Abstract
Research indicates that high levels of sedentary behavior (sitting or lying with low energy expenditure) are adversely associated with health. A key factor in improving our understanding of the impact of sedentary behavior (and patterns of sedentary time accumulation) on health is the use of objective measurement tools that collect date and time-stamped activity information. One such tool is the activPAL monitor. This thigh-worn device uses accelerometer-derived information about thigh position to determine the start and end of each period spent sitting/lying, standing, and stepping, as well as stepping speed, step counts, and postural transitions. The activPAL is increasingly being used within field-based research for its ability to measure sitting/lying via posture. We summarise key issues to consider when using the activPAL in physical activity and sedentary behavior field-based research with adult populations. It is intended that the findings and discussion points be informative for researchers who are currently using activPAL monitors or are intending to use them. Pre-data collection decisions, monitor preparation and distribution, data collection considerations, and manual and automated data processing possibilities are presented using examples from current literature and experiences from 2 research groups from the UK and Australia.
Keywords: Inclinometer, Measurement, Physical activity, Posture, Sedentary behavior, Sitting
1. Introduction
Over the past decade, there has been substantial, and growing, scientific interest in sedentary behavior.1, 2, 3 In 2012, an expert consensus defined sedentary behavior as “any waking activity characterised by an energy expenditure ≤1.5 metabolic equivalents and a sitting or reclining posture”.4 It is now recognised that sedentary behavior is common (on average adults spend 46%–73% of waking hours sedentary),5, 6, 7, 8, 9, 10 and that too much time spent sedentary may be detrimental to health both in the short term11, 12, 13, 14 and long term.3, 15, 16, 17
The availability of objective measurement tools with date and time-stamped information about activity is a key factor in improving our understanding of the impact of sedentary behavior and patterns of sedentary time accumulation on health. Most of the evidence on the associations of objectively assessed sedentary time and health has been derived from tools that infer sedentary time from a lack of movement.8, 10, 18, 19, 20 However, this can lead to misclassification of low-intensity non-sedentary behaviors as sedentary behaviors.21 A key example of this is standing. Like sitting or lying, standing involves minimal movement and low energy expenditure.22 However, unlike sitting or lying, this behavior is characterised by its upright posture which elicits higher muscle contractile activity23 with associated beneficial impacts on physiological processes such as glucose metabolism.11, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24
Notably, while the 2012 definition of sedentary behavior includes both energy expenditure and postural elements,4 no field-based tool as yet directly and accurately captures both of these elements. The thigh-mounted activPAL monitor (activPALTM, activPAL3TM, and activPAL3TM micro; PAL Technologies Ltd., Glasgow, UK) is 1 measurement device that directly measures the postural aspect of sedentary behavior. The activPAL device (referring to all models) is a small and slim thigh-worn monitor. Via proprietary algorithms (Intelligent Activity Classification), accelerometer-derived information about thigh position and acceleration are used to determine body posture (i.e., sitting/lying and upright) and transition between these postures, stepping, and stepping speed (cadence), from which energy expenditure is inferred indirectly. The activPAL has almost perfect correlation and excellent agreement with direct observation for sitting/lying time, upright time, sitting/lying to upright transitions and for detecting reductions in sitting.21, 25, 26, 27 Additionally, it accurately distinguishes standing from stepping26 and identifying stepping speed (cadence);28 however, accuracy for detecting stepping is compromised at very slow (i.e., <0.5 m/s) walking speeds.29 As such, the use of the activPAL device in physical activity and sedentary behavior research has increased rapidly in recent years (460% increase from 2008 to 2014 on the Scopus citation database).
With the increasing use of activPAL monitors to address important questions in sedentary behavior research, it is timely to consider some of the methodological and practical considerations specific to these monitors. Existing best practice recommendations for objective activity monitoring, such as those outlined by Matthews et al.,30 provide an excellent starting point. However, these are either general, or focused on other monitors that have key differences to activPAL devices, from the method and location of attachment, to the properties of the resultant data. Accordingly, some existing recommendations may not be applicable, and the unique opportunities and challenges specific to activPAL monitors warrant consideration and further elucidation.
This report provides an overview of the key data collection and processing issues to consider when using the activPAL activity monitor in physical activity and sedentary behavior field-based research with adult populations. The considerations discussed are categorised under: pre-data collection, monitor preparation and distribution, data collection, data processing, and data reporting. The considerations are mainly based on the procedures and protocols reported in the current literature (free-living adult studies identified from the PAL Technologies' bibliography (September 2014) and by searching the term “activPAL” in PubMed (October 2015)). Only those accessible in full-text form were included (Table 1). However, given the paucity of detail in the published literature, we also based considerations on the experiences from 2 international research groups (Table 2). These experiences span across both epidemiological and intervention study designs, various adult population groups and settings. It is intended that these findings and discussion points be informative for researchers who are both currently using activPAL monitors or are intending to use such devices. It is not intended that the practices employed to date should be taken as best practice for the field.
Table 1.
Summary of activPAL use reported in full-text accessible articles of free-living studies in adults.
| Reference | Study design | Intended wear period | Attachment | Periods of interest analysed, with any corroborating data, and by what method of ascertainment | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model | File | Day | Hour | Method | Location | Other data | Analysed | How achieved | ||
| Aadahl et al., 201440 | RCT | activPAL3 | Events | 7 | 24/7 | PAL stickies (removed during water activities) | Anterior upper right thigh | Log of bed, wake, removal, other sleep times | Waking wear Valid: removed <2 h |
NA |
| Aguilar-Farias et al., 201542 | Cross-sectionala | activPAL3 | Eventsb | 7 | 24/7 | Waterproofed and Tegaderm | Middle-anterior right thigh; written instructions | Log of wake, sleep, and removal times | Waking wear Valida |
Matching to other monitor; “non-wear” based on unspecified method |
| Aguilar-Farias et al., 201450 | Cross-sectionala | activPAL3 | Events | 7 | 24/7 | Waterproofed and Tegaderm | Middle-anterior right thigh | Log of wake, sleep, removal times | Waking wear Valid: ≥10 h |
“Semi-automated” filter to merge log data |
| Alkhajah et al., 201257 | Non-randomised trial | activPAL3 | 15 s epoch | 7 | 24/7 | NA | NA | Log of awake, asleep, removal, and work times | Waking wear/working wear Valid: removed <90 min/<10% |
Periods identified from log |
| Barreira et al., 201634 | Cross-sectional | NA | NA | NA | Wake | NA | NA | Log of on and off times | Waking wear Valid: ≥10 h |
Non-wear determined by log and data file, i.e., >3 h continuous lying/sitting with 0 or 1 count in the accelerometer channel |
| Barreira et al., 201547 | Cross-sectional | Uniaxial | NA | 7 | 24/7 | NA (removed during water activities) | Right thigh | NA | 7:00 a.m.–10:00 p.m. Valid: NA |
NA |
| Barry et al., 201541 | Cross-sectional | Uniaxial | Events | 7 | 24/7 | PAL stickies and Hypafix (removed during water activities) | Upper thigh | NA | NA | NA |
| Berendson et al., 201443 | Cross-sectionala | activPAL3 | Eventsb | ≥3 | 24/7 | Waterproofed and Tegaderm | NA | Time use diary collected every 15 min during waking hours | NA | “Matched” with time use diary; limited detail |
| Chastin et al., 201177 | Cross-sectional | NA | Eventsb | 7 | 24/7 | NA | NA | NA | All hours NA Wear Valid: NA |
NA |
| Chastin et al., 201469 | Cross-sectional | NA | NA | 7 | 24/7 | NA (removed during water activities) | NA | NA | Waking wear Valid: worn continuously for 3 weekdays and 1 weekend day |
Waking defined as first standing event after ≥2 h of non-upright posture between midnight and 9:00 a.m. to last standing event before >3 h of non-upright posture after 10:30 p.m. |
| Chau et al., 201478 | RCT | activPAL3 | NA | 5 | Work time | NA | Front mid-thigh | Log of work start and end times | NA | Work time data determined by the log |
| Craft et al., 201236 | Cross-sectional | NA | NA | 7 | Wake | Hypafix | Front of right thigh, midway between knee and hip; written instructions | Log of time on and off each day | Waking wear Valid: ≥10 h |
Wake time determined by log and activPAL data; treats all overnight removal as sleep |
| Di Fabio et al., 201579 | Longitudinal | Uniaxial | NA | 7 | 24/7 | Unspecified adhesive (removed during water activities) | Right leg over quadriceps | NA | All wear hours | Matched to other monitor for non-wear |
| Dollman et al., 201658 | Cross-sectional | Uniaxial | 15 s epoch | 3 | 24 | Waterproofed and unspecified tape | Mid-anterior right thigh | Log of removals, time going to and getting out of bed | All hours (controlling for time in bed but not removing it) Valid: all hours |
Time in bed identified in event files using log, corrected based on monitor data |
| English et al., 201680 | Cross-sectional | activPAL3 | Events | 7 | 24/7 | Waterproofed and NA | Anterior thigh, unaffected leg | Log of sleep, wake, and removals | Waking wear Valid: NA |
Waking hours determined from the log, incorrect data (identified using heat maps) adjusted using events file data |
| Esbensen et al., 201581 | RCT protocol | activPAL3 | Events | 7 | 24/7 | Unspecified waterproof dressing and adhesive tape | Anteriorly on upper right thigh | Diary of resting and sleeping time | NA | Sleep time determined by the diary |
| Evans et al., 201259 | RCT | NA | Eventsb | 5 | Work time | NA | NA | Log of monitor on and off each work day | Work hours: NA Wear Valid: ≥4 h (work) |
Sitting/lying bouts included if <10 min was outside the log reported work period |
| Fitzsimons et al., 201382 | Pre–post study | NA | NA | 7 | 24/7 | NA | NA | NA | All hours: NA Wear Valid: full days |
NA |
| Gardner et al., 201483 | RCT protocol | activPAL3 | NA | 7 | 24/7 | Unspecified waterproof dressing | NA | NA | NA | NA |
| Gennuso et al., 201684 | Cross-sectional | NA | Eventsb | 7 | Wake | Medipore tape | Midline of thigh | Log of wear time | Waking wear Valid: ≥10 h |
Matched to other monitor and wear log |
| George et al., 201471 | Cross-sectional | NA | Events | 7 | Wake | NA | Mid-right thigh | Log of time got up/into bed and monitor wear | Waking wear Valid: ≥10 h |
NA |
| Godfrey et al., 201451 | Cross-sectional | Uniaxial | Both: NA | 7 | 24/7 | PAL stickies and Hypafix (removed during water activities) | Upper thigh | NA | All wear hours for sedentary and ambulatory time: NA Valid: NA | Non-wear: periods >8 h; sedentary bouts 8:00 a.m.–8:00 p.m. |
| Gorman et al., 201360 | Pre–post study | activPAL3 | Events | 7 | 24/7 | Waterproofed and unspecified adhesive | Right anterior thigh | Log of awake, asleep, removal, and work times | Working wear Valid: removed <20% |
Bouts assigned the log classification that mostly (≥50%) applies |
| Granat et al., 201585 | Cross-sectional | Uniaxial | Events | 7 | 24/7 | NA | Anterior aspect of thigh | NA | NA | NA |
| Júdice et al., 201572 | RCT | NA | 15 s epoch | 14 | 24/7 | Unspecified adhesive (removed during water activities) | Middle anterior line of right thigh | Log of waking/sleeping hours and removals | Waking wear Valid: ≥10 h |
Matched to other monitors for waking period and checked with log |
| Klenk et al., 201586 | Cross-sectional | Uniaxial | NA | 7 | 24/7 | NA | NA | NA | All hours | NA |
| Kozey-Keadle et al., 201221 | Pre–post study | Uniaxial | 15 s epoch | 7 | NA | Unspecified adhesive | Anteriorly on right mid-thigh Written instructions | Log of wake/bed time, monitor on/off times, removals >10 min | Waking wear Valid: ≥10 h |
NA |
| Kunkel et al., 201439 | Longitudinal | NA | NA | NA | Staff work | NA | Unaffected leg | NA | NA | NA |
| Lord et al., 201187 | Cross-sectional | Uniaxial | Eventsb | 7 | NA | NA | NA | NA | NA | NA |
| Lowe et al., 201488 | Cross-sectional | activPAL3 | NA | ≤7 | 24/7 | PAL stickies (removed during water activities) | Anterior mid-thigh | NA | All hours: NA Wear Valid: NA |
NA |
| Lyden et al., 201589 | Pre–post study | Uniaxial | Events | 7 | Wake | Unspecified adhesive pad | Midline of right thigh | Log of monitor wear times and removals | Waking wear Valid: ≥10 h |
Wear time determined from log |
| Martin-Borras et al., 201490 | RCT protocol | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Matthews et al., 201367 | Cross-sectionala | NA | Events | 7 | Wake | NA (removed during water activities) | Mid-right thigh | Log of time out of/into bed and time when monitor worn | Waking wear Valida |
Log data and Choi algorithm applied to activPAL movement |
| Mau-Moeller et al., 201491 | RCT | Uniaxial | NA | 5 and 7 | 24/7 | NA (removed during water activities) | Anterior thigh, middle of knee and hip | NA | All hours: NA Wear Valid: NA |
NA |
| Mutrie et al., 201275 | RCT | NA | NA | 7 | 24/7 | NA | Anterior thigh | NA | NA Valid: ≥1000 steps |
NA |
| Neuhaus et al., 201474 | RCT | activPAL3 | Events | 7 | 24/7 | Adhesive (breathable) and waterproofing | Anterior midline right thigh | Log of wake/sleep, work, and removal times | Wear at work Valid: worn ≥80% of time at work |
NA |
| Paul et al., 201549 | Cross-sectional | Uniaxial | NA | 7 | 24/7 | Tegaderm and waterproofing | Anterior thigh, unaffected leg | NA | NA | NA |
| Pontt et al., 201592 | Cross-sectional | Uniaxial | Event | 3 | 24 | Adhesive and waterproofing | NA | Log of removals, bed, wake, and work times | All hours | Time in bed identified by log and refined by event data |
| Reid et al., 201331 | Cross-sectional | activPAL3 | Both | 7 | 24/7 | Hypafix and waterproofing | Anterior midline right thigh | Log of awake/sleep/nap and removal times | Waking wear Valid: ≥80% of waking hours |
Log periods (15 s epoch); bouts assigned the log classification that mostly (≥50%) applies (events); days defined by sleep/wake cycle |
| Reid et al., 201593 | Cross-sectional | activPAL3 | 15 s epoch | 7 | 24/7 | Tegaderm and waterproofing | Mid-thigh | Log of sleep and removals | Waking wear Valid: ≥22 h |
Log data used to isolate waking wear using MATLAB |
| Rosenberg et al., 201594 | Pre–post study | Uniaxial | NA | 7 | Wake | Mild–gel | Front of thigh | Log of wear times | Waking wear Valid: NA |
Non-wear determined by log times |
| Ryan et al., 201195 | Cross-sectional | NA | Eventsb | 7 | NA | NA | NA | Working and non-working days indicated | Wear at work Valid: visual inspection |
Bouts mostly ≥50% in work period (assumed 09:00–17:00); visual non-wear method |
| Sande et al., 201496 | Pre–post study | NA | NA | 14 | NA | NA | Anterior thigh | NA | NA | NA |
| Smith et al., 201468 | Cross-sectional | NA | NA | 7 | 24/7 | Waterproofed and Tegaderm | Midway between right hip and knee | NA | Waking hours: NA Wear. Valid: NA | Waking hours determined by 07:00–23:59; non-wear method |
| Smith et al., 201552 | Cross-sectional | activPAL3 | 15 s epoch | 5 | 24 | Waterproofed and adhesive dressing | Middle of thigh | X | Valid: all hours | Waking hours determined by 07:00–23:00 |
| Stephens et al., 201456 | Non-randomised trial | activPAL3 | Events | 7 | 24/7 | Waterproofed and breathable dressing | Anterior midline of right thigh | Log of wake/sleep and work times | Wear at work Valid: removed <20% |
Bouts that were mostly (≥50%) sleep, non-wear or not at work according to log excluded; days from wake to wake |
| Stewart et al., 201497 | Pre–post study | NA | NA | 7 | NA | NA | NA | NA | NA | NA |
| Swartz et al., 201437 | Pre–post studya | Uniaxial | 15 s epoch | 3 | Work time | PAL stickies and athletic tape | Midline of right thigh | Log of monitor on/off times | Wear at work Valida |
Matched with log; limited detail |
| Swartz et al., 201438 | RCT | Uniaxial | 15 s epoch | 3 | Work time | PAL stickies | Midline, anterior right thigh | Log of start/end of workday | Wear at work Valid: ≥6 h (work) |
Matched with log; limited detail |
| Thomas et al., 201498 | RCT protocol | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Tieges et al., 201573 | Longitudinal | NA | Eventsb | 7 | 24/7 | NA | Unaffected leg | NA | Valid: all 24 h | Sleep time not removed |
| Tigbe et al., 201199 | Cross-sectional | Uniaxial | NA | 7 | 24/7 | PAL stickies (removed during water activities) | Anterior mid-thigh | Work/non-work days and hours | All hours/work: NA Wear Valid: 24 h periods |
Matched with work hours; non-wear method |
| Watne et al., 2014100 | RCT | NA | NA | In hospital | 24/7 | NA | Anterior non-affected thigh | NA | NA | NA |
| Wilmot et al., 201176 | RCT protocol | NA | NA | 10 | NA | Unspecified adhesive | NA | NA | NA | NA |
| You et al., 2015101 | Cross-sectionala | NA | 15 s epoch | 7 | NA | NA | NA | GPS and travel diary | NA Valida |
Accepted all data (noted problems after) |
Abbreviations: GPS = global positioning system; NA = not available; RCT = randomized controlled trial; X = did not collect.
Study is for measurement (e.g., validity); other data collected for measurement study purposes; “valid” data included related to multiple methods due to measurement study.
Events file implied from description of activPAL data “bouts” or uses data clearly not obtainable from the 15 s epoch file.
Table 2.
Summary of the studies used to inform the report—all of which used activPAL3.
| STAND76 | Walking away from diabetes102 | PROPELS103 | AusDiab104 | Stand Up Victoria61 | |
|---|---|---|---|---|---|
| Study design | Randomised controlled trial | Cluster randomised controlled trial | Randomised controlled trial | Longitudinal | Cluster randomised controlled trial |
| Data collection points | Baseline, 3 and 12 months | Baseline, 12, 24, and 36 months (activPAL only at 36 months) | Baseline, 12 and 48 months | Waves 1, 2, and 3 (activPAL only at Wave 3) | Baseline, 3 and 12 months |
| Total sample size (n) | 187 | 808 | 1308 | 782 | 231 |
| Study population/setting | At risk of type 2 diabetes/free-living | At risk of type 2 diabetes/free-living | At risk of type 2 diabetes/free-living | General adult population/free-living | Office workers/free-living overall and at the workplace |
| Age group | 18–40 years (mean: 33 years) | 30–75 years (mean: 63 years) | 24–75 years (mean: 60 years) | 36–89 years (mean: 58.4 years) | 23–65 years (mean: 45.6 years) |
| Men (%) | 31 | 64 | 51 | 43 | 32 |
| Country | UK | UK | UK | Australia | Australia |
| Years of study | 2011–2012 | 2013 | 2014–2019 | 2011–2012 | 2012–2014 |
| Wear protocol | activPAL3 | activPAL3 | activPAL3 | activPAL3 | activPAL3 |
| 10 days | 7 days | 7 days | 7 days | 7 days | |
| Continuous (24 h) | Continuous (24 h) | Continuous (24 h) | Continuous (24 h) | Continuous (24 h) | |
| Waterproofed | Waterproofed | Waterproofed | Waterproofed | Waterproofed | |
| Distributed at examination center, returned by mail | Distributed at examination center, returned by mail | Distributed at examination center, returned by mail | Distributed at examination center, returned by mail | Distribute/returned via workplace | |
| Self adhered to thigh by hypafix/tegaderm and checked by nurse | Self adhered to thigh by hypafix/tegaderm and checked by nurse | Self adhered to thigh by hypafix/tegaderm and checked by nurse | Staff adhered to thigh by hypafix/tegaderm | Adhered by staff (baseline only) or self to thigh with hypafix/tegaderm | |
| Concomitant data | Paper diary (sleep and wear) | Paper diary (sleep and wear) | Paper diary (sleep and wear) | Paper diary (sleep and wear) | Paper diary (sleep, wear and work) |
Note: Sample sizes reported are not necessarily reflective of all data available.
2. Pre-data collection considerations
2.1. Wear period: number of days of monitoring
The number of days of monitoring ideally depends on the study design and purpose. The majority of studies (71%) that we considered in the literature (Table 1) and those in Table 2 have asked participants to wear the activPAL for 7 full days. To our knowledge only 1 study has reported how many days of monitoring are required to provide adequate reliability for several activPAL outputs (sitting, standing, stepping, and transitions) in adults.31 Applying the Spearman–Brown Prediction Formula,32 Reid et al.31 showed to achieve intra-class correlations (ICCs) of 0.8 and 0.9, respectively, 5 days and 11 days respectively were needed for sitting, 5 days and 10 days respectively for standing, and 7 days and 15 days respectively for stepping in a population of older adults living in residential care. However, this approach has limitations, as each day is treated as randomly sampled (but they consecutive) and no distinction is made between particular days of the week. In reality, mean activity levels and correlations are likely to vary by day of the week.33
More recently, generalisability theory has been applied to investigate the reliability of activPAL measured sitting time and moderate-to-vigorous physical activity (MVPA).34 Generalisability theory gives a better indication of repeatability than the ICCs, particularly when more sources of variation, including seasonality, are considered.35 Barreira et al.34 showed that in women, to achieve G-coefficients (interpreted identically to an intra-ICC value) of 0.8 and 0.9, respectively, 4 and 9 wear days were needed for sitting and 7 and 21 wear days were needed for MVPA. Achieving an acceptable degree of repeatability, whether by ICC or G-coefficients, indicates that within-individual variation is low in proportional to other sources of variation. The number of days required to achieve a particular ICC or G-coefficient relates to both properties of the measure and the population, and therefore should be reported for a wider range of outputs and populations using up-to-date methods.
From a practical perspective, researchers are also limited by the 16 MB (32 MB for activPAL3 micro) memory capacity of the activPAL3 monitor, which with a sampling frequency of 20 Hz (80 Hz available in research mode) allows up to 14 days of monitoring. The activPAL3 micro has a larger memory capacity, yet still only allows for up to 14 days of monitoring. Pending better recommendations, for a single assessment, studies should use a protocol that is at least 7 days and ideally up to the 14 days limitation of the monitor. This recommendation takes into consideration that the number of days requirements are largely unknown, but at times exceed 7 days. Multiple assessments, including covering multiple seasons, have been shown to improve reliability and better estimate long-term activity over single-season assessments.35
2.2. Wear period: time of wear
In studies where the wear protocol was clear (Table 1, 38/55 studies), 32% asked participants to wear the monitor during waking hours only (e.g., Ref. 36), working hours only (e.g., Refs. 37, 38) or during periods based on researcher convenience (i.e., staff working hours; e.g., Ref. 39). In these studies, the activPAL was usually attached with PAL stickies (PAL Technologies Ltd.) or an unspecified adhesive. A slightly smaller percentage of studies (26%) employed a 24 h protocol while requested that participants remove the monitor for showering/bathing (e.g., Refs. 40, 41). Again these studies tended to use PAL stickies for attachment. A higher percentage (42%) of the studies we examined requested participants to wear the activPAL monitor 24 h per day during waking and sleeping hours and water-based activities (e.g., Refs. 42, 43); therefore, it appears that researchers are favoring this type of wear protocol for this monitor. This is in contrast to the ActiGraph device where researchers have mostly employed a waking wear protocol.30 A continuous wear protocol can easily be achieved with the activPAL monitor by waterproofing the device with a small flexible sleeve to cover the monitor, wrapping it in 1 piece of waterproof medical grade adhesive dressing (e.g., Tegaderm, Hypafix, or Opsite) and then attaching to the leg using adhesive dressing. A continuous wear protocol like this may increase wear time compliance.44
3. Monitor preparation and distribution
3.1. Initialisation
The activPAL software allows researchers to select an immediate start time for recording (from the time the device is unplugged from the docking station until the battery runs out, the memory is full, or the device is plugged into the docking station again), or a future date and time, along with the stop date and time. Unfortunately, there is only a 4-day limit on initialisation. For example, to begin recording on a Monday morning, the earliest that the device could be initialised would be on the previous Thursday morning.
The default sampling frequency in the software is 20 Hz for the activPAL3, but 80 Hz can be selected in research mode, or 10 Hz for the activPAL (uniaxial version). The software also gives researchers the option of changing the minimum sitting/upright time period to define a new posture from 1 s to 100 s. The default of 10 s (i.e., ≥10 s of sitting/lying or upright data is needed to register as a new event) is recommended by the manufacturer. In the studies in Table 2, and in other published studies (e.g., Ref. 45), the default of 10 s has been selected; however, research suggests that this may not be appropriate for all populations.46 In a sample of very young children (mean age of 4.5 years), Alghaeed et al.46 found that a 2 s, in comparison to 1 s, 5 s, and 10 s, minimum sitting/upright time period had the smallest error in detecting the number of breaks performed against direct observation. This suggests that young children transition rapidly between postures and the default of 10 s to register a new event may not be appropriate for this age group. Therefore, it is important that researchers apply the appropriate settings for their population, and report the settings in publications. However, to our knowledge, similar studies have yet to be conducted with other populations so the extent to which this setting impacts on the number of breaks in adult populations, for example, remains unclear.
An important, and often overlooked, consideration when initialising the monitors is to be aware of the system used to record the date/time-stamped data, especially when intending to match the monitor data with date–time stamped data from other monitors and diaries, or when collecting data in a time-zone that involves discontinuities (such as “losing” or “gaining” 1 h with daylight savings). Furthermore, when dealing with activPAL data as part of a multi-sensor data collection that requires matching output on fine time scales, clock drift should be considered.47
3.2. Attachment location and method
The algorithm used by the activPAL software uses information from static acceleration (due to gravity) and angle of the thigh to classify posture (lying/sitting vs. upright) and dynamic acceleration (due to body movement) to determine stepping.48 Accordingly, it is important that the activPAL device is worn on the midline anterior aspect of the upper thigh as recommended by the manufacturer. An example of correct placement for the activPAL is shown in the example instruction sheet (the example instruction sheet can be found as Supplementary File 1). Of the studies in Table 1 that did report information on the exact activPAL location (i.e., where on the leg and which leg), they all reported attaching the activPAL to the right thigh apart from studies conducted in stroke populations where it was attached to the unaffected leg (e.g., Refs. 39, 49). While it can be useful to standardise which leg the activPAL is attached to, participants involved in the studies in Table 2 occasionally experienced slight irritation from the adhesive dressing. In this situation they were advised to attach the activPAL to the opposite leg. This enabled the participant to attach the monitor in the same optimal location on the opposite leg in preference to using a sub-optimal location on the same leg (e.g., too far away from the midline) or ceasing to wear the monitor completely. Two studies42, 50 in Table 1 mentioned collecting the times and reasons from participants of every occasion when the monitor was removed from the indicated position.
The orientation in which the activPAL monitor is worn is critical to how the software classifies posture. The correct orientation is indicated by the figure on the front of the activPAL monitor (Fig. 1A), but this can be obscured when using waterproof coverings. In this case, we have redrawn the orientation figure on the waterproof covering (Fig. 1B). If, however, participants wear the device upside down, the activPAL software (from Version 7.2.32) allows researchers to reprocess the data as though it were worn in the correct orientation. There is no automatic function within the software to determine when the device has been worn in the incorrect orientation so it may be useful to ask participants to record this in a wear log.
Fig. 1.
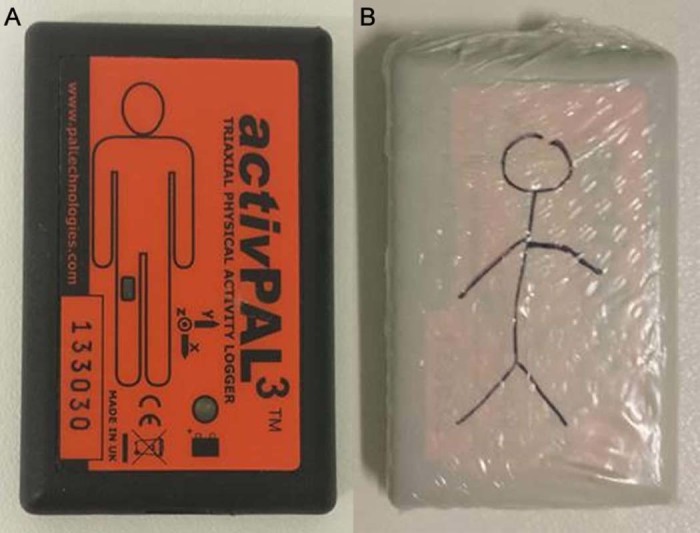
(A) The figure on the front of the activPAL indicating the correct orientation of the device. (B) An activPAL with waterproof coverings and a stick man to indicate correct orientation.
As stated in Section 2.2 the activPAL monitor is attached using various different adhesives (i.e., PAL stickies, medical dressing, e.g., Hypafix); the type of adhesive being largely dependent on the wear protocol. Some of the adhesives are designed to be short lasting (i.e., 1 day) and some longer term (i.e., 5–7 days). Although manufacturers state that a piece of the hypoallergenic waterproof dressing can stay attached for 5–7 days, participants involved in the studies outlined in Table 2 preferred to change their dressing every 2–3 days. Therefore, for a 7-day monitoring period, participants were provided with 4 dressings for re-attachment and 4 alcohol wipes to assist in the attachment and removal of the dressing. This has cost implications, but may enhance wear time compliance. The provision of additional dressing was also reported in 3 studies41, 51, 52 in Table 1.
3.3. Instructions to participants
Only 3 studies in Table 1 reported providing participants with written placement instructions to take away with them in addition to the standard verbal instructions.36, 42, 50 To our knowledge, no evidence exists on various instructional techniques and their impact on correct monitor attachment/reattachment or compliance. Example written instructions as used in the studies in Table 2 are provided in Supplementary File 1, Supplementary File 2. Media could also be used for participants to access at home, such as these instruction videos posted on YouTube (http://youtu.be/BuaRHz_BOA4 and https://www.youtube.com/watch?v=CHCCX2GW3DM).
4. Data collection
4.1. activPAL wear, sleep, and key periods of interest log/diary
Over half of the studies (55%) in Table 1 reported collecting some form of log/diary data (e.g., working hours, sleep, and wake times) to assist them with isolating key periods of interest such as worn waking hours during data processing (see Section 5). Requesting that participants complete a wear diary/log may act as a reminder to participants to keep wearing the monitor and to re-attach the monitor each day in a waking hours only protocol. Recording removal reasons and “other comments” from participants (e.g., reactions to dressing, device not flashing, worn upside down) via a diary/log can also be informative, particularly for a new population group and/or pilot data collection. General measurement principles suggest that instructions should be aimed at shifting the diary/log reporting towards “recording” rather than “recalling” and “estimating” for better accuracy, and that pilot testing should be used to ensure usability of the diary/log for your target population.
The studies in Table 1 reported limited detail about the content of their logs/diaries. In the studies in Table 2, diaries/logs were paper-based and ranged from a single page to detailed page-per-day booklets with accompanying instructions (the example instructions sheet can be found as Supplementary File 2, Supplementary File 3). All were tailored to the interests of each study (e.g., work-based studies included work details). The paper-based diaries (both short and long) have been well received by our participants but have typically entailed much missing data and high amounts of time entering data. Recently we have developed and trialled electronic diaries in a sample of office workers with the aim of reducing turn-around time, data entry costs, and missing data (by setting some fields as mandatory). Depending on the electronic approach used, the data can be available to the researcher on a daily basis, enabling the researcher to query issues of missing or questionable data and request clarification from participants in a timely manner. This may be more important for information, such as work times, that are essential for analysis and cannot be inferred from the monitor data alone. The electronic diary method shows promise, but may not be universally suitable. What works best is likely to depend on the study population, study size and requirements, and the resources and skills available in the research team.
4.2. Compliance
In accelerometer studies generally, compliance is typically considered in terms of the amount of time the monitor is worn during the period of interest (e.g., waking hours) and the number of valid wear days provided (i.e., the number of days on which wear time was adequate to consider that monitoring has sufficiently captured most of the period of interest). Table 3 presents the compliance figures for 4 of the studies outlined in Table 2. These data may be helpful in indicating the degree to which the sample size should be inflated to allow for missing data due to non-compliance. For comparison, we also present compliance figures for the hip-worn ActiGraph accelerometer (ActiGraph, Pensacola, FL, USA) worn in the same studies but with a waking hours only and removal during water-based activities protocol. Both provided a similar number of “valid” days, but activPAL showed longer waking wear days than the ActiGraph, possibly due to different wear protocols and attachment methods.
Table 3.
Number of valid wear days and wear/wake time (on valid days) for the activPAL and ActiGraph monitors in some of the research studies outlined in Table 2.
| STAND76 Baseline data (n = 187) |
Walking away from diabetes102 Final follow-up data (n = 530) |
AusDiab104 2011–2012 (n = 782) |
Stand Up Victoria61 Baseline data (n = 231) |
|||||
|---|---|---|---|---|---|---|---|---|
| activPAL | ActiGraph | activPAL | ActiGraph | activPAL | ActiGraph | activPAL | ActiGraph | |
| Period | Waking hours | Waking hours | Waking hours | Waking hours | Waking hours | Waking hours | Waking hours | Waking hours |
| Protocol | Continuous | Waking hours | Continuous | Waking hours | Continuous | Waking hoursa | Continuous | Waking hoursa |
| Definition | 10+ h estimated from the monitor data, <95% in any one behavior, <500 steps | 10+ h estimated wear time | 10+ h estimated from the monitor data, <95% in any one behavior, <500 steps | 10+ h estimated wear time | ≥10 h worn waking hours (monitor-corrected diary) | 10+ h estimated wear time | ≥10 h worn waking hours (monitor-corrected diary) | 10+ h estimated wear time |
| Participated in monitor wear (%) | 100 | 100 | 99.2 | 99.6 | 77.1 | 77.1 | 100b | 100b |
| Valid daysc (%) | ||||||||
| 0 | 31.0d | 11.2 | 13.1 | 0 | 5.2 | 4.7 | 0.4 | 1.3 |
| 1 | 1.1 | 1.6 | 2.3 | 0.4 | 0.5 | 1.2 | 0 | 0.4 |
| 2 | 3.2 | 1.6 | 1.1 | 2.5 | 0.8 | 0.8 | 0 | 0.4 |
| 3 | 1.1 | 1.6 | 0.8 | 1.7 | 1.5 | 1.4 | 0 | 0.9 |
| 4 | 2.7 | 3.7 | 2.9 | 4.2 | 1.0 | 1.8 | 1.3 | 1.3 |
| 5 | 9.1 | 6.4 | 3.4 | 5.9 | 2.6 | 3.1 | 1.3 | 5.6 |
| 6 | 7.0 | 7.0 | 9.5 | 13.6 | 9.6 | 7.8 | 6.5 | 14.7 |
| 7+ | 44.9 | 66.9 | 66.9 | 71.7 | 78.8 | 79.3 | 90.5 | 75.3 |
| Wear during waking hours (h)e | 15.3 ± 1.9 | 14.4 ± 1.4 | 15.8 ± 2.2 | 14.3 ± 1.3 | 15.7 ± 1.1 | 15.6 ± 2.5 | 15.8 ± 1.8 | 15.0 ± 1.2 |
For days on which participants deviated from the protocol and wore the monitor to bed, estimated time in bed (sleep) was also removed using an approach based on the Sadeh algorithm105 and visually checking/manual reclassification of erroneous data.
Monitor wear was a study requirement.
Percentage of participants providing a certain number of valid wear days (as a percentage of participants assigned the monitor). Figures exclude study participants who refused to wear the monitor at all (did not participate), but include those with no data due to faulty downloads or lost data in addition to non-compliance.
This includes a high percentage of monitor malfunction that we experienced at the start of the study associated with the “future start time” function during the initialisation process.
mean ± SD.
5. Data processing
5.1. activPAL software and files available
The activPAL software (PAL Technologies) provides a quick and easy-to-use system for initialisation, downloading and exporting data (in raw form and pre-classified by proprietary algorithms), and enabling researchers to visualise pre-classified data (i.e., sitting/lying, standing, stepping) in various formats (e.g., hour by hour, by day, or by week) from individual files. However, it is not a comprehensive, interactive data processing or analytic tool, and therefore even fairly routine requirements, such as isolating sitting/lying during waking hours, excluding periods of non-wear, and linkage to other time-stamped data (e.g., logs), requires processing the data outside of the activPAL software in other software packages (e.g., SAS, STATA, Excel, R). To assist researchers, in the following sections we provide: an overview of the data available from the activPAL; describe ways that our research groups and others have isolated key periods of interest in the activPAL data, identified non-wear and invalid data; and applied external limiters to the data (e.g., analysed only work hours).
When data from the activPAL device are downloaded, they can be saved as csv files in numerous formats. A 15 s epoch summary file shows the number of seconds spent in various activities, number of steps and sit-to-upright transitions occurring during that 15 s time window. These files do not indicate the order in which multiple activities occurred within the 15 s window. Such precise information is available from the event based summaries (“Events” files). These are a chronological list of all bouts of sitting/lying, standing, and each step, with the time each bout begins and bout duration. The “Events X Y Z” files also include triaxial acceleration data. These event-based summaries offer more precise data for the amount of each activity (less rounding error) and are ideally suited for extracting information on bout frequency and duration. The raw data can also be output; these were not reportedly used in the studies we examined (Table 1). Raw data files are currently being used in the context of methods development, including exploring the recognition of activity types not currently available through the activPAL software, such as distinguishing lying from sitting53 and identifying wake time and number of awakenings during sleep54 and cycling.55
5.2. Defining a day
Researchers often define days as calendar days (i.e., midnight to midnight). However, all time-based definitions are problematic when examining “bouts” of behavior or events because a single bout of behavior may begin in one day and end in the next. This poses problems in examining issues such as sitting accumulation because segmenting the bout at the day boundary means systematically underestimating bout duration. A simple modification could be to use calendar days but assign entire bouts to the day or date the bout begins.
The person-oriented day approach, from one wake time to next day wake time (Table 1),56 offers a behaviorally relevant approach that also avoids sub-dividing activity bouts across multiple days and further may increase the number of valid days or amount of waking wear. It reduces the likelihood of pockets of valid data being removed and considered “invalid” just because they occur after an arbitrary time (e.g., midnight) and the following day does not include enough wear to be labelled as valid. For example, in Fig. 2 (which displays only valid waking hours data), a participant was still moving around from late on the 10th of December until the early hours the next morning (11th of December), which was not a valid wear day. A calendar day would discard all data from the 11th of December because it occurs after midnight but the person-oriented day approach would not. Person-oriented day durations are not always 24 h; the practical impact is often non-existent as waking day durations are variable under most definitions.
Fig. 2.
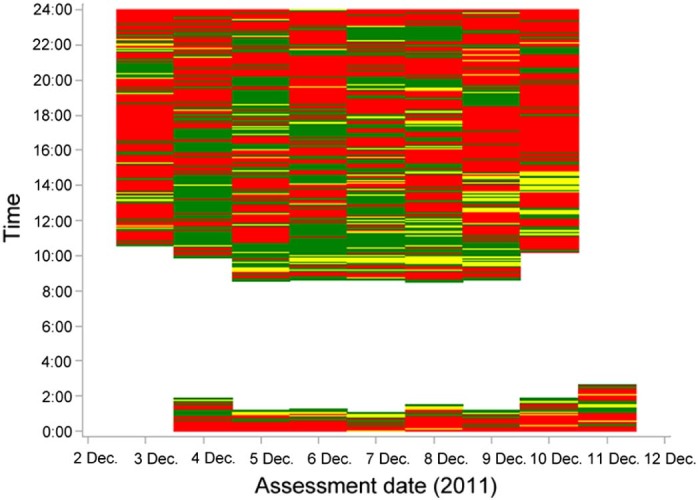
Heat map of waking hours (“sleep” has been removed) activity (green, stepping; yellow, standing; red, sitting; white, sleep or not worn) from a participant showing bouts of behavior after midnight on 4–10 December, 2011.
5.3. Isolating key periods of interest in the data
activPAL monitors provide continuous streams of data, regardless of whether the monitor is being worn or placed on a bedside table, for example. Isolating only the periods reflective of actual participant behavior during the period of interest (e.g., waking hours or working hours) is a necessity for high quality data. The process for differentiating these periods requires researchers to determine from the data, or from other sources of information (e.g., diary), when the monitor was put on in the morning and taken off in the evening (waking hours protocol), what time the participant woke up (or arose out of bed) and went to sleep (or went to bed), or the start and end of work. At present, there is an absence of validated, accurate methods to isolate these periods of interest and studies to date (Table 1) seldom describe in detail the methods they have employed. Methods that have been reported, as well as ones we are currently employing in the studies outlined in Table 2, are described in the following sections.
5.3.1. Time intensive methods
Most (75%) of the studies we examined (Table 1) that described how they isolated data for their period of interest (such as waking wear, time at work) reported using external information collected, typically self-reported logs/diaries. However, this is time intensive to implement. The exact procedure used to match up the diary with the activPAL data is rarely described, but 2 main approaches are apparent from those studies that have included detail. Sometimes, the literal log/diary-reported period is analysed, especially when using 15 s epoch files (for which this approach is easy) (e.g., Ref. 57). Other times, log/diary-reported periods are matched with “bouts” of activity (it is not unreasonable to assume that a change in period, location, or context would coincide with a change in activity), especially when using the events files, and a rule is implemented as to whether to include or exclude an entire bout of activity from the period of interest (e.g., Refs. 58, 59, 60). This method has the advantage of not segmenting bouts when examining bout durations or accumulation. One rule used involved choosing whether including a bout would include too much time outside of the period of interest. For example, sedentary periods crossing the start/end of each workday were included if most of the sedentary period was within the stated work hours and no more than 10 min was outside.59 An alternative rule employed in several studies involved including bouts which crossed the period of interest (e.g., working hours) if ≥50% of that bout was within the period of interest.61 Internal validation work showed excellent agreement (95% of observations within ±5 min) between our events-modified start and finish work times and participants' originally reported times.62
A common occurrence with self-reported logs/diaries is they are often not fully completed. Participants may still wear the activPAL monitor but how these missing data are dealt with is again not described. An example of how this is dealt with is provided by the Stand Up Victoria and AusDiab studies (Table 2). When participants failed to report a time of waking or sleeping for a particular day, these were visually identified from the events files by research staff. The method the staff used was to examine the events files, starting with times around late evening or early morning, for an extremely long bout of sitting/lying or standing. Then depending on this bout duration, the duration and degree of movement observed in the surrounding bouts, either just this long bout or also some of the surrounding bouts, were selected as the likely unreported sleep or wake time.
5.3.2. Low burden methods
Low burden approaches may be preferable for studies that are large, require quick turn-around of data in bulk, and/or have other staffing and resource issues. Low burden approaches have had limited use, especially for continuous wear protocols, until recently (Table 1). As yet validation of such approaches is yet to appear in the peer-reviewed literature but is likely to be forthcoming based on conference abstracts.63, 64, 65
For waking wear protocols, examples of low burden approaches reported in the literature (Table 1) for isolating waking hours data from non-wear data include the classification of very long bouts (>8 h) of sitting/lying as non-wear (e.g., Ref. 51), the application of the Choi method66 (commonly applied to ActiGraph accelerometer data), i.e., 60 min of no movement with an interruption allowance of 2 min or less67 and >3 h of continual sitting/lying with 0 or 1 count in the accelerometer channel.34
For the 24 h protocols, methods also need to be employed to distinguish between sleep and waking hours. A very simple method that has been used is to limit data to time periods when it is assumed participants are awake (e.g., between 07:00 and 23:59, e.g., Ref. 68). The simplicity of this method is appealing but may result in low data quality. Our diary data show that adults' sleep and wake times are highly variable and not well approximated by any single time period. Chastin et al.69 took a similar approach but allowed for individuals to have varying waking periods by classifying the first standing event after ≥2 h of sitting/lying between midnight and 9:00 as the beginning of wake, and the last standing event before >3 h of sitting/lying after 22:30 as the beginning of sleep. This latter method is less restrictive about when sleep occurs but still presupposes a nocturnal sleep pattern, which may not always be the case, such as in shift workers.
5.3.3. Future possibilities
Viewing activPAL data via heat maps from studies outlined in Table 2 suggests that for adults, an automated approach to isolating waking wear from sleep ideally ought to avoid placing assumptions on when sleep occurs and consider that any period identified as sleep may be part of a larger fragmented sleep pattern, i.e., that periods immediately before and after may also be part of what should be isolated from the main waking wear day. For example, sleep rarely occurs as 1 large uninterrupted bout of sitting/lying (Fig. 3A). Many participants have some small amounts of movement (stepping and/or standing) registered throughout sleep (Fig. 3B); these can be genuine waking movements involving arising from bed but in the case of standing can simply reflect leg positioning in bed while asleep, for example if someone has their leg hanging out of the bed. This fragmentation occurs to a lesser extent (but may still occur) when participants have removed their monitors overnight. We are in the process of trialling an approach that considers these factors.63, 65
Fig. 3.
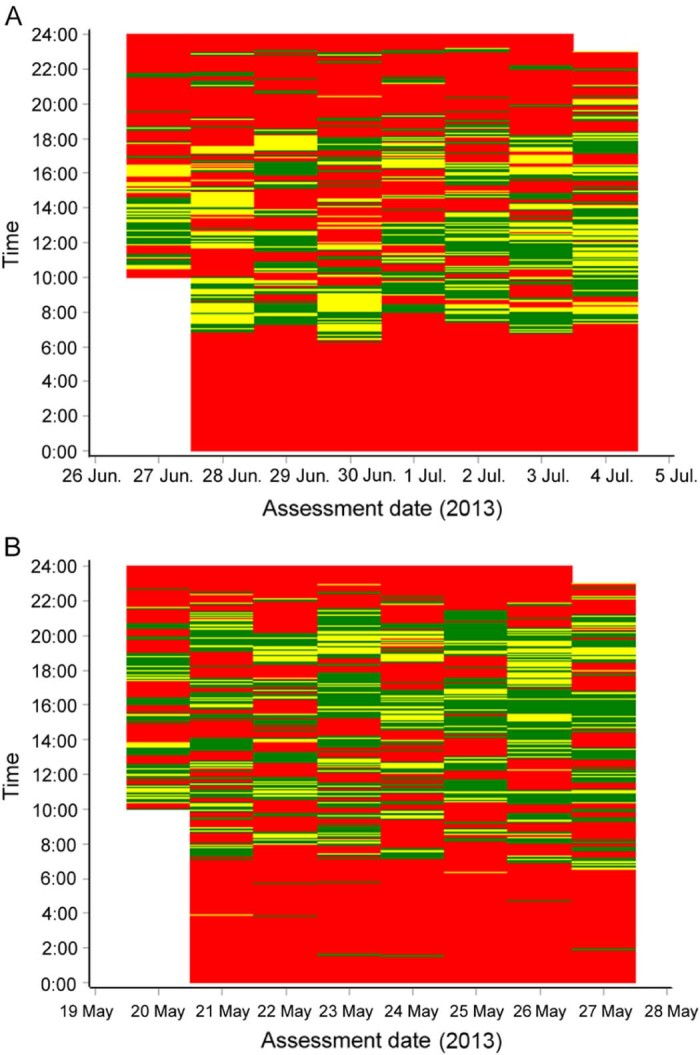
Heat map of activity for the total monitoring period (green, stepping; yellow, standing; red, sitting/lying; white, pre- and post-study). (A) Uninterrupted sleep and (B) interrupted sleep.
It has been contended that an integrated approach considering all movements over a whole day, combining issues relevant for the sedentary, physical activity, and sleep research fields, while acknowledging the inter-dependent nature of these movements may yield relevant insights and opportunities to improve health.70 Continuously worn activity monitors that can also measure parameters of interest to sleep researchers have potential as a cost-effective means of achieving this. It would be useful to develop more sophisticated methods that involve distinction within this broad time period that we have loosely termed sleep (i.e., time in bed asleep, time in bed awake, brief periods out of bed) and can indicate sleep quality. Preliminary attempts in this direction have shown promise.54
5.4. What constitutes a valid day?
The criteria used for the minimum number of hours constituting a valid day or valid time period of interest are irregularly reported (Table 1, 49% reported valid criteria). Those researchers who have reported criteria have used either a minimum of 10 h of wear or waking hours (e.g., Refs. 71, 72), required the full 24 h period (e.g., Refs. 58, 73), considered a day as valid if wear time comprised ≥80% of waking hours,31 or if the monitor had been removed for <2 h in the 24 h time period (e.g., Ref. 31). These criteria have been applied when the full day is of interest. When working hours have been the time period of interest, researchers have applied either a minimum of 4 h or 6 h of valid data per working day (e.g., Refs. 38, 59), or the monitor had to be worn ≥80% or ≥90% of work time (e.g., Ref. 74). For variable duration periods in particular (such as work hours), the percentage approach avoids systematically excluding observations that were short (but were sufficiently complete and therefore valid).
While automated identification of specific non-wear periods is difficult, the identification of entire non-wear days is much simpler. Accordingly, one study75 excluded days with <1000 steps. Similarly in the STAND76 and Walking away studies (Table 2), days with <500 steps were excluded. The optimal cut-offs are likely to depend on the study population (e.g., 1000 steps may be too high for older adults). Additional rules may also be beneficial for activPAL data specifically. Prolonged bouts of standing can occur during the daytime if the activPAL is removed and propped up against something (Fig. 4). It is important that this type of activity is not included in the valid data. We are trialling the identification of a day as “invalid/non-wear” if the vast majority (e.g., >95%) of the day is spent in any one posture, e.g., standing or sitting/lying.
Fig. 4.
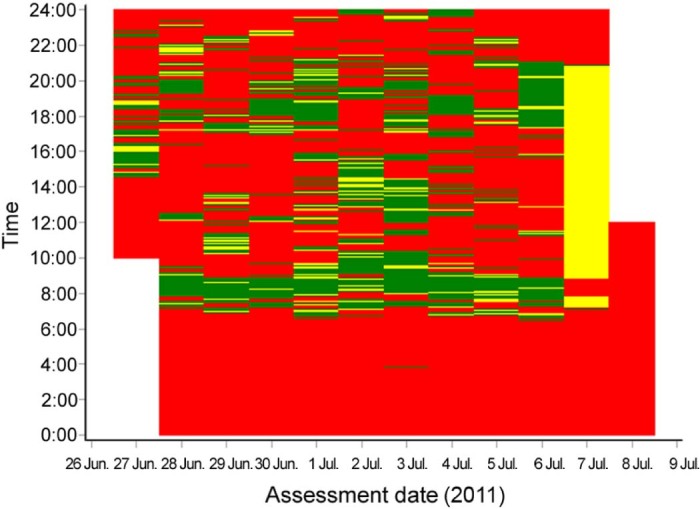
Heat map of activity for the total monitoring period (green, stepping; yellow, standing; red, sitting/lying; white, pre- and post-study) showing an “invalid” day due to the majority of the day standing (indicated by yellow color) on 7th July.
6. Data reporting
Broader reporting issues and guidance when using physical activity monitors have been previously covered by Matthews et al.30 These should be considered for studies using the activPAL. Due to space constraints, researchers typically cannot provide the full level of detail required to replicate studies and judge comparability in study results in their manuscript. They could instead report their methodology as Supplementary material. We present an example table template in Appendix 1.
7. Summary, key recommendations, and future research
The activPAL monitor has demonstrated excellent reliability and validity for use in both physical activity and sedentary behavior research and the device offers exciting possibilities to advance sedentary behavior research specifically. This report provided an overview of the issues to consider, before, during, and after data collection, when using the activPAL monitor in physical activity and sedentary behavior field-based research with adult populations.
Based on the experiences of our research groups with adult populations in the UK and Australia, and the practices observed across a diverse array of epidemiologic studies in free-living adults, we suggest the following key recommendations when using the activPAL monitor in field-based research:
-
•
Employ a 24 h wearing protocol if possible.
-
•
Deploy for at least 7 days.
-
•
Provide verbal, visual, and written instructions to participants on how to wear the device correctly and change dressings; and, if possible, have a study researcher attach the monitor (or demonstrate and check self-attachment).
-
•
Provide a diary (paper or electronic) to collect information on wake and sleep time, time in and out of bed, any removal times, and other contexts of interest (e.g., work times).
-
•
Use events files for data processing, especially if reporting measures relating to bout durations.
-
•
No waking wear identification method is universally accurate and accepted. Use quality controls (e.g., visual examination heat maps) to check classifications, ideally against an external source of data, such as a diary.
-
•
Be transparent when reporting activPAL collection and processing methods.
Future research should focus on the following areas in order to bridge the gaps in our understanding related to the use of the activPAL for measuring physical activity and sedentary behavior:
-
•
Limited research exists on the intra- and inter-individual variability of physical activity and sedentary behavior as measured by the activPAL. This would increase understanding around which populations and measures may require longer observation periods.
-
•
Current literature has employed a variety of wear protocols including waking hours with removals for water activities, waking and sleep hours with removals for water activities and continuous 24 h monitoring. It has been suggested in previous research with ActiGraph accelerometers that wear time compliance increases with continuous wear protocols compared to waking wear protocols. This has yet to be confirmed with the activPAL monitor.
-
•
The accuracy of the minimum sitting/upright period default setting of 10 s (i.e., ≥10 s of sitting/lying or upright data is needed to register as a new event) for detecting the number of breaks in sitting needs to be tested in adult populations.
-
•
Studies have used a variety of attachment methods and it is not clear whether the type of attachment (e.g., PAL stickies vs. piece of Hypafix) may influence wear compliance.
-
•
Most studies reported giving participants verbal instructions on how to wear the activPAL with a small number also providing written instructions for participants to refer to during the wear period. Instruction techniques such as online videos are emerging. However, it is not known to what extent these various methods of instruction impact on correct monitor attachment, re-attachment and wear compliance.
-
•
As noted by Matthews et al.,30 lack of compliance is a source of lost data and can increase cost in research studies. The percentage of participants providing at least 4 days of valid data was reasonable (Table 3) but could still be improved. Research (e.g., qualitative) exploring how to maximise compliance in different populations is needed.
-
•
Studies have employed a variety of methods to isolate key periods of interest from the continuous data that are collected by the activPAL and to define a valid day. The extent to which this impacts on data outputs and therefore comparability between studies is unclear.
-
•
There is currently an absence of validated, accurate methods to isolate key periods of interest (e.g., waking hours) from the continuous data that are collected by the activPAL. The development and validation of automated processes that consider the fragmented sleep patterns that are frequently observed in activPAL data collected continuously is a priority.
-
•
The development of accurate identification methods for additional activity types beyond the current classifications is an important emerging area, both in terms of waking activities (e.g., differentiating lying from sitting, identifying cycling) and sleep (e.g., awakenings during sleep).
Authors' contributions
CLE conceived of the idea for the review, reviewed existing research, and wrote the first draft of the manuscript; GNH conceived of the idea for the review along with CLE and reviewed/edited of the manuscript; EAHW reviewed existing research and wrote the first draft of the manuscript with CLE; DHB helped draft some sections of the manuscript and reviewed/edited the full manuscript; TY, MJD, and DWD reviewed/edited the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
The research was supported by the National Institute for Health Researsch (NIHR) Diet, Lifestyle & Physical Activity Biomedical Research Unit based at University Hospitals of Leicester and Loughborough University, the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care—East Midlands (NIHR CLAHRC—EM) and the Leicester Clinical Trials Unit. The views expressed are those of the authors and not necessarily those of the National Health Service (NHS), the NIHR, or the Department of Health.
Elisabeth Winkler was supported by a National Health and Medical Research Council (NHMRC) Centre for Research Excellence Grant on Sitting Time and Chronic Disease Prevention—Measurement, Mechanisms and Interventions (APP1057608). Genevieve Healy was supported by a Heart Foundation Postdoctoral (PH 12B 7054) and NHMRC Career Development (#1086029) Fellowship. David Dunstan was supported by an Australian Research Council Future Fellowship (FTE 100100918).
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary data to this article can be found online at doi:10.1016/j.jshs.2016.02.002.
Appendix 1
Template table (which expands on the reporting recommendations made by Matthews et al.30) for reporting use of activPAL monitors completed for an example study (STAND76).
| Item | Example response |
|---|---|
| Monitor version | activPAL3 |
| Rationale for selecting activPAL monitor | The STAND intervention aimed to reduce sitting time; objective device required |
| Which behavioral characteristics were of primary interest in making the measurements | Time spent sitting and standing and sit to upright transitions |
| Reliability (inter- and intra-instrument) for the device selected (if available) | Interdevice reliability for the activPAL device ranged from 0.79 to 0.99 (Grant et al.26) |
| Validity information for the activity estimates of interest (e.g., direct measures of predicted values) | A mean percentage difference of 0.19% (limits of agreement from −0.68% to 1.06%) and 1.4% (limits of agreement from −6.2% to 9.1%) between the activPAL monitor and observation for total time spent sitting and standing has been reported (Grant et al.26) |
| Method and location of monitor attachment | Device was waterproofed by covering in nitrile sleeve and wrapped fully in 1 piece of waterproof dressing (Hypafix transparent). Self-adhered to mid-thigh anterior aspect using 1 piece of Hypafix dressing following visual demonstration, with attachment checked by research staff Additional dressings supplied for reattachment during wear period |
| Wear period and number of days | 24 h/day for 10 consecutive days |
| activPAL software version | Version 7.2.29 |
| Settings used: | |
| • Sampling frequency | 20 Hz (default) |
| • Minimum sitting period | 10 s (default) |
| • Minimum upright period | 10 s (default) |
| Diary data collected and details collected | Time woke up, time got up, time went to bed, time went to sleep, and any removal times each day |
| Type of file used for data processing | Events file (X, Y, Z version) |
| Goal for the sampling periods observed (i.e., number of hours per day; number and type of days); state whether a priori | At least 10 h of data per day and 4 days of data (a priori) |
| Method(s) for estimating wearing time/removing time in bed/sleep (report in sufficient detail so that others can replicate the method) | “Sleep”/prolonged removals were removed using an algorithm developed using the study data, which identified the longest sitting/lying and any sitting/lying/standing bouts >5 h in a 24 h period as coded these as sleep, and then searched either side of that sleep bout to identify other bouts to be incorporated into the sleep bout using the following rules: (1) sedentary bouts of ≥2 h within 15 min of sleep plus any interceding movement are considered as sleep time, (2) sedentary bouts of ≥30 min within 15 min of sleep bout and <20 steps in interim plus any interceding movement are considered as sleep time, and (3) sedentary bouts where the only movement between the sleep bout and the sedentary bout is standing are considered as sleep time along with the interceding standing boutb |
| What quality control checks were implemented | Heat maps of included and excluded data visually checked (side by side) for probable errors classification of data to include/exclude. Any likely errors were checked against diaries (when available) and the most plausible classification (subjectively determined) was chosen and applied considering diary data and the typical movement patterns on all days |
| Specify type of action taken when data were determined to be invalid | Data deemed invalid were excluded from analysis of worn waking hours. |
| Compliance criteria to define a valid day of observationa | Day has ≥10 h of worn waking hours, <95% of time spent in any one behavior (i.e., sitting, standing, or stepping) and ≥500 steps |
| Number and type of days required to be included in final analytic samplea | Any 4 days of data |
| Definition of a daya | Midnight to midnight |
| Data processing package used and methods used to generate key summary variables | activPAL software Version 7.2.29 to create events files. STATA Version 13 was used to perform quality checks and determine valid data |
The criteria should be chosen with view to the needs of a particular study's research questions (e.g., whether individual reliable estimates or an unbiased group estimate is most desired), the activity measures, and the study populations and context.
Algorithm still under development.
Appendix. Supplementary material
The following is the supplementary data to this article:
Validation of activPAL self-attachment methods—activity monitor instructions.
Thigh monitor instructions.
Activity monitor instructions and daily log.
References
- 1.Katzmarzyk P.T. Physical activity, sedentary behavior, and health: paradigm paralysis or paradigm shift? Diabetes. 2010;59:2717–2725. doi: 10.2337/db10-0822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Owen N., Healy G., Matthews C., Dunstan D.W. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38:105–113. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tremblay M.S., Colley R.C., Saunders T.J., Healy G.N., Owen N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab. 2010;35:725–740. doi: 10.1139/H10-079. [DOI] [PubMed] [Google Scholar]
- 4.Sedentary Behavior Research Network Standardized use of the terms “sedentary” and “sedentary behaviors”. Appl Physiol Nutr Metab. 2012;37:540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 5.Owen N., Salmon J., Koohsari M.J., Turrell G., Giles-Corti B. Sedentary behavior and health: mapping environmental and social contexts to underpin chronic disease prevention. Br J Sports Med. 2014;48:174–177. doi: 10.1136/bjsports-2013-093107. [DOI] [PubMed] [Google Scholar]
- 6.Shiroma E.J., Freedson P.S., Trost S.G., Lee I.M. Patterns of accelerometer assessed sedentary behavior in older women. JAMA. 2013;310:2562–2563. doi: 10.1001/jama.2013.278896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jefferis B.J., Sartini C., Shiroma E., Whincup P.H., Wannamethee S.G., Lee I.M. Duration and breaks in sedentary behavior: accelerometer data from 1,566 community dwelling older men (British Regional Heart Study) Br J Sports Med. 2015;49:1591–1594. doi: 10.1136/bjsports-2014-093514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henson J., Yates T., Biddle S.J.H., Edwardson C.L., Khunti K., Wilmot E.G. Associations of objectively measured sedentary behavior and physical activity with markers of cardiometabolic health. Diabetologia. 2013;56:1012–1020. doi: 10.1007/s00125-013-2845-9. [DOI] [PubMed] [Google Scholar]
- 9.Matthews C.E., Chen K.Y., Freedson P.S., Buchowski M.S., Beech B.M., Pate R.R. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carson V., Wong S.L., Winkler E., Healy G.N., Colley R.C., Tremblay M.S. Patterns of sedentary time and cardiometabolic risk among Canadian adults. Prev Med. 2014;65:23–27. doi: 10.1016/j.ypmed.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 11.Buckley J.P., Mellor D.D., Morris M., Joseph F. Standing-based office work shows encouraging signs of attenuating post-prandial glycaemic excursion. Occup Environ Med. 2014;71:109–111. doi: 10.1136/oemed-2013-101823. [DOI] [PubMed] [Google Scholar]
- 12.Duvivier B.M., Schaper N.C., Bremers M.A., van Crombrugge G., Menheere P.P., Kars M. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS One. 2013;8:e55542. doi: 10.1371/journal.pone.0055542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thorp A.A., Kingwell B.A., Sethi P., Hammond L., Owen N., Dunstan D.W. Alternating bouts of sitting and standing attenuates postprandial glucose responses. Med Sci Sports Exerc. 2014;46:2053–2061. doi: 10.1249/MSS.0000000000000337. [DOI] [PubMed] [Google Scholar]
- 14.Dunstan D., Kingwell B., Larsen R., Healy G., Cerin E., Hamilton M. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35:976–983. doi: 10.2337/dc11-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thorp A.A., Owen N., Neuhaus M., Dunstan D.W. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41:207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 16.Wilmot E.G., Edwardson C.L., Achana F.A., Davies M.J., Gorely T., Gray L.J. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55:2895–2905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 17.Edwardson C.L., Gorely T., Davies M.J., Gray L.J., Khunti K., Wilmot E.G. Association of sedentary behavior with metabolic syndrome: a meta-analysis. PLoS One. 2012;7:e34916. doi: 10.1371/journal.pone.0034916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Healy G.N., Wijndaele K., Dunstan D.W., Shaw J.E., Salmon J., Zimmet P.Z. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian diabetes, obesity and lifestyle study (AusDiab) Diabetes Care. 2008;31:369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 19.Gennuso K.P., Gangnon R.E., Matthews C.E., Thraen-Borowski K.M., Colbert L.H. Sedentary behavior, physical activity, and markers of health in older adults. Med Sci Sports Exerc. 2013;45:1493–1500. doi: 10.1249/MSS.0b013e318288a1e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Healy G.N., Matthews C.E., Dunstan D.W., Winkler E.A.H., Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32:590–597. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kozey-Keadle S., Libertine A., Staudenmayer J., Freedson P. The feasibility of reducing and measuring sedentary time among overweight, non-exercising office workers. J Obes. 2012;2012:282–303. doi: 10.1155/2012/282303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levine J., Miller J. The energy expenditure of using a “walk-and-work” desk for office workers with obesity. Br J Sports Med. 2007;41:558–561. doi: 10.1136/bjsm.2006.032755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tikkanen O., Haakana P., Pesola A.J., Häkkinen K., Rantalainen T., Havu M. Muscle activity and inactivity periods during normal daily life. PLoS One. 2013;8:e52228. doi: 10.1371/journal.pone.0052228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henson J., Davies M.J., Bodicoat D.H., Edwardson C.L., Gill J.M.R., Stensel D.J. Breaking up prolonged sitting with standing or walking attenuates the postprandial metabolic response in post-menopausal women: a randomised acute study. Diabetes Care. 2016;39:130–138. doi: 10.2337/dc15-1240. [DOI] [PubMed] [Google Scholar]
- 25.Lyden K., Kozey-Keadle S.L., Staudenmayer J.W., Freedson P.S. Validity of two wearable monitors to estimate breaks from sedentary time. Med Sci Sports Exerc. 2012;44:2243–2252. doi: 10.1249/MSS.0b013e318260c477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grant P.M., Ryan C.G., Tigbe W.W., Granat M.H. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med. 2006;40:992–997. doi: 10.1136/bjsm.2006.030262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kozey-Keadle S., Libertine A., Lyden K., Staudenmayer J., Freedson P.S. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc. 2011;43:1561–1567. doi: 10.1249/MSS.0b013e31820ce174. [DOI] [PubMed] [Google Scholar]
- 28.Ryan C.G., Grant P.M., Tigbe W.W., Granat M.H. The validity and reliability of a novel activity monitor as a measure of walking. Br J Sports Med. 2006;40:779–784. doi: 10.1136/bjsm.2006.027276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stansfield B., Hajarnis M., Sudarshan R. Characteristics of very slow stepping in healthy adults and validity of the activPAL3TM activity monitor in detecting these steps. Med Eng Phys. 2015;37:42–47. doi: 10.1016/j.medengphy.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 30.Matthews C.E., Hagstromer M., Pober D.M., Bowls H.R. Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc. 2012;44(Suppl. 1):S68–76. doi: 10.1249/MSS.0b013e3182399e5b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reid N., Eakin E., Henwood T., Keogh J.W.L., Senior H.E., Gardiner P.A. Objectively measured activity patterns among adults in residential aged care. Int J Environ Res Public Health. 2013;10:6783–6798. doi: 10.3390/ijerph10126783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kelly T.L. The applicability of the Spearman-Brown Formula for the measurement of reliability. J Educ Psychol. 1925;16:300–303. [Google Scholar]
- 33.Baranowski T., Mâsse L.C., Ragan B., Welk G. How many days was that? We're still not sure, but we're asking the question better! Med Sci Sports Exerc. 2008;40(Suppl. 7):S544–9. doi: 10.1249/MSS.0b013e31817c6651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barreira T.V., Hamilton M.T., Craft L.L., Gapstur S.M., Siddique J., Zderic T.W. Intra-individual and inter-individual variability in daily sitting time and MVPA. J Sci Med Sport. 2016;19:476–481. doi: 10.1016/j.jsams.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wickel E.E., Welk G.J. Applying generalizability theory to estimate habitual activity levels. Med Sci Sports Exerc. 2010;42:1528–1534. doi: 10.1249/MSS.0b013e3181d107c4. [DOI] [PubMed] [Google Scholar]
- 36.Craft L.L., Zderic T.W., Gapstur S.M., VanIterson E.H., Thomas D.M., Siddique J. Evidence that women meeting physical activity guidelines do not sit less: an observational inclinometry study. Int J Behav NutrPhys Act. 2012;9:122. doi: 10.1186/1479-5868-9-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Swartz A.M., Rote A.E., Cho Y.I., Welch W.A., Strath S.J. Responsiveness of motion sensors to detect change in sedentary and physical activity behaviour. Br J Sports Med. 2014;48:1043–1047. doi: 10.1136/bjsports-2014-093520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Swartz A.M., Rote A.E., Welch W.A., Maeda H., Hart T.L., Cho Y.I. Prompts to disrupt sitting time and increase physical activity at work, 2011–2012. Prev Chronic Dis. 2014;11:E73. doi: 10.5888/pcd11.130318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kunkel D., Fitton C., Burnett M., Ashburn A. Physical inactivity post-stroke: a 3-year longitudinal study. Disabil Rehabil. 2014;37:304–310. doi: 10.3109/09638288.2014.918190. [DOI] [PubMed] [Google Scholar]
- 40.Aadahl M., Linneberg A., Møller T.C., Rosenørn S., Dunstan D.W., Witte D.R. Motivational counseling to reduce sitting time: a community-based randomized controlled trial in adults. Am J Prev Med. 2014;47:576–586. doi: 10.1016/j.amepre.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 41.Barry G., Galna B., Lord S., Rochester L., Godfrey A. Defining ambulatory bouts in free-living activity: impact of brief stationary periods on bout metrics. Gait Posture. 2015;42:594–597. doi: 10.1016/j.gaitpost.2015.07.062. [DOI] [PubMed] [Google Scholar]
- 42.Aguilar-Farias N., Brown W.J., Olds T.S., Geeske Peeters G.M. Validity of self-report methods for measuring sedentary behavior in older adults. J Sci Med Sport. 2015;18:662–666. doi: 10.1016/j.jsams.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 43.Berendsen B.A., Hendriks M.R., Meijer K.F., Plasqui G., Schaper N.C., Savelberg H.H. Which activity monitor to use? Validity, reproducibility and user friendliness of three activity monitors. BMC Public Health. 2014;14:749. doi: 10.1186/1471-2458-14-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tudor-Locke C., Barreira T.V., Schuna J.M., Mire E.F., Chaput J.P., Fogelholm M. Improving wear time compliance with a 24-hour waist-worn accelerometer protocol in the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE) Int J Behav Nutr Phys Act. 2015;12:11. doi: 10.1186/s12966-015-0172-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oliver M., Schofield G.M., Badland H.M., Shepherd J. Utility of accelerometer thresholds for classifying sitting in office workers. Prev Med. 2010;51:357–360. doi: 10.1016/j.ypmed.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 46.Alghaeed Z., Reilly J.J., Chastin S.F.M., Martin A., Davies G., Paton J.Y. The influence of minimum sitting period of the activPAL™ on the measurement of breaks in sitting in young children. PLoS One. 2013;8:e71854. doi: 10.1371/journal.pone.0071854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barreira T.V., Zderic T.W., Schuna J.M., Hamilton M.T., Tudor-Locke C. Free-living activity counts-derived breaks in sedentary time: are they real transitions from sitting to standing? Gait Posture. 2015;42:70–72. doi: 10.1016/j.gaitpost.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 48.Bassett D.R., John D., Conger S.A., Rider B.C., Passmore R.M., Clark J.M. Detection of lying down, sitting, standing, and stepping using two activPAL monitors. Med Sci Sports Exerc. 2014;46:2025–2029. doi: 10.1249/MSS.0000000000000326. [DOI] [PubMed] [Google Scholar]
- 49.Paul L., Brewster S., Wyke S., Gill J.M.R., Alexander G., Dybus A. Physical activity profiles and sedentary behavior in people following stroke: a cross-sectional study. Disabil Rehabil. 2015;38:362–367. doi: 10.3109/09638288.2015.1041615. [DOI] [PubMed] [Google Scholar]
- 50.Aguilar-Farias N., Brown W.J., Peeters G.M. ActiGraph GT3X+ cut-points for identifying sedentary behavior in older adults in free-living environments. J Sci Med Sport. 2014;17:293–299. doi: 10.1016/j.jsams.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 51.Godfrey A., Lord S., Galna B., Mathers J.C., Burn D.J., Rochester L. The association between retirement and age on physical activity in older adults. Age Ageing. 2014;43:386–393. doi: 10.1093/ageing/aft168. [DOI] [PubMed] [Google Scholar]
- 52.Smith L., Hamer M., Ucci M., Marmot A., Gardner B., Sawyer A. Weekday and weekend patterns of objectively measured sitting, standing, and stepping in a sample of office-based workers: the active buildings study. BMC Public Health. 2015;15:9. doi: 10.1186/s12889-014-1338-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dall P., Lyden K., John D., Granat M. 2015. Differentiating lying down from sitting using a single activPAL3™ monitor: a pilot study. International Conference on Ambulatory Monitoring of Physical Activity and Movement. Limerick, Ireland. 10–12 June. [Google Scholar]
- 54.Lyden K., John D., Dall P., Granat M., Moehlman T., Depner C. 2015. Distinguishing periods of wake during overnight sleep using the activPAL activity monitor. International Conference on Ambulatory Monitoring of Physical Activity and Movement. Limerick, Ireland. 10–12 June. [Google Scholar]
- 55.Savelberg H. 2015. Does distinguishing cycling time contribute to understanding physical activity behavior? Loch Lomond lectures “context is the key: unlocking physical behavior”. Loch Lomond, Scotland. 7–8 June. [Google Scholar]
- 56.Stephens S., Winkler E., Trost S., Dunstan D., Eakin E., Chastin S. Intervening to reduce workplace sitting time: how and when do changes to sitting time occur? Br J Sports Med. 2014;48:1037–1042. doi: 10.1136/bjsports-2014-093524. [DOI] [PubMed] [Google Scholar]
- 57.Alkhajah T.A., Reeves M., Eakin E., Winkler E., Owen N., Healy G.N. Sit-stand workstations: a pilot intervention to reduce office sitting time. Am J Prev Med. 2012;43:298–303. doi: 10.1016/j.amepre.2012.05.027. [DOI] [PubMed] [Google Scholar]
- 58.Dollman J., Pontt J.L., Rowlands A.V. Validity of self-reported sedentary time differs between Australian rural men engaged in office and farming occupations. J Sport Sci. 2016;34:1154–1158. doi: 10.1080/02640414.2015.1094185. [DOI] [PubMed] [Google Scholar]
- 59.Evans R., Fawole H., Sheriff S., Dall P., Grant P., Ryan C.G. Point-of-choice prompts to reduce sitting time at work: a randomized trial. Am J Prev Med. 2012;43:293–297. doi: 10.1016/j.amepre.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 60.Gorman E., Ashe M.C., Dunstan D.W., Hanson H.M., Madden K., Winkler E.A. Does an “activity-permissive” workplace change office workers' sitting and activity time? PLoS One. 2013;8:e76723. doi: 10.1371/journal.pone.0076723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dunstan D.W., Weisner G., Eakin E.G., Neuhaus M., Owen N., LaMontague A.D. Reducing office workers' sitting time: rationale and study design for the Stand Up Victoria cluster randomized trial. BMC Public Health. 2013;13:1057. doi: 10.1186/1471-2458-13-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Winkler E., Eakin E., Weisner G., Dunstan D., Owen N., Healy G. 2012. Integrating self-report and device-based measures to measure workplace sitting time and sitting patterns. International Congress on Physical Activity and Public Health. Sydney, Australia. 31 October–4 November. [Google Scholar]
- 63.Edwardson C.L., Bakrania K., Bodicoat D., Yates T., Healy G., Winkler E. 2015. Validation of an automated STATA algorithm developed for isolating waking wear data in activPAL data. International Conference on Ambulatory Monitoring of Physical Activity and Movement. Limerick, Ireland. 10–12 June. [Google Scholar]
- 64.van Der Berg J., Willems P., van der Velde J., Savelberg H., Schaper N., Schram M. 2015. Validation of an automated algorithm to identify waking and sleeping time in 24 hour accelerometry data. International Conference on Ambulatory Monitoring of Physical Activity and Movement. Limerick, Ireland. 10–12 June. [DOI] [PubMed] [Google Scholar]
- 65.Winkler E., Healy G., Sebastien Chastin S., Bodicoat D., Edwardson C.L., Bakrania K. 2015. Automated identification of waking wear time from continuously worn activPAL3 data: a SAS tool. International Conference on Ambulatory Monitoring of Physical Activity and Movement. Limerick, Ireland. 10–12 June. [Google Scholar]
- 66.Choi L., Liu Z., Matthews C.E., Buchowski M.S. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43:357–364. doi: 10.1249/MSS.0b013e3181ed61a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Matthews C., Kozey-Keadle S., Sampson J., Lyden K., Bowles H., Moore S. Validation of a previous-day recall measure of active and sedentary behaviors. Med Sci Sports Exerc. 2013;45:1629–1638. doi: 10.1249/MSS.0b013e3182897690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Smith L., Thomas E.L., Bell J.D., Hamer M. The association between objectively measured sitting and standing with body composition: a pilot study using MRI. BMJ Open. 2014;4:e005476. doi: 10.1136/bmjopen-2014-005476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chastin S.F.M., Culhane B., Dall P.M. Comparison of self-reported measure of sitting time (IPAQ) with objective measurement (activPAL) Physiol Meas. 2014;35:2319–2328. doi: 10.1088/0967-3334/35/11/2319. [DOI] [PubMed] [Google Scholar]
- 70.Chaput J.P., Carson V., Gray C.E., Tremblay M.S. Importance of all movement behaviors in a 24 hour period for overall health. Int J Environ Res Public Health. 2014;11:12575–12581. doi: 10.3390/ijerph111212575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.George S.M., Alfano C.M., Groves J., Karabulut Z., Haman K.L., Murphy B.A. Objectively measured sedentary time is related to quality of life among cancer survivors. PLoS One. 2014;9:e87937. doi: 10.1371/journal.pone.0087937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Júdice P.B., Santos D.A., Hamilton M.T., Sardinha L.B., Silva A.M. Validity of GT3X and Actiheart to estimate sedentary time and breaks using ActivPAL as the reference in free-living conditions. Gait Posture. 2015;41:917–922. doi: 10.1016/j.gaitpost.2015.03.326. [DOI] [PubMed] [Google Scholar]
- 73.Tieges Z., Mead G., Allerhand M., Duncan F., Wijck F.V., Fitzsimons C. Sedentary behavior in the first year after stroke: a longitudinal cohort study with objective measures. Arch Phys Med Rehabil. 2015;96:15–23. doi: 10.1016/j.apmr.2014.08.015. [DOI] [PubMed] [Google Scholar]
- 74.Neuhaus M., Healy G.N., Dunstan D.W., Owen N., Eakin E.G. Workplace sitting and height-adjustable workstations: a randomized controlled trial. Am J Prev Med. 2014;46:30–40. doi: 10.1016/j.amepre.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 75.Mutrie N., Doolin O., Fitzsimons C.F., Grant P.M., Granat M., Grealy M. Increasing older adults' walking through primary care: results of a pilot randomized controlled trial. Fam Pract. 2012;29:633–642. doi: 10.1093/fampra/cms038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wilmot E.G., Davies M.J., Edwardson C., Gorely T., Khunti K., Nimmo M. Rationale and study design for a randomised controlled trial to reduce sedentary time in adults at risk of type 2 diabetes mellitus: project STAND (Sedentary Time ANd Diabetes) BMC Public Health. 2011;11:908. doi: 10.1186/1471-2458-11-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chastin S.F.M., Ferriolli E., Stephens N.A., Fearon K.C.H., Greig C. Relationship between sedentary behaviour, physical activity, muscle quality and body composition in healthy older adults. Age Ageing. 2011;41:111–114. doi: 10.1093/ageing/afr075. [DOI] [PubMed] [Google Scholar]
- 78.Chau J.Y., Daley M., Dunn S., Srinivasan A., Do A., Bauman A.E. The effectiveness of sit-stand workstations for changing office workers' sitting time: results from the Stand@Work randomized controlled trial pilot. Int J Behav Nutr Phys Act. 2014;11:127. doi: 10.1186/s12966-014-0127-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Di Fabio D.R., Blomme C.K., Smith K.M., Welk G.J., Campbell C.G. Adherence to physical activity guidelines in mid-pregnancy does not reduce sedentary time: an observational study. Int J Behav Nutr Phys Act. 2015;12:27. doi: 10.1186/s12966-015-0191-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.English C., Healy G.N., Coates A., Lewis L., Olds T., Bernhardt J. Sitting and activity time in people with stroke. Phys Ther. 2016;96:193–201. doi: 10.2522/ptj.20140522. [DOI] [PubMed] [Google Scholar]
- 81.Esbensen B.A., Thomsen T., Hetland M.L., Beyer N., Midtgaard J., Løppenthin K. The efficacy of motivational counseling and SMS-reminders on daily sitting time in patients with rheumatoid arthritis: protocol for a randomized controlled trial. Trials. 2015;16:23. doi: 10.1186/s13063-014-0540-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fitzsimons C.F., Kirk A.F., Baker G.F., Michie F.F., Kane C.F., Mutrie N. Using an individualised consultation and activPAL feedback to reduce sedentary time in older Scottish adults: results of a feasibility and pilot study. Prev Med. 2013;57:718–720. doi: 10.1016/j.ypmed.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 83.Gardner B., Thune-Boyle I., Iliffe S., Thune-Boyle I., Fox K.R., Jefferis B.J. “On your feet to earn your seat”, a habit-based intervention to reduce sedentary behaviour in older adults: study protocol for a randomized controlled trial. Trials. 2014;15:368. doi: 10.1186/1745-6215-15-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gennuso K.P., Thraen-Borowski K.M., Gangnon R.E., Colbert L.H. Patterns of sedentary behavior and physical function in older adults. Aging Clin Exp Res. 2016;28:943–950. doi: 10.1007/s40520-015-0386-4. [DOI] [PubMed] [Google Scholar]
- 85.Granat M., Clarke C., Holdsworth R., Stansfield B., Dall P. Quantifying the cadence of free-living walking using event-based analysis. Gait Posture. 2015;42:85–90. doi: 10.1016/j.gaitpost.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 86.Klenk J., Rapp K., Denkinger M., Nagel G., Nikolaus T., Peter R. Objectively measured physical activity and vitamin D status in older people from Germany. J Epidemiol Community Health. 2015;69:388–392. doi: 10.1136/jech-2014-204632. [DOI] [PubMed] [Google Scholar]
- 87.Lord S., Chastin S.F., McInnes L., Little L., Briggs P., Rochester L. Exploring patterns of daily physical and sedentary behaviour in community-dwelling older adults. Age Ageing. 2011;40:205–210. doi: 10.1093/ageing/afq166. [DOI] [PubMed] [Google Scholar]
- 88.Lowe S.S., Danielson B., Beaumont C., Watanabe S.M., Baracos V.E., Courneya K.S. Associations between objectively measured physical activity and quality of life in cancer patients with brain metastases. J Pain Symptom Manage. 2014;48:322–332. doi: 10.1016/j.jpainsymman.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 89.Lyden K., Keadle S.K., Staudenmayer J., Braun B., Freedson P.S. Discrete features of sedentary behavior impact cardiometabolic risk factors. Med Sci Sport Exerc. 2015;47:1079–1086. doi: 10.1249/MSS.0000000000000499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Martin-Borras C., Gine-Garriga M., Martinez E., Martin-Cantera C., Puigdomenech E., Sola M. Effectiveness of a primary care-based intervention to reduce sitting time in overweight and obese patients (SEDESTACTIV): a randomized controlled trial; rationale and study design. BMC Public Health. 2014;14:228. doi: 10.1186/1471-2458-14-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mau-Moeller A., Behrens M., Finze S., Bruhn S., Bader R., Mittelmeier W. The effect of continuous passive motion and sling exercise training on clinical and functional outcomes following total knee arthroplasty: a randomized active-controlled clinical study. Health Qual Life Outcomes. 2014;12:68. doi: 10.1186/1477-7525-12-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pontt J.L., Rowlands A.V., Dollman J. Comparison of sedentary behaviours among rural men working in offices and on farms. Aust J Rural Health. 2015;23:74–79. doi: 10.1111/ajr.12143. [DOI] [PubMed] [Google Scholar]
- 93.Reid R.E.R., Carver T.E., Andersen K.M., Court O., Andersen R.E. Physical activity and sedentary behavior in bariatric patients long-term post-surgery. Obes Surg. 2015;25:1073–1077. doi: 10.1007/s11695-015-1624-8. [DOI] [PubMed] [Google Scholar]
- 94.Rosenberg D.E., Gell N.M., Jones S.M.W., Renz A., Kerr J., Gardiner P.A. The feasibility of reducing sitting time in overweight and obese older adults. Health Educ Behav. 2015;42:669–676. doi: 10.1177/1090198115577378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ryan C.G., Dall P.M., Granat M.H., Grant P.M. Sitting patterns at work: objective measurement of adherence to current recommendations. Ergonomics. 2011;54:531–538. [Google Scholar]
- 96.Sande T.A., Scott A.C., Laird B.J., Wan H.I., Fleetwood-Walker S.M., Kaasa S. The characteristics of physical activity and gait in patients receiving radiotherapy in cancer induced bone pain. Radiother Oncol. 2014;111:18–24. doi: 10.1016/j.radonc.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 97.Stewart A.D., Rolland C., Gryka A., Findlay S., Smith S., Jones J. Morphological and health-related changes associated with a 12-week self-guided exercise programme in overweight adults: a pilot study. J Sports Sci. 2014;32:164–171. doi: 10.1080/02640414.2013.812791. [DOI] [PubMed] [Google Scholar]
- 98.Thomas S., Fazakarley L., Thomas P.W., Brenton S., Collyer S., Perring S. Testing the feasibility and acceptability of using the Nintendo Wii in the home to increase activity levels, vitality and well-being in people with multiple sclerosis (Mii-vitaliSe): protocol for a pilot randomised controlled study. BMJ Open. 2014;4:e005172. doi: 10.1136/bmjopen-2014-005172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tigbe W.W., Lean M.E.J., Granat M.H. A physically active occupation does not result in compensatory inactivity during out-of-work hours. Prev Med. 2011;53:48–52. doi: 10.1016/j.ypmed.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 100.Watne L.O., Torbergsen A.C., Conroy S., Engedal K., Frihagen F., Hjorthaug G.A. The effect of a pre- and postoperative orthogeriatric service on cognitive function in patients with hip fracture: randomized controlled trial (Oslo Orthogeriatric Trial) BMC Med. 2014;12:63. doi: 10.1186/1741-7015-12-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.You Y., Wang W., Yang M., Thompson R.G. Determining commuting behaviour from monitoring technologies. Adv Mech Eng. 2015;7:167849. [Google Scholar]
- 102.Yates T., Davies M.J., Henson J., Troughton J., Edwardson C., Gray L.J. Walking away from type 2 diabetes: trial protocol of a cluster randomized controlled trial evaluating a structured education programme in those at high risk of developing type 2 diabetes. BMC Fam Pract. 2012;13:46. doi: 10.1186/1471-2296-13-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yates T., Griffin S., Bodicoat D., Brierly G., Dallosso H., Davies M.J. Promotion of physical activity through structured education with differing levels of ongoing support for people at high risk of type 2 diabetes (PROPELS): study protocol for a randomised controlled trial. Trials. 2015;16:289. doi: 10.1186/s13063-015-0813-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tanamas S., Magliano D., Lynch B., Sethi P., Willenberg L., Polkinghorne K. Baker IDI Heart and Diabetes Institute; Melbourne: 2013. AusDiab 2012. The Australian diabetes, obesity and lifestyle study. [Google Scholar]
- 105.Sadeh A., Sharkey K.M., Carskadon M.A. Activity-based sleep–wake identification: an empirical test of methodological issues. Sleep. 1994;17:201–207. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Validation of activPAL self-attachment methods—activity monitor instructions.
Thigh monitor instructions.
Activity monitor instructions and daily log.


