Abstract
Objectives
This study examined associations between ethnic minority therapists’ reports of acculturation and adaptations made to multiple evidence-based practices (EBPs) in children’s community mental health services. Multilevel models examined therapist-, and practice-level predictors of Augmenting and Reducing/Reordering adaptations.
Methods
An online survey was completed by 235 therapists (86.0% female, Mage = 34.82 years, 68.1% Hispanic/Latino) as part of a larger study examining EBP sustainment in Los Angeles County. Acculturation was measured through therapist reports of cultural identity and language use.
Results
Analyses showed that the effect of heritage cultural identity on Augmenting adaptations was moderated by heritage language use. There was a significant interaction between heritage and US cultural identity dimensions in predicting Reducing/ Reordering adaptations. Therapists who reported higher levels of heritage cultural identity and lower levels of US cultural identification reported the fewest Reducing/Reordering adaptations, whereas therapists who reported higher levels of affiliation with both their heritage culture and US culture reported making the most Reducing/Reordering adaptations. Language acculturation and other cultural factors such as ethnicity and generational status did not predict either adaptation type. Therapists who reported more favorable perceptions of the EBP reported making fewer Reducing/Reordering adaptations.
Conclusions
Findings suggest that cultural identity is linked to the likelihood that ethnic minority therapists may adapt EBPs.
Keywords: Implementation, Adaptation, Evidence-Based Practice, Acculturation, Community Therapists
Evidence-based practices (EBPs) are increasingly being implemented in community settings that serve diverse children and families (Cooper et al., 2008). To inform these implementation efforts, it is important to understand how EBPs are delivered, and potentially adapted, by therapists. Given that many EBPs were developed and tested in research settings with predominately non-Hispanic White (NHW) clients, therapists in community mental health settings frequently question the cultural appropriateness of EBPs (Aarons et al., 2010; Southam-Gerow, Rodríguez, Chorpita, & Daleiden, 2012). Accordingly, many therapists recognize that EBPs may need to be adapted to better address the needs of the ethnic minority families they serve (Aisenberg, 2008; Bernal & Scharrón-del-Río, 2001; Cabassa & Baumann, 2013). In line with Chambers and Norton’s (2016) proposed creation of an “adaptome,” or common data platform to systematically characterize adaptations to EBPs across populations and contexts, various frameworks have been developed to describe adaptations in community settings (Baumann, Cabassa, & Stirman, 2017; Lau et al., 2017; Stirman et al., 2015). For example, building on Stirman and colleagues’ (2015) framework, the Augmenting and Reducing/Reordering Framework was developed within a multiple-EBP implementation context to characterize how community therapists make adaptations that augment (e.g., tailor the presentation, integrate supplemental content, lengthen the pacing) EBP delivery or reduce or reorder components of EBPs (Lau et al., 2017). Using this framework, information on the variability in how community therapists deliver EBPs could be used to provide feedback to intervention developers and inform implementation strategies to promote fit of EBPs for diverse communities.
Research has frequently focused on the development of systematic adaptations to EBPs to make interventions culturally responsive to particular ethnic groups (e.g., BigFoot & Schmidt, 2010; Domenech Rodríguez, Baumann, & Schwartz, 2011). Meta-analyses have supported that culturally-adapted EBPs have moderate to large effect sizes in general, but findings are mixed regarding whether adapted EBPs demonstrate superior effects compared to non-adapted EBPs (Gardner, Montgomery, & Knerr, 2016; Hall, Ibaraki, Huang, Marti, & Stice, 2016; Huey & Polo, 2008). In addition, group-specific cultural adaptations face the practical barriers involved in developing a different tailored protocol for every EBP and cultural group, making their strategic use challenging for a given mental health system or single provider. A more feasible alternative is a dynamic adaptation process that engages multiple stakeholders to systematically guide adaptations for different contexts (Aarons et al., 2012). In line with a dynamic adaptation process, the current study utilizes the Augmenting and Reducing/Reordering Framework (Lau et al., 2017) to understand the adaptations diverse therapists make to multiple EBPs within community mental health settings that predominately serve ethnic minority youth and families.
Culturally competent delivery of EBPs may involve adaptations to improve fit for the targeted community while maintaining fidelity. Some therapist adaptations may augment the EBP to attend to population-specific risk and protective factors, or focus on improving the engagement of diverse clients in the core components of an EBP (Hall et al., 2016; Lau, 2006). Adaptations focused on engagement may include framing interventions to be congruent with the vocabulary and metaphors clients use, emphasizing rapport building, and addressing clients’ perceptions and expectations (Bernal & Domenech Rodríguez, 2012), in line with Augmenting adaptations. Further, adaptations may involve dosing or pacing of interventions to improve outcomes, such as increasing opportunities to rehearse culturally unfamiliar skills, or slowing the pace of treatment (Lau, Fung, Ho, Liu, & Gudiño, 2011). However, some evidence suggests that therapists adapt EBPs by omitting core components that they perceive to be culturally unacceptable, in ways that represent drift and could compromise outcomes (Kumpfer, Alvarado, Smith, & Bellamy, 2002; Lau, 2012), reflective of Reducing/Reordering adaptations. Consequently, Reducing/Reordering adaptations may run the risk of omitting core components of EBPs that are responsible for therapeutic effects. Yet, evidence also suggests that some components of behavioral interventions may be trimmed while maintaining outcomes (e.g., Cognitive Behavioral Therapy focusing on behavioral activation, without cognitive restructuring; Dimidjian et al., 2006). One might presume that Augmenting adaptations have less potential for interfering with fidelity. Yet, some studies suggest that adding supplementary services or treatment components can undermine treatment effects (e.g., Chaffin et al., 2004).
It is especially important to examine adaptations among therapists from diverse backgrounds. Ethnic minority therapists are increasingly representing a larger proportion of the public mental health workforce (Lin, Nigrinis, Christidis, & Stamm, 2015) and are likely to serve ethnic minority clients, as these individuals represent a majority of recipients of public mental health services (U.S. Department of Health and Human Services, 2015). Ethnic minority therapists’ adaptations to EBPs may be influenced by their experience serving ethnic minority clients and their own cultural identity and experiences (Baumann et al., 2017). To date, findings have been mixed in regard to diverse community therapists’ perceptions of EBPs and their reports of adaptations to EBPs. Contrary to prior research (Aarons et al., 2010), recent studies have found that culturally diverse therapists may perceive EBPs more positively than previously suggested. For example, one study found that Latino therapists held more positive attitudes towards EBPs than NHW therapists in the context of system-driven implementation of multiple EBPs (Barnett et al., 2017). Within the same mental health system, Latino therapists were more likely than NHW therapists to report adaptations that augment the delivery of EBPs (i.e., tailoring language, integrating supplemental content, extending the pacing of practice), but were not more likely to report adaptations involving removing core components of EBPs (Lau et al., 2017).
Among ethnic minority therapists, variation in acculturation and enculturation may pattern perceptions of EBPs developed and tested within middle class NHW contexts. Clinician identification with United States (US) mainstream culture (i.e., acculturation) as well as their identification with their heritage culture (i.e., enculturation) may be associated with the likelihood that they may perceive the need to adapt EBPs. Acculturation has been described as a multidimensional phenomenon that encompasses changes in an individual’s cultural practices (e.g., language use, daily routines) as well as cultural identifications and values (Schwartz, Unger, Zamboanga, & Szapocznik, 2010). In particular, cultural identity formation has been viewed as a key facet of psychological acculturation (Schwartz, Montgomery, & Briones, 2006), and language use has been argued to be key to cultural learning (Masgoret & Ward, 2006). Although many large studies of American ethnic minorities have relied upon proxies for acculturation, such as nativity (Corral & Landrine, 2008) and years spent in the US (Alegria et al., 2007), we utilized more direct measures of cultural identification and language use and employed a bidimensional framework considering both acculturation toward host society language (i.e., English) and national identity (i.e., American identity), and enculturation toward heritage cultural identity and language (Sam & Berry, 2010). Consistent with Berry’s bidimensional model of acculturation, ethnic minority therapists may integrate both their heritage culture and mainstream culture into a bicultural identity (i.e., integration), they may strongly identify with mainstream American culture and may have more limited affiliation with their heritage cultural identity (i.e., assimilation), they may have strong affiliation with their heritage cultural identity and little orientation toward mainstream culture (i.e., separation), or finally they may identify with neither their heritage cultural identity nor the mainstream culture (i.e., marginalization) (Berry, 1997).
There is some evidence that therapists’ acculturation may shape aspects of psychotherapy training and delivery. Nilsson and Anderson (2004) found that more acculturated international counseling doctoral students reported higher levels of self-efficacy. A therapist’s ethnic identity and acculturation level may also affect the formation of the client-therapist relationship (Garcia & Zea, 1997; Lee & Zane, 1998; Sue & Sue, 2012). Certainly, bilingual competence impacts the extent to which therapists are able to provide services to ethnic minority families (Bean, Perry, & Bedell, 2001). Both cultural knowledge and the ability to communicate in a client’s preferred language may allow therapists to adapt treatment to better fit clients, build rapport (Comas-Diaz & Griffith, 1988; Kapasi & Melluish, 2015; Padilla & Salgado, 1987), and increase client retention (Sue, 1991). Further, ethnic minority therapists are more involved in communities of color, more likely to use cultural frameworks in their clinical practice, perceive their practice to be more culturally sensitive, report greater multicultural awareness and better therapeutic relationships with their clients compared to NHW therapists (Berger, Zane, & Hwang, 2014). Given the heterogeneity within and between ethnic minority groups, it is likely that aspects of individual therapists’ cultural identity might impact their implementation experiences with EBPs.
The role of acculturation has not been investigated in relation to community therapists’ implementation of or adaptations to EBPs. EBPs have largely been developed by NHW treatment developers and validated in samples with limited racial/ethnic diversity in clinical research settings (Bernal & Scharrón-del-Río, 2001.) Thus, it is plausible that ethnic minority therapists with greater acculturation to majority US culture may be more receptive to EBPs and may make fewer adaptations that reduce core components (i.e., Reducing/Reordering adaptations). Alternatively, ethnic minority therapists with stronger affiliation to their heritage culture and language may be both inclined and equipped to make culturally responsive adaptations that increase the fit of an EBP for an ethnic minority client. For example, these adaptations could include modifying the presentation of treatment by accommodating their clients’ language and cultural values (i.e., Augmenting adaptations). Interactive effects between acculturation and enculturation (i.e., identification with heritage cultural identity) factors are also possible. For example, ethnic minority therapists who have a strong heritage cultural identity and high heritage language use, as well as a strong mainstream American identity (i.e., integration), may be more likely to make Augmenting adaptations, as they may be open to using EBPs but may be motivated to increase their fit for ethnic minority clients. Therapists with a strong heritage cultural identity and high heritage language use, and low affinity for mainstream American culture (i.e., separation), may have the most reservations about standard EBPs and their fit for their own worldview and the clients they serve, and thus may be likely to engage in Reducing/Reordering adaptations that omit or de-emphasize EBP elements. Meanwhile, therapists who reject their heritage culture and language while adopting mainstream culture (i.e., assimilated) may be less likely to make any modifications to standard EBPs, as they may be open to using EBPs while not feeling the need to increase fit of EBPs with clients. The current study seeks to explore the effect of a mismatch between heritage cultural identity and language use on therapist-reported adaptations. In particular, the study will examine whether linguistic access moderates the association between heritage cultural identity and adaptations to EBPs. Language use is particularly important to examine in relation to enculturation because it is likely that therapists who identify with their heritage culture will vary in their heritage language use, which may be associated with differences in adaptations to EBPs.
Thus, the current study investigates how cultural identification may predict ethnic minority therapists’ adaptations to EBPs within the context of a system-driven implementation of multiple EBPs in children’s mental health services in Los Angeles County Department of Mental Health (LACDMH). Racial/ethnic minority therapists trained to deliver multiple EBPs in community settings completed a survey assessing two types of therapist-reported adaptations (i.e., Augmenting adaptations, Reducing/Reordering adaptations). We examined the extent to which cultural identity and language acculturation predicted therapist-reported EBP adaptations. Specifically, we examined the independent contributions of enculturation to the heritage culture and acculturation to American culture as well as their interaction while controlling for therapist characteristics related to cultural identity (e.g., race/ethnicity, generational status), previously-identified predictors of therapist adaptations (i.e., therapist attitudes towards specific EBPs) (Lau et al., 2017), and standard participant demographics (i.e., therapist gender and age).
Method
Study Context
The current study took place in the context of a system-driven implementation of multiple EBPs in children’s mental health services in LACDMH, the nation’s largest county mental health department. Beginning in Fiscal Year ‘10–11, through funds from the Prevention and Early Intervention program generated from the California Mental Health Services Act, LACDMH offered agencies reimbursement for the delivery of select EBPs. This new funding opportunity helped to offset what could have been a devastating cut in LACDMH services after a state budget shortfall. LACDMH initially provided implementation support (e.g., provider training) for six of the selected EBPs to address an array of youth mental health problems. These included Cognitive Behavioral Intervention for Trauma in Schools (CBITS), Child-Parent Psychotherapy (CPP), Managing and Adapting Practice (MAP), Seeking Safety (SS), Trauma-Focused Cognitive Behavior Therapy (TF-CBT), and Positive Parenting Program (Triple P) (see Regan et al., 2017 for further details about the system-driven reform).
Recruitment and Procedures
Data for the current study were collected as part of the larger Knowledge Exchange on Evidence-based Practice Sustainment (4KEEPS) study (Lau & Brookman-Frazee, 2016), examining sustainment of the six EBPs that were initially implemented. Therapists were eligible for the parent study if they billed for core psychotherapy services to at least one of the EBPs of interest. Therapists were recruited from participating community-based agencies. Of the 98 eligible agencies, 69 agencies (70.4%) provided therapist contact information or the option for therapists to sign up directly for the survey. In the larger study, 789 community-based mental health therapists completed surveys related to their experiences delivering the six EBPs, including the adaptations they made (see Lau et al., 2017 for further details about recruitment of the full study sample).
In order to pursue additional questions related to therapist workforce diversity, a supplemental Cultural Background Questionnaire was sent to the 789 therapist participants approximately 6 months later. Respondents included 416 therapists, for a response rate of 52.72%. Participants received a $10 incentive for completing this supplemental survey. Institutional Review Boards at [Masked for Review] approved all procedures for this study.
Participants
Of the 416 participants who completed both the 4KEEPS Therapist Survey and the Cultural Background Questionnaire, 147 therapists (35.3%) were excluded because they identified as NHW, and 34 therapists (8.2%) were excluded because they had not delivered one of the six EBPs of interest within the previous two months, and 237 therapists (57.0%) qualified for the current study. Two therapists did not provide complete data on the Cultural Background Questionnaire and so were excluded from analyses. Therefore, 235 therapists were included in the analyses. Within the Cultural Background Questionnaire completers, ethnic minority therapists had significantly fewer years of clinical experience (M = 5.2, SD = 4.1) than NHW therapists (M = 8.95, SD = 8.10), t = −6.00, p < .001). Ethnic minority therapists reported making more Reducing/Reordering adaptations than their NHW counterparts to SS, t = 2.37, p = 0.019, and TF-CBT, t = 2.22, p = 0.027.
Therapists were predominately female (86.0%) and were 34.82 years old (SD = 8.05) on average. The sample was 68.1% Hispanic/Latino, 16.6% Asian/Pacific Islander, 9.4% African American, and 4.3% multiracial, while 1.7% therapists indicated an unlisted racial/ethnic background. Therapists predominantly served Hispanic/Latino clients (M = 77.2%, SD = 26.2%). The majority of therapists (57.4%) were 2nd generation Americans (i.e., born in the US with at least one parent born in another country), 22.6% were 1st generation Americans (i.e., born in another country), and 20.0% were 3rd or later generation Americans. Most therapists reported being able to deliver services in a language other than English, with 63.8% reporting that they could deliver services in Spanish, 7.7% reporting another language (e.g., Farsi, Korean), and 0.9% in Spanish and another language. In terms of professional training, therapists were predominately Master’s-level therapists (89.8%) and unlicensed (69.8%). The most common mental health discipline was Marriage and Family Therapy (54.5%), followed by Social Work (34.9%).Therapists had been practicing, on average, for 5.2 years (SD = 4.1). See Table 1 for therapist characteristics.
Table 1.
Participant Characteristics (N = 235)
| Characteristic | Mean (SD) or n (%) |
|---|---|
| Age | 34.82 (8.05) |
| Gender | |
| Male | 33 (14.0%) |
| Female | 202 (86.0%) |
| Race/Ethnicity | |
| Hispanic/ Latino | 160 (68.1%) |
| Asian/ Pacific Islander | 39 (16.6%) |
| African American | 22 (9.4%) |
| American Indian or Alaska Native | 0 (0%) |
| Multiracial | 10 (4.3%) |
| Other | 4 (1.7%) |
| Generational Status | |
| 1st Generation | 53 (22.6%) |
| 2nd Generation | 135 (57.4%) |
| 3rd Generation & Above | 47 (20.0%) |
| Deliver Services in > 1 Language | |
| Spanish | 150 (63.8%) |
| Other Language | 18 (7.7%) |
| Spanish and Other Language | 2 (0.9%) |
| Caseload Race/Ethnicity Composition | |
| Hispanic/ Latino | 77.2% (26.2%) |
| Non-Hispanic, White | 5.4% (9.0%) |
| Asian/ Pacific Islander | 2.1% (9.1%) |
| African American | 12.8% (20.5%) |
| American Indian or Alaska Native | 0.7% (6.9%) |
| Other | 2.0% (9.9%) |
| Clinical Experience (years) | 5.2 (4.1) |
| Licensure Status | |
| Licensed | 71 (30.2%) |
| Unlicensed | 164 (69.8%) |
| Education Level | |
| Bachelor’s Degree or less | 5 (2.1%) |
| Master’s Degree | 211 (89.8%) |
| Doctoral Degree | 19 (8.1%) |
| Mental Health Discipline | |
| Marriage and Family Therapy | 128 (54.5%) |
| Social Work | 82 (34.9%) |
| Psychology | 22 (9.4%) |
| Other | 3 (1.3%) |
Measures
Therapist Characteristics
Questions about therapist characteristics were derived from the Therapist Background Questionnaire (Brookman-Frazee, Drahota, & Stadnick, 2012). Therapists completed questions about their personal and professional characteristics, including age, gender, race/ethnicity, and licensure status. Therapists also reported on which of the six EBPs they had 1) received training, 2) ever delivered, and 3) delivered in the previous two months.
Cultural Background Questionnaire
The Cultural Background Questionnaire is a 19-item self-report measure used to assess therapist generational status and acculturation, including cultural identity and language use. Generational status was assessed by asking therapists to identify whether they, their parents, and their grandparents were born in the US. Therapists who reported being born in another country specified their birth country as well as how many years they have lived in the US.
Cultural identity items were adapted from the Abbreviated Multidimensional Acculturation Scale (AMAS-ZABB; Zea, Asner-Self, Birman, & Buki, 2003), which was developed to assess acculturation in a Latino sample. The original AMAS-ZABB yielded a total US acculturation scale and a total Latino/Latina acculturation scale. Each total acculturation scale was composed of three subscales: Cultural identity, English/Spanish language, and cultural competence. The current study included three items from the original 6-item cultural identity subscale, and items were adapted to capture therapists’ culture of origin beyond Latino culture (i.e., “I feel good about being a member of my culture of origin;” “Being a member of my culture of origin plays an important part in my life;” “I have a strong sense of being a member of my culture of origin”). Therapists who come from a multicultural family reported on the culture of origin they related to most. Therapists rated items on a 4-point Likert-type scale (1 = strongly disagree, 4 = strongly agree). Two composite scores (possible range: 1–4) were calculated from the mean of items for Heritage Cultural Identity and US American Identity, with higher scores representing stronger feelings of identification with a particular culture. These scales demonstrated acceptable internal consistency in the current sample, with Cronbach’s alpha of α=.85 for the Heritage Cultural Identity scale and α=.87 for the US American Identity scale.
Language use items were adapted from the Adolescents Coping with Everyday Stress study (Lau et al., 2016). Three items captured language competency (e.g., “How well do you speak and understand this language?”), and two items captured frequency of language use (e.g., “How often to you speak this language with your friends?”). All therapists completed these language use items on their use of English. In addition, therapists who indicated that they spoke a heritage language other than English completed the same items concerning that language. Therapists who spoke more than one language other than English reported on the language they used most frequently. Therapists rated items on a 4-point Likert-type scale (1= not at all or never, 4 = extremely well or most of the time). Therapists who reported not speaking a heritage language were coded to receive 1’s on all items of the heritage language use scale. Two mean composite scores (possible range: 1–4) were generated for Heritage Language Use and English Language Use, with higher scores representing greater language use. The Cronbach’s alpha indicated that the internal consistency was excellent for the Heritage Language Use scale (α =.94) and acceptable for the English Language Use scale (α =.64).
Adaptations to Evidence-Based Practices Scale (AES; Lau et al., 2017)
The AES is a six-item self-report measure to assess adaptations therapists report making to EBPs. Items were developed for the AES questionnaire based on a framework of EBP modifications (Stirman et al., 2015). The six items related to: 1) modifying the presentation, 2) shortening or condensing the pacing of the practice, 3) lengthening or extending the pacing of the practice, 4) integrating supplemental content or strategies, 5) removing or skipping components, and 6) adjusting the order of sessions or components. Therapists completed the AES for every EBP that they reported using within the past two months. Using a 5-point Likert-type scale (0 = not at all, 4 = a very great extent), therapists indicated the extent to which they used the adaptation when delivering a specified EBP. A multi-level confirmatory factor analysis, which took into account that therapists reported on multiple EBPs, revealed that the AES had good model fit (CFI = .96, RMSEA = .06) for two factors that represented two types of adaptations: Augmenting and Reducing/Reordering (Lau et al., 2017). The Augmenting adaptation scale characterized adaptations that effectively added to the EBP (i.e., tailoring presentation, integrating supplemental content, lengthening the pacing), while the Reducing/Reordering adaptations involved omitting or re-arranging components. The Cronbach’s alpha for the current study indicated that the internal consistency was acceptable for the Augmenting adaptations scale (α=.75) and for the Reducing/Reordering adaptations scale (α=.71).
Perceived Characteristics of Intervention Scale (PCIS; Cook, Thompson, & Schnurr, 2015)
The PCIS was developed to allow for the comparison of therapist perceptions of different EBPs. In the original PCIS, 10, 2-item scales were developed to measure the theory-based model of 10 perceived characteristics of innovation (Rogers, 1962; Rogers, 2003), though psychometric properties indicated that the scale measured a unidimensional construct of attitudes (Cook et al., 2015). To reduce measurement fatigue given the repeated nature of this measure, we administered four complete scales of the original PCIS, including Relative Advantage (e.g., “[EBP] is more effective than other therapies I have used.”), Compatibility (e.g., “[EBP] is aligned with my clinical judgment.”), Complexity (e.g., “[EBP] is easy to use.”), and Potential for Reinvention (e.g., “[EBP] can be adapted to meet the needs of my patients.”). Therapists rated each item on a 5-point Likert-type scale (1 = not at all, 5 = a very great extent). In the current study, the 8-item scale had excellent internal consistency (α =.93), so consistent with scoring of the original PCIS, a composite mean score was used to measure therapists’ perceptions of each practice. In the analyses of the current data, therapists’ perceptions of a given practice was used as a level 1 predictor of reported adaptations to that same practice.
Data Analysis
Two sets of multilevel models were run to assess practice- and therapist-level predictors of therapist reports of Augmenting and Reducing/Reordering adaptations. Intraclass correlation coefficients (ICC) of null models were used assess the variance in outcomes at the therapist and agency level. Therapist accounted for 48.24% to 69.08% of the variance in adaptations and agency accounted for 0.04% to 2.14% of the variance in adaptations. Because clustering was minimal at the agency level, two-level models with EBPs nested within therapists were conducted to predict the extensiveness of each type of adaptation (Hayes, 2006). One set of models included language acculturation and therapist characteristics as predictors of either Augmenting or Reducing/Reordering adaptations, while the other set of models included identity-based acculturation and therapist characteristics as predictors. The language acculturation (i.e., Heritage Language Use, English Language Use) and identity-based acculturation (i.e., Heritage Cultural Identity, US American Identity) scales were grand mean-centered to examine interaction effects. A third exploratory model was run to examine the interaction of Heritage Language Use X Heritage Cultural Identity, to assess whether Heritage Cultural Identity moderated the relationship between Heritage Language Use and reported adaptations.
African American participants (n = 22) were excluded from the analyses examining language acculturation, as the majority of our African American participants (86.4%) did not report speaking a language other than English. Furthermore, acculturation scales for African Americans have tended to omit language use items due to limited relevance of heritage language use to racial and ethnic identity in this population (Snowden & Hines, 1999).
In each model, the EBP delivered and therapist attitudes towards each specific EBP (i.e., PCIS score) were included as level 1 predictors to test if the type of adaptation (i.e., Augmenting or Reducing/Reordering) varied significantly by practice and attitudes. Level 2 predictors included therapist characteristics, including: gender, race/ethnicity (Hispanic/Latino, Other Ethnic Minority), age, generational status, and identity-based acculturation level or language acculturation level. See Table 2 for descriptive statistics of study variables.
Table 2.
Descriptive Statistics of Study Variables
| Predictor | Mean (SD) or n (%) |
|---|---|
| Level 1 Predictors | |
| Practice | |
| CBITS | 3 (0.7%) |
| CPP | 41 (9.2%) |
| MAP | 155 (34.8%) |
| Seeking Safety | 78 (17.5%) |
| TF-CBT | 133 (29.9%) |
| Triple P | 35 (7.9%) |
| Practice-Specific PCIS | 29.81 (range: 27.61 – 34.33) |
| Level 2 Predictors | |
| Age | 34.82 (8.05) |
| Gender | |
| Male | 33 (14.0%) |
| Female | 202 (86.0%) |
| Race/Ethnicity | |
| Hispanic/ Latino | 160 (68.1%) |
| Other Ethnic Minority | 75 (31.9%) |
| Generational Status | |
| 1st Generation | 53 (22.6%) |
| 2nd Generation | 135 (57.4%) |
| 3rd Generation & Above | 47 (20.0%) |
| Heritage Cultural Identity | 3.63 (.53) |
| US American Identity | 3.64 (.51) |
| Heritage Language Use | 2.77 (1.00) |
| English Language Use | 3.86 (.26) |
| Dependent Variables | |
| Augmenting Adaptations | 2.22 (.93) |
| Reducing / Reordering Adaptations | 1.16 (.86) |
Results
Practice-Level Predictors
Given that separate models were run for language and identity-based acculturation, there were slight differences in the predictive values of practice-level variables. See Tables 3 and 4 for summaries of predictors and omnibus tests of fixed effects. Augmenting adaptations did not significantly differ by EBP, but EBP was significantly associated with Reducing/Reordering adaptations in both models. In particular, therapists reported making more Reducing/Reordering adaptations to SS, CPP, TF-CBT, and Triple P, compared with the reference group (MAP). Therapists’ attitudes towards EBPs did not have a significant effect on Augmenting adaptations. However, EBP-specific perceptions were significantly associated with Reducing/Reordering adaptations in both models. Therapists who perceived an EBP more positively reported fewer Reducing/Reordering adaptations.
Table 3.
Unstandardized estimates of effects of predictors of therapist-reported adaptations: Identity-based acculturation model (N=235)
| Augmenting Adaptations | Reducing/Reordering Adaptations | |||||
|---|---|---|---|---|---|---|
| Predictor | F | Estimate | SE | F | Estimate | SE |
| Intercept | 72.39*** | 3.06*** | .39 | 59.62*** | 2.78*** | .34 |
| Level 1 Predictors | ||||||
| Practicea | 0.37 | 15.15*** | ||||
| CBITS | – | .21 | .37 | – | −.50 | .35 |
| CPP | – | −.11 | .11 | – | −.45*** | .11 |
| Seeking Safety | – | −.01 | .09 | – | .33*** | .08 |
| TF-CBT | – | −.06 | .07 | – | −.33*** | .07 |
| Triple P | – | −.05 | .12 | – | −.31** | .11 |
| Practice-Specific PCIS | 0.03 | .00 | .01 | 28.87*** | −.03*** | .01 |
| Level 2 Predictors | ||||||
| Age | 6.87** | −.02** | .01 | 2.46 | −.01 | .01 |
| Gender (Female) | 0.36 | −.10 | .17 | 3.99* | −.29* | .14 |
| Race/Ethnicity (Hispanic/Latino) | 1.06 | .13 | .13 | 0.14 | −.04 | .11 |
| Generational Statusb | 0.91 | 0.31 | ||||
| 2nd Generation | – | −.13 | .14 | – | −.004 | .12 |
| 3rd Generation & Above | – | −.23 | .17 | – | −.10 | .15 |
| Heritage Cultural Identity | 0.01 | .01 | .12 | 0.00 | −.01 | .10 |
| US American Identity | 0.37 | −.07 | .12 | 0.68 | .09 | .10 |
| Heritage Cultural Identity X US American Identity | 0.13 | .05 | .13 | 5.51* | .26* | .11 |
=p<.10,
=p<.05,
=p<.01,
=p<.001
MAP is reference group,
1st Generation is reference group
Table 4.
Unstandardized estimates of effects of predictors of therapist-reported adaptations: Language-based acculturation model (n=213)
| Augmenting Adaptations | Reducing/Reordering Adaptations | |||||
|---|---|---|---|---|---|---|
| Predictor | F | Estimate | SE | F | Estimate | SE |
| Intercept | 51.76*** | 2.80*** | .43 | 319.83*** | 2.41*** | .37 |
| Level 1 Predictors | ||||||
| Practicea | 0.22 | 13.46*** | ||||
| CBITS | – | .20 | .38 | – | −.51 | .36 |
| CPP | – | −.09 | .12 | – | −.42*** | .12 |
| Seeking Safety | – | −.02 | .09 | – | .34*** | .09 |
| TF-CBT | – | −.04 | .08 | – | −.32*** | .08 |
| Triple P | – | −.05 | .13 | – | −.30* | .12 |
| Practice-Specific PCIS | 0.01 | .00 | .01 | 25.76*** | −.03*** | .01 |
| Level 2 Predictors | ||||||
| Age | 4.49* | −.02* | .01 | 0.64 | −.01 | .01 |
| Gender (Female) | 0.08 | −.05 | .17 | 2.03 | −.21 | .15 |
| Race/Ethnicity (Hispanic/Latino) | 1.84 | .21 | .15 | 0.29 | .08 | .13 |
| Generational Statusb | 1.14 | 1.11 | ||||
| 2nd Generation | – | −.07 | .15 | – | .05 | .13 |
| 3rd Generation & Above | – | −.32 | .22 | – | −.19 | .19 |
| Heritage Language Use | 0.07 | −.03 | .10 | 0.14 | −.03 | .08 |
| English Language Use | 2.01 | .51 | .36 | 1.01 | .31 | .31 |
| Heritage Language Use X English Language Use | 3.10+ | −.88+ | .50 | 2.95+ | −.73+ | .43 |
=p<.10,
=p<.05,
=p<.01,
=p<.001
MAP is reference group,
1st Generation is reference group
Therapist-Level Predictors
Therapist-level background characteristics included gender, age, ethnicity (Hispanic/Latino or Other Race/Ethnicity), and generational status. As shown in Tables 3 and 4, age significantly predicted Augmenting adaptations, as older therapists reported fewer Augmenting adaptations. Therapist gender significantly predicted Reducing/Reordering adaptations in the identity-based model, F(1, 224.75) = 3.99, p = .047. In particular, female therapists reported making fewer Reducing/Reordering adaptations than male therapists, Estimate = −.29, SE = .14, p = .047. No other therapist background characteristics significantly predicted therapist-reported Augmenting or Reducing/Reordering adaptations. There were no significant main effects of identity-based or language-based acculturation variables on therapist-reported Augmenting adaptations in the main models. There was a significant interaction between therapist’s heritage cultural identity and US American identity in predicting Reducing/Reordering adaptations, F(1, 265.11) = 5.51, p = .02 (see Figure 1).
Figure 1.
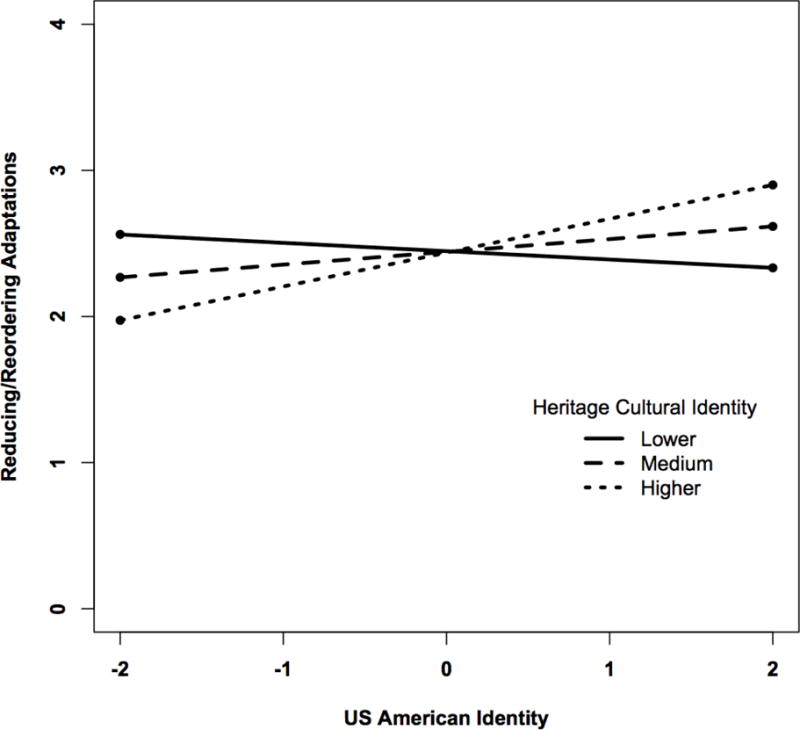
Heritage Cultural Identity X US American Identity Interaction Predicting Reducing/Reordering Adaptations
Heritage Cultural Identity as a Moderator
An exploratory interaction model was run to examine the effect of heritage cultural identity on the relationship between therapists’ heritage language use and reported adaptations. As shown in Table 5, there was a significant interaction between heritage language use and heritage cultural identity in predicting Augmenting adaptations, F(1, 209.91) = 4.70, p = .031 (see Figure 2). There was no significant interaction effect on Reducing/Reordering adaptations, F(1, 201.35) = 1.96, p = .163.
Table 5.
Unstandardized estimates of effects of predictors of therapist-reported adaptations: Language-based acculturation model with heritage cultural identity as a moderator (n=213)
| Augmenting Adaptations | Reducing/Reordering Adaptations | |||||
|---|---|---|---|---|---|---|
| Predictor | F | Estimate | SE | F | Estimate | SE |
| Intercept | 318.03*** | 2.99*** | .42 | 320.13*** | 2.54*** | .37 |
| Level 1 Predictors | ||||||
| Practicea | 0.24 | 13.42*** | ||||
| CBITS | – | .22 | .38 | – | −.50 | .36 |
| CPP | – | −.10 | .12 | – | −.42*** | .11 |
| Seeking Safety | – | −.03 | .09 | – | .34*** | .09 |
| TF-CBT | – | −.04 | .08 | – | −.33*** | .08 |
| Triple P | – | −.05 | .13 | – | −.29* | .12 |
| Practice-Specific PCIS | 0.05 | .00 | .01 | 24.22*** | −.03*** | .01 |
| Level 2 Predictors | ||||||
| Age | 5.26* | −.02* | .01 | 0.91 | −.01 | .01 |
| Gender (Female) | 0.05 | −.04 | .17 | 1.48 | −.18 | .15 |
| Race/Ethnicity (Hispanic/Latino) | 2.04 | .22 | .15 | 0.29 | .07 | .13 |
| Generational Statusb | 1.41 | 0.94 | ||||
| 2nd Generation | – | −.16 | .15 | – | −.02 | .13 |
| 3rd Generation & Above | – | −.37+ | .22 | – | −.23 | .19 |
| Heritage Language Use | 1.70 | −.12 | .09 | 2.53 | −.12 | .08 |
| English Language Use | 0.00 | .02 | .24 | 0.25 | −.10 | .20 |
| Heritage Cultural Identity | 0.38 | −.08 | .12 | 1.13 | −.11 | .11 |
| Heritage Language Use X Heritage Cultural Identity | 4.70* | −.24* | .11 | 1.96 | −.13 | .10 |
=p<.10,
=p<.05,
=p<.01,
=p<.001
MAP is reference group,
1st Generation is reference group
Figure 2.
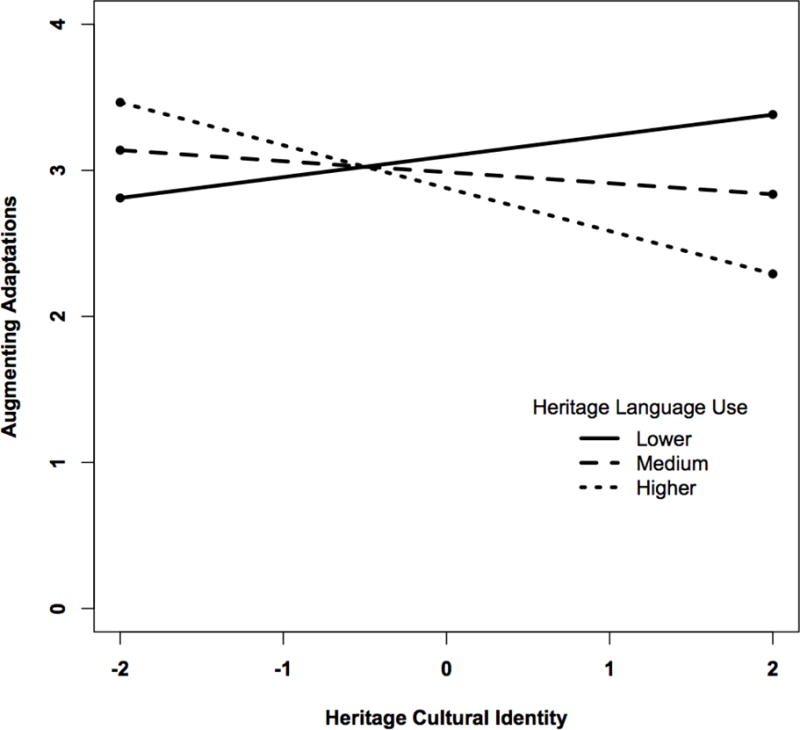
Heritage Language Use X Heritage Cultural Identity Interaction Predicting Augmenting Adaptations
Discussion
This study investigated the role of cultural identity in the adaptations that therapist reported making to multiple EBPs delivered in diverse, community settings. Understanding how ethnic and racial minority therapists adapt EBPs is important, as adaptations have the potential to improve client engagement, but could also indicate risk of drift away from fidelity (Lau, 2012; Stirman et al., 2013). It is important to note that while studies on different types of adaptations have characterized particular types of adaptations as maintaining or compromising fidelity to interventions (Stirman et al., 2015), EBPs differ in the flexibility they allow for therapist adaptations. More research is needed to understand types of adaptations and their impact on fidelity across different EBPs. This study expanded upon past research, suggesting that ethnic minority therapists may wish to make adaptations to EBPs when serving culturally diverse clients (Aisenberg, 2008; Bernal & Scharrón-del-Río, 2001; Cabassa & Baumann, 2013; Lau et al., 2017). Given the heterogeneity within and between ethnic minority therapists, we specifically examined whether therapist cultural factors, such as acculturation, were associated with reported adaptations in community-based delivery of EBPs.
Dimensions of cultural identity predicted the extent to which therapists reported Augmenting adaptations. As depicted in Figure 1, the effect of heritage cultural identity on Augmenting adaptations was moderated by heritage language use. Therapists who reported higher levels of affiliation with their heritage culture and higher levels of heritage language use reported the fewest Augmenting adaptations. On the other hand, therapists who reported higher levels of affiliation with their heritage culture and lower levels of heritage language use, or lower levels of affiliation with their heritage culture and higher levels of heritage language use, reported the most Augmenting adaptations. These findings suggests that therapists who are higher on both heritage cultural identity and heritage language use may be more likely to only use language to tailor treatment and not feel the need to augment treatment in other ways. Meanwhile, therapists with lower heritage language use but higher heritage cultural identity may find other ways to tailor EBPs beyond language translation.
Augmenting adaptations were the most commonly reported type of adaptation, including tailoring language and framing of interventions, introducing complementary activities, and lengthening treatment for more skill practice. These types of adaptations have been frequently included in researcher-developed cultural adaptations of EBPs (BigFoot & Schmidt, 2010; Domenech Rodríguez et al., 2011; Lau, 2012). Indeed, our results suggest that community therapists making adaptations consistent with those promoted in the literature on cultural adaptations, are much less likely to engage in adaptations that remove core content or decrease dose in ways that may compromise EBP integrity when working with diverse clients (Lau et al., 2017; Koslofsky & Domenech Rodríguez, 2017).
Cultural orientations, however, were related to Reducing/Reordering adaptations. Therapists who reported higher levels of affiliation with their heritage culture and lower levels of affiliation with US culture (i.e., separated) reported the fewest adaptations that reduce or rearrange EBP content, whereas therapists who reported higher levels of affiliation with both their heritage culture and US culture (i.e., integrated) reported making the most adaptations that reduce or rearrange EBP content, which may represent drift. As depicted in Figure 1, US acculturation seemed to have minimal associations with adaptations for therapists with lower levels of heritage cultural identity. Although this finding was not expected, it may be that highly enculturated ethnic minority therapists may be most adherent to their EBP training, but more bicultural therapists may be most vigilant to the ways that western-developed EBPs may be out of alignment with ethnic values and norms. Previous studies in which therapists have noted hesitance about teaching certain culturally unfamiliar skills to immigrant clients (Lau, 2012) may have included more bicultural therapists. It is worth noting that community therapists’ concerns about the culturally appropriateness of EBPs have at times not been shared by community consumers of EBPs (Lau, 2012). Some research has suggested that less acculturated Latino caregivers show higher levels of engagement and persistence in community mental health clinics delivering EBPs (Kim, Lau, & Chorpita, 2016). Further research is needed to understand how therapist cultural orientations impact their delivery of EBPs.
Language acculturation and other cultural factors such as ethnicity and generational status did not predict either Augmenting or Reducing/Reordering adaptations. Although this study only included ethnic minority therapists, in another study, Latino therapists reported making more Augmenting adaptations than NHW therapists (Lau et al., 2017).
In regard to therapist-level predictors of adaptations, therapist age significantly predicted Augmenting adaptations while therapist gender significantly predicted Reducing/Reordering adaptations. Older therapists reported making significantly fewer Augmenting adaptations. This is consistent with the finding in the larger study sample that therapists with more years of professional therapy experience reported making significantly fewer Augmenting adaptations (Lau et al., 2017). Younger therapists may be more willing to adapt treatment to respond to clients’ needs, or alternatively, younger therapists may augment EBPs in ways that relate to their own anxieties about being a novice clinician. It is still unclear whether the augmentations made by beginning therapists improve the fit of EBPs for clients, or whether they may actually compromise EBP fidelity.
In regards to practice-level predictors, therapists who reported more favorable perceptions of the EBP reported making fewer Reducing/Reordering adaptations. This supports past studies (Lau et al., 2017) and reflects the rational expectation that therapists are more likely to maintain integrity to interventions that they find appealing and useful. Furthermore, therapists reported making more Reducing/Reordering adaptations for MAP and SS, which is reasonable as these EBPs do not have session-by-session prescribed content, but rather allow therapists to choose the skills and content to cover, as well as the order in which content is covered.
Limitations
It is important to acknowledge several limitations of this study. First, although this study includes a racially and ethnically diverse sample of therapists, the generalizability is limited by the cultural groups represented and the fact that many participants rated themselves as having high levels of both heritage culture and US American identities, suggesting that therapists in this context frequently identified as having a bicultural identity. As such, this sample may not be representative of groups with less biculturalism, different geographical regions within the US or country of origin populations. Additionally, because our sample consisted primarily of Hispanic/Latino and Asian/Pacific Islander therapists, and African American therapists were excluded from the language models, generalization of findings to other racial/ethnic groups should be made with caution. It is unclear whether our findings concerning the cultural factors in therapist reported adaptations may generalize to implementation contexts not shaped by a system-driven reform involving reimbursement for EBP delivery. It is possible that ethnic minority therapists in community contexts where EBP adoption is individually determined may feel more discretion to freely to adapt interventions, and cultural orientation may play a larger role in their implementation. Further research in community EBP implementation among diverse therapists is warranted. Given that the majority of therapists in our sample were unlicensed, generalizations to more experienced workforces should be made with caution. Finally, generalization of findings is also limited due to the fact that this study focused on children’s mental health services and did not examine adult populations. Another limitation is the fact that data were collected through self-report measures. It would be important to validate therapist reports of adaptations with observer ratings of intervention fidelity. The final limitation of the current study is the lack of information regarding therapist training (e.g., length of EBP training received, time from training to data collection) and the types of fidelity monitoring used, as these factors may impact the likelihood and types of adaptations that community therapists make. Further, therapists are most likely to deliver EBPs with fidelity when provided with implementation supports, including coaching and consultation (Beidas, Edmunds, Marcus, & Kendall, 2012). Ethnic minority therapists serving diverse clients may particularly benefit from culturally competent consultation or participation in learning collaboratives with peers and experts familiar with their communities and service setting contexts.
Notwithstanding these limitations, this study addressed an important question regarding the role cultural identity plays in how ethnic minority therapists deliver EBPs. This study has several strengths. First, the unique context of the study allowed for the investigation of how multiple EBPs are delivered by a large and diverse group of therapists serving predominately ethnic minority clients. This was one of the first studies that looked specifically at cultural identity as a factor that could impact implementation outcomes in an increasingly diverse workforce serving largely ethnic minority communities. This is an important area to address, as findings have been mixed regarding how ethnic minority therapists perceive and deliver EBPs (Aarons et al., 2010; Barnett et al., 2017; Lau et al., 2017; Southam-Gerow et al., 2012).
Future Directions
Given the study limitations, future research should examine the role of therapist cultural identity on EBP implementation among a geographically diverse sample. Additionally, therapist cultural identity should be more closely examined among different ethnic groups to assess intraracial diversity in EBP delivery. Attention to how therapist cultural identity impacts EBP delivery may be important to consider in future implementation efforts, as our findings suggest that there are likely differences within ethnic and racial minority groups in regards to the ways in which EBPs are adapted and delivered. Future research should also examine the implications of these adaptations for client outcomes.
Contributor Information
Dana Saifan, University of California, Los Angeles.
Lauren Brookman-Frazee, University of California, San Diego.
Miya Barnett, University of California, Santa Barbara.
Juan Carlos Gonzalez, University of California, Santa Barbara.
Anna S. Lau, University of California, Los Angeles
References
- Aarons GA, Glisson C, Hoagwood K, Kelleher K, Landsverk J, Cafri G. “Psychometric properties and U.S. national norms of the Evidence-Based Practice Attitude Scale (EBPAS)”: Correction to Aarons et al. (2010) Psychological Assessment. 2010;22(3):701–701. doi: 10.1037/a0021103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Green AE, Palinkas LA, Self-Brown S, Whitaker DJ, Lutzker JR, Chaffin MJ. Dynamic adaptation process to implement an evidence-based child maltreatment intervention. Implementation Science. 2012;7(1):32. doi: 10.1186/1748-5908-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aisenberg E. Evidence-based practice in mental health care to ethnic minority communities: Has its practice fallen short of its evidence? Social Work. 2008;53(4):297–306. doi: 10.1093/sw/53.4.297. [DOI] [PubMed] [Google Scholar]
- Alegria M, Shrout PE, Woo M, Guarnaccia P, Sribney W, Vila D, Canino G. Understanding differences in past year psychiatric disorders for Latinos living in the US. Social Science and Medicine. 2007;65(2):214–230. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett M, Brookman-Frazee L, Regan J, Saifan D, Stadnick N, Lau AS. How intervention and implementation characteristics relate to community therapists’ attitudes toward evidence-based practices: A mixed methods study. Administration and Policy in Mental Health and Mental Health Services Research. 2017;0(0):1–14. doi: 10.1007/s10488-017-0795-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumann AA, Cabassa LJ, Stirman SW. Adaptation in dissemination and implementation science. In: Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and implementation research in health: Translating science to practice. New York, NY: Oxford University Press; 2017. p. 285. [Google Scholar]
- Bean RA, Perry BJ, Bedell TM. Developing culturally competent marriage and family therapists: guidelines for working with Hispanic families. Journal of Marital and Family Therapy. 2001;27(1):43–54. doi: 10.1111/j.1752–0606.2001.tb01138.x. [DOI] [PubMed] [Google Scholar]
- Beidas RS, Edmunds JM, Marcus SC, Kendall PC. Training and consultation to promote implementation of an empirically supported treatment: A randomized trial. Psychiatric Services. 2012;63(7):660–665. doi: 10.1176/appi.ps.201100401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger LK, Zane N, Hwang WC. Therapist ethnicity and treatment orientation differences in multicultural counseling competencies. Asian American Journal of Psychology. 2014;5(1):53–65. doi: 10.1037/a0036178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernal G, Domenech Rodríguez MM. In: Cultural adaptations: Tools for evidence-based practice with diverse populations. Bernal G, Domenech Rodríguez MM, editors. Washington, DC: American Psychological Association; 2012. [DOI] [Google Scholar]
- Bernal G, Scharrón-del-Río MR. Are empirically supported treatments valid for ethnic minorities? Toward an alternative approach for treatment research. Cultural Diversity & Ethnic Minority Psychology. 2001;7(4):328–342. doi: 10.1037//1099-9809.7.4.328. [DOI] [PubMed] [Google Scholar]
- Berry JW. Immigration, acculturation, and adaptation. Applied Psychology. 1997;46(1):5–34. doi: 10.1080/026999497378467. [DOI] [Google Scholar]
- BigFoot DS, Schmidt SR. Honoring children, mending the circle: Cultural adaptation of trauma-focused cognitive-behavioral therapy for american indian and alaska native children. Journal of Clinical Psychology. 2010;66(8):847–856. doi: 10.1002/jclp.20707. [DOI] [PubMed] [Google Scholar]
- Brookman-Frazee LI, Drahota A, Stadnick N. Training community mental health therapists to deliver a package of evidence-based practice strategies for school-age children with autism spectrum disorders: A pilot study. Journal of Autism and Developmental Disorders. 2012;42(8):1651–1661. doi: 10.1007/s10803-011-1406-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabassa LJ, Baumann AA. A two-way street: bridging implementation science and cultural adaptations of mental health treatments. Implementation Science. 2013;8(1):90. doi: 10.1186/1748-5908-8-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaffin M, Silovsky JF, Funderburk B, Valle LA, Brestan EV, Balachova T, Bonner BL. Parent-child interaction therapy with physically abusive parents: Efficacy for reducing future abuse reports. Journal of Consulting and Clinical Psychology. 2004;72(3):500–510. doi: 10.1037/0022–006X.72.3.500. [DOI] [PubMed] [Google Scholar]
- Chambers DA, Norton WE. The adaptome: Advancing the science of intervention adaptation. American Journal of Preventive Medicine. 2016;51(4):S124–S131. doi: 10.1016/j.amepre.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comas-Diaz L, Griffith EEH, editors. Clinical guidelines in cross-cultural mental health. Oxford: John Wiley & Sons; 1988. [Google Scholar]
- Cook JM, Thompson R, Schnurr PP. Perceived Characteristics of Intervention Scale. Assessment. 2015;22(6):704–714. doi: 10.1177/1073191114561254. [DOI] [PubMed] [Google Scholar]
- Cooper JL, Aratani Y, Knitzer J, Douglas-Hall A, Masi R, Banghart PL, Dababnah S. Unclaimed children revisited: The status of children’s mental health policy in the United States. Columbia University Academic Commons. New York, NY: 2008. Retrieved from http://hdl.handle.net/10022/AC:P:8917. [Google Scholar]
- Corral I, Landrine H. Acculturation and ethnic-minority health behavior: A test of the operant model. Health Psychology. 2008;27(6):737–745. doi: 10.1037/0278-6133.27.6.737. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, Jacobson NS. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74(4):658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Domenech Rodríguez MM, Baumann AA, Schwartz AL. Cultural adaptation of an evidence based intervention: From theory to practice in a Latino/a community context. American Journal of Community Psychology. 2011;47(1):170–186. doi: 10.1007/s10464-010-9371-4. [DOI] [PubMed] [Google Scholar]
- Garcia JG, Zea MC. Psychological interventions and research with latino populations. Needham Heights, MA: Allyn & Bacon; 1997. [Google Scholar]
- Gardner F, Montgomery P, Knerr W. Transporting evidence-based parenting programs for child problem behavior (age 3–10) between countries: Systematic review and meta-analysis. Journal of Clinical Child and Adolescent Psychology. 2016;45(6):749–762. doi: 10.1080/15374416.2015.1015134. [DOI] [PubMed] [Google Scholar]
- Hall GCN, Ibaraki AY, Huang ER, Marti CN, Stice E. A meta-analysis of cultural adaptations of psychological interventions. Behavior Therapy. 2016;47(6):993–1014. doi: 10.1016/j.beth.2016.09.005. [DOI] [PubMed] [Google Scholar]
- Huey SJ, Polo AJ. Evidence-based psychosocial treatments for ethnic minority youth. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):262–301. doi: 10.1080/15374410701820174. https://doi.org/Doi10.1080/15374410701820174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapasi Z, Melluish S. Language switching by bilingual therapists and its impact on the therapeutic alliance within psychological therapy with bilingual clients: a systematic review. International Journal of Culture and Mental Health. 2015;8(4):458–477. doi: 10.1080/17542863.2015.1041994. [DOI] [Google Scholar]
- Kim RE, Lau AS, Chorpita BF. The impact of Latino caregiver acculturation on treatment engagement in children’s community mental health services. Journal of Child and Family Studies. 2016;25(3):891–901. doi: 10.1007/s10826-015-0259-7. [DOI] [Google Scholar]
- Koslofsky S, Domenech Rodriguez MM. Cultural adaptations to psychotherapy: Real-world applications. Clinical Case Studies. 2017 doi: 10.1177/1534650116668273. [DOI]
- Kumpfer KL, Alvarado R, Smith P, Bellamy N. Cultural sensitivity and adaptation in family-based prevention interventions. Prevention Science. 2002 doi: 10.1023/A:1019902902119. [DOI] [PubMed]
- Lau AS. Making the case for selective and directed cultural adaptations of evidence-based treatments: Examples from parent training. Clinical Psychology: Science and Practice. 2006 doi: 10.1111/j.1468-2850.2006.00042.x. [DOI]
- Lau AS. Reflections on adapting parent training for Chinese immigrants: Blind alleys, thoroughfares, and test drives. In: Bernal G, Domenech Rodríguez MM, editors. Cultural adaptations: Tools for evidence-based practice with diverse populations. Washington, DC: American Psychological Association; 2012. pp. 133–156. [Google Scholar]
- Lau AS, Barnett M, Stadnick N, Saifan D, Regan J, Wiltsey Stirman S, Brookman-Frazee L. Therapist report of adaptations to delivery of evidence-based practices within a system-driven reform of publicly funded children’s mental health services. Journal of Consulting and Clinical Psychology. 2017;85(7):664–675. doi: 10.1037/ccp0000215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau AS, Brookman-Frazee L. The 4KEEPS study: identifying predictors of sustainment of multiple practices fiscally mandated in children’s mental health services. Implementation Science. 2016;11(1):31. doi: 10.1186/s13012-016-0388-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau AS, Fung JJ, Ho LY, Liu LL, Gudiño OG. Parent training with high-risk immigrant chinese families: A pilot group randomized trial yielding practice-based evidence. Behavior Therapy. 2011;42(3):413–426. doi: 10.1016/j.beth.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau AS, Guo S, Tsai W, Nguyen DJ, Nguyen HT, Ngo V, Weiss B. Adolescents’ stigma attitudes toward internalizing and externalizing disorders: Cultural influences and implications for distress manifestations. Clinical Psychological Science. 2016;4(4):704–717. doi: 10.1177/2167702616646314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee LC, Zane NW. Handbook of asian american psychology. Thousand Oaks, CA: SAGE Publications; 1998. [Google Scholar]
- Lin L, Nigrinis A, Christidis P, Stamm K. Demographics of the US psychology workforce: Findings from the American Community Survey American Psychological Association 2015 [Google Scholar]
- Masgoret AM, Ward C. Culture learning approach to acculturation. In: Sam DL, Berry JW, editors. The Cambridge Handbook of Acculturation Psychology. Cambridge, United Kingdom: Cambridge University Press; 2006. pp. 58–77. [Google Scholar]
- Nilsson JE, Anderson MZ. Supervising international students: The role of acculturation, role ambiguity, and multicultural discussions. Professional Psychology: Research and Practice. 2004;35(3):306–312. doi: 10.1037/0735-7028.35.3.306. [DOI] [Google Scholar]
- Padilla AM, Salgado DS. Counseling hispanics: Strategies for effective intervention. In: Pedersen P, editor. Handbook of Cross-cultural Counseling and Therapy. New York, NY: Greenwood Press Praeger Publishers; 1987. pp. 157–164. [Google Scholar]
- Regan J, Lau AS, Barnett M, Stadnick N, Hamilton A, Pesanti K, Brookman-Frazee L. Agency responses to a system-driven implementation of multiple evidence-based practices in children’s mental health services. BMC Health Services Research. 2017;17(1):671. doi: 10.1186/s12913-017-2613-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of innovations. The Free Press; New York, NY: 1962. [Google Scholar]
- Rogers EM. Diffusion of Innovations. 5th. New York, NY: Free Press; 2003. [Google Scholar]
- Sam DL, Berry JW. Acculturation: When individuals and groups of different cultural backgrounds meet. Perspectives on Psychological Science. 2010;5(4):472–481. doi: 10.1177/1745691610373075. [DOI] [PubMed] [Google Scholar]
- Schwartz SJ, Montgomery MJ, Briones E. The role of identity in acculturation among immigrant people: Theoretical propositions, empirical questions, and applied recommendations. Human Development. 2006;49(1):1–30. doi: 10.1159/000090300. [DOI] [Google Scholar]
- Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: Implications for theory and research. American Psychologist. 2010;65(4):237–251. doi: 10.1037/a0019330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snowden LR, Hines AM. A scale to assess African American acculturation. Journal of Black Psychology. 1999;25(1):36–47. doi: 10.1177/0095798499025001003. [DOI] [Google Scholar]
- Southam-Gerow MA, Rodríguez A, Chorpita BF, Daleiden EL. Dissemination and implementation of evidence based treatments for youth: Challenges and recommendations. Professional Psychology: Research and Practice. 2012;43(5):527–534. doi: 10.1037/a0029101. [DOI] [Google Scholar]
- Stirman SW, A Gutner C, Crits-Christoph P, Edmunds J, Evans AC, Beidas RS. Relationships between clinician-level attributes and fidelity-consistent and fidelity-inconsistent modifications to an evidence-based psychotherapy. Implementation Science. 2015;10(1):115. doi: 10.1186/s13012-015-0308-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stirman SW, Calloway A, Toder K, Miller CJ, DeVito AK, Meisel SN, Crits-Christoph P. Community mental health provider modifications to cognitive therapy: Implications for sustainability. Psychiatric Services. 2013;64(10):1056–1059. doi: 10.1176/appi.ps.201200456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sue DW, Sue D. Counseling the Culturally Diverse: Theory and Practice. 6th. 6th. Hoboken, NJ: John Wiley & Sons; 2012. Counseling the culturally diverse: Theory and practice. [Google Scholar]
- Sue S. Ethnicity and culture in psychological research and practice. In: Goodchilds J, editor. Psychological perspectives on human diversity in America. Washington, DC: American Psychological Association; 1991. pp. 51–85. [Google Scholar]
- U.S. Department of Health and Human Services. The Comprehensive Community Mental Health Services for Children with Serious Emotional Disturbances Program, Report to Congress. 2015 Retrieved from http://store.samhsa.gov/shin/content//PEP16-CMHI2015/PEP16-CMHI2015.pdf.
- van Mourik K, Crone MR, de Wolff MS, Reis R. Parent Training Programs for Ethnic Minorities: a Meta-analysis of Adaptations and Effect. Prevention Science. 2017:1–11. doi: 10.1007/s11121-016-0733-5. [DOI] [PMC free article] [PubMed]
- Zea MC, Asner-Self KK, Birman D, Buki LP. The Abbreviated Multidimentional Acculturation Scale: Empirical validation with two Latino/Latina samples. Cultural Diversity & Ethnic Minority Psychology. 2003;9(2):107–126. doi: 10.1037/1099-9809.9.2.107. [DOI] [PubMed] [Google Scholar]


