Abstract
Background
Physical activity (PA) has been shown to benefit cognitive function in older adults. However, the cognitive benefits of exercising for older Chinese adults have not been systematically documented. This study was to conduct a systematic review on evidence that PA is beneficial for cognitive functioning in older Chinese adults.
Methods
Major databases, including PubMed, EMBASE, Cochrane Library, WanFang, CNKI, and VIP, were searched for studies published in English or Chinese between January 2000 and December 2015. Randomized and non-randomized controlled trials (RCTs and non-RCTs), cohort, case-control and cross-sectional studies that evaluated PA and cognitive function among older Chinese adults were included in this review.
Results
Of 53 studies included and reviewed, 33 were observational (22 cross-sectional, 7 case-control, and 4 cohort) and 20 were experimental (15 RCTs, 5 non-RCTs). Observational studies showed an association of reduced risk of cognitive-related diseases (i.e., mild cognitive impairment, Alzheimer's disease, and dementia) through PA, whereas experimental studies reported exercise-induced improvement in multiple domains of cognitive function (i.e., global cognitive function, memory, executive function, attention, language, and processing recourse).
Conclusion
This systematic review provides initial evidence that PA may benefit cognition in older Chinese adults. Further studies of individuals with cognitive impairments and prospective and RCT studies having high scientific rigor are needed to corroborate the findings reported in this review.
Keywords: Chinese elderly, Cognition, Dementia, Exercise, Public health, Systematic review
1. Introduction
With the unprecedented economic reform taking place over the past 30 years, China has experienced a significant demographic transition. As a result of an increase in life expectancy and decades of implementing the one-child policy, the Chinese population is aging rapidly.1 In 2014, it was estimated that in China there were about 212 million adults aged 60 and older, accounting for 15% of its total population.2 Advancing age is associated with a high risk of decline in cognitive functioning and with an increase in both prevalence and incidence of neurodegenerative disorders, including Alzheimer's disease (AD), vascular dementia, and dementia with Lewy bodies.3 In an analysis of epidemiologic studies, the authors estimated that in 2010 the number of dementia cases in China was about 9.19 million (20% of the worldwide total),4 with 30 million dementia cases predicted by 2050.5 In the coming decades, various brain-related diseases will begin to exert substantial health and economic burdens on Chinese society and the country's health care system.6
China will undoubtedly continue to face the tremendous public health and socioeconomic challenges that accompany a rapidly aging population who suffers from late-life declines in cognitive function. However, research has shown that one-third of AD cases worldwide (9.6 million) were attributable to modifiable risk factors, including physical inactivity.7 In fact, studies have shown that physical activity (PA) may be neuroprotective in preventing age-related cognitive decline, reducing the incidence of mild cognitive impairment (MCI) and delaying the onset of dementia.8, 9 An increasing number of studies also suggest that PA may be effective in managing cognitive impairment and dementia.10
Although studies conducted in Western countries have shown that there are cognitive benefits to be gained from PA, there is a scarcity of scientific knowledge regarding the health benefits of PA on cognitive function in older Chinese populations. This may be due in part to the absence of systematic reviews of studies conducted in China that provide evidence on the influence of PA on cognition. Access to this information is of high public health importance given the increasing number of older Chinese adults and the continued upward trend in both prevalence and incidence of cognitive impairments in this population. The purpose of this article was to fill this knowledge gap by conducting a systematic review of empirical studies that have evaluated the health benefits of PA on cognitive function among older Chinese adults.
2. Methods
2.1. Data sources and search strategy
We conducted an extensive search using several major electronic databases. These included PubMed, EMBASE, Cochrane Library, WanFang, CNKI, and VIP. The search covered studies published in English or Chinese between January 2000 and December 2015. No other sources or search strategies were sought. A search of article titles and abstracts was conducted by the primary author. The keyword terms used in the search included “physical activity”, “exercise”, “running”, “walking”, “aerobic training”, “cycling”, “Tai Chi” or “Tai Ji”, “Qigong”, “cognition”, “brain”, “neural plasticity”, “hippocampus”, “BDNF”, “dementia”, “Alzheimer”, “neurodegenerative”, “older adults”, “elderly”, “China”, “Chinese”, “Hong Kong”, and “Taiwan”. Review articles were also used as a source in a search for additional studies.
Citations were downloaded into an Excel spreadsheet and assessed for relevance against the prespecified inclusion and exclusion criteria (described later). Full-text articles were obtained for all studies entering the review. Any uncertainties or discrepancies about entering the review were resolved by consensus and, if necessary, by a third reviewer.
2.2. Inclusion and exclusion criteria
Eligible studies included 2 types: (1) experimental studies, comprising randomized controlled trials (RCTs) and non-randomized studies (non-RCTs) and (2) observational studies (cross-sectional, case-control, and cohort). To be eligible, studies must have measured at least 1 cognitive domain and required at least 1 type of PA practiced by older adults (50 years and older) with or without cognitive impairment. Finally, eligible studies had to have been conducted in the Mainland of China, Hong Kong or Taiwan, China.
Studies were excluded if they (1) were published without an English title or abstract, (2) did not include a minimal-attention control condition (in the case of experimental studies), (3) were duplicates of other studies, (4) simply described research protocols, or (5) were review articles.
2.3. Data extraction
Two reviewers extracted data into a form that identified the study methodology and characteristics of each study. Categories included (1) sample, (2) design, (3) details of the outcome (i.e., PA, cognitive function), (4) study duration, (5) intervention including intensity, frequency, and intervention duration, and (6) results. Data were extracted and synthesized separately for experimental studies and observational studies. No meta-analysis was conducted owing to significant variability in study design and methodologies. Instead, a narrative synthesis of all studies was produced.
2.4. Quality assessment
Because of the lack of a consistent instrument to assess methodological quality across studies having various designs, RCTs were the only studies in this review that were assessed using the core criteria from the Cochrane risk of bias assessment tool for RCTs.11 Specifically, each RCT was rated initially using a binary coding scheme of 1 (meeting the criteria) and 0 (not meeting the criteria). The rating assessed 5 methodological components: sequence, allocation, blinding, intent-to-treat, and completeness in reporting prespecified study outcomes. RCTs that provided no information on any of these criteria were coded as “not meeting the criteria”. A numerical rating for meeting any of these criteria was tabulated and summarized into 3 quality ratings: low (those that met 1 or 2 criteria), moderate (those that met 3 criteria), and high (those that met 4 or 5 criteria).
3. Results
3.1. Search results and study characteristics
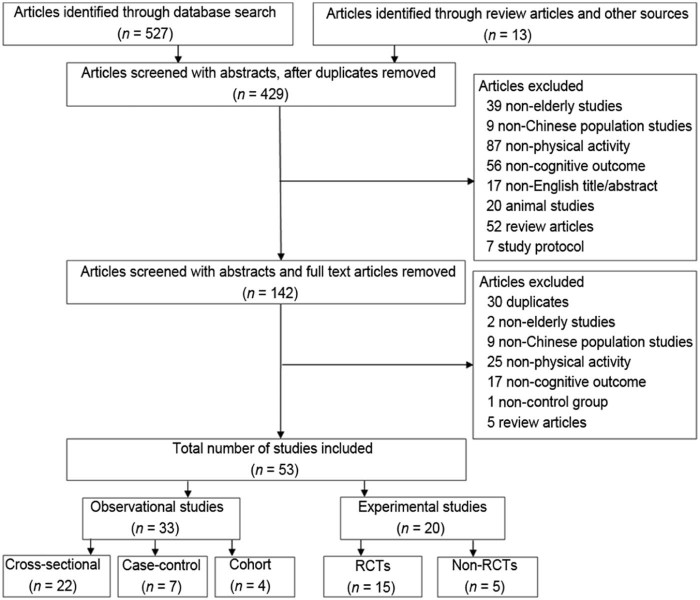
Overall, 540 articles were identified using our search strategy; of these, 487 were excluded from the review. A total of 53 studies met the inclusion and exclusion criteria (Fig. 1) and were subsequently reviewed in full. Of the 53 studies reviewed, 33 were observational (22 cross-sectional, 7 case-control, and 4 cohort) and 20 were experimental (15 RCTs and 5 non-RCTs).
Fig. 1.
Flow diagram of study selection. Non-RCTS = non-randomized controlled trials; RCTs = randomized controlled trials
The characteristics of the studies included in the review are summarized, organized by study design, in Table 1 (observational) and Table 2 (experimental). Of the 53 studies, 37 were conducted in the Mainland of China (23 observational (1 also took place in Hong Kong57), 14 experimental), 12 took place in Hong Kong, China (7 observational, 5 experimental), and 5 were conducted in Taiwan, China (4 observational, 1 experimental). Study sample sizes varied significantly, ranging from 135 to 27,651 participants (median = 988) for observational studies and from 29 to 555 participants (median = 84) for experimental studies. Although observational studies enrolled a mix of healthy older adults and those with cognitive impairment, most experimental studies (60%) targeted older adults with cognitive impairment (i.e., MCI and dementia).
Table 1.
Observational studies: physical activity and cognitive function.
| Study | Region | Subjects (age, mean ± SD) | Study type | Main outcome |
|---|---|---|---|---|
| Ho et al., 200127 | Hong Kong | 988 elderly (77.40 ± 5.99) | Cohort (with 3-year follow-up) | CI |
| Hong et al., 200340 | Mainland* | 254 older adults (80.70 ± 7.71) | Case-control | AD |
| Chan et al., 200556 | Hong Kong | 140 adults (65.69 ± 4.95) | Cross-sectional | Cognition |
| Zhang et al., 200741 | Mainland* | 258 older adults (79.09 ± 9.56) | Case-control | AD |
| Huang et al., 200928 | Mainland | 681 unrelated nonagenarians or centenarians (93.48 ± 3.30) | Cross-sectional | CI, MMSE |
| Lam et al., 200950 | Hong Kong | 782 community living older adults (72.11 ± 7.33) | Cross-sectional | Cognition |
| Yang et al., 200929 | Mainland* | 2161 older adults (69.77 ± 7.31) | Cross-sectional | CI |
| Jiao et al., 201030 | Mainland* | 673 older adults: 165 MCI patients and 508 controls (76.95 ± 0.59) | Case-control | MCI |
| Man et al., 201058 | Hong Kong | 135 older adults (68.38 ± 7.40) | Cross-sectional | Attention, memory |
| Gao et al., 201131 | Mainland* | 1900 older adults (age > 60 years, mean ± SD: NR) | Cross-sectional | MCI |
| Wu et al., 201132 | Taiwan | 2119 older adults (73.30 ± 5.9) | Cross-sectional | CI |
| Xu et al., 201133 | Hong Kong | 27,651 participants (62.06 ± 7.07) | Cross-sectional | MCI, memory |
| Yin et al., 201134 | Mainland* | 2164 older adults (age > 60 years, mean ± SD: NR) | Cross-sectional | MCI |
| Zhang and Zhang, 201151 | Mainland* | 380 community living older adults (age ≥ 60 years, mean ± SD: NR) | Cross-sectional | Cognition |
| Ku et al., 201249 | Taiwan | 1160 adults (age ≥ 67 years, mean ± SD: NR) | Cohort (with 11-year follow-up) | Cognition |
| Zhuang et al., 201235 | Mainland | 3176 home-living residents (69.70 ± 9.53) | Cross-sectional | CI |
| Fu et al., 201352 | Mainland* | 418 older adults in rest homes (age = 60–101 years, mean ± SD: NR) | Cross-sectional | Cognition |
| He et al., 201336 | Mainland* | 1393 community-dwelling elderly (73.17 ± 8.30) | Cross-sectional | CI |
| Liu et al., 201342 | Mainland* | 480 older adults: 120 patients with AD; 240 controls (age ≥ 60 years, mean ± SD: NR) | Case-control | AD |
| Song et al., 201353 | Mainland* | 1985 community-dwelling older adults (70.60 ± 5.16) | Cross-sectional | Cognition |
| Wang et al., 201355 | Mainland | 1463 healthy older adults (71.0 ± 5.0) | Cohort (with 2-year follow-up) | Cognition |
| Zhang et al., 201337 | Mainland* | 2460 community-dwelling older adults, (70.61 ± 7.06) | Cross-sectional | MCI |
| Chen et al., 201443 | Mainland* | 170 retired cadres from troops (85.47 ± 3.79) | Cross-sectional | AD |
| Gao et al., 201459 | Mainland* | 190 adults (62.18 ± 6.36) | Cross-sectional | Cognition |
| Li, 201444 | Mainland* | 2451 older adults (age > 60 years, mean ± SD: NR) | Cross-sectional | AD |
| Wei et al., 201447 | Mainland | 1324 highly educated elderly people (72.06 ± 8.71) | Cross-sectional | Dementia |
| Yang et al., 201445 | Taiwan | 942 older adults: 292 AD; 144 VaD; 506 controls (75.85 ± 7.24) | Case-control | ApoE e4, AD/VaD |
| Fan et al., 201548 | Taiwan | 7964 residents with 929 people with dementia (75.69 ± 6.58) | Cross-sectional | Dementia |
| Gao et al., 201554 | Mainland* | 190 adults (59.36 ± 6.09) | Cross-sectional | Cognition |
| Lee et al., 201546 | Hong Kong | 15,589 community-dwelling older adults (mean age = 74.17 years, SD: NR) | Cohort (with 6-year follow-up) | Dementia |
| Luo et al., 201538 | Mainland* | 1981 older adults: 299 MCI patients and 1682 controls (75.45 ± 6.48) | Case-control | MCI |
| Su et al., 201557 | Mainland and Hong Kong | 557 community elderly (260 in Hong Kong and 297 in Guangzhou) (73.4 ± 6.5) | Cross-sectional | Cognition |
| Zhao et al., 201539 | Mainland | 404 subjects, including 98 MCI and 306 cognitively normal (74.46 ± 8.72) | Case-control | MCI |
Abbreviations: AD = Alzheimer's disease; ApoE = apolipoprotein E; CI = cognitive impairment; Hong Kong = Hong Kong, China; Mainland = the Mainland of China; MCI = mild cognitive impairment; MMSE = Mini-Mental State Examination; NR = not reported; Taiwan = Taiwan, China; VaD = vascular dementia.
Published in Chinese.
Table 2.
Experimental studies: physical activity and cognitive function.
| Study | Region | Subjects (age, mean ± SD) | Study design | Interventions | Duration (weeks) | Main outcome |
|---|---|---|---|---|---|---|
| Lam et al., 201012 | Hong Kong | 74 older persons with dementia (83.45 ± 6.91) | RCT | Intervention: functional and skills training; 45 min/session, 2 sessions/week; control: occupational therapy | 8 | Global cognition |
| Kwok et al., 201164 | Hong Kong | 40 elderly with normal cognition (79.0 ± 5.8) | Non-RCT | Intervention: simplified version of Tai Chi; control stretching exercise; both, 40 min/session, 1 session/week | 8 | Cognitive function |
| Cao and Wei, 201260 | Mainland* | 163 patients with MCI (73.77 ± 7.20) | Non-RCT | Intervention: aerobic exercise (≥3 days/week, ≥30 min/day); control: no exercise | 24 | Cognitive function |
| Cui and Yang, 201263 | Mainland* | 29 women with normal cognition (66.18 ± 4.11) | Non-RCT | Intervention: Taiji ball exercise, ≥3 days/week, 60 min/day; control: no exercise | 48 | Memory |
| Lam et al., 201213 | Hong Kong | 389 subjects with aMCI (77.82 ± 6.48) | RCT | Intervention: 24-style Tai Chi; control: stretching exercise; both, ≥ 30 min/day, 3 days/week | 48 | Risk of dementia Cognitive function |
| Liu, 201220 | Mainland* | 40 patients with MS (68.05 ± 4.18) | RCT | Intervention: Wu Qin Xi exercise, 60 min/day, 6 days/week; control: no exercise | 24 | Cognitive function |
| Mortimer et al., 201214 | Mainland | 120 community elderly (67.80 ± 5.80) | RCT | Tai Chi and walking group: 50 min/session, 3 sessions/week; social interaction: 1 h/session, 3 sessions/week; control: no intervention | 40 | Cognitive function MRI |
| Liu and Wei, 201361 | Mainland* | 190 healthy older adults (63.96 ± 2.61) | Non-RCT | Aerobic exercise and mental activities group: ≥3 days/week, ≥30 min/day; control: no intervention | 48 | Cognitive function |
| Zheng et al., 201321 | Mainland* | 90 older adults with MCI (64.77 ± 5.37) | RCT | Intervention: Six Healing Sounds, twice a day, 30 min/time, ≥5 days/week; control: no exercise | 24 | Cognitive function EEG |
| Hu et al., 201422 | Mainland | 198 patients with MCI (age ≥ 65 years, mean ± SD: NR) | RCT | Intervention: jogging (30 min/session) and Tai Chi (60 min/session), 1 session/week; control: no exercise | 24 | Cognitive functions |
| Law et al., 201415 | Hong Kong | 83 older adults with MCI (73.8 ± 7.1) | RCT | Intervention (FcTsim): functional task exercise, 13 sessions (40–50 min/session); control: cognitive training, 6 sessions (60 min/session) | 10 | Cognitive function |
| Wei and Ji, 201423 | Mainland | 60 older adults with MCI (66.00 ± 5.08) | RCT | Intervention: handball training, 30 min/day, 5 days/week; control: no training | 24 | Global cognition |
| Zhang et al., 201462 | Mainland | 150 healthy older adults (64.79 ± 4.50) | Non-RCT | Swimming, running, square dancing, and Tai Chi groups: 65%–75% VO2max, 30–60 min/day, ≥4 days/week; control: no exercise | 72 | EEG (P300 test) |
| Lü et al., 201516 | Mainland | 45 community elderly with MCI (69.73 ± 4.78) | RCT | Intervention: momentum-based dumbbell training, 1 h/session, 3 sessions/week; control: no training | 12 | Cognitive function |
| Lam et al., 201517 | Hong Kong | 555 older adults with MCI (75.38 ± 6.47) | RCT | Physical exercise: 1 stretching/toning, 1 MB and 1 aerobic exercise session in a week; cognitive activity: 3 sessions/week; cognitive-physical exercise: 1 cognitive and 2 MB exercise; social activity: 3 sessions/week; all sessions lasted 1 h | 48 | Cognitive function |
| Sun et al., 201519 | Mainland | 150 healthy elderly with 138 included in analysis (66.55 ± 6.71) | RCT | Intervention: Yang-style Tai Chi, 60 min/session, 2 sessions/week; control: no exercise | 24 | Global cognition |
| Yang et al., 201524 | Mainland | 50 patients with mild AD (71.96 ± 6.92) | RCT | Intervention: cycling training with 70%VO2max, 40 min/day, 3 days/week; control: health education | 12 | Global cognition Biomarkers |
| Yeh et al., 201525 | Taiwan | 34 adults with physical disability (79.09 ± 10.40) | RCT | Intervention: physical (35 min resistance training) and cognitive (50 min cards, paired and reading) intervention, 2 sessions/week; control: no exercise | 12 | Cognitive function |
| Zheng et al., 201518 | Mainland | 45 healthy older adults with 34 included in analysis (70.12 ± 5.06) | RCT | Intervention: combined eighteen 1 h cognitive, eighteen 1 h Tai Chi, six 90 min group counseling sessions; control: two 120 min health education sessions | 6 | Cognitive function fMRI |
| Zhu et al., 201526 | Mainland* | 86 DM patients with MCI and 78 included in analysis (69.92 ± 6.41) | RCT | Intervention: Ba Duan Jin, 40 min/day, 5 days/week; control: no exercise | 48 | Global cognition |
Abbreviations: aMCI = amnestic mild cognitive impairment; DM = diabetes mellitus; EEG = electroencehalography; FcTsim = simulated functional tasks; fMRI = functional magnetic resonance imaging; Hong Kong = Hong Kong, China; Mainland = the Mainland of China; MB = mind–body; MRI = magnetic resonance imaging; MS = metabolic syndrome; NR = not reported; RCT = randomized controlled trial; Taiwan = Taiwan, China; VO2max = maximum oxygen uptake.
Published in Chinese.
3.2. Quality assessment
A detailed quality assessment of 15 RCTs is summarized in Table 3. Per the quality assessment scheme used in this review, 7 RCTs12, 13, 14, 15, 16, 17, 18 (47%) were judged to be of high quality, 1 (6%) was rated as moderate,19 and 7 (47%) were rated as being of low quality.20, 21, 22, 23, 24, 25, 26
Table 3.
Quality rating of randomized controlled trials.
| Study | Sequence | Allocation | Blinding | Intent-to-treat | Completeness in reporting prespecified study outcomes | Overall quality |
|---|---|---|---|---|---|---|
| Lam et al., 201012 | 1 | 1 | 1 | 1 | 1 | High |
| Lam et al., 201213 | 1 | 1 | 1 | 1 | 1 | High |
| Lam et al., 201517 | 1 | 1 | 1 | 1 | 1 | High |
| Law et al., 201415 | 1 | 1 | 1 | 1 | 1 | High |
| Liu, 201220 | 0 | 0 | 0 | 0 | 0 | Low |
| Lü et al., 201516 | 1 | 0 | 1 | 1 | 1 | High |
| Mortimer et al., 201214 | 1 | 1 | 0 | 1 | 1 | High |
| Hu et al., 201422 | 0 | 0 | 0 | 0 | 0 | Low |
| Sun et al., 201519 | 1 | 1 | 1 | 0 | 0 | Moderate |
| Wei and Ji, 201423 | 0 | 0 | 0 | 0 | 0 | Low |
| Yang et al., 201524 | 1 | 0 | 0 | 1 | 0 | Low |
| Yeh et al., 201525 | 0 | 0 | 0 | 0 | 0 | Low |
| Zheng et al., 201321 | 1 | 1 | 0 | 0 | 0 | Low |
| Zheng et al., 201518 | 1 | 1 | 1 | 0 | 1 | High |
| Zhu et al., 201526 | 1 | 1 | 0 | 0 | 0 | Low |
Note: 1 = meeting the criteria; 0 = not meeting the criteria.
3.3. Results from observational studies
3.3.1. PA and risk of cognitive impairment
3.3.1.1. Mild cognitive impairment or cognitive impairment
A total of 13 studies reported an association between PA and MCI or cognitive impairment.27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 A cohort study with a 3-year follow-up showed that a lack of exercise in older women was associated with increased risk of cognitive impairment (odds ratio (OR) = 2.2; 95% confidence interval (CI): 1.2–3.8).27 In contrast, a number of studies showed that an increased level of PA was associated with low risk for MCI or cognitive impairment among older adults living in the Mainland of China,28, 29, 30, 31, 33, 34, 35, 36, 37, 38, 39 Hong Kong,27 and Taiwan, China.32 Results from case-control studies also reported a reduced risk of MCI with a high level of PA (OR: 0.382–0.570).30, 38, 39 In addition, several cross-sectional studies reported a negative association between PA and the prevalence of MCI or cognitive impairment in older adults.28, 29, 31, 32, 33, 34, 35, 36, 37
3.3.1.2. AD
A total of 6 studies examined the association between PA and risk of AD.40, 41, 42, 43, 44, 45 Results from 4 case-control studies showed that older adults who engaged in PA were associated with a lower incidence of AD.40, 41, 42, 45 For example, Yang et al.45 reported that a higher level of leisure PA was associated with a lower risk of AD (adjusted OR (AOR) = 0.45; 95%CI: 0.30–0.68) and vascular dementia (AOR = 0.38; 95%CI: 0.23–0.63). In contrast, a study by Hong et al.40 showed that compared with healthy controls, older adults diagnosed with cognitive impairment who reported no time spent on daily PA were associated with an increased risk of AD (OR = 1.68; 95%CI: 1.304–2.172). Cross-sectional studies showed that the complete absence of PA was related to an increased AD prevalence (p < 0.01)43 and that a lack of PA in early life was associated with an increased likelihood of AD incidence (OR = 2.537, p < 0.001).44
3.3.1.3. Dementia
Three studies examined the relationship between PA and risk of dementia.46, 47, 48 One cohort study with a 6-year follow-up showed that community-dwelling older adults who participated in 2 habitual PAs were associated with a low risk of developing dementia for aerobic exercise (OR = 0.81; 95%CI: 0.68–0.95) and for mind–body exercises (OR = 0.76; 95%CI: 0.63–0.92).46 Two cross-sectional studies also reported that among highly educated older adults, a lack of PA was associated with dementia (OR = 2.56; 95%CI: 1.18–5.84),47 whereas regular exercise was associated with a decreased risk for dementia among community-dwelling older adults (OR = 0.12; 95%CI: 0.09–0.16).48
3.3.2. PA and cognitive function
3.3.2.1. Global cognitive function
A total of 10 studies assessed the relationship between PA and global cognitive function.28, 49, 50, 51, 52, 53, 54, 55, 56, 57 One cohort study49 with an 11-year follow-up showed an association between initial levels of PA and a slower decline in late-life global cognitive performance (β = 0.22, p < 0.05) and a positive relationship between changes in PA and changes in cognitive function during the long-term follow-up(β = 0.36, p < 0.05). Six cross-sectional studies28, 50, 51, 52, 53, 54 reported significant positive associations between older adults' PA and global cognitive function. For example, Lam et al.50 showed that older adults with long-term exercise habits of performing aerobic and mind–body exercises had better cognitive test scores, including scores on the Mini-Mental State Examination (MMSE) and Alzheimer's Disease Assessment Scale–cognitive subscale (ADAS-Cog), with a significantly better performance among young-old participants (65–75 years old). However, these findings were not consistent. For example, 1 cohort with a 2-year follow-up55 and 2 cross-sectional studies56, 57 showed no significant differences in global cognitive function measures between exercisers and nonexercisers.
3.3.2.2. Memory
The relationship between PA and memory was assessed in 7 studies.33, 50, 55, 56, 57, 58, 59 One cohort study with a 2-year follow-up showed that a high level of PA was mildly associated with less decline in episodic memory among older adults (β = −0.08, p < 0.05).55 Six cross-sectional studies33, 50, 56, 57, 58, 59 reported better memory performance outcomes (e.g., verbal memory, episodic memory) observed in the delayed recall test and digit and visual span test among older adults with higher levels of PA.
3.3.2.3. Executive function
One cross-sectional study57 reported that the total amount of PA positively but mildly correlated with executive function in the Category Verbal Fluency Test (CVFT) (r = 0.15, p < 0.01) but not with the Trail Making Test (r = 0.02, p > 0.05). One cohort study55 also showed no significant association between PA and executive function as measured by the Indiana University Tokens Test (β = 0.04, p > 0.05).
3.3.2.4. Attention
Two cross-sectional studies50, 58 showed that healthy community-dwelling older adults participating in regular aerobic and mind–body exercises (e.g., Tai Chi, yoga) showed better sustained and selective attention. However, these benefits were not supported in a cohort study in which PA was found not to be associated with attention among older adults living in Hong Kong, China and the Mainland of China.57
3.3.2.5. Language
Both cohort55 and cross-sectional50, 57 studies demonstrated a significant positive association between PA and verbal fluency as measured by the CVFT or the animal fluency test. However, in a cross-sectional study,56 researchers from Hong Kong, China found that language function in older adults was weakly associated with PA.
3.3.2.6. Processing resource
Only 1 study examined PA and its relationship to processing resource in older adults. In a cross-sectional study, Gao et al.59 reported that older adults who regularly exercised tended to perform better in a number of cognitive processing outcome measures, including sensory function, processing speed, and reasoning and processing capacity.
3.4. Results from experimental studies
3.4.1. Aerobic exercise
A total of 4 studies (3 non-RCTs and 1 RCT) conducted in the Mainland of China showed that aerobic exercise, when compared with a non-exercise control condition, resulted in a significant improvement in cognitive function (e.g., global cognitive function, executive function, language)24, 60, 61, 62 and reductions in disease symptoms associated with AD.24 For example, an RCT study reported by Yang et al.24 showed that a 3-month cycling training regimen significantly reduced symptoms of dementia (as indexed by change in ADAS-Cog) and improved global cognitive function and plasma apoprotein A1 levels. In a non-RCT study of 150 healthy older adults, Zhang et al.62 evaluated the health benefits of 4 different exercises (i.e., swimming, running, square dancing, and Tai Ji Quan) on cognitive function after a 12-month intervention. Compared with the control participants, participants in the exercise groups improved their event-related potential in the P300 test—a time-locked measure of electrical activity of the cerebral surface (as indexed by reduced P2, N2, and P3 latencies and response time). In addition, a stronger effect was observed among those who participated in the Tai Ji Quan exercise when compared with those assigned to other 3 exercise groups. Not all aerobic-based exercises were found to be effective in improving cognition. For example, 1 RCT14 involving a 40-week walking intervention showed no improvement in cognition among community-dwelling older adults.
3.4.2. Traditional Chinese exercises
3.4.2.1. Tai Ji Quan
Three RCTs13, 14, 19 and 3 non-RCTs62, 63, 64 evaluated the cognitive health benefits of Tai Ji Quan (or Taiji ball).14, 19, 62, 63, 64, 65 In an RCT, Mortimer et al.14 showed that a 40-week Tai Ji Quan intervention in a sample of healthy community-dwelling older adults resulted in a significant increase in brain volume and improvements in cognitive function as indexed in several neuropsychological measures, including the Mattis Dementia Rating Scale, Trail Making Test, Auditory Verbal Learning Test, and CVFT.
Two other RCTs involving older adults with MCI also showed consistent results of cognitive benefits from Tai Ji Quan.13, 22 For example, in a 1-year study of 389 older adults with MCI, Lam et al.13 showed that compared with those in a control group, participants in the Tai Ji Quan exercise group significantly lowered their risk of developing dementia (OR = 0.21; p = 0.04) and improved their delay recall. Similarly, Hu et al.22 showed that a 6-month Tai Ji Quan intervention for older adults with MCI resulted in a significant improvement in immediate memory (p < 0.001) and delayed recall (p = 0.004) function.
3.4.2.2. Qigong
Three RCTs conducted in the Mainland of China showed the cognitive benefits of Qigong exercises (e.g., Wu Qin Xi, Ba Duan Jin, and Six Healing Sounds).20, 21, 26, 65 One of these studies, a 6-month RCT,21 showed that the Six Healing Sounds exercise significantly improved the global cognitive function (i.e., in MMSE and Montreal Cognitive Assessment (MoCA)) and electroencephalographic results among older adults with MCI. Two other RCTs involving patients with metabolic disease evaluated the effects of Wu Qin Xi and Ba Duan Jin exercises and showed improved cognitive outcomes (i.e., in MMSE, MoCA, executive function, naming, attention, delay recall, and orientation).20, 26
3.4.3. Specialized exercises
There were 4 specialized exercise interventions conducted with older adults who had MCI or dementia. These involved handball exercise,23 functional tasks exercise,12, 15 and momentum-based dumbbell training.16 All 4 studies showed a significant improvement in cognitive function. For example, an RCT reported by Lü et al.16 showed that a 12-week momentum-based dumbbell intervention significantly improved cognitive performance (i.e., global cognitive function, executive function, immediate memory, and attention) in older adults with MCI.
3.4.4. Multimodal exercise-based interventions
There were 5 RCTs that used multimodal exercise-based or lifestyle interventions.17, 18, 22, 25, 61 These modalities involved a combination of various types of exercises (e.g., aerobic, strength, body–mind exercises) or activities related to cognitive health (e.g., cognitive training, social interaction). One 48-week RCT17 conducted in Hong Kong, China showed a significant improvement in ADAS-Cog, delayed recall test, and verbal fluency test. Another RCT conducted in Taiwan, China25 also showed that a 12-week resistance exercise program combined with cognitive training significantly improved MoCA and its subscales (i.e., naming, attention, delayed recall, and orientation).
The remaining 3 RCTs focused on a multicomponent exercise intervention in patients with MCI22 and a cognitive-psychological-physical intervention in healthy older adults.18, 61 Li and colleagues18, 66, 67 showed that a 6-week cognitive-psychological-physical intervention was effective in maintaining a healthy brain and improving executive function. Using functional magnetic resonance imaging, the study also showed exercise-induced brain functional plasticity, including reorganized regional homogeneity of spontaneous fluctuations, improved resting-state functional connectivity, and enhanced intrinsic brain activity in brain regions correlated with cognition.
4. Discussion
4.1. Summary of evidence
Over the past 15 years, a growing number of studies in China have examined the potential of PA for positively affecting cognitive health in older adult populations. This review has synthesized for the first time both observational and experimental studies that have contributed to our initial understanding of the relationship between PA and cognitive function among older Chinese adults.
Preliminary evidence presented in this systematic review suggests an important protective role of PA in preventing age-related cognitive decline and improving cognitive function for healthy older Chinese adults and those with cognitive impairment. Findings from observational studies indicate that in general, physically active older Chinese adults, especially those with long-term engagement or participation in PA early in life, are likely to have a lower risk of cognitive impairment and have better cognitive health and cognitive performance later in life.40, 45, 46 Similarly, some findings consistently indicate that exercise-based interventions can have a positive effect on lowering the risk of developing dementia and improving multiple domains of cognitive function, with the greatest benefits achieved through aerobic exercises24 and traditional Chinese physical activities such as Tai Ji Quan.13, 14
Although most studies have documented some positive associations or effects between PA and cognitive function, a few discrepancies in the findings were noted across both observational55, 56, 57 and experimental studies.14 These discrepancies can likely be attributed to differences in the selection of study populations, the type of PA or intervention, and/or methodological limitations. In addition, this review provides no evidence suggesting that the type, intensity, or frequency of various physical activities leads to a reduction in the incidence of MCI or AD or to improved cognitive function.
The limited number of studies examined, the wide range of sample sizes, the use of limited-exposure assessments and self-report measures, and the lack of rigorously designed studies temper the findings described in this review. All these factors may have contributed to results that are not always consistent across different types of study design, settings, and interventions. In this respect, the interpretation and generalizability of the findings presented here may be limited to only a few of the studies that displayed a high degree of scientific rigor in their designs and methodologies. In addition, of the 33 observational studies reviewed here, a vast majority (n = 22, 67%) were cross-sectional in design, making it impossible to infer causality. Similarly, only a few longitudinal studies on the relationship between PA and the incidence of cognitive impairment have been conducted in China.
Of the 15 RCTs reviewed, only a limited number were rigorously designed and were rated as being of high quality or showing low risk of bias. Many of the RCTs had notable limitations, including poorly defined clinical characteristics of study participants, poorly executed randomization procedures without proper concealment of allocation, an absence of interventions that specifically integrated a cognitive component with exercise training, and the small and often inadequately powered study sample sizes. These limitations make conducting meta-analyses and planning for the future quite difficult.
4.2. Future research
The evidence for the cognitive health benefits that older Chinese adults might gain from participating in PAs remains fragmented and inconclusive owing to the limited epidemiologic studies in this area and their lack of quality and scientific rigor. Given the increased life expectancy in China,1 long-term cohort studies are needed to better understand the relationship between PA and development of MCI, AD, and other types of dementia. Differences in the types and levels of PA and their relative benefits for cognitive function should be examined across various ethnic groups, urban–rural settings, and gender. For example, data from a representative cross-section of theChinese population have shown clear differences in cognitive function between older men and older women, with larger declines observed for older women.68
Given the limited number of RCTs exploring the relationship between exercise and cognitive function, especially from the Mainland of China, additional trials are clearly needed to corroborate the findings reported in this review. Interestingly, aerobic and low-intensity exercises such as Tai Ji Quan or Qigong appear to offer great potential in preventing cognitive decline and delaying the onset of dementia or slowing down its progression. Intervention studies that target older adults who are at higher risk of developing AD and dementia are urgently needed. In addition, new interventions that combine exercise movements and cognition components that might stimulate brain health should be developed and tested.
4.3. Implications for public health
The findings described in this review provide initial evidence regarding the potential cognitive health benefits of PA for older Chinese adults. These findings, however, must be corroborated by future studies, especially RCTs. It is also important to conduct research on the type, intensity, and frequency of PA that is needed to produce the greatest cognitive health benefits. Given this lack of research and evidence, it is not possible to develop up-to-date public health guidelines that make dependable recommendations for specific PAs that will prevent cognitive decline. Nevertheless, the mounting evidence in the PA literature indicating that PA offers older adults multiple health benefits,69, 70 including improved cognitive function,71, 72, 73 supports the idea that PA should be considered a primary prevention tool in maintaining normal cognitive function, preventing cognitive decline, and reducing the incidence of AD and dementia.
4.4. Limitations
This review has several limitations: (1) it is restricted to studies that were published within the past 15 years; (2) it may have omitted studies from the “gray” literature; and (3) it lacks an assessment of effect sizes. In addition, the quality assessment of the RCTs reviewed was limited in scope and depth. Future reviews should include a more detailed assessment of quality and include elements of design, analysis, and reporting of key information (i.e., dropout rates and consistency and clarity in reporting trial outcomes). Given these methodological limitations, caution should be exercised when interpreting the synthesized results presented here.
5. Conclusion
This systematic review provides some initial evidence showing that PA is beneficial for the cognitive health of older Chinese adults. Additional research is needed, including prospective studies examining relationships between PA and cognitive function over time and RCTs evaluating the efficacy of aerobic-based exercises specifically designed to preserve cognitive health in older Chinese adults and to slow down progression of cognitive decline in individuals with cognitive impairments.
Authors' contributions
JL participated in design of the study, searched articles, extracted data, performed quality assessment, drafted the manuscripts, and approved the final manuscript. WF participated in the data extraction and read and approved the final manuscript. YL conceived of the study, participated in its design and helped to draft the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
None of the authors declare competing financial interests.
Acknowledgment
The work presented in this article is supported by research grant from the National Natural Science Foundation of China (No.11372194). The authors thank Dr. Fuzhong Li for his help with the data synthesis and helpful advice and constructive comments during the various stages of writing this manuscript.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.World Health Organization China country assessment report on ageing and health. http://www.who.int/ageing/publications/china-country-assessment/en/ Available at: accessed 13.05.2016.
- 2.National Bureau of Statistics of China Statistical communique on China's 2014 national economic and social development. http://www.chinadaily.com.cn/business/2015-02/26/content_19660254.htm Available at: accessed 13.05.2016.
- 3.Yuan J., Zhang Z., Wen H., Hong X., Hong Z., Qu Q. Incidence of dementia and subtypes: a cohort study in four regions in China. Alzheimers Dement. 2016;12:262–271. doi: 10.1016/j.jalz.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Chan K.Y., Wang W., Wu J.J., Liu L., Theodoratou E., Car J. Epidemiology of Alzheimer's disease and other forms of dementia in China, 1990–2010: a systematic review and analysis. Lancet. 2013;381:2016–2023. doi: 10.1016/S0140-6736(13)60221-4. [DOI] [PubMed] [Google Scholar]
- 5.Prince M., Wimo A., Guerchet M., Ali G.C., Wu Y.T., Prina M. 2015. World Alzheimer Report 2015. The global impact of dementia: an analysis of prevalence, incidence, cost and trends. London: Alzheimer's Disease International. [Google Scholar]
- 6.Keogh-Brown M.R., Jensen H.T., Arrighi H.M., Smith R.D. The impact of Alzheimer's disease on the Chinese economy. E Bio Med. 2015;4:184–190. doi: 10.1016/j.ebiom.2015.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Norton S., Matthews F.E., Barnes D.E., Yaffe K., Brayne C. Potential for primary prevention of Alzheimer's disease: an analysis of population-based data. Lancet Neurol. 2014;13:788–794. doi: 10.1016/S1474-4422(14)70136-X. [DOI] [PubMed] [Google Scholar]
- 8.Blondell S.J., Hammersley-Mather R., Veerman J.L. Does physical activity prevent cognitive decline and dementia?: a systematic review and meta-analysis of longitudinal studies. BMC Public Health. 2014;14:510. doi: 10.1186/1471-2458-14-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sofi F., Valecchi D., Bacci D., Abbate R., Gensini G., Casini A. Physical activity and risk of cognitive decline: a meta-analysis of prospective studies. J Intern Med. 2011;269:107–117. doi: 10.1111/j.1365-2796.2010.02281.x. [DOI] [PubMed] [Google Scholar]
- 10.Paillard T., Rolland Y., de Souto Barreto P. Protective effects of physical exercise in Alzheimer's disease and Parkinson's disease: a narrative review. J Clin Neurol. 2015;11:212–219. doi: 10.3988/jcn.2015.11.3.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins J.P., Altman D.G., Gotzsche P.C., Juni P., Moher D., Oxman A.D. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343 doi: 10.1136/bmj.d5928. d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lam L.C.W., Lui V.W., Luk D.N., Chau R., So C., Poon V. Effectiveness of an individualized functional training program on affective disturbances and functional skills in mild and moderate dementia—a randomized control trial. Int J Geriatr Psychiatry. 2010;25:133–141. doi: 10.1002/gps.2309. [DOI] [PubMed] [Google Scholar]
- 13.Lam L.C., Chau R.C., Wong B.M., Fung A.W., Tam C.W., Leung G.T. A 1-year randomized controlled trial comparing mind body exercise (Tai Chi)with stretching and toning exercise on cognitive function in older Chinese adults at risk of cognitive decline. J Am Med Dir Assoc. 2012;13:568. doi: 10.1016/j.jamda.2012.03.008. e15–20. [DOI] [PubMed] [Google Scholar]
- 14.Mortimer J.A., Ding D., Borenstein A.R., DeCarli C., Guo Q., Wu Y. Changes in brain volume and cognition in a randomized trial of exercise and social interaction in a community-based sample of non-demented Chinese elders. J Alzheimers Dis. 2012;30:757–766. doi: 10.3233/JAD-2012-120079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Law L.L., Barnett F., Yau M.K., Gray M.A. Effects of functional tasks exercise on older adults with cognitive impairment at risk of Alzheimer's disease: a randomised controlled trial. Age Ageing. 2014;43:813–820. doi: 10.1093/ageing/afu055. [DOI] [PubMed] [Google Scholar]
- 16.Lü J., Sun M., Liang L., Feng Y., Pan X., Liu Y. Effects of momentum-based dumbbell training on cognitive function in older adults with mild cognitive impairment: a pilot randomized controlled trial. Clin Interv Aging. 2015;11:9–16. doi: 10.2147/CIA.S96042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lam L.C., Chan W.C., Leung T., Fung A.W., Leung E.M. Would older adults with mild cognitive impairment adhere to and benefit from a structured lifestyle activity intervention to enhance cognition?: a cluster randomized controlled trial. PLoS One. 2015;10:e0118173. doi: 10.1371/journal.pone.0118173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zheng Z., Zhu X., Yin S., Wang B., Niu Y., Huang X. Combined cognitive-psychological-physical intervention induces reorganization of intrinsic functional brain architecture in older adults. Neural Plast. 2015;2015 doi: 10.1155/2015/713104. 713104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sun J., Kanagawa K., Sasaki J., Ooki S., Xu H., Wang L. Tai chi improves cognitive and physical function in the elderly: a randomized controlled trial. J Phys Ther Sci. 2015;27:1467–1471. doi: 10.1589/jpts.27.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu H. Correlation research on effect of wuqinxi exercise on cognitive function in older people with metabolic syndrome. J Wuhan Inst Phys Educ. 2012;46:56–61. in Chinese. [Google Scholar]
- 21.Zheng X., Yu J., Tu R., Sun S., Sun H., Wang X. Rehabilitation of “Six Healing Sounds” on MCI of the old-aged persons. Int J Tradit Chin Med. 2013;35:968–972. in Chinese. [Google Scholar]
- 22.Hu J.P., Guo Y.H., Wang F., Zhao X.P., Zhang Q.H., Song Q.H. Exercise improves cognitive function in aging patients. Int J Clin Exp Med. 2014;7:3144–3149. [PMC free article] [PubMed] [Google Scholar]
- 23.Wei X.H., Ji L.L. Effect of handball training on cognitive ability in elderly with mild cognitive impairment. Neurosci Lett. 2014;566:98–101. doi: 10.1016/j.neulet.2014.02.035. [DOI] [PubMed] [Google Scholar]
- 24.Yang S.Y., Shan C.L., Qing H., Wang W., Zhu Y., Yin M.M. The effects of aerobic exercise on cognitive function of Alzheimer's disease patients. CNS Neurol Disord Drug Targets. 2015;14:1292–1297. doi: 10.2174/1871527315666151111123319. [DOI] [PubMed] [Google Scholar]
- 25.Yeh I., Chang C.M., Chen K.C., Hong W.C., Lu Y.H. The influence of functional fitness and cognitive training of physical disabilities of institutions. Sci World J. 2015;2015 doi: 10.1155/2015/686498. 686498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhu H., Zhang N., Ji C. Influence of Baduanjin on mild cognitive impairment in elderly diabetic patients. Chin J Pract Nurs. 2015;31:1202–1204. in Chinese. [Google Scholar]
- 27.Ho S.C., Woo J., Sham A., Chan S.G., Yu A.L. A 3-year follow-up study of social, lifestyle and health predictors of cognitive impairment in a Chinese older cohort. Int J Epidemiol. 2001;30:1389–1396. doi: 10.1093/ije/30.6.1389. [DOI] [PubMed] [Google Scholar]
- 28.Huang C.Q., Dong B.R., Zhang Y.L., Wu H.M., Liu Q.X. Association of cognitive impairment with smoking, alcohol consumption, tea consumption, and exercise among Chinese nonagenarians/centenarians. Cogn Behav Neurol. 2009;22:190–196. doi: 10.1097/WNN.0b013e3181b2790b. [DOI] [PubMed] [Google Scholar]
- 29.Yang Y., Chen C.C., Li J.M., Zhao J.Q., Zhang F.F. The relationship between daily exercise and the age-related cognitive impairment. Mod Prev Med. 2009;36:2327,31. in Chinese. [Google Scholar]
- 30.Jiao F.B., Tan J.P., Wang L.N. A case-control study on psychosocial risk factors for mild cognitive impairment in elders. Chin J Contemp Neurol Neurosurg. 2010;10:203–207. in Chinese. [Google Scholar]
- 31.Gao L.W., Jiang L.L., Gao Y.Z., Nie H.W., Xu Y. Prevalence of mild cognitive impairment and its risk factors among elderly people in Canglang district of Suzhou city. Occup Health. 2011;27:2676–2678. in Chinese. [Google Scholar]
- 32.Wu M.S., Lan T.H., Chen C.M., Chiu H.C., Lan T.Y. Socio-demographic and health-related factors associated with cognitive impairment in the elderly in Taiwan. BMC Public Health. 2011;11:22. doi: 10.1186/1471-2458-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu L., Jiang C.Q., Lam T.H., Zhang W.S., Thomas G.N., Cheng K.K. Dose-response relation between physical activity and cognitive function: Guangzhou biobank cohort study. Ann Epidemiol. 2011;21:857–863. doi: 10.1016/j.annepidem.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 34.Yin S.Q., Nie H.W., Xu Y. The prevalence and risk factors of mild cognitive impairment among the aged in Huzhou. Chin J Pract. 2011;14:4145–4147. in Chinese. [Google Scholar]
- 35.Zhuang J.P., Wang G., Cheng Q., Wang L.L., Fang R., Liu L.H. Cognitive impairment and the associated risk factors among the elderly in the Shanghai urban area: a pilot study from China. Transl Neurodegener. 2012;1:22. doi: 10.1186/2047-9158-1-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.He X.Y., Cao R.F., Zhao G.Q., Jiang Q.P., Luo Y., Wang Y.G. A survey on cognitive function in Hangzhou community-dwelling elderly: prevalence and associated factors. Zhejiang Prev Med. 2013;25:8–10. in Chinese. [Google Scholar]
- 37.Zhang J.A., Jiang H., Wang F.C., Gao L.L. Investigation and analysis on mild cognitive impaiment among the elderly in the communities of Taicang city. Pract Geriatr. 2013;27:859–862. in Chinese. [Google Scholar]
- 38.Luo X., Tang M.N., Shen Y.E., Yu J.C., Huang R.Y., Ren J.J. Risk factors for mild cognitive impairment in community residents. Chin J Ceriatr Heart Brain Vessel Dis. 2015;17:227–230. in Chinese. [Google Scholar]
- 39.Zhao X., Yuan L., Feng L., Xi Y., Yu H., Ma W. Association of dietary intake and lifestyle pattern with mild cognitive impairment in the elderly. J Nutr Health Aging. 2015;19:164–168. doi: 10.1007/s12603-014-0524-2. [DOI] [PubMed] [Google Scholar]
- 40.Hong Z., Zhou F., Huang M.S., Zeng J., Ding D., Jin M.H. Exercise and activity as protection factors of Alzheimer's disease. Chin J Clin Rehabil. 2003;7:24–5,43. in Chinese. [Google Scholar]
- 41.Zhang Y.L., Huang H.L., Zhou Y.S. A 1:1 matched case-control study on factors of Alzheimer's disease. Chin J Contr Chron Non-commun Dis. 2007;15:328–330. in Chinese. [Google Scholar]
- 42.Liu X.B., Yan J.F., Zhou D.S., Chen Z.M. Lifestyle and risk of dementia: a case-study. Chin Pre Med. 2013;14:171–174. in Chinese. [Google Scholar]
- 43.Chen C.T., Shi X.Q., Zhang W.Z., Zhang L. An investigation and analysis of Alzheimer's factors affecting daily life of the special group. Mil Med J Southeast China. 2014;16:171–173. 211; in Chinese. [Google Scholar]
- 44.Li Q.P. Analyze and study the regional infection situation of Alzheimer's disease. J ZheJiang Chin Med Univ. 2014;38:654–656. in Chinese. [Google Scholar]
- 45.Yang S.Y., Weng P.H., Chen J.H., Chiou J.M., Lew-Ting C.Y., Chen T.F. Leisure activities, apolipoprotein E e4 status, and the risk of dementia. J Formos Med Assoc. 2014;114:1216–1224. doi: 10.1016/j.jfma.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 46.Lee A.T., Richards M., Chan W.C., Chiu H.F., Lee R.S., Lam L.C. Intensity and types of physical exercise in relation to dementia risk reduction in community-living older adults. J Am Med Dir Assoc. 2015;16:899. doi: 10.1016/j.jamda.2015.07.012. e1–7. [DOI] [PubMed] [Google Scholar]
- 47.Wei C.J., Cheng Y., Zhang Y., Sun F., Zhang W.S., Zhang M.Y. Risk factors for dementia in highly educated elderly people in Tianjin, China. Clin Neurol Neurosurg. 2014;122:4–8. doi: 10.1016/j.clineuro.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 48.Fan L.Y., Sun Y., Lee H.J., Yang S.C., Chen T.F., Lin K.N. Marital status, lifestyle and dementia: a nationwide survey in Taiwan. PLoS One. 2015;10 doi: 10.1371/journal.pone.0139154. e0139154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ku P.W., Stevinson C., Chen L.J. Prospective associations between leisure-time physical activity and cognitive performance among older adults across an 11-year period. J Epidemiol. 2012;22:230–237. doi: 10.2188/jea.JE20110084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lam L.C., Tam C.W., Lui V.W., Chan W.C., Chan S.S., Chiu H.F. Modality of physical exercise and cognitive function in Hong Kong older Chinese community. Int J Geriatr Psychiatry. 2009;24:48–53. doi: 10.1002/gps.2072. [DOI] [PubMed] [Google Scholar]
- 51.Zhang J., Zhang J.H. Analyses on influencing factors of cognitive function of the aged in city. J Shanxi Med Coll Contin Educ. 2011;21:62–65. in Chinese. [Google Scholar]
- 52.Fu J.M., Sun S.D., Pang W., Tan L., Li H.Q., Zhang Y. The study of correlation between physical activity and cognitive function in elderly residents. Chin J Prev Contr Chron Dis. 2013;21:22–25. in Chinese. [Google Scholar]
- 53.Song Y.J., Zhang B.L., Li J.Y., Li X.H., Shang L., Li J. Survey of cognitive impairment and associated factors for the elderly in community in Beijing. Chin J Rehabil Theory Pract. 2013;19:583–585. in Chinese. [Google Scholar]
- 54.Gao X., Chai J., Meng Y. Positive effects of physical exercise on cognitive function of the elder: based on the checking of psychological intermediary model of attitude toward aging and general self-efficacy. J Shenyang Sport Univ. 2015;34:7–12. in Chinese. [Google Scholar]
- 55.Wang H.X., Jin Y., Hendrie H.C., Liang C., Yang L., Cheng Y. Late life leisure activities and risk of cognitive decline. J Gerontol A Biol Sci Med Sci. 2013;68:205–213. doi: 10.1093/gerona/gls153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chan A.S., Ho Y.C., Cheung M.C., Albert M.S., Chiu H.F., Lam L.C. Association between mind-body and cardiovascular exercises and memory in older adults. J Am Geriatr Soc. 2005;53:1754–1760. doi: 10.1111/j.1532-5415.2005.53513.x. [DOI] [PubMed] [Google Scholar]
- 57.Su E.X., Lin Y.Q., Zhang S.L., Leung G.T., Lam L.C., Chiu H.F. Physical activity and cognitive function of community Chinese elderly in Hong Kong (HK) and Guangzhou (GZ) Int Psychogeriatr. 2015;27:959–966. doi: 10.1017/S1041610214002488. [DOI] [PubMed] [Google Scholar]
- 58.Man D.W., Tsang W.W., Hui-Chan C.W. Do older t'ai chi practitioners have better attention and memory function? J Altern Complement Med. 2010;16:1259–1264. doi: 10.1089/acm.2009.0462. [DOI] [PubMed] [Google Scholar]
- 59.Gao S.Q., Mao Z.X., Zhang L.C. Psychological mechanism of physical exercise delaying aging of primary mental ability: mediation model of cognitive processing resources. J Tianjin Univ Sport. 2014;29:461–466. in Chinese. [Google Scholar]
- 60.Cao M., Wei W.S. Clinical research intervention of rule physical exercise on mild cognitive dysfunction in the elderly. Ceriatr Health Care. 2012;18:173–174. in Chinese. [Google Scholar]
- 61.Liu J.W., Wei S.M. Effect of different leisure activities on the intellectual levels of elderly. Mod Prev Med. 2013;40:3801–3804. in Chinese. [Google Scholar]
- 62.Zhang X., Ni X., Chen P. Study about the effects of different fitness sports on cognitive function and emotion of the aged. Cell Biochem Biophys. 2014;70:1591–1596. doi: 10.1007/s12013-014-0100-8. [DOI] [PubMed] [Google Scholar]
- 63.Cui J., Yang L. Effects of taiji ball on the estrogen, muscle strength and cognitive function of the aging women. China Sport Sci Technol. 2012;48:108–112. in Chinese. [Google Scholar]
- 64.Kwok T.C.Y., Lam K.C., Wong P.S., Chau W.W., Yuen K.S.L., Ting K.T. Effectiveness of coordination exercise in improving cognitive function in older adults: a prospective study. Clin Interv Aging. 2011;6:261–267. doi: 10.2147/CIA.S19883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Guo Y., Shi H., Yu D., Qiu P. Health benefits of traditional Chinese sports and physical activity for older adults: a systematic review of evidence. J Sport Health Sci. 2016;5:270–280. doi: 10.1016/j.jshs.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li R., Zhu X., Yin S., Niu Y., Zheng Z., Huang X. Multimodal intervention in older adults improves resting-state functional connectivity between the medial prefrontal cortex and medial temporal lobe. Front Aging Neurosci. 2014;6:39. doi: 10.3389/fnagi.2014.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yin S., Zhu X., Li R., Niu Y., Wang B., Zheng Z. Intervention-induced enhancement in intrinsic brain activity in healthy older adults. Sci Rep. 2014;4:7309. doi: 10.1038/srep07309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Smith J.P., Strauss J., Zhao Y. Healthy aging in China. J Econ Ageing. 2014;4:37–43. doi: 10.1016/j.jeoa.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nelson M.E., Rejeski W.J., Blair S.N., Duncan P.W., Judge J.O., King A.C. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 70.World Health Organization Physical activity and older adults. 2011. http://www.who.int/dietphysicalactivity/factsheet_olderadults/en/ Available at: accessed 13.05.2016.
- 71.Bherer L., Erickson K., Liu-Ambrose T. A review of the effects of physical activity and exercise on cognitive and brain functions in older adults. J Aging Res. 2013;2013 doi: 10.1155/2013/657508. 657508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Carvalho A., Maeve Rea I., Parimon T., Cusack B.J. Physical activity and cognitive function in individuals over 60 years of age: a systematic review. Clin Interv Aging. 2014;9:661–682. doi: 10.2147/CIA.S55520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Larson E.B., Wang L., Bowen J.D., McCormick W.C., Teri L., Crane P. Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann Intern Med. 2006;144:73–81. doi: 10.7326/0003-4819-144-2-200601170-00004. [DOI] [PubMed] [Google Scholar]