To the editor,
Cervical cancer most commonly affects young women, and between 2012 and 2014, it was estimated that approximately one in 368 women younger than 50 years of age will be diagnosed with invasive cervical cancer in the United States [1]. In this population of young women, future fertility is often desired, and thus preservation of reproductive function can be a key treatment concern [1]. Fertility-sparing surgery with trachelectomy is the treatment of choice in these women, however, trachelectomy has generally been only offered to women with at most stage IB1 cervical cancer with a tumor size less than or equal to 2 cm per the current guideline recommendations [2]. To date, population-based statistics regarding utilization of trachelectomy in women with stage IB1 cervical cancer with tumors larger than 2 cm are lacking. This study examined trends and characteristics of reproductive-aged women who underwent trachelectomy for stage IB1 cervical cancer with tumors larger than 2 cm.
A retrospective study examining the Surveillance, Epidemiology, and End Results (SEER) program between 1998 and 2014 was conducted. This database is a population-based tumor registry that is supported and managed by the National Cancer Institute in the United States. It is both publicly available and de-identified, thus this study was deemed exempt by the University of Southern California Institutional Review Board. Women less than 45 years of age with stage IB1 cervical cancer and tumor size 2.1–4.0 cm were included. Cases prior to 1998 were excluded due to lack of detailed information regarding the surgical procedure. Histology types examined in this study were squamous cell carcinoma, adenocarcinoma, and adenosquamous carcinoma, as these 3 types are generally recommended for trachelectomy per the current guidelines in the United States [2]. Other rare histology types were excluded from the study.
Information extracted from the database included patient demographics (age, race/ethnicity, marital status, registry area, and calendar year at diagnosis), tumor information (histology type and tumor differentiation grade), treatment types (surgery type for trachelectomy or radical hysterectomy, use of pelvic lymphadenectomy, adjuvant radiotherapy, and adjuvant chemotherapy), and survival outcome (cause-specific survival). Clinico-pathological characteristics and oncologic outcomes were compared between women who underwent trachelectomy and those who had hysterectomy.
The primary interest of this analysis was to examine trends in utilization of trachelectomy in young women with stage IB1 cervical cancer and tumors larger than 2.0 cm in size. The secondary interest of this analysis was to identify factors contributing to trachelectomy use as well as impact on cervical cancer mortality compared to hysterectomy.
The Joinpoint Regression Program (version 4.6.0.0) provided by the National Cancer Institute (Bethesda, MD, USA) was utilized to evaluate temporal trends, which were analyzed by linear segmented regression. Log-transformation was then performed to determine the annual percent change of the slope with 95% confidence intervals (CIs) as previously described [3,4,5]. Multivariable analysis with a binary logistic regression model (conditional backward method) was used to determine the independent contributing factors for trachelectomy use. In this model, all covariates with a p-value of less than 0.05 on univariable analysis were entered into the initial model, and the least significant covariate was removed from the model sequentially until the final model retained only covariates with p-values of less than 0.05. The Hosmer-Lemeshow test was then utilized to assess the goodness-of-fit in the final model, and a p-value of greater than 0.05 was considered a good-fit model.
For survival analysis, the Kaplan-Meier method was used to construct survival curves for cause-specific survival, and the log-rank test was used to assess statistical significance between the curves. Cause-specific survival was defined as the time interval between cervical cancer diagnosis and death from cervical cancer. Cases deemed to be alive at the last follow-up were censored. A p-value of less than 0.05 was considered statistically significant (all, 2-tailed hypothesis). Statistical Package for Social Sciences (version 25.0; IBM SPSS, Armonk, NY, USA) was used for statistical analysis.
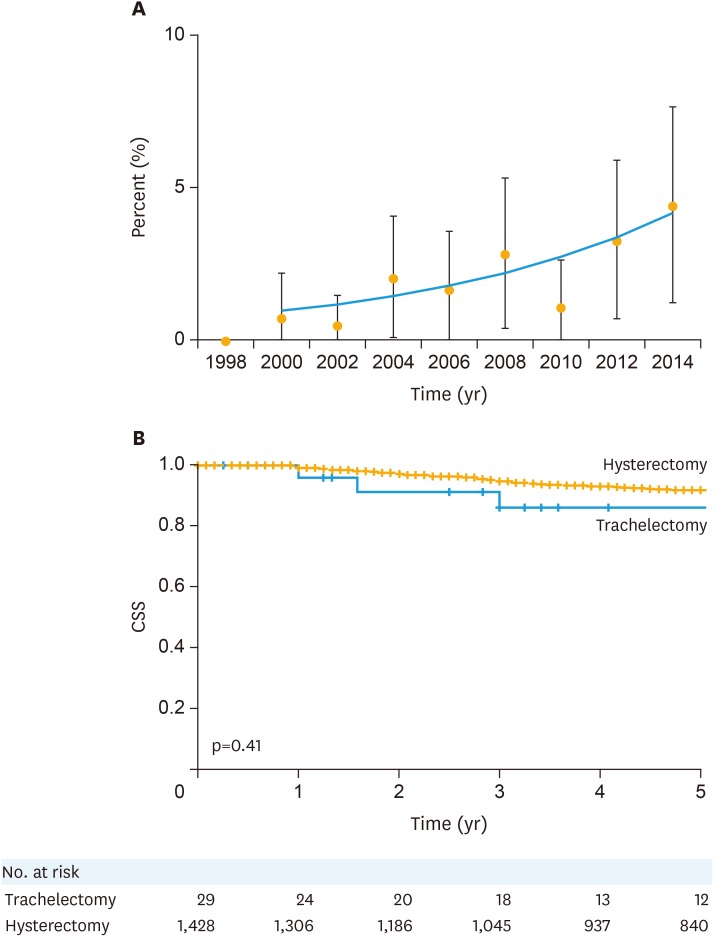
There were 1,457 women younger than 45 years of age who met the inclusion criteria, with stage IB1 cervical cancer and tumor size greater than 2.0 cm. Among those eligible cases, 29 (2.0%, 95% CI=1.3–2.7) women underwent trachelectomy. Patient demographics are shown in Table 1. Women who underwent trachelectomy were significantly younger than those who had hysterectomy (median, 31 vs. 37, p<0.001). The proportion of women who underwent trachelectomy significantly increased during the study period (0.5% in 1998–2002, 2.2% in 2003–2008, and 2.9% in 2009–2014, p=0.04). The annual percent change between 2000 and 2014 was 11.2, 95% CI=2.5–20.7 (p=0.019, Fig. 1A). Other clinico-pathological factors were similar between the 2 groups (all, p>0.05). On multivariable analysis (Table 1), younger age and more recent year of diagnosis were independent factors associated with performance of trachelectomy (both, adjusted-p<0.05).
Table 1. Contributing factors for trachelectomy use for large stage IB1 cervical cancer.
| Characteristic | Trachelectomy | Hysterectomy | p-value* | Adjusted-OR (95% CI) † | Adjusted-p-value | |
|---|---|---|---|---|---|---|
| No. | 29 (2.0) | 1,428 (97.9) | ||||
| Age (yr) | 31 (28–35) | 37 (33–41) | <0.001 | |||
| ≥40 | 1 (0.2) | 489 (99.8) | 1 | |||
| <40 | 28 (2.9) | 939 (97.1) | 14.90 (2.02–109.80) | 0.008 | ||
| Race/ethnicity | 0.42 | |||||
| White | 18 (2.3) | 748 (97.7) | ||||
| Black | 3 (2.1) | 139 (97.9) | ||||
| Hispanic | 4 (1.0) | 393 (99.0) | ||||
| Others | 4 (2.6) | 148 (97.4) | ||||
| Marital status | 0.90 | |||||
| Single | 10 (2.2) | 448 (97.8) | ||||
| Married | 14 (1.8) | 751 (98.2) | ||||
| Others | 5 (2.0) | 229 (97.9) | ||||
| Registry area | 0.61 | |||||
| West | 19 (2.1) | 868 (97.9) | ||||
| Central | 6 (2.3) | 255 (97.7) | ||||
| East | 4 (1.3) | 305 (98.7) | ||||
| Year at diagnosis | 0.04 | <0.05 | ||||
| 1998–2002 | 2 (0.5) | 386 (99.5) | 1 | |||
| 2003–2008 | 12 (2.2) | 535 (97.8) | 4.45 (0.99–20.10) | 0.052 | ||
| 2009–2014 | 15 (2.9) | 507 (97.1) | 5.90 (1.34–26.00) | 0.019 | ||
| Histology | 0.53 | |||||
| Squamous | 18 (2.1) | 824 (97.9) | ||||
| Adenocarcinoma | 10 (2.1) | 466 (97.9) | ||||
| Adenosquamous | 1 (0.7) | 138 (99.3) | ||||
| Grade | 0.28 | |||||
| 1 | 4 (2.3) | 173 (97.7) | ||||
| 2 | 9 (1.5) | 587 (98.5) | ||||
| 3 | 12 (2.0) | 585 (98.0) | ||||
| Unknown | 4 (4.6) | 83 (95.4) | ||||
| Pelvic lymphadenectomy | 0.35 | |||||
| No | 0 | 95 (100) | ||||
| Yes | 29 (2.1) | 1,332 (97.9) | ||||
| Adjuvant radiotherapy | 0.02 | |||||
| None | 25 (2.7) | 916 (97.3) | ||||
| Performed | 4 (0.8) | 512 (99.2) | ||||
| Adjuvant chemotherapy | 0.82 | |||||
| None/unknown | 24 (2.1) | 1,121 (97.9) | ||||
| Performed | 5 (1.6) | 307 (98.4) | ||||
Values are presented as number (%).
CI, confidence interval; OR, odds ratio.
*Univariable analysis; †A binary logistic regression model (conditional backward) for adjusted values. All covariates with p<0.05 on univariable analysis was entered in the initial model, and the least significant covariate was removed until the final model retains only covariates with p<0.05. Hosmer-Lemeshow test shows p=0.92 indicated a goodness-of-fit in the final model.
Fig. 1. Trends and outcomes related to trachelectomy for large stage IB1 cervical cancer. (A) Trends of trachelectomy use per calendar year. Calendar year was grouped every 2 years. (B) CSS from cervical cancer. X-axis was truncated to 5 years.
CSS, cause-specific survival.
The median follow-up of the entire cohort was 6.3 years (inter-quartile range=2.8–10.9), and there were 120 (8.2%) cervical cancer deaths. Although it did not reach statistical significance, women who underwent trachelectomy had a higher 5-year cervical cancer-specific mortality rate than those who had hysterectomy (14.4% vs. 8.4%, unadjusted-hazard ratio=1.61; 95% CI=0.51–5.06; p=0.41; Fig. 1B).
Although performance of trachelectomy remained uncommon, our study showed a gradual increase in the utilization of trachelectomy for reproductive-aged women with stage IB1 cervical cancer with tumors larger than 2 cm in the United States. Our results partly support the recent study using the National Cancer Database that demonstrated a significant increase in the utilization of fertility-sparing trachelectomy for women aged younger than 30 years with early-stage cervical cancer in the United States [6]. However, population-based statistics specific to stage IB1 cervical cancer with tumor size larger than 2 cm have not been examined previously. Thus, our results certainly imply that both surgeons and patients are seeking out opportunities for fertility preservation beyond the current guideline recommendations, which reserve trachelectomy in stage IB1 disease for tumors less than 2 cm. A recent retrospective study, however, reported that nearly one third of women with tumors 2–4 cm may be candidates for trachelectomy, emphasizing that expansion of the indication criteria for trachelectomy would allow these women the option of future fertility [7].
Yet, the safety of trachelectomy for tumors of the cervix larger than 2 cm remains undetermined. While recent population-based studies show that survival outcomes are comparable between less invasive surgery including trachelectomy and definitive hysterectomy for early-stage cervical cancer, these studies did not specifically examine trachelectomy for stage IB1 disease with tumor size larger than 2 cm [6,8]. In this specific subset of patients with tumors larger than 2 cm, our study and a prior pooled analysis reported a 6%–17% recurrence risk and a 1%–4% death rate. Given that current studies are limited by both sample size and follow-up, further studies are needed before trachelectomy can be considered a safe treatment option for women with tumors larger than 2 cm in diameter [7,9].
A limitation of our study is that this is a retrospective population-based study, and there may be possible confounding factors that could have impacted results. For instance, route of surgical approach for both trachelectomy and hysterectomy was not available in this database. A recent phase III randomized controlled trial found that minimally invasive hysterectomy was significantly associated with increased risk of recurrence and cancer mortality compared to abdominal approach [10]. Moreover, other surgical-pathological factors that certainly impact clinical and treatment decision-making such as lympho-vascular space invasion, depth of cervical stromal invasion, details of nodal status, and information regarding parametrial invasion are missing in the SEER database, and thus detailed risk-adjustment was not applicable in this study. Surgeon quality and surgical volume per institution were also not available in the SEER database, both of which may impact patient prognosis. Finally, details of chemotherapy including use of neoadjuvant chemotherapy were not retrievable in the SEER database.
In summary, there has been a significant increase in the use of fertility-sparing surgery with trachelectomy in young women with stage IB1 cervical cancer with tumors larger than 2 cm in recent years in the United States. While this trend may be encouraging for reproductive-aged women with cervical cancer who desire future fertility, oncologic safety remains undetermined in this subset of women with tumors >2 cm. At this time, when trachelectomy is considered in women with stage IB1 cervical cancer with tumors >2 cm, careful counseling and individualized treatment discussions with patients are imperative given the unknown safety of fertility-sparing treatment in this population.
Footnotes
Funding: This work was supported by Ensign Endowment for Gynecologic Cancer Research (M.K.).
Conflict of Interest: J.D.W. is consultant for Tesaro and Clovis Oncology and E.T. has personal fee from Chugai and Astra Zeneca.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 2.National Comprehensive Cancer Network (US) NCCN Clinical Practice Guideline in Oncology. Cervical cancer [Internet] Fort Washington, PA: National Comprehensive Cancer Network; 2017. [cited 2018 May 8]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf. [Google Scholar]
- 3.Machida H, Blake EA, Eckhardt SE, Takiuchi T, Grubbs BH, Mikami M, et al. Trends in single women with malignancy of the uterine cervix in United States. J Gynecol Oncol. 2018;29:e24. doi: 10.3802/jgo.2018.29.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matsuo K, Machida H, Grubbs BH, Sood AK, Gershenson DM. Trends of low-grade serous ovarian carcinoma in the United States. J Gynecol Oncol. 2018;29:e15. doi: 10.3802/jgo.2018.29.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matsuo K, Ross MS, Machida H, Blake EA, Roman LD. Trends of uterine carcinosarcoma in the United States. J Gynecol Oncol. 2018;29:e22. doi: 10.3802/jgo.2018.29.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cui RR, Chen L, Tergas AI, Hou JY, St Clair CM, Neugut AI, et al. Trends in use and survival associated with fertility-sparing trachelectomy for young women with early-stage cervical cancer. Obstet Gynecol. 2018;131:1085–1094. doi: 10.1097/AOG.0000000000002613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wethington SL, Sonoda Y, Park KJ, Alektiar KM, Tew WP, Chi DS, et al. Expanding the indications for radical trachelectomy: a report on 29 patients with stage IB1 tumors measuring 2 to 4 centimeters. Int J Gynecol Cancer. 2013;23:1092–1098. doi: 10.1097/IGC.0b013e318296034e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tseng JH, Aloisi A, Sonoda Y, Gardner GJ, Zivanovic O, Abu-Rustum NR, et al. Less versus more radical surgery in stage IB1 cervical cancer: a population-based study of long-term survival. Gynecol Oncol. 2018;150:44–49. doi: 10.1016/j.ygyno.2018.04.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pareja R, Rendón GJ, Vasquez M, Echeverri L, Sanz-Lomana CM, Ramirez PT. Immediate radical trachelectomy versus neoadjuvant chemotherapy followed by conservative surgery for patients with stage IB1 cervical cancer with tumors 2cm or larger: a literature review and analysis of oncological and obstetrical outcomes. Gynecol Oncol. 2015;137:574–580. doi: 10.1016/j.ygyno.2015.03.051. [DOI] [PubMed] [Google Scholar]
- 10.Ramirez RT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, et al. Phase III randomized trial of laparoscopic or robotic versus abdominal radical hysterectomy in patients with early-stage cervical cancer: LACC Trial; Proceedings of the 49th Annual Meeting of the Society of Gynecologic Oncologists; 2018 Mar 24??7; New Orleans, LA. Chicago, IL: Society of Gynecologic Oncology; 2018. [Google Scholar]