Abstract
Objective:
To present the results of a treatment development study designed to examine the feasibility, acceptability, and preliminary efficacy of motivational enhancement therapy (MET) for substance using, truant adolescents plus the Family Check-Up (FCU) for parents.
Method:
A randomized controlled trial was used to test the hypothesis that MET plus the FCU (MET/FCU) would lead to greater reductions in alcohol and marijuana use as well as truant behavior compared to a psychoeducation (PE) condition delivered to both adolescents and parents. Participants (n= 69; mean age 15.8 years) were 39% female, 59% white, and 31% Hispanic/Latino. Adolescents were referred from family court, school truancy courts, school counselors, or after presentations in high school health classes. Eligible participants reported using marijuana at least three times in the prior 90 days and a history of school truancy in the prior school year.
Results:
The MET/FCU condition was found to be feasible to implement and was acceptable to both adolescents and parents. The PE condition was also found to be an acceptable and credible comparison condition by participants. Results at the six month follow-up favored MET/FCU over PE on: days of marijuana use and number of times marijuana was smoked per day (medium effect); high volume drinking days and other drug use (small to medium effects); truancy indicators (small effects); and parental monitoring (medium to large effects); and parent-teen problem solving (medium to large effects).
Conclusions:
A larger study to test the efficacy of the MET/FCU appears warranted based on these promising findings.
Keywords: adolescents, substance use, truancy, parenting, brief interventions
Adolescence is a time of rapid personal development, which can bring greater opportunities to engage in problem behaviors (Steinberg et al., 2008) such as substance use and school truancy. According to the Social Development Model (SDM; Catalano & Hawkins, 1996), school bonding is a critical component to pro-social development. Therefore, students who are not well bonded to school are more likely to follow an antisocial and problematic developmental trajectory through adolescence. Indeed, school truancy is associated with both earlier initiation of substance use and higher levels of actual use (Henry, Knight, & Thornberry, 2012; Henry & Thornberry, 2010). Further, early initiation of substance use increases risk for poor school performance, school dropout, delinquency, and future substance use disorders (D’Amico, Ellickson, Collins, Martino, & Klein, 2005; Vaughn, Maynard, Salas-Wright, Perron, & Abdon, 2013)). Consequently, within this theoretical framework, truant youth engaging in substance use are an important target for early interventions.
According to SDM, parents and peers represent two of the most influential socialization units within an adolescent’s development. Research has consistently demonstrated that low levels of parental monitoring are related to early substance use (Jackson & Schulenberg, 2013). Poor parental monitoring also increases the likelihood of affiliation with deviant peers, which increases an adolescent’s opportunity to engage in substance use ((e.g., Van Ryzin, Fosco, & Dishion, 2012). Therefore, within the SDM framework, parental monitoring and supervision, as well as deviant peer affiliations, represent important elements to target during intervention.
Adolescents’ perception of rewards associated with substance use are strongly influenced by expectancies and perceived social norms, and thus represent another important focus of intervention. For instance, literature suggests that positive substance use expectancies, such as beneficial global changes, enhancement of social behavior, increased positive arousal, increased cognitive/motor abilities, increased relaxation, and increased tension reduction with use contribute to the initiation, frequency, and severity of substance use problems (Alfonso & Dunn, 2007). Further, distorted perceptions of peer substance use have also been associated with increased use of substances (Wu, Swartz, Brady, & Hoyle, 2015).
Interventions for Adolescent Substance Use and Truancy
Literature demonstrates that the effects of interventions targeting truancy are generally positive, with effects sizes in the small to moderate range (Maynard, Salas-Wright, Vaughn, & Peters, 2012). A comprehensive review of 16 truancy interventions including school-based, court-based, and community-based interventions, found that overall, interventions demonstrated a significant, though relatively modest, positive effect on attendance outcomes with an increase in school attendance of approximately five days (Maynard et al., 2012). However, with the exception of one intervention (Dembo et al., 2014), extant interventions only address truancy but no other factors that affect truancy, such as substance use, parenting, and peer affiliations.
According to the SDM (Catalano & Hawkins, 1996), multiple interventions may be needed when there are multiple direct and indirect pathways to problem behaviors. Motivational Enhancement Therapies (METs) represent one promising approach to addressing adolescent intrapersonal factors related to both substance use and truancy. METs are flexible, individual interventions delivered in a motivational interviewing (MI) style (Miller, 2000) consisting of both assessment and personalized feedback. A meta-analysis of 21 studies revealed a small, but significant, effect on alcohol or drugs for MI/MET with adolescents post treatment and at follow-up (Jensen et al, 2011). Another review found seven out of nine studies reporting reductions in marijuana following an MI/MET (Barnett, Sussman, Smith, Rohrback, & Spruijt-Metz, 2012).
Brief family based motivational interventions for adolescent substance use are less common than brief adolescent MI and MET interventions. One exception is the Family Check-up (FCU; Dishion, Nelson, & Kavanagh, 2003), a brief assessment and feedback intervention based on MET principles and that is designed to enhance parental recognition of youth risk behaviors, such as truancy and substance use, as well as motivation for reducing these problem behaviors and associated risk factors. The FCU is brief, which may increase the willingness of families with multiple stressors and time constraints to engage in the intervention. Further, providing individualized feedback using MI techniques may also increase the likelihood of parental participation. Dishion et al. (2003) found that substance use among 9th grade students was lower than a comparison group three years after receiving an FCU, and that the prevention effect of the FCU was mediated by changes in parental monitoring. In another study of adolescents (ages 13–17), who were treated in an urban hospital emergency department for an alcohol-related event (Spirito et al., 2011), the FCU, in combination with adolescent MET, was found to be superior to MET alone in reducing high-volume drinking at six months.
The current study was designed to test the feasibility and acceptability of a preventive intervention combining a parent-based FCU to address parenting and peer mechanisms associated with truancy and substance use; and an individual, adolescent MET to address adolescent mechanisms, such as expectancies and social norms. The intervention’s preliminary efficacy was examined in comparison to a parent and adolescent psychoeducation (PE) condition in a pilot, randomized control design. The sample consisted of truant adolescents, including those referred by truancy court programs, who had already begun to experiment with substances. Based on the literature suggesting the efficacy of MI/MET, as well as the influences highlighted by SDM on adolescent substance use, it was hypothesized that the MET/FCU condition would have significantly better short-term effects on marijuana and alcohol use than PE. Further, following Catalano and Hawkins (1996) advice to address multiple pathways of influence with multiple interventions, we integrated two motivational approaches to address truancy and substance use. Thus, we also hypothesized a significantly better effect on truancy in the MET/FCU condition than the PE condition. Because of its focus on parenting strategies, a hypothesized mechanism through which MET/FCU is expected to exert its effects, it was also hypothesized that the MET/FCU would have better effects on parental monitoring than PE.
Method
Participants
The sample consisted of 82 adolescents from a suburban/urban area of the Northeast, United States, recruited between August 2010 and April 2013 from family court, local school district truancy courts (a Family Court program in which a Magistrate monitors attendance), school attendance counselors, after presentations in high school health classes, and clinic advertisements. The proposed sample size (75) was consistent with the goals of National Institutes of Health (NIH) treatment development grants, and suitable to determine the experimental intervention’s feasibility and acceptability. Table 1 presents the demographic characteristics of the sample.
Table 1.
Demographics
| TEEN N=69 |
PARENT N=69 |
|||
|---|---|---|---|---|
| FCU n=34 |
PE n=35 |
FCU n=34 |
PE n=35 |
|
| Age: | ||||
| Mean (SD) | 15.7 (1.4) | 16.0 (1.2) | 41.3 (8.0) | 43.1 (8.6) |
| Gender: | ||||
| Female | 41.2% | 37.1% | 88.2% | 94.3% |
| Male | 58.8% | 62.9% | 11.8% | 5.7% |
| Race: | ||||
| White | 66.7% | 51.4% | 73.9% | 45.7% |
| Black | 19.0% | 28.6% | 13.0% | 22.9% |
| Native American | -- | -- | -- | -- |
| Asian | -- | -- | -- | -- |
| >1 Race | 14.3% | 20.0% | 13.0% | 8.6% |
| Hispanic: | 38.2% | 22.9% | 32.4% | 22.9% |
| Parent Incomea: | -- | -- | ||
| 0 to $25,999 | 40.6% | 57.4% | ||
| $26,000 to $49,999 | 31.3% | 18.8% | ||
| $50,000 or more | 28.1% | 18.8% | ||
| Parent Marital Status: | -- | -- | ||
| Single/Never Married | 35.3% | 25.7% | ||
| Living Together/ Married | 41.2% | 28.6% | ||
| Divorced/Widowed | 23.5% | 45.7% | ||
| Parent Highest Level of Educationb: | -- | -- | ||
| Some school prior to High School | 6.3% | 20% | ||
| High School/GED | 46.9% | 45% | ||
| 2YR/4YR College | 40.6% | 25% | ||
| >4YR College | 6.3% | 10% | ||
| Child Behavior Checklist | ||||
| Internalizing subscale | ||||
| Mean | 59.0 | 59.5 | ||
| SD | 11.4 | 10.7 | ||
| Externalizing subscale | ||||
| Mean | 65.2 | 64.8 | ||
| SD | 8.4 | 9.2 | ||
Six parents did not report Parent Income.
Three parents did not report Parent Education.
Note: There were no statistically significant differences between conditions on any of these variables.
Procedure
Potential participants were screened in person or by phone, to determine study eligibility. To be eligible, adolescents had to: 1) be between the ages of 13 and 18 years; 2) be living at home with a parent or legal guardian; 3) have used marijuana at least three times in the prior 90 days; and, 4) have a history of school truancy in the past school year, defined here as having at least 10 incidences of skipping classes, unexcused absences, and/or unexcused tardies, and/or involvement in truancy court. The marijuana inclusion criterion was set low in order to target adolescents whose substance use was more amenable to a brief family-based preventive intervention given that MET interventions are most appropriate for individuals who have not yet reached the severe end of the spectrum of a specific health risk behavior. The primary age range of our sample was chosen to recruit adolescents who were living at home, and thus likely to have parents still monitoring their child’s behavior. Further, in recognition of the importance of developmental transitions on adolescent problem behaviors highlighted in the SDM (Catalano & Hawkins, 1996), we also selected adolescents in the critical period just prior to the transition to emerging adulthood, when problem behaviors may become severe and engrained.
Adolescents with developmental or psychiatric disorders which rendered study procedures incomprehensible were ineligible to participate. Further, parents who were unable to speak and understand either English or Spanish sufficiently well to complete study procedures, were also ineligible. Once deemed eligible, parental consent and adolescent assent (consent for 18 year olds; n = 6) were obtained by research staff. Following consent, a 45 minute assessment battery was administered to the parent and adolescent; each received $50 at baseline as compensation for their time, and $75 for follow-ups. All procedures were approved by the university’s Institutional Review Board.
During the time of recruitment for the current study, two additional trials for adolescent substance use were also being conducted. A total of 662 telephone screens were conducted for all three trials. Of those eligible for the current trial (n = 182), 79 were lost to further contact and never received study details. Of the 103 families who received an explanation of the study, 82 (79.6%) were enrolled, including 11 for an initial open pilot trial (data not reported here). Of the 71 participants enrolled in the pilot RCT, two only partially completed their baseline assessment and were unable to be randomized. Therefore, 69 participants (97% of enrolled; See Figure 1) were randomized and included in the outcome data analysis.
Figure 1.
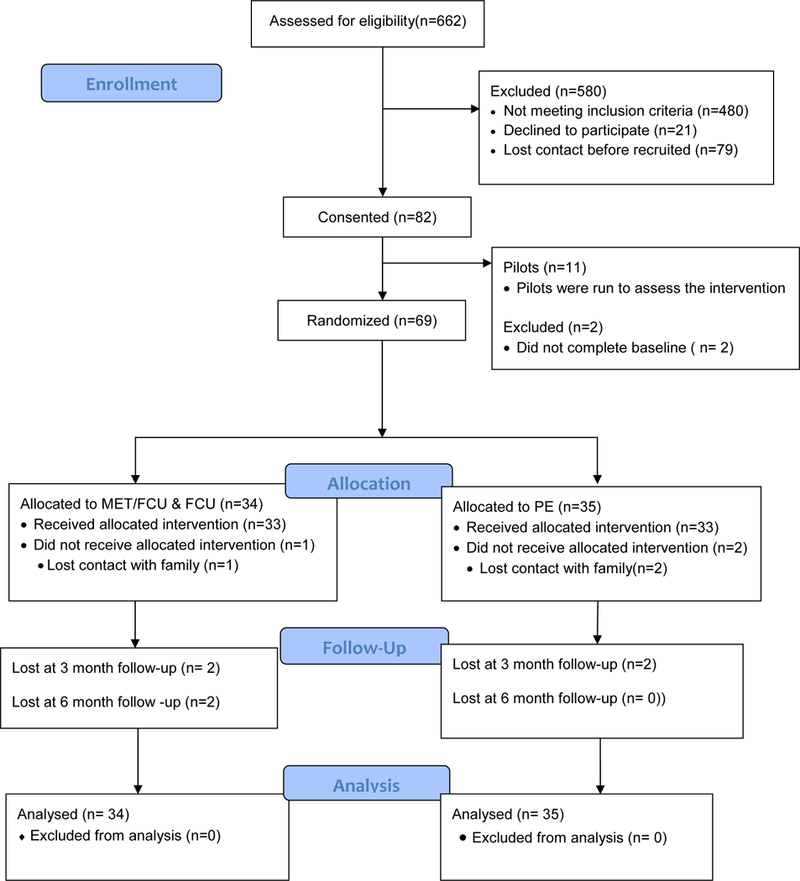
CONSORT 2010 Flow Diagram
After completion of the baseline assessment, an interventionist handed condition assignment, based a1:1 randomization schedule and using an urn randomization procedure (Stout, Wirtz, Carbonari, & Del Boca, 1994). Variables used in the urn randomization included age (above or below 15 years old) and scores above or below the clinical cutoff (7 or above) for substance abuse on a commonly used screener, the Global Appraisal of Individual Needs – Quick screener’s (GAIN-Q) Substance Problem Scale plus Substance Use and Abuse Scale (Dennis, Titus, White, Unsicker, & Hodkgins, 2002). Urns were generated for each combination of variables by treatment condition and then placed in opaque envelopes to ensure that study staff members were masked to allocation sequence until baseline assessments were complete.
Follow-up outcome data were collected at three and six months following the baseline assessment by research staff with conditions masked. At three months, 94% of the sample in both conditions completed follow-up, while at six months, 88% of the participants in the experimental condition and 94% in the comparison condition were reassessed.
Intervention Conditions
The MET/FCU consisted of one baseline, 45 minute assessment session followed by one session of a MET for the adolescent and one session of the FCU for the parent(s). The adolescent and parent session occurred simultaneously, and lasted about 90 minutes each. The PE condition completed the same assessment battery and 60 minute PE sessions for adolescent and parent that occurred simultaneously. The interventionists were four Masters-level therapists with training in social work or mental health counseling and one with a PhD in developmental psychology. Two of the therapists were also fluent in Spanish.
Motivational Enhancement Therapy (MET).
The MET session incorporated open-ended exploration, personalized feedback, and discussion about the adolescent’s substance use and truancy. The MET session incorporated the central principles of MI (W. R. Miller & Rollnick, 1991) but was structured to include four components: establishing rapport, assessing motivation for change, motivational enhancement, and establishing goals for change. The counselor emphasized that the intention of the interview was not to tell adolescents what to do, but to have adolescents determine for themselves what decisions and choices about substance use and school they would like to make. Next, level of motivation for change was assessed by asking the adolescents to talk about their likes and dislikes regarding substance use. The counselor then tailored the session to these pros and cons. Enhancement of motivation to change was accomplished by utilizing individualized normative feedback, examining decisional balance, and providing information and advice, if the teen requested it. The individualized feedback was derived from the baseline assessment and included discussion of: (1) the teen’s substance use paired with normative information from age matched peers, (2) consequences of substance use, including truancy, money spent, sexual risk taking, and other health consequences, (3) attitudes towards their peers’ substance use, and (4) efficacy to make a change in their substance use and truancy behaviors. In addition to providing feedback, the substance use and truancy section was designed to correct overestimations (i.e., the false consensus effect) common among adolescents about the prevalence of substance use and truancy (D. B. Henry, Kobus, & Schoeny, 2011).
Following the presentation of the feedback, counselors examined the adolescent’s decisional balance by asking the adolescent to “envision the future,” and to think about what positive things might happen if their substance use were to decrease and what would be the worst thing that could happen if their substance use were to stay the same. In the final phase of the intervention, the adolescent and counselor developed a plan for the future. This included identifying goals for behavior change, exploring barriers to change, and providing strategic advice. A “goals sheet” contained a variety of substance use moderation and harm reduction goals as well as some blank spaces for filling in other goals, including school attendance.
Family Check-Up (FCU).
In the FCU, the baseline assessment data were used to identify strengths and challenges in the family while the videotaped observational task was used to provide feedback on the parent-teen interactional style. “Macro” clinical scores were calculated on the Family Assessment Task (FAsTask) and coded as an area of “strength,” “needs improvement,” or “challenge,” and provided as feedback during the FCU session. Macro scores were calculated on positive relationships, monitoring, limit setting, problem solving, school attendance and substance use norms. These data, along with parenting measures, were used to generate the individualized feedback report for use in the FCU parent feedback session.
The parents attended the FCU feedback session without the adolescent. There were four specific phases of the FCU feedback session (Dishion & Kavanagh, 2003): (1) Self-assessment: Parents were asked if they learned anything about their family from participating in the assessment. (2) Support and clarification: The counselor supported the family’s self-assessment efforts, assessed their level of understanding of the family, and clarified issues within the family. (3) Feedback: The assessment findings was summarized into categories including family context (e.g., life stress), parenting practices (e.g., substance use expectations for teens), teen behavior (e.g., positive and problem behaviors), and peer and sibling relationships (e.g., peer substance use). Normative information regarding escalation in substance use rates from 7th through 12th grades was also presented. (4) Menu of options: Parent motivation for and barriers to change and steps for making positive changes were discussed. Parents were also asked to consider how they anticipated their teen reacting to any changes, problem solving any potential negative reactions.
Comparison condition.
The comparison condition consisted of individual psychoeducation (PE) sessions for the parent and teen. An interventionist reviewed a set of educational materials with the parents. The session started with detailed information about marijuana, including immediate and long-term effects as well as myths about medical marijuana, and alcohol, and high-risk situations for use of either substance. Information about truancy was then reviewed including its relation to substance use and ways to prevent truancy. Throughout the discussion, the interventionist referred to 10 educational handouts from NIH and other sources. The interventionist reviewed information regarding marijuana, alcohol, and school attendance with the teen. Parents and teens were given the handouts after the session.
Booster Contacts.
Parents in both conditions received nine brochures between baseline and their final follow-up, on topics such as communicating with your teen and monitoring teen behavior. Parents and adolescents in both conditions also received a 30 minute booster session after the three month follow-up assessment. In the experimental condition, counselors reviewed the action plans that were generated during the intervention session, and they asked both parents and teens if they were able to implement their change plans, what the experience was like, and whether they experienced any other positive changes as a result. If the change plan was successfully implemented, participants were encouraged to identify another goal that they would like to work towards and develop another change plan. If parents and adolescents did not implement their change plan, obstacles were discussed along with strategies for overcoming these obstacles. In the PE condition, the content of the original session was reviewed.
Training and supervision of counselors.
In order to control for counselor-specific effects, counselors delivered both conditions. Over the course of the study, four masters level and one doctoral level counselor delivered both the MET/FCU and PE conditions. Counselor training started with an eight hour-long MI workshop followed by instruction specific to the MET/FCU protocol. Protocol specific materials were reviewed, practiced by the counselor, and then role-played with doctoral-level supervisors. For the PE condition, the PE materials were reviewed and delivering the PE session was role-played. Emphasis was placed on not using MI skills and techniques in the PE session. Weekly supervision and tape reviews were conducted.
Adherence and competency.
For the MET, a total of 13 out of 34 of English-speaking MET tapes (38%) were rated on 30 protocol-based components using a “no/yes” scale. Two coders rated all 13 tapes. For adherence, there was 93% agreement on whether the protocol components were administered, and on average 86% of the expected elements of the intervention were administered. As can be seen in Table 2, all project-specific competency items were above the expected score of three on a one to five Likert scale, with the exception of “Support Self-Efficacy” which was slightly lower (M = 2.85; SD = 0.66). Competency was also rated using the Motivational Interviewing Treatment Integrity Code Version 3.0 (MITI 3.0; Moyers, Martin, Manuel, Miller, & Ernst, 2010). As seen in Table 2, competence ratings were all above 4.0. Interrater reliability was very high, with an intraclass correlation of .85 across items.
Table 2.
Rater scores for MI competence, FCU competence and MITI scores
| Item | (N = 13) |
|---|---|
| M (SD) | |
| Project MI Competence Ratings | |
| Express empathy | 3.88 (0.51) |
| Develop discrepancy | 3.73 (0.60) |
| Roll with resistance a | 3.25 (0.35) |
| Support self-efficacy | 2.85 (0.66) |
| Open-ended questions | 4.19 (0.43) |
| Reflective listening | 4.27 (0.56) |
| Affirm | 3.88 (0.65) |
| Summarize | 3.15 (0.59) |
| Elicit change talk | 3.85 (0.47) |
| MITI Scores | |
| Evocation | 4.46 (0.32) |
| Collaboration | 4.46 (0.56) |
| Autonomy | 4.42 (0.28) |
| Direction | 4.65 (0.24) |
| Empathy | 4.23 (0.53) |
| Project FCU Competence Ratings | |
| Balance of strengths and challenges | 3.96 (0.52) |
| Provide examples from the videotaped assessment | 4.00 (0.50) |
| Responded appropriately to confusionb | 3.50 (0.00) |
| Express empathy | 4.11 (0.42) |
| Develop discrepancy | 3.35 (0.52) |
| Roll with resistancec | 3.00 (0.00) |
| Support self-efficacy | 2.58 (0.64) |
| Open-ended questions | 4.08 (0.34) |
| Reflective listening | 4.31 (0.48) |
| Affirm | 4.27 (0.63) |
| Summarize | 2.96 (0.69) |
| Elicit change talk | 3.73 (0.56) |
| MITI Scores | |
| Evocation | 4.35 (0.38) |
| Collaboration | 4.65 (0.43) |
| Autonomy | 4.58 (0.40) |
| Direction | 4.27 (0.70) |
| Empathy | 4.35 (0.47) |
Note: Competence ratings were answered on a 5-point scale: 1 “Poor”, 3 “Good”, 5 “Excellent”. MITI refers to Motivational Interviewing Treatment Integrity 3.0. Items were answered on a 5-point scale from 1 “low” to 5 “high”.
FCU = Family Check-up
2 cases were rated on this item; for the rest resistance was not identified.
1 case was rated on this item; for the rest confusion was not identified.
1 case was rated on this item; for the rest resistance was not identified.
For the FCU, a total of 13 out of 34 English-speaking FCU tapes (38%) were rated on 41 protocol-based components using a “no/yes” scale. Two coders rated all 13 tapes. For adherence, the agreement on whether protocol components were administered was 87%, and on average, 80% of the expected elements of the intervention were administered. All project-specific competence scores were at or above the expected score of three on a one to five Likert scale, with the exception of “Support Self-Efficacy” (M = 2.58; SD = 0.64). The MITI scores were consistently strong as well with competence ratings all above 4.0. Inter-rater reliability was very high, with an intraclass correlation of .86 across items.
Measures
Treatment Acceptability.
Adolescents completed four items from the Session Evaluation Forms (SEF; Harper, Contreras, Bangi, & Pedraza, 2003) at the end of the intervention: (1) “I will apply what I learned from this session in my life,” (2) “The topic of this session was relevant to my life,” (3) “I felt comfortable participating in this session,” and (4) “This session was helpful to me.” Items were rated on a four-point Likert scale from ‘strongly agree’ to ‘strongly disagree.’
Marijuana use.
Quantity and frequency of marijuana use were assessed using the Timeline Follow-Back (Sobell & Sobell, 1996), a widely used research and clinical assessment tool that uses a calendar format with temporal cues (i.e. holidays and special occasions) to assist in recall. Marijuana was recorded as “yes” or “no” on each day and adolescents were asked how many times they smoked marijuana each day.
Alcohol use.
The Adolescent Drinking Questionnaire (ADQ; Jessor, Donovan, & Costa, 1989) measured alcohol use in the three months prior to each assessment. Items included number of drinking days (frequency), number of drinks consumed per drinking episode (quantity), and the number of high volume drinking days, defined as five or more drinks per occasion.
Drug use
was recorded as positive if adolescents reported they had used any of 9 drugs in the prior year, such as cocaine, PCP, heroin, and prescription drugs. A urine drug screen (UDS; Redwood Toxicology) was also administered at the final follow-up point.
Truancy.
The TLFB was adapted in this study to assess truancy, including frequency of unexcused school absences, skipping classes, tardies, and suspensions.
Parent-teen interaction variables.
The Videotaped Family Assessment Task (FAsTask), adapted by Dishion, Andrews, Kavanagh, and Soberman (1996), to assess in vivo parent-child interactions, was administered at baseline and at six month follow-up. Parent(s) and teens were given a set of instructions and asked to discuss family topics for five minutes. Family topics included a time when teens were without supervision (monitoring) and family problem solving regarding school truancy (problem solving-truancy). All FAsTask videos were coded by two study staff who watched each segment of the videotape together but completed separate coding sheets. Depending on the task, there were 19 – 21 items coded, such as, “Does this parent seem to be monitoring with whom the child spends time?” An inter-rater reliability estimate (i.e., % of ratings within two points on a 9-point scale) was created for ratings. Percentage of inter-rater reliability within each case ranged from 71 to 96%, mean = 86%. When there was disagreement, the two raters discussed the rating and consensus was reached. The consensus score was used in data analyses. Internal consistency for the monitoring task across both baseline and six months ranged between α =.94 and .88 for father ratings, and α =.87 and .84 for mother ratings. The family problem solving task yielded alpha coefficients of α =.82 and .77 for the family as a whole. α =.97 and .68 for fathers, α =.91 and .90 for mothers, and α =.95 and .91 for teens.
Statistical analyses
The analytical approach is based on an analysis of covariance (ANCOVA) for randomized clinical trials. The outcome variables observed at follow-up were regressed on the values of the outcomes observed at baseline and a treatment effect dummy variable, contrasting MET/FCU versus PE. The outcomes at three and six month follow-ups were modeled simultaneously. For continuous variables, a mixed effect model was used to adjust standard errors for the clustering due to repeated observations on the same individuals, and also included in the model was a fixed effect for time (six month versus three month follow-up) and a time by treatment interaction. For categorical variables, a complex model with fixed effects only and ordered logistic regression was used. Effect sizes were calculated using Cohen’s f2, which is the proportion of unexplained/ explained variance accounted for by the predictors, but are recast as d statistics based on transformed f statistics; 0.20 and 0.50 demarcate small and medium effects.
Results
Acceptability and Feasibility
The experimental condition’s feasibility was evidenced by completion of 92% of the counseling and booster sessions. Average number of days from recruitment to completion of the baseline counseling session was 8.2 days. Acceptability was indicated by the high percentage (80%) of participants in the experimental condition endorsing “agree” or “strongly agree” (or an equivalent metric) for all items on the SEF (see Table 3).
Table 3.
Participant responses to individual “acceptability” questions
| Parent FCU Characteristics | Mean | Range | Response (%) |
| Therapist Characteristics | “A little or a lot” | ||
| Was easy to talk to | 4.0 | 0 | 100 |
| Was concerned about me and my child | 4.0 | 0 | 97.1 |
| Understood me | 4.0 | 1 | 100 |
| Helped me believe that I can help my teenager | 4.0 | 0 | 97.1 |
| Intervention Characteristics | “Not at all or a little” | ||
| Difficulty in implementing your change plan | 1.8 | 2 | 70.6 |
| “Pretty or very” | |||
| Confidence in implementing your change plan | 4.2 | 3 | 79.4 |
| Relevance of the parenting information provided | 4.6 | 4 | 91.2 |
| Overall Satisfaction | |||
| Happiness with the session | 4.8 | 1 | 97 |
| Adolescent MET Characteristics | Mean | Range | Response (%) |
| Therapist Characteristics | “A little or a lot” | ||
| Was concerned about me | 2.3 | 3 | 85.3 |
| Understood me | 2.7 | 2 | 91.2 |
| Gave me helpful ideas for avoiding marijuana | 2.7 | 1 | 94.1 |
| Helped me believe that I can change | 2.8 | 1 | 94.1 |
| “Disagree a little or a lot” | |||
| Argued with me | 0.3 | 2 | 91.1 |
The PE condition was also perceived as credible. For instance, 100% of parents reported the session helped them believe they could help their teenager “a little” or “a lot” (see Table 3).
Marijuana and Other Drug Use
As can be seen in Table 4, the MET/FCU condition had stronger outcomes than the PE condition on: (1) percentage of days marijuana was used over the prior 90 days as reported on the TLFB, whether examined continuously (d = .35, small to medium effect size) or categorically as “no use,” “use on 29 days or less,” “use on 30 to 89 days,” or “use every day” (d = .49, medium effect), and, (2) number of times per day marijuana was used (d = .53, medium effect). Positive UDS screens for THC also trended lower in the MET/FCU (43.3%) versus PE (64.5%) at the six month follow-up, χ2 (1,60) = 2.76, p = .08.
Table 4.
Summary of outcome variables at all observations and results of ANCOVA models.
| Observed means (and SD) or % |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 Month | 6 Month | ||||||||||||
| MET/FCU | PE | MET/FCU | PE | MET/FCU | PE | ANCOVA | ||||||||
| Outcome | M† | SD | M† | SD | M† | SD | M† | SD | M† | SD | M† | SD | d (95% CI) | |
| Average MJ-use days in previous 90 days (M, SD) | 35 | 29 | 49 | 35 | 27 | 35 | 41 | 36 | 21 | 28 | 41 | 35 | +0.35 (0.00, 0.69) | |
| Days in previous 90 used MJ (%) | +0.49 (0.13, 0.84) * | |||||||||||||
| 0 days | 0 | 0 | 30 | 9 | 27 | 10 | ||||||||
| 1-29 days | 56 | 37 | 37 | 41 | 47 | 32 | ||||||||
| 30-89 days | 32 | 43 | 30 | 32 | 30 | 42 | ||||||||
| 90 days | 12 | 20 | 3 | 18 | 7 | 16 | ||||||||
| Number times per day used MJ on average (%) | +0.11 (−0.24, 0.87) | |||||||||||||
| None | 21 | 17 | 53 | 26 | 47 | 34 | ||||||||
| Once | 24 | 39 | 15 | 29 | 18 | 23 | ||||||||
| Two to three | 32 | 40 | 26 | 29 | 26 | 26 | ||||||||
| Four or more | 24 | 14 | 6 | 17 | 9 | 17 | ||||||||
| Drinks per month over previous 90 days (%) | +0.26 (−0.09, 0.61) | |||||||||||||
| None | 18 | 14 | 33 | 29 | 30 | 29 | ||||||||
| Less than one | 24 | 14 | 43 | 21 | 37 | 19 | ||||||||
| One or more | 59 | 71 | 23 | 50 | 33 | 52 | ||||||||
| Amount consumed per average drinking episode (%) | +0.00 (−0.35, 0.35) | |||||||||||||
| None | 18 | 14 | 33 | 29 | 30 | 29 | ||||||||
| Less than four | 38 | 51 | 23 | 29 | 30 | 35 | ||||||||
| Four or more | 44 | 34 | 43 | 41 | 40 | 35 | ||||||||
| Days consumed more than 5 (%) | +0.35 (−0.01, 0.70) | |||||||||||||
| None | 50 | 34 | 57 | 53 | 53 | 42 | ||||||||
| One to two | 38 | 54 | 37 | 35 | 43 | 32 | ||||||||
| Two or more | 12 | 11 | 7 | 12 | 3 | 26 | ||||||||
| Any other drug use (% yes) | 12 | 14 | 3 | 18 | 7 | 16 | +0.38 (0.02, 0.73) | |||||||
| FAST Parental monitoring [1-9, higher better] (M, SD) | 5.0 | 1.3 | 4.5 | 1.4 | -- | -- | 5.2 | 1.2 | 4.4 | 1.1 | -0.58 (−1.09, −0.05) * | |||
| FAST Parental problem solving [1-9, higher better) (M, SD) | 6.0 | 1.5 | 6.0 | 1.8 | -- | -- | 6.7 | 1.1 | 6.0 | 1.3 | -0.42 (−0.94, 0.11) * | |||
| FAST Teen problem solving [1-9, higher better] (M, SD) | 4.6 | 1.9 | 4.6 | 1.7 | -- | -- | 5.8 | 1.5 | 4.5 | 1.6 | −0.66 (−1.17, −0.11) * | |||
| Any absent days over previous 90 days (% yes) | 68 | 77 | 44 | 47 | 31 | 45 | +0.19 (−0.16, 0.53) | |||||||
| Any tardy days over previous 90 days (% yes) | 68 | 60 | 44 | 50 | 47 | 39 | +0.17 (−0.18, 0.15) | |||||||
| Any skip days over previous 90 days (% yes) | 38 | 29 | 28 | 24 | 12 | 27 | +0.30 (−0.04, 0.64) | |||||||
Notes. d statistics based on transformed f statistics comparing nested generalized linear mixed effect models for binary, ordinal, or continuous outcomes, as appropriate given the scale of the outcome. 95% confidence intervals (CI) for d are derived from reference to a non-central T distribution. A + sign indicates the expected mean (or proportion) of the outcome at follow-up is higher in the PE group than in the MET/FCU group controlling for baseline, whereas a -sign indicates the expected mean (or proportion) at follow-up is lower in the PE group than the MET/FCU group (also controlling for baseline).
Statistical significance (P < .05) is indicated with and indicates that the main effect of treatment at follow-up, and/or the interaction of treatment with time suggests deviation from chance level variation.
Indicates the summary statistic in the M column is a percent; M, SD denote mean and standard deviation.Marijuana use and truancy assessed with the TLFB, alcohol with the ADQ, other drug use with the DUQ, and parenting variables with the FAST
Any other drug use, examined dichotomously as yes or no in the prior year (d = .38, small to medium effect size), also favored the MET/FCU condition over PE. Only two MET/FCU and one PE participant had a positive UDS for something other than THC.
Alcohol
As can be seen in Table 5, the MET/FCU condition had stronger outcomes than the PE condition on: (1) alcohol use frequency, examined categorically as “no drinking,” “drinking less than once per month,” and “drinking monthly or more” (d = .26, small effect), and, (2) days consumed 5 or more drinks, examined categorically as “no drinking days,” “one day,” and “2 or more days” (d = .35, small to medium effect).
Table 5.
CONSORT 2010 checklist of information to include when reporting a randomised trial*
| Section/Topic | Item No | Checklist item | Reported on page No |
|---|---|---|---|
| Title and abstract | |||
| 1a | Identification as a randomised trial in the title | 1 |
|
| 1b | Structured summary of trial design, methods, results, and conclusions (for specific guidance see CONSORT for abstracts) | Abstract , 2 |
|
| Introduction | |||
| Background and objectives | 2a | Scientific background and explanation of rationale | 3-6 |
| 2b | Specific objectives or hypotheses | 6 |
|
| Methods | |||
| Trial design | 3a | Description of trial design (such as parallel, factorial) including allocation ratio | 6 |
| 3b | Important changes to methods after trial commencement (such as eligibility criteria), with reasons | NA |
|
| Participants | 4a | Eligibility criteria for participants | 7 |
| 4b | Settings and locations where the data were collected | 7 |
|
| Interventions | 5 | The interventions for each group with sufficient details to allow replication, including how and when they were actually administered | 8-11 |
| Outcomes | 6a | Completely defined pre-specified primary and secondary outcome measures, including how and when they were assessed | 13-14 |
| 6b | Any changes to trial outcomes after the trial commenced, with reasons | NA |
|
| Sample size | 7a | How sample size was determined | Amt of pilot funding |
| 7b | When applicable, explanation of any interim analyses and stopping guidelines | NA |
|
| Randomisation: | |||
| Sequence generation | 8a | Method used to generate the random allocation sequence | 8 |
| 8b | Type of randomisation; details of any restriction (such as blocking and block size) | 8 |
|
| Allocation concealment mechanism | 9 | Mechanism used to implement the random allocation sequence (such as sequentially numbered containers), describing any steps taken to conceal the sequence until interventions were assigned | 8 |
| Implementation | 10 | Who generated the random allocation sequence, who enrolled participants, and who assigned participants to interventions | 8 |
| Blinding | 11a | If done, who was blinded after assignment to interventions (for example, participants, care providers, those assessing outcomes) and how | 8 |
| 11b | If relevant, description of the clarity of interventions | ||
| Statistical methods | 12a | Statistical methods used to compare groups for primary and secondary outcomes | 14-15 |
| 12b | Methods for additional analyses, such as subgroup analyses and adjusted analyses | ||
| Results | |||
| Participant flow (a diagram is strongly recommended) | 13a | For each group, the numbers of participants who were randomly assigned, received intended treatment, and were analysed for the primary outcome | 6, Table 1 |
| 13b | For each group, losses and exclusions after randomisation, together with reasons | CONSORT figure |
|
| Recruitment | 14a | Dates defining the periods of recruitment and follow-up | 6 |
| 14b | Why the trial ended or was stopped | NA |
|
| Baseline data | 15 | A table showing baseline demographic and clinical characteristics for each group |
Table 1 |
| Numbers analysed | 16 | For each group, number of participants (denominator) included in each analysis and whether the analysis was by original assigned groups | Consort , Table 4 |
| Outcomes and estimation | 17a | For each primary and secondary outcome, results for each group, and the estimated effect size and its precision (such as 95% confidence interval) |
Table 4 |
| 17b | For binary outcomes, presentation of both absolute and relative effect sizes is recommended | NA |
|
| Ancillary analyses | 18 | Results of any other analyses performed, including subgroup analyses and adjusted analyses, distinguishing pre-specified from exploratory | NA |
| Harms | 19 | All important harms or unintended effects in each group (for specific guidance see CONSORT for harms) | NA |
| Discussion | |||
| LMET/FCUtations | 20 | Trial limitations, addressing sources of potential bias, imprecision, and, if relevant, multiplicity of analyses | 19 |
| Generalisability | 21 | Generalisability (external validity, applicability) of the trial findings | 18-19 |
| Interpretation | 22 | Interpretation consistent with results, balancing benefits and harms, and considering other relevant evidence | 18-19 |
| Other information | |||
| Registration | 23 | Registration number and name of trial registry | 1 |
| Protocol | 24 | Where the full trial protocol can be accessed, if available | 1 |
| Funding | 25 | Sources of funding and other support (such as supply of drugs), role of funders | 1 |
Truancy
As can be seen in Table 4, the MET/FCU condition had stronger outcomes than the PE condition on: (1) percentage of adolescents reporting any absent days (d = .19, small effect); (2) percentage of adolescents reporting any tardy days (d = .17, small effect); and (3) percentage of adolescents reporting any skipped days (d = .30, small effect).
Parenting variables
As can be seen in Table 4, the MET/FCU condition had stronger outcomes than the PE condition on the FAsTask parent monitoring (d = −.58, medium effect), parent problem solving (d = −.42, close to medium effect), and teen problem solving (d = - .66, medium to large effect).
Clinical Significance
We observed mean effect sizes of 0.49 for days used marijuana in the past 90, −0.58 for FAST parental monitoring, and −0.66 for FAST teen problem solving. Under the assumption that the reliability of these measures is R = .77 (Yasui & Dishion, 2008), standardized mean differences of 0.5 amount to a 1 standard error of measurement difference, a common threshold for clinical significance (de Vet et al., 2006).
Discussion
The first goal of this treatment development project was to determine the feasibility of a preventive intervention integrating a parent-based and an individual adolescent MET. The sample was reasonably diverse with respect to race/ethnicity, gender, and socioeconomic status. The large majority of families completed the intervention, as well as the booster session, in a timely fashion. Parent and teen engagement in the intervention seemed positive, as reflected in exit interview ratings and comments about the interventions.
Participants in the PE condition, especially parents, also reported the intervention to be helpful, suggesting that an active, plausible comparison condition was employed in the study. Observations by the interventionists suggest that for some adolescents and parents in the PE condition, level of knowledge about the negative effects of using various substances was low. Consequently, both adolescents and parents benefited from the knowledge gained through the PE condition. Thus, one potential hypothesis to explore in future studies is whether knowledge, either parent or teen, about substance use moderates intervention outcomes and whether outcomes improve by providing substance use education prior to conducting a MET.
Effect size calculations indicate that medium treatment effects were found for the experimental condition, relative to PE, on days of marijuana use and number of times marijuana was smoked per day. The UDS results were consistent with the self-report findings. Although there was a reduction in use in both conditions, rates of marijuana use remained fairly high after the delivery of both interventions. This was likely due to the high marijuana use rates adolescents reported at baseline assessment and may suggest that perhaps a brief intervention may not be intensive enough to lead to significant reductions in marijuana use.
Small to medium effects were found for other drug use and heavy drinking days. These results, combined with the finding on the lower number of times marijuana was smoked per day, suggest a potential harm reduction effect (Marlatt & Witkiewitz, 2002), which is central to the MET intervention. That is, there was some continued drinking and marijuana use, but a reduction in heavy drinking and marijuana use days.
The experimental intervention appeared to more strongly affect substance use than truancy. Small effects favoring the MET/FCU condition were found for days absent, skipped days, and tardies. This is consistent with the focus of the MET/FCU intervention as more time was spent addressing substance use than truancy. For example, the goals sheet always set substance use goals, but not necessarily truancy goals. Because truancy can be multi-determined, a more thorough investigation of the causes for truancy might be conducted in future studies and incorporated into the experimental condition, if they are deemed amenable to a MET.
This study also examined whether the experimental condition affected the potential mechanisms presumed to underlie its effectiveness, i.e., parental monitoring and parent and teen problem solving. Medium effects on parental monitoring and medium to large effects on parent-teen problem solving were evident in the experimental condition as assessed by FAsTask observer ratings. These data provide some support for parental monitoring, as well as parent-teen problem solving, as potential mechanisms by which improvement in adolescent substance use, and secondarily in truancy, may have been obtained in the experimental condition. The fact that this effect on parental monitoring was based on observer ratings lends credence to the finding and underscores the importance of observer ratings in assessing parenting.
Limitations
The current study’s findings must be considered within the context of a number of limitations. The small sample size suggests that the findings may not be stable (Kraemer et al., 2006). All adolescents in this sample exhibited truancy, thus the results may not be generalizable to other adolescent substance using populations. Sample size also precluded mediational analyses, which would have enabled us to look at whether the presumed parenting mechanisms resulted in improvements in substance use and truancy. In addition, substance use was not corroborated by any secondary observers, although research staff oversaw the UDS at six month follow-up.
Despite these limitations, this study fills a major gap in the literature by combining two theory driven, effective brief interventions, an adolescent and parent MET to target both substance use and school truancy, concurrently. Future research examining the efficacy of the intervention in a larger sample, as well as mechanisms and moderators, is warranted. If proven efficacious in a larger trial, this protocol would join a handful of already available interventions listed on the SAMSHA National Registries of Evidence-based Programs and Practices (http://nrepp.samhsa.gov/landing.aspx) that address adolescent substance problems, such as Active Parenting of Teens: Families in Action, and/or use MI approaches with adolescents. The brevity of the protocol distinguishes it from most other evidence-based programs and increases the probability that this intervention would be adopted by schools and courts.
References
- Alfonso J, & Dunn ME (2007). Differences in the marijuana expectancies of adolescents in relation to marijuana use. Substance Use & Misuse, 42(6), 1009–1025. doi: 10.1080/10826080701212386 [DOI] [PubMed] [Google Scholar]
- Barnett E, Sussman S, Smith C, Rohrback LA, & Spruijt-Metz D (2012). Motivational interviewing for adolescent substance use: A review of the literature. Addictive Behaviors, 37(12), 1325–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano RF, & Hawkins JD (1996). The Social Development Model: A theory of antisocial behavior In Hawkins JD (Ed.), Delinquency and Crime: Current Theories. New York: Cambridge University Press. [Google Scholar]
- D’Amico EJ, Ellickson PL, Collins RL, Martino S, & Klein DJ (2005). Processes linking adolescent problems to substance-use problems in late young adulthood. J Stud Alcohol, 66(6), 766–775. [DOI] [PubMed] [Google Scholar]
- de Vet HC, Terwee CB, Ostelo RW, Beckerman H, Knol DL, & Bouter LM (2006). Minimal changes in health status questionnaires: distinction between minimally detectable change and minimally important change. Health and Quality of Life Outcomes, 4(1), 54. doi: 10.1186/1477-7525-4-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dembo R, Briones-Robinson R, Barrett K, Ungaro R, Winters KC, Belenko S, . . . Wareham J. (2014). Brief intervention for truant youth sexual risk behavior and marijuana use. Journal of Child & Adolescent Substance Abuse, 23(5), 318–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Titus J, White M, Unsicker J, & Hodkgins D (2002). Global Appraisal of Individual Needs (GAIN): Administration guide for the GAIN and related measures. Bloomington, IL: Chestnut Health Systems. [Google Scholar]
- Dishion TJ, Andrews DW, Kavanagh K, & Soberman L (1996). Preventive interventions for high-risk youth: The adolescent transitions program In Peters RD & McMahon RJ (Eds.), Preventing childhood disorders, AOD abuse, and delinquency (pp. 184–214). Thousand Oaks, CA: Sage. [Google Scholar]
- Dishion TJ, & Kavanagh K (2003). Intervening in adolescent problem behavior: A family-centered approach. New York: Guilford Press. [Google Scholar]
- Dishion TJ, Nelson SE, & Kavanagh K (2003). The family check-up with high-risk young adolescents: Preventing early-onset substance use by parent monitoring. Behavior Therapy, 34(4), 553–571. [Google Scholar]
- Harper G, Contreras R, Bangi A, & Pedraza A (2003). Collaborative process evaluation: Enhancing community relevance and cultural appropriateness in HIV prevention. Journal of Prevention and Intervention in the Community, 26, 53–71. [Google Scholar]
- Henry DB, Kobus K, & Schoeny ME (2011). Accuracy and bias in adolescents’ perceptions of friends’ substance use. Psychology of Addictive Behaviors, 25(1), 80–89. doi: 10.1037/a0021874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry KL, Thornberry TP. Truancy and escalation of substance use during adolescence (2010). Journal of Studies on Alcohol and Drugs, 71(1), 115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry KL, Thornberry TP, & Huizinga DH (2009). A discrete-time survival analysis of the relationship between truancy and the onset of marijuana use. Journal of Studies on Alcohol and Drugs, 70(1), 5–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, & Schulenberg JE (2013). Alcohol use during the transition from middle school to high school: National panel data on prevalence and moderators. Developmental Psychology, 49(11), 2147–2158. doi: 10.1037/a0031843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen CD, Cushing CC, Aylward BS, Craig JT, Sorell DM, & Steele RG (2011). Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: A meta-analytic review. Journal of Consulting and Clinical Psychology, 79(4), 433–440. doi: 10.1037/a0023992 [DOI] [PubMed] [Google Scholar]
- Jessor R, Donovan JE, & Costa FM (1989). Health Behavior Questionnaire. Boulder, CO: University of Colorado. [Google Scholar]
- Marlatt GA, & Witkiewitz K (2002). Harm reduction approaches to alcohol use: health promotion, prevention, and treatment. Addict Behav, 27(6), 867–886. [DOI] [PubMed] [Google Scholar]
- Maynard BR, Salas-Wright CP, Vaughn MG, & Peters KE (2012). Who are truant youth? Examining distinctive profiles of truant youth using latent profile analysis. Journal of Youth and Adolescence, 41, 1671–1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR (2000) Motivational Enhancement Therapy: Description of Counseling Approach in Boren JJ Onken LS, & Carroll KM. (Eds.) Approaches to Drug Abuse Counseling, US Department of Health and Human Services; NIH Publication No. 00–4151 edition (2000) [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, & Ernst D (2010). Motivational Interviewing Treatment Integrity (MITI 3.1.1): Center on Alcoholism, Substance Abuse and Addictions: University of New Mexico. [Google Scholar]
- Spirito A, Sindelar-Manning H, Colby SM, Barnett NP, Lewander W, Rohsenow DJ, & Monti PM (2011). Individual and family motivational interventions for alcohol-positive adolescents treated in an emergency department: Results of a randomized clinical trial. Archives of Pediatric and Adolescent Medicine, 165(3), 269–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L, Albert D, Cauffman E, Banich M, Graham S, & Woolard J (2008). Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: Evidence for a dual systems model. Developmental Psychology, 44(6), 1764–1778. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, & Del Boca FK (1994). Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol and Drugs, 12, 70–75. [DOI] [PubMed] [Google Scholar]
- Wu LT, Swartz MS, Brady KT, & Hoyle RH (2015). Perceived cannabis use norms and cannabis use among adolescents in the United States. J Psychiatr Res, 64, 79–87. doi: 10.1016/j.jpsychires.2015.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ryzin MJ, Fosco GM, & Dishion TJ (2012). Family and peer predictors of substance use from early adolescence to early adulthood: An 11-year prospective analysis. Addictive Behaviors, 37, 1314–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughn M, Maynard B, Salas-Wright C, Perron B, & Abdon A (2013). Prevalence and correlates of truancy in the US: Results from a national sample. Journal of Adolescence, 36(4), 767–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasui M, & Dishion TJ (2008). Direct observation of family management: Validity and reliability as a function of coder ethnicity and training. Behavior Therapy, 39(4), 336–347. doi: 10.1016/j.beth.2007.10.001 [DOI] [PubMed] [Google Scholar]


