Abstract
The long Iraq and Afghanistan conflicts have thrust Combat Related Post-Traumatic Stress Disorder (CR-PTSD) into the public consciousness and promoted national dialogue on the incidence and results of war related psychological trauma. In the first of a two part series we outline our contemporary understanding of CR-PTSD, the evolution of the diagnosis throughout the history of modern warfare, its impact on the mind and body, and its treatment. PTSD has become the mental health issue of our time.
Prologue [excerpted from Historia Verdadera de la Conquista de Nueva Espana].
“We were all in that great city a warring, thinking, fearing that from one hour to the next they were going to give us war. Orteguilla and the page of Montezuma were all crying and we were always ready.
I said that we were always ready and that there was no need for us to be told because day and night we always carry our weapons and equipment and we slept with them and our beds were hay mats of grass. We slept with our boots on and all kinds of weapons ready and our horses saddled. We were all so prepared that we were holding our arms and were awake and alert at night. No soldier was asleep.
And I say without bragging that I became so accustomed to going carrying arms and to sleeping that way that after new Spain was conquered, I have the custom to sleep with my clothes on, without a bed that nowadays, when I visit different towns I don’t carry any bed, and if they force me sleep in a bed, I sleep with clothes on and will also say that I cannot sleep but a little during the night that I had to get up and watch the sky in the dark and I cannot cover my head with anything because of my habit and I have said this so that you will know how we, the true conquistadores conducted ourselves and how we were accustomed to be armed and to be vigilant...”
1517–1521: During the fall of Tenochtitlan-the center of the Aztec Empire. Bernal Diaz del Castillo, Historia Verdadera de la Conquista de Nueva Espana. Coleccion Austral-Espasa Calpe, Madrid, 1989, 8th Edition. Chap.108 P229
Post Traumatic Stress Disorder Evolution of Diagnostic Criteria
Post Traumatic Stress Disorder (PTSD) is a specific cluster of psychiatric symptoms which may develop in direct response to an exogenous, overwhelming traumatic event. This diagnosis was introduced in 1980 by the American Psychiatric Association in the 3rd Edition of Diagnostic Statistical Manual (DSM III). In previous editions (DSMI,1952; DSMII, 1968) a diagnosis “Gross Stress Reaction” captured traumatic reactions or such symptoms were simply assigned to “Situational Disturbances of Adult Life.” The conceptualization of traumatic psychological injury and diagnosis were continuously refined in subsequent classifications. In its current iteration, the DSMIV (2000)2, the diagnostic criteria (See Table 1) have evolved, particularly with respect to the understanding of the role of a traumatic stressors and those characteristics which distinguish it from other stressful events.
Table 1.
309.81 Posttraumatic Stress Disorder
| In 2000, the American Psychiatric Association revised the PTSD diagnostic criteria in the fourth edition of its Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). |
| Diagnostic criteria for PTSD include a history of exposure to a traumatic event meeting two criteria and symptoms from each of three symptom clusters: intrusive recollections, avoidant/numbing symptoms, and hyper-arousal symptoms. A fifth criterion concerns duration of symptoms and a sixth assesses functioning. |
|
Criterion A: Stressor The person has been exposed to a traumatic event in which both of the following have been present:
|
|
Criterion B: Intrusive Recollection The traumatic event is persistently re-experienced in at least one of the following ways:
|
|
Criterion C: Avoidant/Numbing Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by at least three of the following:
|
|
Criterion D: Hyper-Arousal Persistent symptoms of increasing arousal (not present before the trauma), indicated by at least two of the following:
|
|
Criterion E: Duration Duration of the disturbance (symptoms in B, C, and D) is more than one month. |
|
Criterion F: Functional Significance The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. Specify if:
Specify if:
|
Source: American Psychiatric Association. (2000).
However, there remain differences among military and civilian psychiatry regarding the role of traumatic stressors in producing PTSD. Some researchers question whether PTSD is the most common illness triggered by trauma. In Australians, Bryant3 found that depression, generalized anxiety disorder and agoraphobia were also associated with traumatic exposure and that only 9% of those with a diagnosis of PTSD had no co-morbid disorder.
DSM V
The 5th Edition of DSM is in preparation and the conceptualization and diagnosis of traumatic conditions remains hotly debated. A draft is available for review and comment at www.dsm5.org. Chu4 discusses the work of Lanius et al 5 positing that PTSD is best divided into subtypes, based on differential consequences of traumatic exposure identified by neurobiological evidence. For example, in some exposed to prolonged, repeated traumatic experiences (e.g. chronic childhood trauma or combat), a “dissociative” subtype of PTSD, marked by emotional numbing of feelings, detachment and dissociative amnesia may develop. Lanius goes on to describe how over-modulation of emotions and a “subjective disengagement from the emotional content of the traumatic memory,” where defense mechanisms of derealization and/or depersonalization are employed.
Because hyper-inhibition of the limbic system by prefrontal areas occurs in high emotional stimulation, such detachment may be produced by the suppression of the limbic system, and diminish hippocampal activity. In contrast, when exposed primarily to acute trauma, a subtype of hyper-arousal and intrusion often develops. With advances in functional MRI, studies are able to identify neurobiological differences in these subtypes which may lend further understanding to these differences in symptom development and expression.
The History of PTSD in Warfare
Some form of traumatic injury has existed as long as humans have waged war on one another. Soldiers are called to serve, and while answering their call they are exposed to the horror of war, to death, to deprivations, to extremes of the environment, and perhaps most psychologically damaging of them all, to the perfidy of men in war. Exposure to these innumerable stressors may injure them for life; PTSD is one of the unseen wounds.
Reports of the psychological effects of combat can be found in ancient literature, as is evident in John Shay’s analysis of Homer’s Iliad and Odyssey.6 In the conquest of America, Bernal Diaz de Castillo provides additional examples. In The Book of War,7 John Keegan reviews battles and episodes that describe aspects of war from the heroic, to the “gentlemen’s wars” to present brutal and unbridled conflicts. In Airman’s Odyssey, 8 Saint Exupery, described the qualities of men sent to war, how their sense of responsibility guide them to complete their missions at all cost, at the same time, in Fly to Arras9 he discusses the futility of war.
Irrespective of the war’s era, participants, or their rationale, psychiatric casualties result from them all. The common denominator is simply the psychological toxicity stemming from the cruelty and inhumanity of warfare.
The American Civil War
PTSD has long existed under different names. During the Civil War, physicians labeled these conditions based on presumed etiologies or symptom expression. (See Figure 1) For example, diagnoses of the era were “soldier’s heart”, “irritable heart,” “sunstroke,” or “nostalgia.”
Figure 1.
Union soldiers, Petersburg, Virginia 1865. These men knew that many of them would not survive the coming battle.
Source: National Archives
Disease killed more Confederates (150,000) than battle deaths (50,000). For the Union it was about 224,586 and 110,070. (See Figure 2) Psychiatric casualties were not mentioned.10
Figure 2.
Union and Confederate dead soldiers. Gettysburg, PA. 1863 The mental stress of combat incapacitated solders on both sides.
Source: National Archives
In Doctors in Gray10, it was reported that “psychoneurosis were caused by a combination of past experiences and the sympathy that soldiers received behind the lines….actual battle experiences, it appears, are not as important as secondary mental processes in the causation.”
Accordingly, the pathology was thought to result from internal vs. external (i.e., traumatic) experiences.
However, battlefield physicians of the time were beginning to entertain the notion that trauma could have a role in producing psychiatric illness; this is mentioned in their hypothesis that “...some diseases of the brain and nervous system had a traumatic origin.”
As the Civil War wore on, surgeons became aware of the symptoms of emotional distress and the role of psychiatric symptoms in battlefield medical outcomes: “Men were...subject to spells of homesickness, or ‘nostalgia’ and anxiety, when they suffered them to a morbid degree, that did more than anything else to cause death.” As soldiers continued to die in the hospital of “nostalgia,” surgeons discovered that a furlough was the best treatment and better than all medications; indeed, the promise of escaping the horror of battle and returning home proved a powerful intervention.
In the last year of the war, the number of psychiatric casualties increased to the point that Medical Director Carrington informed Surgeon General Moore of the need to establish a Confederate Hospital for “cases of lunacy and dementia.” Though there are limited epidemiological records of the period, it is likely many of these cases were suffering from “soldier’s heart” or other diagnostic precursors of CR-PTSD. In spite of the mass carnage of the civil war and the likely high numbers of psychiatric casualties, traumatic psychic injuries remained an unappreciated contributing factor to the suffering of survivors.
Though perhaps formally unacknowledged in military medicine, the literature of the period captured the psychological effects of war. For example, Walt Whitman, who observed this damage first hand tending to the wounded both in Union hospitals and in the field, described these effects in poems such as the “Memoranda During the War”, “The Wound Dresser” and others.11, 12
World War I
The military’s stance towards psychiatric injury did not show much progress in the wars of the early 20th century. Indeed, the military continued to view trauma-induced psychiatric problems as a deficiency of character. Men whose symptoms we can now recognize as those resulting from true psychiatric breakdown were shot for desertion or dereliction of duty during the early years of WWI. When the only escape from the horrors of war was possible execution, the fear of this penalty yielded hysterical conversion symptoms. Cases of hysterical blindness, paralysis and other nervous system diseases became epidemic in the trenches. Faced with overwhelming numbers of these casualties and limited treatment options, the military re-conceptualized these conditions as consequences of nervous system damage secondary to the unprecedented use of massed artillery endemic to trench warfare. A major WWI offensive often began with over a million rounds of heavy artillery. The new term, “shell shock,” ushered in a shift in medical/military response and military physicians rediscovered the restorative power of removing soldiers from the front lines. (See Figure 3) Consequently, these conditions were then considered medical illnesses that required treatment. Such cases were referred to as “NYDN” (Not Yet Diagnosed, Nervous) and were treated in hospitals.13
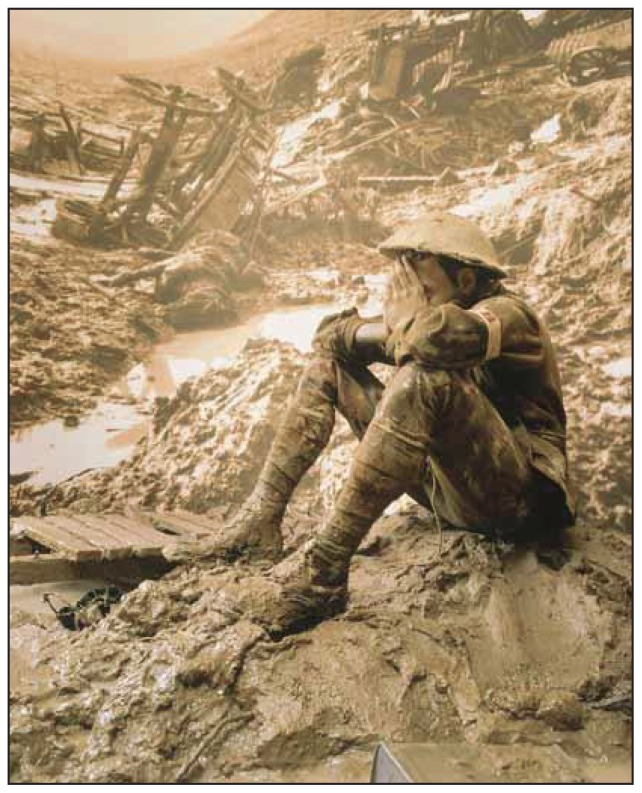
Figure 3.
Massive and unrelenting artillery bombardment killed more soldiers in WWI than gunfire and led to the term “shell shock” a form of PTSD.
Source: Australian War Memorial
As the promise of escape from the lines without threat of execution spread, the number of such cases dramatically increased among troops. This triggered a review in 1916 and using the psychiatric science of the time (i.e., psychoanalysis), the condition was classified as “hysteria” and as such, was considered to be a defect due to pre-existing personality disorder. In so doing, governments were exonerated from paying disability for such cases as the illness was attributed to ‘characterological’ problems rather than psychological injury secondary to traumatic combat exposure.14
World War II
As the science of psychiatry evolved, so did conceptualizations of the role of mental factors in combat functioning on the battlefield. British and American psychiatrists insisted on the recognition of psychiatric combat-related cases. Revolutionary advances in psychological assessment, screening tests were employed to select only the psychologically fit for wartime military duty. As the high rates of psychiatric casualties in WWII would prove, this testing was not able to predict who will develop combat-borne mental conditions. As the war progressed, more soldiers were leaving the battlefield due to psychiatric reasons than could be replaced by fresh soldiers coming out of basic training (See Figure 4).
Figure 4.
Iwo Jima, Mount Suribachi February 19, 1945. In a little more than six weeks, US forces sustained about 7,000 deaths and 19,500 wounded.
Once again, the reality of human psychological limits in war forced reconsideration of traumatic phenomenon. Military psychiatrists soon learned that peri-traumatic psychological processes (i.e., the impact of the stress of combat) were stronger predictors than pre-trauma or post-trauma factors. Psychiatric casualties were subsequently recognized and diagnosed with “combat exhaustion” or “battle fatigue” and thus reclassified as neuropsychiatric (vs. hysterical) disorders. Furthermore, with increased research attention, studies produced more reliable statistics on psychiatric casualty rates. Epidemiological figures varied but between “2 to 30% of battlefield injuries were classified as psychiatric casualties.”15
Indeed, when more systematic studies were conducted, the American official report on “combat exhaustion” stated “almost all soldiers exposed to continuous or semi- continuous combat broke down,” and that a soldier passed his peak combat-effectiveness within the first 90 days of active fighting. After that, most combatants suffered from mental exhaustion and became at risk for psychological break down. One conclusion is, “there is no such thing as getting used to combat.”
Following the war, Swank and Marchland16 studied combat effectiveness as a function of battlefield exposure. They found that after 60 days of continuous combat, 98% of all surviving soldiers became a psychiatric casualty of one type or another. This data was instrumental in changing military doctrine (e.g., rotating troops, lengths of deployments, etc.) during the Korean and Vietnam wars. This discovery is of timely interest given the current military policies on multiple deployments and the potential relationship of repeated combat exposure to the development of PTSD.
Korean War
Though referred to as the “forgotten war” (1950–53), this conflict produced tremendous casualties and unrecognized psychiatric injury to its combatants. Korean War veterans, like their WWII counterparts, share in their reluctance to complain and to describe their symptoms.
We recall a humble patient who was concerned because he was “taking our time when others have more serious problems;” he was involved in the taking of Mount Suribachi (See Figure 4). At our request he brought in his papers: there were citations for a Bronze and Silver Stars. Many of the combatants participated in the exhaustive retreat across the frozen Korean peninsula after China joined the war. Some witnessed or experienced torture and saw executions of US prisoners by Korean and Chinese soldiers. The Korean War never officially ended. Korean War veterans frequently feel that their pain, suffering and the deaths of their comrades are forgotten and unappreciated by the American public.
The Viet Nam War
The Vietnam War marked a turning point in our national understanding and dialogue of the role of traumatic injury in war. The result of this was the National Vietnam Veterans Readjustment Study (NVVRS).17 which estimated that 15.2% of all male and 8.5% of all female Vietnam veterans suffer from PTSD (total number estimated at 450,000). Lifetime occurrence rates estimated that 30.6% male and 26.9% female have had the full blown PTSD syndrome at some time since their war experience. Though this study was conducted in the 1980s, these veterans continue come into our clinics, many of have been isolated and avoiding treatment for 35–40 years. Many of these veterans coped with their PTSD symptoms through constructive or destructive means, or often times, both.
One PTSD Vietnam veteran remarked, “I got through it because I worked a lot, and I drank a lot.” Many have presented after retirement, as their war memories, no longer suppressed or distracted, now vie for expression. After the Indonesian War (1945–1949), Dutch soldiers suffered similar problems; after retirement they were affected by PTSD. The combat-related post traumatic stress disorder soldiers-sailors and airmen are still at war: in the frozen forests of Europe, the steamy jungles of the Pacific, in sinking submarines, the flak and SAM filled skies over Hanoi, the desert in Iraq, everywhere the US has placed their troops in harm’s way. Living with war is a daily struggle not relieved by an honorable discharge and a return to civilian life.
The Gulf War
Though relatively brief in duration, many Desert Storm/Gulf War soldiers were exposed to sundry traumatic stressors. The “Highway of Death” is but one example, soldiers saw burned, maimed bodies, smells of burnt flesh, and images of human carnage. Some troops were also exposed to artillery/missile attacks and the threat of chemical/biological weapons.
The Institute of Medicine in Gulf War and Health, Vol. 8: Update of Health Effects of Serving in the Gulf War, reported that the Persian Gulf war’s traumatic events led to PTSD and other psychiatric conditions to include generalized anxiety disorder, substance abuse, and depression. The prevalence of psychiatric disorders continued for a least a period of ten years, with prevalence rates two times those of non-deployed Gulf War era troops. In addition to psychiatric diagnoses, gastro-intestinal disturbances (irritable bowel syndrome), dyspepsia, and other multi-symptom difficult to explain illnesses (known as Gulf War illness or syndrome) became the hallmark condition of this war.18 Additional advances during this time lead to the investigation of functional neurological markers of PTSD which offered promise in diagnosis and disorder classification.19
Iraq and Afghanistan Wars
The “signature neuropsychiatric injuries” of the current wars are PTSD and traumatic brain injury (TBI), the latter usually secondary to sophisticated and enormously powerful improvised explosive devices (IEDs) blast injuries that are ubiquitous in these war zones (See Figure 5). As technology is employed (i.e., body armor, blast resistant armored vehicles, etc.) to protect our soldiers against IEDs, many are surviving traumatic injury that would PTSD: Part I - a Micro Series have typically resulted in death in past wars. Accordingly, survivors are now facing a host of mental and physical injuries at rates yet to be determined.
Figure 5.
Improvised explosive devices (IEDs) are the leading cause of death and poly-trauma. IEDs kill hundreds of civilians and are oft en constructed with materials and expertise supplied by Iran.
Source: Source: http://www.awsg.us/2010/06/
Often, these disorders co-occur and have given rise to the “poly-trauma” concept in VA hospitals. The addition of TBI has added complexity to the already difficult-to-treat PTSD spectrum disorders. At this time, the VA is putting substantial resources into better understanding and treating these types of multi-system traumatic injuries. Recent figures suggest 300,000 Operation Iraqi Freedom/Operation Enduring Freedom veterans are suffering from PTSD and TBI and estimates of PTSD for returning veterans run from 12–20%. Additional research findings are available at www.ptsd.va.gov.
Biography
Juan C. Corvalan, MD, Col USAFR, (Ret), MSMA member since 1976, is a psychiatrist at the St. Louis VA Medical Center, an Emeritus Assistant Professor at Washington University School of Medicine, and serves on the Missouri MedicineEditorial Board. David Klein, PsyD, also practices at the St. Louis VA Medical Center and is an Adjunct Instructor in the Department of Psychiatry at Saint Louis University.
This is the first in a two-part series.
Contact: Juan.Corvalan@va.gov

Footnotes
Disclosure
None reported.
References
- 1.del Castillo Bernal Diaz. Historia Verdadera de la Conquista de Nueva Espana. 8th Edition. Chap 108. Coleccion Austral-Espasa Calpe; Madrid: 1989. p. P229. [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and statistical manual of mental disorders DSM-IV-TR. Fourth edition. Washington D.C: American Psychiatric Association; 2000. [Google Scholar]
- 3.Bryant Richard, PhD, et al. The Psychiatric Sequelae of Traumatic Injury. American J Psychiatry. 2010;167:312–320. doi: 10.1176/appi.ajp.2009.09050617. [DOI] [PubMed] [Google Scholar]
- 4.Chu James A., MD Posttraumatic Stress Disorder: Beyond DSM-IV. Am J Psychiatry. 2010;167:615–617. doi: 10.1176/appi.ajp.2010.10030310. [DOI] [PubMed] [Google Scholar]
- 5.Lanius Ruth A, et al. Emotion Modulation in PTSD: Clinical and Neurobiological Evidence for a Dissociative Subtype. Am J Psychiatry. 2010;167:640–647. doi: 10.1176/appi.ajp.2009.09081168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shay J. Combat Trauma and the Un of Character. First Edition. Touchstone Book; N.Y: 1995. Achilles in Vietnam. [Google Scholar]
- 7.Keegan John. The Book of War. Penguin Group; New York: 1999. [Google Scholar]
- 8.de Saint Exupery A. Airman’s Odyssey. Harcourt Brace Jovanovich; 1984. [Google Scholar]
- 9.de Saint Exupery A. 1- Terre des Hommes. Gallimard; 1939. [Google Scholar]
- 10.Cunningham HH. Doctors in Grey: The Confederate Medical Service. Baton Rouge: Louisiana State University Press; 1958. pp. P5pp. 181–183.pp. 211–217. [Google Scholar]
- 11.Whitman Walt. Memoranda During the War. Applewood Books; Bedford, Massachusetts: Originally published by the author in 1875. [Google Scholar]
- 12.Whitman Walt. The Civil War Poems. Barnes & Noble Books; New York: 1994. [Google Scholar]
- 13.Keegan John. The Face of Battle. London: The Folio Society; 1976. MMVIII.P306. [Google Scholar]
- 14.Nash WP, et al. The Historic Origins of Military and Veteran Mental Health Stigma and the Stress Injury Model as a Means to Reduce It. Psychiatric Annals. 2009 Aug;39:8 P789. [Google Scholar]
- 15.Keegan John. The Face of Battle. London: The Folio Society; 1976. MMVIII. P307. [Google Scholar]
- 16.Swank RL, Marchland WE. Combat Neuroses: development of combat exhaustion. Archives of Neurology and Psychology. 1946;55:236–47. doi: 10.1001/archneurpsyc.1946.02300140067004. [DOI] [PubMed] [Google Scholar]
- 17.Kulka RA, et al. Al The National Vietnam Veterans Readjustment Study. Brunner/Mazel; NY: 1990. [Google Scholar]
- 18.Schneider ME. IOM: Gulf War Combat Trauma Led to PTSD. Clinical Psychiatric News. 2010;38(5):1–5. [Google Scholar]
- 19.Georgopoulos AP, et al. The synchronous neural interactions test as a functional neuromarker for post-traumatic stress disorder (PTSD): a robust classification method based on the bootstrap. J Neural Eng. 2010:7. doi: 10.1088/1741-2560/7/1/016011. [DOI] [PubMed] [Google Scholar]; Georgopoulos AP, et al. J Neural Eng. 2007;4:349–55. doi: 10.1088/1741-2560/4/4/001. [DOI] [PubMed] [Google Scholar]