Abstract
Background and Aims:
Bag mask ventilation (BMV) allows for oxygenation and ventilation of patients until a definitive airway is secured and when definitive airway is difficult/impossible. This study hypothesised that the EO (thumb and index finger form a O shape around the mask) technique of mask holding provides better mask seal with the novices compared to the classic EC clamp technique (thumb and index finger form a C shape around the mask).
Methods:
Sixty patients participated in this double blinded, prospective, crossover study. The patients were randomly allocated to either EC or EO group. After adequate anaesthesia and neuromuscular blockade, a novice (experience of less than five attempts at BMV) held the mask with preferred hand with the allotted technique, while the ventilator provided five breaths at set pressure control of 15 cm H2O with one second each for inspiration and expiration. After recording the exhaled tidal volume (primary objective) for each breath for five consecutive breaths, the study was repeated with the other technique. Secondary outcome variables were minute ventilation, audible mask and epigastric leak.
Results:
The tidal volume and minute ventilation were significantly better with EO technique compared with the EC technique (P = 0.001, a tidal volume difference of 46 mL and P = 0.001, a minute volume difference of 0.51 L).
Conclusion:
The EO technique provides better mask seal (superior tidal volumes) than the conventional EC technique during single-handed mask holding performed by novices in the absence of other factors contributing to difficulty in mask ventilation.
Key words: Bag mask ventilation, EC clamp technique, EO technique
INTRODUCTION
Bag mask ventilation (BMV) is one of the most essential skills to be mastered by all those providing airway care. Often, in emergency situations, the initial care givers might be less experienced in these techniques as anaesthesiologists may not be available at hand immediately. Therefore, each healthcare professional dealing with the airway care of patients requires to master the art of BMV. Conventionally, the EC clamp technique of mask holding is taught for BMV for beginners where one hand is used to hold the mask over the victim's face in such a way that the little finger provides jaw thrust while the ring and middle fingers rest softly on the rim of the mandible forming an E shape while the thumb and the index finger form C shape attempting to secure the mask tightly around the victim's mouth and nose. This technique is described classically as EC clamp technique of mask holding while the other hand is used to squeeze the bag (a self-inflating bag or a reservoir bag). There can be several factors contributing to inadequate BMV that can be classified as patient-related (such as beard, edentulous, thick neck, etc.), equipment-related (inappropriate size mask, non-cushioned rim of the masks, etc.), or operator-related factors (inexperience, improper technique). Overall, inadequate BMV is contributed by either leak around the mask or an unrelieved airway obstruction or a combination of both.[1,2] One of the reasons for failure to provide adequate BMV in the absence of predictors for difficult mask ventilation is inexperience of the operator.[3,4,5] The technique of BMV requires a reasonable degree of understanding of facial contour, mask design, and its effective application.[5] This requires sufficient experience as shown by difficulty in providing effective BMV by novices, emergency room technicians, operating room personnel other than anaesthesiologists, pre-hospital team personnel, and nurses who perform BMV occasionally.[4,5] Therefore, alternate techniques and devices such as cuffed oropharyngeal airway and ergonomically designed facemask are being developed to improve effectiveness of BMV by such personnel.[6] Leak around the mask is one of the contributors to ineffective mask ventilation.[1] If an experienced individual can demonstrate effective BMV on an airway devoid of any predictors of difficult BMV, then a novice too should be able to perform effective BMV. On the contrary, a study that evaluated effectiveness of BMV on a manikin using the conventional EC clamp technique found that novices failed to provide effective BMV, whereas experienced individuals succeeded.[4] This study highlighted the problem in the mask seal provided by novices. Authors of this study argued that when novices perform BMV using the conventional EC clamp technique of mask holding, adequate seal usually occurs along the point of contact of hand, whereas it fails to achieve airtight seal on the contralateral side of the mask contributing to significant leak. Hence, they suggested an alternate technique for mask holding, the EO technique where the web between the index finger and the thumb comes close to the neck of the mask, thus bringing the wrist and forearm to a semi-prone position from the conventional lateral position. The remaining three fingers help provide chin lift. The study comes to two important conclusions. EO technique of mask holding improved the effectiveness of BMV considerably from EC technique of mask holding with novices, whereas experienced individuals could provide effective BMV with either techniques of mask holding.[4] The main aim of this study was to evaluate the effectiveness of mask seal offered by the two different techniques of mask holding (EC and EO) when performed by novices during single person BMV in patients undergoing general anaesthesia.
METHODS
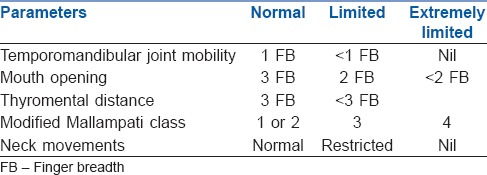
The study was double blind, randomised, prospective, and crossover in nature. After obtaining Institutional Ethical Committee approval, the study methodology was explained to patients scheduled for elective general anaesthesia. All patients aged between 18 and 85 years belonging to either gender that are adequately fasting were considered for the study. Written informed consent was obtained from those willing to participate in the study. Patient details such as age, gender, weight, height, and body mass index were noted. Airway examination was performed and the following airway parameters were noted (modified Mallampati class, thyromental distance, mouth opening, neck movements, temporomandibular joint mobility, presence of beard, edentulous patient, any obvious airway pathology that may contribute to difficult mask ventilation such as obstructive sleep apnoea or neck circumference >42 cm). Those patients with anticipated or known difficult airway [Table 1: any parameter falling under the limited or extremely limited column] and those not requiring general anaesthesia with non-depolarising neuromuscular blockade or at risk for regurgitation were excluded from the study. Premedication was administered to patients as per the discretion of the anaesthesia team in charge and standard nil per oral orders were given to all the patients.
Table 1.
Airway parameter assessment table of patient
All patients were assigned to one of the two groups first followed by the other group by a computer-generated randomisation table. EC technique: Conventional “EC” technique where the little, ring, and middle fingers form an “E” and rest on the mandible and provide chin lift, whereas the index finger and the thumb form a “C” around the mask to provide a tight fit of facemask over patient's face [Figure 1]. EO technique: The “EO” technique of mask holding had the index finger and thumb forming a near complete circle around the mask neck by bringing the web between these two fingers close to the mask neck, whereas the remaining three fingers were placed over the chin to provide chin lift. This technique requires the wrist and forearm to be in a semi-prone position [Figure 2].
Figure 1.
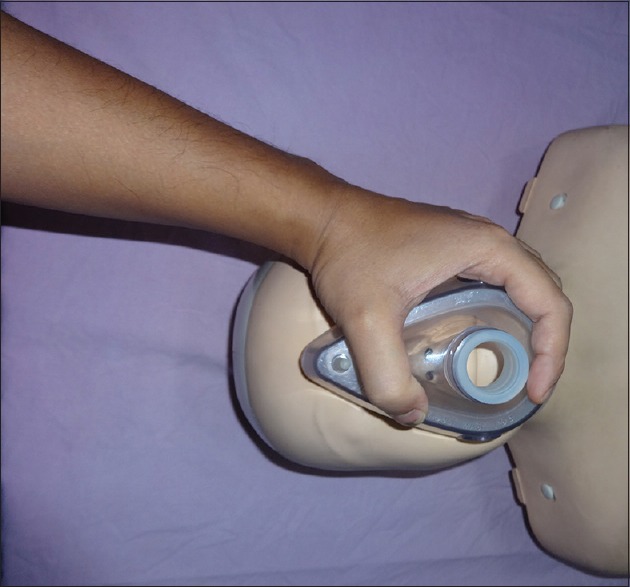
Conventional “EC” technique where the little, ring, and middle fingers form an “E” and rest on the mandible and provide chin lift while the index finger and the thumb form a “C” around the mask to provide a tight fit of facemask over patient's face
Figure 2.
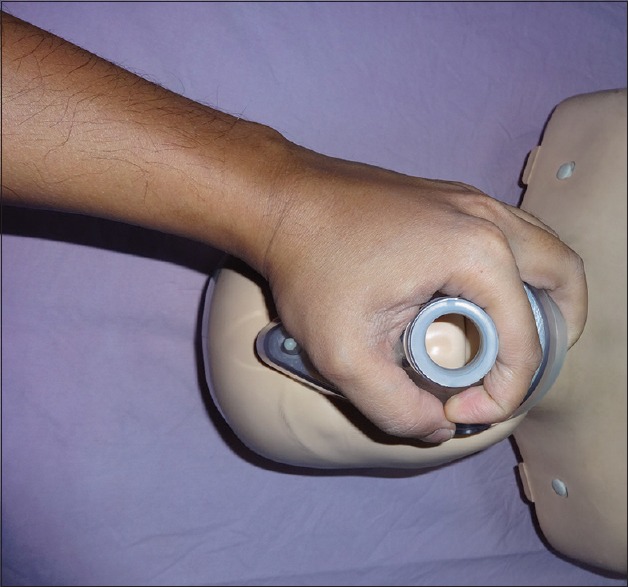
The “EO” technique of mask holding with the index finger and thumb forming a near complete circle around the mask neck by bringing the web between these two fingers close to the mask neck while the remaining three fingers are placed over the chin to provide chin lift
The person (observer 1) who evaluated the airway of patients preoperatively also recorded the study parameters that included tidal volume values from the ventilator screen and any audible leak during BMV. Another study investigator (observer 2) placed stethoscope over the patient's epigastrium to auscultate for any audible gurgling sounds. Both observers 1 and 2 were blinded to the randomisation sequence. One study investigator (observer 3) helped and ensured that the novice has placed the hand as per the randomisation sequence (EC or EO) for BMV. To ensure appropriate blinding, a non-transparent screen separated the head, neck, and upper chest of the patient from the rest of the body and the ventilator monitor panel was placed behind the novice volunteer. This ensured that the novice volunteer could observe the capnograph trace from the monitor and chest expansion but could not visualise the tidal volume recordings on the ventilator monitor panel. The non-transparent screen prevented the observer 2 from having the knowledge of the mask holding technique. Further, observer 1 was placed directly behind the observer 3 and the novice volunteer with back towards the novice such that observer 1 could see the ventilator panel and hear for audible leak but could not see the mask ventilation technique being employed.
Just prior to starting the study, the ventilator was set to pressure controlled ventilation mode with peak inspiratory pressure 15 cm H2O, inspiration to expiration ratio (I: E) 1:1, and 30 breaths per minute (bpm). It was ensured that the bellows (ascending bellows) were set to touch the top of the ventilator bottle.
Once the patients were shifted to the operating room, monitoring was established as per the standard practice that included electrocardiogram, pulse oximeter (SpO2), non-invasive blood pressure, waveform capnograph (ETCO2), and peripheral nerve stimulator. After securing an intravenous (IV) access, anaesthesia was induced with propofol 2–3 mg/kg IV and fentanyl 2 μg/kg IV. Neuromuscular blockade was achieved with vecuronium 0.1 mg/kg IV after an experienced anaesthesiologist ensured ability to provide BMV manually using a cushioned transparent masks (Flexicare Medical Limited, Cynon Velley Business Park, UK) of appropriate sizes. Manual BMV by experienced anaesthesiologist was continued with isoflurane 1.5%–2% in 6 L/min oxygen till the train-of-four ratio was zero. An appropriate size oropharyngeal airway was inserted into the airway of every patient and ability to effectively perform single handed BMV was confirmed by an experienced anaesthesiologist prior to asking the novice to attempt BMV. The study commenced at this point. A novice volunteer was assisted by observer 3 in holding the mask using either the EC or the EO technique as per the computer generated randomisation table. Once the volunteer was satisfied with hand position, the ventilator was turned on to provide breaths. A total of five breaths were to be given with each technique of mask holding at a fresh gas flow of 6 L/min oxygen. During the study, the volunteer was not allowed to change the hand position, however, was allowed to adjust the head tilt or chin lift observing for chest expansion and capnograph trace as guide. The study parameters obtained were recorded. Following completion of the study with one technique, observer 3 placed the hand of the novice volunteer as per the other technique of mask holding and the study was repeated. After noting the parameters, the patient's trachea was intubated with appropriate size tracheal tube by an experienced anaesthesiologist. Any difficulty in laryngoscopy or intubation were also noted.
Novice volunteers for the study included anaesthesia technician students and medical interns who had seen BMV being performed, however, had very limited experience in providing BMV (none or less than five attempts at BMV). The age, gender, dominant hand, and the hand used for mask holding by the novice were recorded.
The main outcome variable for the study was to evaluate the effectiveness of mask seal by the objective parameter average tidal volume achieved with each technique of mask holding. Other variables included the minute ventilation as displayed in the monitor panel (computed value), audible mask leak (AML), audible epigastric leak (AEL), incidence of inadequate mask ventilation, dominant hand of the novice, and the preferred hand for performing BMV. Inadequate mask ventilation was defined as a tidal volume of <150 mL with features such as insufficient chest rise, absence of fogging in the mask, lack of or <10 mm Hg ETCO2 was also observed and documented for every breath. The study was aborted if at any point the SpO2 dropped to <95% or any other serious adverse event was noted. In such instance, the patient was managed by experienced as the situation demanded.
A pilot study of eight patients was conducted which showed a tidal volume difference of 40 mL between the groups. The EC technique group had minimum and maximum tidal volumes of 60 and 374.80 mL with mean ± SD of 247.975 ± 107.59. Similarly, the EO technique group had minimum and maximum tidal volumes of 199.60 and 455 mL with mean ± SD of 314.75 ± 104.63. For a two tailed test, the effect size d was 0.629. Considering an α error probability of 0.05, for a power of 90% using independent t-test in G*Power software, we required a sample size of 55 patients in each group. Since the study is crossover in nature, we needed 55 patients in total. To compensate for any fallout, we included 60 patients in the study.
The data were analysed using the SPSS (Statistical Package for Social Sciences) version 16.0 (SPSS Inc. Chicago, IL., USA). The data were subjected to Kolmogorov–Smirnov test to test for the type of distribution. Normally distributed data were presented as mean and standard deviation. Paired t-test was applied for comparing the average of five tidal volumes and minute ventilation and also for comparing each of the five tidal volumes/breaths between the two techniques. For comparing AML, AEL, and adequacy of mask ventilation, McNemar test was applied. A P value of <0.05 was considered statistically significant.
RESULTS
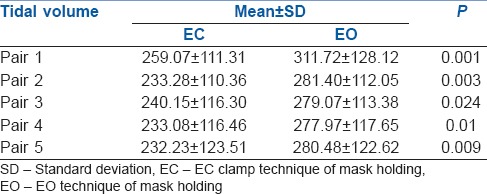
In total, 68 patients were approached for the study and sixty were enrolled successfully. All 60 patients completed the study. The demographic data of the patients is given in Table 2. None of the patients had any difficulty in mask ventilation with the expert anaesthesiologist or with the laryngoscopy and intubation. The demographic data of the novice volunteers is also given in Table 2. Although 57/60 volunteers were right handed, 59 preferred to use left hand for mask holding. The average tidal volume difference between the groups was about 46.5 ± 106.6 mL over five breaths with EO technique providing superior values compared with EC technique (286.12 ± 107.41 vs 239.56 ± 103.95 mL, P = 0.001). Similarly, the average minute ventilation achieved was 2.86 ± 1.05 L/min with EO technique compared with 2.35 ± 1.12 L/min with EC technique, P = 0.001. Individual comparison of each tidal volume between the two techniques, demonstrated statistically superior tidal volumes for all the five breaths with EO technique compared with EC technique [Table 3].
Table 2.
Demographic data of patients and novices
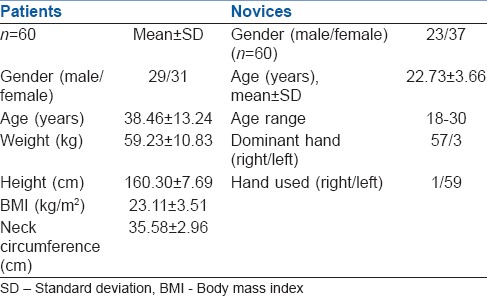
Table 3.
Comparison of individual tidal volumes between EC and EO techniques
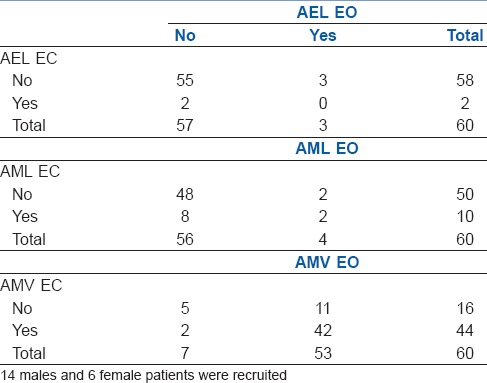
AEL was observed in two patients with EC grip and three patients with EO grip. The EO grip improved the mask ventilation (no AEL) in both patients who had AEL with EC grip. Similarly, EC grip improved the mask ventilation (no AEL) for all three patients who had AEL with EO grip [Table 4, P value = 1.000, McNemar Test]. AML was observed in a total of four patients with EO grip and 10 patients with EC grip. Of the four who had AML with EO grip, EC grip provided better mask seal in two patients (no AML). Similarly, of the 10 who had AML with EC grip, EO grip provided better mask seal in 8 (no AML) [Table 4, P = 0.109, McNemar test]. Mask ventilation was inadequate in a total of 16 patients with EC grip of which EO grip provided better mask ventilation in 11 patients. Similarly, seven did not receive adequate mask ventilation with EO grip of which EC grip improved mask ventilation in two which was statistically significant [Table 4, P = 0.022, McNemar test].
Table 4.
Comparison of AEL, AML, and adequacy of mask ventilation between the groups
DISCUSSION
This prospective randomised double-blinded crossover study evaluated the effectiveness of mask seal provided by two different techniques of mask holding (the classical EC clamp technique and the novel EO technique) by the novices. The mask leak was assessed subjectively by AML, whereas it was also assessed by a more objective parameter, that is, tidal volume achieved at a specific peak airway pressure. Since conventional BMV would render objective evaluation difficult due to variability of tidal volume and peak airway pressure with each breath and possibility of gastric insufflation if peak airway pressures exceeded 20 cm H2O, we employed single handed mask holding along with pressure controlled ventilation with the aid of a ventilator. The peak airway pressure was kept constant (15 cm H2O) to minimise the risk of gastric insufflation and tidal volume was used as the objective parameter to evaluate the difference between the two techniques of mask holding.
Our study results demonstrate that the EO technique of mask holding provides better mask seal in the hands of novices as reflected by better tidal volumes and minute ventilation achieved and higher incidence of adequate mask ventilation as compared with the conventional EC technique of mask holding [Tables 3 and 4]. We believe that had the peak airway limit had been higher (may be 20 cm H2O as against 15 cm H2O used in the study, the difference between the two techniques in the tidal volumes achieved would have become even more obvious). The EO technique of mask holding is essentially a modification of the conventional EC technique. There are two important features that make the EO technique differ from the EC technique: (i) the web space between the thumb and index finger of the hand that holds the mask is placed along the mask border in the EC technique, whereas this web space is brought as close to the mask neck as possible with the EO technique such that the thumb and index finger make a near complete or complete circle around the mask neck [Figure 2] and (ii) the forearm is brought into a semi-prone position with the EO technique from the conventional lateral position of the EC technique [Figure 2]. These two differences in the technique help to provide uniform distribution of pressure over the mask ensuring better mask fit over the patient's facial contours thus minimising air leak. Interestingly, this study demonstrates comparable AML incidence between the technique though the tidal volumes achieved were better with one group. This may be due to two factors: low peak airway pressure 15 cm H2O employed in the study would have resulted in smaller volume of leak around the mask, which was not audible and the fact that the person who evaluated AML was not exactly positioned with his/her ear next to the mask but was standing upright to also document the tidal volumes and minute ventilation values from the ventilator panel.
Single person BMV by novices or healthcare providers is not advocated during cardiopulmonary resuscitation because of its ineffectiveness and the time delay it might cause in positioning of the rescuer for BMV at head end of the victim followed by at the side of the victim for chest compressions.[7,8] However, a recent study demonstrates that over-the-head positioning of the rescuer in relation to the victim for both chest compressions and BMV can improve the effectiveness of cardiopulmonary resuscitation by minimising the time delay.[9] Further, single person BMV is a useful skill to be acquainted by all individuals responsible for managing the airway. Therefore, better technique of mask holding by novices (such as the EO technique) may help minimise the risk of ineffective single person BMV in the absence of other factors contributing to difficulty such as predictors of difficult mask ventilation or inappropriate equipment.
In anaesthesia, we generally tend to use left hand for mask holding and right hand for bagging. In this study, we wanted to analyse which hand would be used by novices and the study results showed that irrespective of which was the dominant hand, all volunteers used left hand for mask holding. The only instance where right hand was used during the study for mask holding was by the volunteer who participated the fourth time in the study [Table 2]. During cardiopulmonary resuscitation, the current recommendation is for 1 second for inspiration and 1 second for expiration while performing BMV. Our study outcome would be useful in these scenarios as often novices or less experienced individuals would be involved in BMV, hence the study included 1 second each for inspiration and expiration.
There were a few limitations to our study. The study was conducted in a controlled environment in the presence of qualified and experienced anaesthesiologists. Hence, during emergency situations in the absence of experienced personnel for support, performance of novices with EO technique of mask holding during single person BMV needs to be studied. The ventilator alarms could provide positive or negative feedback to those well oriented to these. However, in our study as novices were included, we did not silence the ventilator alarms and we do not know whether this could have in any way influenced the results of this study.
CONCLUSION
The EO technique of mask holding provides better mask seal as reflected by improved tidal volumes than the conventional EC clamp technique when single handed mask holding is performed by novices in the absence of other factors contributing to difficulty in mask ventilation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ramachandran SK, Klock PA., Jr . Definition and incidence of the difficult airway. In: Hagberg CA, editor. Benumof and Hagberg's Airway Management. 3rd ed. Philadelphia: Elsevier Saunders; 2013. pp. 201–8. [Google Scholar]
- 2.Kheterpal S, Han R, Tremper KK, Shanks A, Tait AR, O'Reilly M, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006;105:885–91. doi: 10.1097/00000542-200611000-00007. [DOI] [PubMed] [Google Scholar]
- 3.El-Orbany M, Woehlck HJ. Difficult mask ventilation. Anesth Analg. 2009;109:1870–80. doi: 10.1213/ANE.0b013e3181b5881c. [DOI] [PubMed] [Google Scholar]
- 4.Umesh G, Krishna R, Chaudhuri S, Tim TJ, Shwethapriya R. E-O technique is superior to E-C technique in manikins during single person bag mask ventilation performed by novices. J Clin Monit Comput. 2014;28:269–73. doi: 10.1007/s10877-013-9531-9. [DOI] [PubMed] [Google Scholar]
- 5.Ortega R, Mehio AK, Woo A, Hafez DH. Videos in clinical medicine. Positive-pressure ventilation with a face mask and a bag-valve device. N Engl J Med. 2007;357:e4. doi: 10.1056/NEJMvcm071298. [DOI] [PubMed] [Google Scholar]
- 6.Elling R, Politis J. An evaluation of emergency medical technicians' ability to use manual ventilation devices. Ann Emerg Med. 1983;12:765–8. doi: 10.1016/s0196-0644(83)80254-6. [DOI] [PubMed] [Google Scholar]
- 7.Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF, et al. Part 5: Adult basic life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S685–705. doi: 10.1161/CIRCULATIONAHA.110.970939. [DOI] [PubMed] [Google Scholar]
- 8.Morrison LJ, Deakin CD, Morley PT, Callaway CW, Kerber RE, Kronick SL, et al. Advanced life support chapter collaborators. Adult advanced cardiovascular life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S729–67. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]
- 9.Nasiri E, Nasiri R. A comparison between over-the-head and lateral cardiopulmonary resuscitation with a single rescuer by bag-valve mask. Saudi J Anaesth. 2014;8:30–7. doi: 10.4103/1658-354X.125923. [DOI] [PMC free article] [PubMed] [Google Scholar]


