Abstract
Objectives
Limited data are available on the correlation of mHealth features and statistically significant outcomes. We sought to identify and analyze: types and categories of features; frequency and number of features; and relationship of statistically significant outcomes by type, frequency, and number of features.
Materials and Methods
This search included primary articles focused on app-based interventions in managing chronic respiratory diseases, diabetes, and hypertension. The initial search yielded 3622 studies with 70 studies meeting the inclusion criteria. We used thematic analysis to identify 9 features within the studies.
Results
Employing existing terminology, we classified the 9 features as passive or interactive. Passive features included: 1) one-way communication; 2) mobile diary; 3) Bluetooth technology; and 4) reminders. Interactive features included: 1) interactive prompts; 2) upload of biometric measurements; 3) action treatment plan/personalized health goals; 4) 2-way communication; and 5) clinical decision support system.
Discussion
Each feature was included in only one-third of the studies with a mean of 2.6 mHealth features per study. Studies with statistically significant outcomes used a higher combination of passive and interactive features (69%). In contrast, studies without statistically significant outcomes exclusively used a higher frequency of passive features (46%). Inclusion of behavior change features (ie, plan/goals and mobile diary) were correlated with a higher incident of statistically significant outcomes (100%, 77%).
Conclusion
This exploration is the first step in identifying how types and categories of features impact outcomes. While the findings are inconclusive due to lack of homogeneity, this provides a foundation for future feature analysis.
Keywords: mHealth, mobile health, chronic respiratory diseases, hypertension, diabetes
BACKGROUND AND SIGNIFICANCE
The healthcare field is experiencing exponential growth in mHealth (mobile health). According to the World Health Organization (WHO), mHealth refers to the utilization of mobile devices to support medical and public health practices.1 Currently, there are an estimated 325 000 health, fitness, and medical mobile apps available.2 This emerging field is viewed as a mechanism to enhance patient-centered care and improve patient outcomes from the perspective of healthcare providers (HCPs) and patients.3 For example, Ramirez and colleagues reported 86% of patients at multiple California primary care facilities expressed an interest in using mHealth for chronic health management and as a tool to learn about their health.4 mHealth interventions focused on chronic diseases have the potential to significantly affect the overall state of health in the United States; however, an initial look at the mHealth literature revealed mixed results, with some studies reporting no statistically significant outcomes (SSOs).5,6
Previous reviews
An appraisal of existing mHealth systematic reviews and meta analyses revealed some notable information on mHealth features. First, bi-directional and personalized, tailored short message services (SMSs) appear to be more effective in producing SSOs than generic uni-directional SMSs in managing chronic health conditions.7–12 Next, several reviews and meta-analyses examined how patients and HCPs communicated via a mHealth app with inconclusive results.13–15 Other reviews examined mHealth features, but did not correlate the features to SSOs.16–23 Stephani and colleagues identified 3 intervention categories along with personalization and interactivity of the intervention in each study; no direct correlation of outcomes with intervention was reported.24 These reviews presented exceptional details on mHealth, but how mHealth features and categories correlate with outcomes was unclear.
Another finding from these reviews was the diverse categories of mHealth features. A lack of consensus on categories and definitions of mHealth features became apparent. Some reviews used very broad feature categories15,16,18,24 while other reviews described very specific features.19,21 This diversity of categories and definitions may serve as a barrier to the translation of effective mHealth features.
One must ask why the use of some mHealth apps improves patient outcomes while other mHealth apps do not. These disparate outcomes need further analysis to identify the differences between the 2 groups (ie, mHealth studies with SSOs vs mHealth studies without SSOs). One possible explanation for the differences in outcomes may depend on the categories and types of features contained within the mHealth app. Apps may include a mix of functions; for example, one weight loss app may offer features that allow weight tracking and calorie intake documentation, another may include a support group option, while still another may push daily inspirational messages to the user. A focus on an app’s specific features, rather than the app as a whole, may yield a more complete understanding.
Second, chronic disease self-management relies on the use of behavior change techniques (BCTs) to successfully manage the disease.25 BCTs originated from Michie and colleagues’ seminal classification of interventions to promote behavior change within healthcare.26,27 Some findings suggested that BCTs are unique based upon the desired outcome.28,29 Maintaining or starting healthy behaviors such as medication adherence documentation or completion of biometric measurements may require BCTs different from stopping a negative health behavior, such as cigarette smoking. Similarly, specific app features that facilitate stopping a negative health behavior may be quite different from those relevant to stopping or maintain a positive health behavior. Previous work on mHealth may have been confounded by a failure to examine studies based on the type of BCT.
OBJECTIVE
Based upon these assumptions, we focused the current exploration on primary studies that used mHealth tools to start or maintain health behaviors in the context of chronic diseases. mHealth may enhance the self-monitoring process, especially when monitoring chronic diseases with specific biometric measurements (ie, blood glucose, blood pressure [BP], peak flow) that are recorded by the patient and shared with an HCP for review and feedback. Chronic respiratory diseases (ie, asthma, chronic obstructive pulmonary disease [COPD]), diabetes, and hypertension (HTN) are 3 chronic diseases that monitor biometric measurements. These 3 diseases affect almost 44% of the U.S. population with $271 billion in direct healthcare cost in the United States.30–34 Furthermore, diabetes and HTN increase a patient’s risk for development of cardiovascular disease, which further expands healthcare costs.35 As the application of mHealth tools is very similar in the management of these conditions, we decided to focus on these illnesses to yield more details on mHealth app-specific features and how they may correlate with outcomes.
To address the gap involving mHealth features, we conducted a targeted exploration to identify specific mHealth features and how they potentially correlated with SSOs. We hypothesized that types and categories of mHealth features would be associated with SSOs. The purpose of the exploration was to specifically identify and analyze: 1) types and categories of mHealth features; 2) overall frequency and number of mHealth features; and 3) relationship of SSOs by type, frequency, and number of mHealth features.
MATERIALS AND METHODS
Prior to searching the literature, we defined the term mHealth feature, also known as interventions or BCTs, as a distinctive attribute or tool within a mobile app that assists patients in managing and monitoring all aspects of health.18,36 While previous literature suggested specific features were potentially relevant to starting and maintaining healthy behaviors (eg, SMS), we did not use a circumscribed list to prevent bias. Instead we employed a thematic analysis approach to identify features within the studies.37,38 The process required a careful and thorough analysis of the feature descriptions in each study with 1 author recording the descriptions in a spreadsheet, which was then reviewed and analyzed for themes by all authors. This method allowed the evidence to guide the identification of the mHealth features.
For studies involving 2 or more groups (ie, intervention and control), we included only outcomes reported between groups as the purpose of a control group is to isolate the independent variable’s effect (ie, mHealth app). However, we reported the within-group outcomes for single group studies. All reported outcomes compared baseline data with the final data. Also, subgroup outcomes were not included in the analysis, as the subgroup methodology was not defined prior to the study onset, which does not meet best practices standards.39 Finally, 3 studies included 2 intervention groups that introduced an additional independent variable (ie, intensive insulin therapy, bi-weekly telemedicine consultations, face-to-face health counseling).13,40,41 While all intervention groups used mHealth, the introduction of an additional independent variable clouded the analysis of mHealth efficacy. For these studies, we included only the comparison between the standard care control group and the standard care mHealth intervention group.
Search process
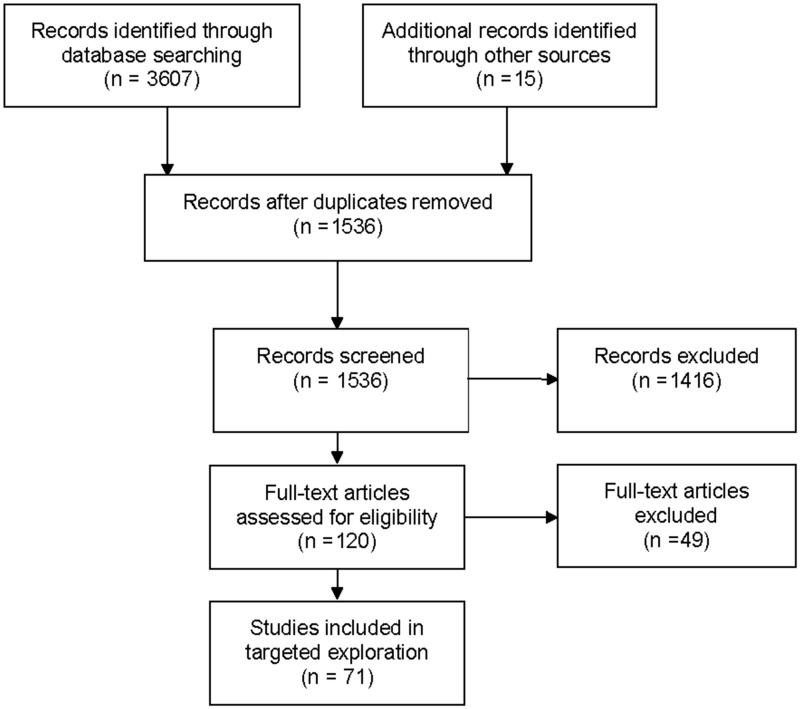
The search included primary articles focused on app-based interventions for the management of chronic respiratory diseases, diabetes, and HTN from the following databases: Cumulative Index to Nursing and Allied Health Literature, PubMed, EBSCO Academic Database, Cochrane Library, and Google Scholar. Search dates included 2002 to 2018. Two significant mobile advances occurred in 2002—SMS capability among networks and wireless email via Blackberry Smartphone—and provided researchers with new mHealth options.42,43 The search terms included key words in multiple combinations and used medical subject headings: self-monitoring, mobile application, mobile app, mHealth, text messaging, SMS, hypertension, high blood pressure, diabetes, asthma, COPD, chronic respiratory disease, wireless communication, cell phone, mobile phone, and mobile device. Initial search results yielded 3622 studies (See Figure 1).
Figure 1.
mHealth exploration flowchart.
Inclusion criteria
Inclusion of primary quantitative and mixed-methods studies was dependent upon the utilization of mHealth as defined by WHO—utilization of mobile devices to support medical and public health practices—in chronic respiratory diseases, diabetes, and HTN.1 For this exploration, only the quantitative results of mixed-methods studies were included. Primary journal articles available via university library sources including inter-library loan and written in English were included. Finally, reference lists of articles and reviews were examined to ensure inclusion of all relevant literature. The exploration included randomized control trials, descriptive studies, and pilot trials that tested and reported the efficacy of mHealth interventions.
Exclusion criteria
The use of eHealth, a broader term that incorporates other technologies not exclusive to mHealth, prompted exclusion from this literature exploration (n = 191).44 Unrelated studies (n = 902), qualitative studies (n = 49), reviews and meta-analyses (n = 163), research design and proposals (n = 90), and studies not available through university libraries (n = 9) or not available in English (n = 12) were removed from the analysis. After careful review, an additional 49 studies did not meet the inclusion criteria or had mitigating issues and were excluded (see Supplementary MaterialTable S1).45–93
Finally, 71 appropriate studies from 30 countries were included. Nundy and colleagues reported the same study in 2 separate articles.94,95 These 2 articles were merged into a single study to prevent duplication in the analysis. Most studies (81%) included at least 1 intervention group and control group in either a randomized methodology (n = 41) or a quasi-experimental methodology (n = 16). The remaining studies followed pre/post-test methodology with a single intervention group (n = 13). Supplementary MaterialTable S2 provides the mHealth feature details on each study.40,41,94–161,169
RESULTS
Using thematic analysis, we identified 9 mHealth features used 185 times in the 70 studies. Differences in the level of interaction between the patient and the features were observed. Other researchers described the interaction as 1-way or uni-directional features and 2-way or bi-directional features.24,97,98,104 Using these existing terms, human-computer interaction standards, and BCTs, we classified the features as passive or interactive based upon the level of interactivity between the patient and the feature.24,162–166 For this review, passive features were defined as features that do not require any additional response or action from the patient within the mHealth app. With passive features, the patient completes only the initial task (ie, reading the SMS or reminder, taking the biometric measurement). Passive features included: 1) 1-way SMS; 2) mobile diary to store and graphically display biometric measurements; 3) upload biometric measurements via Bluetooth; and 4) reminders.
In contrast, interactive features require patients to provide a response or modify the content in real time.163 Interactive features included: 1) interactive prompts; 2) direct upload of biometric measurements to HCP for review and timely feedback; 3) action treatment plan/personalized health goals; 4) 2-way communication (ie, texting, messaging, e-mail) between HCP and patient that is tailored to the patients’ biometric measurements, health goals, or health beliefs; and 5) clinical decision support system (CDSS).
Types of features
Passive features
As defined above, passive features did not require the patient to perform any additional task or response within the mHealth app. However, they delivered essential self-monitoring elements by providing education or health tips, displaying previous biometric measurements, uploading biometric measurements, and reminding the patient of upcoming events, tasks, or medications.
One-way SMS and messaging. One-way SMSs, also known as unidirectional messaging, are messages sent from the HCP or computer to the patient.97,98,104 The patient can only read the message. Researchers used these messages to educate, instruct, advise, increase awareness, and motivate the patient on specific health conditions and behaviors.96,101,140,142,149 Examples included: “Physical activity helps to maintain normal blood sugar and blood pressure” and “Were there many missed walks this month? No worries, start today.”142 Bell and colleagues used a slightly different approach by sending daily video messages instead of written messages.97 The frequency and timing of the messages varied from 1 per month to daily.97,117,121,159 Twelve studies used 1-way SMS as the only mHealth feature with 7 (58%) reporting SSOs.99,106,118,121,132,140,142 Ten additional studies combined 1-way SMS with other features. Only 2 studies (20%) reported no SSOs.105,132
Mobile diary. This feature stores biometric measurements and graphically displays the information for the patient to identify patterns and trends in the biometric measurements. Twenty studies included a mobile diary feature in addition to other mHealth features. Six studies (30%) reported no SSOs.13,107,108,110,114,150
Bluetooth technology. Bluetooth technology allows medical devices (ie, glucometers, BP cuffs, scales, etc.) to automatically upload data to the mHealth app.167 Nineteen studies incorporated Bluetooth with other features. Seven (37%) of these studies reported no SSOs.13,107,108,110,114,122,150
Reminders. A reminder is a message that reminds the patient about an upcoming action or task (ie, take medication, attend appointment). The patient does not respond to the reminder. Strandbygaard and colleagues used a reminder as the sole mHealth feature and reported SSOs.151 Twenty-eight additional studies included a reminder in combination with other features. Five studies (18%) reported no SSOs.105,107,108,122,132
Interactive features
Interactive features differ from passive features by providing feedback based upon patient input or requiring the patient to perform a responsive action within the app. These are bi-directional features. The patient engages with the mHealth app by sharing health data, setting health plans/goals, responding to tailored health questions, or receiving feedback based on biometric measurements.
Interactive prompts. This feature moves beyond reminders by requiring the patient to enter an appropriate response. These prompts originate from a computer algorithm, which differentiates this feature from the personalized 2-way SMS between an individual and the patient. Most interactive prompts elicited additional information from the patient such as symptoms, medication refills, appointment changes, and biometric measurements.101,102,104,105,129 Two studies used interactive prompts exclusively; Han and colleagues reported SSOs while Tasker and colleagues did not.119,153 Thirteen additional studies included interactive prompts with other mHealth features, and 3 (23%) reported no SSOs.105,141,147
Action treatment plan/personalized health goals with HCP. This process includes defining a behavior goal into quantifiable measurements with re-evaluation and modifications as goals are achieved.26 Twelve studies utilized an action treatment plan or personalized health goals with other features. All 12 studies (100%) reported statistically significant outcomes.40,41,109,111,129,130,143–146,152,161
Two-way or tailored communication between HCP and patient. Two-way communication includes SMS and e-mail between the HCP and patient. This interaction is dynamic, as it involves 2 or more individuals, which is different from the computer-based algorithms used in interactive prompts. HCPs provided feedback on biometric measurements or changed the patient’s health regime. In addition, content-tailored SMS messages encouraged changes in health beliefs and behaviors based upon the patients’ health beliefs and understanding of the disease process and management, which originated from surveys and questionnaires.26 Examples of personalized, 2-way SMSs included: “Your fasting blood glucose level is very high compared with the appropriate target level for type 2 diabetes (< 7.2 mmol / l). If this high level recurs often, diabetic complications might result. Reduce your calorie intake and avoid foods high in fat. In addition, plan for regular exercise after your meals” and “Hi <patient name>- Another pretty good week—just a bit concerned about some odd higher levels in the morning—looks like some of these are forgotten doses - would that be right? Otherwise all are getting better and no real hypos. Be aware you may need to tweak basal if those highs are not related to forgotten doses. Your thoughts?”125,160 This personalization recognized the patient as a unique individual with unique health needs and goals. Petrie and colleagues exclusively used 2-way communication with SSOs.139 Twenty additional studies used 2-way communication in conjunction with other mHealth features with 1 (5%) study reporting no SSOs.108
Upload biometric measurements to HCP for review and real-time feedback. This feature includes the transfer of health data directly to the HCP for review and feedback in a timely manner. Twenty-six studies included this mHealth feature in combination with other features. Four studies (15%) reported no SSOs.107,108,141,147
CDSS. The CDSS provides patient-specific feedback on biometric measurements to assist the patient with self-management.168 The patient receives relevant feedback on biometric parameters, disease specific information such as insulin or medication doses, and timely advice on when to call the HCP or go to the emergency department. The CDSS complexity varied from very basic color-coated alerts to complex insulin algorithms.147,160 Orsama and colleagues utilized only CDSS, and reported SSOs.135 Twenty additional studies combined CDSS with other features and 3 (14%) reported no SSOs.147,150,169
Frequency of features
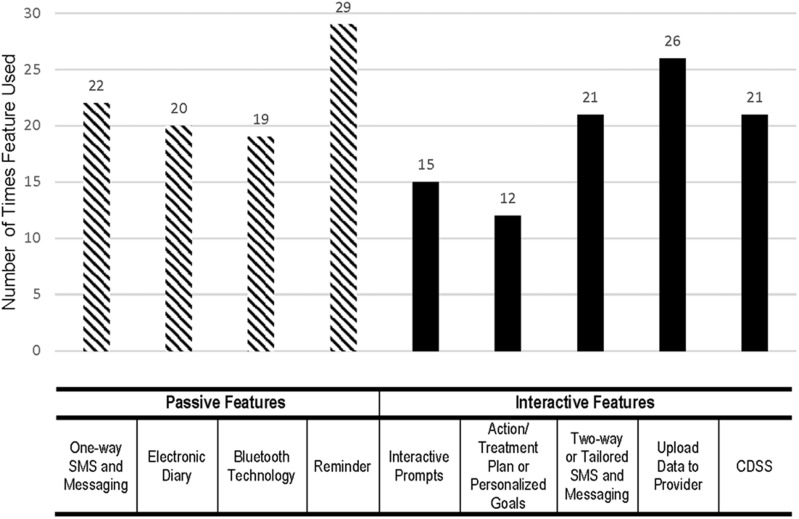
The most frequently included feature was reminders (n = 29), and the least frequent was action treatment plan/personalized health goals (n = 12). The overall average feature frequency was 20.6 times, which indicates that each feature was used in less than one-third of the studies. Researchers used interactive features slightly more frequently (51.4%) than passive features (48.6%). Figure 2 provides the frequency analysis.
Figure 2.
Frequencies of features in all studies.
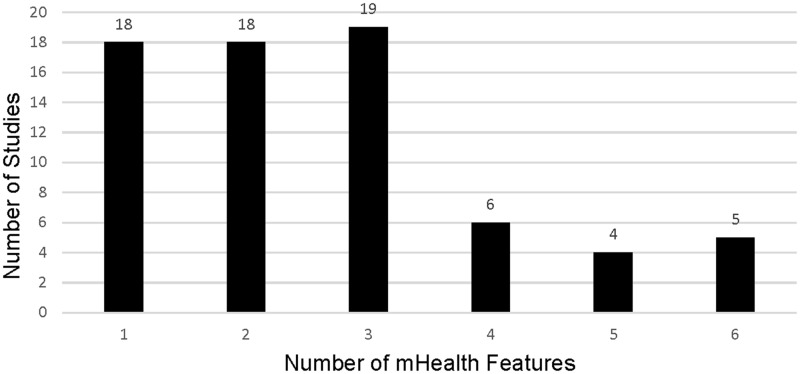
Further analysis evaluated the number of mHealth features used in each study (see Figure 3). A higher number of studies used a lower number of mHealth features. Closer examination showed 55 (79%) studies utilized 3 or fewer mHealth features.
Figure 3.
Number of features used in each study.
Analysis of mHealth categories and outcomes
An essential element of this exploration was to examine potential relationships between categories of mHealth features and SSOs (P ≤ .05). The studies were divided into 2 groups—studies with SSOs (n = 53) and studies without SSOs (n = 17).
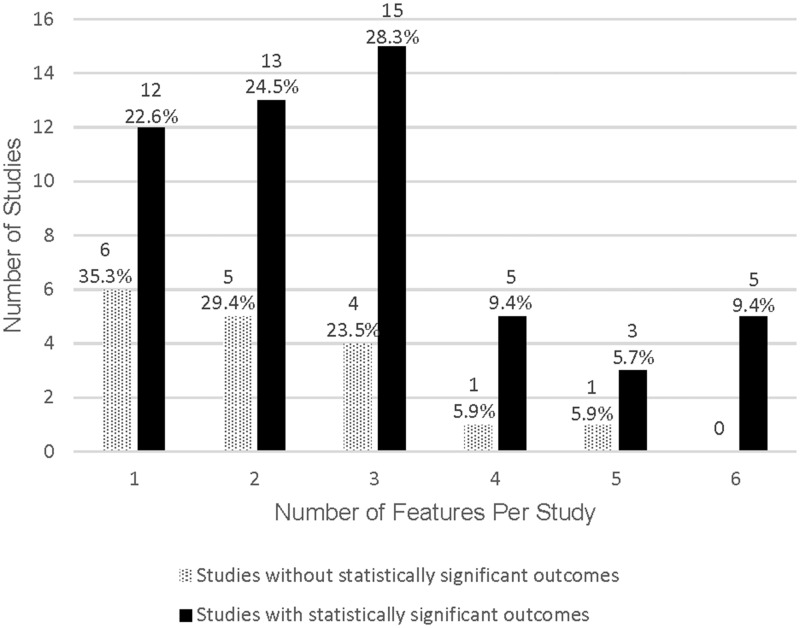
A comparison of the 2 groups revealed the studies without SSOs used a higher number of passive features (67%) than interactive features (44%). In contrast, the group with SSOs used fewer passive features (44%) and a slightly higher number of interactive features (56%). This group also used a higher number of features per study. The group with SSOs included 4 or more features in 25% of the studies compared to 12% in the group without SSOs. See Table 1 and Figure 4 for additional details.
Table 1.
Feature frequencies by outcomes
| mHealth features | Studies without significant outcomes |
Studies with significant outcomes |
||
|---|---|---|---|---|
| Number | Percentage | Number | Percentage | |
| Passive features | ||||
| One-way SMS and messaging | 7 | 18.9% | 15 | 10.1% |
| Mobile diary | 6 | 16.2% | 14 | 9.5% |
| Bluetooth technology | 7 | 18.9% | 12 | 8.1% |
| Reminder | 5 | 13.6% | 24 | 16.2% |
| Passive feature totals | 25 | 67.6% | 65 | 43.9% |
| Interactive features | ||||
| Interactive prompts | 4 | 10.8% | 11 | 7.4% |
| Action treatment plan/personalized goals | 0 | 0.0% | 12 | 8.1% |
| Two-way or tailored SMS and messaging | 1 | 2.7% | 20 | 13.5% |
| Upload data to HCP | 4 | 10.8% | 22 | 14.9% |
| CDSS | 3 | 8.1% | 18 | 12.2% |
| Interactive feature totals | 12 | 32.4% | 83 | 56.1% |
Figure 4.
Number of features per study by outcomes.
Further investigation identified the number of studies that used passive features, interactive features, or a combination of passive and interactive features (see Table 2). Studies without SSOs exclusively used passive features at a higher incident (46%) than studies with SSOs (17%). A slightly different trend was observed in studies with SSOs, which predominately used a combination of passive and interactive features (69%).
Table 2.
Comparison of studies by classification of features
| Classifications of features | Studies without significant outcomes |
Studies with significant outcomes |
||
|---|---|---|---|---|
| Number | Percentage | Number | Percentage | |
| Used only passive features | 9 | 45.5% | 8 | 16.7% |
| Used only interactive features | 3 | 18.2% | 7 | 14.6% |
| Used combination of both | 5 | 36.3% | 33 | 68.7% |
DISCUSSION
This exploration expanded on the existing mHealth literature and attempted to identify how mHealth features impact patient outcomes. Previous reviews and meta-analyses exploring the efficacy of SMS suggested that 2-way SMS was more effective than 1-way SMS.7–12 Our analysis also revealed a difference between 1-way and 2-way SMS outcomes. Overall, 68% (n = 15) of studies with 1-way SMS reported SSOs. In comparison, 95% (n = 20) of studies using 2-way SMS reported SSOs. Further comparison between studies using 1-way SMS exclusively vs studies with 1-way SMS in conjunction with other features revealed additional variances. When 1-way SMS was the exclusive feature, 58% (n = 7) of the studies reported SSOs.99,106,115,118,121,140,142 However, when used with other features, 80% (n = 8) of the studies reported SSOs.40,96,98,100,101,104,131,138 These 8 studies used 1-way SMS with at least 1 interactive feature.
Several mHealth features correlated with Michie and colleagues’ work on BCTs, such as the mobile diary—an essential element of self-monitoring.25–27 Less than one-third (n = 20) of the studies included a mobile diary. Of these 20 studies, 17 used a mobile diary with at least 1 interactive feature, and 77% (n = 13) reported SSOs.41,109,111,116,125,126,128,137,144–146,152,158
Another BCT feature is goals/planning, which allows the patient to actively participate in the health process by collaborating with the HCP to develop achievable health goals.26 These goals/plans merge the HCP’s medical expertise with the patient’s abilities and objectives. Only 12 (17%) studies included this mHealth feature in conjunction other interactive and/or passive features. All 12 (100%) reported SSOs.
Overall, the inclusion of CDSS appears to correlate with SSOs (86%). A closer examination of the 3 studies without SSOs revealed all 3 used basic color-coated CDSS. Furthermore, 2 of these studies combined the CDSS with only passive features.13,150 These studies do not provide sufficient details to explain the relationship between the CDSS complexity and passive features.
An essential element of uploading biometric measurements is real-time communication with the patient. Accessibility to timely data allows the HCP to provide feedback and judicious changes to the health regime to promote improved disease management and prevent costly hospital visits. This phenomenon was particularly evident in 2 studies.133,136 In the first study, McGillicuddy and colleagues reported the intervention group had twice the number of medication changes and successfully achieved an optimal BP compared to the control group.133 Next, Ostojic and colleagues reported the control group had >3 times the number of asthma-related hospital visits (n = 7) compared to the intervention group (n = 2).136 In contrast, 2 studies provided feedback via a written letter mailed to the patient.114,122 Both studies reported no SSOs. It is unclear why traditional mail was used rather than quick, secure mHealth communication methods (ie, SMS, e-mail), and if the delayed communication impacted the absence of SSOs.
Bluetooth technology to upload biometric measurements into the app was used in 19 studies with 63% reporting SSOs. An analysis revealed 3 studies used only passive features in combination with the Bluetooth feature.13,107,122 All 3 studies (100%) reported no SSOs. In comparison, 16 studies used Bluetooth in combination with at least 1 interactive feature, and 75% reported SSOs. No pattern between Bluetooth and the types of interactive features was identified.
Limitations
One limitation was the lack of consistency in describing mHealth features in the articles, which potentially resulted in missed interventions. The intervention description did not always include clear details of the mHealth features with some features located in the screen shots provided in the article.125 Thematic analysis allowed a methodical review of the studies with each feature recorded and analyzed to ensure all mHealth features were identified.
Another limitation was the lack of homogeneity among the studies, which restricts the generalizability of the findings. This broad examination of the mHealth literature was necessary for a thorough exploration and identification of mHealth features. Next steps will include more rigorous methods and homogenous studies to refine and confirm these initial findings.
Directions for future research
We recognize this is a first step in examining the correlation of the 9 mHealth features with outcomes. Isolating the efficacy of specific features is difficult, as 74% of the studies used 2 or more features. Therefore, we examined efficacy based on a feature’s interaction with categories of features. While these initial findings require further exploration on how the types and combination of features impact outcomes, it provides a foundation to guide a more rigorous analysis.
Additional areas for future research include the evaluation of mHealth features for other chronic health conditions and overall health and wellness (eg, weight loss, smoking cessation). Expanding the number of studies along with types of health conditions will assist in corroborating these initial findings.
As previously stated, each feature was included in approximately 20 studies, which is less than one-third of the studies with a mean of 2.6 features per app. For patients, the inclusion of only 2 or 3 features may translate into limited selection of apps with available technology to assist in self-management of chronic respiratory disease, diabetes, and HTN. For example, goals/planning, an essential element of self-management, was used in only 12 studies (17%); and the mobile diary, another self-management BCT, was included in less than one-third of studies. Furthermore, Bluetooth technology, which is widely available, was used in only 19 (27%) studies. This finding appears to correlate with prior findings that mHealth is not harnessing the available technology to assist self-monitoring and not including evidence-based self-management recommendations.5,19 Additional exploration is necessary to identify why more mHealth features are not included in apps for chronic respiratory diseases, diabetes, and HTN. Focus group discussions with mHealth developers are one option to investigate barriers to the inclusion of mHealth features.
CONCLUSION
To our knowledge, this is the first targeted exploration using thematic analysis to identify mHealth features and to specifically examine categories of mHealth features related to SSOs. Thematic analysis revealed 9 unique features separated into 2 categories—passive and interactive. Overall, each feature was included in only one-third of the studies. Studies with SSOs used a higher combination of passive and interactive features compared to studies without SSOs. This phenomenon was observed when Bluetooth, 1-way SMS, or goals/planning was combined with at least 1 interactive feature. There may be a synergist effect between specific features and types of categories.
This targeted exploration is a first step in identifying and defining features used in mHealth. We hope this exploration initiates a discussion on mHealth features that may result in universal definitions and categories to advance the adoption of mHealth to improve patient outcomes.
FUNDING
This research was supported by National Institutes of Health/National Library of Medicine F31 grant number 1 F31 LM012402-01A1 and Jonas Philanthropies.
CONTRIBUTORS
All authors contributed to the conception and development of concept, drafting, and revising of the article, and final approval of the article, and agree to be accountable for the content of the article.
Sara B. Donevant: development of concept, drafting and revising, approved final version of article, and agree to be accountable.
Joan M. Culley: development of concept, drafting and revising, approved final version of article, and agree to be accountable.
Robin D. Estrada: development of concept, drafting and revising, approved final version of article, and agree to be accountable.
Brian Habing: development of concept, drafting and revising, approved final version of article, and agree to be accountable.
Swann A. Arp: development of concept, drafting and revising, approved final version of article, and agree to be accountable.
Conflict of interest statement. None declared.
Supplementary Material
REFERENCES
- 1. Kay M. mHealth: New Horizons for Health Through Mobile Technologies [Report] 2011. http://www.who.int/goe/publications/goe_mhealth_web.pdf? ua=1. Accessed March 3, 2018.
- 2. Research2Guidance. 325, 000 Mobile Health Apps Available in 2017—Android Now the Leading mHealth Platform 2017. https://research2guidance.com/325000-mobile-health-apps-available-in-2017/. Accessed January 13, 2018.
- 3. Ricciardi L, Mostashari F, Murphy J, et al. A national action plan to support consumer engagement via e-health. Health Aff 2013; 322: 376–84. [DOI] [PubMed] [Google Scholar]
- 4. Ramirez V, Johnson E, Gonzalez C, et al. Assessing the use of mobile health technology by patients: an observational study in primary care clinics. JMIR mHealth Uhealth 2016; 42: e41..http://mhealth.jmir.org/2016/2/e41/ (accessed 2017 Apr 19). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aitken M, Lyle J.. Patient Adoption of mHealth: Use, Evidence and Remaining Barriers to Mainstream Acceptance. Parsippany, NJ: IMS Institute for Healthcare Informatics; 2015. [Google Scholar]
- 6. Monroe CM, Thompson DL, Bassett DR Jr, et al. Usability of mobile phones in physical activity–related research: a systematic review. Am J Health Educ 2015; 464: 196–206. [Google Scholar]
- 7. Free C, Phillips G, Watson L, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med 2013; 101: e1001363.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Poorman E, Gazmararian J, Parker RM, et al. Use of text messaging for maternal and infant health: a systematic review of the literature. Matern Child Health J 2015; 195: 969–89. [DOI] [PubMed] [Google Scholar]
- 9. Holcomb LS. A taxonomic integrative review of short message service (SMS) methodology: a framework for improved diabetic outcomes. J Diabetes Sci Technol 2015; 96: 1321.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wald DS, Butt S, Bestwick JP.. One-way versus two-way text messaging on improving medication adherence: meta-analysis of randomized trials. Am J Med 2015; 12810: 1139.e1–5. [DOI] [PubMed] [Google Scholar]
- 11. Vargas G, Cajita MI, Whitehouse E, et al. Use of short messaging service for hypertension management. A systematic review. J Cardiovasc Nurs 2017; 323: 260–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Orr JA, King RJ.. Mobile phone SMS messages can enhance healthy behaviour: a meta-analysis of randomised controlled trials. Health Psychol Rev 2015; 94: 397–416. [DOI] [PubMed] [Google Scholar]
- 13. Holmen H, Wahl AK, Cvancarova Smastuen M, Ribu L, Tailored communication within mobile apps for diabetes self-management: a systematic review. J Med Internet Res 2017; 196: e227.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hou C, Xu Q, Diao S, et al. Mobile phone applications and self-management of diabetes: a systematic review with meta-analysis, meta-regression of 21 randomized trials and GRADE. Diabetes Obes Metab 2018; doi:10.1111/dom.13307. [DOI] [PubMed] [Google Scholar]
- 15. Whitehead L, Seaton P.. The effectiveness of self-management mobile phone and tablet apps in long-term condition management: a systematic review. J Med Internet Res 2016; 185: e97.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang Y, Xue H, Huang Y, et al. A systematic review of application and effectiveness of mHealth interventions for obesity and diabetes treatment and self-management. Adv Nutr 2017; 83: 449–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hood M, Wilson R, Corsica J, et al. What do we know about mobile applications for diabetes self-management? A review of reviews. J Behav Med 2016; 396: 981–94. [DOI] [PubMed] [Google Scholar]
- 18. Wang J, Wang Y, Wei C, et al. Smartphone interventions for long-term health management of chronic diseases: an integrative review. Telemed J E Health 2014; 206: 570–83. [DOI] [PubMed] [Google Scholar]
- 19. Chomutare T, Fernandez-Luque L, Årsand E, et al. Features of mobile diabetes applications: review of the literature and analysis of current applications compared against evidence-based guidelines. J Med Internet Res 2011; 133: e65.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mendiola MF, Kalnicki M, Lindenauer S.. Valuable features in mobile health apps for patients and consumers: content analysis of apps and user ratings. JMIR mHealth Uhealth 2015; 32: e40.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bellei EA, Biduski D, Cechetti NP, et al. Diabetes mellitus m-Health applications: a systematic review of features and fundamentals. Telemed J E Health 2018; doi:10.1089/tmj.2017.0230. [DOI] [PubMed] [Google Scholar]
- 22. Wu Y, Yao X, Vespasiani G, et al. Mobile app-based interventions to support diabetes self-management: a systematic review of randomized controlled trials to identify functions associated with glycemic efficacy. JMIR mHealth and uHealth 2017; 53 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5373677/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sama PR, Eapen ZJ, Weinfurt KP, et al. An evaluation of mobile health application tools. JMIR mHealth Uhealth 2014; 22: e19..https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4114419/ (accessed 01 May 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stephani V, Opoku D, Quentin W.. A systematic review of randomized controlled trials of mHealth interventions against non-communicable diseases in developing countries. BMC Public Health 2016; 161: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Beck J, Greenwood DA, Blanton L, et al. 2017 National standards for diabetes self-management education and support. Diabetes Educ 2018; 441: 35.. [DOI] [PubMed] [Google Scholar]
- 26. Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013; 461: 81–95. [DOI] [PubMed] [Google Scholar]
- 27. Michie S, Wood CE, Johnston M, et al. Behaviour change techniques: the development and evaluation of a taxonomic method for reporting and describing behaviour change interventions (a suite of five studies involving consensus methods, randomised controlled trials and analysis of qualitative data). Health Technol Assess 2015; 1999: 1–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Michie S, Ashford S, Sniehotta FF, et al. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011; 2611: 1479–98. [DOI] [PubMed] [Google Scholar]
- 29. Hall AK, Cole-Lewis H, Bernhardt JM.. Mobile text messaging for health: a systematic review of reviews. Annu Rev Public Health 2015; 361: 393.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Centers for Disease Control and Prevention. Trends in Asthma Prevalence, Health Care Use and Mortality in the United States, 2001-2010 2015. http://www.cdc.gov/nchs/products/databriefs/db94.htm. Accessed June 10, 2016.
- 31. American Diabetes Association. Statistics About Diabetes 2016. http://www.diabetes.org/diabetes-basics/statistics/. Accessed June 10, 2016.
- 32. Centers for Disease Control and Prevention. Health Expenditures 2015. http://www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed March 3, 2018.
- 33. American Thoracic Society. Asthma Costs the U.S. Economy More Than $80 Billion per Year 2018. https://www.thoracic.org/about/newsroom/press-releases/journal/asthma-costs-the-us-economy-more-than-80-billion-per-year.php. Accessed April 4, 2018.
- 34. Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996–2013. JAMA 2016; 31624: 2627–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Song Y, Liu X, Zhu X, et al. Increasing trend of diabetes combined with hypertension or hypercholesterolemia: NHANES data analysis 1999–2012. Sci Rep 2016; 61 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5090961/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vollmer Dahlke D, Fair K, Hong YA, et al. Apps seeking theories: results of a study on the use of health behavior change theories in cancer survivorship mobile apps. JMIR mHealth Uhealth 2015; 31: e31.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Clarke V, Braun V.. Thematic Analysis. Encyclopedia of Critical Psychology. New York, NY: Springer; 2014: 1947–52. [Google Scholar]
- 38. Braun V, Clarke V, Terry G. Thematic analysis. In: Cooper H, Camic PM, Long DL, Panter AT, Rindskopf D, Sher KJ, eds. APA handbook of research methods in psychology. Vol 2. Washington, D.C.: American Psychological Association; 2012:57–71. [Google Scholar]
- 39. Wallach JD, Sullivan PG, Trepanowski JF, et al. Evaluation of evidence of statistical support and corroboration of subgroup claims in randomized clinical trials. JAMA Intern Med 2017; 1774 https://jamanetwork-com.pallas2.tcl.sc.edu/journals/jamainternalmedicine/fullarticle/2601419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Franklin VL, Waller A, Pagliari C, et al. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabetic Med 2006; 2312: 1332–8. [DOI] [PubMed] [Google Scholar]
- 41. Charpentier G, Benhamou P-Y, Dardari D, et al. The Diabeo software enabling individualized insulin dose adjustments combined with telemedicine support improves HbA1c in poorly controlled type 1 diabetic patients: a 6-month, randomized, open-label, parallel-group, multicenter trial (TeleDiab 1 study). Diabetes Care 2011; 343: 533–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Appschopper Blog. History-mystery of mobile applications development revealed here [Blog post]. Apps Chopper. New York, NY: AppsChopper; 2012. [Google Scholar]
- 43. MelonMobile. History of mobile apps through the eyes of advanced call manager, an eyewitness [Blog post]. Melon Mobile's Blog Sofia, Bulgaria: Melon Mobile; 2013. [Google Scholar]
- 44. Aitken M, Gauntlett C.. Patient Apps for Improved Healthcare from Novelty to Mainstream IMS Institute for Healthcare Informatics: IMS Institute for Healthcare Informatics; 2013.
- 45. Aikens JE, Zivin K, Trivedi R, et al. Diabetes self-management support using mHealth and enhanced informal caregiving. J Diabetes Complicat 2014; 282: 171–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Baron JS, Hirani S, Newman SP.. A randomised, controlled trial of the effects of a mobile telehealth intervention on clinical and patient-reported outcomes in people with poorly controlled diabetes. J Telemed Telecare 2017; 232: 207–16. [DOI] [PubMed] [Google Scholar]
- 47. Block G, Azar KM, Romanelli RJ, et al. Diabetes prevention and weight loss with a fully automated behavioral intervention by email, web, and mobile phone: a randomized controlled trial among persons with prediabetes. J Med Internet Res 2015; 1710: e240–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bloss CS, Wineinger NE, Peters M, et al. A prospective randomized trial examining health care utilization in individuals using multiple smartphone-enabled biosensors. Peer J 2016; 4: e1554.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Cho JH, Choi YH, Kim HS, et al. Effectiveness and safety of a glucose data-filtering system with automatic response software to reduce the physician workload in managing type 2 diabetes. J Telemed Telecare 2011; 175: 257–62. [DOI] [PubMed] [Google Scholar]
- 50. Drion I, Pameijer LR, van Dijk PR, et al. The effects of a mobile phone application on quality of life in patients with type 1 diabetes mellitus: a randomized controlled trial. J Diabetes Sci Technol 2015; 95: 1086–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Durso SC, Wendel I, Letzt AM, et al. Older adults using cellular telephones for diabetes management: a pilot study. Medsurg Nurs 2003; 125: 313–7. [PubMed] [Google Scholar]
- 52. Fukuoka Y, Gay CL, Joiner KL, et al. A novel diabetes prevention intervention using a mobile app: a randomized controlled trial with overweight adults at risk. Am J Prev Med 2015; 492: 223–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kim HS. A randomized controlled trial of a nurse short-message service by cellular phone for people with diabetes. Int J Nurs Stud 2007; 445: 687–92. [DOI] [PubMed] [Google Scholar]
- 54. Kim HS, Jeong HS.. A nurse short message service by cellular phone in type-2 diabetic patients for six months. J Clin Nurs 2007; 166: 1082–7. [DOI] [PubMed] [Google Scholar]
- 55. Limaye T, Kumaran K, Joglekar C, et al. Efficacy of a virtual assistance-based lifestyle intervention in reducing risk factors for type 2 diabetes in young employees in the information technology industry in India: LIMIT, a randomized controlled trial. Diabet Med 2017; 344: 563–8. [DOI] [PubMed] [Google Scholar]
- 56. Hanauer DA, Wentzell K, Laffel N, et al. Computerized automated reminder diabetes system (CARDS): e-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes. Technol Ther 2009; 112: 99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hsu WC, Lau KH, Huang R, et al. Utilization of a cloud-based diabetes management program for insulin initiation and titration enables collaborative decision making between healthcare providers and patients. Diabetes Technol Ther 2016; 182: 59–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Huang JS, Terrones L, Tompane T, et al. Preparing adolescents with chronic disease for transition to adult care: a technology program. Pediatrics 2014; 1336: e1639–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kollmann A, Riedl M, Kastner P, et al. Feasibility of a mobile phone-based data service for functional insulin treatment of type 1 diabetes mellitus patients. J Med Internet Res 2007; 95: e36. (accessed 31 Dec 2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lim S, Kang S, Kim K, et al. Multifactorial intervention in diabetes care using real-time monitoring and tailored feedback in type 2 diabetes. Acta Diabetol 2016; 532: 189–98. [DOI] [PubMed] [Google Scholar]
- 61. Levy N, Moynihan V, Nilo A, et al. The mobile insulin titration intervention (MITI) for insulin adjustment in an urban, low-income population: randomized controlled trial. J Med Internet Res 2015; 177: e180.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Mulvaney SA, Anders S, Smith AK, et al. A pilot test of a tailored mobile and web-based diabetes messaging system for adolescents. J Telemed Telecare 2012; 182: 115–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Naghibi SA, Moosazadeh M, Zhyanifard A, et al. Analyzing short message services application effect on diabetic patients' self-caring. Int J Prev Med 2015; 6.www.ijpvmjournal.net/article.asp? issn=2008-7802; year=2015; volume=6; issue=1; spage=75; epage=75; aulast=Naghibi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Patnaik L, Joshi A, Sahu T.. Mobile phone-based education and counseling to reduce stress among patients with diabetes mellitus attending a tertiary care hospital of India. Int J Prev Med 2015; 61: 37.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Patrick K, Norman GJ, Davila EP, et al. Outcomes of a 12-month technology-based intervention to promote weight loss in adolescents at risk for type 2 diabetes. J Diabetes Sci Technol 2013; 73: 759–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Quinn CC, Clough SS, Minor JM, et al. WellDoc™ mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther 2008; 103: 160–8. [DOI] [PubMed] [Google Scholar]
- 67. Quinn CC, Shardell MD, Terrin ML, et al. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care 2011; 1–9. doi:10.2337/dc11-0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Quinn CC, Khokhar B, Weed K, et al. Older adult self-efficacy study of mobile phone diabetes management. Diabetes Technol Ther 2015; 177: 455–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Quinn CC, Shardell MD, Terrin ML, et al. Mobile diabetes intervention for glycemic control in 45- to 64-year-old persons with type 2 diabetes. J Appl Gerontol 2016; 352: 227–43. [DOI] [PubMed] [Google Scholar]
- 70. Rami B, Popow C, Horn W, et al. Telemedical support to improve glycemic control in adolescents with type 1 diabetes mellitus. Eur J Pediatr 2006; 16510: 701–5. [DOI] [PubMed] [Google Scholar]
- 71. Schreier G, Eckmann H, Hayn D, et al. Web versus app - compliance of patients in a telehealth diabetes management programme using two different technologies. J Telemed Telecare 2012; 188: 476–80. [DOI] [PubMed] [Google Scholar]
- 72. Seid M, D'Amico EJ, Varni JW, et al. The in vivo adherence intervention for at risk adolescents with asthma: report of a randomized pilot trial. J Pediatr Psychol 2012; 374: 390–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Takenga C, Berndt RD, Musongya O, et al. An ICT-based diabetes management system tested for health care delivery in the African context. Int J Telemed Appl 2014; 2014: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Vähätalo M, Virtamo H, Viikari J, et al. Cellular phone transferred self blood glucose monitoring: prerequisites for positive outcome. Pract Diab Int 2004; 215: 192–4. [Google Scholar]
- 75. Yoon KH, Kim HS.. A short message service by cellular phone in type 2 diabetic patients for 12 months. Diabetes Res Clin Pract 2008; 792: 256–61. [DOI] [PubMed] [Google Scholar]
- 76. Bain TM, Jones ML, O’Brian CA, et al. Feasibility of smartphone-delivered diabetes self-management education and training in an underserved urban population of adults. J Telemed Telecare 2015; 211: 58–60. [DOI] [PubMed] [Google Scholar]
- 77. Burbank AJ, Lewis SD, Hewes M, et al. Mobile-based asthma action plans for adolescents. J Asthma 2015; 526: 583–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Ferrer-Roca O, Cárdenas A, Diaz-Cardama A, et al. Mobile phone text messaging in the management of diabetes. J Telemed Telecare 2004; 105: 282–5. [DOI] [PubMed] [Google Scholar]
- 79. Holtz B, Whitten P.. Managing asthma with mobile phones: a feasibility study. Telemed J E Health 2009; 159: 907–9. [DOI] [PubMed] [Google Scholar]
- 80. Meltzer EO, Kelley N, Hovell MF.. Randomized, cross-over evaluation of mobile phone vs paper diary in subjects with mild to moderate persistent asthma. Open Respir Med J 2008; 2.https://www-ncbi-nlm-nih-gov.pallas2.tcl.sc.edu/pmc/articles/PMC2606655/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Stuckey M, Fulkerson R, Read E, et al. Remote monitoring technologies for the prevention of metabolic syndrome: the diabetes and technology for increased activity (DaTA) study. J Diabetes Sci Technol 2011; 54: 936–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Schiel R, Thomas A, Kaps A, et al. An innovative telemedical support system to measure physical activity in children and adolescents with type 1 diabetes mellitus. Exp Clin Endocrinol Diabetes 2011; 11909: 565. [DOI] [PubMed] [Google Scholar]
- 83. Doocy S, Paik KE, Lyles E, et al. Guidelines and mHealth to improve quality of hypertension and type 2 diabetes care for vulnerable populations in Lebanon: longitudinal cohort study. JMIR mHealth Uhealth 2017; 510: e158.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Kleinman NJ, Shah A, Shah S, et al. Impact of the gather mHealth system on A1C: primary results of a multisite randomized clinical trial among people with type 2 diabetes in India. Diabetes Care 2016; 3910: e169.. [DOI] [PubMed] [Google Scholar]
- 85. Torbjornsen A, Jenum AK, Smastuen MC, et al. A low-intensity mobile health intervention with and without health counseling for persons with type 2 diabetes, part 1: baseline and short-term results from a randomized controlled trial in the Norwegian part of RENEWING HEALTH. JMIR mHealth Uhealth 2014; 24: e52.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Zolfaghari M, Mousavifar SA, Pedram S, et al. The impact of nurse short message services and telephone follow‐ups on diabetic adherence: which one is more effective? J Clin Nurs 2012; 21 (13–14): 1922–31. [DOI] [PubMed] [Google Scholar]
- 87. Faridi Z, Liberti L, Shuval K, et al. Evaluating the impact of mobile telephone technology on type 2 diabetic patients' self-management: the NICHE pilot study. J Eval Clin Pract 2008; 143: 465–9. [DOI] [PubMed] [Google Scholar]
- 88. Goodarzi M, Ebrahimzadeh I, Rabi A, et al. Impact of distance education via mobile phone text messaging on knowledge, attitude, practice and self efficacy of patients with type 2 diabetes mellitus in Iran. J Diabetes Metab Disord 2012; 111: 10.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Kim MY, Lee SY, Jo EJ, et al. Feasibility of a smartphone application based action plan and monitoring in asthma. Asia Pac Allergy 2016; 63: 174.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Katz R, Mesfin T, Barr K.. Lessons from a community-based mHealth diabetes self-management program: “It's not just about the cell phone. J Health Commun 2012; 17 (sup1): 67–72. [Google Scholar]
- 91. Louch G, Dalkin S, Bodansky J, et al. An exploratory randomised controlled trial using short messaging service to facilitate insulin administration in young adults with type 1 diabetes. Psychol Health Med 2013; 182: 166.. [DOI] [PubMed] [Google Scholar]
- 92. Markowitz JT, Cousineau T, Franko DL, et al. Text messaging intervention for teens and young adults with diabetes. J Diabetes Sci Technol 2014; 85: 1029.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Waki K, Aizawa K, Kato S, et al. DialBetics with a multimedia food recording tool, foodlog: smartphone-based self-management for type 2 diabetes. J Diabetes Sci Technol 2015; 93: 534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Nundy S, Dick JJ, Chia-Hung C, et al. Mobile phone diabetes project led to improved glycemic control and net savings for Chicago plan participants. Health Aff 2014; 332: 265–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Nundy S, Mishra A, Hogan P, et al. How do mobile phone diabetes programs drive behavior change?: evidence from a mixed methods observational cohort study. Diabetes Educ 2014; 406: 806–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Abaza H, Marschollek M.. SMS education for the promotion of diabetes self-management in low & middle income countries: a pilot randomized controlled trial in Egypt. BMC Public Health 2017; 171: 962.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Bell AM, Fonda SJ, Walker MS, et al. Mobile phone-based video messages for diabetes self-care support. J Diabetes Sci Technol 2012; 62: 310.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Benhamou PY, Melki V, Boizel R, et al. One-year efficacy and safety of web-based follow-up using cellular phone in type 1 diabetic patients under insulin pump therapy: the PumpNet study. Diabetes Metab 2007; 333: 220–6. [DOI] [PubMed] [Google Scholar]
- 99. Bin Abbas B, Al Fares A, Jabbari M, et al. Effect of mobile phone short text messages on glycemic control in type 2 diabetes. Int J Endocrinol Metab 2014; 131 https://www-ncbi-nlm-nih-gov.pallas2.tcl.sc.edu/pmc/articles/PMC4338653/pdf/ijem-13-01-18791.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Bin-Abbas B, Jabbari M, Al-Fares A, et al. Effect of mobile phone short text messages on glycaemic control in children with type 1 diabetes. J Telemed Telecare 2014; 203: 153–6. [DOI] [PubMed] [Google Scholar]
- 101. Bobrow K, Farmer AJ, Springer D, et al. Mobile phone text messages to support treatment adherence in adults with high blood pressure (SMS-text adherence support [StAR]): a single-blind, randomized trial. Circulation 2016; 1336 http://circ.ahajournals.org.pallas2.tcl.sc.edu/content/133/6/592.long. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Brar Prayaga R, Jeong EW, Feger E, et al. Improving refill adherence in Medicare patients with tailored and interactive mobile text messaging: pilot study. JMIR mHealth Uhealth 2018; 61: e30.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Brath H, Morak J, Kastenbauer T, et al. Mobile health (mHealth) based medication adherence measurement - a pilot trial using electronic blisters in diabetes patients. Br J Clin Pharmacol 2013; 76: 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Burner E, Lam CN, DeRoss R, et al. Using mobile health to improve social support for low-income Latino patients with diabetes: a mixed-methods analysis of the feasibility trial of TExT-MED + FANS. Diabetes. Technol Ther 2018; 201: 39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Capozza K, Woolsey S, Georgsson M, et al. Going mobile with diabetes support: a randomized study of a text message-based personalized behavioral intervention for type 2 diabetes self-sare. Diabetes Spectr 2015; 282: 83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Celik S, Cosansu G, Erdogan S, et al. Using mobile phone text messages to improve insulin injection technique and glycaemic control in patients with diabetes mellitus: a multi-centre study in Turkey. J Clin Nurs 2015; 24 (11–12): 1525–33. [DOI] [PubMed] [Google Scholar]
- 107. Chau JP-C, Lee DT-F, Yu DS-F, et al. A feasibility study to investigate the acceptability and potential effectiveness of a telecare service for older people with chronic obstructive pulmonary disease. Int J Med Inform 2012; 8110: 674–82. [DOI] [PubMed] [Google Scholar]
- 108. Cho JH, Lee HC, Lim DJ, et al. Mobile communication using a mobile phone with a glucometer for glucose control in type 2 patients with diabetes: as effective as an Internet-based glucose monitoring system. J Telemed Telecare 2009; 152: 77–82. [DOI] [PubMed] [Google Scholar]
- 109. Cingi C, Yorgancioglu A, Cingi CC, et al. The “physician on call patient engagement trial” (POPET): measuring the impact of a mobile patient engagement application on health outcomes and quality of life in allergic rhinitis and asthma patients. Int Forum Allergy Rhinol 2015; 56: 487.. [DOI] [PubMed] [Google Scholar]
- 110. Clements MA, Staggs VS.. A mobile app for synchronizing glucometer data: Impact on adherence and glycemic control among youths with type 1 diabetes in routine care. J Diabetes Sci Technol 2017; 113: 461–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Cook KA, Modena BD, Simon RA.. Improvement in asthma control using a minimally burdensome and proactive smartphone application. J Allergy Clin Immunol Pract 2016; 44: 730–7.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Ding H, Karunanithi M, Kanagasingam Y, et al. A pilot study of a mobile-phone-based home monitoring system to assist in remote interventions in cases of acute exacerbation of COPD. J Telemed Telecare 2014; 203: 128–34. [DOI] [PubMed] [Google Scholar]
- 113. Dobson R, Carter K, Cutfield R, et al. Diabetes text-message self-management support program (SMS4BG): a pilot study. JMIR mHealth Uhealth 2015; 31: e32..http://mhealth.jmir.org/2015/1/e32/ (accessed 2 Jan 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Earle KA, Istepanian RS, Zitouni K, et al. Mobile telemonitoring for achieving tighter targets of blood pressure control in patients with complicated diabetes: a pilot study. Diabetes Technol Ther 2010; 127: 575–9. [DOI] [PubMed] [Google Scholar]
- 115. Fatehi F, Malekzadeh G, Akhavimirab A, et al. The effect of short message service on knowledge of patients with diabetes in Yazd, Iran. IJDO 2010; 21: 27–31. [Google Scholar]
- 116. Garg SK, Shah VN, Akturk HK, et al. Role of mobile technology to improve diabetes care in adults with type 1 diabetes: the remote-T1D study iBGStar® in type 1 diabetes management. Diabetes Ther 2017; 84: 811–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Gatwood J, Balkrishnan R, Erickson SR, et al. The impact of tailored text messages on health beliefs and medication adherence in adults with diabetes: a randomized pilot study. Res Social Adm Pharm 2016; 121: 130–40. [DOI] [PubMed] [Google Scholar]
- 118. Haddad NS, Istepanian R, Philip N, et al. A feasibility study of mobile phone text messaging to support education and management of type 2 diabetes in Iraq. Diabetes. Technol Ther 2014; 167: 454–9. [DOI] [PubMed] [Google Scholar]
- 119. Han Y, Faulkner MS, Fritz H, et al. A pilot randomized trial of text-messaging for symptom awareness and diabetes knowledge in adolescents with type 1 diabetes. J Pediatr Nurs 2015; 306: 850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Hussein WI, Hasan K, Jaradat AA.. Effectiveness of mobile phone short message service on diabetes mellitus management: the SMS-DM study. Diabetes Res Clin Pract 2011; 941: e24.. [DOI] [PubMed] [Google Scholar]
- 121. Shariful Islam MS, Niessen LW, Ferrari U, et al. Effects of mobile phone SMS to improve glycemic control among patients with type 2 diabetes in Bangladesh: a prospective, parallel-group, randomized controlled trial. Dia Care 2015; 388: e112.. [DOI] [PubMed] [Google Scholar]
- 122. Istepanian RS, Zitouni K, Harry D, et al. Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. J Telemed Telecare 2009; 153: 125–8. [DOI] [PubMed] [Google Scholar]
- 123. Kerr DA, Harray AJ, Pollard CM, et al. The connecting health and technology study: a 6-month randomized controlled trial to improve nutrition behaviours using a mobile food record and text messaging support in young adults. Int J Behav Nutr Phys Act 2016; 131: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Kim C, Park S, Kang J, et al. Insulin dose titration system in diabetes patients using a short messaging service automatically produced by a knowledge matrix. Diabetes. Technol Ther 2010; 128: 663–9. [DOI] [PubMed] [Google Scholar]
- 125. Kirwan M, Vandelanotte C, Fenning A, et al. Diabetes self-management smartphone application for adults with type 1 diabetes: randomized controlled trial. J Med Internet Res 2013; 1511: e235.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Larsen ME, Turner J, Farmer A, et al. Telemedicine-supported insulin optimisation in primary care. J Telemed Telecare 2010; 168: 433–40. [DOI] [PubMed] [Google Scholar]
- 127. Lim S, Kang SM, Shin H, et al. Improved glycemic control without hypoglycemia in elderly diabetic patients using the ubiquitous healthcare service, a new medical information system. Diabetes Care 2011; 342: 308.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Liu WT, Huang CD, Wang CH, et al. A mobile telephone-based interactive self-care system improves asthma control. Eur Respir J 2011; 372: 310.. [DOI] [PubMed] [Google Scholar]
- 129. Liu WT, Wang CH, Lin HC, et al. Efficacy of a cell phone-based exercise programme for COPD. Eur Respir J 2008; 323: 651.. [DOI] [PubMed] [Google Scholar]
- 130. Logan AG, Irvine MJ, McIsaac WJ, et al. Effect of home blood pressure telemonitoring with self-care support on uncontrolled systolic hypertension in diabetics. Hypertension 2012; 601: 51–7. [DOI] [PubMed] [Google Scholar]
- 131. Lv Y, Zhao H, Liang Z, et al. A mobile phone short message service improves perceived control of asthma: a randomized controlled trial. Telemed J E Health 2012; 186: 420.. [DOI] [PubMed] [Google Scholar]
- 132. Marquez Contreras E, de la Fiuera von Wichmann M, Gil Guillen V, et al. Effectiveness of an intervention to provide information to patients with hypertension as short text messages of reminders sent to their mobile phone (HTA-Alert). Aten Primaria 2004; 348: 399–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. McGillicuddy JW, Gregoski MJ, Weiland AK, et al. Mobile health medication adherence and blood pressure control in renal transplant recipients: a proof-of-concept randomized controlled trial. JMIR Res Protoc 2013; 22: e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Offringa R, Sheng T, Parks L, et al. Digital diabetes management application improves glycemic outcomes in people with type 1 and type 2 diabetes. J Diabetes Sci Technol 2017; doi:10.1177/1932296817747291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Orsama AL, Lahteenmaki J, Harno K, et al. Active assistance technology reduces glycosylated hemoglobin and weight in individuals with type 2 diabetes: results of a theory-based randomized trial. Diabetes Technol Ther 2013; 158: 662–9. [DOI] [PubMed] [Google Scholar]
- 136. Ostojic V, Cvoriscec B, Ostojic SB, et al. Improving asthma control through telemedicine: a study of short-message service. Telemed J E. Health 2005; 111: 28–35. [DOI] [PubMed] [Google Scholar]
- 137. Patel S, Jacobus-Kantor L, Marshall L, et al. Mobilizing your medications: an automated medication reminder application for mobile phones and hypertension medication adherence in a high-risk urban population. J Diabetes Sci Technol 2013; 73: 630.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Peimani M, Rambod C, Omidvar M, et al. Effectiveness of short message service-based intervention (SMS) on self-care in type 2 diabetes: a feasibility study. Prim Care Diabetes 2016; 104: 251.. [DOI] [PubMed] [Google Scholar]
- 139. Petrie KJ, Perry K, Broadbent E, et al. A text message programme designed to modify patients' illness and treatment beliefs improves self-reported adherence to asthma preventer medication. Br J Health Psychol 2012; 171: 74–84. [DOI] [PubMed] [Google Scholar]
- 140. Pfammatter A, Spring B, Saligram N, et al. mHealth intervention to mprove diabetes risk behaviors in India: a prospective, parallel group cohort study. J Med Internet Res 2016; 188: e207..www.jmir.org/2016/8/e207/ (accessed 5 Aug 2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Prabhakaran L, Chee WY, Chua KC, et al. The use of text messaging to improve asthma control: a pilot study using the mobile phone short messaging service (SMS). J Telemed Telecare 2010; 165: 286–90. [DOI] [PubMed] [Google Scholar]
- 142. Ramachandran A, Snehalatha C, Ram J, et al. Effectiveness of mobile phone messaging in prevention of type 2 diabetes by lifestyle modification in men in India: a prospective, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol 2013; 13: 191. [DOI] [PubMed] [Google Scholar]
- 143. Read E. Feasibility of the diabetes and technology for increased activity (DaTA) study: a pilot intervention in high-risk rural adults. J Phys Act Health 2014; 111: 118.. [DOI] [PubMed] [Google Scholar]
- 144. Rossi MC, Nicolucci A, Pellegrini F, et al. Interactive diary for diabetes: a useful and easy-to-use new telemedicine system to support the decision-making process in type 1 diabetes. Diabetes Technol Ther 2009; 111: 19–24. [DOI] [PubMed] [Google Scholar]
- 145. Rossi MC, Nicolucci A, Lucisano G, et al. Impact of the “Diabetes Interactive Diary” telemedicine system on metabolic control, risk of hypoglycemia, and quality of life: a randomized clinical trial in type 1 diabetes. Diabetes Technol Ther 2013; 158: 670–9. [DOI] [PubMed] [Google Scholar]
- 146. Rossi MC, Nicolucci A, Di Bartolo P, et al. Diabetes interactive diary: a new telemedicine system enabling flexible diet and insulin therapy while improving quality of life. Diabetes Care 2010; 331: 109–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Ryan D, Price D, Musgrave SD, et al. Clinical and cost effectiveness of mobile phone supported self monitoring of asthma: multicentre randomised controlled trial. BMJ 2012; 344 (mar23 1): e1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Ryan EA, Holland J, Stroulia E, et al. Improved A1C levels in type 1 diabetes with smartphone app use. Can J Diabetes 2017; 411: 33–40. [DOI] [PubMed] [Google Scholar]
- 149. Shetty AS, Chamukuttan S, Nanditha A, et al. Reinforcement of adherence to prescription recommendations in Asian Indian diabetes patients using short message service (SMS)—a pilot study. J Assoc Physicians India 2011; 59: 711–4. [PubMed] [Google Scholar]
- 150. Skrovseth SO, Arsand E, Godtliebsen F, et al. Data-driven personalized feedback to patients with type 1 diabetes: a randomized trial. Diabetes. Technol Ther 2015; 177: 482–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Strandbygaard U, Thomsen SF, Backer V.. A daily SMS reminder increases adherence to asthma treatment: a three-month follow-up study. Respir Med 2010; 1042: 166–71. [DOI] [PubMed] [Google Scholar]
- 152. Stuckey M, Russell-Minda E, Read E, et al. Diabetes and technology for increased activity (DaTA) study: results of a remote monitoring intervention for prevention of metabolic syndrome. J Diabetes Sci Technol 2011; 54: 928.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Tasker AP, Gibson L, Franklin V, et al. What is the frequency of symptomatic mild hypoglycemia in type 1 diabetes in the young? Assessment by novel mobile phone technology and computer‐based interviewing. Pediatr Diabetes 2007; 81: 15–20. [DOI] [PubMed] [Google Scholar]
- 154. Van Olmen J, Kegels G, Korachais C, et al. The effect of text message support on diabetes self-management in developing countries - a randomised trial. J Clin Transl Endocrinol 2017; 7: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Vervloet M, van Dijk L, de Bakker DH, et al. Short- and long-term effects of real-time medication monitoring with short message service (SMS) reminders for missed doses on the refill adherence of people with type 2 diabetes: evidence from a randomized controlled trial. Diabet Med 2014; 317: 821.. [DOI] [PubMed] [Google Scholar]
- 156. Vervloet M, van Dijk L, Santen-Reestman J, et al. SMS reminders improve adherence to oral medication in type 2 diabetes patients who are real time electronically monitored. Int J Med Infom 2012; 819: 594. [DOI] [PubMed] [Google Scholar]
- 157. Waki K, Fujita H, Uchimura Y, et al. DialBetics: a novel smartphone-based self-management support system for type 2 diabetes patients. J Diabetes Sci Technol 2014; 82. doi:10.1177/1932296814526495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Wayne N, Perez DF, Kaplan DM, et al. Health coaching reduces HbA1c in type 2 diabetic patients from a lower-socioeconomic status community: a randomized controlled trial. J Med Internet Res 2015; 1710: e224.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Wong CK, Fung CS, Siu SC, et al. A short message service (SMS) intervention to prevent diabetes in Chinese professional drivers with pre-diabetes: a pilot single-blinded randomized controlled trial. Diabetes Res Clin Pract 2013; 1023: 158.. [DOI] [PubMed] [Google Scholar]
- 160. Yoo HJ, Park MS, Kim TN, et al. A ubiquitous chronic disease care system using cellular phones and the Internet. Diabet Med 2009; 266: 628–35. [DOI] [PubMed] [Google Scholar]
- 161. Zhou W, Chen M, Yuan J, et al. Welltang—a smart phone-based diabetes management application—improves blood glucose control in Chinese people with diabetes. Diabetes Res Clin Pract 2016; 116: 105. [DOI] [PubMed] [Google Scholar]
- 162. Montague E, Xu J.. Understanding active and passive users: the effects of an active user using normal, hard and unreliable technologies on user assessment of trust in technology and co-user. Appl Ergon 2012; 434: 702–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Coyle JR, Thorson E.. The effects of progressive levels of interactivity and vividness in web marketing sites. J Advert 2001; 303: 65–77. [Google Scholar]
- 164. Chiang N, Guo M, Amico KR, et al. Interactive two-way mHealth interventions for improving medication adherence: an evaluation using the behaviour change wheel framework. JMIR mHealth Uhealth 2018; 64: e87.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Michie S, van Stralen MM, West R.. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Sci 2011; 61: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Monkman H, Kushniruk A. A health literacy and usability heuristic evaluation of a mobile consumer health application. Stud Health Technol Inform2013; doi:10.3233/978-1-61499-289-9-724. [PubMed]
- 167. Department of Homeland Security. Understanding Bluetooth Technology 2016. https://www.us-cert.gov/ncas/tips/ST05-015. Accessed February 26, 2018).
- 168. HealthIT.gov. Clinical Decision Support 2013. https://www.healthit.gov/policy-researchers-implementers/clinical-decision-support-cds. Accessed February 25, 2018.
- 169. Holmen H, Wahl A, Torbjørnsen A, et al. Stages of change for physical activity and dietary habits in persons with type 2 diabetes included in a mobile health intervention: the Norwegian study in RENEWING HEALTH. BMJ Open Diab Res Care 2016; 41: e000193. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.