Abstract
The medical autopsy is the most reliable and thorough means after the death of a patient that a physician has to evaluate the validity of his/her clinical diagnosis on which care was delivered. There is virtually no dispute in the literature of its value in the assessment of the quality of care. Today the medical autopsy has been largely abandoned except in academic medical centers. Even in the latter setting, the number of autopsies has steadily declined over the past 30–40 years. Approximately 360 autopsies are performed per year at the Washington University Medical Center in St. Louis; this number represents only 20% of all deaths in this medical center. The autopsy is time intensive and expensive in the environment of ever increasing pressure to reduce medical costs on all fronts. Will the autopsy survive? There are many reasons to advocate for the autopsy and they are considered in this discussion. The reasons to perform an autopsy remain as pertinent and relevant today as they did 50 to 100 years ago
Introduction
The Clinician
It is generally regarded as unnecessary in this day and age of high resolution imaging, and the known specificity and sensitivity of laboratory studies. There is nothing further that we need to know about the patient and besides that, we did not know the family well enough to broach the topic. Since I was among the 25% or more of medical students in my class who never witnessed an autopsy, I am not sure that I would even want one done on a member of my own family, much less myself after I die. I know enough about it to know that it disturbs the appearance of the body and is probably disturbing in terms of what goes into performing one. There is also a possibility that something may be found that may cause potential liability for me because I may have overlooked something but I am doubtful of that. After all, I also know that the pathologist is probably not interested in performing one and it always takes forever to get the results back or so I have been told
The Pathologist
My time is valuable and why spend it on a procedure that takes at least an hour or two to perform, then dictate, review the slides next week, then review the chart and put it altogether into a final report? All of this for something that is not billable. We have so few autopsies these days that it is not worth the time and expense of maintaining the facilities so that we can pass the College of American Pathologists inspection. Possibly, if I had a pathologist assistant who could look after all of the necessary preparations before and after, then maybe it would be more feasible. There does not appear to be any need or interest from my clinical colleagues since I can not remember the last time that one of them talked to me about the possibility of performing one
The Hospital Administrator
We do not need to do them in this hospital. It has been 40 years or so since the Joint Commission on Accreditation of Health Care Organizations eliminated the numerical target for autopsies on our hospital deaths.1 Since it is not a direct reimbursable service, there is no way to justify it in my budget which is constantly under stress and pressure. The pathologist has enough to do as it is, or so he tells me
The Reality of It All
The preceding vignettes provide some perspective on the medical, non-forensic autopsy today as viewed by the clinician, pathologist, and hospital administrator. This is the reality of the autopsy in the world of contemporary medicine as practiced in the United States, Canada, and many European countries. Currently in the United States, the autopsy rate is only 7% to 9% whereas in the mid-1960s it was approximately 25% to 35%, and even higher in the 1940s and 1950s when it was 50% of all hospital deaths. 2,3
Background
The autopsy quite literally means to “see for oneself.” Interest in the cause of death dates back to the Greek physicians of three millennia ago who designated the post-mortem examination as an “autopsy.” During the period of the Renaissance, gross dissection of the human body became an integral component of medical education in Paris, Padua, and Parma. Autopsies have attracted the attention of renowned painters (See Figure 1). It was Giovanni Battista Morgagni (1682 – 1771) who published the first comprehensive textbook on pathological anatomy, “On the Seats and Causes of Diseases Investigated by Anatomy,” in 1769. He compared and contrasted the effects of disease on the gross structure of various organs in a systematic fashion that few had thought about. It would not be until the 19th century that substantial progress would be made in the systematic study of disease from the vantage point of the direct examination of the organs, which is the core of pathologic anatomy. Two individuals, Karl Von Rokitansky (1804–1878) in Vienna and Rudolph Ludwig Karl Virchow (1821–1902) in Berlin, are largely responsible for providing the empiric foundation on which we base our gross and microscopic impressions as to the nature of the pathologic process, respectively.4,5 The science rather than the natural philosophy of medicine was initiated by these two pathologists. Rokitansky emphasized the need for meticulous dissection to demonstrate the gross findings at autopsy for the purpose of clinicopathologic correlation. It is said that Rokitansky personally performed 30,000 autopsies and supervised another 70,000. Virchow was equally concerned with the gross examination, but unlike Rokitansky, he was also engaged with the microscopic findings since he believed that disease began at the cellular level (“omnis cellulae cellula”), earning him the sobriquet of “father of cellular pathology.” The emergence of cellular pathology was also concurrent with the recognition of the causative role of microorganisms in the etiology of many common communicable diseases such as tuberculosis, cholera, and plague. The names of both Rokitansky and Virchow remain current since they devised the two principal techniques of gross examination: the in situ method of organ examination ascribed to the former and the organ block method of the latter.5
Figure 1.
Rembrandt van Rijn (Dutch, 1606–1669). The Anatomy Lesson of Dr Nicolaes Tulp, 1632
The apogee of the autopsy occurred well into the mid 20th century at a time when it was regarded as a core scientific method to study diseases in the human. The reputations of many well known and prestigious departments of pathology were based to a considerable degree on the excellence of the faculty in autopsy anatomic pathology, which led to modern experimental pathology with the purpose of creating laboratory models of human disease. The autopsy was not only performed to provide clinicians with the cause of death but to establish the very nature of the pathology which may have been suspected, or to document pathology which was totally unknown during life. From these individual autopsies, the process of systemic analysis of pathologic features with the application of special stains and the addition of increasingly sophisticated techniques culminated in papers in pathology journals. That exercise continues today. One contemporary example of this process which began with the autopsy is the initial cases of a bewildering, catastrophic disease occurring in young men in San Francisco in the early 1980s which we know as human immunodeficiency virus (HIV)-acquired immunodeficiency syndrome
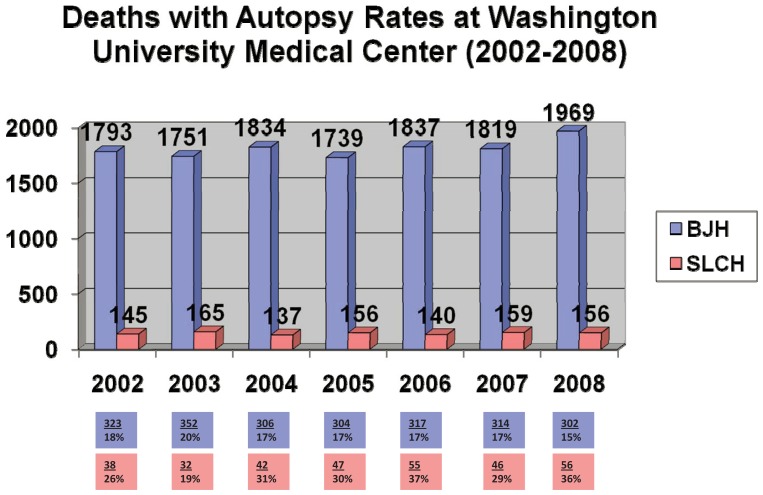
Autopsies at the Washington University Medial Center, Barnes Hospital and the Washington University School of Medicine, began in 1915 and to date, some 48,000 autopsies have been performed in the medical center. The Department of Pathology and Immunology is responsible for the autopsy service for both Barnes-Jewish Hospital (BJH) and St. Louis Children’s Hospital (SLCH). At one time, 600–700 autopsies were performed per year; more recent figures demonstrate that the number of autopsies averages 360 cases per year representing approximately 20% of all institutional deaths (See Figure 2). The autopsy rate is approximately 30% in the pediatric population compared to less than 20% for adults. The higher autopsy rate in children is also true of many other children’s hospitals. Approximately 75% of the pediatric autopsies are performed on infants from the neonatal intensive care unit (NICU); virtually all of these babies are premature with multiorgan complications. Relationships between parents and caregivers in the NICU and PICU create a dynamic for all parties to gather the facts which only an autopsy can provide, since the death of a child in a very real sense is a violation of the natural order. It is widely acknowledged that the autopsy, pediatric and adult alike, is the ultimate measure of quality assurance, but even in an academic medical center, it is under-utilized for that purpose, particularly in adults.6,7
Figure 2.
This color coded bar graph depicts the total number of inpatient deaths over the past seven years at the Washington University Medical Center in St. Louis, MO. The boxes below depict the number of autopsies which were performed in each calendar year from Barnes-Jewish Hospital (blue boxes) and St. Louis Children’s Hospital (pink boxes). There was only one year, 2003, when the autopsy percentage was higher by 1% point in the Barnes-Jewish Hospital population of adults only compared to St. Louis Children’s Hospital population of children only
The Autopsy and Undergraduate and Graduate Medical Education
For those of us of an earlier generation, it is very likely that the observation and even participation in an autopsy(s) was a component of the second year course in pathology. With the time constraints of the overburdened contemporary undergraduate medical curriculum, the pathology course has been distilled to pertinent facts in PowerPoint presentations with minimal opportunity to see a single autopsy, much less be actively involved in one. For medical students who may be thinking about pathology as a career, there are four and six week rotations on the autopsy service in their third and fourth years. These students represent 1% to 2% of the medical student class, which reflects the approximate percentage of medical school graduates who pursue pathology as a career
There was a time when many of the clinical specialties through their respective boards required a pathology rotation in either autopsy or surgical pathology. Currently, only one medical specialty board requires an autopsy experience and that is the American Board of Pathology. The requirement is that the “resident must perform a minimum of 50 autopsies, and a list of completed autopsies performed by the resident must be provided at the time of application. (www.abpath.org). Because the autopsy rate in the United States has plummeted, even in academic medical centers, the American Board of Pathology established this minimum number. With the exception of residents in dermatology who have regular rotations through the dermatopathology service in surgical pathology, no other clinical specialty has a requirement for any benchside experience in pathology
The Whats and Whys of the Autopsy
There are three basic types of autopsies in terms of the extent of the examination. A complete autopsy is anatomically unrestricted with the inclusion of all body cavities and the brain. A limited autopsy generally excludes the brain. A restricted autopsy is one that is confined to a specific body cavity (thorax only or brain only, as examples). A needle-only autopsy is the ultimate minimalist examination in which tissues are sampled with a biopsy needle without opening the body cavities. 8 What would Rokitansky have thought of the needle autopsy given his obsession with the perfect dissection?
Who is empowered to give consent for an autopsy? Assuming that the case does not involve the jurisdiction of the medical examiner, the answer is addressed in Missouri Revised Statute Chapter 194 (MSR 194:115). Permission can be given by the deceased obviously before death if “duly signed and acknowledged prior to his death.” An individual “designated in a durable power of attorney that expressly refers to giving of consent to an autopsy” is next in order, and is followed by the surviving spouse. Any surviving child, parent, or brother or sister (in that order) may sign the permit if there is no surviving spouse of the deceased, or if the living spouse and the deceased had been living apart. On occasion, conflicts arise among family members when the time comes to sign the permit
Who should be the one to approach the family for an autopsy? Ideally it should be the physician who knows and has the best rapport with the family. In an academic medical center, that individual physician may not always be clearly identified. 9 On occasion, the responsibility for requesting an autopsy falls on the shoulders of a junior house officer, likely an individual who went to a medical school where he/she never saw an autopsy and who may or may not be prepared to answer any of the questions that the family may have about the procedure, whether there will be any visible sign of the autopsy after it has been completed, and how long it will take to do the autopsy. Some institutions have trained resource personnel who can assist with various questions relating to the autopsy
Why request an autopsy when I know why my patient died and possibly open myself up to liability issues? Despite the widely held notion that everything there is to know about the patient has been established before death, numerous studies in the literature have compared clinical diagnoses before death with the findings at autopsy.10–14 Two classification schemes have been devised to grade the disparity between the clinical diagnoses and the pathologic findings, within range from complete concordance to major discrepancies. One of the most comprehensive and recent studies utilized “53 distinct autopsy series over a 40-year period” identified in the literature by a Medline search; in this study, Skojania and associates found a major median error rate of 23.5%. 15 They noted a decrease in the major error rate over time, but concluded that it “remains sufficiently high that encouraging ongoing use of the autopsy appears warranted.”
There is nothing to suggest a relationship between the autopsy and number of claims of medical liability and negligence. Most liability cases center upon issues of standard of care rather than causation, and it’s the later whose focus is the autopsy. In fact, Bove et al found that autopsy results were infrequently at the center of a “successful legal argument” for either side in a malpractice action. 16 Nichols and associates reviewed a series of autopsies in their institution and one case (0.6%) of 176 cases proceeded to a malpractice claim, but not for reasons on the basis of the autopsy findings. 17
Revelations at the Time of Autopsy
Some of the most interesting and challenging autopsy cases are those in which there was bewilderment about the nature of the underlying disease process. These patients are often characterized as having multisystem involvement, and all efforts during life failed to establish the diagnosis. In most cases, it is either a widely disseminated, predominantly microscopic malignancy (a small primary carcinoma of the lung, pancreas, or intestinal tract) or a systemic fungal or viral infection
Gravely ill patients without a definitive diagnosis tend to gravitate to an academic medical center such as ours and over a relatively brief period of time, they often have a series of sophisticated imaging, endoscopic and laboratory studies whose purpose is to attempt to establish a diagnosis, which may in the end only be revealed at autopsy. The argument could be made that our autopsy rate should be considerably higher than it is given the nature of our inpatient population. In any event, it should come as no surprise that among our autopsy population there are patients whose death was directly or indirectly related to treatment(s) or complications incurred either avoidably or unavoidably while hospitalized. These are the cases with highest obvious quality assurance value. If the future of medical care reimbursement is to be linked to quality of care and outcome, it would seem that the autopsy could very well move from its current peripheral location to the center.3 However, that shift can not occur without a decided change in the attitude of many clinicians, pathologists, and administrators
We have been impressed with the number of families who have requested an autopsy. The apparent motivation is very rarely to find out “what went wrong.” In some cases, the family wants to reassure themselves that they made the “right” end of life decision for their loved one. They are also interested in knowing the extent of the disease, often a malignancy, at the time of death. Parents of children who have died are extremely interested in any genetic implications of a particular disease process, which in their mind can only be answered by an autopsy (whether that is the case or not); the question is often how their children, present and future, will be affected. For all, regardless of their stake in the case, an autopsy has the benefit of closure
When should I expect the final report? One of the longstanding critiques of the autopsy, or more appropriately the pathologist, is the time interval between the actual autopsy and the completion of the final report. That concern on the part of the clinician about the turn around time for the completed autopsy report (often several months) affects the motivation for obtaining an autopsy in the first place. From another perspective, the autopsy loses it relevance for the clinician as time passes. There are few reasons that an autopsy report can not be completed within 30 days of death, if not less, in most cases. If the brain is the focus of the case, it may take somewhat longer as it requires extra fixation prior to thorough gross examination
Vital Statistics, Death Certificates and the Autopsy
The National Vital Statistics System (NVSS) is defined as “the oldest and most successful example of intergovernmental data sharing in public health” according to the Centers for Disease Control and Prevention website (www.cdc.gov). The data on mortality is collected from the death certificate; this document is completed by “funeral directors, attending physicians, medical examiners, and coroners.”
There are numerous studies in the literature which have reviewed the concordance between the death certificate cause of death and the results of the autopsy.18–20 One of the more recent studies evaluated the accuracy of the death certificate in cases of autopsy-proven acute myocardial infarction. Ravakhah reported that almost 50% of death certificates missed the acute myocardial infarction (25 to 52 cases) as the cause of death, but asserted its presence in 36 cases of which nine had no evidence of an acute myocardial infarction; 21 there was concordance between the death certificate and autopsy-proven myocardial infarction in only 27 (52%) of 52 cases. Similarly designed studies have evaluated other disease categories such as malignancy, pneumonia, aortic dissection, and aneurysms. Hoel and associates reported a consistent underestimation of cancer-related death by almost 20%. 18 Hill and Anderson concluded that the “current state of death statistics in the United States would constitute a national embarrassment if it were not for the fact that the rest of the world seems to be similarly afflicted. 22”
There is an insufficient work force of pathologists and pathologist assistants to perform 2.4 million autopsies each year in the United States. However, the reliability of the death certificates and their utilization in the NVSS is a problem of considerable magnitude for epidemiologists and policy markers
Conclusion
After a consideration of the autopsy from various perspectives under discussion in this paper, it is difficult to simply dismiss the autopsy as no longer relevant to the contemporary practice of medicine. However, its diminishing numbers in virtually all developed countries since the middle of the 20th century would seem to indicate that the medical profession as a whole perceives the autopsy as no longer useful despite the results of attitudinal surveys of practicing physicians, including pathologists, residents and medical students, who all espouse its importance. 23 The fact that less than 10% of all hospital deaths on average are followed by an autopsy would seem to belie the results of these attitudinal surveys. There is the prevailing sense among many clinicians that there is “little that I do not already know about my patient whether in life or death.” Few pathologists feel as though they can continue to sacrifice the time and expense in a non-reimbursable medical examination. Many autopsy suites have become darkened storage areas, or have been remodeled for other purposes. Today most medical or non-forensic autopsies are performed in academic medical centers. Since the American Board of Pathology requires that each resident performs at least 50 autopsies to qualify for certificate in anatomic pathology, there is considerable pressure at institutions with pathology residing programs to maintain an adequate number of autopsies. Since pathology requirements have long since disappeared from the curriculum of virtually all clinical residencies, there are few stakeholders in the autopsy service for educational reforms outside of pathology
The argument can be made that the autopsy is the ultimate instrument to evaluate the quality of care. However, most institutions do not include the autopsy in the systematic assessment of quality assurance. The need for continued improvement in clinical diagnosis and management still exists in this era of increasingly sophisticated and expensive technology, yet there are still findings at autopsy whose presence was totally unsuspected during the clinical course of the patient. As we have discussed briefly above, these misperceptions of omission and commission make their way into death certificates and faulty national vital statistics. Finally, there is no direct reimbursement for the pathologist who performs an autopsy. The Council on Scientific Affairs of the American Medical Association recommended that “methods of reimbursement to validate the autopsy as a medical act should be sought.”24 Pathologists are still waiting for action on that recommendation 22 years after it was made. We live in a society where value is measured almost exclusively in monetary terms, and that being the case, it seems that society has already rendered its judgment on the autopsy
Biography
Louis P. Dehner, MD, MSMA member since 1990, is a Professor in the Department of Pathology and Immunology of Washington University School of Medicine in St. Louis. He is also on the Missouri Medicine Editorial Board.
Contact: dehner@path.wustl.edu
Footnotes
Disclosure
None reported
References
- 1.Burton EC. The autopsy: A professional responsibility in assuring quality of care. Am J Med Qual. 2002;17:56–60. doi: 10.1177/106286060201700203. [DOI] [PubMed] [Google Scholar]
- 2.Nemetz PN, Tanglos E, Sands LP, Fisher WP, Jr, Newman WP, 3rd, Burton EC. Attitudes toward the autopsy – an 3- state survey. Med Gen Med. 2006;8:80. [PMC free article] [PubMed] [Google Scholar]
- 3.Xiao J, Krueger G, Buja L, Covinsky M. The impact of declining clinical autopsy: need for revised healthcare policy. Am J Med Sci. 2009;337:41–46. doi: 10.1097/MAJ.0b013e318184ce2b. [DOI] [PubMed] [Google Scholar]
- 4.King LS, Meehan MC. A history of the autopsy. A review. Am J Pathol. 1973;73:514–544. [PMC free article] [PubMed] [Google Scholar]
- 5.Porter R, editor. Blood and Guts - A short history of medicine. WW Norton and Company; 2002. [Google Scholar]
- 6.Newton D, Coffin CM, Clark EB, Lowichik A. How the pediatric autopsy yields valuable information in a vertically integrated health care system. Arch Pathol Lab Med. 2004;128:1239–1246. doi: 10.5858/2004-128-1239-HTPAYV. [DOI] [PubMed] [Google Scholar]
- 7.Zarbo RJ, Baker PB, Howanitz PJ. The autopsy as a performance measurement tool – diagnostic discrepancies and unresolved clinical questions: a College of American Pathologists Q-Probes study of 2479 autopsies from 248 institutions. Arch Pathol Lab Med. 1999;123:191–198. doi: 10.5858/1999-123-0191-TAAAPM. [DOI] [PubMed] [Google Scholar]
- 8.Huston BM, Malour NN, Azar HA. Percutaneous needle autopsy sampling. Mod Pathol. 1996;9:1101–1107. [PubMed] [Google Scholar]
- 9.Lowry F. Failure to perform autopsies means some MDs “walking in a fog of misplaced optimism”. Can Med Assoc J. 1995;153:811–814. [PMC free article] [PubMed] [Google Scholar]
- 10.Veress B, Alafuzoff I. Clinical diagnostic accuracy audited by autopsy in a university hospital in two eras. Qual Assur Health Care. 1993;5:281–286. doi: 10.1093/intqhc/5.4.281. [DOI] [PubMed] [Google Scholar]
- 11.Veress B, Alafuzoff I. A retrospective analysis of clinical diagnoses and autopsy findings in 3042 cases during two different time periods. Hum Pathol. 1994;25:140–145. doi: 10.1016/0046-8177(94)90269-0. [DOI] [PubMed] [Google Scholar]
- 12.Carvalho FLP, Cordeiro JA, Cury P. Clinical and pathological disagreement upon the cause of death in a teaching hospital: analysis of 100 autopsy cases in a prospective study. Pathol Int. 2008;58:568–571. doi: 10.1111/j.1440-1827.2008.02272.x. [DOI] [PubMed] [Google Scholar]
- 13.Rossi S, Reale D, Grandi E. Correlation of clinical diagnosis with autopsy findings. IARC Sci Publ. 1991;112:99–108. [PubMed] [Google Scholar]
- 14.Roulson J, Benbow EW, Hasleton PS. Discrepancies between clinical and autopsy diagnosis and the value of post mortem histology; a meta-analysis and review. Histopathology. 2005;47:551–559. doi: 10.1111/j.1365-2559.2005.02243.x. [DOI] [PubMed] [Google Scholar]
- 15.Shojania KG, Burton EC, McDonald KM, Goldman L. Changes in rates of autopsy-detected diagnostic errors over time: a systematic review. JAMA. 2003;289:2849–2856. doi: 10.1001/jama.289.21.2849. [DOI] [PubMed] [Google Scholar]
- 16.Bove KE, Iery C. The role of the autopsy in medical malpractice cases, I. A review of 99 appeals court decision. Arch Pathol Lab Med. 2002;126:1023–1031. doi: 10.5858/2002-126-1023-TROTAI. [DOI] [PubMed] [Google Scholar]
- 17.Nichols L, Aronica P, Babe C. Are autopsies obsolete? Am J Clin Pathol. 1998;110:210–218. doi: 10.1093/ajcp/110.2.210. [DOI] [PubMed] [Google Scholar]
- 18.Hoel DG, Ron E, Carter R, Mabuchi K. Influence of death certificate errors on cancer mortality trends. J Natl Cancer Inst. 1993;85:1063–1068. doi: 10.1093/jnci/85.13.1063. [DOI] [PubMed] [Google Scholar]
- 19.Lee PN. Comparison of autopsy, clinical and death certificate diagnosis with particular reference to lung cancer. A review of the published data. APMIS Suppl. 1994;45:1–42. [PubMed] [Google Scholar]
- 20.Sington JD, Cottrell BJ. Analysis of the sensitivity of death certificates in 440 hospital deaths: a comparison with necropsy findings. J Clin Pathol. 2002;55:499–502. doi: 10.1136/jcp.55.7.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ravakhah K. Death certificates are not reliable: revivification of the autopsy. South Med J. 2006;99:728–733. doi: 10.1097/01.smj.0000224337.77074.57. [DOI] [PubMed] [Google Scholar]
- 22.Hill RB, Anderson RE. The autopsy and health statistics. Leg Med. 1990:57–69. [PubMed] [Google Scholar]
- 23.Burton JL, Underwood J. Clinical, educational and epidemiological value of autopsy. Lancet. 2007;369:1471–1480. doi: 10.1016/S0140-6736(07)60376-6. [DOI] [PubMed] [Google Scholar]
- 24.Council on Scientific Affairs. Autopsy. A comprehensive review of current issues. JAMA. 1987;258:364–369. [PubMed] [Google Scholar]