Abstract
Background:
Carcinoma cervix is one of the two most common cancers of Indian women with very high morbidity and mortality burden. Although India probably is the leading country in numbers patients of cervix treated radically with combination of teletherapy and brachytherapy (BT), there is presumed diversity of practice across the country due to the inequality of available infrastructure, absence of uniform the training of the radiation oncologists, and absence of any national guidelines. The present survey was conducted to determine current practice patterns in management of locally advanced carcinoma cervix with regard to gynecologic high-dose-rate among the radiation oncologist across the country.
Methodology:
A 25-item survey was undertaken to study the standard management pattern of Stage IIB–IIIB cervical cancer with special emphasis on the BT practice patterns among various young radiation oncologist working across the country. The survey was undertaken in person in the form of interview questionnaire among the younger members of association of radiation oncologist of India during two national conferences, along with telephonic interview of other members as obtained from the national directory.
Results:
About 57 young radiation oncologists from 57 centers across the country were surveyed. 25 of them represented private nonacademic centers, 24 represented government academic centers, the rest were from private academic, nongovernmental organization (NGO) run and other centers. The most common teletherapy dose prescribed was 46 Gy/23# for Stage II, and50 Gy/25 # for Stage III disease. HDR after loader with 192Ir is the most common machine (82.6%) in use and computed tomography scan is the most commonly (30/57) used imaging for planning. The most common intracavitary dose pattern for all stages was 7 Gy × 3 fractions (30/57s) and 9 Gy × 2 (12/57) fractions. Although in most centers, computed tomography-based delineation of organs at risk is done routinely; however, target volume delineation and dose prescription/optimization for the same is routinely done in handful of centers (5/57). The mean planned dose to Point A for combined external-beam radiation and BT (EQD210) was about 77.5 Gy for Stage IIIB and 72.6 Gy for Stage II disease.
Conclusion:
Although fractionation patterns may vary, the overall mean dose administered for cervical cancer is similar across the country, which is slightly lower than the recommended doses as per stage by various international guidelines.
Keywords: Brachytherapy, carcinoma cervix, India, practice pattern
Introduction
Carcinoma of the uterine cervix is one of the most common cancers in developing countries like India. More than 80% patients present in a fairly advanced stage.[1] According to the GLOBOCAN statistics, the estimated incidence of cervical cancer in the world is 528,000 per year with 266,000 annual deaths attributed to cervical cancer (approximately 50%).[2] India alone contributes to 23% of the total global cases annually. With an annual 67000 deaths, cervical cancer remains one of the major causes of cancer-related mortality in India.[3] For locally advanced cervical cancer (stage IB2-IVA), external-beam radiation (EBRT) with concurrent chemotherapy followed by brachytherapy (BT) is the current standard of treatment. BT is an irreplaceable component in the curative management of carcinoma of the cervix, and its exclusion/replacement compromises survival.[4,5] BT for carcinoma cervix has undergone major evolution over the times from the early 20th century till the first decade of 21st century. This evolution encompassed from dosing and dose prescription methods, use of imaging and computers, to design and materials of applicators, etc. Moreover, there have been various international guidelines available over time for gynecological BT keeping pace with the above developments; namely ICRU 38 in 1985, American BT Society (ABS) recommendations in 2000 and 2002, the GEC ESTRO recommendation in 2006 and 2008, and finally, the latest ICRU 89 in 2017. Thus, there could be an expected heterogeneity in the system of BT for carcinoma cervix employed at various institutions of the country.
Thus, the present survey was undertaken to study the pattern of existing practice of radiotherapy for locally advanced cancer cervix with special emphasis on BT among young radiation oncologists of the country.
Methodology
A 25-point survey was undertaken to study the standard management pattern of Stage IIB–IIIB cervical cancer with special emphasis on the BT practice patterns among various young radiation oncologist (<10 years of practice) working across the country. The survey was undertaken in three phases between January 2014 and April 2015. The survey was undertaken among participants attending in two subsequent Young radiation oncologists of India conferences in 2014 and 2015. The first phase was in the form of personal interview with a checklist among the younger members of the Association of Radiation Oncologist of India (AROI) during the two national conferences. In the second phase, the questionnaire was mailed to the individual oncologists with a follow-up telephonic interview in the third phase, as obtained from the national directory. The 25-point questionnaire or the interview checklist consisted of two parts, Part A being about general information and Part B about specific information regarding workload, infrastructure, and specific practice pattern (attached in supplements). The questionnaire was pretested in a small sample and necessary corrections were made. The young radiation oncologists were asked about the most common prevailing practice in their institute about a particular issue or technique. The details of the existing infrastructure were also noted. An internal check with the facilities available and practice pattern was carried out for each center for coherence. Centers who did not have any BT facility were excluded from the analyses (9 responders). In cases of multiple respondents from a single institution, the common responses were noted. In cases where a number of different practices were found in the same institution, the most common one was noted. In case of discrepancies, a telephonic interview was conducted. The planned dose for total treatment of advanced carcinoma cervix was estimated by EQD2 model. Dose per fraction from BT, when combined with EBRT, was normalized to 2 Gy/weighted dose in equivalent 2 Gy fractions with an α/β= 10.
Formula is Nd (1 + d)/α/β ÷1.2 (N = No of fraction, d = dose per fraction, α/β = 10).
Results
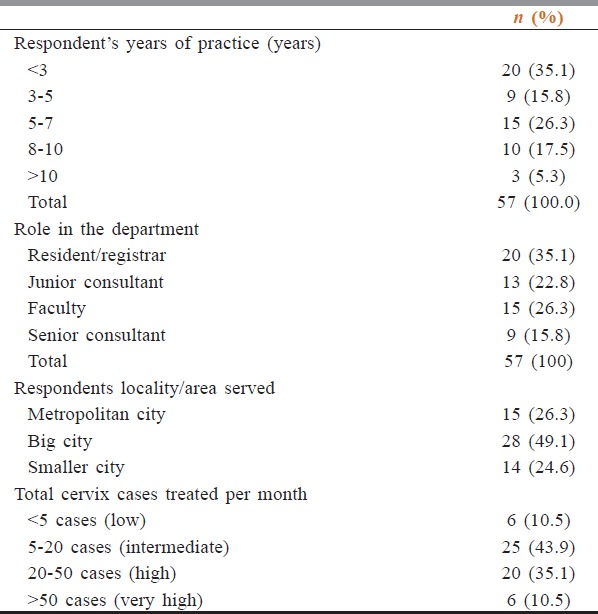
Respondent characteristics
A total of 156 young radiation oncologists were contacted for the survey. About 57 young radiation oncologists from 57 centers across the country responded in any of the three phases (response rate 36.3%). More than 90% were within 10 years of completion of their qualifying exam (MD or DNB). Three RO with experience of more than 10 years were excluded, all of them were accompanying their juniors, and hence, there was no loss of data [Table 1]. Majority of them were residents or junior consultants or faculty and most of them were treating 5–50 cases of cervical carcinoma per month. Nineteen of them represented private nonacademic centers, 28 represented government academic centers, the rest were from private academic, NGO run and other centers.
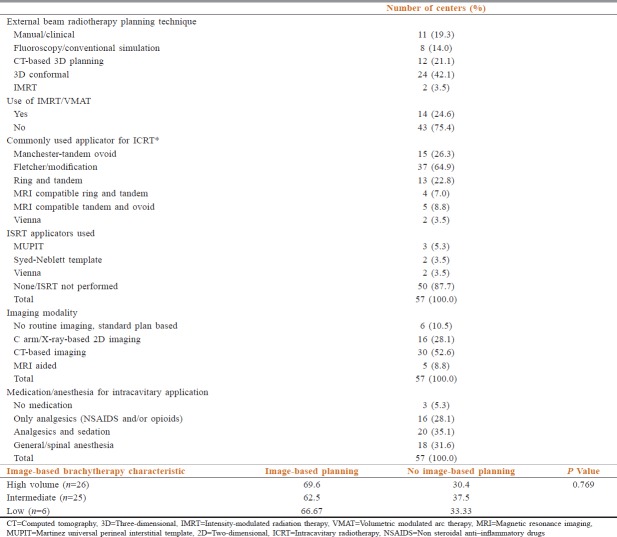
Table 1.
Characteristics of respondents as per experience, area served, and analgesia or anesthesia used
External-beam radiation to the cervix
Physicians were queried regarding the standard EBRT dose prescribed for treating carcinoma cervix patients. Regarding EBRT doses for Stage II, the most common EBRT doses are 46 Gy/23 fractions are prescribed in 24 centers (42.1%), and 50 Gy in 25# is prescribed in 23 centers (40.4%). For Stage III, most common fractionation regimen 50 Gy in 25# is prescribed in 39 centers (68.4%), and 46 Gy in 23# is prescribed in 14 centers (24.6%).
Regarding planning technique three-dimensional (3D) conformal planning is used most commonly in 24 centers (42.1%) for cervical carcinoma. Computed tomography (CT)-based 3D planning (two field/four field box without MLC) is used in 12 centers (21.1%). Conventional simulation-based planning for advanced cervical cancers is practiced in 8 centers (14.0%). IMRT (with or without SIB) used in 14 centers (24.6%). Contouring and planning are initially done by residents in 32 (56.1%) and by junior consultants in 14 (24.6%) and by senior consultants/Faculty in 10 (17.5%). About 75% respondents stated that concurrent chemotherapy with EBRT is prescribed in their institution usually for all eligible cases whereas about 25% said they do so only in selected cases.
Brachytherapy
With regard to dose rate, 51 respondents (about 90%) have high-dose-rate (HDR) available and 5 reportedly had (12.1%) low dose-rate (LDR) facility at the time of the interview. Iridium192 is the most commonly used isotope in 48 centers (82.8%) and cesium137 used in 5 centers (12.1%) and Co60 used in 3 centers (5.2%) [Table 2]. Respondents were possessing cesium during the survey in 2014, of which recent trail reveals it has been dismantled from two centers.
Table 2.
External beam radiotherapy and brachytherapy characteristics
There was some variability in the type of applicator used for intracavitary applications with the tandem and ovoid applicator being the preferred one in 15 centers followed by Ring and Tandem The Fletcher suit applicator or its modification is the most frequently used applicator for HDR intracavitary (ICRT); it is used in 37 centers (64.9%). Among them, MR compatible tandem ovoid is used in 5 centers (8.8%) and MR compatible ring and tandem are in use at four centers (7%). Interstitial application is done using MUPIT (Martinez Universal Perineal Interstitial Template) in 3 centers (5.3%) Syed-Neblet applicator in 2 (3.5%) and Vienna applicators in 2 (3.5%) two centers [Table 2]. Advance applications or combination of ICRT-ISRT was done in only five centers. For application insertion, 67.7% of respondents patients received some sort of anesthesia/sedation, consisting of general/spinal anesthesia (31.6%), and intravenous (IV) sedation (injectable opioids/benzodiazepines/combination) (35.1%) while 28.1% received analgesics (nonsteroidal anti-inflammatory drugs/tramadol) only.
Regarding to imaging the BT applicator after insertion, 90% radiation oncologists said that they use imaging for planning. 16 centers (28.1%) reported that they used X-ray-based two-dimensional (2D) planning, 30 centers (52.6%) reported that they used CT based imaging while magnetic resonance imaging (MRI) is routinely used (for contouring or planning or both) only in 5 centers (8.8%). Two centers responded that they use both CT and X-ray based imaging. Majority of the centers (44 out of 57) use some form imaging (2D/3D) for first the first fraction only while only in seven centers imaging (2D or 3D) is done for all fractions routinely.
Those centers who are using orthogonal X-ray-based planning, prescriptions are made at point A and dose reported for bladder and rectal points. In centers using volumetric imaging, 80% contour organs at risks (OARs) (rectum and bladder) in axial slices and report doses to at least one of the volumes (2cc most commonly 21 out of 24). Sigmoid is routinely contoured in only few centers (7 out of 30) by the young radiation oncologists. Gross tumor volume (GTV), high-risk clinical target volume (HRCTV), and intermediate clinical target volume are drawn in five centers routinely with prescriptions are made to point A in most of them, with reporting of HRCTV and GTV doses. A planning aim of 80% to bladder (point/2cc) and 75% to rectum (rectal point or 2cc) of the prescribed dose is followed in the majority of centers (38 of 57) as per the respondents. Various institutes follow different recommendeations for planning, prescribing and reporting dose constraints, 14 out of 57 folowthe GEC ESTRO recommendations, 12 follow the ABS guidelines while the rest follow the ICRU 38 recommendations. The pattern of routine use of 3D imaging for brachytherapy planning did not significantly differ among government and private centers, nor did it correlate with the volume of cervical cancer patients treated at the particular center or institute.
A large heterogeneity was observed regarding the fractionation schedule adopted at various centers and by different young radiation oncologists. The most common fractionation regimen 7 Gy × 3# is prescribed by 30 centers (52.6%). Second most common regimen 9 Gy × 2# is used in 7 centers (12.3%). Scheduling of BT was done mainly after completion of EBRT, with about 86% of centers starting ICRT within 2 weeks of completion of EBRT. Only two centers were practicing interdigitation of BT fractions with external beam radiotherapy routinely as an institutional protocol. The mean planned combined EQD210 was about 78.78 Gy for Stage IIIB and 71.1 Gy for Stage IIB disease [Figures 1 and 2]. Mean planned combined EQD210 was slightly higher in patients treated in private organizations than in government institution in both carcinoma cervix Stage II and Stage III.
Figure 1.
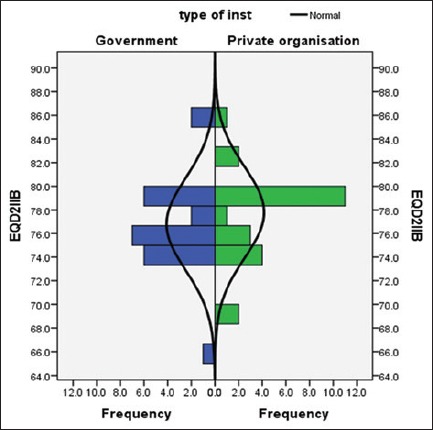
Comparison of the Planned EQD210Gy for carcinoma cervix Stage IIB among Government owned and Private Institutions
Figure 2.
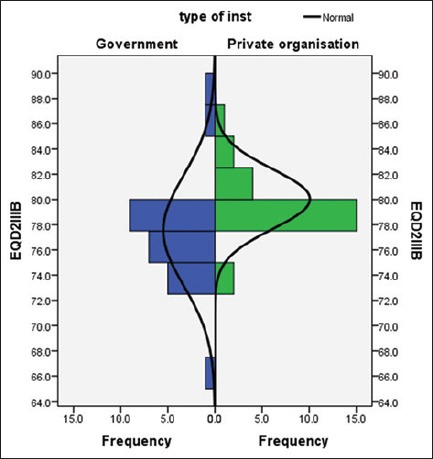
Comparison of the Planned EQD210Gy for carcinoma cervix Stage IIIB among government-owned and private Institutions
Discussion
Globally, cervical cancer represents the most common gynecologic malignancy in women.[6] As most of the cases present at advanced stages, such as Stage III and Stage IV, in which surgery is not possible, radiotherapy plays an important role in these patients.[7,8,9,10] Radiation has been used successfully to treat cervical cancer for nearly a century. The effective combination of external beam irradiation and concurrent chemotherapy followed by BT has been shown to be an effective treatment for cervical cancer patients since the Teletherapy aims to sterilize and control the pelvic disease and the BT aim to eradicate the central disease. The present survey was undertaken to study the pattern care delivered by young radiation oncologist across the country to treat this disease with radiotherapy; the diversity of techniques used, methodology of planning the prescribed doses, and the guidelines followed. Although practice pattern or pattern of care surveys are undertaken and reported from other countries, this is probably the second study after the study by Gandhi et al. assessing practice and attitude of BT use.
The respondents of our study were mostly young radiation oncologists which suggest they have completed their training in recent years and probably are well versed with international recommendations. That a majority of them belonged to academic centers also negates the biases of treatment protocol due to financial implications. This is important since per pocket payment may lead to treatment curtailment or modifications for cost concerns.
In our study, among 57 oncologists, 24 of them (42.1%) used EBRT at the dose of 46.0 Gy in 23# and 23 (i.e., 40.4%) used 50.0 Gy in 25# in carcinoma cervix Stage II and 39 oncologists (i.e., 68.4%) used EBRT 50 Gy in 25# in carcinoma cervix Stage III. 30 among all the oncologists (52%) used BT at the dose of 3 × 7 Gy started within 1–2 weeks of completion of EBRT. The mean combined EQD210 was about 78.78 Gy for Stage IIIB and 71.1 Gy for Stage IIB disease.
The ABS recommends multiple HDR insertions to allow progressive tumor volume reduction, allowing more effective disease coverage with subsequent applications. Four to eight fractions of HDR-ICRT, with the dose ranging from 5.3 to 7.5 Gy per fraction and the total dose by EBRT from 20 to 50.4 Gy for early and late stages of the diseases.[8]
In the United States, the most commonly used regimens are 45 Gy EBRT to the pelvis (possibly with a sidewall boost) with concurrent cisplatin-based chemotherapy and HDR BT either 5.5 Gy per fraction for 5 fractions (for patients treated with concurrent chemotherapy who have had either a complete response or have <4 cm of residual disease) or 6 Gy for 5 fractions (for patients with tumors >4 cm after EBRT). Over the past decade, the most common HDR fraction size used in the United States for all stages of cervix cancer has been 6 Gy for five fractions, but concerns have been raised about potential toxicity to the sigmoid colon and rectum in patients treated with chemoradiation.[11] As a result, recent clinical trials have included a range of lower fractional doses, such as 5.5 Gy for five fractions. Contrary to the above practice, in India, majority of the centers use three or less fractions with individual fraction size more than 6 Gy.
Although fractionation patterns may vary, the overall mean planned dose (EQD210 Gy) administered for cervical cancer is quite similar across the country (76.89 Gy for IIB And 78.55 Gy for IIIB) which is slightly lower than the recommended doses as per stage by various international guidelines. However, similar planned dose rates were also reported from a survey in UK also.[12]
This study yields information on human and material resources available for BT from India for the first time. The information presented provides valuable insight into the current state of BT practice in this region. While CT is the most frequently used method for BT imaging, 2D X ray- based is still in vogue which the standard imaging used before the 1990s in the developed nations. In an ABS survey, 70% of respondents used CT after BT applicator insertion and as compared to 52.6% in this survey.[23] Since the integration of CT into radiation oncology departments is integral to 3D imaging for external beam, use of CT for BT has also increased; which has been reflected in this study. In our survey, 8.8% reported that they used MRI-based planning and 15% have MRI compatible applicators, indicating many are planning tpo start MRI based Bt in near future. In spite of costs and the use of MRI in cervical BT in 2014–2015 is an encouraging sign and points to the adaptation of better volume-based concepts in the future years. Also that more than 50% of centers are using CT-based planning is also encouraging.
In this survey, HDR available in 87.9% and LDR/pulsed dose rate/medium dose rate in 12.1% institutions. Due to technological and imaging advances, the HDR BT are increasingly become popular and the usage of LDR BT seems to be limited. In the high-volume centers of India, the use of LDR is decreasing fast because of the resource and workforce constraints. The fact that studies from the country have shown the equivalence of HDR to LDR BT regarding survival outcomes may have also contributed to this fact.[13] Advantages of HDR BT include opportunities for outpatient treatment, avoidance of exposure to staff from the radiation source, consistent and reproducible applicator positioning, and dose optimization attained with a variable dwell-time stepping source.[14,15,16,17,18,19,20] The use of HDR-BT in India is on a steep raise.[21]
A recent Quality Research in Radiation Oncology (QRRO, formerly Patterns of Care) survey from 2007 to 2009 the most common fractionation used was 7 Gy in 3#.[22] The current study demonstrates that the planned EQD2 is practiced across the country is empirical, many times inadequate, not adaptive (depending on volume of disease at the time of BT) in most of the centers This may be due to lack of training of young radiation oncologists, infrastructural deficiencies or lack of proper imaging facilities. Hopefully, the current joint workshops by AROI and ESTRO being organized countrywide will spread the message of image-based and adaptive planning. The proper training along with the allocation of huge funds by the government for up gradation of cancer centers will help a long way.
In this survey for applicator insertion, patient received general or spinal anesthesia only in 31.6% and IV sedation only in 35.1%. Thus, need for more focus on patient comfort, pain care, and quality of application should be made. The application of ICRT application without proper sedation as practiced in many centers. On probing further into the matter, it was found unavailability of dedicated operation theatre and anesthesia facilities remains a constraint. The recent increase in training facilities by the government to produce more trained anesthetists might possibly solve the problem. Another finding of our survey was that after EBRT treated only few cases are being treated by transperineal ISRT (MUPIT only in 5.3% and Neblet in 3.5%). Thus, there is a possibility that majority centers in the country are undertreating a significant proportion of the advanced cervical cancers. Resource limitations both regarding infrastructure and human capital might be the barrier.
The mean planned EQD210 was higher in private centers as compared to academic/government and high volume centers suggesting probably a safer and standard fit for all protocol approach being practiced in such centers, due resource constraints. The fact that 57% of these centers practice image based BT as compared 74% of the private low-volume centers explains the above (P = 0.075).
Clearly, the most important limitation of this study is the response rate, which was negatively influenced by the limited participation of RT. As a result, it is merely impossible to make any conclusions about ideal BT practice pattern. Apart from the obvious biases associated with questionnaire/interview based cross-sectional study, another important drawback was that this study was not linked with any facility survey or outcome audit of the various centers. However, still, with its limitation, this study provides a useful insight into the BT practices of the country and helps to identify the opportunities for improvement. This would also help policymakers and national organizations for structuring trainings courses of young oncologist.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Shrivastava S, Mahantshetty U, Engineer R, Tongaonkar H, Kulkarni J, Dinshaw K, et al. Treatment and outcome in cancer cervix patients treated between 1979 and 1994: A single institutional experience. J Cancer Res Ther. 2013;9:672–9. doi: 10.4103/0973-1482.126480. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay JS, Evrik I, Forman M, Bray FD. Lyon, France: International Agency for Research on Cancer; 2012. Cancer Incidence and Mortality Worldwide 2013: IARC Cancer Base No. 11. [Google Scholar]
- 3.Nandakumar A, Ramnath T, Chaturvedi M. The magnitude of cancer cervix in India. Indian J Med Res. 2009;130:219–21. [PubMed] [Google Scholar]
- 4.Lanciano RM, Won M, Coia LR, Hanks GE. Pretreatment and treatment factors associated with improved outcome in squamous cell carcinoma of the uterine cervix: A final report of the 1973 and 1978 patterns of care studies. Int J Radiat Oncol Biol Phys. 1991;20:667–76. doi: 10.1016/0360-3016(91)90007-q. [DOI] [PubMed] [Google Scholar]
- 5.Montana GS, Hanlon AL, Brickner TJ, Owen JB, Hanks GE, Ling CC, et al. Carcinoma of the cervix: Patterns of care studies: Review of 1978, 1983, and 1988-1989 surveys. Int J Radiat Oncol Biol Phys. 1995;32:1481–6. doi: 10.1016/0360-3016(95)00177-Z. [DOI] [PubMed] [Google Scholar]
- 6.Saibishkumar EP, Patel FD, Sharma SC. Evaluation of late toxicities of patients with carcinoma of the cervix treated with radical radiotherapy: An audit from India. Clin Oncol (R Coll Radiol) 2006;18:30–7. doi: 10.1016/j.clon.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 7.Nag S, Erickson B, Thomadsen B, Orton C, Demanes JD, Petereit D, et al. The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2000;48:201–11. doi: 10.1016/s0360-3016(00)00497-1. [DOI] [PubMed] [Google Scholar]
- 8.Foroudi F, Bull CA, Gebski V. Radiation therapy for cervix carcinoma: Benefits of individualized dosimetry. Clin Oncol (R Coll Radiol) 2002;14:43–9. doi: 10.1053/clon.2001.0024. [DOI] [PubMed] [Google Scholar]
- 9.Sundar S, Symonds P, Deehan C. Tolerance of pelvic organs to radiation treatment for carcinoma of cervix. Clin Oncol (R Coll Radiol) 2003;15:240–7. doi: 10.1016/s0936-6555(02)00455-7. [DOI] [PubMed] [Google Scholar]
- 10.Forrest JL, Ackerman I, Barbera L, Barnes EA, Davidson M, Kiss A, et al. Patient outcome study of concurrent chemoradiation, external beam radiotherapy, and high-dose rate brachytherapy in locally advanced carcinoma of the cervix. Int J Gynecol Cancer. 2010;20:1074–8. doi: 10.1111/IGC.0b013e3181e6f321. [DOI] [PubMed] [Google Scholar]
- 11.Stewart AJ, Viswanathan AN. Current controversies in high-dose-rate versus low-dose-rate brachytherapy for cervical cancer. Cancer. 2006;107:908–15. doi: 10.1002/cncr.22054. [DOI] [PubMed] [Google Scholar]
- 12.Simmor T, Conibear J, Diez P, Miles E, McCormack M. 2nd ed. Geneva: Estro Forum; 2013. A Survey of UK Practice in Cervical Cancer Radiotherapy aimed at Developing Trial Specific Quality Assurance. PD-0266; p. S104. [Google Scholar]
- 13.Patel FD, Sharma SC, Negi PS, Ghoshal S, Gupta BD. Low dose rate vs. High dose rate brachytherapy in the treatment of carcinoma of the uterine cervix: A clinical trial. Int J Radiat Oncol Biol Phys. 1994;28:335–41. doi: 10.1016/0360-3016(94)90055-8. [DOI] [PubMed] [Google Scholar]
- 14.Fu KK, Phillips TL. High-dose-rate versus low-dose-rate intracavitary brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 1990;19:791–6. doi: 10.1016/0360-3016(90)90511-h. [DOI] [PubMed] [Google Scholar]
- 15.Hareyama M, Sakata K, Oouchi A, Nagakura H, Shido M, Someya M, et al. High-dose-rate versus low-dose-rate intracavitary therapy for carcinoma of the uterine cervix: A randomized trial. Cancer. 2002;94:117–24. doi: 10.1002/cncr.10207. [DOI] [PubMed] [Google Scholar]
- 16.Inoue T. The trail of the development of high-dose-rate brachytherapy for cervical cancer in Japan. Jpn J Clin Oncol. 2003;33:327–30. doi: 10.1093/jjco/hyg069. [DOI] [PubMed] [Google Scholar]
- 17.Teshima T, Inoue T, Ikeda H, Miyata Y, Nishiyama K, Inoue T, et al. High-dose rate and low-dose rate intracavitary therapy for carcinoma of the uterine cervix. Final results of Osaka University Hospital. Cancer. 1993;72:2409–14. doi: 10.1002/1097-0142(19931015)72:8<2409::aid-cncr2820720819>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 18.Wang X, Liu R, Ma B, Yang K, Tian J, Jiang L, et al. High dose rate versus low dose rate intracavity brachytherapy for locally advanced uterine cervix cancer. Cochrane Database Syst Rev. 2010;(7):CD007563. doi: 10.1002/14651858.CD007563.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Petereit DG, Sarkaria JN, Potter DM, Schink JC. High-dose-rate versus low-dose-rate brachytherapy in the treatment of cervical cancer: Analysis of tumor recurrence – The university of Wisconsin experience. Int J Radiat Oncol Biol Phys. 1999;45:1267–74. doi: 10.1016/s0360-3016(99)00262-x. [DOI] [PubMed] [Google Scholar]
- 20.Lertsanguansinchai P, Lertbutsayanukul C, Shotelersuk K, Khorprasert C, Rojpornpradit P, Chottetanaprasith T, et al. Phase III randomized trial comparing LDR and HDR brachytherapy in treatment of cervical carcinoma. Int J Radiat Oncol Biol Phys. 2004;59:1424–31. doi: 10.1016/j.ijrobp.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 21.Banerjee S, Mahantshetty U, Shrivastava S. Brachytherapy in India – A long road ahead. J Contemp Brachytherapy. 2014;6:331–5. doi: 10.5114/jcb.2014.45761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eifel P. Patterns of radiotherapy practice for patients treated for intact cervical cancer in 2005-2007: A QRRO study. Int J Radiat Biol Phys. 2010;78:S119. doi: 10.1016/j.ijrobp.2013.11.228. [DOI] [PubMed] [Google Scholar]
- 23.Viswanathan AN, Erickson BA. Three-dimensional imaging in gynecologic brachytherapy: A survey of the American Brachytherapy Society. Int J Radiat Oncol Biol Phys. 2010;76:104–9. doi: 10.1016/j.ijrobp.2009.01.043. [DOI] [PubMed] [Google Scholar]