Abstract
Objectives
To estimate trends in prevalence and incidence of syphilis, gonorrhea and chlamydia in adult men and women in South Africa.
Methods
The Spectrum-STI tool estimated trends in prevalence and incidence of active syphilis, gonorrhea and chlamydia, fitting South African prevalence data. Results were used, alongside programmatic surveillance data, to estimate trends in incident gonorrhea cases resistant to first-line treatment, and the reporting gap of symptomatic male gonorrhea and chlamydia cases treated but not reported as cases of urethritis syndrome.
Results
In 2017 adult (15–49 years) the estimated female and male prevalences for syphilis were 0.50% (95% CI: 0.32–0.80%) and 0.97% (0.19–2.28%), for gonorrhea 6.6% (3.8–10.8%) and 3.5% (1.7–6.1%), and for chlamydia 14.7% (9.9–21%) and 6.0% (3.8–10.4%), respectively. Between 1990 and 2017 the estimated prevalence of syphilis declined steadily in women and men, probably in part reflecting improved treatment coverage. For gonorrhea and chlamydia, estimated prevalence and incidence showed no consistent time trend in either women or men. Despite growing annual numbers of gonorrhea cases − reflecting population growth − the estimated number of first line treatment-resistant gonorrhea cases did not increase between 2008 and 2017, owing to changes in first-line antimicrobial treatment regimens for gonorrhea in 2008 and 2014/5. Case reporting completeness among treated male urethritis syndrome episodes was estimated at 10–28% in 2017.
Conclusion
South Africa continues to suffer a high STI burden. Improvements in access and quality of maternal, STI and HIV health care services likely contributed to the decline in syphilis prevalence. The lack of any decline in gonorrhea and chlamydia prevalence highlights the need to enhance STI services beyond clinic-based syndromic case management, to reinvigorate primary STI and HIV prevention and, especially for women, to screen for asymptomatic infections.
Introduction
South Africa has some of the highest rates of sexually transmitted infections (STIs) in the world and the government views them as a major public health problem. In 2007 the South African government introduced its first national strategic plan (NSP) for HIV and STIs and its latest plan for 2017–2022 includes STI interventions and targets [1]. STIs in South Africa have been managed syndromically using standardized national syndromic management guidelines since the mid-1990s [2]. Key strategies directed at preventing STIs include increasing access to sexual and reproductive health services including promotion of condom use, conducting prevention activities in non-traditional outlets, screening for syphilis in antenatal care, and implementing a comprehensive national social and behavioural change communication strategy with a focus on key populations.
STI surveillance in South Africa is focused on Male Urethritis Syndrome (MUS). All Primary Health Clinics (PHCs) are required to report monthly to the National Indicator Dataset (NIDS) of the South African District Health Information System [3]. The National Institute of Communicable Diseases (NICD) also undertakes etiological surveillance of STI syndromes annually at sentinel PHCs in Gauteng Province and biennially in other provinces [4,5], to validate and update existing STI syndromic management guidelines. In 2008 monitoring of antimicrobial resistance in culture isolates of Neisseria gonorrheae, the predominant cause of MUS [4,5] was introduced and South Africa is a participating country in the World Health Organization (WHO)’s Gonococcal Antimicrobial Surveillance Programme (GASP) [6].
Data on the prevalence of syphilis in adults in South Africa is collected regularly through sentinel surveys of women attending antenatal clinics (ANCs) [7,8] and integrated biological and behavioural surveys in key populations [9]. In addition, in 2009 South Africa started collecting test results from routine programmatic screening in ANC. For gonorrhea and chlamydia these type of data are not available; prevalence data come from research projects and clinical trials.
South Africa’s STI survey and surveillance data have been used to estimate national prevalence patterns and distributions using dynamic STI transmission models. A first round used STI prevalence data collected up to 2002 [10], and the most recent round data up to 2011 [11,12]. The results suggested that syphilis and gonorrhea prevalence began to decline in the late 1990s. Much of this decline was attributed to increased condom use in response to HIV communication programmes and the introduction of syndromic management protocols; in contrast, chlamydia prevalence did not change [13]. However, South African STI prevalence data have not been systematically reviewed after 2005, and dynamic models have not been updated to incorporate more recent STI prevalence data. STI prevalence trends estimated by transmission dynamic models are useful tools for looking at how STIs are spread, but the results reflect the underlying assumptions about trends in sexual behaviors, population networks and STI treatment, and may not reflect true trends if the assumptions are unrealistic. There is thus a need to assess STI prevalence trends using alternative (static or non-dynamic) models that require fewer assumptions. There is also a need for model-based estimates that reflect more recent STI prevalence data.
High rates of STIs estimated historically, and high rates of antimicrobial resistant gonorrhea detected in ongoing surveillance, prompted South Africa to undertake a national STI estimation effort including estimation of trends in the population burden of antimicrobial resistant gonorrhea. A national workshop as held in March 2018, that brought together experts and stakeholders from national STI, HIV and reproductive health programs and academia to collate and synthesize recent national STI data. It used the epidemiological modelling tool Spectrum-STI [14–18]. Spectrum-STI (http://avenirhealth.org/software-spectrum.php) is a statistical trend estimation model developed by Avenir Health, with support from the World Health Organization (WHO), for use by national health officials to synthesize STI surveillance data and generate national trend estimates. For South Africa’s use, Spectrum-STI was adapted to additionally assess population-based trends in resistant gonorrhea cases using surveillance-based trends in antimicrobial resistance.
This paper documents the results from the South Africa Spectrum-STI estimation. The main outputs are adult prevalence and incidence trends for active syphilis, gonorrhea and chlamydia in adult women and men, and trends in the number of new cases of antibiotic-resistant gonorrhea in men. In addition, we compare estimated numbers of symptomatic and treated gonorrhea and chlamydia cases with numbers of MUS cases reported in South Africa, to gauge the completeness of routine case reporting.
Methods
No individual-patient data or records were used. We only used already published, population-aggregated data sets, which were all fully anonymized.
Syphilis: Prevalence and incidence
Prevalence data were identified from studies conducted between 1985 and 2017 in populations representative of the general adult (15–49 year-old) population in South Africa (S1 File) [11,12]. Eligible study populations included pregnant women in ANC care (routine screening or surveys), women attending family planning clinics, and women and men sampled in household surveys and other community-based studies. For women, all data from ANC and non-ANC women were pooled, assuming no systematic prevalence differences between them, as in the 2012 WHO methodology [19] and supported by a recent global meta-analysis of risk factors for adult syphilis [20].
Data were adjusted for diagnostic test performance to reflect ‘active’ syphilis, defined as concurrent positivity on both non-treponemal Rapid Plasma Reagin (RPR) and treponemal tests (e.g. the Treponema pallidum haemagglutination assay (TPHA)[21], using the same assumptions as other Spectrum estimates [22]. Prevalence data from studies that used both a treponemal and non-treponemal test were not adjusted. Prevalence values for studies using rapid treponemal tests were multiplied by 0.70, studies using only treponemal or only non-treponemal tests without confirmatory test were multiplied by 0.53, and studies where the diagnostic test was unknown by 0.75. Each adjustment multiplier was assumed to have a standard error of ±25%. In addition, each syphilis data point data increased by 10% to account for under-sampling of high-risk populations [19], an adjustment in keeping with key group prevalences from Integrated Bio-Behavioural Surveys in South Africa [9,23,24], and estimated population sizes [9]. No adjustments were made for age or location. The adjusted data points were each assigned a weight to reflect national coverage and representativeness. Nationally representative data were assigned a weight of 100% whilst data representative of smaller areas, or from a subset of sentinel surveillance sites were weighted accordingly [22] (S1 File).
The Spectrum-STI model fitted the prevalence data by segmented polynomials regression [25,26] applying a second-order spline curve. Both the number and positions of the knots were estimated, and the Akaike Information Criterion was used for model selection’ [22]. Estimated prevalence was constrained to be within 0–20% [22]. Uncertainty bounds were generated using bootstrapping, with 10,000 replications [22].
Annual incidence was derived by dividing the estimated prevalence by the average duration of infection [19] using the 2012 WHO average durations of infection values for countries with low and intermediate treatment access (S1 File). In the default scenario the proportion of symptomatic episodes treated was set at 35% (the WHO estimates for countries with low treatment access [19]) between 1990 and 1997 and then assumed to increase linearly to 60% in 2006 and to remain constant after this. The increase between 1997 and 2006 was included to reflecting the roll-out of syndromic management [2,12,13] in the mid-1990s [27].
Gonorrhea and chlamydia: Prevalence and incidence
Prevalence data were identified from studies conducted between 1990 and 2017 in female and male populations representative of the general adult 15–49 year-old population in South Africa (S1 File) [11,12]. Eligible populations included pregnant women attending ANC, women and men attending family planning clinics or PHCs, and adult women and men tested as part of household or community surveys. Eligible diagnostic tests were Nuclear Acid Amplification Tests (e.g. Polymerase Chain Reaction and Ligase Chain Reaction) and culture.
Prevalence data from each study were adjusted for diagnostic test performance [19,28,29], geographical location and age, using the same approach and parameters as the WHO’s 2012 STI estimates [19]. Diagnostic tests were adjusted using fixed sensitivities and specificities, and studies conducted in exclusively rural or urban sites were converted into a national prevalence by applying a rural-to-urban ratio of 0.9, and South Africa’s annual urban and rural population sizes [30]. Each prevalence data point was also increased by 10% to account for the contribution of higher-risk populations [19], an adjustment in keeping with key group prevalences measured in South Africa [24,31], and estimated population sizes [9].
For chlamydia in women, prevalence data were adjusted for age reflecting the decline with age of chlamydia prevalence observed in recent surveys of women in South Africa [32,33], the United Kingdom [34] and the United States of America [35] and among women in South Africa presenting to clinics for vaginal discharge syndrome (VDS) [5,36]. This marked age pattern reflects acquired immunity against reinfection with chlamydia [37]. In order to obtain prevalence estimates for the 15–49 age range, prevalence data from studies that only sampled younger populations (15–24 years of age) prevalence estimates were therefore multiplied by 0.60, and studies of exclusively older populations (25 and over) by 1.39. In the absence of similar data for men, we did not assume an age pattern for chlamydia in men. No adjustments were made for age for gonorrhea in either men or women, lacking clear evidence.
Each data point was assigned a weight to reflect its representativeness. Studies that used NAAT diagnostic tests in populations representative of the overall adult population were assigned a weight of 1.0; all other studies were assigned a weight of 0.10 reflecting uncertainties in diagnostic tests, age adjustors and the representativeness of the population sampled.
Spectrum-STI was used to generate estimates for gonorrhea and chlamydia in women and in men separately. A moving average time trend curve was fitted through the adjusted and weighted prevalence data, as there was insufficient data to use a segmented polynomials regression. Uncertainty bounds were calculated by bootstrapping (10,000 replications)[14].
Trends in annual incidence for both infections were estimated using the same approach as syphilis, and the same default assumptions for treatment coverage. Duration estimates were based on the WHO 2012 assumptions with one change: the probability of a man with chlamydia developing symptoms was set at the value used in South African transmission dynamic models, 0.33 [10,38], rather than the WHO global value of 0.54.
Male urethritis syndrome: Case load and reporting completeness in 2017
Spectrum-estimated numbers of symptomatic cases of gonorrhea and chlamydia in 2017, and the subsets of these symptomatic cases treated, were compared to the national-level MUS case reports for 2017 collated by the South African District Health Management Information System (S2 File). Based on etiological data on the causes of MUS from South Africa [5,36,39,40] we have assumed 76% of MUS cases are due to gonorrhea and 24% to chlamydia, considering that 5% of MUS cases do not have a gonococcal and/or chlamydial etiology, but that the etiological studies found considerable rates of dual gonococcal plus chlamydia etiologies.
Gonorrhea: Antibiotic-resistance
The Spectrum-estimated incident cases in men were multiplied by antibiotic resistance prevalence estimates from the NICD gonococcal antimicrobial resistance surveillance among men with MUS in four provinces [4,5,41,42] to estimate the incident numbers of antibiotic-resistant gonorrhea in men from 2007 to 2017.
Sensitivity analysis
Univariate sensitivity analyses looked at relaxing the data inclusion criteria to include blood donors, who were excluded from the default estimation because of their likely non-representativeness of overall populations, as transfusion services often exclude donors with self-reported risks or observed infections (syphilis only); removing the representativeness weight adjustment (all three infections); and assuming no change in treatment coverage over time (all three infections). More general assumptions of the Spectrum-STI methodology have been addressed in sensitivity analyses in earlier publications [14,18,22].
Results
Syphilis
A total of 44 prevalence data points from pregnant women attending ANC were identified from 1985 and later: 5 data points from nation-wide routine ANC screening, and 39 national and sub-national sentinel surveys and prevalence studies (S2 File). In addition, 11 prevalence measurements from non-pregnant women (1990–2017) were also identified that met the study inclusion criteria. Fig 1A shows the adjusted prevalence data and the Spectrum estimation for women.
Fig 1. Estimated trends in active syphilis in South African adults, 15–49 years.
(a) prevalence in women; (b) prevalence in men; (c) incidence in women and men. Prevalence data shown have been adjusted for diagnostic test performance and under sampling of high-risk populations, as described in the methods and detailed in S1 File. Solid lines are the best estimate; dotted lines are 95% Confidence Intervals. Blood donor data are shown, but these were not used in the default scenario, they were only used in the sensitivity analysis.
The estimated prevalence in 2017 was 0.50% (0.32–0.80%) (Table 1), a marked decrease from the 1990 estimate of 11.3% (8.5–16.4%).
Table 1. Spectrum-estimated STI prevalence, incidence rates and incident case numbers, in South African women and men 15–49 years in 2017.
| STI | Metric | Women | Men | ||
|---|---|---|---|---|---|
| Point estimate | 95% CI | Point estimate | 95% CI | ||
| Active syphilis | Prevalence | 0.50% | 0.32% to 0.80% | 0.97% | 0.19% to 2.38% |
| Incidence rate per 100 000 adult person-years | 153 | 65 to 414 | 316 | 34 to 1,162 | |
| New incident cases | 23,175 | 9,900 to 62,500 | 47,500 | 5,100 to 173,000 | |
| Gonorrhea | Prevalence | 6.6% | 3.8% to 10.8% | 3.5% | 1.7% to 6.1% |
| Incidence rate per 100 000 adult person-years | 16,100 | 7,700–38,900 | 14,200 | 6,900–24,700 | |
| New incident cases | 2.3 million | 1.1–5.0 million | 2.2 million | 1.1–3.8 million | |
| Chlamydia | Prevalence | 14.7% | 9.9% to 21% | 6.0% | 3.8 to 10.4% |
| Incidence rate per 100 000 adult person-years | 14,400 | 8,000–33,100 | 24,900 | 14,100–40,800 | |
| New incident cases | 1.9 million | 1.1–3.8 million | 3.9 million | 2.2–6.3 million | |
95% CI = 95% confidence interval.
Fig 1B shows the corresponding prevalence estimates for men. In men, owing to a lack of data pre-1995 the prevalence from 1990 to 1995 was fixed at the 1995 level. Between 1995 and 2017 prevalence fell from 8.2% (4.1–13.2) to 0.97 (0.19–2.38). These estimates were based on the 8 data points identified in male general populations.
The number of new cases in 2017 (Table 1) was estimated to be 23,175 (9,900–62,500) in women and 475,000 (5,100–173,000) in men. The annual incidence (Fig 1C) mirrored the decline in prevalence, with incidence in 2017 9-fold lower in women and 5-fold lower in men than in 1995. The decline in incidence was less than the decline in prevalence reflecting a decrease in the average duration of infection between 1997 and 2006 owing to our assumption that treatment coverage increased over this period.
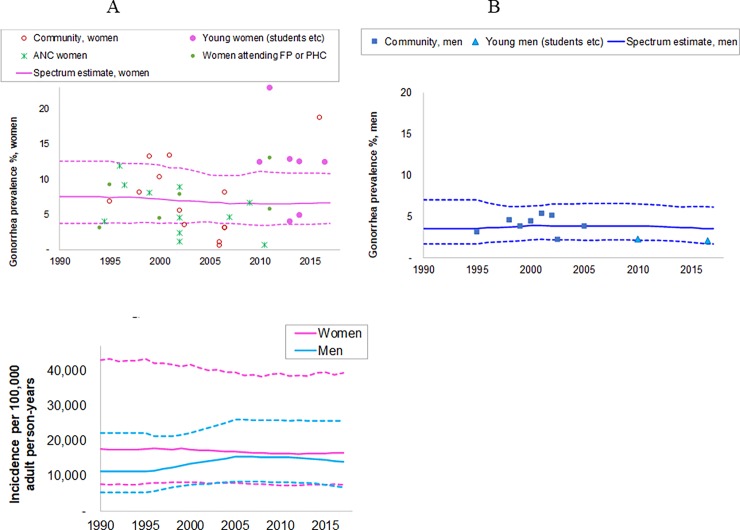
Gonorrhea
Forty-nine eligible prevalence measurements (36 female and 10 male) were identified between 1990 and 2017 (S1 File, Fig 2A and 2B). The data represented both urban and rural locations in all nine provinces.
Fig 2.
Estimated trends in gonorrhea in South African adults, 15–49 years: (a) prevalence in women; (b) prevalence in men; (c) incidence in women and men. Prevalence data shown have been adjusted for diagnostic test performance, urban/rural location, and under sampling of high-risk populations, as described in the methods and detailed in S1 File. Solid lines are best estimates; dotted lines are 95% Confidence Intervals. ANC = antenatal care clinic attendees, FP = family planning clinic attendees; PHC = Primary health clinic attendees.
The Spectrum estimated gonorrhea prevalence in 2017 was 6.6% (95% CI: 3.8–10.8%) in women and 3.5% (1.7–6.1%) in men (Fig 2A and 2B). Prevalence over 1990–2017 was stable in both sexes. The time trend in incidence of new infections mirrored this (Fig 2C), except for a slight increase between 1997 and 2006 in men when treatment coverage was assumed to increase to reflect the roll-out of syndromic treatment.
Spectrum estimated there were 2.3 (1.1–5.0) million and 2.2 (1.1–3.8) million new gonorrhea cases (i.e. episodes) in women and men in 2017 (Table 1). The case incidence rate and number of new cases were similar in men and women, despite the prevalence being higher in women, reflecting the longer average duration of infection in women.
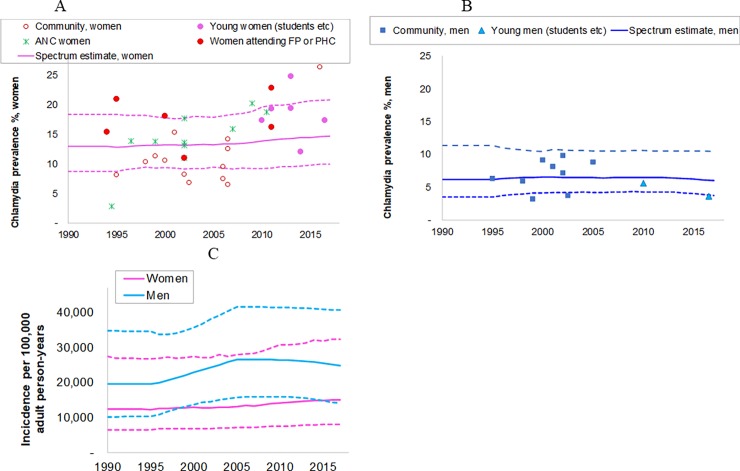
Chlamydia
For chlamydia, 46 prevalence data points (35 female and 11 male) were identified from the period 1994 to 2017 from urban and rural locations across all 9 provinces of South Africa.
Chlamydia prevalence in 2017 was estimated at 14.7% (9.9–21%) in women and 6.0% (3.8–10.4%) in men (Fig 3A & 3B). The time trend in prevalence over 1990–2017 was stable for both sexes and the incidence trend mirrored this apart from an increase over 1997 to 2006 when treatment coverage was assumed to increase.
Fig 3.
Estimated trends in chlamydia in South African adults, 15–49 years: (a) prevalence in women; (b) prevalence in men; (c) incidence in women and men. Prevalence data shown have been adjusted for diagnostic test performance, urban/rural location, and under sampling of high-risk populations, as described in the methods and detailed in S1 File. Solid lines are best estimates; dotted lines are 95% Confidence Intervals. ANC = antenatal care clinic attendees, FP = family planning clinic attendees; PHC = Primary health clinic attendees.
Spectrum estimated that there were 1.9 (1.1–3.8) million new chlamydia cases in women and 3.9 (2.2–6.3) million new infections in men in 2017 (Table 1). The chlamydia case incidence rate and number of new cases were higher in men than in women, despite chlamydia prevalence being higher in women, reflecting the longer average duration of infection in women.
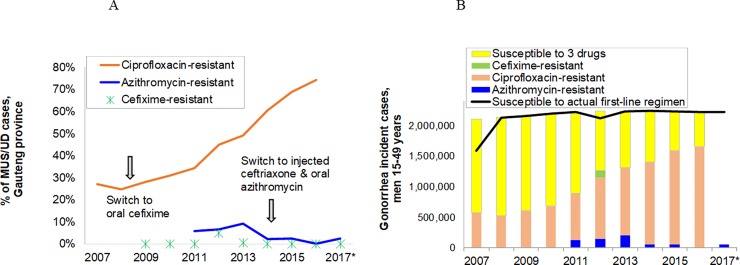
Gonorrhea: Antibiotic-resistance
Fig 4A shows the evolution of antibiotic resistance for gonorrhea, based on sentinel surveillance data from 2007 to 2017. In response to antimicrobial resistance trends, South Africa changed its first-line treatment regimen for MUS in 2008 from ciprofloxacin (used since 1993) to oral cefixime, and in 2014/15 from oral cefixime to dual injectable single-dose ceftriaxone & oral azithromycin [2], in accordance with WHO recommendations [43]. Dual antimicrobial cover for gonorrhoea is a strategy designed to curtail the emergence of extensively-drug resistant N. gonorrhoeae that is resistant to the extended-spectrum cephalosporins. This gained additional importance in 2012 with the first reports of cefixime resistance and resultant treatment failure for male urethritis in South Africa in two MSM [42], in recognition of the fact that there is a paucity of gonococcal antimicrobial resistance surveillance data from key population groups in the country.
Fig 4.
Spectrum estimates of antibiotic resistant gonorrhea, South Africa: (a) Proportion of gonorrhea cases among men presenting to PHCs with male urethritis syndrome in national sentinel surveillance; (b) estimated annual incident gonorrhea cases resistant and susceptible to the 3 first-line antibiotic treatments shown in Fig 4A. • Ciprofloxacin: Resistance data shown includes intermediate resistance (Minimum Inhibitory Concentration (MIC) = 0.12–0.50 μg/mL, and full resistance (MIC of ≥1 μg/mL) ([68]. • Azithromycin: Resistance as estimated and shown is defined as Intermediate resistance, i.e. MIC = 0.50 μg/mL [69]; • Cefixime: Resistance as estimated and shown is defined as MIC = 0.25 μg/mL [69]. Annual surveillance in Gauteng province did not detect any consistent, progressive and sustained increase by year in MIC50 (minimum antimicrobial concentration needed to inhibit 50% of isolates) & MIC90 (minimum antimicrobial concentration needed to inhibit 90% of isolates). • Ceftriaxone: Resistance, defined as MIC = 0.25 μg/mL (EUCAST 2018; version 8.0), was detected in 2/324 (0.6%) of cases surveyed in 2009, but in 0% of cases in 2008 and 2010–2017 (number of cases ranged from 128 to 338); and no significant increase in the MIC over time was detected. • In 2017 ciprofloxacin resistance was not tested by NICD; cefixime (CXM), ceftriaxone were tested and no resistance detected to the extended-spectrum cephalosporins. The prevalence of intermediate resistance to azithromycin was 1.8%. Sources: National Institute of Communicable Diseases [4,5,41,42].
The observed antibiotic resistance prevalence estimates from four provinces were applied to the population-level male gonorrhea prevalence estimates for 2007 to 2017. In each year the majority of cases were susceptible to the prevailing year’s first-line treatment (Fig 4B). The continued increase in the prevalence of N. gonorrheae resistance to ciprofloxacin after its withdrawal from use in STI syndromic management algorithms may reflect ongoing antimicrobial selection pressure arising from its use for other indications or its continued use by public and private STI treatment providers during shortages or stock-outs of the first line treatment [44]. In addition, there may be a fitness benefit conferred by ciprofloxacin-resistance associated mutations [45].
Male urethritis: Case load and reporting completeness
In 2017, of the 2.2 million Spectrum-estimated gonorrhea cases in adult men, 1.4 million were symptomatic and 850,000 million were treated (Table 2). For chlamydia Spectrum estimated 3.9 million cases in adult men in 2017 of which 1.3 million were symptomatic and 765,000 were treated. Using the gonorrhea estimates and assuming 74% of symptomatic MUS cases are due to gonorrhea the estimated number of treated MUS cases in 2017 was 1.1 million. A similar calculation for chlamydia, assuming 26% of symptomatic cases are due to chlamydia, comes to 3.2 million treated MUS cases.
Table 2. Incident cases of gonorrhea, chlamydia and male urethritis syndrome, and the subset who are symptomatic, treated and reported, and the implied MUS case reporting completeness in men 15–49 years in South Africa, 2017.
| Gonorrhea | Chlamydia | Source & assumptions | |
|---|---|---|---|
| Estimated incident cases | 2.21 million | 3.87 million | Spectrum-STI estimate |
| Estimated symptomatic cases | 1.42 million | 1.28 million | Assumed 64% of gonorrhea [19] and 33% of chlamydial infections [10] symptomatic. |
| Estimated symptomatic cases of gonorrhea or chlamydia treated | 850,000 | 765,000 | Assumed 60% of symptomatic cases treated [19]. |
| Estimated symptomatic MUS cases (all etiologies) treated | 1.12 million | 3.19 million | Assumed 74% of MUS cases due to gonorrhea and 26% due to chlamydia [5,36,39,40]. The 1.12 million and 3.11 million are two alternative, mutually exclusive estimates. |
| Actual new MUS case reports | 310,921 | ||
| Reporting completeness among treated MUS cases | 310,921 / 1.12 million = 28% |
310,921 / 3.19 million = 10% |
The 28% and the 10% are two alternative, mutually exclusive estimates. |
Abbreviations: MUS = Male Urethritis Syndrome.
The actual number of MUS cases reported by the South African STI program from public clinics was 310,921 (S2 File). Comparing the actual MUS cases to the Spectrum estimates of MUS cases treated suggests that case reporting completeness, among treated MUS cases, is somewhere between 10% and 28%.
Sensitivity analyses
Table 3 summarizes the results of the sensitivity analyses. Relaxing the study eligibility criteria for syphilis to include national blood donor screening data from 2015–2018 (S1 File) reduced the estimated prevalence of syphilis in women from 0.50% to 0.38% and in men from 0.97% to 0.35%. Including blood donor data had less of an impact on the prevalence in women than men owing to the large number of data points for women from ANC surveys and ANC-based routine screening. Including blood donors markedly reduced the male-to-female prevalence ratio, from almost 1.9:1 to 0.92:1, a figure much closer to the 1:1 ratio found in studies within South Africa [46], across East and Southern Africa [47–49], and elsewhere [20].
Table 3. Sensitivity analysis–effect of varying (selected) assumptions and values, on estimated national STI prevalence and numbers of new infections for adult men or women (15–49 years) in South Africa, in 2017.
| Scenario & STI | Syphilis | Gonorrhea | Chlamydia | Syphilis | Gonorrhea | Chlamydia | |||
|---|---|---|---|---|---|---|---|---|---|
| Metric | Prevalence | Incident cases | |||||||
| Sex | Women | Men | Women | Men | Women | Men | Men | Men | Men |
| Default scenario | 0.50% (0.32–0.80) |
0.97% (0.19–2.38) |
6.6% (3.8–10.8) |
3.5% (1.7–6.1) |
14.7% (9.9–21) |
6.0% (3.8–10.6) |
47,500 (5,100–173,000) |
2.2 (1.1–3.8) million |
3.9 (2.2–6.3) million |
| Including sex-specific blood donor screening data from 2015 to 2018 (see S1 File) | 0.38% (0.25–0.69) |
0.35% (0.19–0.52) |
− | − | − | − | 16,000 (4,900–49,800) |
− | − |
| All gonorrhea & chlamydia data points assigned the same statistical weight | − | − | 8.4% (4.7–13.4) |
2.7% (1.1–5.6) |
17.3% (11.7–23.9) |
5.1% (2.4–9.3) |
− | 1.8 (0.70–3.2) million |
3.2 (1.5–6.5) million |
| Scenario 4. All 3 STIs: Assume that treatment coverage stays at 35% throughout 2017 (instead of improving to 65%; for syphilis in M&F and for NG and CT in M) | − | − | − | − | − | − | 39,100 (4,200–142,700) |
1.8 (0.75–3.1) million |
3.4 (2.2–5.9) million |
‘−‘ means: Not assessed, because the outcome was not affected by the scenario.
Assigning the same weight to all studies increased the prevalence in 2017 of gonorrhea and chlamydia in women from 6.6% to 8.4% and from 14.7% to 17.3% (Table 3) reflecting the prevalence in two studies from 2017 that documented high prevalences for both infections in young women [50] and in a rural area with relatively poor access to health care [51]. For men, the prevalence of gonorrhea decreased from 3.5% to 2.7% and of chlamydia from 6.0% to 5.1% reflecting data from a study in young men [50]. Gonorrhea and chlamydia incidence estimates in men decreased proportionally; relative to the incidence estimates in this scenario, we would have estimated a correspondingly higher reporting completeness of routine national MUS case reporting: 11–35% of symptomatic treated cases, compared to 10–28% in the default estimates. The weighting did not materially change results for syphilis (Table 3).
Changing the treatment coverage assumptions such that treatment coverage had not improved between 1997 and 2006 and instead remained at the 1997 level reduced the estimated number of new cases in men in 2017 from 45,000 to 37,100 for syphilis, from 2.2 million to 1.8 million for gonorrhea, and from 3.8 to 3.4 million for chlamydia. The lower number of new cases in 2017 in this scenario reflects the assumed longer average duration of infection (constant throughout 1990–2017), driven by a lower (constant) treatment coverage throughout 2017.
Discussion
The Spectrum-STI estimates confirm the high burden of STIs in South Africa. The 2017 adult prevalence estimates of 6.6% and 3.4% for gonorrhea and 14.7% and 6.0% for chlamydia in women and men, respectively, are among the highest in the world [19] and the estimated prevalence of active syphilis of above 0.5% in both men and women remains high, too. Whilst the prevalence estimates of syphilis have fallen by more than an order of magnitude since 1990, gonorrhea and chlamydia prevalence have remained almost unchanged despite South Africa’s large investment in HIV and STI prevention and treatment efforts. The Spectrum estimates are comparable to those from the earlier South African transmission dynamic modeling exercises for 1990 to 2006 [10,13], which also estimated declines in syphilis but little change in gonorrhea or chlamydia.
STI case reports tell a slightly different story: data from the national reporting system show a steady decline in Genital Ulcer Syndrome (GUS), MUS and VDS between 2005 and 2016 from sentinel sites and national PHC clinics (S2 File). As the main causes of MUS are gonorrhoea and chlamydia and among sexually-transmitted aetiologies of VDS, chlamydia is predominant, assuming no changes in access to health care or in the reporting systems, this would suggest that the incidence of both infections had fallen. The discrepancy between the case reports and the estimates from both the Spectrum statistical model and transmission dynamic models highlight the need for renewed efforts to improve access to and reporting by health services, and collect independent population-level (non-clinic-based) data for these two infections on a regular basis. STI case reports are a useful piece of information, but as many other middle-income countries [17,52,53] have noted are not, on their own, sufficient indicators for monitoring STI progress or impact, or as programmatic goals.
The decline in the prevalence of syphilis is consistent with the decline in the proportion of genital ulcer syndromes (GUS) attributed to syphilis among mineworkers in Carletonville (Gauteng province) over 1986–1998 [54], and data from sub-national [39] and national syndrome etiological surveillance since 2007 [5,36,40]. It may reflect improvements in clinical STI services, including the expansion of syndromic management for GUS and partner notification in the public sector [55], rolling out a national ANC-based syphilis screening program between 1998 and 2013, screening for syphilis as part of the HIV program, and since 2009 offering (free) medical male circumcision. However, the decline may also have been driven by selective HIV/AIDS mortality among higher-risk individuals [56].
The decrease in syphilis in adult females has driven a parallel decline in congenital syphilis (CS) [57] and, whilst South Africa’s CS case rate is still above the WHO elimination threshold of 50 per 100,000 live births, progress is being made towards eliminating mother-to-child transmission of CS, a key objective of the NSP [1]. Expansion of dual syphilis/HIV testing at ANC, especially in more remote rural areas, and at PHCs for late ante-natal bookers, should help South Africa reach this target quicker.
The persistently high gonorrhea and chlamydia rates, similar to stable etiological fractions of these STIs in national etiological surveillance studies of VDS (S2 File) and MUS [5,36,39,40], indicate that the impact of primary HIV/STI prevention on gonorrhea and chlamydia has been modest. The picture for HIV is similar: epidemiological modelling of South Africa’s HIV epidemic and response indicates that whilst HIV incidence has declined from the levels reached at the end of the 1990s it remains high despite prevention efforts and increasing coverage of antiretroviral treatment [58].
Comparing the Spectrum estimates of the number of symptomatic men with gonorrhea or chlamydia with the number of MUS cases reported each year suggests that less than 28% of symptomatic cases in men (even apart from additional asymptomatic cases) are treated and reported through the NIDS. The missing cases are either not treated at all, treated in the public sector but not reported, or treated in the private sector or by informal providers and not reported. Getting a better understanding on these missing cases will help target surveillance, control and treatment efforts. There is also a need to better understand treatment and reporting in women.
Spectrum incidence estimates combined with gonococcal antimicrobial resistance prevalence data in Gauteng Province suggest that annual numbers of cases of gonorrhea resistant to first-line treatment have not increased, owing to changes made to the treatment regimens for gonorrhea in 2008 and 2014/5 (Fig 4B). As a result of effective monitoring of antimicrobial resistance and policy changes tailored according to resistance trends, the emergence and spread of extensively-drug resistant gonorrhea has not been observed.
The South African Spectrum STI estimation exercise provides information that can be used to inform STI estimation exercises in other countries. The male-to-female prevalence ratios for 2017, 0.53 for gonorrhea and 0.41 for chlamydia, are in line with earlier modeling estimates for South Africa [10–13] but are lower than the global ratios used in the WHO 2012 estimates (0.86 and 0.80) [19]. The lower male to female ratios in South Africa, compared to the global figures are in keeping with the relatively high STI burden in South Africa and the national STI syndromic management policy. Syndromic treatment is expected to treat more male than female STI patients as women are more often asymptomatic, symptoms in women are frequently non-specific, and women often have poorer access to health care services or decide not to seek care [59].
Limitations
The Spectrum-STI South African estimates are limited by the quality and representativeness of prevalence data, and by assumptions underlying the model and those made in the absence of data. Whilst there was a sufficient base to generate time trends for the three STIs for both men and women, there is considerable uncertainty for gonorrhea and chlamydia as the data are from studies done in different populations using different study designs. Many of the prevalence data points, especially for gonorrhea and chlamydia, are from research projects and the study population may not be representative of the general population. In addition, the studies are from different age groups and we have only made age adjustments in the case of chlamydia in women and these are crude adjustments. Other limits to the data include the range of different diagnostic tests used and whilst we have corrected for diagnostic sensitivities and specificities the correction factors may not be correct. For example, our prevalence estimates for 2017 may be too high if the studies included for recent years over-sampled higher-risk populations, or for chlamydia younger populations, or if recent studies used diagnostic tests of higher sensitivity than we assumed. The lack of data also precludes any analysis at the sub-national level, which with the current non-systematic data set would risk to confound diversity in demographic, socio-economic and behavioural variations with real geographical patterns.
The present estimates focused on data from the general population and were not informed by prevalence data from high-risk groups. A new version of the Spectrum model is under development that incorporates risk groups and means that the current, crude approach of adding 10% to the general population estimate to reflect these missing populations will no longer be required.
Recommendations
STI surveillance and control in South Africa would clearly benefit from regular, systematic prevalence screening. For surveillance, the ideal would be periodic (e.g. 3-yearly) cluster-sample surveys, in men and women, in selected urban and rural sites. Securing funding for expanded etiological STI screening will be challenging, but there are opportunities to add to existing or planned activities, such as in pregnant women, adolescent girls, young women and other high-risk women, and priority populations such as MSM [60]. In both routine health care settings and through outreach, this would ideally use point-of-care tests (POCTs) with acceptable performance characteristics (affordability, equipment-free testing and delivery of results within 30 minutes), and be accompanied by partner notification and treatment. Of commercially available POCTs for gonorrhoea and chlamydia screening, the Cepheid geneXpert CT/NG (duplex for Neisseria gonorrhoeae and Chlamydia trachomatis) has demonstrated acceptable performance in terms of sensitivity and specificity, including when used on non-invasive specimens such as first-void urine [61]. With the Cepheid Xpert MTB/Rif assay now widely implemented for tuberculosis screening across public health sector laboratories in South Africa, existing geneXpert diagnostic capacity for TB could be leveraged to include screening for asymptomatic STIs in at-risk populations, which would also enable pathogen-directed expedited partner therapy. Additionally, there is a need to reinforce the training of both public and private sector healthcare workers in correct STI syndromic management, through the use of continuing medical education activities and educational material, including visual aids. Studies evaluating STI services at both private and public healthcare facilities in South Africa have revealed that general knowledge regarding STI aetiologies and management and compliance with national treatment guidelines among healthcare workers is suboptimal [44,62], and this compromises quality of care resulting in the prescription of incorrect treatment regimens for STI syndromes.
There is also a need to strengthen case reporting in both the public and private sector if trends in case reports to be a meaningful indicator. For a start, conducting regular, periodic data quality audits at facility-level could assess the quality of existing reporting systems, and determine the degree of under-reporting. Also, MUS could be added to South Africa's Rapid Internal Performance Data Audit (RIPDA) tool [63,64], used by health facilities for internal auditing before the Auditor General evaluates the Department of Health performance by comparing data as found in facility-level source documents with data in the District Health Information System 2. Third, quarterly feedback to provinces and districts about STI indicator performance, could stimulate action. Fourth, printed booklets of the STI surveillance tools will promote consistent and frequent data collection in sentinel sites. Finally, setting case finding targets can be a helpful mechanism to promote consistent case reporting, especially when coupled with period evaluation of actual performance against those targets.
The stable high rates of gonorrhea and chlamydia highlight that syndromic case management is not sufficient to control STIs. One policy change that would make a difference is to remove the current age constraint on STI treatment among women presenting with VDS; at present a woman presenting with VDS is treated for an STI only if she is below 35 years of age, gives a history of a male partner with urethral discharge, or if she is a returning patient and reports no improvement in symptoms [2].
For gonorrhea treatment, the regularly revised treatment guidelines are adequate in view of antimicrobial resistance patterns in public-sector surveillance. However, antimicrobial resistance monitoring clearly remains a priority area–and there may be scope to extend screening for extensively-drug resistant gonorrhea to key populations such as MSM, to expand sampling to include symptomatic and asymptomatic men at both genital and extra-genital sites, and to expand resistance surveillance and prescription patterns in the private sector where ciprofloxacin continues to be prescribed [44].
South Africa’s high STI rates also underscore the national policy to not limit VMMC to HIV-negative men, but to also enable HIV-infected men, after clinical assessment and enrolment into HIV care, to receive VMMC, which may reduce their and their partners’ STI rates [65,66].
Conclusion
The Spectrum-STI estimates, based on STI surveillance and monitoring data, highlight the high burden of STIs in South Africa. Whilst the prevalence and incidence of syphilis in adults has fallen between 1990 and 2017, the prevalence and incidence of gonorrhea and chlamydia, with high burden especially in women who are often asymptomatic, have remained almost unchanged and are high relative to other countries. Both gonorrhea and chlamydia have health consequences for the infected individual and for babies born to infected mothers, and are established co-factors for HIV transmission [67], especially in partnerships where the HIV-infected partner is not on ART. Intensification of actions to prevent, detect and control STIs alongside HIV are important if the burden of STIs is to be reduced and would benefit from strengthened surveillance.
Supporting information
Including:
A Table. Syphilis prevalence data from surveys, studies and routine ANC-based program screening, used in the Spectrum-STI estimation of adult syphilis prevalence in South Africa With references: [7, 8, 19, 46, 50, 70–97].
B Table. Spectrum assumptions on proportion of episodes symptomatic, proportions of symptomatic episodes treated, episode durations for treated and untreated episodes, and the resulting treatment coverage-weighted average episode durations. With references: [10, 19, 38].
C Table. Gonorrhea and chlamydia prevalence data used, and adjustments for diagnostic test performance and missing high-risk populations, and for chlamydia for age, in the Spectrum-STI prevalence trend estimation for 15–49 year-old adults, South Africa. With references: [32, 46, 50, 51, 72, 77, 80, 81, 86, 91–93, 95, 98–116].
(XLSX)
(DOCX)
Acknowledgments
We thank Ms Eva Maruo and Ms Lufuno Malala (STI/HIV Prevention Unit, National Department of Health), Dr. Marion Vermeulen (South Africa National Blood Services, Head of Diagnostic Testing), Dr. Sinead Delaney-Moretlwe (University of the Witwatersrand, Wits Reproductive Health & HIV Institute), Ali Feizzadeh (UNAIDS South Africa) and other participants of a workshop in Pretoria, April 2018, for supporting data collection, Dr. Guy Mahiané (Avenir Health) for supporting adult syphilis estimations and the statistical design of Spectrum-STI, and Kendall Hecht (Avenir Health) for programming Spectrum’s online user interface, Prof. Laith Abu-Raddad (Weill Cornell Medical College—Qatar, Cornell University, Doha, Qatar) for support and advice regarding assumptions on chlamydia epidemiology, and Dr. Theodora Wi (WHO) for advice on antibiotic resistance surveillance and estimation. We wish to acknowledge and thank Dr Busisiwe Msimanga-Radebe (WHO South Africa) for her support and assistance with workshop logistics.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The project was funded by the World Health Organization, Department of Reproductive Health and Research. The views expressed in this paper are those of the authors and do not necessarily represent the position of the World Health Organization, or other affiliated organizations.
References
- 1.South African National AIDS Council. National Strategic Plan for HIV, TB and STIs 2017–2022. Pretoria 2017. http://sanac.org.za/wp-content/uploads/2017/05/NSP_FullDocument_FINAL.pdf
- 2.National Department of Health—Republic of South Africa. Sexually Transmitted Infections Management Guidelines, adapted from Standard Treatment Guidelines and Essential Drugs List Primary Health Care In: Standard Treatment Guidelines and Essential Drugs List for Primary Healthcare, editor.2015. [Google Scholar]
- 3.South Africa National Department of Health. National Integrated District Health Information System. Pretoria [cited 2018 07 June]; Available from: https://za.dhis.dhmis.org/dhis-web-commons/security/login.action.
- 4.Kularatne R, Maseko V, Gumede L, Readebe F, Kufa-Chakezha T. Neisseria gonorrhoeae antimicrobial resistance surveillance in Gauteng province, South Africa. Johannesburg 2016 September 3. http://www.nicd.ac.za/assets/files/Neisseria%20gonorrhoeae.pdf
- 5.Kularatne R. Aetiological surveillance of sexually transmitted infection syndromes at sentinel sites: GERMS-SA 2014–2016. Public Health Surveillance Bulletin. 2017. November;15:114–22. [Google Scholar]
- 6.World Health Organization. The Gonococcal Antimicrobial Surveillance Programme (GASP). Geneva [cited 2018 3 July]; Available from: http://www.who.int/reproductivehealth/topics/rtis/gasp_network/en/.
- 7.Dinh TH, Kamb ML, Msimang V, Likibi M, Molebatsi T, Goldman T, et al. Integration of preventing mother-to-child transmission of HIV and syphilis testing and treatment in antenatal care services in the Northern Cape and Gauteng provinces, South Africa. Sex Transm Dis. 2013. November;40(11):846–51. 10.1097/OLQ.0000000000000042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.South Africa National Department of Health. 2015 National Antenatal Sentinel HIV & Syphilis Survey Report. Pretoria 2017. http://www.health.gov.za/index.php/shortcodes/2015-03-29-10-42-47/2015-04-30-08-18-10/2015-04-30-08-21-56?download = 2584:2015-national-antenatal-hiv-prevalence-survey-final-23oct17
- 9.University of California San Francisco (UCSF), Anova Health Institute, Wits Reproductive Health and HIV Research Institute (WRHI). South African Health Monitoring Survey (SAHMS): An Integrated Biological and Behavioural Survey among Female Sex Workers, South Africa 2013–2014 Final Report San Francisco 2016 February. http://sanac.org.za/wp-content/uploads/2016/03/UCSF-South-African-Health-Monitoring-Survey_SAHMS_2016.pdf
- 10.Johnson LF, Alkema L, Dorrington RE. A Bayesian approach to uncertainty analysis of sexually transmitted infection models. Sex Transm Infect. 2010. June;86(3):169–74. 10.1136/sti.2009.037341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson LF, Coetzee DJ, Dorrington RE. Sentinel surveillance of sexually transmitted infections in South Africa: a review. Sex Transm Infect. 2005. August;81(4):287–93. 10.1136/sti.2004.013904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson LF, Geffen N. A Comparison of Two Mathematical Modeling Frameworks for Evaluating Sexually Transmitted Infection Epidemiology. Sex Transm Dis. 2016. March;43(3):139–46. 10.1097/OLQ.0000000000000412 [DOI] [PubMed] [Google Scholar]
- 13.Johnson LF, Dorrington RE, Bradshaw D, Coetzee DJ. The effect of syndromic management interventions on the prevalence of sexually transmitted infections in South Africa. Sex Reprod Healthc. 2011. January;2(1):13–20. 10.1016/j.srhc.2010.08.006 [DOI] [PubMed] [Google Scholar]
- 14.Korenromp EL, Mahiané G, Rowley J, Nagelkerke N, Abu-Raddad L, Ndowa F, et al. Estimating prevalence trends in adult gonorrhoea and syphilis prevalence in low- and middle-income countries with the Spectrum-STI model: results for Zimbabwe and Morocco from 1995 to 2016. Sex Transm Infect. 2017. 21 March;sextrans-2016-052953. 10.1136/sextrans-2016-052953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El Kettani A, Mahiané G, Abu-Raddad L, Smolak A, Rowley J, Nagelkerke N, et al. Trends in adult chlamydia and gonorrhea prevalence, incidence and urethral discharge case reporting in Morocco over 1995 to 2015 –estimates using the Spectrum-Sexually Transmitted Infection model. Sex Transm Dis. 2017. September;44(9):557–64. 10.1097/OLQ.0000000000000647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bennani A, El Rhilani H, El Kettani A, Alami K, Hançali A, Youbi M, et al. The prevalence and incidence of active syphilis in Morocco, 1995–2016: model-based estimation and implications for STI surveillance. PLoS One. 2017. 24 August;12(8):e0181498 10.1371/journal.pone.0181498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Badrakh J, Zayasaikhan S, Davaalkham J, Erdenetungalag E, Jadambaa N, Munkhbaatar S, et al. Trends in adult chlamydia and gonorrhea prevalence, incidence and urethral discharge case reporting in Mongolia over 1995–2016 –estimates using the Spectrum-STI model. Western Pac Surveill Response J. 2017. November;8(4). 10.5365/wpsar.2017.8.2.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Enkhbat E, Korenromp EL, Badrakh J, Zayasaikhan S, Baya P, Orgiokhuu E, et al. Estimating adult female syphilis prevalence, Congenital Syphilis case incidence and adverse birth outcomes due to Congenital Syphilis using the Spectrum Sexually Transmitted Infection surveillance tool, Mongolia 2000–2016. Infectious Disease Modelling. 2018;3:13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Newman L, Rowley J, VanderHoorn S, Wijesooriya NS, Unemo M, Stevens G, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS One. 2015;10(12):e0143304 10.1371/journal.pone.0143304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smolak A, Rowley J, Nagelkerke N, Kassebaum N, Chico RM, Korenromp EL, et al. Trends and predictors of syphilis prevalence in the general population: Global pooled analyses of 1103 prevalence measures including 136 million syphilis tests. Clin Infect Dis. 2017;November 9 10.1093/cid/cix975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ham DC, Lin C, Newman L, Wijesooriya NS, Kamb M. Improving global estimates of syphilis in pregnancy by diagnostic test type: A systematic review and meta-analysis. Int J Gynaecol Obstet. 2015. June;130 Suppl 1:S10–4. 10.1016/j.ijgo.2015.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Korenromp EL, Mahiané SG, Nagelkerke N, Taylor M, Williams R, Chico RM, et al. Syphilis prevalence trends in adult women in 132 countries–estimations using the Spectrum Sexually Transmitted Infections model. Scientific Reports. 2018;8(1). 10.1038/s41598-018-29805-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwartz S, Lambert A, Phaswana-Mafuya N, Kose Z, McIngana M, Holland C, et al. Engagement in the HIV care cascade and barriers to antiretroviral therapy uptake among female sex workers in Port Elizabeth, South Africa: findings from a respondent-driven sampling study. Sex Transm Infect. 2017. June;93(4):290–6. 10.1136/sextrans-2016-052773 [DOI] [PubMed] [Google Scholar]
- 24.Vickerman P, Terris-Prestholt F, Delany S, Kumaranayake L, Rees H, Watts C. Are targeted HIV prevention activities cost-effective in high prevalence settings? Results from a sexually transmitted infection treatment project for sex workers in Johannesburg, South Africa. Sex Transm Dis. 2006. October;33(10 Suppl):S122–32. 10.1097/01.olq.0000221351.55097.36 [DOI] [PubMed] [Google Scholar]
- 25.Gallant AR, Fuller WA. Fitting Segmented Polynomial Regression Models Whose Join Points Have to Be Estimated. J Am Statistical Association. 1973. March;68(341):144–7. [Google Scholar]
- 26.Park SH. Experimental Designs for Fitting Segmented Polynomial Regression Models. Technometrics 1978. May;20(2):151–4. [Google Scholar]
- 27.Lewis DA, Maruma E. Revision of the national guideline for first-line comprehensive management and control of sexually transmitted infections: what’s new and why?. South Afr J Epidemiol Infect. 2009;24(2):6–9. [Google Scholar]
- 28.Chico RM, Mayaud P, Ariti C, Mabey D, Ronsmans C, Chandramohan D. Prevalence of malaria and sexually transmitted and reproductive tract infections in pregnancy in sub-Saharan Africa: a systematic review. JAMA. 2012. May 16;307(19):2079–86. 10.1001/jama.2012.3428 [DOI] [PubMed] [Google Scholar]
- 29.Orroth KK, Korenromp EL, White RG, Changalucha J, de Vlas SJ, Gray RH, et al. Comparison of STD prevalences in the Mwanza, Rakai, and Masaka trial populations: the role of selection bias and diagnostic errors. Sex Transm Infect. 2003. April;79(2):98–105. 10.1136/sti.79.2.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Population Prospects: the 2015 revision 2015. Available from: http://esa.un.org/unpd/wpp/.
- 31.Rebe K, Lewis D, Myer L, de Swardt G, Struthers H, Kamkuemah M, et al. A Cross Sectional Analysis of Gonococcal and Chlamydial Infections among Men-Who-Have-Sex-with-Men in Cape Town, South Africa. PLoS One. 2015;10(9):e0138315 10.1371/journal.pone.0138315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peters RP, Dubbink JH, van der Eem L, Verweij SP, Bos ML, Ouburg S, et al. Cross-sectional study of genital, rectal, and pharyngeal Chlamydia and gonorrhea in women in rural South Africa. Sex Transm Dis. 2014. September;41(9):564–9. 10.1097/OLQ.0000000000000175 [DOI] [PubMed] [Google Scholar]
- 33.Kapiga S, Kelly C, Weiss S, Daley T, Peterson L, Leburg C, et al. Risk factors for incidence of sexually transmitted infections among women in South Africa, Tanzania, and Zambia: results from HPTN 055 study. Sex Transm Dis. 2009. April;36(4):199–206. 10.1097/OLQ.0b013e318191ba01 [DOI] [PubMed] [Google Scholar]
- 34.Adams EJ, Charlett A, Edmunds WJ, Hughes G. Chlamydia trachomatis in the United Kingdom: a systematic review and analysis of prevalence studies. Sex Transm Infect. 2004. October;80(5):354–62. 10.1136/sti.2003.005454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.USA Centers for Disease Control and Prevention. Sexually Transmitted Diseases Surveillance: Chlamydia Profiles, 2011. Atlanta 2011, updated March 2013. http://www.cdc.gov/std/chlamydia2011/default.htm
- 36.Kularatne R. Sentinel surveillance of sexually transmitted infection syndrome aetiologies and HPV genotypes among patients attending Primary Health Care facilities in South Africa, April 2014—September 2015 Johannesburg: Center for HIV and STIs, National Institute for Communicable Diseases; 2017. April 3. [Google Scholar]
- 37.Omori R, Chemaitelly H, Althaus CL, Abu-Raddad L. Does infection with Chlamydia trachomatis induce long-lasting partial immunity? Insights from mathematical modeling. Sex Transm Infect. 2018. 10.1136/sextrans-2018-053543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Korenromp EL, Sudaryo MK, de Vlas SJ, Gray RH, Sewankambo NK, Serwadda D, et al. What proportion of episodes of gonorrhoea and chlamydia becomes symptomatic? Int J STD AIDS. 2002. February;13(2):91–101. 10.1258/0956462021924712 [DOI] [PubMed] [Google Scholar]
- 39.Mhlongo S, Magooa P, Muller EE, Nel N, Radebe F, Wasserman E, et al. Etiology and STI/HIV coinfections among patients with urethral and vaginal discharge syndromes in South Africa. Sex Transm Dis. 2010. September;37(9):566–70. 10.1097/OLQ.0b013e3181d877b7 [DOI] [PubMed] [Google Scholar]
- 40.Kularatne R, Puren A. Sentinel surveillance of sexually transmitted infection (STI) syndrome aetiologies among patients attending a public healthcare facility in Johannesburg: report on the findings from 2015 and comparison with 2014 data. Johannesburg 2016 February 2. http://www.nicd.ac.za/assets/files/Sentinel%20surveillance-STI.pdf
- 41.Lewis DA, Scott L, Slabbert M, Mhlongo S, van Zijl A, Sello M, et al. Escalation in the relative prevalence of ciprofloxacin-resistant gonorrhoea among men with urethral discharge in two South African cities: association with HIV seropositivity. Sex Transm Infect. 2008. October;84(5):352–5. 10.1136/sti.2007.029611 [DOI] [PubMed] [Google Scholar]
- 42.Lewis DA, Sriruttan C, Muller EE, Golparian D, Gumede L, Fick D, et al. Phenotypic and genetic characterization of the first two cases of extended-spectrum-cephalosporin-resistant Neisseria gonorrhoeae infection in South Africa and association with cefixime treatment failure. J Antimicrob Chemother. 2013. June;68(6):1267–70. 10.1093/jac/dkt034 [DOI] [PubMed] [Google Scholar]
- 43.World Health Organization. Guidelines for the treatment of Neisseria gonorrhoeae. Geneva 2016 June. www.who.int/reproductivehealth/publications/rtis/gonorrhoea-treatment-guidelines/en [PubMed]
- 44.Kohler PK, Marumo E, Jed SL, Mema G, Galagan S, Tapia K, et al. A national evaluation using standardised patient actors to assess STI services in public sector clinical sentinel surveillance facilities in South Africa. Sex Transm Infect. 2017. June;93(4):247–52. 10.1136/sextrans-2016-052930 [DOI] [PubMed] [Google Scholar]
- 45.Unemo M, Shafer WM. Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century: past, evolution, and future. Clin Microbiol Rev. 2014. July;27(3):587–613. 10.1128/CMR.00010-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Williams BG, Taljaard D, Campbell CM, Gouws E, Ndhlovu L, Van Dam J, et al. Changing patterns of knowledge, reported behaviour and sexually transmitted infections in a South African gold mining community. AIDS. 2003. September 26;17(14):2099–107. 10.1097/01.aids.0000076323.42412.26 [DOI] [PubMed] [Google Scholar]
- 47.ICAP project at Columbia University, Centers for Disease Control USA, Zimbabwe National AIDS Council (NAC), Zimbabwe National Statistics Agency (ZIMSTAT), Zimbabwe Biomedical Research and Training Institute (BRTI). Zimbabwe population-based HIV impact assessment ZIMPHIA 2015–2016. Fact sheet. Washington DC 2016 December. http://phia.icap.columbia.edu/wp-content/uploads/2016/11/ZIMBABWE-Factsheet.FIN_.pdf
- 48.Zambia Ministry of Communicable Diseases Maternal and Child Health, United States of America Centers for Disease Control and Prevention, ICAP at Columbia University, Zambia Central Statistical Office, Zambia Tropical Diseases Research Centre University of Zambia, University Teaching Hospital, Zambia National HIV/AIDS/STI/TB Council, Zambian National Public Health Institute, WESTAT. Zambia Population-based HIV impact assessment (ZAMPHIA) 2016. First report. Lusaka 2017 December. http://phia.icap.columbia.edu/wp-content/uploads/2017/11/FINAL-ZAMPHIA-First-Report_11.30.17_CK.pdf
- 49.ICAP project at Columbia University, Centers for Disease Control USA, Westat. Uganda population-based HIV impact assessment UPHIA 2016–2017. Summary sheet: preliminary findings. Washington DC 2017 December. http://phia.icap.columbia.edu/wp-content/uploads/2017/09/UPHIA-Uganda-factsheet_A4.new_HR.pdf
- 50.Francis SC, Mthiyane TN, Baisley K, McHunu SL, Ferguson JB, Smit T, et al. Prevalence of sexually transmitted infections among young people in South Africa: A nested survey in a health and demographic surveillance site. PLoS Med. 2018. February;15(2):e1002512 10.1371/journal.pmed.1002512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hoffman CM, Mbambazela N, Sithole P, Morre SA, Dubbink JH, Railton J, et al. Provision of STI services in a mobile clinic reveals high unmet need in remote areas of South Africa: a cross-sectional study. Submitted. [DOI] [PubMed] [Google Scholar]
- 52.Korenromp EL, Rios CY, Sabogal Apolinar AL, Caicedo S, Cuellar D, Cardenas Cañon IM, et al. Adult syphilis, chlamydia and gonorrhea prevalence and incidence, and congenital syphilis incidence in Colombia, 1995–2016 –estimates using the Spectrum-STI model. Pan-American journal of Public Health. 2018;42:e118 doi: 10.26633/RPSP.2018.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rowley J, Korenromp EL. A pilot application of the Spectrum-STI model in a low-prevalence setting: Estimation of STI prevalence and incidence trends in Georgia. Technical Report, based on a workshop in Tbilisi, Georgia, August 23-24th 2017. London 2017 13 December. https://spectrummodel.zendesk.com/hc/en-us/articles/115003492452-Georgia-Spectrum-STI-estimation-2017-final-report & https://spectrummodel.zendesk.com/hc/en-us/articles/115003469011-Georgia-Spectrum-STI-estimation-2017-annex-to-final-report
- 54.Htun Y, Radebe F, Fehler HG, Ballard RC. Changes in the patterns of sexually transmitted infection among South African mineworkers, associated with the emergence of the HIV/AIDS epidemic. S Afr Med J. 2007. November;97(11 Pt 3):1155–60. [PubMed] [Google Scholar]
- 55.Department of Health Republic of South Africa. Sexually Transmitted Infections. Johannesburg 2008 July-September 3.
- 56.Kenyon CR, Osbak K, Buyze J, Chico RM. The changing relationship between bacterial STIs and HIV prevalence in South Africa—an ecological study. Int J STD AIDS. 2015. July;26(8):556–64. 10.1177/0956462414546392 [DOI] [PubMed] [Google Scholar]
- 57.Korenromp EL, Rowley J, Alonso MA, Brito de Mello M, Wijesooriya S, Mahiané G, et al. Global burden of maternal and congenital syphilis and associated adverse birth outcomes–estimates for 2016 and progress since 2012 Submitted (June 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johnson LF, Hallett TB, Rehle TM, Dorrington RE. The effect of changes in condom usage and antiretroviral treatment coverage on human immunodeficiency virus incidence in South Africa: a model-based analysis. J R Soc Interface. 2012. July 7;9(72):1544–54. 10.1098/rsif.2011.0826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Meyer-Weitz A, Reddy P, Van den Borne HW, Kok G, Pietersen J. Health care seeking behaviour of patients with sexually transmitted diseases: determinants of delay behaviour. Patient Educ Couns. 2000. Oct-Nov;41(3):263–74. [DOI] [PubMed] [Google Scholar]
- 60.World Health Organization. Global health sector strategy on sexually transmitted infections 2016–2021. Towards ending STIs. Report. Geneva 2016 June. Report No.: WHO/RHR/16.09. http://apps.who.int/iris/bitstream/10665/246296/1/WHO-RHR-16.09-eng.pdf?ua=1
- 61.Unemo M, Bradshaw CS, Hocking JS, de Vries HJC, Francis SC, Mabey D, et al. Sexually transmitted infections: challenges ahead. Lancet Infect Dis. 2017. August;17(8):e235–e79. 10.1016/S1473-3099(17)30310-9 [DOI] [PubMed] [Google Scholar]
- 62.Ham DC, Hariri S, Kamb M, Mark J, Ilunga R, Forhan S, et al. Quality of Sexually Transmitted Infection Case Management Services in Gauteng Province, South Africa: An Evaluation of Health Providers' Knowledge, Attitudes, and Practices. Sex Transm Dis. 2016. January;43(1):23–9. 10.1097/OLQ.0000000000000383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Solomon W, Brown J, editors. South Africa Rapid Internal Performance Data Audit (RIPDA). Health Systems Trust Conference; 2016 May; Boksburg.
- 64.Department of Health Republic of South Africa. South Africa's Rapid Internal Performance Data Audit (RIPDA) tool & guideline. 2018 [cited 2018 26 Sept.]; Pretoria. Available from: https://ripda.dhis.dhmis.org/.
- 65.Friedman B, Khoury J, Petersiel N, Yahalomi T, Paul M, Neuberger A. Pros and cons of circumcision: an evidence-based overview. Clin Microbiol Infect. 2016. September;22(9):768–74. 10.1016/j.cmi.2016.07.030 [DOI] [PubMed] [Google Scholar]
- 66.Grund JM, Bryant TS, Jackson I, Curran K, Bock N, Toledo C, et al. Association between male circumcision and women's biomedical health outcomes: a systematic review. Lancet Glob Health. 2017. November;5(11):e1113–e22. 10.1016/S2214-109X(17)30369-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Korenromp EL, de Vlas SJ, Nagelkerke NJ, Habbema JD. Estimating the magnitude of STD cofactor effects on HIV transmission: how well can it be done? Sex Transm Dis. 2001. November;28(11):613–21. [DOI] [PubMed] [Google Scholar]
- 68.M100 Performance Standards for Antimicrobial Susceptibility Testing. 28th ed. Weinstein MP, editor2018.
- 69.European Committee on Antimicrobial Susceptibility Testing: guidelines 2018 version 8.02018.
- 70.O'Farrell N, Hoosen AA, Kharsany AB, van den Ende J. Sexually transmitted pathogens in pregnant women in a rural South African community. Genitourin Med. 1989. August;65(4):276–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Donders GG, Desmyter J, De Wet DH, Van Assche FA. The association of gonorrhoea and syphilis with premature birth and low birthweight. Genitourin Med. 1993. April;69(2):98–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Auvert B, Males S, Puren A, Taljaard D, Carael M, Williams B. Can highly active antiretroviral therapy reduce the spread of HIV?: A study in a township of South Africa. J Acquir Immune Defic Syndr. 2004. April 20;36(1):613–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Coetzee N. Syphilis in women attending antenatal clinics in the Western Cape: a pilot investigation into the use of a laboratory based surveillance scheme. Cape Town: University of Cape Town Department of Community Health; 1994. [Google Scholar]
- 74.Dietrich M, Hoosen AA, Moodley J, Moodley S. Urogenital tract infections in pregnancy at King Edward VIII Hospital, Durban, South Africa. Genitourin Med. 1992. February;68(1):39–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Opai-Tetteh ET, Hoosen AA, Moodley J. Re-screening for syphilis at the time of delivery in areas of high prevalence. S Afr Med J. 1993. October;83(10):725–6. [PubMed] [Google Scholar]
- 76.Qolohle DC, Hoosen AA, Moodley J, Smith AN, Mlisana KP. Serological screening for sexually transmitted infections in pregnancy: is there any value in re-screening for HIV and syphilis at the time of delivery? Genitourin Med. 1995. April;71(2):65–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Govender L, Hoosen AA, Moodley J, Moodley P, Sturm AW. Bacterial vaginosis and associated infections in pregnancy. Int J Gynaecol Obstet. 1996. October;55(1):23–8. 0020729296027440 [pii] [DOI] [PubMed] [Google Scholar]
- 78.Kharsany AB, Hoosen AA, Moodley J. Bacterial vaginosis and lower genital tract infections in women attending out-patient clinics at a tertiary institution serving a developing community. J Obstet Gynaecol. 1997. March;17(2):171–5. 10.1080/01443619750113807 [DOI] [PubMed] [Google Scholar]
- 79.Funk M, Pistorius LR, Pattison RC. Antenatal screening for bacterial vaginosis using the amine test. S Afr J Epidemiol Infect. 1996;11:74–6. [Google Scholar]
- 80.Sturm A, Moodley P, Sturm P, Karim F, Khan N, editors. Trends in the prevalence of sexually transmitted infections and HIV in pregnant women in KwaZulu/Natal from 1995 to 2002. South African AIDS Conference; 2003; Durban.
- 81.Sturm AW, Wilkinson D, Ndovela N, Bowen S, Connolly C. Pregnant women as a reservoir of undetected sexually transmitted diseases in rural South Africa: implications for disease control. Am J Public Health. 1998. August;88(8):1243–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mashiane Y, Chephe JH, Hoosen AA. Syphilis in pregnancy at Ga-Rankuwa Hospital: high prevalence and the need for intervention. Southern African Journal of Epidemiology and Infection 1999;14:13–5. [Google Scholar]
- 83.Dawadi BR, Joubert G, Hiemstra LA. Syphilis serology testing of pregnant women in Whittlesea district, Eastern Cape province, South Africa. Southern African Journal of Epidemiology and Infection. 2001;16:117–21. [Google Scholar]
- 84.Myer L, Wilkinson D, Lombard C, Zuma K, Rotchford K, Karim SS. Impact of on-site testing for maternal syphilis on treatment delays, treatment rates, and perinatal mortality in rural South Africa: a randomised controlled trial. Sex Transm Infect. 2003. June;79(3):208–13. 10.1136/sti.79.3.208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bronzan RN, Mwesigwa-Kayongo DC, Narkunas D, Schmid GP, Neilsen GA, Ballard RC, et al. On-site rapid antenatal syphilis screening with an immunochromatographic strip improves case detection and treatment in rural South African clinics. Sex Transm Dis. 2007. July;34(7 Suppl):S55–60. 10.1097/01.olq.0000245987.78067.0c [DOI] [PubMed] [Google Scholar]
- 86.Frohlich JA, Abdool Karim Q, Mashego MM, Sturm AW, Abdool Karim SS. Opportunities for treating sexually transmitted infections and reducing HIV risk in rural South Africa. J Adv Nurs. 2007. November;60(4):377–83. 10.1111/j.1365-2648.2007.04405.x [DOI] [PubMed] [Google Scholar]
- 87.Mothupi R, Mtezuka L, Bereda E, Mbelle N, Moodley S, Buchmann EJ, editors. A retrospective study of the seroprevalence of syphilis in antenatal admissions at Chris Hani Baragwanath Hospital. 2nd Joint Congress of the Federation of Infectious Diseases Societies of Southern Africa; 2007; Cape Town, South Africa.
- 88.South Africa Dept. of Health. National HIV and Syphilis antenatal seroprevalence surveys in South Africa. Pretoria 2000, 2002, 2003, 2004, 2006, 2007, 2008, 2009, 2010, 2011, 2015. http://www.gov.za/sites/www.gov.za/files/hivsyphilis_0.pdf and others
- 89.Sebitloane HM, Moodley J, Esterhuizen TM. Pathogenic lower genital tract organisms in HIV-infected and uninfected women, and their association with postpartum infectious morbidity. S Afr Med J. 2011. June 27;101(7):466–9. [PubMed] [Google Scholar]
- 90.Perti T, Nyati M, Gray G, De Bruyn G, Selke S, Magaret A, et al. Frequent genital HSV-2 shedding among women during labor in Soweto, South Africa. Infect Dis Obstet Gynecol. 2014;2014:258291 10.1155/2014/258291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Colvin M, Abdool Karim SS, Connolly C, Hoosen AA, Ntuli N. HIV infection and asymptomatic sexually transmitted infections in a rural South African community. Int J STD AIDS. 1998. September;9(9):548–50. 10.1258/0956462981922683 [DOI] [PubMed] [Google Scholar]
- 92.Williams BG, Gilgen D, Campbell C, Taljaard D, MacPhail C. The natural history of HIV / AIDS in South Africa: A biomedical and social survey in Carletonville. Johannesburg:. Johannesburg: Council for Scientific and Industrial Research; 2000. [Google Scholar]
- 93.Ndhlovu L, Searle C, Van Dam J, Mzaidume Y, Rasego B, Moema S. Reducing the transmission of HIV and sexually transmitted infections in a mining community: Findings from the Carletonville Mothusimpilo intervention project: 1998 to 2001. Washington, DC: Population Council2005. http://www.popcouncil.org/pdfs/horizons/crltnvll.pdf
- 94.Cronje HS, Joubert G, Muir A, Chapman RD, Divall P, Bam RH. Prevalence of vaginitis, syphilis and HIV infection in women in the Orange Free State. S Afr Med J. 1994. September;84(9):602–5. [PubMed] [Google Scholar]
- 95.Schneider H, Coetzee DJ, Fehler HG, Bellingan A, Dangor Y, Radebe F, Ballard RC. Screening for sexually transmitted diseases in rural South African women. Sex Transm Infect. 1998. June;74 Suppl 1:S147–52. [PubMed] [Google Scholar]
- 96.Devjee J, Moodley J, Singh M. Syphilis in pregnancy—prevalence at different levels of health care in Durban. S Afr Med J. 2006. November;96(11):1182–4. [PubMed] [Google Scholar]
- 97.McKinnon L, Kharsany ABM, Cawood C, Khanyile D, Grobler A, Goodman T, et al. High rates of sexually transmitted infections: results from the population-based household survey in KwaZulu-Natal, South Africa. International AIDS Conference; Durban, South Africa2016.
- 98.Pettifor AE, Kleinschmidt I, Levin J, Rees HV, MacPhail C, Madikizela-Hlongwa L, et al. A community-based study to examine the effect of a youth HIV prevention intervention on young people aged 15–24 in South Africa: results of the baseline survey. Trop Med Int Health. 2005. October;10(10):971–80. 10.1111/j.1365-3156.2005.01483.x [DOI] [PubMed] [Google Scholar]
- 99.Auvert B, Buve A, Lagarde E, Kahindo M, Chege J, Rutenberg N, et al. Male circumcision and HIV infection in four cities in sub-Saharan Africa. Aids. 2001. August;15 Suppl 4:S31–40. [DOI] [PubMed] [Google Scholar]
- 100.Hurkchand HP, Levine JB, Makuluma H, Molefe N, editors. Measuring the impact of HIV and STIs in a cluster designed household prevalence survey in a coal mining community, eMbalenhle, Mpumalanga, South Africa. 15th International AIDS Conference; 2004; Bangkok, Thailand.
- 101.Black V, Magooa P, Radebe F, Myers M, Pillay C, Lewis DA. The detection of urethritis pathogens among patients with the male urethritis syndrome, genital ulcer syndrome and HIV voluntary counselling and testing clients: should South Africa's syndromic management approach be revised? Sex Transm Infect. 2008. August;84(4):254–8. 10.1136/sti.2007.028464 [DOI] [PubMed] [Google Scholar]
- 102.O'Leary A, Jemmott JB 3rd, Jemmott LS, Teitelman A, Heeren GA, Ngwane Z, Icard LD, Lewis DA. Associations between psychosocial factors and incidence of sexually transmitted disease among South African adolescents. Sex Transm Dis. 2015. March;42(3):135–9. 10.1097/OLQ.0000000000000247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rours GIJG, Verkooyen RP, Ye H, Radebe F, Rothberg AD, Cooper PA, et al. Sexually transmitted infections in pregnant urban South African women: socio-economic characteristics and risk factors. Southern African Journal of Epidemiology and Infection 2006;21:14–9. [Google Scholar]
- 104.Odendaal HJ, Schoeman J, Grové D, de Jager M, Theron GB, Orth H, et al. The association between Chlamydia trachomatis genital infection and spontaneous preterm labour. South African Journal of Obstetrics and Gynaecology. 2006;12:146–9. [Google Scholar]
- 105.Sturm PD, Connolly C, Khan N, Ebrahim S, Sturm AW. Vaginal tampons as specimen collection device for the molecular diagnosis of non-ulcerative sexually transmitted infections in antenatal clinic attendees. Int J STD AIDS. 2004. February;15(2):94–8. 10.1258/095646204322764271 [DOI] [PubMed] [Google Scholar]
- 106.De Jongh M, Lekalakala MR, Le Roux M, Hoosen AA. Risk of having a sexually transmitted infection in women presenting at a termination of pregnancy clinic in Pretoria, South Africa. J Obstet Gynaecol. 2010;30(5):480–3. 10.3109/01443611003797687 [DOI] [PubMed] [Google Scholar]
- 107.Moodley D, Moodley P, Sebitloane M, Soowamber D, McNaughton-Reyes HL, Groves AK, et al. High prevalence and incidence of asymptomatic sexually transmitted infections during pregnancy and postdelivery in KwaZulu Natal, South Africa. Sex Transm Dis. 2015. January;42(1):43–7. 00007435-201501000-00010 [pii] 10.1097/OLQ.0000000000000219 [DOI] [PubMed] [Google Scholar]
- 108.Jespers V, Crucitti T, Menten J, Verhelst R, Mwaura M, Mandaliya K, et al. Prevalence and correlates of bacterial vaginosis in different sub-populations of women in sub-Saharan Africa: a cross-sectional study. PLoS One. 2014;9(10):e109670 10.1371/journal.pone.0109670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fehler HG, Lyall M, Htun Y, Muiznieks S, Khoza BD, Ballard RC. Genital tract infections among women attending an urban family planning clinic. Southern African Journal of Epidemiology and Infection. 1998;13:79–82. [Google Scholar]
- 110.Kleinschmidt I, Rees H, Delany S, Smith D, Dinat N, Nkala B, et al. Injectable progestin contraceptive use and risk of HIV infection in a South African family planning cohort. Contraception. 2007. June;75(6):461–7. 10.1016/j.contraception.2007.02.002 [DOI] [PubMed] [Google Scholar]
- 111.Guffey MB, Richardson B, Husnik M, Makanani B, Chilongozi D, Yu E, et al. HPTN 035 phase II/IIb randomised safety and effectiveness study of the vaginal microbicides BufferGel and 0.5% PRO 2000 for the prevention of sexually transmitted infections in women. Sex Transm Infect. 2014. August;90(5):363–9. 10.1136/sextrans-2014-051537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.McCormack S, Ramjee G, Kamali A, Rees H, Crook AM, Gafos M, et al. PRO2000 vaginal gel for prevention of HIV-1 infection (Microbicides Development Programme 301): a phase 3, randomised, double-blind, parallel-group trial. Lancet. 2010. October 16;376(9749):1329–37. 10.1016/S0140-6736(10)61086-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kleppa E, Holmen SD, Lillebo K, Kjetland EF, Gundersen SG, Taylor M, et al. Cervical ectopy: associations with sexually transmitted infections and HIV. A cross-sectional study of high school students in rural South Africa. Sex Transm Infect. 2015. March;91(2):124–9. sextrans-2014-051674 [pii] 10.1136/sextrans-2014-051674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Palanee-Phillips T, Schwartz K, Brown ER, Govender V, Mgodi N, Kiweewa FM, et al. Characteristics of Women Enrolled into a Randomized Clinical Trial of Dapivirine Vaginal Ring for HIV-1 Prevention. PLoS One. 2015;10(6):e0128857 10.1371/journal.pone.0128857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Giuliano AR, Botha MH, Zeier M, Abrahamsen ME, Glashoff RH, van der Laan LE, et al. High HIV, HPV, and STI prevalence among young Western Cape, South African women: EVRI HIV prevention preparedness trial. J Acquir Immune Defic Syndr. 2015. February 1;68(2):227–35. 10.1097/QAI.0000000000000425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Barnabas SL, Dabee S, Passmore JS, Jaspan HB, Lewis DA, Jaumdally SZ, et al. Converging epidemics of sexually transmitted infections and bacterial vaginosis in southern African female adolescents at risk of HIV. Int J STD AIDS. 2018. May;29(6):531–9. 10.1177/0956462417740487 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Including:
A Table. Syphilis prevalence data from surveys, studies and routine ANC-based program screening, used in the Spectrum-STI estimation of adult syphilis prevalence in South Africa With references: [7, 8, 19, 46, 50, 70–97].
B Table. Spectrum assumptions on proportion of episodes symptomatic, proportions of symptomatic episodes treated, episode durations for treated and untreated episodes, and the resulting treatment coverage-weighted average episode durations. With references: [10, 19, 38].
C Table. Gonorrhea and chlamydia prevalence data used, and adjustments for diagnostic test performance and missing high-risk populations, and for chlamydia for age, in the Spectrum-STI prevalence trend estimation for 15–49 year-old adults, South Africa. With references: [32, 46, 50, 51, 72, 77, 80, 81, 86, 91–93, 95, 98–116].
(XLSX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.