Abstract
This study examined the carriage of Streptococcus pneumoniae in healthy Danish children aged 8–19 months and assessed the effect of the probiotics Lactobacillus rhamnosus GG and Bifidobacterium animalis subsp lactis on the pneumococcal carriage during daycare enrolment. Potential risk factors of pneumococcal carriage were analysed and the carriage study was compared with registered invasive pneumococcal disease (IPD) data. This study is a part of the ProbiComp study, which was a double-blind, randomized controlled trial, including 290 children allocated to probiotics or placebo for 6 months and recruited during two autumn seasons (2014/2015). Pneumococci were identified by optochin sensitivity, bile solubility, α-hemolysis and/or capsular reaction. Serotyping was performed by latex agglutination kit and Quellung reaction. The carriage rate of S. pneumoniae was 26.0% at baseline and 67.4% at the end of intervention. No significant difference was observed between the placebo group and the probiotics group (p = 0.508). Children aged 8–19 months were carriers of non-pneumococcal vaccine serotypes causing IPD in children aged 0–4 years. However, serotypes causing most IPD cases in Danish elderly were either not found or found with low prevalence suggesting that children are not the main reservoir of those serotypes and other age groups need to be considered as carriers.
Introduction
Streptococcus pneumoniae can cause invasive pneumococcal disease (IPD) which worldwide is associated with high mortality and morbidity at all ages despite the use of effective vaccines1. S. pneumoniae colonizes the epithelium of the nasopharynx and at least 92 different serotypes are known2,3. S. pneumoniae can cause meningitis, otitis media, pneumonia, sinusitis and bacteremia primarily in young children and elderly4.
Carriage of S. pneumoniae is a prerequisite for developing IPD, and is most frequent in young children, who act as reservoirs4. High carriage rate is associated with a high prevalence of respiratory infections5 and it is believed that children transmit IPD serotypes to other age groups6–8. However, transmission from adults to children is also observed8. Potential risk factors of pneumococcal carriage include attending daycare, young age, having siblings in daycare, having siblings <5 years and genetic and environmental factors such as socioeconomic conditions and passive smoking4,9,10. Daycare attendance is considered a major risk factor9,11,12. The currently available vaccines protect against a limited number of the known serotypes3. The 7-valent pneumococcal conjugate vaccine (PCV7) was included in the Danish Childhood Immunization Program in 2007 and was replaced by PCV13 in 20101. PCV7 includes serotype 4, 6B, 9V, 14, 18C, 19F, and 23F while PCV13 includes the PCV7-serotypes and additional serotypes 1, 3, 5, 6A, 7F, and 19A1,7. PCV7 led to a significant reduction in IPD caused by PCV7-serotypes markedly among children aged <2 years1,3,6,13, but also a significant reduction in IPD cases and carriage of vaccine serotypes among older children and adults was seen, especially in the age group 65+ years3,8. This phenomenon is known as herd protection8. With the reduction of PCV-serotypes, an increase in the incidences of IPD caused by non-vaccine serotypes has been observed1,6,7. Thus, it is important to continue surveillance of serotype distribution.
Only a few pneumococcal carriage studies in children have been conducted in Denmark, the most recent was prior to the introduction of PCV79.
The purpose of this study was to assess the effect of probiotics on S. pneumoniae carriage in healthy Danish children aged 8–19 months, determine serotype distribution and analyse risk factors for pneumococcal carriage. Furthermore, to assess whether the carried serotypes are also isolated in IPD cases of all age groups as described by Slotved et al. (2016)14,15 and Harboe et al.16.
Methods
Study population
This study is part of the ProbiComp study, which was a randomised, double-blind, placebo-controlled parallel study investigating the effect of probiotics on infections in young children starting daycare described in details in Laursen et al.17.
The ProbiComp study included 290 healthy children aged 8–13 months starting daycare within 12 weeks after start of intervention. They were randomly assigned to a combination of the probiotics Lactobacillus rhamnosus GG (LGG) and Bifidobacterium animalis subsp lactis (BB-12), administered orally, in a dose of 109 colony-forming units/day (CFU/day) of each or placebo (maltodextrin) for 6 months. Children were examined at baseline before start of intervention and 6 months later at the end of intervention. The children were recruited during two autumn seasons from mid-August to mid-December in 2014 and 2015. LGG and BB-12 are registered trademarks of Chr. Hansen A/S. For exclusion criteria see Laursen et al.17. Study design, compliance, randomisation, data collection, outcome measurements and sample size calculation are described in Laursen et al.17. Briefly, both parents and study personnel were blinded to group allocation, and the placebo powder and the probiotics powder did not differ in smell, taste or colour. Parents registered daily whether the child had ingested the product and by the end of intervention the parents returned the registration sheets and unused sachets with powder to evaluate compliance. PCV13 is administered in a 2 + 1 dose schedule at the age of 3, 5 and 12 months1. At baseline 98.2% of the children examined were covered by at least one dose of PCV13, while 92.6% were covered by two doses. At the end of intervention 88.0% of the children were covered by all three doses of PCV13. Vaccination data were obtained at the Danish Vaccination Register (DDV) (record number 2015-57-0102). Information regarding the children’s background and health were obtained by interviewing parents and during the intervention period occurrence of children’s symptoms of illness, absence from daycare, doctor’s visits, and doctor-diagnosed illnesses were registered by the parents in weekly and daily web-based questionnaires17.
Nasal swab sampling
Two autumn seasons were included in the study. At baseline, samples were analysed from 141 children from the first season (2014) and 144 children from the second season (2015). At the end of intervention, samples from 124 children from the first season and 134 children from the second season were analysed.
Nasal swab samples were collected by a modified version of Satzke et al.18. Minitip flocked swabs (FLOQSwabs™, Copan, Italy) were used to take the samples. The swabs were inserted as far as possible into the nasal cavity and rotated, although within the limitations of the children’s comfort. They were then placed in 1 mL Luria-Bertani (LB) broth with 10% glycerol in cryotubes, and stored at −80 °C until analysis.
Identification of pneumococcal serotypes
Identification of pneumococcal serotypes was performed as previously described4. Briefly, 10 µL of each sample was added to 3 mL serum-ox broth and incubated overnight at 37 °C in 5% CO2, before plating. The following day 1 µL of each serum-ox broth was cultured on 10% horse blood agar plates, which were incubated overnight at 37 °C, 5% CO2. S. pneumoniae were identified based on optochin sensitivity, bile solubility, α-hemolysis and/or capsular reaction (Quellung reaction). Pneumotest latex agglutination kit (SSI Diagnostica, Hillerød, Denmark) was performed on the serum-broth to determine pneumococcal group. Serotypes were identified by the Quellung reaction (Neufeld test) using serotype specific antisera (SSI Diagnostica, Hillerød, Denmark). The specimens were screened by pneumotest latex agglutination kit for multiple serotypes. If multiple serotypes were found, they were isolated and serotyped.
Invasive pneumococcal disease data
Data on invasive pneumococcal isolates in the period 2014–2016 were obtained from the Danish laboratory surveillance system at the National Neisseria and Streptococcus Reference Laboratory (NSR), Statens Serum Institut (SSI) as described by Slotved et al. (2016)14,15. Briefly, information on age and serotype was used. An IPD case was defined as S. pneumoniae occurring in normally sterile sites such as cerebrospinal fluid or blood. The coverage and evaluation of the database in Denmark was described by Harboe et al.16.
Data analysis
RStudio version 1.0.136 and R version 3.4.1 for Windows was used for calculation of odds ratios (OR), confidence intervals (95% CI), and p-values using two tailed Fisher’s Exact Test (http://www.r-project.org/ last accessed: 02.20.2018). A p-value < 0.05 was considered significant. RStudio was also used to make graphical illustrations.
We examined several risk factors for pneumococcal carriage including sex, having siblings <5 years, breastfeeding at baseline examination, living with a dog or cat, passive smoking exposure in the household, having respiratory infections such as bronchitis, pneumonia or otitis media during the intervening period and the effect of receiving antibiotics during the intervening period of 6 months. We did not have access to dates on when antibiotics were received. Univariate logistic regression was not undertaken as confounders were evenly distributed during the randomization process, therefore multivariate logistic regression was not required. Crude odds ratio of pneumococcal carriage was estimated in each characteristic (sex, having siblings <5, breastfeeding, respiratory infections including bronchitis, pneumonia and otitis media, antibiotic use, passive smoking exposure and exposure to cats or dogs) using two-tailed Fisher’s exact test.
Ethical considerations
The ProbiComp study protocol was approved by the Committees on Biomedical Research Ethics for the Capital Region of Denmark (H-4-2014-032), and we hereby confirm that all methods were performed according to the guidelines and regulations approved by the Committees on Biomedical Research Ethics. The study was registered at clinicaltrials.gov (identifier NCT02180581 (Supplementary file), posted 02/07/2014)17. Informed consent from parents and legal guardians of the children was required. Participation in the study was voluntary and parents could withdraw their consent at any time17.
Regarding IPD data, no ethical approval or informed consent was required since data were collected routinely for national surveillance purposes. Using the data is approved by the Danish Data Protection Agency (record number 2007-41-0229).
Results
Carriage study
The carriage rate of S. pneumoniae at baseline of the two seasons were comparable with no statistical significant difference between the two seasons as seen in Table 1. Hence, the two seasons were combined as one baseline group for further analysis. The mean carriage rate at baseline therefore was 26.0% (CI 20.8–31.1%) (Table 1).
Table 1.
Comparison of carriage rate of the two seasons and a comparison of the placebo groups and the probiotics groups. Odds ratios (OR) and p-values were calculated by two-tailed Fisher’s exact test.
| Carriage rate, % (95% CI) | OR (95% CI)* | p-value* | |
|---|---|---|---|
| Baseline | |||
| Season 1 (2014) | 27.7 (20.3–35.0%) | 1.00 | 1.00 |
| Season 2 (2015) | 24.3 (17.3–31.3%) | 0.840 (0.477–1.477) | 0.589 |
| End of intervention | |||
| Season 1 placebo group | 60.7 (48.4–72.9%) | 1.00 | 1.00 |
| Season 2 placebo group | 69.6 (58.7–80.4%) | 1.478 (0.674–3.268) | 0.356 |
| Season 1 probiotics group | 76.2 (65.7–86.7%) | 1.00 | 1.00 |
| Season 2 probiotics group | 63.1 (51.3–74.8%) | 0.536 (0.229–1.228) | 0.127 |
| Placebo group | 65.4 (57.2–73.6%) | 1.00 | 1.00 |
| Probiotics group | 69.5 (61.6–77.5%) | 1.207 (0.694–2.107) | 0.508 |
| Overall carriage rate | |||
| Baselinea | 26.0 (20.8–31.1%) | 1.00 | 1.00 |
| End of interventionb | 67.4 (61.7–73.2%) | 5.884 (4.007–8.715) | <0.001c |
aMean of season 1 (2014) and season 2 (2015). bMean of the placebo group and the probiotics group. cComparison of the baseline and the end of intervention. *Calculated by Fisher’s Exact Test in RStudio. CI: confidence intervals, OR: odds ratio.
At the end of intervention half of the children had received the probiotics LGG and BB-12 for 6 months, hence each season included both a placebo group and a probiotics given group (Table 1). The two seasons were alike with no statistical significant difference between the two placebo groups and the two probiotics groups, hence data were combined into one placebo group and one probiotics group (Table 1).
The carriage rate of S. pneumoniae in children receiving the probiotics LGG and BB-12 was 69.5% (CI 61.6–77.5%) while the carriage rate in the placebo group was 65.4% (CI 57.2–73.6%). Thus, probiotics do not have a significant effect on the pneumococcal carriage rate (p = 0.508) (Table 1). Furthermore, the serotype diversity/distribution in the probiotics group and placebo group were not significantly different (data not shown). The placebo group and the probiotics group were therefore combined into one group representing the end of intervention for further analysis. The carriage rate at the end of intervention was 67.4% (CI 61.7–73.2%), which is significantly higher than the carriage rate at baseline (p < 0.001) (Table 1).
All the cases of multiple serotype carriage involved two serotypes except one child at the end of intervention, who carried three serotypes (Table 2).
Table 2.
Carriage rate and proportion of carriers with multiple serotypes.
| Baseline | End of intervention | |
|---|---|---|
| Number of children analyzed | 285 | 258 |
| Age | 8–13 months | 14–19 months |
| Year of swab sample collection | 2014 and 2015 (autumn) | 2015 and 2016 (spring) |
| Carriage rate, % (N) | 26.0 (74) | 67.4 (174) |
| Proportion carriers with >1 serotype, % (N) | 2.5 (7) | 4.3 (11) |
| Proportion carriers with >2 serotype, % (N) | 0 (0) | 0.4 (1) |
N: number of carriers.
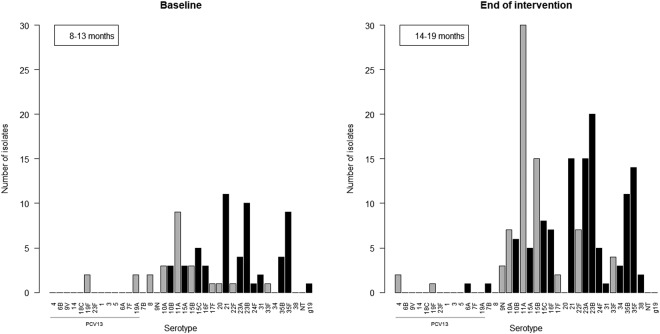
The 81 isolates found at baseline belonged to 21 different serotypes and 1 serogroup (where serotyping was not possible) (Fig. 1). The most common serotype isolated at baseline was serotype 21 constituting 13.6% of all isolates. Serotype 23B, 35F and 11A were also commonly isolated, constituting 12.3%, 11.1% and 11.1% of all isolates respectively (Fig. 1). The only PCV13-serotypes isolated at baseline were 19A and 19F, which both constituted 2.5% of all isolates.
Figure 1.
Carriage study and serotype distribution in Danish children at baseline and at the end of intervention. Grey color indicates PPV23-serotypes, black is non-PPV23 serotypes. Serotypes are listed with PCV7-serotypes first, then PCV13-serotypes followed by non-PCV13-serotypes.
At the end of intervention we found 185 isolates belonging to 24 different serotypes. Serotype 11A was the most common serotype constituting 16.2% of all isolates. Serotype 23B, 15B, 21, 23A and 35F were also common, constituting 10.8%, 8.1%, 8.1%, 8.1% and 7.6% of all isolates respectively (Fig. 1). Serotype 4, 19F and 6A were the only PCV13-serotypes found at the end of intervention, only constituting 1.1%, 0.5% and 0.5% of all isolates respectively (Fig. 1).
Serotype 8 was only found in two children at baseline (Fig. 1).
Risk factors
Sex did not influence the carriage rate of S. pneumoniae significantly (p = 0.280 at baseline and p = 0.187 at end of intervention) (Tables 3 and 4).
Table 3.
Potential risk factors for pneumococcal carriage in the baseline group and at the end of study. The table shows number of carriers, total number of children, carriage rates, p-values, odds ratios (OR) and confidence intervals (CI).
| Number of carriers (total number of children) | Carriage rate % (95% CI) | OR (95% CI)* | p-value* | ||
|---|---|---|---|---|---|
| Baseline | |||||
| Sex | Females | 32 (140) | 22.9 (15.9–29.8%) | 1.00 | 1.00 |
| Males | 42 (145) | 29.0 (21.6–36.3%) | 1.375 (0.781–2.436) | 0.280 | |
| Siblings <5 years | No** | 14 (148) | 9.5 (4.7–14.2%) | 1.00 | 1.00 |
| Yes | 49 (94) | 52.1 (42.0–62.2%) | 10.299 (5.043–22.217) | <0.001 | |
| Breastfeeding at baseline examination | No | 32 (150) | 21.3 (14.8–27.9%) | 1.00 | 1.00 |
| Yes | 42 (135) | 31.1 (23.3–38.9%) | 1.662 (0.944–2.950) | 0.078 | |
| Respiratory infections during intervening period *** | No | N/A | N/A | N/A | N/A |
| Yes | N/A | N/A | N/A | N/A | |
| Bronchitis | No | N/A | N/A | N/A | N/A |
| Yes | N/A | N/A | N/A | N/A | |
| Pneumonia | No | N/A | N/A | N/A | N/A |
| Yes | N/A | N/A | N/A | N/A | |
| Otitis media | No | N/A | N/A | N/A | N/A |
| Yes | N/A | N/A | N/A | N/A | |
| Systemic antibiotic during intervening period | No | N/A | N/A | N/A | N/A |
| Yes | N/A | N/A | N/A | N/A | |
| Passive smoking | No | 67 (247) | 27.1 (21.6–32.7%) | 1.00 | 1.00 |
| Yes | 7 (38) | 18.4 (6.1–30.7%) | 0.608 (0.215–1.495) | 0.322 | |
| Living with a dog or cat | No | 56 (221) | 25.3 (19.6–31.1%) | 1.00 | 1.00 |
| Yes | 14 (47) | 29.8 (16.7–42.9%) | 1.249 (0.574–2.608) | 0.584 | |
*Odds ratios, confidence intervals and p-values were calculated by two-tailed Fisher’s Exact Test. **No siblings at all ***including bronchitis, pneumonia, sore throat, sinusitis, croup and otitis media N/A = not available.
CI: confidence interval, OR: odds ratio.
Table 4.
Potential risk factors for pneumococcal carriage in the baseline group and at the end of intervention. The table shows number of carriers, total number of children, carriage rates, p-values, odds ratios (OR) and confidence intervals (CI).
| Number of carriers (total number of children) | Carriage rate % (95% CI) | OR (95% CI)* | p-value* | ||
|---|---|---|---|---|---|
| End of intervention | |||||
| Sex | Females | 90 (126) | 71.4 (63.5–79.3%) | 1.00 | 1.00 |
| Males | 84 (132) | 63.6 (55.4–71.8%) | 0.701 (0.400–1.222) | 0.187 | |
| Siblings <5 years | No** | 89 (130) | 68.5 (60.5–76.4%) | 1.00 | 1.00 |
| Yes | 59 (88) | 67.0 (57.2–76.9%) | 0.938 (0.506–1.748) | 0.883 | |
| Breastfeeding at baseline examination | No | 89 (134) | 66.4 (58.4–74.4%) | 1.00 | 1.00 |
| Yes | 85 (124) | 68.5 (60.4–76.7%) | 1.102 (0.633–1.922) | 0.791 | |
| Respiratory infections during intervening period*** | No | 97 (139) | 69.8 (62.2–77.4%) | 1.00 | 1.00 |
| Yes | 77 (119) | 64.7 (56.1–73.3%) | 0.795 (0.456–1.384) | 0.425 | |
| Bronchitis | No | 164 (236) | 69.5 (63.6–75.4%) | 1.00 | 1.00 |
| Yes | 10 (22) | 45.5 (24.6–66.3%) | 0.367 (0.135–0.975) | 0.031 | |
| Pneumonia | No | 149 (222) | 67.1 (60.9–73.3%) | 1.00 | 1.00 |
| Yes | 25 (36) | 69.4 (54.4–84.5%) | 1.113 (0.495–2.650) | 0.85 | |
| Otitis media | No | 127 (182) | 69.8 (63.1–76.5%) | 1.00 | 1.00 |
| Yes | 47 (76) | 61.8 (50.9–72.8%) | 0.703 (0.387–1.285) | 0.244 | |
| Systemic antibiotic during intervening period | No | 113 (163) | 69.3 (62.2–76.4%) | 1.00 | 1.00 |
| Yes | 61 (95) | 64.2 (54.8–73.9%) | 0.795 (0.45–1.41) | 0.411 | |
| Passive smoking | No | 152 (226) | 67.3 (61.1–73.4%) | 1.00 | 1.00 |
| Yes | 22 (32) | 68.8 (52.7–84.8%) | 1.071 (0.458–2.669) | 1 | |
| Living with a dog or cat | No | 141 (200) | 70.5 (64.2–76.8%) | 1.00 | 1.00 |
| Yes | 24 (42) | 57.1 (42.2–72.1%) | 0.559 (0.268–1.181) | 0.103 | |
*Odds ratios, confidence intervals and p-values were calculated by two-tailed Fisher’s Exact Test. **No siblings at all ***including bronchitis, pneumonia, sore throat, sinusitis, croup and otitis media N/A = not available.
CI: confidence interval, OR: odds ratio.
Having siblings <5 years significantly increased the carriage rate of S. pneumoniae in children at baseline (p < 0.001), but did not influence the carriage rate of children at the end of intervention (p = 0.883) (Tables 3 and 4).
Breastfeeding at the time of baseline examination, receiving systemic antibiotics during the intervention period, exposure to passive smoking or living with a dog or cat did not influence the carriage rate of S. pneumoniae (Tables 3 and 4).
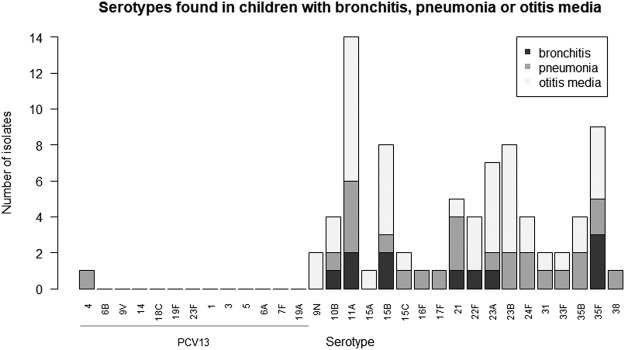
We examined if children with respiratory infections during the intervening period had an increased risk of pneumococcal carriage, but no significant difference in carriage rate was observed between children having had respiratory infections or children not affected by respiratory infections (p = 0.425) (Table 4). However, children who had experienced bronchitis during intervention seemed to have a lower carriage rate compared to children who had not experienced bronchitis (p = 0.031), but this result may not be reliable due to the low number of children in the cohort (Table 4). Serotype distribution in children who have experienced bronchitis, pneumonia or otitis media is shown in Fig. 2.
Figure 2.
Serotypes and number of isolates found in children who have experienced bronchitis, pneumonia and/or otitis media in the intervening period between baseline and the end of intervention. Infections were at any time during the intervening period. Serotypes are mentioned as PCV7-serotypes first, then PCV13-serotypes followed by non-PCV13-serotypes.
Registered invasive pneumococcal diseases in Denmark
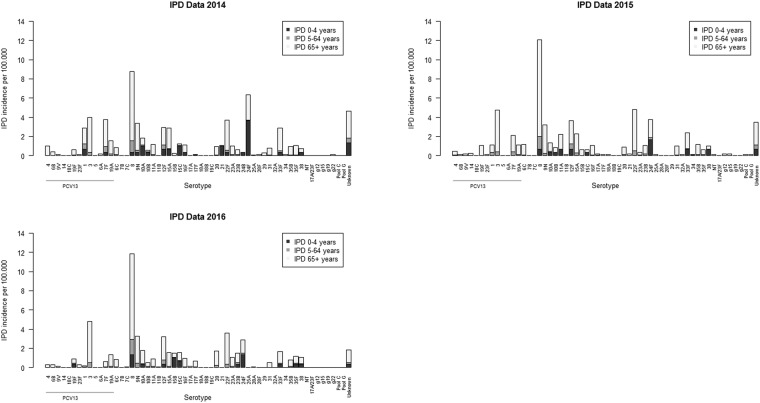
Data regarding IPD-causing serotypes in Denmark were obtained from the Danish laboratory surveillance system as mentioned in the methods section and Fig. 3 shows the data. Serotype 24F caused most of the IPDs in Denmark among 0–4 years old children in 2014 and 2015. Other commonly isolated serotypes from this patient group was 10A, 15C and 21 in 2014 and 8, 12F, 33F, 11A and 38 in 2015. In 2016 serotype 8 was causing most of the IPDs among 0–4 years old and the second most common serotype isolated was 24F.
Figure 3.
Serotypes found in patients with IPD aged 0–4 years, 5–64 years and 65+ years. The figure shows IPD incidences per 100.000. Serotypes are mentioned as PCV7-serotypes first, then PCV13-serotypes followed by non-PCV13-serotypes. Data were obtained from the Danish laboratory surveillance system at the National Neisseria and Streptococcus Reference Laboratory (NSR), Statens Serum Institut (SSI) as described by Slotved et al. (2016)14,15.
Among 5–64 years old serotype 8 was causing most of the registered IPDs in both 2014–2016. Among 65+ years old serotype 8 was also causing most of the IPD cases in Denmark in 2014–2016. Serotype 3, 7F, 9N, 22F and 12F were also common serotypes isolated in patients aged 65+ years in 2014–2016.
Discussion
To our knowledge this is the first carriage study of S. pneumoniae in children after the introduction of PCV in Denmark in 2007.
Oral administration of probiotics to children aged 8–13 months for 6 months had no effect on the carriage of pneumococcal serotypes as tested in two different years (2014 and 2015). Furthermore, we found an overall carriage rate in children attending daycare (end of intervention) of 67.4% as compared to a carriage rate of 69% before the introduction of PCV7 into the Danish Childhood Immunization Program9,19. Thus, PCV-use seems not to have influenced the overall carriage rate in children.
Pneumococcal vaccine-serotypes such as 6A, 23F, 14 and 19F, were frequently observed as carried serotypes in Denmark prior to the introduction of PCVs9. Our study revealed that vaccine-serotypes have almost disappeared in Danish children aged <2 years after the introduction of PCV13 and have been replaced by non-vaccine serotypes such as 11A, 23B, 23A, 21, 15B, 15C, 35F and 35B (Fig. 1) as observed in other countries7,10,20–22.
Living with siblings <5 years of age significantly increased the risk of pneumococcal carriage before starting in daycare (baseline) (p < 0.001) (Table 3). This has also been observed by others10–12. We found no significant difference in carriage rate of S. pneumoniae among children receiving probiotics and children receiving placebo (Table 1). Nasopharyngeal carriage of S. pneumoniae is considered a prerequisite for developing pneumococcal associated diseases such as otitis media, pneumonia, bronchitis and other respiratory infections5,23,24. Wong et al. reported that the probiotic LGG inhibits the adherence of S. pneumoniae to human epithelial cells in vitro25. Clinical studies investigating the effect of administrating probiotics on the incidence of respiratory tract infections have shown inconclusive results. Laursen et al.17 did not find LGG and BB-12 to reduce the number of days absent from daycare because of respiratory or gastrointestinal infections in the same children as included in our study, and the probiotics did not affect the endogenous gut microbiota composition in those children26. A Swedish study involving 248 healthy children aged 1–5 years and attending daycare showed a significantly lower incidence of otitis media in children who ingested milk with 107 CFU/mL Lactobacillus rhamnosus LB21 compared to placebo27. However, a study including 309 otitis media-prone children aged 10 months to 6 years showed no significant difference in the incidence of otitis media or nasopharyngeal carriage of S. pneumoniae between the group receiving capsules containing probiotics (8–9 × 109 CFU/capsule) and the placebo group28. Others found that LGG and Bifidobacterium lactis ingested orally reduced the risk of otitis media and recurrent respiratory infections in children <2 years29, as did milk containing LGG in healthy children aged 1–6 years30, while Skovbjerg et al.31 report that nasal delivery of the probiotic Lactobacillus rhamnosus did not affect nasopharyngeal pneumococcal carriage in children aged 1–8 years with secretory otitis media31.
The carriage rate at the end of intervention was significantly higher than at baseline (p < 0.001) (Table 1). The age difference between these two groups was small (8–13 months at baseline and 14–19 months at the end of intervention), and the use of probiotics during intervention did not affect the carriage rate (Table 1), hence these factors could not be the reason for this difference. Baseline samples were collected during autumn season, while samples at the end of intervention were collected 6 months later (spring season), however the effect of seasonality on the carriage of S. pneumoniae is not clear4. The children were not attending daycare at baseline, while all the children attended daycare at the end of intervention. Attending daycare is considered an important risk factor in relation to acquisition of pneumococcal carriage9,11,12, hence the higher carriage rate at the end of intervention might be explained by daycare attendance.
Since we consider our data non-parametric and the general choice of statistical test within this field is two-tailed Fishers exact test we have used the univariate analysis by two-tailed Fisher’s Exact Test to calculate the risk factors. This is not an age-matched group however the range of the age group is very small and we have not found studies showing such small age range to chance the carriage rate but external factors do chance the carriage rate such as daycare attendance9,11,12. Most studies include children aged 0–24 months as one group3,4,7,9,20,29 and since the children included in our study are aged 8–19 months we believe the age range is not significant. The main differences between the baseline group (aged 8–13 months) and end of intervention group (aged 14–19 months) is daycare attendance and whether the children have received probiotics or not.
It is believed that children with high colonization rates of S. pneumoniae are the key transmitters of non-vaccine serotypes causing IPD to other age groups6,8,22,32. IPD caused by vaccine-serotypes has declined significantly after the implementation of PCV in children, while IPD caused by non-vaccine serotypes has increased8,14,33. This is consistent with the decline in carriage of vaccine-serotypes and an increase in carriage of non-vaccine serotypes in children which is supported here (Fig. 1) and by others7,20,22,34. Despite the use of effective vaccines, serotypes 3, 7F and 19A, which are included in PCV13, are still causing IPD among elderly in Denmark13,14 (Fig. 3). The low carriage rate of serotype 8 among 8–19 months old Danish children in our study contrasts the high prevalence of serotype 8 seen among elderly patients with IPD in Denmark. The other 5 most common serotypes (3, 22F, 9N, 12F and 7F) isolated from elderly with IPD in 2014–2016 were either not found or found with low prevalence (Figs 1 and 3). It has been assumed that immunization of infants alone would result in herd immunity and hence protect adults and elderly against disease caused by vaccine-serotypes21,35,36. Our findings suggest that children aged 8–19 months are not the main reservoir of serotypes causing IPD in elderly, but suggest that other age groups need to be considered as main carriers of some pneumococcal serotypes.
We detected that children aged 8–19 months were carriers of serotypes 24F, 10A, 11A, 15A, 15B, 21, which cause IPD in children aged 0–4 years (Figs 1 and 3).
The limitation of this study is that it included a narrow age group of children (8–19 months) and that the study only included children living in the capital region of Denmark. The strength of the study is, that we have examined very young children who usually are difficult to collect swab samples from and were able to obtain detailed background information regarding the participants.
In conclusion, this study revealed that PCV-serotypes have disappeared in children and been replaced by non-PCV serotypes after the introduction of PCVs in Denmark. The probiotics LGG and BB-12 did not prevent carriage of S. pneumoniae in children attending daycare. Having a sibling <5 years before daycare increased the risk of pneumococcal carriage significantly. Children aged 8–19 months are carriers of pneumococcal serotypes causing IPD in children aged 0–4 years. However, the children seem not to be carriers of serotypes causing the majority of IPD cases in elderly in Denmark.
Electronic supplementary material
Acknowledgements
We are sincerely grateful to the children and their parents for participating in this study. We are grateful to Inge Birgit Rasmussen, KU, for the collection of nasal swabs. A special thanks to Kirsten Burmeister and Monja Hammer, SSI, for their laboratory analysis of the swab samples and input to this study. This work was supported by the Innovation Fund Denmark (IFD) under File No. DFF – 6166-00035 to K.A. Krogfelt, SSI. The ProbiComp study was funded by Innovation Fund Denmark [grant number 0603-00579B] to Michaelsen K.F., Department of Nutrition, Exercise and Sports, Faculty of Science, University of Copenhagen, Denmark, and by Chr. Hansen A/S, Denmark.
Author Contributions
S.F. and H.C.S. coordinated the investigation of the carriage study of the greater ProbiComp study. S.F. analysed the swab samples, interpreted the data and wrote the manuscript. H.C.S. helped interpreting data and formulating the manuscript. H.C.S., K.A.K. and K.F. helped with laboratory coordination at Statens Serum Institut. A.L. and C.M. designed the ProbiComp intervention study. Data regarding the participants’ background and health were obtained by R.P.L., as well as the nasal swabs. All authors helped with data analysis, and critically revised and approved the final manuscript.
Competing Interests
Hans-Christian Slotved are involved with projects supported by Pfizer. Christian Mølgaard has received financial support from Chr. Hansen A/S. All other authors had no conflicts of interest.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-33583-9.
References
- 1.Harboe ZB, et al. Impact of 13-valent pneumococcal conjugate vaccination in invasive pneumococcal disease incidence and mortality. Clin. Infect. Dis. 2014;59:1066–1073. doi: 10.1093/cid/ciu524. [DOI] [PubMed] [Google Scholar]
- 2.Kapatai G, et al. Whole genome sequencing of Streptococcus pneumoniae: development, evaluation and verification of targets for serogroup and serotype prediction using an automated pipeline. PeerJ. 2016;4:e2477. doi: 10.7717/peerj.2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steens A, Bergsaker MAR, Aaberge IS, Rønning K, Vestrheim DF. Prompt effect of replacing the 7-valent pneumococcal conjugate vaccine with the 13-valent vaccine on the epidemiology of invasive pneumococcal disease in Norway. Vaccine. 2013;31:6232–6238. doi: 10.1016/j.vaccine.2013.10.032. [DOI] [PubMed] [Google Scholar]
- 4.Navne JE, et al. Nasopharyngeal bacterial carriage in young children in Greenland: A population at high risk of respiratory infections. Epidemiol. Infect. 2016;144:3226–3236. doi: 10.1017/S0950268816001461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia-Rodriguez JA. Dynamics of nasopharyngeal colonization by potential respiratory pathogens. J. Antimicrob. Chemother. 2002;50:59–74. doi: 10.1093/jac/dkf506. [DOI] [PubMed] [Google Scholar]
- 6.Waight PA, et al. Effect of the 13-valent pneumococcal conjugate vaccine on invasive pneumococcal disease in England and Wales 4 years after its introduction: an observational cohort study. Lancet. Infect. Dis. 2015;15:535–43. doi: 10.1016/S1473-3099(15)70044-7. [DOI] [PubMed] [Google Scholar]
- 7.Steens A, Caugant DA, Aaberge IS, Vestrheim DF. Decreased carriage and genetic shifts in the Streptococcus pneumoniae population after changing the seven-valent to the thirteen-valent pneumococcal vaccine in Norway. Pediatr. Infect. Dis. J. 2015;34:875–883. doi: 10.1097/INF.0000000000000751. [DOI] [PubMed] [Google Scholar]
- 8.Van Der Linden M, Falkenhorst G, Perniciaro S, Imöhl M. Effects of infant pneumococcal conjugate vaccination on serotype distribution in invasive pneumococcal disease among children and adults in Germany. PLoS One. 2015;10:1–17. doi: 10.1371/journal.pone.0131494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harboe ZB, Slotved H-C, Konradsen HB, Kaltoft MS. A Pneumococcal Carriage Study in Danish Pre-school Children before the Introduction of Pneumococcal Conjugate Vaccination. Open Microbiol. J. 2012;6:40–4. doi: 10.2174/1874285801206010040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spijkerman J, et al. Carriage of Streptococcus pneumoniae 3 years after start of vaccination program, the Netherlands. Emerg Infect Dis. 2011;7:584–91. doi: 10.3201/eid1704.101115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Principi N, Marchisio P, Schito GC, Mannelli S. Risk factors for carriage of respiratory pathogens in the nasopharynx of healthy children. Ascanius Project Collaborative Group. Pediatr. Infect. Dis. J. 1999;18:517–23. doi: 10.1097/00006454-199906000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Huang SS, et al. Continued impact of pneumococcal conjugate vaccine on carriage in young children. Pediatrics. 2009;124:e1–11. doi: 10.1542/peds.2008-3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Slotved HC. Other age groups than children need to be considered as carriers of Streptococcal pneumoniae serotypes. Human Vaccines and Immunotherapeutics. 2016;12:2670–2674. doi: 10.1080/21645515.2016.1197451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slotved H, Dalby T, Hoffmann S. The effect of pneumococcal conjugate vaccines on the incidence of invasive pneumococcal disease caused by ten non-vaccine serotypes in Denmark. Vaccine. 2016;34:769–74. doi: 10.1016/j.vaccine.2015.12.056. [DOI] [PubMed] [Google Scholar]
- 15.Slotved HC, et al. The incidence of invasive pneumococcal serotype 3 disease in the Danish population is not reduced by PCV-13 vaccination. Heliyon. 2016;2:e00198. doi: 10.1016/j.heliyon.2016.e00198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harboe ZB, et al. Temporal Trends in Invasive Pneumococcal Disease and Pneumococcal Serotypes over 7 Decades. Clin. Infect. Dis. 2010;50:329–337. doi: 10.1086/649872. [DOI] [PubMed] [Google Scholar]
- 17.Laursen RP, et al. Probiotics and Child Care Absence Due to Infections: A Randomized Controlled Trial. Pediatrics. 2017;140:e20170735. doi: 10.1542/peds.2017-0735. [DOI] [PubMed] [Google Scholar]
- 18.Satzke C, et al. Standard method for detecting upper respiratory carriage of Streptococcus pneumoniae: updated recommendations from the World Health Organization Pneumococcal Carriage Working Group. Vaccine. 2014;32:165–79. doi: 10.1016/j.vaccine.2013.08.062. [DOI] [PubMed] [Google Scholar]
- 19.Kaltoft MS, Skov Sørensen UB, Slotved HC, Konradsen HB. An easy method for detection of nasopharyngeal carriage of multiple Streptococcus pneumoniae serotypes. J. Microbiol. Methods. 2008;75:540–544. doi: 10.1016/j.mimet.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 20.Sigurdsson S, et al. Pneumococcal vaccination: Direct and herd effect on carriage of vaccine types and antibiotic resistance in Icelandic children. Vaccine. 2017;35:5242–5248. doi: 10.1016/j.vaccine.2017.08.020. [DOI] [PubMed] [Google Scholar]
- 21.Van Hoek AJ, et al. Pneumococcal carriage in children and adults two years after introduction of the thirteen valent pneumococcal conjugate vaccine in England. Vaccine. 2014;32:4349–4355. doi: 10.1016/j.vaccine.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 22.Bosch AATM, et al. Nasopharyngeal carriage of Streptococcus pneumoniae and other bacteria in the 7th year after implementation of the pneumococcal conjugate vaccine in the Netherlands. Vaccine. 2016;34:531–539. doi: 10.1016/j.vaccine.2015.11.060. [DOI] [PubMed] [Google Scholar]
- 23.Simell B, et al. The fundamental link between pneumococcal carriage and disease. Expert Rev. Vaccines. 2012;11:841–855. doi: 10.1586/erv.12.53. [DOI] [PubMed] [Google Scholar]
- 24.Syrjänen RK, Auranen KJ, Leino TM, Kilpi TM, Mäkelä PH. Pneumococcal acute otitis media in relation to pneumococcal nasopharyngeal carriage. Pediatr. Infect. Dis. J. 2005;24:801–806. doi: 10.1097/01.inf.0000178072.83531.4f. [DOI] [PubMed] [Google Scholar]
- 25.Wong S-S, et al. Inhibition of Streptococcus pneumoniae adherence to human epithelial cells in vitro by the probiotic Lactobacillus rhamnosus GG. BMC Res. Notes. 2013;6:135. doi: 10.1186/1756-0500-6-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Laursen MF, et al. Administration of two probiotic strains during early childhood does not affect the endogenous gut microbiota composition despite probiotic proliferation. BMC Microbiol. 2017;17:1–9. doi: 10.1186/s12866-017-1090-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stecksén-Blicks C, Sjöström I, Twetman S. Effect of long-term consumption of milk supplemented with probiotic lactobacilli and fluoride on dental caries and general health in preschool children: a cluster-randomized study. Caries Res. 2009;43:374–81. doi: 10.1159/000235581. [DOI] [PubMed] [Google Scholar]
- 28.Hatakka K, et al. Treatment of acute otitis media with probiotics in otitis-prone children-A double-blind, placebo-controlled randomised study. Clin. Nutr. 2007;26:314–321. doi: 10.1016/j.clnu.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 29.Rautava S, Salminen S, Isolauri E. Specific probiotics in reducing the risk of acute infections in infancy - A randomised, double-blind, placebo-controlled study. Br. J. Nutr. 2009;101:1722–1726. doi: 10.1017/S0007114508116282. [DOI] [PubMed] [Google Scholar]
- 30.Hatakka K, et al. Effect of long term consumption of probiotic milk on infections in children attending day care centres: double blind, randomised trial. BMJ. 2001;322:1327. doi: 10.1136/bmj.322.7298.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Skovbjerg S, et al. Spray bacteriotherapy decreases middle ear fluid in children with secretory otitis media. Arch Dis Child. 2009;94:92–8. doi: 10.1136/adc.2008.137414. [DOI] [PubMed] [Google Scholar]
- 32.Hamaluba M, et al. A Cross-Sectional Observational Study of Pneumococcal Carriage in Children, Their Parents, and Older Adults Following the Introduction of the 7-Valent Pneumococcal Conjugate Vaccine. Medicine (Baltimore). 2015;94:e335. doi: 10.1097/MD.0000000000000335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Knol MJ, et al. Invasive pneumococcal disease 3 years after introduction of 10-valent pneumococcal conjugate vaccine, the Netherlands. Emerg. Infect. Dis. 2015;21:2040–2044. doi: 10.3201/eid2111.140780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hammitt LL, et al. Population effect of 10-valent pneumococcal conjugate vaccine on nasopharyngeal carriage of Streptococcus pneumoniae and non-typeable Haemophilus influenzae in Kilifi, Kenya: Findings from cross-sectional carriage studies. Lancet Glob. Heal. 2014;2:e397–e405. doi: 10.1016/S2214-109X(14)70224-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Almeida ST, et al. Low prevalence of pneumococcal carriage and high serotype and genotype diversity among adults over 60 years of age living in Portugal. PLoS One. 2014;9:1–10. doi: 10.1371/journal.pone.0090974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Le Polain de Waroux, O., Flasche, S., Prieto-Merino, D. & Edmunds, W. J. Age-dependent prevalence of nasopharyngeal carriage of Streptococcus pneumoniae before conjugate vaccine introduction: A prediction model based on a meta-analysis. Plos One9 (2014). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.