older patients and its associated costs has increased over the past two decades in the United States (US). Within a progressively aging population, analyses of trends have revealed a rise in the number of cervical procedures, an increase in costs from $12,933 in 2002 to $19,130 in 2010, comparatively shorter hospital stays, and low mortality.[1,2,3] Reasons for increasing costs include additional medical charges to manage older, more comorbid patients, regional variability in service delivery, and the impact of specialized instrumentation and advanced techniques in spinal fusion.[1,4] Evidence-based spine surgery, especially in an expensive health-care climate, dictates the need to improve the characterization of major perioperative events that contribute to morbidity and growing health-care expenditures.
Anterior cervical fusion (ACF) remains the most frequently used approach taken for cervical interbody fusion; however, in patients with severe stenosis and multilevel involvement, outcomes compared to posterior cervical fusion (PCF) are equivalent.[5] The surgical strategy relies on individual pathology and surgeon preference, and risks of complications exist for each approach.[6,7] Procedural risks to ACF include retraction-related injury to the hypoglossal and recurrent laryngeal nerves, esophagus, trachea, and nearby vascular structures.[8,9] PCF is associated with increased spinal cord, nerve root, or vascular injury.[10,11]
While cost trends of cervical fusion by patient, hospital, and regional variability have been previously reported,[1,2,4] an in-depth economic analysis of the costs associated with complications lacks in the literature. In a shifting climate of health-care economics, accurately assessing savings achieved in reducing complications have become increasingly necessary. The goal of this study is to describe the incidence of inpatient complications and identify the costliest complications after cervical spinal fusion.
MATERIALS AND METHODS
Data source
We extracted data from the National Inpatient Sample (NIS) years 2002–2014, which is sponsored and maintained by the Agency for Healthcare Research and Quality (AHRQ). Data use agreements were completed, and all AHRQ guidelines were followed. The NIS is the largest all-payer inpatient database in the US containing approximately seven million hospital discharges each year, which provides a stratified sample of 20% of all hospitals to represent 95% of the national population. Each case includes the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes. All patients’ data are de-identified, and the Institutional Review Board approval was not required. The statement of Human and Animal Rights is not applicable to our study.
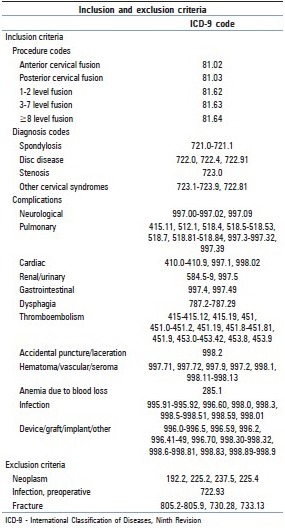
Inclusion and exclusion criteria
We queried for all patients at least 18 years old undergoing elective cervical fusion for spine degeneration [Supplementary Table 1]. Procedures are subcategorized by the number of levels fused (1–2 levels, 3–7 levels, and ≥8 levels) and by surgical approach (anterior, posterior, and combined). We excluded patients with the following diagnoses: all neoplasms associated with the spinal cord, spinal meninges, or nerve sheaths; intraspinal abscess; osteomyelitis; and spinal fractures.
Supplementary Table 1.
Inclusion and exclusion criteria
Patient, hospital characteristics, and cost
Patient demographics and clinical variables include age, sex (male and female), race (Caucasian, African–American, Hispanic, and other), insurance (Medicare, Medicaid, private, and other), severity of illness (minor, moderate, and major/extreme), and mortality risk (minor, moderate, and major/extreme) as determined by All Patient Refined Disease-Related Group. Hospital variables include US region (Northeast, Midwest, South, and West), location/teaching status (rural, urban nonteaching, and urban teaching), and bed size (small, medium, and large).
Complications and cost
Inpatient complications were extracted using ICD-9-CM diagnosis codes and comprised the following: neurological, pulmonary, cardiac, renal/urinary, gastrointestinal, dysphagia, thromboembolism, accidental puncture/laceration, hematoma/vascular/seroma, anemia from blood loss, infection, and device/graft/implant/other [Supplementary Table 1]. We dichotomized patients into with and without complications. Cost was calculated from the hospital charge and the year-specific, hospital-specific cost-to-charge ratio provided by AHRQ (charge × [cost/charge ratio]). Inflation was adjusted to 2014 US dollar values.
Statistical analysis
Descriptive variables are presented using proportions for categorical variables and means and standard errors for continuous variables. National estimates were calculated using the weighted discharges supplied by AHRQ. Analyses of variance and multivariable linear regression analyses of the weighted sample were performed evaluating for predictors of the total estimated cost. Multivariable regression adjusted for the demographic and clinical variables. Mean differences (B) and 95% confidence intervals were reported. A statistical significance was assessed at P = 0.001. No data were reported for any groups with <10 patients. All data extraction, aggregation, and statistical analyses were executed using the Statistical Package for the Social Sciences, version 25 (IBM Corporation, Chicago, IL, USA).
RESULTS
Patient characteristics
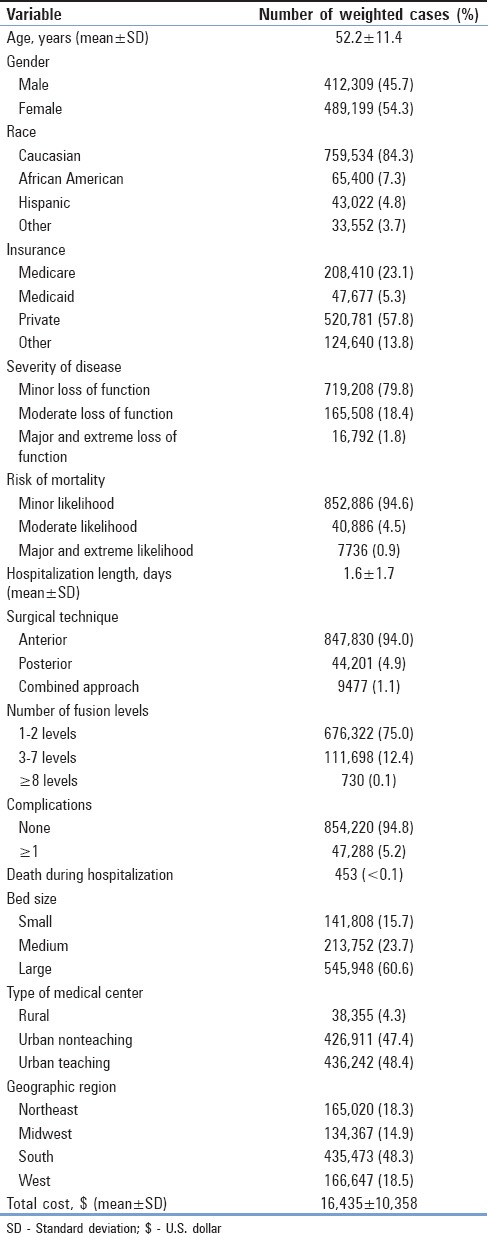
A weighted sample of 901,508 adults was identified between 2002 and 2014. Patients were 52.2 ± 11.4 years old, 54.3% of females, 84.3% Caucasian, and 57.8% privately insured. Mean hospitalization was 1.6 ± 1.7 days with an overall cost of $16435 ± 10358 per hospital admission [Table 1]. Most patients had minor loss of function (79.8%) and minor mortality risk (94.6%). ACF was most frequently utilized (94.0%), and 1–2 levels’ fusions comprised 75.0% of patients. Supplementary Table 2 shows univariate analysis of patient variables and overall cost.
Table 1.
Patient and hospital characteristics
Supplementary Table 2.
Univariate analysis of cost for patient and hospital characteristics
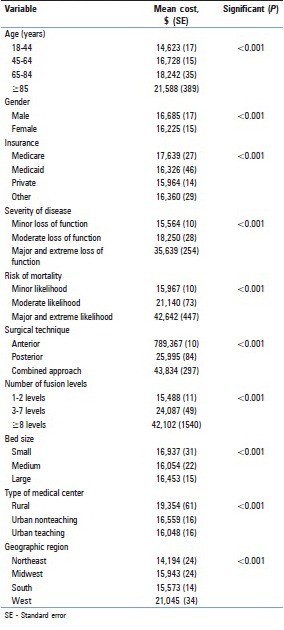
Multivariate linear regression indicated that age per year increment (B = $39 [37, 41], P < 0.001) and female patients (B = −$246 [−283, −208], P < 0.001) associated with decreased cost. Relative to Medicare, hospitals received more reimbursements for Medicaid (B = $722 [626, 817], P < 0.001), private (B = $550 [496, 603], P < 0.001), and other insurance (B = $811 [741, 882], P < 0.001). PCF (B = $7043 [6953, 7133], P < 0.001) and combined (B = $21261 [21,077, 21,445], P < 0.001) approach had higher cost relative to ACF. Three-to-seven levels’ fusions (B = $6052 [5994, 6110], P < 0.001) and 8 levels’ fusions (B = $17645 [17,007, 18,284], P < 0.001) were more expensive.
Hospital characteristics
Supplementary Table 2 shows the univariate analysis of hospital characteristics. Most procedures were done in hospitals with large bed size (60.6%), urban nonteaching hospitals (47.4%), and the South (48.3%). Multivariate analysis showed decreased cost in urban teaching hospitals (B = -$3951 [−4045, −3857], P < 0.001) and urban nonteaching hospitals (B = −$4152 [−4246,−4058], P < 0.001) compared to rural hospitals. Medium (B = −$1378 [−1438, −1317], P < 0.001]) and large (B = −$1796 [−1848 to − 1743], P < 0.001) hospitals had lower inpatient costs. Surgeries in the Midwest (B = $1484 [1419, 1549], P < 0.001), South (B = $1208 [1155, 1261], and West (B = $6525 [6461, 6588], P < 0.001) had higher costs.
Complications
Table 2 shows the incidences and univariate analyses. Dysphagia (1.6%) was the most common complication, followed by pulmonary (1.0%), device related (0.9%), anemia from blood loss (0.8%), renal/urinary (0.4%), hematoma/vascular/seroma (0.4%), cardiac (0.3%), gastrointestinal (0.2%), neurological (0.2%), accidental puncture/laceration (0.2%), thromboembolism (0.1%), and infection (0.1%). A total of 42 (<0.1%) inpatient deaths occurred. In patients who died, complication incidences were pulmonary (65.2%), cardiac (25.7%), renal/urinary (15.7%), neurological (14.9%), infection (13.9%), hematoma/vascular/seroma (10.6%), thromboembolism (9.6%), anemia (4.8%), and dysphagia (2.7%) [Table 2].
Table 2.
Univariate analysis of cost for complications
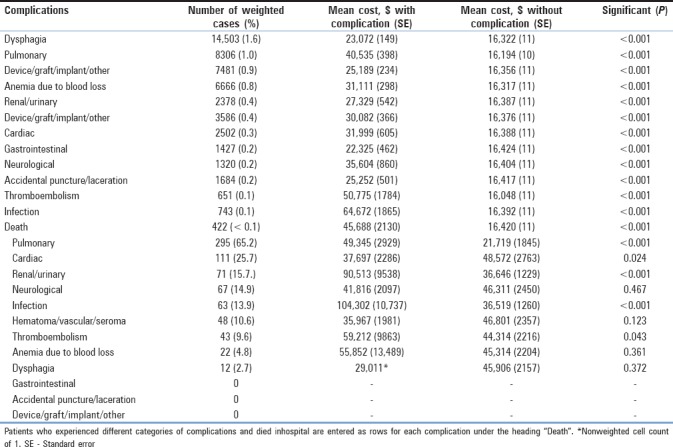
Table 3 shows multivariate regression of cost of care for each complication. Infection associated with highest increase in cost (B = $25359 [24,723, 25,994], P < 0.001), followed by thromboembolism (B = $17480 [16,808, 18,153], P < 0.001), neurological (B = $10,098 [9629, 10567], P < 0.001), pulmonary (B = $9334 [9110, 9558], P < 0.001), cardiac (B = $5159 [4813, 5505], P < 0.001], hematoma/vascular/seroma (B = $5744 [5455, 6032], P < 0.001), anemia (B = $3874, [3660, 4088], P < 0.001), puncture/laceration (B = $3918 [3504, 4332], P < 0.001), device related (B = $3125 [2927, 3324], P < 0.001), dysphagia (B = $2624 [2476, 2771], P < 0.001), gastrointestinal (B = $1940 [1490, 2389], P < 0.001), and renal/urinary (B = $1920 [1634, 2206], P < 0.001).
Table 3.
Multivariate regression of overall hospital cost
DISCUSSION
In a weighted national sample of elective cervical fusion patients, we show that inhospital costs associated not only with the presence of complications but also that complication-associated costs vary greatly by the specific types of complication. Previous investigations have discussed general cost and procedure volume trends in the past two decades;[1,2,3,4] however, the absence of cost analysis controlling for complications has precluded the potential to understand the drivers of variation in spending. Findings from the present study may serve as evidence to assist with clinical strategies to provide cost-effective surgical care and expedite recovery.
Trends in care, outcomes, and cost
The overall cost of treatment and hospitalization was $16435 ± 10358. Our inflation-adjusted cost analysis demonstrates that spending increased 37.5%, from $13,545 to $18,626 between 2002 and 2011. This is consistent with previous results as well as with the trends in other spine surgeries.[1,3,4] Notably, cost declined 13.7% to $16,080 between 2012 and 2014 [Figure 1], which may parallel the shifts in health-care delivery in this period. National reforms under the Affordable Care Act beginning in 2010 steered away from volume-based, fee-for-service reimbursement, toward bundled-payment and performance-linked initiatives.[12] We show that overall charges have increased at a greater rate than cost [Figure 1]. When estimating health-care costs, the distinction between charge versus cost should not be overlooked. We see that Medicare status associated with lower reimbursement, and thus, the impact of payer status on health-care economics should be closely monitored in a progressively older patient population.
Figure 1.
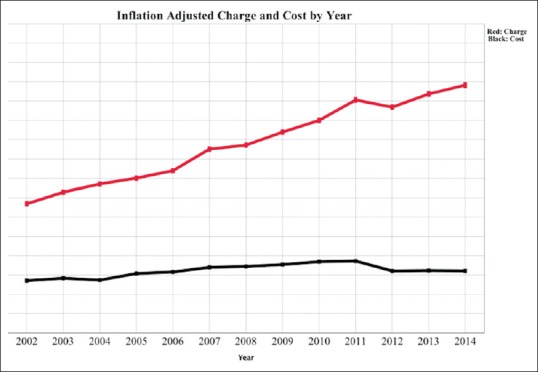
Cervical fusion, inflation adjusted charge and cost by year. Mean per patient charge versus cost for patients undergoing elective cervical fusion in the National Inpatient Sample years 2002–2014
Health-care costs increase with disease severity and mortality risk, likely from more intensive postoperative care acuity. For patients who need extensive stabilization, 3–7 levels’ fusions increase costs by $6052 and ≥8 levels’ fusions increase costs by $17,645. ACF is more commonly performed (94.8%) and less expensive compared to PCF and combined approaches [Figure 2]. PCF often involves additional instrumentation, and combined approach is reserved for patients with complex cervical disease entities. Older age and male gender associated with marginal increases in expenditure. In line with prior findings,[4] we report lower costs at high-volume, urban institutions, demonstrating possible economic leverage specific to larger institutions. Surgery in the western US is the most expensive and the least expensive in the Northeast. Reasons for the geographic differences are not well understood, which may reflect differences in labor cost, administrative and medical infrastructure, and the potential influence of state-level health legislature.
Figure 2.
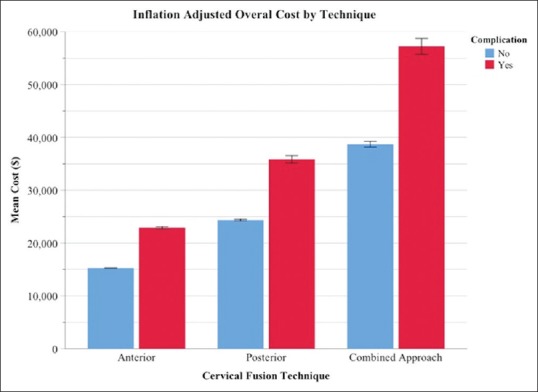
Mean cost for patients undergoing elective cervical fusion by the incidence of complications and type of surgical approach in the National Inpatient Sample Years 2002-2014
Common inpatient complications and cost of care
From 2002 to 2014, the proportion of patients with ≥1 complication was 5.2%. Complication rates in cervical surgery historically range from 3.0% to 6.7%.[13,14,15] Differential rates often depend on patient sample, study design, and the targeted profile of complications, for which we employed a comprehensive search to capture the adverse events during the hospitalization. Our study shows that the most frequent complications and their adjusted costs were dysphagia (1.6%, $2624), pulmonary (1.0%, $9334), and device/graft/implant/other (0.9%, $3125). Overretraction during ACF on the trachea, esophagus, and surrounding soft tissues is well described in relation to swallowing difficulty postoperatively, with the incidence ranging from 1.7% to 50.3% based on the inclusion criteria and symptom severity.[16,17,18] Known risk factors of postoperative dysphagia include older age, multilevel fusion, and the use of bone morphogenetic protein.[19] Older surgical patients are prone to pulmonary events even after controlling for comorbidities,[20] and cervical surgery can further impede the return to respiratory baseline. Minimizing ventilation-related barotrauma or mechanical trauma, the use of long-acting muscle relaxants and adequate pain control is thought to improve recovery.
Whereas our study comprises only inhospital records, the course of recovery at follow-up, particularly for patients with dysphagia and respiratory dysfunction, would provide more information on long-term morbidity. Inpatient mortality following elective cervical fusion is rare at <0.1%, but it is of clinical importance to understand the major complications associated with deaths and to reduce these risks. Respiratory (65.2%), cardiac (25.7%), and renal (15.7%) events are frequently seen with inpatient mortality. Especially, in older patients undergoing cervical surgery, evaluation of cardiopulmonary and renal status should be prioritized throughout hospital stay. Blood pressure and volume management in the setting of significant volume loss and long procedures are important to reducing postoperative myocardial infarction.[21]
Complications with highest cost of care
Although overwhelmingly rare, infection after cervical fusion results in the highest cost increase at $25,359, which is consistent with previous findings from smaller cohorts.[22,23] Intraoperative bacterial seeding and poor wound care are risk factors of infections resulting in prolonged hospital stay and predisposition to reoperation and readmission, all of which undoubtedly increase morbidity and expenditures. Similarly, the incidence of venous thromboembolism extends hospitalization and adds to the overall expenditure burden by $17,480. Venous insufficiency, cardiac arrhythmia, obesity, and ischemic heart disease are risk factors of postoperative thromboembolism. Our findings corroborate incremental costs due to deep venous thrombosis in other inpatient settings[24] and further highlight the need to adhere to standardized prophylaxis guidelines to reduce the burden of postoperative recovery and cost.
Following the cost of care for infection and thromboembolism, neurological complications were the third costliest type of events at $10,098. Spinal cord and nerve root associated injuries are more prevalent in patients who present with complex spinal disease and/or require instrumentation, factors that make the operation more technically challenging and extend the operative duration. Maintaining adequate cord perfusion intraoperatively and avoidance of excessive flexion and/or extension are encouraged to reduce the risk of medullary lesion in spine surgery. Nerve root injury most often occurs at C5, and the time of symptom onset can range from immediately to several months postoperatively.[25] Intraoperative neuromonitoring is commonplace in many large academic centers although its cost-effectiveness in reducing the rate of neurologic complications remains in need of further clarification.
Limitations
An important limitation is a reliance on reimbursement estimates using cost-to-charge ratios provided by the AHRQ for each hospital. There was no exact cost breakdown available in the NIS, e.g., cost of surgical procedure versus hospital stay, type of instrumentation and/or bone grafts used, and health system delivery may greatly affect overall costs related to surgery. Adjustments made in NIS sampling methodology, for example, sampling different hospitals year to year, or sampling different volume of cases per hospital year to year may explain some variability in trends. However, relative rates of complication within the study population remain highly relevant. NIS data include only inhospital events that were coded, which may often be subject to the assessment of nonclinical staff and may explain a component of variability in trends. Late complications, readmission events, and long-term outcome measures, all of which greatly contribute to additional expenditures, were not available for analysis and represented important future directions.
CONCLUSIONS
In a national sample of patients with degenerative spine disease undergoing cervical fusion, we characterize the incidences and quantify the inpatient costs associated with specific perioperative complications. The overall complication rate was 5.2%, of which the most common types were dysphagia, pulmonary, and device related. Hospital costs increased from 2002 to 2011, followed by a decreasing trend from 2012 to 2014. After adjusting for demographic/clinical variables and regional characteristics, we found that the cost increases are the greatest in the setting of infection, thromboembolism, and neurologic injury. Targeted evidence-based strategies may help optimize postoperative recovery and reduce complication-associated healthcare spending.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The study examined the national cost differences of inpatient complications for cervical fusion using discharge data from the NIS and the Nationwide Inpatient Sample, Healthcare Cost and Utilization Project and AHRQ. The authors have completed the mandatory training as per the AHRQ guidelines. This study contains no identifiable patient data.
REFERENCES
- 1.Marquez-Lara A, Nandyala SV, Fineberg SJ, Singh K. Current trends in demographics, practice, and in-hospital outcomes in cervical spine surgery: A national database analysis between 2002 and 2011. Spine (Phila Pa 1976) 2014;39:476–81. doi: 10.1097/BRS.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 2.Lad SP, Patil CG, Berta S, Santarelli JG, Ho C, Boakye M, et al. National trends in spinal fusion for cervical spondylotic myelopathy. Surg Neurol. 2009;71:66–9. doi: 10.1016/j.surneu.2008.02.045. [DOI] [PubMed] [Google Scholar]
- 3.Patil PG, Turner DA, Pietrobon R. National trends in surgical procedures for degenerative cervical spine disease: 1990-2000. Neurosurgery. 2005;57:753–8. [PubMed] [Google Scholar]
- 4.Liu CY, Zygourakis CC, Yoon S, Kliot T, Moriates C, Ratliff J, et al. Trends in utilization and cost of cervical spine surgery using the national inpatient sample database, 2001 to 2013. Spine (Phila Pa 1976) 2017;42:E906–13. doi: 10.1097/BRS.0000000000001999. [DOI] [PubMed] [Google Scholar]
- 5.Yue JK, Upadhyayula PS, Deng H, Sing DC, Ciacci JD. Risk factors for 30-day outcomes in elective anterior versus posterior cervical fusion: A matched cohort analysis. J Craniovertebr Junction Spine. 2017;8:222–30. doi: 10.4103/jcvjs.JCVJS_88_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawrence BD, Jacobs WB, Norvell DC, Hermsmeyer JT, Chapman JR, Brodke DS, et al. Anterior versus posterior approach for treatment of cervical spondylotic myelopathy: A systematic review. Spine (Phila Pa 1976) 2013;38:S173–82. doi: 10.1097/BRS.0b013e3182a7eaaf. [DOI] [PubMed] [Google Scholar]
- 7.Fehlings MG, Smith JS, Kopjar B, Arnold PM, Yoon ST, Vaccaro AR, et al. Perioperative and delayed complications associated with the surgical treatment of cervical spondylotic myelopathy based on 302 patients from the AOSpine North America cervical spondylotic myelopathy study. J Neurosurg Spine. 2012;16:425–32. doi: 10.3171/2012.1.SPINE11467. [DOI] [PubMed] [Google Scholar]
- 8.Beutler WJ, Sweeney CA, Connolly PJ. Recurrent laryngeal nerve injury with anterior cervical spine surgery risk with laterality of surgical approach. Spine (Phila Pa 1976) 2001;26:1337–42. doi: 10.1097/00007632-200106150-00014. [DOI] [PubMed] [Google Scholar]
- 9.Flynn TB. Neurologic complications of anterior cervical interbody fusion. Spine (Phila Pa 1976) 1982;7:536–9. doi: 10.1097/00007632-198211000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Cheung JP, Luk KD. Complications of anterior and posterior cervical spine surgery. Asian Spine J. 2016;10:385–400. doi: 10.4184/asj.2016.10.2.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gu Y, Cao P, Gao R, Tian Y, Liang L, Wang C, et al. Incidence and risk factors of C5 palsy following posterior cervical decompression: A systematic review. PLoS One. 2014;9:e101933. doi: 10.1371/journal.pone.0101933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blumenthal D, Abrams M, Nuzum R. The affordable care act at 5 years. N Engl J Med. 2015;373:1580. doi: 10.1056/NEJMc1510015. [DOI] [PubMed] [Google Scholar]
- 13.Romano PS, Campa DR, Rainwater JA. Elective cervical discectomy in California: Postoperative in-hospital complications and their risk factors. Spine (Phila Pa 1976) 1997;22:2677–92. doi: 10.1097/00007632-199711150-00018. [DOI] [PubMed] [Google Scholar]
- 14.Stulik J, Pitzen TR, Chrobok J, Ruffing S, Drumm J, Sova L, et al. Fusion and failure following anterior cervical plating with dynamic or rigid plates: 6-months results of a multi-centric, prospective, randomized, controlled study. Eur Spine J. 2007;16:1689–94. doi: 10.1007/s00586-007-0451-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nasser R, Yadla S, Maltenfort MG, Harrop JS, Anderson DG, Vaccaro AR, et al. Complications in spine surgery. J Neurosurg Spine. 2010;13:144–57. doi: 10.3171/2010.3.SPINE09369. [DOI] [PubMed] [Google Scholar]
- 16.Smith-Hammond CA, New KC, Pietrobon R, Curtis DJ, Scharver CH, Turner DA, et al. Prospective analysis of incidence and risk factors of dysphagia in spine surgery patients: Comparison of anterior cervical, posterior cervical, and lumbar procedures. Spine (Phila Pa 1976) 2004;29:1441–6. doi: 10.1097/01.brs.0000129100.59913.ea. [DOI] [PubMed] [Google Scholar]
- 17.Singh K, Marquez-Lara A, Nandyala SV, Patel AA, Fineberg SJ. Incidence and risk factors for dysphagia after anterior cervical fusion. Spine (Phila Pa 1976) 2013;38:1820–5. doi: 10.1097/BRS.0b013e3182a3dbda. [DOI] [PubMed] [Google Scholar]
- 18.Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: A prospective study. Spine (Phila Pa 1976) 2002;27:2453–8. doi: 10.1097/00007632-200211150-00007. [DOI] [PubMed] [Google Scholar]
- 19.Epstein NE. Complications due to the use of BMP/INFUSE in spine surgery: The evidence continues to mount. Surg Neurol Int. 2013;4:S343–52. doi: 10.4103/2152-7806.114813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smetana GW. Postoperative pulmonary complications: An update on risk assessment and reduction. Cleve Clin J Med. 2009;76(Suppl 4):S60–5. doi: 10.3949/ccjm.76.s4.10. [DOI] [PubMed] [Google Scholar]
- 21.Bijker JB, van Klei WA, Vergouwe Y, Eleveld DJ, van Wolfswinkel L, Moons KG, et al. Intraoperative hypotension and 1-year mortality after noncardiac surgery. Anesthesiology. 2009;111:1217–26. doi: 10.1097/ALN.0b013e3181c14930. [DOI] [PubMed] [Google Scholar]
- 22.Kuhns BD, Lubelski D, Alvin MD, Taub JS, McGirt MJ, Benzel EC, et al. Cost and quality of life outcome analysis of postoperative infections after subaxial dorsal cervical fusions. J Neurosurg Spine. 2015;22:381–6. doi: 10.3171/2014.10.SPINE14228. [DOI] [PubMed] [Google Scholar]
- 23.Theologis AA, Demirkiran G, Callahan M, Pekmezci M, Ames C, Deviren V, et al. Local intrawound vancomycin powder decreases the risk of surgical site infections in complex adult deformity reconstruction: A cost analysis. Spine (Phila Pa 1976) 2014;39:1875–80. doi: 10.1097/BRS.0000000000000533. [DOI] [PubMed] [Google Scholar]
- 24.Bullano MF, Willey V, Hauch O, Wygant G, Spyropoulos AC, Hoffman L, et al. Longitudinal evaluation of health plan cost per venous thromboembolism or bleed event in patients with a prior venous thromboembolism event during hospitalization. J Manag Care Pharm. 2005;11:663–73. doi: 10.18553/jmcp.2005.11.8.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nassr A, Eck JC, Ponnappan RK, Zanoun RR, Donaldson WF, 3rd, Kang JD, et al. The incidence of C5 palsy after multilevel cervical decompression procedures: A review of 750 consecutive cases. Spine (Phila Pa 1976) 2012;37:174–8. doi: 10.1097/BRS.0b013e318219cfe9. [DOI] [PubMed] [Google Scholar]


