Abstract
Background
Although Tai Ji Quan has been shown to relieve pain and improve functional mobility in people with knee osteoarthritis (OA), little is known about its potential benefits on gait characteristics among older Chinese women who have a high prevalence of both radiographic and symptomatic knee OA. This study aims to assess the efficacy of a tailored Tai Ji Quan intervention on gait kinematics for older Chinese women with knee OA.
Methods
A randomized controlled trial involving 46 older women in Shanghai, China, with clinically diagnosed knee OA. Randomized (1:1) participants received either a 60 min Tai Ji Quan session (n = 23) 3 times weekly or a 60 min bi-weekly educational session (n = 23) for 24 weeks. Primary outcomes were changes in gait kinematic measures from baseline to 24 weeks. Secondary outcomes included changes in scores on the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) and Short Physical Performance Battery (SPPB).
Results
After 24 weeks the Tai Ji Quan group demonstrated better performance in gait velocity (mean difference, 8.40 cm/s, p = 0.01), step length (mean difference, 3.52 cm, p = 0.004), initial contact angle (mean difference, 2.19°, p = 0.01), and maximal angle (mean difference, 2.61°, p = 0.003) of flexed knees during stance phase compared to the control group. In addition, the Tai Ji Quan group showed significant improvement in WOMAC scores (p < 0.01) (mean difference, −4.22 points in pain, p = 0.002; −2.41 points in stiffness, p < 0.001; −11.04 points in physical function, p = 0.006) and SPPB scores (mean difference, 1.22 points, p < 0.001).
Conclusion
Among older Chinese women with knee OA, a tailored Tai Ji Quan intervention improved gait outcomes. The intervention also improved overall function as indexed by the WOMAC and SPPB. These results support the use of Tai Ji Quan for older Chinese adults with knee OA to both improve their functional mobility and reduce pain symptomatology.
Keywords: Gait, Pain, Physical function, Rheumatic diseases, Tai Chi Quan
1. Introduction
The incidence of knee osteoarthritis (OA), an articular pathology, increases with age,1 with older adults being the most frequently affected. In China, epidemiological studies have shown a high prevalence of knee OA among middle-aged and older Chinese.2, 3, 4, 5 For example, a cross-sectional study in Beijing indicated that 15% of women and 5.6% of men aged 60 years and over had symptomatic knee OA.2 The study further showed that when compared with Caucasian women of the same age living in the US (i.e., from Framingham, MA), older women in Beijing had a roughly 50% higher prevalence of both radiographic and symptomatic knee OA and a twofold higher prevalence of bilateral cases.2, 3 From a global public health perspective, knee OA is considered a major cause of chronic disability, particularly for older adults who often experience deterioration in physical function, thereby impacting their quality of life and requiring medical treatments that add significant costs to the healthcare system.6, 7
Exercise, which has been shown to help alleviate symptoms and improve physical function,8 is recommended in all clinical guidelines9, 10, 11, 12 as a non-pharmacological approach for managing and treating knee OA. However, many forms of physical activity are either very intense or highly monotonous, making them difficult to implement and maintain in practice. One approach that does not have these disadvantages is Tai Ji Quan (also known as Tai Chi Chuan and Tai Chi). This traditional Chinese practice has long been used to cultivate and nurture physical and mental well-being, prevent chronic disease progression, and enhance fitness.13 Research increasingly shows that many OA signs and symptoms, such as reduced joint mobility, poor balance, pain, increased joint stiffness, and limited physical function, can be ameliorated by Tai Ji Quan training.5, 14, 15, 16, 17, 18, 19, 20 The accumulating evidence has led the American College of Rheumatology to recommend Tai Ji Quan as a treatment option for patients with knee OA.12
Due to the degradation of the knee joint, people with knee OA exhibit gait impairments such as reduced walking speed, shorter step length, and decreased knee-joint motion,21, 22, 23, 24 characteristics that could have a significant impact on their ability to perform routine daily activities. Previous randomized controlled trials (RCTs), however, have rarely utilized objective measures to quantify changes in gait characteristics18, 19 following Tai Ji Quan training. Therefore, the extent to which this modality promotes functional gait characteristics remains to be further evaluated. Furthermore, the need to establish its treatment efficacy is of high public health importance in China, where no RCTs have been conducted among Chinese women. Finally, no RCTs have been conducted specifically using tailored Tai Ji Quan movements to evaluate its therapeutic benefits for those with knee OA.
To fill these gaps, we designed an RCT to determine the efficacy of a specifically tailored Tai Ji Quan training intervention to enhance objectively quantified gait kinematic outcomes among older Chinese women with knee OA. On the basis of prior research,18 we hypothesized that a tailored Tai Ji Quan intervention would improve spatiotemporal gait and knee range-of-motion outcomes.
2. Methods
2.1. Trial design
The study used a parallel-group RCT design to compare a Tai Ji Quan intervention with a health education control across a 24-week period. The trial included a 3-time-per-week intervention with classes conducted in local community centers. The study design and protocols (assessment, group assignment, and training) have been described elsewhere.25 The trial protocol was approved by the Ethics Committee of the Shanghai University of Sport and was performed in accordance with the World Medical Association Declaration of Helsinki-Ethical Principles for Medical Research involving Human Subjects. A written informed consent was received from all participants. Chinese Clinical Trial Registry (June 16, 2013): ChiCTR-TRC-13003264.
2.2. Study population and participants
Chinese women were the targeted study population because they have been shown to have a high prevalence of symptomatic and radiographic knee OA.2, 3, 4, 5 Major inclusion criteria for participating included (1) having a clinical diagnosis of knee OA per the criteria provided by the American College of Rheumatology,26 diagnosed through the use of knee radiographs and physical examination, (2) being between 60 and 70 years of age, and (3) being available 3 times a week over a 24-week period. In addition, a radiographic assessment of the erect anterior-posterior and medial-lateral views of both knees was conducted with classification made on the anterior-posterior and tibial-femoral radiographs using the Kellgren–Lawrence (K/L) grading scale (0–4) for knee OA,27 in which a grade of ≥1 was regarded as knee OA. Individuals who met the KL 1–3 grade standard were recruited.
Exclusion criteria included (1) having had lower limb surgery, (2) having other orthopedic problems of the hip, knee, or ankle, (3) having a neurological disease (e.g., Parkinson's, dementia, vertigo, or cerebral apoplexy), or (4) engaging in a current program of regular exercise. Also excluded were individuals who were unable to stand or walk and those who had received other forms of therapy in the preceding 2 months. Finally, those who expected to have major changes in their medication regimen or who were part of a rehabilitation program during the study were also excluded.
Participants were recruited between January and March in 2013 through contacts with community leaders and presentations at various community centers. A follow-up appointment was made for those who responded to the study promotion and indicated an interest in participating. These individuals were asked to visit a designated research facility where a detailed knee OA screening procedure and baseline assessments were conducted. Those who qualified per the study eligibility criteria were subsequently assigned to either the Tai Ji Quan group (TG) or the control group (CG). Intervention began within 1 week after the baseline assessment was completed.
2.3. Randomization and blinding
The individuals who met the eligibility criteria were allocated in a 1:1 ratio using a computer-generated random sequence with a permutated block size of 4. All assignments were made by a research staff member who was not directly involved in the trial. The assessors who conducted the outcome measures were blind to group allocation and were unaware of the study hypotheses. All statistical analyses were performed with masking maintained.
2.4. Intervention
2.4.1. Tai Ji Quan group
Individuals in this group participated in a 60 min session 3 times weekly for 24 weeks. The training protocol included 8 Tai Ji Quan forms: “Withdraw and push”, “Fan through the back”, “Wave hands like clouds”, “Lift hand”, “Brush knee and twist steps”, “Step back to repulse monkey”, “Fair lady works at shuttles”, and “Golden pheasant stands with one leg (right and left)”. All 8 forms were adapted primarily from a 24-form practice routine.28 To avoid over-strenuous activities around the knee joints, modifications were made to specifically focus on reducing and avoiding sustained unilateral weight bearing, dynamic rotation of the knee joints, and excessive knee flexion (i.e., low stance). The overall training protocol followed an easy-to-difficult progression, beginning with standing postures that focused on vertical body alignment, centering of the body mass, multi-directional weight shifting, and gentle and low-friction load-bearing knee flexion and extension exercises.
The protocol included 3 distinctive phases, with the first phase (Weeks 1–2) focusing on fundamental Tai Ji Quan preparatory movement exercises (e.g., weight shifting, heel strike, knee flexion and extension, push-off with the toes, stepping in various directions, and meditation and rhythmic breathing techniques). The second phase (Weeks 3–4) focused on learning and practicing forms with their associated movements. The third phase (Weeks 5–24) emphasized practicing and reinforcing the sequence and precision of the forms with variations in practice configuration (i.e., change in directions).
Intervention movements were closely integrated with rhythmic breathing. Each exercise session included a 5 min warm-up, a 50 min practice, and a 5 min cool-down period. Two instructors with more than 15 years of training and an academic specialization in Tai Ji Quan delivered the intervention. A nationally recognized academic and professional specialist in Tai Ji Quan curriculum and teaching trained the 2 instructors and monitored the fidelity of the intervention delivery on a weekly basis.
2.4.2. Control group
Participants in this group attended one 60 min wellness education lecture bi-weekly. In addition, a 10–15 min weekly check-in phone call was made by research staff members to monitor each participant's weekly activities, including levels of physical activity and changes in knee pain status and medication use. Each group session consisted of a 40 min lecture and a 20 min discussion on topics related to diagnostic criteria of knee OA, diet and nutrition, pain management and control, wellness and lifestyle changes, physical therapies, and management of medication use. Orthopedic surgeons, nutritionists, and health consultants from local universities and hospitals delivered the lectures. Participants were asked to maintain their regular daily activities and not to start any new exercise programs.
2.5. Study procedures and assessment
At baseline and again at 24 weeks, participants visited the laboratory at the Shanghai University of Sport, where study assessors blinded to study conditions took information related to demographics (age, education), clinical profiles (duration of knee pain, chronic conditions), anthropometric measures (height, weight), and study outcome measures (temporal-spatial gait parameters and physical function). A standardized report form was used to document adverse reactions throughout the 24-week intervention period. The form assessed unanticipated or undesirable experiences or reactions to the intervention exercises or laboratory-based assessment, including any falls, muscle discomfort, and exacerbations of knee-pain symptoms.
2.6. Outcome measures
2.6.1. Primary outcomes
The primary outcomes were changes in gait kinematics of the lower limbs from baseline to 24 weeks, including (1) velocity (cm/s), (2) step length (cm), (3) initial contact angle (°) of the flexed knee, and (4) maximal angle (°) of the flexed knee during the stance phase of walking. Participants were instructed to walk along a 12 m walkway (120 × 90 cm, length × width) at a comfortable pace, with gait cycles for each limb recorded for 3 trials per established protocol at our laboratory. Three-dimensional kinematic data on walking were collected using a 16-camera infrared motion analysis system (Vicon; Oxford Metrics, Oxford, UK). The lower extremity kinematics (velocity, step length, joint angles) were determined from markers placed on the ankles, knees, and hips and estimated joint center displacement data.29 The mean value from the 3 trials was calculated for each of the four measures.
2.6.2. Secondary outcomes
Secondary outcomes included measures of the Western Ontario McMaster Universities Osteoarthritis Index (WOMAC)30 and the Short Physical Performance Battery (SPPB).31 The WOMAC, which has been shown to be reliable, valid, and sensitive to change in knee OA populations,30 consists of 24 questions assessed on a 10 cm visual analog scale that measures 3 domains: pain (5 items), stiffness (2 items), and functional limitation (17 items). The SPPB, which has psychometric evidence established for older adults,31 is composed of 3 tests: (1) 3 increasingly challenging standing balance tests, (2) a short-distance (4 m) walk at a normal pace, and (3) standing 5 times from a seated position in a chair. Each test was scored on an ordinal scale ranging from 0 (worst performance) to 4 (best performance). A total score was constructed using the sum of the 3 tests (ranged from 0 to 12), with higher scores indicating better physical performance.
2.7. Sample size
The study was aimed at assessing the efficacy of a tailored Tai Ji Quan intervention on gait kinematics for older Chinese women with knee OA by detecting a between-group difference on the primary outcome of gait velocity in 24 weeks. Based on unpublished data from a prior pilot trial, it was expected that the Tai Ji Quan intervention would result in an 8 cm/s improvement relative to the CG (TG = 135 cm/s, CG = 127 cm/s, SD = 8). With a 5% significance level and 80% power, 17 participants per group (34 total) would be needed to provide 80% power. With an anticipated 20% attrition rate, 42 total participants were needed.
2.8. Statistical analysis
Baseline demographic and outcome measures across the 2 groups were compared using analysis of variance for continuous variables, the χ2 test for categorical variables, or independent t test for proportions. Results were presented as mean ± SD or percentages for all outcome measures. Main analyses, based on the intention-to-treat principle, wereperformed to examine change from baseline using independent t test with a 95% confidence interval (CI). A paired Student's t test was also performed to compare within-group differences. Scores on gait kinematics were collapsed across both limbs to form an average score in the final analysis. Sensitivity analyses adjusting for potential baseline confounders, including body mass index (BMI), duration of knee pain (in months), chronic conditions, and severity of knee OA as measured by radiography, were also performed.
A 95%CI was reported with each mean value. To adjust for multiple testing, Bonferroni corrections were made with an α level of 0.01 or less (2-sided) in determining statistical significance. Analyses were performed using SPSS 17.0 software (SPSS Inc., Chicago, IL, USA)
3. Results
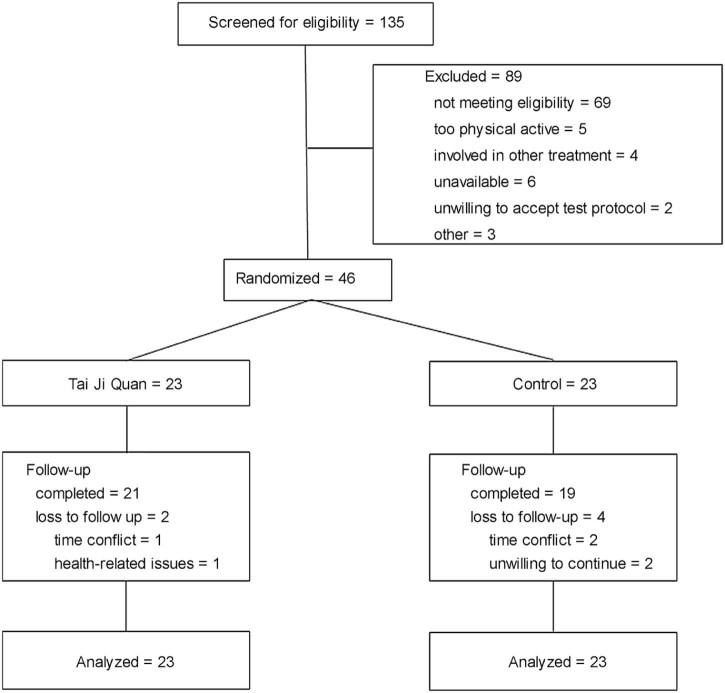
Fig. 1 provides a flow chart for study participation and follow-up. A total of 135 individuals responded to the study promotion. Of these individuals, 89 were excluded for various reasons. Forty-six individuals were qualified and subsequently randomized into either the TG (n = 23) or the educational CG (n = 23). Thirty-three participants (72%) were in high knee-OA grades (i.e., KL 2–3). Participant characteristics at baseline across the 2 study groups are presented in Table 1. There were no differences between the 2 groups on baseline characteristics.
Fig. 1.
Flow chart for study participation.
Table 1.
Baseline characteristics of the study participants.
| Measure | Tai Ji Quan (n = 23) | Control (n = 23) |
|---|---|---|
| Age (year, mean ± SD) | 64.61 ± 3.40 | 64.53 ± 3.43 |
| Body mass index (mean ± SD) | 25.23 ± 3.46 | 25.05 ± 3.42 |
| Education (n (%)) | ||
| Primary | 15(66) | 14(61) |
| Secondary | 4(17) | 4(17) |
| College/university | 4(17) | 5(22) |
| Duration of knee pain(month, mean ± SD) | 22 ± 13 | 22 ± 12 |
| Self-reported coexisting illness(n(%)) | ||
| Neck pain | 2(9) | 3(13) |
| Low back pain | 4(17) | 3(13) |
| Heart disease | 1(4) | 0 |
| Hypertension | 7(30) | 8(34) |
| Radiographic severity of knee(n(%)) | ||
| K/L grade 1 | 7(30) | 6(26) |
| K/L grade 2 | 12(52) | 14(61) |
| K/L grade 3 | 4(17) | 3(13) |
Abbreviation: K/L = Kellgren/Lawrence.
The 24-week primary and secondary outcomes were completed by 21 of 23 participants (91%) in the TG and 19 of 23 participants (90%) in the educational CG (Fig. 1). No adverse events (i.e., falls, significant joint pain or injury, cardiac arrest) were observed during the 24-week study period.
The average attendance rate (defined as the mean percentage of the exercise or education sessions that were completed by participants within each study group) across the 24-week intervention period was 87% for the TG and 78% for the CG. Six participants (n = 2 in Tai Ji Quan, n = 4 in control) withdrew from the study. Table 2 presents descriptive statistics on the primary outcomes. At 24 weeks, relative to the CG the TG showed greater improvement in gait velocity (8.40 cm/s, p = 0.01) and step length (3.52 cm, p = 0.004). In addition, compared to the CG the TG increased significantly in the initial contact angle (2.19°, p = 0.012) and maximal angle at the knee joint during the stance phase (2.61°, p = 0.003). Sensitivity analyses showed the outcome results were not affected by baseline characteristics (i.e., BMI, duration of knee pain, or severity of knee OA).
Table 2.
Changes in gait kinematics from baseline to the 24-week follow-up (mean ± SD).
| Variable | Group | Baseline | 24 weeks | Within group | Between group | ||
|---|---|---|---|---|---|---|---|
| Effect size (95%CI) | p | Effect size (95%CI) | p | ||||
| Gait velocity (cm/s) | TG | 135.72 ± 12.98 | 140.24 ± 11.82 | 4.52(0.52–8.52) | 0.029 | 8.40(1.62–15.18) | 0.01 |
| CG | 130.34 ± 10.93 | 131.84 ± 10.98 | 1.50(−2.14to5.16) | 0.401 | |||
| Step lengtha(cm) | TG | 65.61 ± 4.49 | 67.39 ± 3.95 | 1.78(0.70–2.87) | 0.002 | 3.52(1.21–5.83) | 0.004 |
| CG | 63.65 ± 2.87 | 63.87 ± 3.83 | 0.22(−1.03to1.47) | 0.722 | |||
| Initial contact angle of knee jointb(°) | TG | 2.56 ± 3.10 | 5.23 ± 2.50 | 2.67(1.30–4.03) | 0.001 | 2.19(0.52–3.87) | 0.012 |
| CG | 2.64 ± 3.61 | 3.04 ± 3.11 | 0.39(−0.08to0.87) | 0.102 | |||
| Maximal angle of knee jointc(°) | TG | 18.01 ± 3.65 | 21.03 ± 2.78 | 3.02(1.93–4.11) | <0.001 | 2.61(0.97–4.24) | 0.003 |
| CG | 17.55 ± 3.66 | 18.42 ± 2.74 | 0.87(0.26–1.49) | 0.008 | |||
Abbreviations: CG = control group; CI = confidence interval; TG = Tai Ji Quan group.
The distance between the point of initial contact of one foot and that of the opposite foot.
Measured at the moment when the foot strikes the ground.
Measured for the maximal angle for 1 leg during the stance phase.
After 24 weeks, compared to the CG the TG demonstrated a significantly greater decrease in knee pain (−4.22 points, p = 0.002), knee stiffness (−2.41 points, p < 0.001), and functional limitation (−11.04 points, p = 0.006). Similarly, compared to those in the CG, participants in the TG showed a significantly greater improvement in SPPB scores (1.22 points, p < 0.001) (Table 3).
Table 3.
Changes in secondary outcome measures of WOMAC and SPPB from baseline to the 24-week follow-up (point, mean ± SD).
| Variable | Group | Baseline | 24 weeks | Within group | Between group | ||
|---|---|---|---|---|---|---|---|
| Effect size (95%CI) | p | Effect size (95%CI) | p | ||||
| WOMAC-paina | TG | 8.46 ± 4.90 | 5.15 ± 3.24 | −3.30(−4.62to−1.99) | <0.001 | −4.22(−6.80to−1.63) | 0.002 |
| CG | 9.65 ± 5.64 | 9.37 ± 5.23 | −0.28(−1.78to1.21) | 0.699 | |||
| WOMAC-stiffnessb | TG | 3.57 ± 2.69 | 1.76 ± 1.32 | −1.80(−2.42to−1.19) | <0.001 | −2.41(−3.70to−1.13) | <0.001 |
| CG | 4.76 ± 3.00 | 4.17 ± 2.75 | −0.59(−1.10to−0.08) | 0.025 | |||
| WOMAC-functional limitationc | TG | 24.70 ± 12.95 | 15.85 ± 7.60 | −8.85(−12.38to−5.31) | <0.001 | −11.04(−18.70to−3.39) | 0.006 |
| CG | 25.37 ± 14.64 | 26.89 ± 16.56 | −1.52(−3.30to−6.34) | 0.519 | |||
| SPPBd | TG | 9.00 ± 0.60 | 11.09 ± 0.90 | 2.09(1.64–2.54) | <0.001 | 1.22(0.7–1.73) | <0.001 |
| CG | 9.22 ± 1.00 | 9.87 ± 0.82 | 0.65(0.25–1.06) | 0.003 | |||
Abbreviations: CI = confidence interval; WOMAC = Western Ontario and McMaster University Osteoarthritis Index; SPPB = Short Physical Performance Battery; TG = Tai Ji Quan group; CG = control group.
Ranged from 0 to 10 for each question; a total of 5 pain questions, with higher scores indicating greater pain.
Ranged from 0 to 10 for each question; a total of 2 stiffness questions, with higher scores indicating greater stiffness.
Ranged from 0 to 10 for each question; a total of 17 functional limitation questions, with higher scores indicating worse physical performance.
Higher scores indicate better physical performance.
4. Discussion
In this RCT we examined whether a tailored Tai Ji Quan intervention would improve gait kinematics and physical function among a population of Chinese older adult women diagnosed with knee OA. The findings from this 24-week intervention revealed that individuals receiving Tai Ji Quan training showed significant improvements in gait velocity, stride length, initial contact angle of the knee, and maximal angle of the knee compared to those in the educational control. The study also showed that Tai Ji Quan participants had a meaningful improvement in physical function as measured by both the WOMAC (>35% improvement in all 3 subscale measures from baseline) and SPPB (>1.0).31 The intervention was shown to be well tolerated by the participants as evidenced by the absence of any adverse events and a low attrition rate.
Compared to the CG, the TG demonstrated improved range of motion at the knee joint during the stance phase of gait. Although the mechanism(s) by which the intervention improved gait outcomes remains to be determined, the changes may be attributed to the specific characteristics inherent in the training protocol that focus on controlling posture and strengthening muscles around major joints (hip, knees, and ankles). Specifically, these exercises include postural alignment (standing and transitioning to upright poses, knee alignment in the support phase of gait), pre-movement preparation (expectant weight-shifting), movement initiation (stepping with hip flexion, knee extension, plantar- and dorsi-flexion), lateral and diagonal performance of forms (strengthening hip adduction and external rotation), and slow and controlled unipedal standing positions (strengthening leg muscles with unilateral weight-bearing).
The gait kinematics findings from this study are congruent with those reported from an uncontrolled study in the US, which showed, among other outcomes, improved stride length and frequency, and gait velocity.18 Taken together, the emerging research indicates not only encouraging evidence for therapeutic application but also points to the possibility of incorporating this program for prevention among those with significant risk factors for developing knee OA.
The study has some notable strengths. First, our study represents the first known RCT that specifically targeted a female Chinese population with a high prevalence of knee OA.2, 3, 4, 5 It is also the first study to use a specifically tailored Tai Ji Quan routine to treat women with knee OA. This is an important effort since not all Tai Ji Quan-based movements are considered functionally appropriate and safe for people with knee OA. A tailored training approach is recommended for evaluating specific health benefits of Tai Ji Quan.32 Finally, the use of the laboratory-based gait measures enhanced the objectivity of the study outcomes.
There are also some important limitations in this trial that future research should address. First, the fact that only self-selected older Chinese women with knee OA participated in our study limits the generalizability of the findings to other population groups with knee OA. Second, the intervention contact time across the 2 study conditions was not equivalent due to logistical constraints, so participants in the Tai Ji Quan intervention may have improved because of their additional exposure time. Third, since the study lacked an exercise control condition, future studies should include a comparable exercise control group with equal time allocated to each condition. Finally, studies that include a follow-up assessment after a period of time beyond the active intervention would help determine whether the benefits of Tai Ji Quan can be maintained beyond the initial training sessions.
The study points to the need for continued research to delineate the mechanism(s) through which the Tai Ji Quan intervention produced effects on gait. Since our gait measures were limited in scope, they preclude an in-depth analysis of the therapeutic effects of Tai Ji Quan for people with knee OA. For example, with the improved range of motion at the knee joint, the biomechanical impact of heel-landing on the knee joint during the stance phase of gait remains to be explored. In addition, because knee OA affects both medial and lateral compartments of the tibiofemoral joint among Chinese adults,3 future studies should examine the potential biomechanical influence of ankle and hip joint kinetics after completion of a Tai Ji Quan intervention on change in pain and gait outcomes in people with either medial or lateral knee OA.
5. Conclusion
Among older Chinese women with knee OA, a tailored, 24-week Tai Ji Quan intervention was shown to be efficacious in improving gait and other physical health outcomes. With the increase in the aging population in China and the accompanying high prevalence of knee OA, additional trials with more rigorous design and methodology are needed to understand the full potential of Tai Ji Quan for improving biomechanical characteristics and functional mobility as well as reducing pain symptomatology in knee OA patients.
Authors' contributions
YL and JXL contributed to the conception, protocol development, and design of the study. QZ and LH participated in data acquisition, analysis, and interpretation. XW, LW, YZ, and MF contributed to data acquisition, gait kinematics testing, and data interpretation. All authors have contributed significantly to the various stages in the writing of this manuscript and approved the final version of the paper. All authors agree with the order of presentation of the authors.
Competing interests
None of the authors declare competing financial interests.
Acknowledgments
The authors would like to thank all participants for their full cooperation and support during the conduct of this study, as well as the Martial Arts Department of the Shanghai University of Sport for its assistance in providing technical support and teaching of the intervention classes. The authors would also like to thank the administrative departments of the community-based organizations and local government agencies (especially the People's Government of Wu Jiao Chang in the Yangpu District in Shanghai), as well as Mrs. Zhihua Lu, for their assistance in recruiting study participants.
This study was funded by the Shanghai City Committee of Science and Technology Key Project (No. 12490503200) and the National Science Foundation for Distinguished Young Scholars of China (No. 81025022).
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Contributor Information
Yu Liu, Email: yuliu@sus.edu.cn.
Jing Xian Li, Email: jli@uottawa.ca.
References
- 1.Nguyen U.S., Zhang Y., Zhu Y., Niu J., Zhang B., Felson D.T. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med. 2011;155:725–732. doi: 10.1059/0003-4819-155-11-201112060-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang Y., Xu L., Nevitt M.C., Aliabadi P., Yu W., Qin M. Comparison of the prevalence of knee osteoarthritis between the elderly Chinese population in Beijing and whites in the United States: the Beijing osteoarthritis study. Arthritis Rheum. 2001;44:2065–2071. doi: 10.1002/1529-0131(200109)44:9<2065::AID-ART356>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 3.Felson D.T., Nevitt M.C., Zhang Y., Aliabadi P., Baumer B., Gale D. High prevalence of lateral knee osteoarthritis in Beijing Chinese compared with Framingham Caucasian subjects. Arthritis Rheum. 2002;46:1217–1222. doi: 10.1002/art.10293. [DOI] [PubMed] [Google Scholar]
- 4.Kang X., Fransen M., Zhang Y., Li H., Ke Y., Lu M. The high prevalence of knee osteoarthritis in a rural Chinese population: the Wuchuan osteoarthritis study. Arthritis Rheum. 2009;61:641–647. doi: 10.1002/art.24464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jiang L., Rong J., Zhang Q., Hu F., Zhang S., Li X. Prevalence and associated factors of knee osteoarthritis in a community-based population in Heilongjiang, Northeast China. Rheumatol Int. 2012;32:1189–1195. doi: 10.1007/s00296-010-1773-y. [DOI] [PubMed] [Google Scholar]
- 6.Bijlsma J.W., Berenbaum F., Lafeber F.P. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377:2115–2126. doi: 10.1016/S0140-6736(11)60243-2. [DOI] [PubMed] [Google Scholar]
- 7.Peat G., McCarney R., Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis. 2001;60:91–97. doi: 10.1136/ard.60.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fransen M., McConnell S., Harmer A.R., Van der Esch M., Simic M., Bennell K.L. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med. 2015;49:1554–1557. doi: 10.1136/bjsports-2015-095424. [DOI] [PubMed] [Google Scholar]
- 9.McAlindon T.E., Bannuru R.R., Sullivan M.C., Arden N.K., Berenbaum F., Bierma-Zeinstra S.M. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22:363–388. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Jevsevar D.S. Treatment of osteoarthritis of the knee evidence-based guideline (2nd ed.) J Am Acad Orthop Surg. 2013;21:571–576. doi: 10.5435/JAAOS-21-09-571. [DOI] [PubMed] [Google Scholar]
- 11.Australian Government National Health and Medical Research Council Guideline for the non-surgical management of hip and knee osteoarthritis. https://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/cp117-hip-knee-osteoarthritis.pdf Available at: accessed 01.02.2016.
- 12.Hochberg M.C., Altman R.D., April K.T., Benkhalti M., Guyatt G., McGowan J. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012;64:465–474. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 13.Guo Y.C., Qiu P.X., Liu T.G. Tai Ji Quan: an overview of its history, health benefits, and cultural value. J Sport Health Sci. 2014;3:3–8. [Google Scholar]
- 14.Brismée J.M., Paige R.L., Chyu M.C., Boatright J.D., Hagar J.M., McCaleb J.A. Group and home-based Tai Chi in elderly subjects with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2007;21:99–111. doi: 10.1177/0269215506070505. [DOI] [PubMed] [Google Scholar]
- 15.Lauche R., Langhorst J., Dobos G., Cramer H. A systematic review and meta-analysis of Tai Chi for osteoarthritis of the knee. Complement Ther Med. 2013;21:396–406. doi: 10.1016/j.ctim.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 16.Lee H.J., Park H.J., Chae Y., Kim S.Y., Kim S.N., Kim S.T. Tai Chi Qigong for the quality of life of patients with knee osteoarthritis: a pilot, randomized, waiting list controlled trial. Clin Rehabil. 2009;23:504–511. doi: 10.1177/0269215508101746. [DOI] [PubMed] [Google Scholar]
- 17.Lee M.S., Pittler M.H., Ernst E. Tai chi for osteoarthritis: a systematic review. Clin Rheumatol. 2008;27:211–218. doi: 10.1007/s10067-007-0700-4. [DOI] [PubMed] [Google Scholar]
- 18.Shen C.L., James C.R., Chyu M.C., Bixby W.R., Brismée J.M., Zumwalt M.A. Effects of Tai Chi on gait kinematics, physical function, and pain in elderly with knee osteoarthritis—a pilot study. Am J Chin Med. 2008;36:219–232. doi: 10.1142/S0192415X08005734. [DOI] [PubMed] [Google Scholar]
- 19.Song R., Lee E.O., Lam P., Bae S.C. Effects of Tai Chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: a randomized clinical trial. J Rheumatol. 2003;30:2039–2044. [PubMed] [Google Scholar]
- 20.Wang C., Schmid C.H., Hibberd P.L., Kalish R., Roubenoff R., Rones R. Tai Chi is effective in treating knee osteoarthritis: a randomized controlled trial. Arthritis Rheum. 2009;61:1545–1553. doi: 10.1002/art.24832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bejek Z., Paróczai R., Illyés A., Kiss R.M. The influence of walking speed on gait parameters in healthy people and in patients with osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2006;14:612–622. doi: 10.1007/s00167-005-0005-6. [DOI] [PubMed] [Google Scholar]
- 22.Elbaz A., Mor A., Segal G., Debi R., Shazar N., Herman A. Novel classification of knee osteoarthritis severity based on spatiotemporal gait analysis. Osteoarthritis Cartilage. 2014;22:457–463. doi: 10.1016/j.joca.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 23.Huang S.C., Wei I.P., Chien H.L., Wang T.M., Liu Y.H., Chen H.L. Effects of severity of degeneration on gait patterns in patients with medial knee osteoarthritis. Med Eng Phys. 2008;30:997–1003. doi: 10.1016/j.medengphy.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 24.Zeni J.A., Higginson J.S. Differences in gait parameters between healthy subjects and persons with moderate and severe knee osteoarthritis: a result of altered walking speed? Clin Biomech. 2009;24:372–378. doi: 10.1016/j.clinbiomech.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang X.Q., Huang L.Y., Liu Y., Li J.X., Wu X., Li H.P. Effects of Tai Chi program on neuromuscular function for patients with knee osteoarthritis: study protocol for a randomized controlled trials. Trials. 2013;14:375. doi: 10.1186/1745-6215-14-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Altman R., Asch E., Bloch D., Bole G., Borenstein D., Brandt K. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Arthritis Rheum. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 27.Kellgren J.H., Lawrence J.S. Radiographic assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.China Sports Editorial Board . China Sports Editorial Board; Beijing: 1980. Simplified “Taijiquan”. in Chinese. [Google Scholar]
- 29.Kadaba M.P., Ramakrishnan H.K., Wootten M.E. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8:383–392. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 30.Bellamy N., Buchanan W.W., Goldsmith C.H., Campbell J., Stitt L.W. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 31.Guralnik J.M., Simonsick E.M., Ferrucci L., Glynn R.J., Berkman L.F., Blazer D.G. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 32.Li F. Transforming traditional Tai Ji Quan techniques into integrated movement therapy–Tai Ji Quan: moving for better balance. J Sport Health Sci. 2014;3:9–15. doi: 10.1016/j.jshs.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]