Abstract
Objective
This study characterized overall and specific costs associated with hearing conservation programs (HCPs) at US metal manufacturing sites, and examined the association between these costs and several noise-induced hearing loss (NIHL) outcomes.
Design
We interviewed personnel and reviewed records at participating facilities. We also measured noise for comparison to the ten-year average of measurements made by each facility. NIHL outcomes assessed included rates of standard threshold shifts (STS) and high-frequency hearing loss, as well as prevalence of hearing impairment, for each participating facility. We used linear regression to identify per-person HCP costs that best predicted the NIHL outcomes.
Study Sample
We evaluated 14 US metal manufacturing facilities operated by a single company.
Results
Annual HCP costs ranged from roughly $67,000 to $400,000 (average $308±80 per worker). Our full-shift noise measurements (mean 83.1 dBA) showed good agreement with the facilities’ measurements (mean 82.6 dBA). Hearing impairment prevalence was about 15% overall. Higher expenditures for training and hearing protector fit-testing were significantly associated with reduced STS prevalence. Higher training expenditures were also related to lower hearing impairment prevalence and high-frequency hearing loss rates.
Conclusions
HCP costs were substantial and variable. Increased workplace spending on training and fit-testing may help minimize NIHL.
Keywords: Noise, Hearing Conservation/Hearing Loss Prevention, Psychoacoustics/Hearing Science, Medical Audiology
INTRODUCTION
The US Occupational Safety and Health Administration (OSHA) began regulating occupational noise in the US in 1971 with the promulgation of a Permissible Exposure Limit (PEL) of 90 A-weighted decibels (dBA) as an 8-hour time-weighted average (TWA) (OSHA, 1971). However, recognizing the inadequacy of this limit to adequately protect workers from noise-induced hearing loss (NIHL), in 1983 OSHA issued a Hearing Conservation Amendment (HCA) which required employers to create and manage a hearing conservation program (HCP) for workers exposed at levels greater than or equal to an Action Level (AL) of 85 dBA TWA (OSHA, 1983). The HCA requires that HCPs provide to workers, at a minimum: baseline and annual audiometric testing; a variety of hearing protection devices (HPDs); training and education; noise monitoring and evaluation; and maintenance of relevant records for all individuals exposed at levels equal to or greater than the AL (OSHA, 1983). Programs not in compliance with these requirements risk potential citations and fines following an inspection by OSHA compliance officers.
Although the HCA provides general guidelines for program compliance, it is a performance standard, and many different methods of implementation can be used to comply with the standard. HCPs across industries may vary widely, and even within companies, substantial differences in how sites interpret and administer both federal and corporate requirements can exist (Brueck et al., 2013). While it is generally assumed that maintaining a compliant HCP reduces rates of NIHL among workers, current research is conflicting (Adera et al., 1993; Wolgemuth et al., 1995; Davies, Marion and Teschke, 2008; Oestenstad, Norman and Borton, 2008; Fonseca et al., 2016; Muhr et al., 2016). Occupational NIHL rates in US industries remain high, even thirty years after adoption of the OSHA HCA (Masterson et al., 2016).
The apparent limited effectiveness of HCPs highlights current gaps in knowledge regarding individual program aspects and their effects on hearing health outcomes. Some researchers have suggested education and awareness as a key focus for effective HCPs (Rogers et al., 2009; Muhr and Rosenhall, 2011; O’Brien, Driscoll and Ackermann, 2014), while others point to HPD use (Heyer et al., 2011) and fit (Prince et al., 2004; Muhr and Rosenhall, 2011) or noise controls (Davies, Marion and Teschke, 2008). No studies to date appear to have quantitatively examined the relationship between company expenditures on different aspects of HCPs and rates of hearing impairment.
Given the gaps in available knowledge regarding the cost-effectiveness of US HCPs, we sought to better characterize costs associated with HCPs. Specifically, we: 1) evaluated overall costs and costs associated with individual program elements (e.g., training, noise monitoring, etc), and; 2) examined the association between overall and program element costs and several metrics of NIHL. The information obtained through this research has relevance to occupational hearing conservation efforts in the US, and also provides methods that may be useful for evaluating the cost-effectiveness of other occupational health programs.
METHODS
This study was approved for human subjects research by the Yale University Institutional Review Board (HIC: 0509000588). From 2012–2015, our team conducted site visits to 14 US metal manufacturing facilities operated by a single company for the purposes of developing evidence-based metrics to evaluate the effectiveness of hearing conservation programs. Site visits included structured interviews with health and safety managers, staff, and occupational nurses and physicians at each facility. During these interviews, information was collected from HCP managers and other company personnel regarding the costs associated with noise exposure and operating that site’s hearing conservation program; the cost categories and calculations used to compute costs are presented in Table 1. Our team also reviewed cost information from invoices and procurement if that information was available from management. Final spreadsheets incorporating all identified program costs were provided to each facility along with a comprehensive report to elicit feedback on any missing or incorrect data, which was corrected and updated as necessary. While workers’ compensation claims related to NIHL and hearing loss investigation costs may also be evaluated as outcome variables indicative of an ineffective HCP, they were included as program costs in order to more accurately describe the price associated with noise exposure and HCP management at the participating facilities.
Table 1.
Cost calculator categories, factors, and equations used for the overall assessment of hearing conservation program (HCP) costs at metals manufacturing facilities in the US (N=14).
| Description of Cost | Equation |
|---|---|
| Program management | For each employee with HCP responsibilities, including EHS technicians and managers, nurses, physicians, and administrative workers, if time has not already been counted in other cost categories: Hours per week spent on HCP × hourly rate (including fringe benefits) OR hourly rate (including fringe benefits) × percent of time required × 2000 hours per year |
| Audiometric testing | |
| Nurse’s time for initial employee audiograms | Hourly wage × time per test × tests per year |
| Employee’s time for initial audiogram | Average hourly wage × time per test × tests per year? |
| Nurse’s time for subsequent/follow-up testing | Hourly wage × time per test × tests per year |
| Employee’s time for subsequent/follow-up testing | Average hourly wage × time per test × tests per year |
| Nurse’s time for scheduling/rescheduling audiograms | Hourly wage × time |
| Workers’ Compensation | Cost per person for applicable workers’ comp claims/relevant time frame in years |
| Hearing protection devices (HPDs) | |
| ALL HPDs (except custom molds) | Cost per person × number of employees wearing OR total cost from vendor invoices |
| Custom-molded HPDs | Cost per person × number of employees wearing OR total cost from vendor invoices |
| Training | |
| Cost of materials | Flat rate OR cost per item × number of items produced |
| Employees’ time for initial training | Average hourly wage × time for training in hours × average number of employees completing training per year |
| Employees’ time for toolbox1 training | Average hourly wage × time for training in hours × average number of employees completing training per year |
| Employees’ time for annual training | Average hourly wage × time for training in hours × average number of employees completing training per year |
| Supervisor’s time for training | Average hourly wage × time for training in hours × average number of supervisors conducting training per year x number of trainings conducted per year |
| Fit-testing | |
| Employees’ time for fit-testing | Average hourly wage × time for fit-testing in hours × average number of employees completing fit-testing per year |
| Industrial hygiene | |
| IH consultant | Annual cost per year of all consulting services OR cost per hour × billable consulting hours per year |
| HCP software | Annual cost per year of software license OR cost of license / allowable years of use |
| Employees’ time for sampling | Average hourly wage × employee time required per sample × average number of samples taken per year |
| Hearing loss investigation | |
| Specialty referral fee | Cost per referral to a specialist × number of cases |
| Employee time for hearing loss case | Average hourly wage × time per referral appointment × number of referral cases per year |
| Equipment | |
| Sound level meter/dosimeter calibration | Flat rate, annually |
| Fit-test machine | Flat rate / useful life |
| Audiometer and headphone calibration | Flat rate, annually |
| Audiometric software | Flat rate / useful life |
| Audiometer | Flat rate / useful life |
| Sound level meter/dosimeter purchase | Flat rate / useful life |
| Council for the Accreditation of Hearing Conservationists | |
| Certification | (Cost of course + travel/lodging/per diem + wage cost for week-long course)(Number of certified individuals)/number of years covered |
| 5-year recertification | ([Cost + travel/lodging/per diem + wage cost for one day course][Number of certified individuals])/([number of years covered][5 years]) |
| Corporate software | Flat rate, annually |
Toolbox training is an informal shop floor training on a specific topic (e.g., noise and/or hearing loss) that is provided by a worker’s direct supervisor and may occur immediately before or after a work shift or during breaks.
Up to 45 full-shift personal noise measurements on workers were made by our team utilizing the OSHA AL standards during each site evaluation (85 dBA criterion level with 5 dB exchange rate). Measurements with a run time between 6–10 hours were corrected to an 8-hour TWA; measurements outside of this duration range were rare (<20% of all measurements), and were left as the average level over the actual runtime (LAVG), rather than normalized to a TWA. These measurements were compared to the ten-year noise measurement averages obtained for each facility from the company’s comprehensive corporate noise database; these measurements were also collected using OSHA AL criteria and corrected to an 8-hour TWA. For facilities that had operated for fewer than ten years, all available yearly noise measurement averages were provided.
Due to an ongoing research and data sharing relationship between Yale University and the company, we were able to utilize audiometric surveillance data as well as company noise exposure measurements for each of the 14 facilities participating in the study. These included age- and non-age-corrected Standard Threshold Shift (STS) rate (%), high-frequency hearing loss rate (in dB/year), and prevalence of hearing impairment (%). An STS was defined as an increase of at least 10 dB in the average audiometric threshold taken at 2000, 3000, and 4000 Hz compared to the baseline audiogram. Age-correction was performed using standard OSHA age-correction tables (OSHA, 1993). Both age- and non-age-corrected STS rates were calculated as a percentage of employees receiving annual hearing tests within the population of the HCP over the five years preceding our site evaluation. High-frequency hearing loss was calculated as the average change per year (dB/year) of the 3000, 4000, and 6000 Hz thresholds averaged across all workers (two measurements per worker, one for each ear) over the ten years preceding our site evaluation. The prevalence of hearing impairment was calculated according to the guidelines of the American Medical Association (AMA), where individuals were classified as hearing impaired if average hearing thresholds at 500, 1000, 2000, and 3000 Hz exceeded 25 dB hearing loss in either ear (AMA, 2001). This percentage value represented the percent of hearing impaired individuals within the facility’s HCP for the most recent year available.
IBM SPSS Statistics Version 24 (Armonk, NY) was used for all statistical analyses. Variables were summed by category (Table 1), and split into wage- and non-wage-related costs for descriptive statistics and further analyses. To standardize costs across facilities with different workforce sizes, cost category totals were also divided by the number of individuals within the associated HCP at the time of the evaluation, to yield a per-person cost. The average noise exposure trend was calculated in dBA per year, where a negative value indicates a decreasing average noise exposure and a positive value indicates increasing average noise exposures; trends of −0.05 dBA and below were chosen to represent facilities with decreasing (i.e., not relatively stable or increasing) noise exposure trends. We conducted bi-variate analyses (e.g., correlation coefficients and scatterplots) to assess potential co-linearity among the cost calculator and noise exposure variables, and we performed linear regression modeling to identify per-person cost variables that best predicted the four hearing health outcomes. In addition to using standard significance testing (α=0.05), we evaluated our results using Bonferroni corrections, due to the increased likelihood of Type 1 error when performing repeated significance testing using a single outcome variable (Dunn, 1961).
RESULTS
The 14 participating facilities represented primary and secondary processes of metal manufacturing (one and 11 sites, respectively), with some facilities encompassing both processes (two sites). HCPs at the participating sites ranged in size from 225–1513 workers, with a median of 567 workers (mean=666, total=8578 workers). HCP management varied by site, with nine facilities performing all HCP elements in-house, and the remaining five sites using a contractor or hospital to assist with some level of program administration.
Noise and Hearing
The average age-corrected STS prevalence of 3.1% (range: 1.4–6.6%) was substantially lower than the non-age-corrected prevalence of 7.6% (3.2–11.2%, Table 2). Age-corrected and non-age-corrected STS rates were significantly correlated (r=0.83, p<0.001, Figure 1), although average employee age was not significantly related to the available hearing health outcomes (data not shown). On average, high-frequency hearing thresholds improved over time (mean −0.1 dB/year), though some plants showed increasing rates of high-frequency hearing loss (maximum 0.4 dB/year). The mean hearing impairment prevalence rate was approximately 15% across all facilities, with a large range (7.7% to 38%). While age- and non-age-corrected STS prevalence and high-frequency hearing loss rates were all related, hearing impairment prevalence for the most recent year was only related to high-frequency hearing loss rate (r=0.55, p=0.04, Figure 1). Full-shift noise exposures measured during the HCP evaluation site visit (mean=83.1 dBA) showed good agreement with measurements received from the corporate noise surveillance database (mean TWA=82.6 dBA), as shown in Figure 1 (r=0.59, p=0.03). The three sites that included some level of primary metal manufacturing had significantly lower average 10-year noise levels than facilities encompassing only secondary metal manufacturing aspects (79.0 vs. 83.5 dBA TWA, p=0.01). In an examination of the relationship between noise exposures and hearing health outcomes, the ten-year noise exposure trend (average change in noise TWA exposure in dBA/year) was also significantly related to non-age-corrected STS prevalence (r=0.54, p=0.045). Only three facilities reported a 10-year noise TWA exposure level of >85 dBA, and our measurements indicated an additional two facilities with an average full-shift noise exposure >85 dBA. In a comparison of the facilities with >85 dBA and ≤85 dBA exposure levels (both historically and during our assessment), we found no significant difference in any of the available hearing health outcomes between the groups.
Table 2.
Descriptive statistics for program costs (in US dollars) and noise and hearing loss rates at metals manufacturing facilities in the US (N=14).
| Overall Cost (USD) | Per Person Cost (USD) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cost Variables | N plants reporting costs | Mean | SD | Min | Max | Mean | SD | Min | Max | |
| Total costs | 14 | 191,417 | 99,542 | 67,016 | 396,638 | 308 | 80 | 203 | 438 | |
| Cost by wages vs. non-wages | ||||||||||
| Wages | 14 | 118,474 | 54,013 | 51,610 | 231,329 | 199 | 63 | 101 | 333 | |
| Non-wages | 14 | 72,943 | 58,513 | 15,406 | 196,400 | 108 | 57 | 56 | 253 | |
| Cost by program element1 | ||||||||||
| Program management | 14 | 56,270 | 39,010 | 10,600 | 132,725 | 94 | 50 | 20 | 186 | |
| Audiometry | 14 | 48,670 | 36,969 | 9,876 | 158,205 | 76 | 35 | 40 | 143 | |
| Workers Comp Claims | 2 | 42,218 | 50,893 | 6,231 | 78,204 | 90 | 96 | 22 | 159 | |
| HPDs | 14 | 44,559 | 45,077 | 9,175 | 183,500 | 64 | 43 | 25 | 161 | |
| Training | 14 | 14,045 | 10,436 | 2,819 | 34,600 | 23 | 13 | 7 | 46 | |
| Fit-testing | 4 | 3,818 | 2,460 | 825 | 6,656 | 9 | 11 | 0.9 | 25 | |
| Training + fit-testing | 14 | 15,136 | 11,306 | 2,819 | 39,249 | 25 | 15 | 7 | 52 | |
| Industrial hygiene | 13 | 7,102 | 6,149 | 483 | 22,822 | 15 | 14 | 0.4 | 42 | |
| Hearing loss investigation | 13 | 7,814 | 10,174 | 701 | 39,620 | 11 | 10 | 0.9 | 41 | |
| Equipment | 14 | 2,936 | 3,474 | 300 | 12,900 | 5 | 5 | 0.6 | 17 | |
| CAOHC2 certifications | 12 | 1,207 | 1,113 | 100 | 3,731 | 3 | 5 | 0.2 | 17 | |
| Noise and Hearing Loss Variables (N=14) | Mean | SD | Min | Max | ||||||
| Hearing loss | ||||||||||
| 10 dB age-corrected STS3 5-year average (%) | 3.1 | 1.4 | 1.4 | 6.6 | ||||||
| 10 dB non-age-corrected STS3 5-year average (%) | 7.6 | 2.5 | 3.2 | 11.2 | ||||||
| Average high-frequency hearing loss per year (dB) | −0.1 | 0.2 | -0.4 | 0.2 | ||||||
| Hearing impairment prevalence (%) | 15.2 | 7.5 | 7.7 | 38.0 | ||||||
| Noise | ||||||||||
| Mean noise exposure measured by research team during visit (dBA4) | 83.1 | 3.7 | 77.5 | 88.5 | ||||||
| Mean noise TWA exposure measured by facility over past 10 years (dBA) | 82.6 | 2.9 | 78.4 | 87.5 | ||||||
| Mean trend in noise TWA exposure for facility over past 10 years (dBA) | −0.9 | 1.5 | −5.0 | 0.5 | ||||||
Corporate software descriptives not included due to standardized prices across facilities; however, corporate software costs are included in total costs and non-wage costs in statistics above, but were otherwise not used for predictive modelling.
Council for the Accreditation of Occupational Hearing Conservationists
Standard Threshold Shift, as defined by the Occupational Safety and Health Administration, averaged over the five years preceding the site evaluation.
Measurements recorded during research team visit with run times between 6–10 hours in length were corrected to an 8-hour TWA. All other measurements (<20% of data) represent an LAVG value.
Figure 1.
Correlation matrix of hearing loss outcomes, including age-corrected standard threshold shift (STS) prevalence, non-age-corrected STS prevalence, age-corrected high frequency hearing loss rate (dB/year), hearing impairment prevalence, average noise exposure during hearing conservation program (HCP) assessment (dBA1), average 10-year noise TWA exposure for the facility (dBA), and 10-year average noise exposure change rate (dBA/year) for 14 metals manufacturing facilities in the US. (Note: scales vary based on data range)
HCP Cost
Annual HCP costs ranged from about $67,000 to almost $400,000, with an average cost of $308 per person each year. The range in costs per person per year was large ($203–438, Table 2), and the most costly facility program spent more than twice the amount per worker as the least-expensive. A majority of the overall costs of the HCPs across all categories were related to personnel wages (65% of per person costs), at an average rate of $199/person enrolled in the HCP each year. Among the different cost categories represented in Table 2, program management costs accounted for the greatest share, both overall (mean=$56,270) and by person (mean=$94), representing approximately 30% of all costs. Only two facilities reported Workers’ Compensation costs (mean=$42,218 or $90/person), and only four facilities reported performing fit-testing (categorized for our purposes as a specific type of training), with an average cost of $9 per person ($3,818 overall mean). The average reported cost of HPDs was $64 per person, per year, while training expenditures (including fit-testing) averaged approximately $23/person each year.
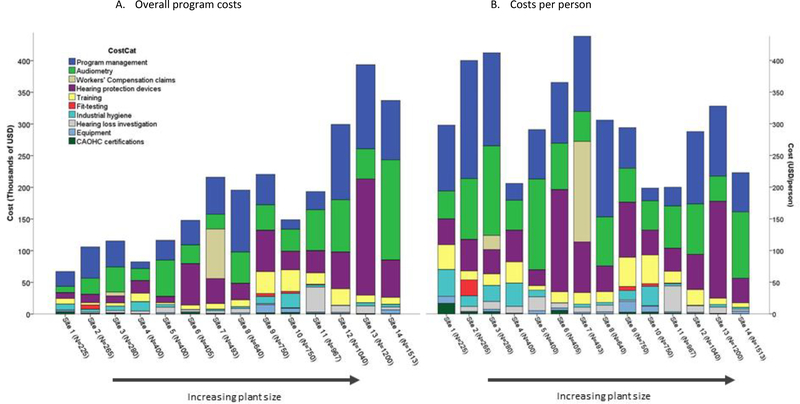
In general, as plant size increased, overall program cost also increased, but the four plants with the highest per-person costs all had under 500 workers in their HCPs (Figure 2). Figure 2 also shows large variability in the distribution of spending across cost categories, although program management, audiometry, and HPD costs commonly accounted for the highest proportion of both overall and per-person costs. As an example of cost variability, Sites 4, 5, and 6 all had approximately 400 workers in their HCPs, but their per-person costs varied by about $200, with Site 5 spending considerably more on audiometry, and Site 6 spending a larger percentage on HPDs. Sites that spent more on equipment also spent more on training (p=0. 004), and sites with higher industrial hygiene-related (IH) costs spent more on Council for the Accreditation of Occupational Hearing Conservationists (CAOHC) certification (p=0.03) and training (p=0.01). The majority of non-wage-related costs were associated with more spending on HPDs (p=0.01), and wage-related costs were significantly associated with program management (p<0.001). No significant differences in program costs were found between sites that performed all HCP aspects in-house and those that contracted out various elements of their HCPs.
Figure 2.
Hearing conservation program (HCP) costs by cost category for 14 metals manufacturing facilities in the US, where N represents the number of individuals enrolled in the associated HCP at the time of the study, ordered from smallest to largest facility in both figures. Figure 2(A) represents overall costs and Figure 2(B) represents costs per person in the associated HCP. (Note: Corporate software costs not included due to standardized expenditures across facilities and minimal generalizability)
Association between Program Costs and Hearing Outcomes
Per-person total HCP costs were not significant predictors of any of the four hearing health outcomes assessed (Table 3). However, in unadjusted analyses, higher expenditures on training plus any fit-testing costs and fit-testing alone were significant predictors of lower rates of non-age-corrected hearing loss (p=0.006 and 0.001, respectively), while fit-testing spending alone predicted lower rates of age-corrected STSs (p=0.045). Higher training costs plus any fit-testing cost and higher training costs alone were related to decreased rates of hearing impairment (p=0.01 and 0.04, respectively), while training costs that included fit-testing were related to lower 10-year average high-frequency hearing loss rates (p=0.03). Although only four facilities reported performing fit-testing, these facilities had the lowest percentages of age-corrected STSs, and three of the four facilities had the lowest rates of non-age-corrected STSs. All four facilities that performed fit-testing operated entirely in-house HCPs and did not contract any aspect of their program to an outside organization.
Table 3.
Unadjusted models for predicting percentage of age-corrected and non-age-corrected standard threshold shifts (STS) at metal manufacturing facilities in the US (N=14).
| Per Person Cost (USD) | Age-corrected STS1 (%) | Non-Age-Corrected STS1 (%) | High-Frequency Hearing Loss Rate2 (dB/year) | Hearing Impairment3 (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | β | SE | P | β | SE | p | β | SE | p | β | SE | p |
| Total costs | 0.001 | 0.005 | 0.782 | −0.003 | 0.008 | 0.716 | 0.001 | 0.001 | 0.207 | 0.027 | 0.024 | 0.263 |
| Cost by wages vs. non-wages | ||||||||||||
| Wages | 0.002 | 0.006 | 0.692 | −0.001 | 0.010 | 0.892 | <0.001 | 0.001 | 0.827 | 0.003 | 0.032 | 0.926 |
| Non-wages | 0.000 | 0.006 | 0.961 | −0.004 | 0.012 | 0.719 | 0.001 | 0.001 | 0.120 | 0.050 | 0.033 | 0.130 |
| Cost by program element4 | ||||||||||||
| Program management | 0.004 | 0.007 | 0.577 | 0.002 | 0.013 | 0.875 | 0.001 | 0.001 | 0.141 | 0.039 | 0.039 | 0.313 |
| Audiometry | 0.000 | 0.011 | 0.999 | 0.025 | 0.018 | 0.158 | <0.001 | 0.002 | 0.908 | −0.010 | 0.058 | 0.861 |
| Workers Comp Claims | −0.001 | 0.009 | 0.930 | −0.006 | 0.016 | 0.675 | 0.002 | 0.001 | 0.191 | 0.012 | 0.048 | 0.803 |
| HPDs | −0.001 | 0.009 | 0.945 | −0.011 | 0.015 | 0.454 | 0.001 | 0.001 | 0.604 | 0.090 | 0.041 | 0.026* |
| Training | −0.004 | 0.027 | 0.871 | −0.063 | 0.047 | 0.178 | −0.006 | 0.004 | 0.112 | −0.274 | 0.133 | 0.040* |
| Fit-testing | −0.095 | 0.048 | 0.045* | −0.239 | 0.074 | 0.001*** | −0.010 | 0.007 | 0.161 | −0.339 | 0.285 | 0.233 |
| Training + fit-testing | −0.023 | 0.024 | 0.332 | −0.098 | 0.035 | 0.006** | −0.007 | 0.003 | 0.029* | −0.283 | 0.111 | 0.011* |
| Industrial hygiene | 0.028 | 0.025 | 0.259 | −0.002 | 0.046 | 0.964 | 0.001 | 0.004 | 0.749 | −0.133 | 0.138 | 0.333 |
| Hearing loss investigation | −0.021 | 0.035 | 0.549 | 0.031 | 0.063 | 0.619 | −0.005 | 0.005 | 0.333 | 0.150 | 0.190 | 0.428 |
| Equipment | 0.018 | 0.077 | 0.813 | −0.034 | 0.140 | 0.805 | −0.12 | 0.011 | 0.280 | −0.605 | 0.398 | 0.128 |
| CAOHC5 certifications | 0.204 | 0.063 | 0.001*** | 0.147 | 0.146 | 0.314 | 0.010 | 0.012 | 0.379 | −0.125 | 0.462 | 0.788 |
Standard Threshold Shift, as defined by the Occupational Safety and Health Administration, averaged over the five years preceding the site evaluation.
Average threshold loss per year at 3000, 4000, and 6000 Hz over the ten years preceding our site evaluation. If the facility’s hearing conservation program was under ten years old, then all available years of data were used.
Hearing impairment as defined by the American Medical Association for the most recent year available at the time of the site evaluation.
Corporate software descriptives not included due to standardized prices across facilities; however, corporate software costs are included in total costs and non-wage costs in statistics above, but were otherwise not used for predictive modelling.
Council for the Accreditation of Occupational Hearing Conservationists.
Significant at the 0.05 α level
Significant at the 0.01 α level
Significant at the Bonferonni-corrected α level of 0.004
Facilities that spent more money on CAOHC certification for audiometric technicians had significantly higher prevalence of age-corrected STSs (p= 0.001), and facilities with higher HPD expenditures had higher rates of hearing impairment (p=0.03, Table 3). Although not statistically significant (p=0.19), a negative relationship did exist between number of individuals in an HCP and age-corrected STSs, where larger facilities had lower percentages of age-corrected STSs (r=−0.37). Additionally, facilities that did not report using contracted companies for any element of their HCP had lower rates of high-frequency hearing loss than those facilities that utilized a contractor for their program management (−0.17 dB/year vs. 0.04 dB/year, p=0.05). When accounting for repeated evaluations of linear relationships on the same outcome variable using Bonferroni corrections, higher expenditures on fit-testing remained a significant predictor of reduced non-age-corrected STS rates, while increased CAOHC spending was still significantly related to an increase in age-corrected STS rates.
DISCUSSION
To our knowledge, this study is the first to evaluate financial costs associated with operating an industrial HCP, and to attempt to link program costs and cost distributions to hearing health outcomes. Our analysis of 14 metal manufacturing facilities within the US demonstrated a significant link between training expenditures that included fit-testingand reduced STS prevalence, with fit-testing expenditures being the strongest predictor of reduced non-age-corrected STS rates. Increased training spending plus fit-testing spending was also related to reduced hearing impairment prevalence and lower high-frequency hearing loss rates.
We found significant inter-variable correlation between many of the hearing health outcomes that we evaluated, and we also found significant relationships between point-in-time noise measurements performed by our research team and those performed by the company and recorded within the corporate hygiene database over the preceding ten years. Interestingly, our models showed higher prevalence of age-corrected STS among facilities reporting more spending on CAOHC certifications, which remained a significant predictor even after performing Bonferroni corrections. We furthermore found an association between higher spending on HPDs and higher facility rates of hearing impairment. While the reasons for this are unclear, one possibility is that since age-corrected STS is a lagging indicator of hearing loss, facilities with more age-corrected standard threshold shifts may consequently begin spending larger portions of their HCP budget on certifying individuals to provide more comprehensive hearing loss services to workers, in order to combat increasing rates of NIHL. Similar effects may be occurring with HPD spending: Since the hearing impairment prevalence variable represented the most recent year of data available, higher rates of recent hearing impairment may have been recognized and triggered increased spending on HPDs. Non-age-corrected STS rates and high-frequency hearing impairment trends may be more challenging for facilities to identify, and therefore less likely to spark corrective actions through increased HPD and certification spending. We also believe non-age-corrected STS is a more leading indicator of hearing loss (Rabinowitz et al., 2007), and our results suggest that this may be an important metric for facilities to explore in assessing the effectiveness of their HCP.
This study has a number of limitations. First, all study sites were operated by the same company. While there were clearly differences in costs and program elements across the 14 surveyed sites, and some variability in HCP execution (i.e., fit-testing was relatively rare among the participating facilities), there were nevertheless underlying similarities in the programs assessed which may limit the generalizability of our results to other companies and industries. The second limitation is the relatively small sample size of 14 sites. While this is the largest analysis of hearing conservation program costs and performance that appears to have been published to date, it nevertheless represents a small sample of facilities in a single industry. A larger sample size would allow for multiple linear regression modeling and controlling for important modifying variables, such as employee age and facility noise levels, when assessing the effects of spending on hearing health outcomes.
The third limitation is that there were at least two costs that we did not formally account for in our analysis: the cost of workplace safety and health insurance premiums (D. Driscoll, pers. comm., 25 Feb 2017), and the cost of noise controls. Insurance costs can vary substantially depending on the occupational health and safety performance of insured facilities and companies, and it is possible that the participating sites with the worst hearing loss performance may have had additional insurance premium costs that are not reflected in the analyses presented here, and which could influence the observed relationships between hearing conservation program costs and hearing loss outcomes. We evaluated noise control efforts at the plant, but were not able to collect noise control cost information in a systematic way due to complexities in costs associated with engineering, maintenance, and other aspects of controls.
The fourth limitation is that all of the participating facilities adhered to the same exposure limit – the OSHA AL. The company’s use of the 5 dB exchange rate (and our resulting use of the same for comparison purposes) results in a reduced estimation of hearing loss risk for a given noise exposure level compared to the estimation of hearing loss risk that would result from the use of a 3 dB exchange rate. While not the primary focus of our analyses, this potentially affected our characterization of the facilities’ noise exposure and associated hearing loss metrics. Additionally, it is unclear whether the results presented here would be relevant to other facilities that use different exposure limits (for example, the Threshold Limit Value put forth by the American Conference of Governmental Industrial Hygienists, or the Recommended Exposure Limit used by the National Institute for Occupational Safety and Health). A related issue involved our treatment of measurements outside a duration of 6–10 hours as non-normalized (LAVG) values. In non-manufacturing environments with highly variable noise levels, this approach could potentially have introduced some bias into our exposure estimates. However, given the relatively stable levels observed in the participating facilities, we believe this approach was warranted, as it allowed us to use the small fraction of our measurements (<20%) that were outside of typical shift lengths. Despite these limitations, the analysis and results presented here represent an important step forward in assessing the cost-effectiveness of efforts to prevent occupational noise-induced hearing loss.
CONCLUSION
This study provides a basis for the use of HCP cost data and corporate noise and hearing loss records as a means to determine the most cost-effective aspects of HCPs, and also supports increased spending on training and fit-testing to minimize NIHL in the workplace. Additional research is needed to evaluate whether the associations between noise exposure, hearing health outcomes, and HCP program costs observed here are generalizable to other industries.
ACKNOWLEDGEMENTS
This research was funded by grants from the National Institute on Aging (Disease, Disability and Death in an Aging Workforce, NIH/NIA, 1 R01 AG026291–06), National Institute for Occupational Health and Safety (Assessing hearing conservation effectiveness, 1 R01 OH010132–01), and a contract with Alcoa Inc. At the time of the site visits, LFC received a portion of her compensation at Yale through a long-standing contractual agreement with Alcoa, Inc. The authors wish to thank the participating worksites, without whose support this research would not have been possible.
Abbreviations:
- AL
Action Level
- AMA
American Medical Association
- CAOHC
Council for the Accreditation of Occupational Hearing Conservationists
- dBA
A-weighted decibels
- dBHL
Decibels hearing loss
- HCA
Hearing Conservation Amendment
- HCP
Hearing Conservation Program
- HPD
Hearing protection device
- NIHL
Noise-induced hearing loss
- NIOSH
National Institute of Occupational Safety and Health
- OSHA
Occupational Safety and Health Administration
- PEL
Permissible Exposure Limit
- STS
Standard Threshold Shift
REFERENCES
- Adera T, Donahue AM, Malit BD and Gaydos JC (1993) ‘Assessment of the proposed Draft American National Standard method for evaluating the effectiveness of hearing conservation programs.’, J Occup Med: official publication of the Industrial Medical Association, 35(6), pp. 568–73. Available at: http://www.ncbi.nlm.nih.gov/pubmed/8331436 (Accessed: 28 June 2013). [DOI] [PubMed] [Google Scholar]
- AMA (2001) Guides to the Evaluation of Permanent Impairment. 5th edn. Edited by Andersson GBJ and Cocchiarella L. American Medical Association. [Google Scholar]
- Brueck SE, Prince Panaccio M, Stancescu D, Woskie S, Estill C and Waters M (2013) ‘Noise exposure reconstruction and evaluation of exposure trends in two large automotive plants.’, Ann Occup Hyg, 57(9), pp. 1091–104. doi: 10.1093/annhyg/met035. [DOI] [PubMed] [Google Scholar]
- Davies H, Marion S and Teschke K (2008) ‘The impact of hearing conservation programs on incidence of noise-Induced hearing loss in Canadian workers’, Am J Ind Med, 51(12), pp. 923–931. doi: 10.1002/ajim.20634. [DOI] [PubMed] [Google Scholar]
- Dunn OJ (1961) ‘Multiple comparisons among means’, J Am Stat Assoc, 56(293), pp. 52–64. Available at: http://www.jstor.org/stable/2282330 (Accessed: 19 June 2017). [Google Scholar]
- Fonseca VR, Marques J, Panegalli F, Gonçalves CG de O and Souza W (2016) ‘Prevention of the Evolution of Workers’ Hearing Loss from Noise-Induced Hearing Loss in Noisy Environments through a Hearing Conservation Program.’, Int Arch Otorhinolaryngol, 20(1), pp. 43–7. doi: 10.1055/s-0035-1551554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyer N, Morata TC, Pinkerton LE, Brueck SE, Stancescu D, Panaccio MP, Kim H, Sinclair JS, Waters MA, Estill CF and Franks JR (2011) ‘Use of historical data and a novel metric in the evaluation of the effectiveness of hearing conservation program components’, Occup Environ Med, 68(7), pp. 510–517. doi: 10.1136/oem.2009.053801. [DOI] [PubMed] [Google Scholar]
- Masterson EA, Bushnell PT, Themann CL and Morata TC (2016) ‘Hearing impairment among noise-exposed workers - United States, 2003–2012.’, MMWR. Morb Morta Wkly Rep, 65(15), pp. 389–94. doi: 10.15585/mmwr.mm6515a2. [DOI] [PubMed] [Google Scholar]
- Muhr P, Johnson A-C, Skoog B and Rosenhall U (2016) ‘A demonstrated positive effect of a hearing conservation program in the Swedish armed forces’, Int J Audio, 55(3), pp. 168–172. doi: 10.3109/14992027.2015.1117662. [DOI] [PubMed] [Google Scholar]
- Muhr P and Rosenhall U (2011) ‘The influence of military service on auditory health and the efficacy of a hearing conservation program’, Noise Health, 13(53), p. 320. doi: 10.4103/1463-1741.82965. [DOI] [PubMed] [Google Scholar]
- O’Brien I, Driscoll T and Ackermann B (2014) ‘Description and Evaluation of a Hearing Conservation Program in Use in a Professional Symphony Orchestra’, Ann Occup Hyg, 59(3), pp. 265–76. doi: 10.1093/annhyg/meu092. [DOI] [PubMed] [Google Scholar]
- Oestenstad RK, Norman MW and Borton TE (2008) ‘Efficacy of the U.S. Army policy on hearing conservation programs.’, Mil Med, 173(10), pp. 992–8. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19160618 (Accessed: 30 May 2017). [DOI] [PubMed] [Google Scholar]
- OSHA (1971) ‘Occupational Noise Exposure (general industry)’. Edited by and H OS. Administration. Washington, DC: US Department of Labor, p. 10466,10518. [Google Scholar]
- OSHA (1983) ‘Occupational Noise Exposure: Hearing Conservation Amendment; Final Rule’, Fed Reg. Washington, D.C.: US Department of Labor, pp. 9738–9785. [Google Scholar]
- OSHA (1993) ‘Noise exposure standard and impairment adjustments’, 29 CFR 1910.95 App F. Available at: https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=9741.
- Prince MM, Colligan MJ, Stephenson CM and Bischoff BJ (2004) ‘The contribution of focus groups in the evaluation of hearing conservation program (HCP) effectiveness.’, J Safety Res, 35(1), pp. 91–106. doi: 10.1016/j.jsr.2003.12.001. [DOI] [PubMed] [Google Scholar]
- Rabinowitz PM, Galusha D, Ernst CD and Slade MD (2007) ‘Audiometric “Early Flags” for Occupational Hearing Loss’, J Occup Environ Med, 49(12), pp. 1310–1316. doi: 10.1097/JOM.0b013e31815d1076. [DOI] [PubMed] [Google Scholar]
- Rogers B, Meyer D, Summey C, Scheessele D, Atwell T, Ostendorf J, Randolph SA and Buckheit K (2009) ‘What Makes a Successful Hearing Conservation Program?’, AAOHN J, 57(8), pp. 336–337. doi: 10.3928/08910162-20090729-07. [DOI] [PubMed] [Google Scholar]
- Wolgemuth KS, Luttrell WE, Kamhi AG and Wark DJ (1995) ‘The effectiveness of the Navy’s Hearing Conservation Program.’, Mil Med, 160(5), pp. 219–22. Available at: http://www.ncbi.nlm.nih.gov/pubmed/7659208 (Accessed: 28 June 2013). [PubMed] [Google Scholar]