Abstract
The principle subdivisions of aesthetic breast surgery are: breast augmentation, mastopexy (breast lift), and reduction mammoplasty (breast reduction). In each of these subdivisions, emerging new technologies and trends have potential to change the management of specific aesthetic problems of the breast. Given the continued increasing popularity of aesthetic breast surgery, an understanding of these newer developments will assist all practitioners in communicating with their patients and colleagues.
The Return of Silicone Gel-filled Breast Implants
In 1992, because of concerns about their durability and safety, the Food and Drug Administration placed a moratorium on silicone gel-filled breast implants significantly limiting their use for breast augmentation.1,2 After the FDA’s moratorium, 90+% of breast augmentation procedures performed in the United States used saline-filled breast implants. In November 2006, the FDA, satisfied that the safety and efficacy concerns had been addressed, approved silicone gel-filled breast implants for breast augmentation. The FDA decision was based on an overwhelming amount of data the demonstrated the safety of silicone gel breast implants. Much of this data was developed in the United States through a series of FDA-approved studies in which all patients receiving a silicone gel-filled implant were required to participate.3
Additional data was also obtained from other developed countries where silicone gel-filled breast implants continued to be used without restrictions.4 Numerous scientific panels also reviewed the data including The National Academy of Science’s Institute of Medicine, multiple scientific and medical professional societies, and others prior to the FDA’s 2006 approval.5 Since the FDA’s approval, the percentage of breast augmentation procedures using saline-filled implants has dropped dramatically while the opposite is true for silicone gel-filled devices. In 2009, less than 30% of breast implants used for breast augmentation will be saline-filled devices.6 Numerous reasons have been implicated for this rapid transition from saline to silicone gel-filled implants including: more natural feel, more natural appearance, less problems with rippling and puckering of the implant, diminished concerns over the long-term safety and durability of the newer generation silicone gel-filled breast implants
The current silicone gel-filled implants approved by the FDA in 2006 are “fourth generation” devices and differ from the second and third generation implants that were subject to the 1992 FDA moratorium. The fourth generation implants have thicker, stronger low-bleed shells and are filled with a more cohesive silicone gel when compared to the earlier generation silicone gel implants. This has resulted in a lower implant failure rate: 3.5% of patients experience an implant failure at six years.7 Patient acceptance of the fourth generation devices is very high with a greater than 95% satisfaction rate three years after undergoing breast augmentation.7,8 Reoperation rates for breast augmentation patients with silicone gel-filled breast implants are 4.8% to 28% with an estimated average of 15% within three years of initial implantation.7,8,9 The most common reasons for re-operation after breast augmentation are in order of occurrence: capsular contracture, patient request for size change, and implant malposition. Implant failure/ rupture represented the least likely cause for re-operation. Patients with fourth generation silicone gel-filled implants enrolled in the Allergan and the Mentor FDA-approved studies will continue to be followed for ten-years from time of implantation. If current trends continue, it is predicted that silicone gel-filled breast implants will be used in nine out of every ten breast augmentation procedures in the near future. This is consistent with the utilization patterns in other developed countries never subject to the silicone gel-filled implant moratorium.
The Next Generation of Breast Implants
In 1994, the McGhan Company (later Inamed and now part of the Allergan Corporation) introduced the first “fifth-generation” breast implant, the Style 410 implant. Widely used in other countries since its introduction, the Style 410 implant is being evaluated in FDA-approved studies in the United States. This device differs from the previous generations of breast implants in numerous ways. The fifth generation implants are filled with an enhanced cohesive silicone gel with significantly increases cross-links in the silicone matrix that give these implants their distinct feel. These devices have been frequently described on the internet as the “gummy bear” implant i.e. similar feel of the implant and gummy bear candy. This increased cross-linking also makes the implant filling material “form stable” meaning that the implant will maintain its shape despite their position. Previous efforts to develop a shaped, anatomic breast implant had failed principally because of the lack of stability of the filling materials.10 Saline and less cohesive silicone filling materials, termed “responsive” fillers, cannot maintain their shape under tissue pressures once placed inside the breast pocket. Frequently they result in a distorted or misshapen breast appearance. (See Figure 1.) Dissatisfaction with the earlier anatomic shaped breast implants resulted in these devices losing favor to round breast implants filled either with saline or responsive silicone gel. With the development of the “form stable” gel matrix for the Style 410 implant, an anatomical shaped breast implant device is possible since these devices are resistant to the tissue forces inside the breast pocket thus maintaining their shape. This allowed an array of implant choices based on variations of all three dimensions that impact breast shape: height, width, and projection of the implant. This represents a fundamental change in how breast implants are selected based upon the patient’s measurements and tissue dynamics; not just on volume alone as with the earlier breast implants.11 The term frequently used to describe this process of implant selection is “Biodimensional Method”. The Allergan Style 410 implant selection is based upon a series of dimensional choices such as full height, moderate height, or low height in combination with width selection based on the patient’s breast width and projection (low, moderate, full, or extra projection) based on the patient’s tissue laxity. There are now almost 250 implant variations of the Allergan form-stable matrix breast implant allowing for optimal patient implant selection. 12
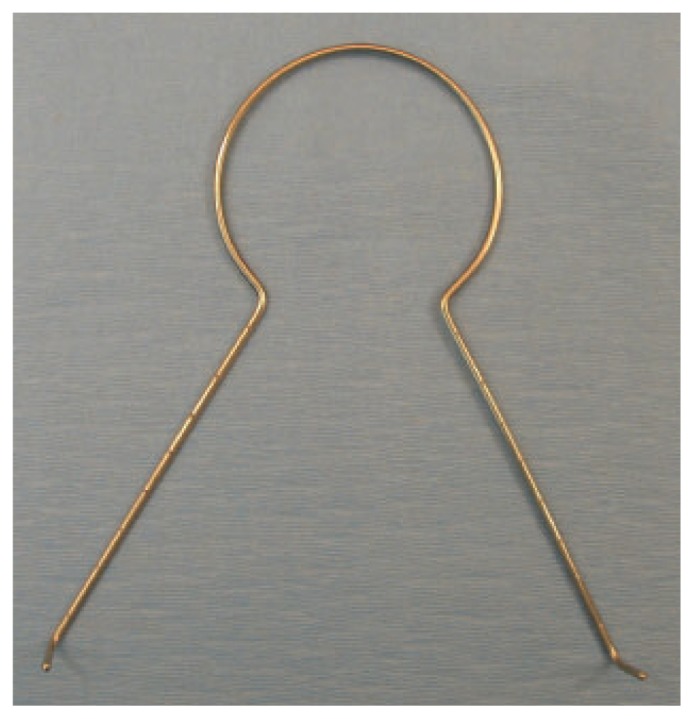
Figure 1.
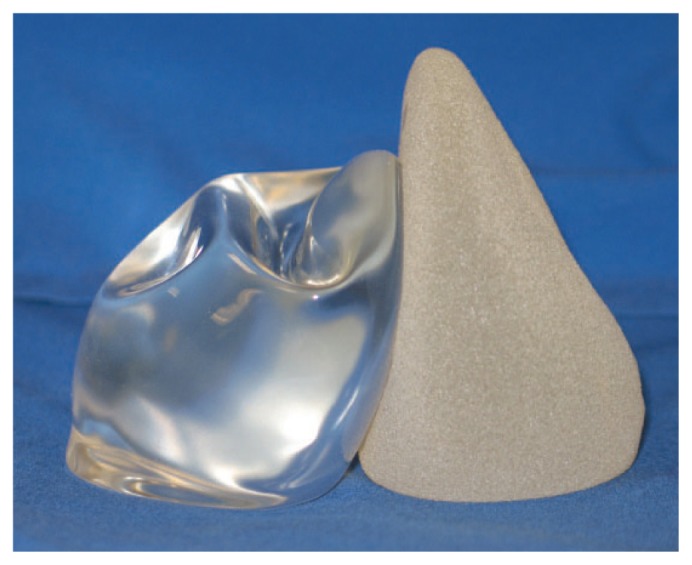
A 290 gram form-stable silicone gel Style 410 implant is on the right and a 300cc fourth-generation responsive silicone gel filled implant is on the left. Note the upper pole collapse of the responsive gel-filled implant despite the implants being of similar size.
The increased cross-linking of the silicone gel in the Style 410 implant also decreases the risk of gel migration should the integrity of the implant shell be compromised. The form stable gel matrix maintains its place and position inside the breast pocket.13 Also, the form-stable gel matrix minimizes movement of the implant shell envelope potentially increasing the life-expectancy of the implant. In a study in which all patients had an implantation time of five to nine years, the Style 410 implant had a 0.3% failure rate on MRI studies compared to a 5–10% failure rate in responsive, non-form stable gel implants. 13
Critically important for the success of an anatomically-shaped breast implant is the ability to control the orientation of the device. Problems with earlier efforts to develop an anatomic, tear-drop shaped device had failed in part because of an inability to restrict implant rotation inside of the breast pocket. 14 Variations of implant surface textures were developed to obtain the correct balance of implant softness and “give” mixed with immobility. Prior to the FDA moratorium, the most successful of such surfaces were the polyurethane devices, often termed “fuzzy implants” because of their distinct covering.15 These implants are no longer available for use in the United States but their surface characteristics acted as a model for future surface texturing designs. The Allergan Style 410 implant uses the Biocell© surface, a proprietary surface texture, that had been developed from its experience with tissue expander devices in the 1980s.16 The Biocell© surface has an open-pore surface with an irregular pattern of depressions designed for tissue in-growth into the surface. This increases tissue adherence and minimizes implant rotation. Critical to the success in using such surfaces is precise pocket size dissection and minimal fluid accumulation around the implant after placement. Follow-up studies demonstrate that if these surgical guidelines are followed, minimal incidence of implant rotation occurs. 17,18
Sometime after Allergan introduced the Style 410 breast implant, the Mentor Company (now part of Johnson and Johnson Corporation) introduced the Contour Profile Gel (CPG) implant. Principle differences between the Style 410 Implant and the CPG implant are the degree of cohesiveness of the silicone gel filling and the implant surfaces. The CPG device has fewer cross-links of the silicone gel filler and therefore is less cohesive than the Style 410 device. The Siltex© surface texture used on the CPG implant has “pebble effect” and does not enhance tissue in-growth. Follow-up studies using the CPG device have demonstrated similar results regarding safety and efficiency as the Style 410 implant. 8,19 The advantages of the form-stable devices are: increased control of breast shape optimizing aesthetic results, potentially increased longevity, lowest incidence of capsular contracture resulting in increased softness, lowest complication rate resulting in lower re-operation rate.
Implementation of the form-stable devices will require a re-learning process for surgeons in both the planning and performance of the surgical procedure. However studies demonstrate once surgeons are trained, this is minimal difficulty adjusting to cohesive, fifth generation breast implants. (See Figure 2.) Given patient demand outside the United States where cohesive devices have been available, it is likely that upon FDA approval, there will be a similar increase in the use of these devices in the United States.
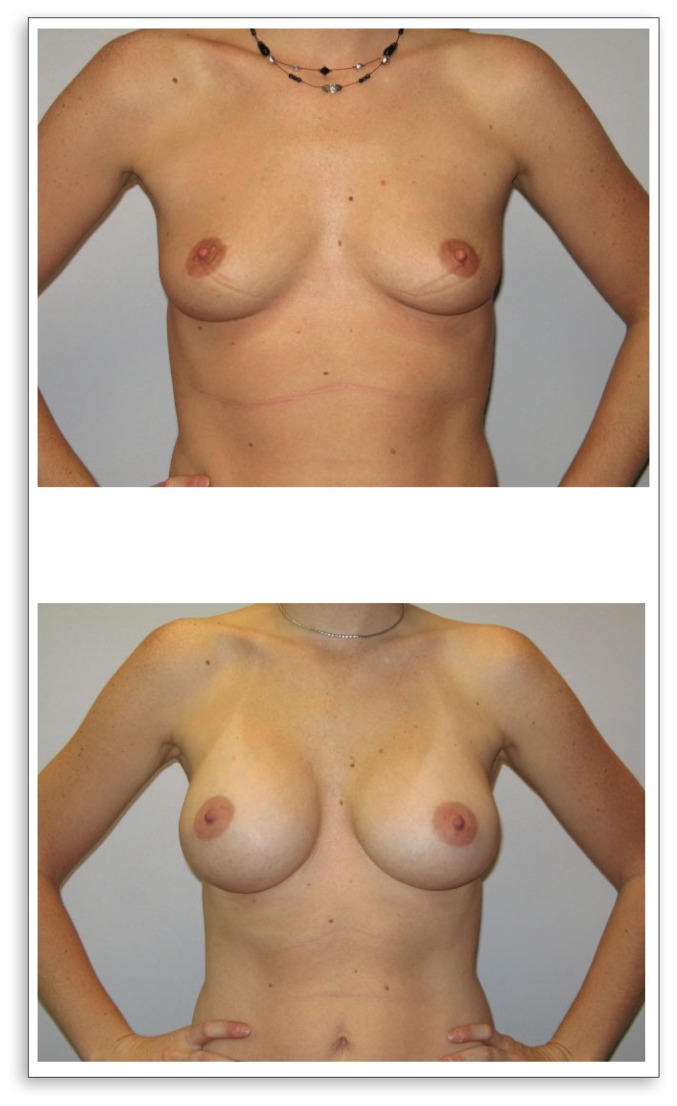
Figure 2.
Above, pre-operative view of patient with a 36B cup size. Below, post-operative view at one year using 475 gram full height, full projection Style 410 breast implants.
Breast Augmentation Using Fat Grating
In 1987, the American Society of Plastic and Reconstructive Surgeons (now The American Society of Plastic Surgeons-ASPS) issued a position paper based on an Ad-Hoc Committee recommendation that “…deplored the use of autologous fat injection in breast augmentation.” The Society made its recommendations because of concern about the possibility of potential interference with the detection of breast carcinomas due to fat necrosis, scarring, and calcifications in the breast after fat grafting.20 Prior to this time, because there was no consistent and safe method to harvest and transfer the fatty tissues required, there had been only a few, scattered reports in the literature about the use of autologous fat for breast augmentation. However, with the advent of liposuction and its ability to harvest large amounts of fat with potential for fat grafting, the incidence of breast augmentation using fat increased followed by a number of published reports.21,22
Since the issuance of the ASPS position paper, progress has been made on the techniques required to correctly harvest and process the fat for transfer. 23,24 While the individual process varies, certain common critical components are consistent. Gentle care in harvesting fat to minimizes injury by mechanical trauma and exposure to air. The least suction required to harvest the grafts should be used with small, minimally traumatic blunt-tip cannulas.
The fat should be processed with as little exposure to air as possible and contamination from blood, serum, and other sources should be avoided. Damaged adipocytes should be removed prior to transfer. Some procedures advocate centrifugation of the fatty tissues while other techniques use a rinse and wash technique to purify the fat.
The injections techniques vary also but it is critical to avoid mechanical damage to the fat graft. Injection using very small blunt-tipped infusion cannulas or needles with multiple passes in several layers maximizes graft survival. The amount of fat transferred with each pass is small to increase the probability of revascularization and graft survival. It is unclear which tissue plane is preferred for fat transfer to the breast. Tissue planes used include: subcutaneous, subglandular, glandular, intrapectorial, and combinations of the above.
Complications do occur with fat grafting of the breast. These include: serious infections, minor bleeding, fat necrosis, pain, cyst formation, and less than expected aesthetic results.23,25
The amount of fat required for grafting varies. Fat grafting often requires more than one treatment since only a limited amount of fat can be transferred in each session in order to maximize graft survival. Over-grafting (the placement of too much fat in a session) may result in fat necrosis, infection, irregular tissue contours, and cyst formation. The time of each session varies. Coleman found placement of the fat grafts required two hours for the first 100cc and approximately 45 minutes for each additional 100cc placed. 24 Many patients required multiple sessions to achieve their desired endpoint. All patients experienced significant edema in the breasts lasting as long as four to six months.
Numerous studies have been performed to determine the effect of fat grafting on the breast and cancer detection. These studies included patients who had fat grafting performed for both aesthetic and reconstruction purposes.23 The radiologic studies indicated that current technologies are able to adequately image breast tissues that have received fat grafts and identify the fat grafts, microcalcifications, and suspicious lesions. 23 Two cases of breast cancer were reported after fat grafting but there were no delays in diagnosis or treatment outcome. These studies were early follow-up studies and long-term follow-up studies are required to better define long-term risks.
Fat grafting is dependent upon the skill and the experience of the surgeon in order to achieve optimal outcomes. The worst results and the highest complications came from patients treated by inexperienced, non-surgical practitioners who failed to understand the need for precision in planning, technique, and follow-up management.
Possible reasons for the limited use of fat grafting for breast enhancement when compared to breast implants include longer operative time, multiple treatment sessions, lack of donor material, and lack of long term studies
In July 2009, ASPS published the report of The Fat Graft Task Force. 23 The task force performed a detailed review of 110 articles on fat grafting. From this review they concluded that fat grafting is a promising technique but lacks long-term clinical studies. Performance of long-term, randomized, controlled trials is critical for determining the safety and efficacy of fat grafting and different techniques for fat transfer. Patient risk factors need to be identified and improved patient selection performed. Further research to enhance cell and tissue viability needs to be performed and techniques standardized. Walden has also summarized the challenges of surgeons choosing to perform fat grafting for breast augmentation.26
Mastopexy
Mastopexy or breast lift, is a procedure for elevating and reshaping of the ptotic breast. Breast ptosis occurs when the breast mound and the nipple-areola descend on the chest. Most commonly breast ptosis occurs due to age, childbearing, nursing, weight-gain, and weight loss. Some women will have ptotic breasts without any of these conditions. In 2007, mastopexy represented the eighth most commonly performed cosmetic procedure in the United States. Over 126,000 breast lift procedures were performed in the 2007 compared to less than 20,000 procedures in 1997, a 534% increase.26 The majority of mastopexy procedures were performed on women between the ages of 35 and 50 years of age with the remainder evenly divided between those below age 35 and age 50 or greater.
Problems that frequently are corrected by mastopexy procedure include: loose, lax skin tissues, malposition of the nipple-areola complex on the breast mound, bottoming out and sagging of the breast parenchyma. The degree of breast ptosis is classified in a Grade I to Grade 3 scale based upon the position of the nipple-areola complex in relation to the base of the breast.27 The type of mastopexy procedure performed is often based upon the grade of breast ptosis.
In the United States, the traditional mastopexy has been performed using an “Inverted T” incision to remove the excessive skin and redistribute the breast parenchyma. This technique allows the surgeon control of the breast tissue but creates a larger scar on the breast. In general only skin is excised and the breast tissue is maintained allowing the retained skin to shape the breast like a “skin bra”. Numerous forms of “short-scar” mastopexy techniques have been developed. Any mastopexy procedure that results in an incision length that is smaller than the traditional “inverted T’ incision is classified as a “short-scar” technique.28
The concept of performing a mastopexy through an incision just around the nipple-areola complex is not new. This technique was described in 1928.29 This and subsequent periareolar mastopexy techniques were limited to mild cases of breast ptosis. These techniques can place excessive tension on the nipple-areola complex which can lead to hypertrophic scarring, enlargement and distortion of the areola. In 1988, Benelli described a modification of the classic periareolar mastopexy in which the breast parenchyma is also resected and reshaped through the periareolar incision to increase the projection of the lifted breast-often described as a “round-block technique”. To control the enlargement of the nipple-areola complex, Benelli incorporated a circumareolar purse-string suture around the areola. This circlage suture serves to take tension off of the areola tissues and diminish the risk of areola distortion and hypertrophic scarring. 30, 31 The original purse-string sutures were absorbable often resulting in widening of the areola and scar. 32 Spear used a permanent suture for the circumareolar purse-string closure. Many of the early permanent suture such as nylon or Prolene© often stiffened or fractured with time. Presently Gore-Tex® sutures are recommended.
In 2007, Dennis Hammond modified the application of using a Gore-Tex® suture for controlling the dimensions of the nipple-areola complex by introducing the “wagon wheel” stitch design to distribute the tension evenly between the areola and the surrounding tissues.33 The combination of using a permanent Gore-Tex® suture with minimal tension on the nippleareola has resulted in enhanced appearance of the final scars and better control over the final size and shape of the nipple-areola complex. (See Figure 3).
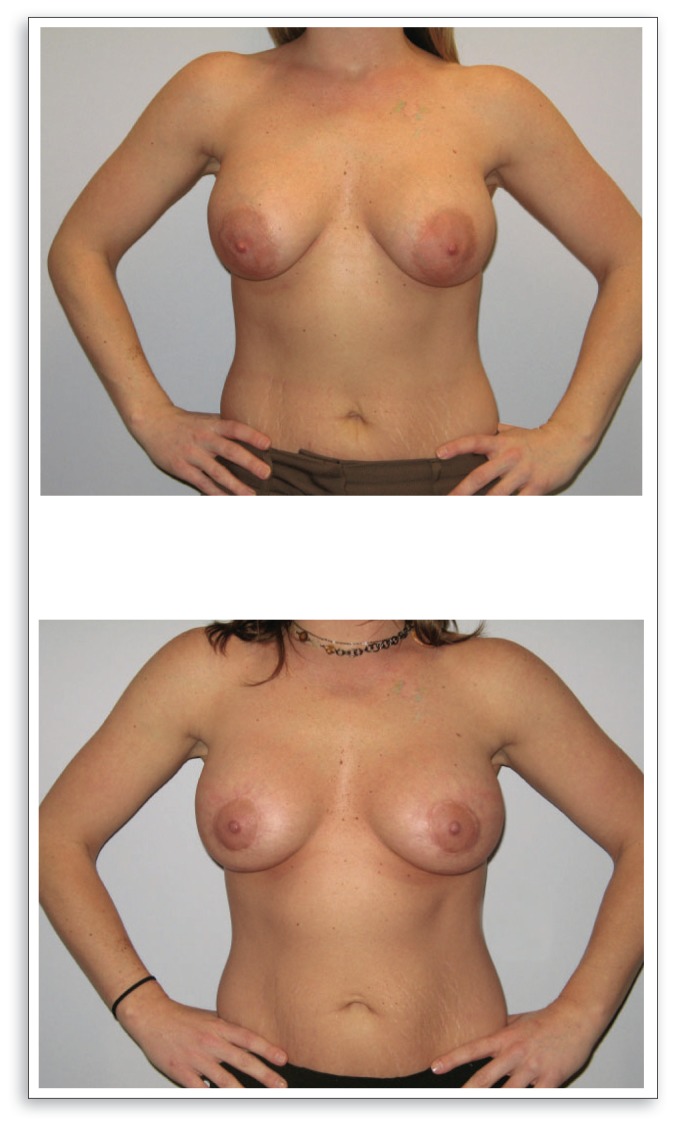
Figure 3.
Above, pre-operative view of a 25-year old patient with breast ptosis and nipple-areola mal-position. Below, ten month postoperative view after a circumareolar mastopexy.
Circumareolar mastopexies are limited by the degree of ptosis correction that can be achieved using this technique. The circumareolar mastopexy is for the most part, a nipple-areola lift procedure that lifts and re-centers the nipple-areola back on the breast mound. If the distance of the nipple-areola lift is too large, then with tightening and closure of the purse-string suture there is potential for significant flattening of the breast mound with loss of the natural flow and projection. If there is large amount of bottoming of the breast as occurs with severe breast ptosis, then performing a circumareolar mastopexy can result in inadequate correction of the fullness in the base of the breast and recurrent ptosis will occur. Therefore, correction of larger grades of ptosis often requires a more aggressive mastopexy with more incisions and manipulation of the breast tissues than the circumareolar lift.
Many of procedures which attempted to incorporate a vertical incision were plagued by the inability to minimize the scarring of the vertical incision from the nipple to the base of the breast. There were also problems with recurrent ptosis due to lack of control of the breast parenchyma in the inferior portion of the breast.
Lassus described a method by which a wedge of skin and breast tissue is removed in a vertical direction directly inferior to the nipple. This leaves a medial and lateral portion of tissue on the lower pole of the breast that has been termed the ‘medial” and “lateral pillars” which when sewn together gain control of the lower shape of the breast 34. This reshapes the breast mound while increasing projection of the nipple-areola complex. 35
Lejour felt that if the pillars were adequately approximated, scaring of the vertical incision is minimal despite its placement on the most prominent part of the breast. This is due to the internal support of the “pillars” which prevent widening and displacement of the scar. The scar itself is barely visible because it fades substantially over time and only rarely becomes hypertrophic36. Later, Graf and Biggs describe an inferiorly based flap passed under a pectoralis muscle loop and secured to the chest wall used in combination with a vertical lift incision.37
The vertical technique has become the mainstay of mastopexy for women with slight to moderate ptosis who have substantial remaining breast parenchyma. This glandular redistribution can be combined with incision patterns, leading to a short oblique scar, an L-shaped scar, a Y-shaped scar or an inverted-T scar.38,39 This procedure has good long term results by increasing upper pole fullness without an implant. Superior results are obtainable in patients who are not candidates for the concentric mastopexy without the need for a permanent suture, though Gore-tex® it is often used regardless. Regardless the method, skin is incised and removed while also allowing the lateral breast pillar to be sewn to the medial breast pillar thus tightening and lifting the lower pole of the breast. The addition of glandular suspension techniques reduces or eliminates the reliance on the skin envelope for suspension, thereby improving long-term results in current Mastopexy surgery.
Limiting the Scars: Vertical Reduction Mammaplasty
Reduction mammaplasty, or breast reduction, is frequently performed as a “medically necessary” treatment for neck, back, and shoulder pain associated with macromastia-hypertrophy. It can also be performed for aesthetic reasons. In 2007, over 150,000 breast reductions were performed in the United States making this the fifth most commonly performed plastic surgery procedure.27 With the common goals being to preserve nipple viability and sensation, maintain skin flap circulation, and achieve an aesthetic breast shape, numerous techniques have been described. The technique most commonly used for the past 25 years has been the inferior pedicle technique using some variation of the “inverted T” incision. This technique has proven to be safe, reproducible, and reliable. This is especially important in the litigious environment of the United States. The addition of the “Wise Pattern” introduced in 1956 further simplified the inferior pedicle technique by developing a simple template that could be adapted and applied to a wide variety of breast shapes and sizes. 40,41 (See Figure 4.) These advantages were offset by increased scarring from the longer incisions, the potential for a more “boxy”, unnatural breast shape, and the persistent problems of recurrent “bottoming out” of the breast because of poor elasticity in the skin tissues required to support the retained breast parenchyma.
Figure 4.
Mckissock Breast Marker 38mm Key Hole for breast reduction based upon the Wise pattern.
In Europe and South America, other techniques for reducing the breast size were developed using either a periareolar incision alone or some form a vertical closure that eliminated the long, horizontal incision along the base of the breast. 42,43,44 The techniques first described were often limited because of restrictions in the amount of breast tissue that could be safely resected, the increased risk of nipple necrosis, or the problems with flattening and misshaping of the breast mound. 45 These techniques are difficult to teach and relied on a great deal of personnel intuition making consistency of the results less than ideal.
In 1999, Hall-Findley published her reduction mammaplasty technique using a vertical closure in combination with a medially-based pedicle. The technique is adaptable to a wide variety of breast shapes and sizes. It is safe with minimal risk of nipple necrosis or skin slough and often maintains excellent nipple sensation. The incisions are limited to around the nipple-areola complex and a single vertical line from 6 o’clock on the areola to the base of the breast on the chest wall. This technique results in an aesthetic breast shape with good nipple-areola projection. (See Figure 5.) The most important aspect of Hall-Findley’s technique is the ease by which it can be learned and taught. Hall-Findley accomplished this by adapting the commonly used Wise pattern that most plastic surgeons in the United States were familiar with for planning a reduction mammaplasty using the inferior pedicle technique for the planning and marking the of the breast prior to using her medial pedicle technique.
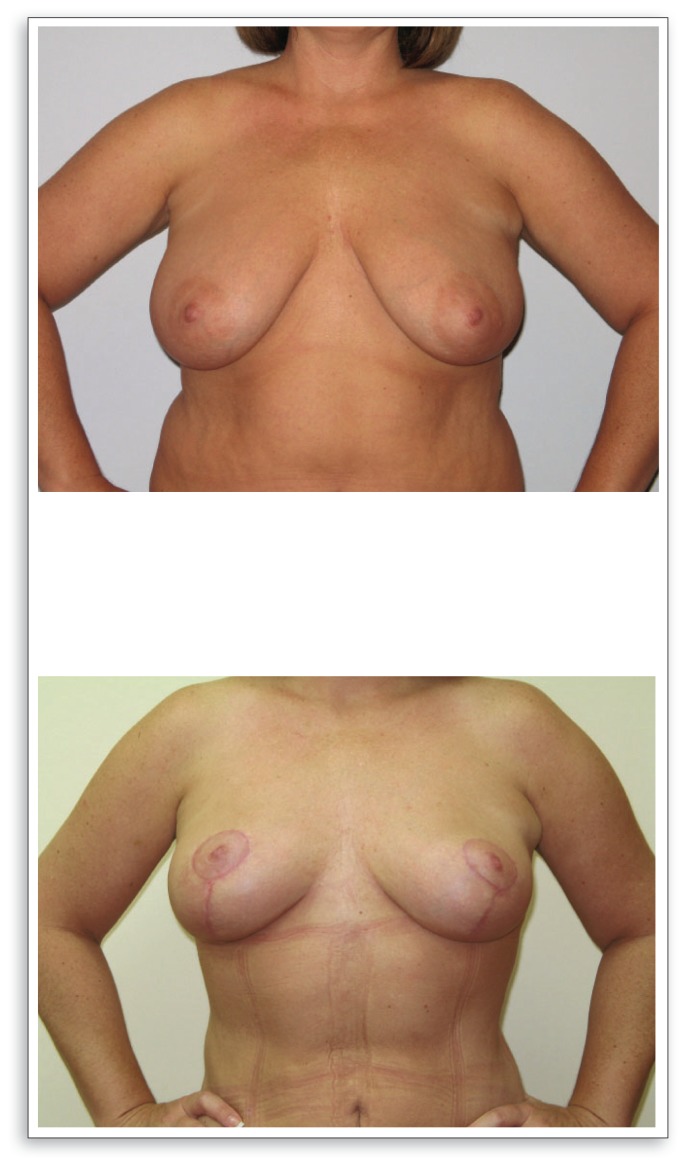
Figure 5.
Above, Pre-operative view of a 39-year old patient with a 34DDD cup size and complaints of back, neck, and shoulder pain. Below, two-month view status post vertical reduction mammaplasty using the Hall-Findley medial pedicle technique. Note the increased projection and shaping of the breast. The incisions will fade significantly within the first year.
Since Hall-Findley’s technique has been published, numerous other vertical reduction Mammaplasty techniques have been described, many using variations of Hall-Findley’s adaption of the Wise pattern for breast reduction. 46,47,48
Liposuction Reduction Mammaplasty
Many of the advances in surgery in latter part of the 20th century have the common thread of using very small incisions instead of the traditional longer incisions. Procedures such as laparoscopic cholycystectomy, laparoscopy, arthroscopic joint procedures and others used minimally-sized incisions with quicker recovery and less morbidity. With the advent of liposuction, the same concept was applied for performing reduction mammaplasty using liposuction alone.49,50
The advantages of using only liposuction to reduce the breast size include: smaller, almost invisible scars, less disturbance of the vascular and sensory structures of the breast better preserving sensation and viability, minimal disruption of the parenchymal support structures of the breast resulting in better shaping of the breast mound, possible preservation of lactation, and the ease of being able to match the opposite breast in shape and size. 51
The most significant disadvantage of using liposuction alone for performing reduction mammaplasty is the limited size and types of breasts in which the technique can be applied. Breasts that are too large in size require a volume resection greater than is safely accomplished using liposuction alone and a more traditional reduction technique may be required. Even in patients with breasts requiring smaller volume resections may not be candidates for liposuction mammaplasty due to poor quality of the skin since this technique is dependent upon skin retraction to achieve the desire final breast shape. Post-menopausal women or those with large stretch marks may not be suitable for this technique. Women with very dense, fibrous breast parenchyma also may not be good candidates for reduction Mammaplasty using liposuction alone.
As with all techniques and procedures, the key to successfully achieving the desired outcome is defining the problem and choosing the correct technique based on the patient’s unique physical characteristics and medical history. Further developments in liposuction technology such as laser-assisted lipolysis, radio-frequency assisted liposuction, and others may increase the applications for using this technology for reduction Mammaplasty in the future.
Biography
Herluf Lund, Jr., MD, MSMA member since 1991, is in a private practice partnership at St. Louis Cosmetic Surgery, Inc. Arthur Kumpf, MD, MSMA member since 2009, is a senior resident in plastic surgery at Saint Louis University.
Contact: hglund@stlcosmeticsurgery.com

Footnotes
Disclosure
Dr. Lund is a principle investigator of the Allergan Style 410 Breast Implant but is not an investor nor stock holder of Allergan stock. He is not compensated for study time but has received two stipends to cover costs to attend study meetings.
References
References exceed space limts. Please email Managing Editor Liz Fleenor at lfleenor@msma.org for list.