Abstract
Progress in evidence-based treatments for child anxiety has been hampered by limited accessibility of quality care. This study utilized a multiple baseline design to evaluate the pilot feasibility, acceptability, and preliminary efficacy of real-time, Internet-delivered, family-based cognitive-behavioral therapy for child anxiety delivered to the home setting via videoconferencing. Participants included 13 anxious youth (Mean age=9.85) with a primary/co-primary anxiety disorder diagnosis. Eleven participants (84.6%) completed treatment and all study procedures. Consistent with hypotheses, the intervention was feasible and acceptable to families (i.e., high treatment retention, high client satisfaction, strong therapeutic alliance, and low barriers to participation). Moreover, the novel videoconferencing treatment format showed preliminary efficacy: 76.9% of the intention-to-treat (ITT) sample and 90.9% of treatment completers were treatment responders (i.e., Clinical Global Impressions-Improvement Scale = 1 or 2 at posttreatment), and 69.2% of the ITT sample and 81.8% of treatment completers were diagnostic responders (as per the Anxiety Disorders Interview for Children). Gains were largely maintained at 3-month follow-up evaluation. Outcome patterns within and across subjects are discussed, as well as limitations and the need for further controlled evaluations. With continued support, videoconferencing treatment formats may serve to meaningfully broaden the reach of quality care for youth anxiety disorders.
Keywords: Anxiety, Telemental Health, Telehealth, CBT, Videoconferencing
Anxiety disorders are among the most common classes of mental disorders in children and adolescents (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003), affecting up to 32% of youth by the time they reach adolescence (Merikangas et al., 2010). Child anxiety is associated with greater risk for comorbid depression (Ramsawh et al., 2011), impaired academic functioning (Green et al., 2017; Hughes, Lourea-Waddell, & Kendall, 2008), sleep-related problems (Caporino et al., 2017; Weiner, Elkins, Pincus, & Comer, 2015), substance use problems (Wu et al., 2010), and suicidality (Balazs et al., 2013). Encouragingly, the past two decades have witnessed tremendous advances in the development and evaluation of effective youth anxiety treatments (see Higa-McMillan et al., 2016). Cognitive-behavioral treatments incorporating exposure tasks, in which youth systematically confront feared situations in treatment, are particularly effective (Kendall et al., 2005).
Problems in the Accessibility of Evidence-Based Care
Despite advances in the development of evidence-based practices, very few children in need actually receive supported care. Large proportions of children with mental disorders never receive services (Merikangas et al., 2010), and among individuals who do receive care, the median delay in treatment initiation after initial disorder onset ranges from 9 to 23 years across the anxiety disorders (Wang et al., 2005). When treatment is eventually received, evidence-based care is rarely delivered (Comer & Barlow, 2014; McHugh & Barlow, 2010). Reasons for the inadequate provision and utilization of supported services include regional mental health workforce shortages, poor dissemination and implementation of supported practices, and geographic and transportation barriers that interfere with the accessibility of quality care (Comer & Barlow, 2014). A considerable proportion of U.S. counties have no psychologist, psychiatrist, or social worker with child expertise (Comer & Barlow, 2014). Large numbers of families have no way to get to a mental health facility or report that mental health care is simply too far away, and high rates of stigma-related beliefs about attending a mental health clinic can also interfere with treatment seeking (Owens et al., 2002).
Telemental Health Formats Can Extend the Reach of Quality Care
Technology-assisted treatment methods hold promise for enhancing treatment and extending access to services (Chou et al., 2016; Comer, 2016; Comer & Barlow, 2014; Doss et al., 2016; Jones, 2014; Kazdin & Blase, 2011; Kendall et al., 2011; Myers & Comer, 2016). In addition to behavioral intervention technologies (BITs) that do not involve real-time interaction with a therapist (e.g., Khanna & Kendall, 2010; Morgan et al., 2017), telemental health (TMH) approaches using videoconferencing to hold real-time, remote treatment with a live therapist have shown increasing support for a range of child problems (Comer et al., 2017a, 2017b; Doss et al., 2016; Sibley et al., 2017, Vigerland et al., 2017). In fact, Comer and colleagues (2017b) found evidence that TMH approaches using videoconferencing to treat behavior problems in home settings may even yield better outcomes than those observed in clinic-based care, possibly due to skills being practiced and immediately generalized in the very settings in which problems regularly occur.
TMH formats delivering real-time treatment have potential to solve several problems in the accessibility and acceptability of evidence-based care. First, such treatment formats can overcome geographic and time barriers to quality care and minimize conflicts with childcare and occupational responsibilities (Comer, Elkins et al., 2014). For example, reduced travel time associated with TMH can decrease interference with parental work schedules. In addition, many parents may be comfortable leaving siblings unattended in another room in their house during sessions (as well as treated children during parent-only sessions), whereas they may be uncomfortable leaving children unattended in a clinic waiting room. In a recent study, Comer and colleagues (2017b) found families remotely treated with real-time videoconferencing methods reported fewer barriers to treatment participation (e.g., scheduling, transportation, child care difficulties) than clinic-treated families. Second, TMH formats may strengthen the ecological validity and generalizability of care by providing real-time feedback to families in natural settings, where problems typically occur (Comer et al., 2015). Real-time treatments using videoconferencing offer increased mobility and an improved ability to accompany the family to naturalistic settings to complete generalizable exposures.
In recent years, research has supported the feasibility and preliminary efficacy of computer-based treatments for child anxiety and related disorders (Comer, Furr et al., 2014; Donovan & March, 2014; Fung, Manassis, Kenny, & Fiksenbaum, 2002; Khanna & Kendall, 2010; Morgan et al., 2017; Spence et al., 2011). However, many of these programs are self-administered, only leverage asynchronous communications between therapists and families, and/or involve minimal therapist contact. To date, synchronous TMH formats that use videoconferencing to deliver real-time treatment between therapists and families have only been applied to target relatively small population subgroups of youth with anxiety-related conditions (e.g., children with OCD; Comer, Furr, Kerns, et al., 2017; Storch et al., 2011), anxious young children below the age of seven (Cooper-Vince et al., 2016), depressed youth (Nelson, Barnard, & Cain, 2004) or externalizing youth (Comer et al., 2017b). Such TMH programs have yielded treatment response rates of 60-80% and have shown relative comparability with clinic-based outcomes, with one TMH program (Comer et al., 2017b) even showing improved outcomes relative to clinic-based care. However, real-time care conducted remotely by a live therapist using videoconferencing techniques have yet to be evaluated in the treatment of school-aged children presenting with principal anxiety disorders.
The Present Study
We used a multiple baseline design to examine the preliminary utility of family-based CBT (FCBT; Howard et al., 2000), delivered over the Internet using videoconferencing to anxious youth ages 7-14. The study was multi-site, with TMH treatment provided to an ethnically and socioeconomically diverse set of families (N=13) across Massachusetts and South Florida. This study offered fully remote treatment to families in their own homes, but recruitment in this pilot proof-of-concept study did not include many families in rural regions. In the context of this proof-of-concept sample, we hypothesized that TMH-delivered FCBT (i.e., TMH-FCBT) would be feasible (as measured by a high percentage of treatment completers, low rates of technical problems, and high levels of treatment adherence), and acceptable to families (as assessed by measures of client satisfaction and therapeutic alliance). In addition, we hypothesized TMH-FCBT would show preliminary efficacy in reducing youth anxiety symptoms and parental accommodation in both the short-term (measured at midtreatment and posttreatment) and at three-month follow-up (3MFU).
Material and Methods
Participants
Participants included anxious youth and their families recruited from one of two anxiety specialty clinics in the Boston, MA and Miami, FL areas. Eligibility criteria were: 1) child age 7-14 at intake; 2) child with principal/co-principal diagnosis of generalized anxiety disorder (GAD), separation anxiety disorder (SepAD), and/or social anxiety disorder (SocAD); 3) at least one parent willing to participate in treatment; 4) family-owned home computing device with webcam and Internet capabilities; and 5) English fluency. Youth with developmental delay, autism spectrum disorder, intellectual disability, or active suicidality were excluded. Youth on a stable dose of psychotropic medication (i.e., 4 weeks stable dose prior to baseline evaluation) were included. Of 33 age-eligible, consecutive children screened at the two clinics, 25 families consented and completed an initial diagnostic evaluation. The remaining 8 families declined to participate—n=4 scheduled intake but did not show up for evaluation, n=2 preferred to see a clinic-based therapist, n=1 wanted treatment services that could last longer than the active study treatment period, and n=1 wanted freedom to adjust medication throughout active treatment phase of the study.
Of the 25 families who consented, 13 were eligible and enrolled. Reasons for ineligibility included: non-anxiety disorder (e.g., major depression, ADHD, adjustment disorder related to medical condition) assigned as the child’s primary diagnosis/concern (n=7), developmental delay (n=2), active suicidality and referral to inpatient psychiatric unit (n=1), family failing to complete baseline procedures (n=1), and sub-clinical anxiety diagnosis (n=1). The resulting randomized intention-to-treat sample included 13 anxious youth ages 8-13 (M=9.85, SD=1.46), and their mothers. Table 1 presents demographic information of the overall sample, as well as across the Boston (n=8) and Miami (n=5) sites. Roughly 40% of participating youth were of ethnic/racial minority backgrounds, and there was an approximately even gender distribution. The majority of participating mothers reported being married and completing a college education. Roughly 31% of the sample came from households with less than $75,000 in annual family income. At baseline, 69.2% of the sample had a primary/co-primary diagnosis of GAD (n=9), 46.2% had a primary/co-primary diagnosis of SepAD (n=6), and 7.7% had a primary/co-primary diagnosis of SocAD (n=1). Regarding secondary diagnoses, 30.8% had ADHD (n=4), 30.8% had GAD (n=4), 23.1% had SocAD (n=3), 15.4% had a specific phobia (n=2), 7.7% had SepAD (n=1), and 7.7% had OCD (n=1). Nearly 31% of mothers had never engaged in videoconferencing prior to the study.
Table 1.
Demographic Characteristics of Total Sample, and By Site
| Total Sample (N=13) | Site
|
Cross-Site Differences | ||
|---|---|---|---|---|
| Boston (n=8) | Miami (n=5) | |||
|
| ||||
| M (SD) | M (SD) | M (SD) | t | |
| Child age, years | 9.9 (1.5) | 10.0 (1.7) | 9.6 (1.1) | -.46 |
| Maternal Age, years | 44.2 (5.2) | 44.9 (5.3) | 43.0 (5.4) | -.62 |
|
|
||||
| N (%) | N (%) | N (%) | χ2 | |
|
|
||||
| Sex | 9.48** | |||
| Male | 6 (46.2) | 1 (12.5) | 5 (100.0) | |
| Female | 7 (53.8) | 7 (87.5) | 0 (0.0) | |
| Child Race/Ethnicity | 13.00*** | |||
| Non-Hispanic Caucasian | 8 (61.5) | 7 (87.5) | 0 (0) | |
| Hispanic Caucasian | 4 (30.8) | 0 (0) | 5 (100) | |
| Asian American | 1 (7.7) | 1 (12.5) | 0 (0.0) | |
| Parents’ Marital Status | 6.24* | |||
| Married | 10 (76.9) | 8 (100) | 2 (40) | |
| Divorced but not remarried | 3 (23.1) | 0 (100) | 3 (60) | |
| Mother Highest Education Level | 2.30 | |||
| Completed High School | 2 (15.4) | 2 (25) | 0 (0) | |
| Completed College | 5 (38.5) | 2 (25) | 3 (60) | |
| Completed Graduate Degree | 6 (46.2) | 4 (50) | 2 (40) | |
| Annual Household Income | 2.44 | |||
| $25,000-75,000 | 4 (30.8) | 2 (25) | 2 (40) | |
| $75,001-150,000 | 3 (23.1) | 1 (12.5) | 2 (40) | |
| >$150,001 | 6 (46.2) | 5 (62.5) | 1 (20) | |
p<.05,
p<.01,
p<.001
Design
Using the multiple-baseline across participants design (Gallo et al., 2013) families were randomly assigned to 1 of 3 baseline intervals to clarify that changes occurred after treatment initiation, and not during the baseline interval. Using a random numbers table, n=2 families had a two-week baseline interval, n=4 families had a three-week baseline interval, and n=7 families had a four-week baseline interval. After Baseline II, families received 16 weeks of TMH-FCBT. Major assessments were conducted at midtreatment, posttreatment, and 3MFU, and brief questionnaire-based assessments were additionally conducted at weeks 4 and 12.
Measures
Feasibility and Acceptability
After each scheduled session the therapist recorded session attendance, lateness to session, last minute cancellations made <24 hours of scheduled session and reason for cancellation, number and types of session interruptions, and number of minutes spent addressing technological issues. Homework compliance ratios were calculated by tallying the number of assignments completed across sessions divided by the number of total assignments given. The44-item parent-report Barriers to Treatment Participation Scale (BTPS; Kazdin et al., 1997) was administered at week 4, midtreatment, week 12, and posttreatment to assess perceived barriers to participation in TMH-FCBT. Items are scored on a 5-point scale with values ranging from 1 (“never a problem”) to 5 (“very often a problem”). The Total Barriers score was presently used (possible range: 44-220), has demonstrated good internal consistency (Cronbach α=0.78 in present sample), and has been shown to be a predictor of treatment dropout (Kazdin et al., 1997).
The 36-item Working Alliance Inventory, Parent-Report and Therapist-Report (WAI) (Horvath & Greenberg, 1989) assessed therapeutic alliance at week 4, midtreatment, week 12, and posttreatment. Items are rated on a 7-point scale with item scores ranging from 1 (“never”) to 7 (“always”). Higher scores indicate greater perceived therapeutic alliance (range: 36-252). The WAI has demonstrated good reliability and validity; internal consistency was high in the present sample (therapist-report Cronbach α=0..96; mother-report Cronbach α=0.73). Mothers were asked to report on their own alliance with the therapist (not their perceptions of their child’s alliance with the therapist).
The 8-item Client Satisfaction Questionnaire (CSQ-8; Attkisson & Zwick, 1982) was admininstered to mothers at posttreatment to evaluate satisfaction with services. The CSQ-8 has demonstrated good internal consistency and validity (Attkisson & Zwick, 1982). Items are rated on a 4-point scale (values of 1-4), with higher scores indicating higher satisfaction (Total score range: 8-32). In the present study, internal consistency was strong (Cronbach α=0.85).
Clinical Outcomes
The Anxiety Disorders Interview Schedule for Children, Child and Parent Interviews (ADIS-C/P; Silverman & Albano, 1996), a semi-structured DSM-based diagnostic interview, was administered to evaluate child diagnostic status at Baseline I, Baseline II, posttreatment, and 3MFU. The ADIS-C/P is the most commonly used diagnostic interview in clinical trials of child anxiety treatment (Silverman & Ollendick, 2005) and has demonstrated good reliability and concurrent validity (Silverman, Saavedra, & Pina, 2001; Wood, Piacentini, Bergman, McCracken, & Barrios, 2002). In addition to categorical assessment of diagnoses, each diagnosis is assigned a Clinical Severity Rating (CSR) on a scale of 0 to 8. CSRs≥4 indicate clinically elevated impairment and interference, whereas CSRs≤3 reflect subclinical presentations. Independent Evaluators (IEs) masked to treatment participation details conducted the ADIS interviews.
The Clinical Global Impressions Scale (CGI; Guy & Benato, 1970), a widely used clinician-reported measure of global impressions, assessed treatment response. The CGI measures both global severity (CGI-S) and global improvement (CGI-I) on 7-point scales with CGI-S scores ranging from 1 (“normal”) to 7 (“among the most severely ill patients”) and CGI-I scores ranging from 1 (“very much improved”) to 7 (“very much worse”). CGI conventions identify youth receiving CGI-I scores of 1 (“very much improved”) or 2 (“much improved”) as “treatment responders.” IEs completed the CGI following diagnostic assessments at the major assessments. To assess global functioning, IEs completed the Clinical Global Assessment Scale (CGAS; Shaffer et al., 1983) at the major assessments. The CGAS is a clinician-reported measure of children’s global functioning, rated on a scale from 0-100 with guidelines for each 10-point range of functioning. The CGAS has demonstrated strong psychometric properties (Shaffer et al., 1983).
The 39-item Multidimensional Anxiety Scale for Children, Child and Parent Reports (MASC-C/P) (March, Parker, Sullivan, Stallings, & Conners, 1997) were used to continuously assess child self-report and parent-report of anxiety symptoms on a weekly basis. The MASC-C and MASC-P include parallel items. Each item is rated on a 4-point scale ranging from 0 (“never true about me”) to 3 (“often true about me”). Higher total scores signify more severe anxiety concerns (range: 0-117). Raw scores are converted to standard scores based on age and gender. The MASC has demonstrated strong psychometric properties (Langer, Wood, Bergman, & Piacentini, 2010; March et al., 1997). Internal consistency was high in the present sample (Cronbach α=0.88).
The Anxiety Problems scale of the Child Behavior Checklist (CBCL 6-18; Achenbach, 1991) was also completed by mothers at Baseline I and II, week 4, midtreatment, week 12, posttreatment, and 3MFU. T-scores>65 reflect anxiety problem scores in the clinical range. The CBCL is widely used and has demonstrated strong psychometric properties (Achenbach & Rescorla, 2000); internal consistency of the anxiety problems scale in the present sample was high (Cronbach α=0.93).
We also assessed family accommodation via the Family Accommodation Checklist and Interference Scale (FACLIS; Thompson-Hollands et al., 2014), a parent-report checklist of 20 various types of common accommodation patterns found in the families of anxious children. The tally of all FACLIS accommodation items endorsed yields an Accommodation Scope score ranging from 0-20. The FACLIS also assesses interference associated with each form of parental accommodation on a 0-8 scale (0 reflects “no interference” and 8 reflects “extreme interference”). Interference ratings for all endorsed accommodation items are summed to yield a Total Accommodation Interference score (possible range of 0-160). The FACLIS has demonstrated strong reliability and validity (Thompson-Hollands et al., 2014). Internal consistency was adequate for the Accommodation Scope score (Cronbach α=0.69) and the Total Accommodation Interference score (Cronbach α=0.86).
Fidelity
Two clinical research assistants coded treatment tapes with an adherence manual (adapted from Chu, 2011) to evaluate fidelity to the FCBT manual implemented in this study. Fidelity coders trained on pilot cases and reliability between coders was confirmed prior to coding for this study. Each session that was successfully recorded (i.e., 95.23% of conducted sessions) was coded by at least one coder. Of available tapes, 14.2% were randomly selected for double-coding by both research assistants; total reliability was adequate, κ=.66 (95% CI: .22, 1.10), p<.001.
Procedure
Study procedures were conducted under the approval of the institutional review boards at [Institution name redacted for masked review] and [Institution name redacted for masked review]. Eligible families were recruited from the flow of families presenting for child anxiety services at one of the two recruitment sites. Informed consent and assent were obtained prior to study participation. Doctoral clinical psychology students who were trained to reliability served as Independent Evaluators (IEs) and conducted ADIS interviews at Baseline I and II, posttreatment, and 3MFU. At these time points, IEs also assigned CGI and CGAS scores. Baseline I assessment was conducted in the clinic, whereas the other major assessments were conducted over the telephone. IEs were not the therapist for any cases, and were kept masked to all treatment related matters. Questionnaires were completed through a secure online survey platform. Following their randomly determined baseline interval, participating families participated in the 16-week active treatment phase prior to completing posttreatment and then 3MFU assessments. Regardless of participant site, treatment was provided by the first author in Boston from a private office with high-speed Internet access, under the supervision of a clinical psychologist licensed in both Massachusetts and Florida.
Intervention
Families participated in 16 sessions of FCBT (Howard et al., 2000), a protocol that has received strong support for the treatment of anxious children ages 7-14 when implemented in the clinic (Kendall et al., 2008). As with most supported CBT programs for child anxiety, the first half of intervention consists of psychoeducation, relaxation training, promoting awareness of and ability to restructure automatic negative thoughts, problem-solving, and development of a fear hierarchy. The second half of treatment focuses on graduated exposure tasks, in which the child systematically confronts increasingly feared and avoided situations and stimuli. Homework is assigned each week to increase out-of-session treatment engagement and optimize generalizability. In addition, FCBT involves parents in all treatment components, incorporates added parental psychoeducation, and places additional emphasis on the role parents can play in the development, maintenance, and/or exacerbation of child anxiety symptoms. FCBT augments traditional exposure therapy by targeting patterns of parental overprotection, family accommodation, and maladaptive parent-child interactions that can inadvertently reinforce child anxiety symptoms.
At the beginning of treatment, families were mailed a hard copy of the FCBT child and parent workbook to accompany the FCBT treatment program. The intervention was delivered in weekly, one-hour sessions for 16 weeks over the Internet to families in their home settings using secure and encrypted software that enabled webconferencing as well as screen-sharing to accommodate sharing of treatment-related worksheets and progress charts. In-depth discussions of TMH security, privacy, logistics, and ethics, as well TMH professional guidelines, can be found elsewhere (Chou et al., 2016; Crum & Comer, 2016; Myers et al., 2017). To ensure families had a private and distraction-free environment during their home-based treatment, parents were asked to choose a closed-off, quiet room in which to hold sessions, to put cell phones on silent and ignore home phone calls, and if possible to obtain childcare or provide activities for other siblings at home.
To increase engagement, electronic versions of treatment worksheets and handouts were developed that allowed families to interactively complete standard session activities, such as an interactive electronic fear hierarchy and psychoeducation materials. For example, worksheets and handouts designed for in-office interactive therapeutic engagement were adapted to allow the child to use the “screen-share” function of the videoconferencing platform that allows the therapist to pass control of the desktop to the family, allowing the child to complete the worksheet with their mouse. Similar “screen-share” strategies for increasing engagement over videoconferencing have been described elsewhere (Comer, Furr et al., 2014). Finally, in TMH-FCBT, we allowed Internet-based exposures to be conducted in public via smartphones as needed.
Data Analysis
Data were analyzed using SPSS, Version 20. Chi-square tests and independent samples t-tests evaluated sociodemographic differences across sites. In multiple baseline designs, with participants beginning treatment at varying and randomly determined lengths from initial baseline assessment, the effect of an intervention is demonstrated when symptom changes occur after treatment, and not before. Absence of change during the baseline interval indicates clinical stability prior to treatment initiation; changes from Baseline II to posttreatment are thus interpreted as treatment-related changes. Paired sample t-tests were used to assess pretreatment stability of measures by comparing means between Baseline I and II, then assessed treatment-related changes by comparing means between Baseline II and posttreatment. Maintenance of treatment-related changes was assessed by comparing means between Baseline II and 3MFU as well as between posttreatment and 3MFU. Consistent with CGI conventions (Walkup et al., 2008), “treatment responders” were defined as participants who were assigned a CGI-I score of 1 (“very much improved”) or 2 (“much improved”) at posttreatment. Diagnostic responders were defined as participants who no longer met criteria for their baseline principal anxiety disorder at posttreatment (i.e., ADIS CSR<4). Diagnostic remission was defined as participants who did not meet diagnostic criteria for any of the target anxiety disorders at posttreatment (i.e., ADIS CSR<4).
Results
Preliminary Findings
As expected, there were no “treatment responders” or “diagnostic responders” from Baseline I to Baseline II. Similarly, child- and mother-report of symptoms and parent accommodation, as well as diagnostic severity ratings, did not significantly change between Baseline I and II (see Table 2). In contrast, CGAS scores did show improvement between Baseline I and II (Cohen’s d= -1.12), suggesting that although symptoms, accommodation, responder status, and diagnostic status did not improve from Baseline I to Baseline II, there were some early improvements in overall child functioning across the baseline interval.
Table 2.
Response To Baseline Interval And Treatment Among ITT Cases (N=13)
| Baseline I (B1) | Baseline II (B2) | Post1 | 3MFU1 | Significance BI to BII | Significance BII to Post1 | Significance Post to 3MFU1 | Significance BII to 3MFU1 | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Child Global Severity and Functioning | M(SD) | M(SD) | M(SD) | M(SD) | t | t | t | t |
| CGI-S | 5.2(.7) | 4.9(0.8) | 2.6(1.3) | 2.2(1.1) | 1.90 | 5.45** | 1.49 | 8.15*** |
| CGAS | 49.3(8.9) | 52.7(9.4) | 69.3(7.7) | 69.0(7.2) | -3.78** | -4.51** | .19 | -4.77** |
|
| ||||||||
| Child Anxiety Symptoms and Diagnoses | M(SD) | M(SD) | M(SD) | M(SD) | t | t | t | t |
|
| ||||||||
| Anxiety Symptoms | ||||||||
| Child | 56.2(7.8) | 54.3(8.1) | 51.7(13.6) | 50.4(12.8) | 1.44 | .37 | .69 | .88 |
| Mother | 58.2(12.4) | 57.0(11.0) | 41.6(10.5) | 41.3(10.8) | 1.16 | 3.33** | .16 | 3.12* |
| Anxiety Problems | ||||||||
| Mother | 72.2(4.8) | 71.5(8.6) | 58.5(6.4) | 58.5(8.2) | .54 | 2.80* | .35 | 3.07* |
| ADIS Principal Diagnosis CSR | 5.7(.6) | 5.5(0.9) | 2.6(1.4) | 2.1(1.5) | 1.90 | 5.43*** | 2.19* | 5.71*** |
|
| ||||||||
| Mother Accommodation | M(SD) | M(SD) | M(SD) | M(SD) | t | t | t | t |
|
| ||||||||
| Accommodation Scope | 5.6(3.4) | 4.9(3.6) | 2.0(2.0) | 2.1(1.6) | 1.09 | 3.30** | -.23 | 2.67* |
| Accommodation Interference | 26.8(25.9) | 21.3(15.9) | 4.1(5.0) | 3.8(4.5) | 1.22 | 3.54** | .26 | 3.45** |
These values and analyses refer to completer sample only (N=11).
p≤.05,
p<.01,
p<.001
Note: Child- and mother-reported anxiety symptoms were measured via the MASC-C/P total t-score, mother-reported anxiety problems was measured via the CBCL Anxiety Problems subscale t-score, and parent accommodation was measured via the FACLIS Accommodation Scope and Interference subscale raw scores.
Feasibility, Engagement, and Acceptability
Adherence to the treatment manual was high (96.77%, SD = 3.44%), including throughout the exposure phase of FCBT, as determined by independent fidelity coders. The majority of families completed their full course of TMH-FCBT (i.e., 84.6% completion rate among ITT youth, with 100% retention at the Boston site and 60% retention at the Miami site). Two participants dropped out after session 4 and 10, respectively, and did not participate in the posttreatment assessments.
Sessions were on average just short of the allotted 60 minutes (M=57.5, SD=3.5), and troubleshooting technical difficulties only took an average of approximately one minute per session (M=0.9, SD=1.2). The majority of sessions (62.5%) had no interruptions, but reasons for interruptions when they did occur were specific to home-based therapy issues that would not have impacted a clinic-based session (e.g., pets, landline ringing). Of note, the two dropout cases and one completer case that did not achieve treatment response were the only families in the sample that experienced interruptions due to parents leaving the computer to complete other parenting duties, such as caring for siblings, making dinner, or unloading groceries and stating that they would be back in a few minutes while the child met with the therapist. Reasons provided for last-minute cancellations were typical of common cancellations for clinic-based appointments.
The majority of TMH-FCBT sessions started on time (65.9%) or within the first five minutes (19.3%). Last minute cancellations (<24 hours advance notice) were uncommon (8.5% of total sessions). Overall, mother-reported barriers to TMH-FCBT participation were extremely low (see Table 3). Mean homework compliance across treatment was relatively high (67.9%). TMH-FCBT was rated as very acceptable to families based on mother-report responses on the CSQ-8 (see Table 3). Very high alliance ratings across treatment, as measured by mother- and therapist-report WAI forms, also speak to the acceptability of TMH-FCBT.
Table 3.
Mother- and Therapist-Reported Feasibility and Acceptability Among Completer Sample (N=11)
| Session 4 | Mid-Treatment | Session 12 | Posttreatment | |
|---|---|---|---|---|
|
| ||||
| M(SD) | M(SD) | M(SD) | M(SD) | |
| Mother-Reported Measure of Feasibility | ||||
|
| ||||
| Barriers to Treatment | 46.9(3.8) | 49.0(4.5) | 50.6(8.0) | 50.1(6.5) |
| Participation (BTPS Total) | ||||
|
| ||||
| Mother-Reported Measures of Acceptability | ||||
|
| ||||
| CSQ-8 | 30.0(2.1) | 31.1(1.2) | 30.7(2.1) | 30.7(2.4) |
| Therapeutic Alliance | ||||
| WAI (Total) Mother-Report | 237.4(12.9) | 240.8(8.8) | 241.2(11.7) | 245.6(5.9) |
| WAI (Total) Therapist-Report | 249.9(4.2) | 245.4(9.1) | 245.1(10.6) | 244.4(11.7) |
Preliminary Efficacy
At posttreatment and again at 3MFU, 90.9% of treatment completers (N=10; and 76.9% of the ITT sample) were “treatment responders” (i.e., CGI-I=1 or 2). The one completer case that was not a treatment responder was nonetheless rated as “minimally improved” (CGI-I=3) at posttreatment and at 3MFU. Moreover, 81.8% of treatment completers (N=9 and 69.2% of ITT sample) were “diagnostic responders” (i.e., free of Baseline I principal diagnosis) at posttreatment and at 3MFU. Furthermore, 72.7% of treatment completers (N=8 and 61.5% of ITT sample) were in “diagnostic remission” (i.e., free of all target anxiety disorders) at posttreatment and at 3MFU.
Among treatment completers (N=11), many significant improvements were observed. From Baseline II to posttreatment, IE ratings reflected very large and significant reductions in Global Severity (CGI-S Cohen’s d= -1.76), severity of baseline primary anxiety diagnosis (Primary CSR Cohen’s d= -1.68) and Global Functioning (CGAS Cohen’s d=1.55) (see Table 2 for means and paired-samples t-test results). These improvements were maintained at 3MFU (CGI-S Cohen’s d= -2.52; Primary CSR Cohen’s d= -1.22; CGAS Cohen’s d=1.59) (see Table 2).
Improvements were also observed in mother reports. Between Baseline II and posttreatment, mothers reported very large and significant improvements in child Anxiety Symptoms (MASC-P Cohen’s d= -1.23) and Anxiety Problems (CBCL Anxiety Problems Cohen’s d= -1.56) (see Table 2). These gains were maintained at 3MFU (MASC-P Cohen’s d= -1.19; CBCL Anxiety Problems Cohen’s d= -1.57). Contrary to IE ratings and mother reports, children did not report significant improvements in child anxiety symptoms at posttreatment or at 3MFU (see Table 2). Figure 1 also graphically presents mean MASC-C/P scores over the course of treatment.
Figure 1.
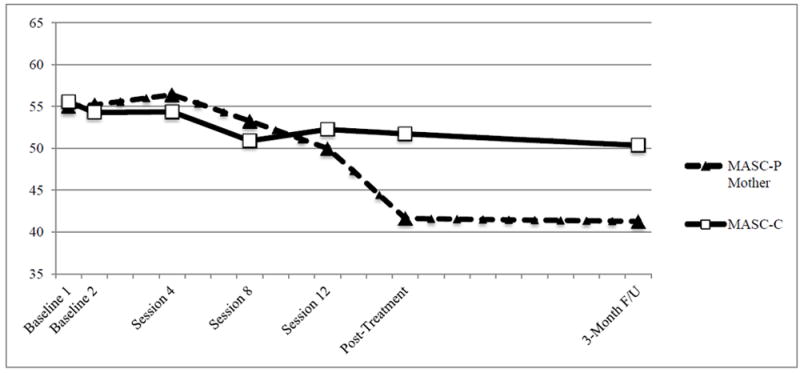
Child- and Mother-Reported Reductions in Anxiety Across Treatment Among Completer Sample (N=11)
Note: Scores represent mean MASC t-scores for each time point
Mothers reported large and significant reductions in parental accommodation of child anxiety from Baseline II to posttreatment (Cohen’s d= -1.61), and from Baseline II to 3MFU (Cohen’s d= -1.19). Significant reductions in interference related to parental accommodation were also observed from Baseline II to posttreatment (Cohen’s d= -2.17) and from Baseline II to 3MFU (Cohen’s d= -2.12) (see Table 2).
Discussion
The present pilot study offers the first evaluation of the use of videoconferencing to remotely deliver supported treatment for child anxiety disorders to the home setting, and findings supported the preliminary feasibility, acceptability, and efficacy of this novel treatment format. The present findings add to a growing body of literature supporting TMH solutions for expanding the reach of supported psychological treatments for children (e.g., Comer et al., 2017a, 2017b; Cooper-Vince et al., 2016; Doss et al., in press; Nelson et al., 2004; Sibley et al., 2017). Whereas recent research has identified benefits of technology-assisted or technology-based treatments for youth with a variety of presenting problems (Vigerland et al., 2016), this literature has almost exclusively focused on self-administered platforms and behavioral intervention technologies with or without minimal therapist support (e.g., Khanna & Kendall, 2010; Spence et al., 2011; Morgan et al., 2017), or technology-enhanced programs that augment face-to-face services conducted in the clinic (e.g., Jones et al., 2014). Such innovations either only afford low-intensity asynchronous communications between clients and therapists (as is the case for self-administered or minimal therapist involvement programs) or still require clients to be able to attend sessions in the clinic and thus fail to extend the reach of supported care (as is the case of technology-enhanced treatments). Prior to this pilot study, synchronous TMH formats that use videoconferencing to deliver real-time treatment between therapists and families have only focused on youth with non-anxiety disorders such as OCD, depression, or externalizing problems (Comer et al., 2017a, 2017b; Storch et al., 2011; Nelson et al., 2004; Sibley et al., 2017), or have begun to consider TMH for child anxiety only in very young children (e.g., Cooper-Vince et al., 2016). With roughly 85% of the pilot sample completing a full course of TMH-FCBT, and roughly 91% of these treatment completers showing successful treatment response, the present study is the first to document the potential benefits of real-time TMH for children in middle childhood presenting with the common anxiety disorders.
The preliminary feasibility and acceptability of TMH-FCBT observed in this pilot evaluation are promising. Treatment retention was high and mothers reported few barriers to treatment engagement that often prove problematic in clinic-based care (e.g., scheduling, time spent traveling to appointments, transportation and sibling childcare concerns). These findings are consistent with recent research conducted with young externalizing children, in which TMH-treated families reported significantly fewer barriers to care than families treated with standard clinic-based care (Comer et al., 2017b). Mothers also reported high consumer satisfaction with the intervention. Of note, only 6.06% of consecutive admissions to the two clinics during the study period (n=2 of 33) declined to participate because they preferred to see a clinic-based therapist.
Although this pilot evaluation was, by design, underpowered to test formal efficacy (see Gallo et al., 2013; Kraemer et al., 2006), there was nonetheless preliminary indication that TMH-FCBT yielded favorable clinical response, as evidenced by multi-informant ratings of significant improvement during the acute treatment phase. Despite the sample size, the majority of outcomes showed significant improvements at posttreatment and again at 3MFU. Although the present pilot study did not include a comparison condition in which families were treated in the clinic, the very high rates of treatment response and diagnostic response, as well as significant improvements across child symptoms and functioning, compare favorably with published outcomes observed for clinic-based FCBT for child anxiety (Kendall et al., 2008).
Of note, in this small pilot sample, children did not self-report significant changes in their anxiety across any of the time points. Such results should be interpreted in the context of evidence of poor parent-child agreement on anxiety symptoms (Comer & Kendall, 2004), and the fact that it is not uncommon for child self-reports to fail to show significant improvements following supported treatment for child anxiety (e.g., Albano et al., 2018).
Interestingly, although symptoms, accommodation, responder status, and diagnostic status did not improve from Baseline I to Baseline II, CGAS scores suggested there were some early improvements in overall child functioning across the baseline interval and before treatment was initiated. This may reflect early expectancy effects associated with the anticipation of Internet-delivered treatment, or may reflect relative instability in the extent of pretreatment functional impairment among youth in the present sample.
Finally, treatment engagement and retention in this pilot sample seemed to vary across sites. At present, it is not clear whether these differences are due to ethnic differences across the two sites, gender differences, or differential comfort with videoconferencing prior to the study, or whether these apparent differences are just due to error variance in an underpowered pilot sample. Controlled evaluations in larger samples can evaluate whether cultural factors, technological literacy, and/or life stress might meaningfully influence family engagement in TMH treatment formats.
Limitations
Several limitations warrant comment. The small sample size and within-subjects design of this pilot evaluation was, by design, underpowered. Idiographic methods and single-case experimental designs are critical for early-stage pilot testing of novel treatment formats (Gallo, Barlow, & Comer, 2013; Kraemer et al., 2006), but the limited power prevented us from conducting formal efficacy evaluations and precluded evaluation of mediators and moderators of treatment response. It will be important for future research to compare TMH-FCBT against clinic-based FCBT. A recent controlled trial that compared outcomes in TMH-based parent training for externalizing youth versus clinic-based parent training found TMH-based parent training actually showed better responses than clinic-based parent training on some clinical dimensions (Comer et al., 2017b). It is possible that delivering treatment to families in their natural setting (i.e., the home) improves the ecological validity of care and may yield more favorable response than clinic-based formats. Studies should also examine TMH-FCBT against treatment-as-usual comparisons in order to evaluate the incremental benefits of TMH-FCBT relative to existing standards of care.
Given the limited sample size, all cases were treated by the same therapist. Accordingly, although differences across cases cannot be attributed to therapist differences, the present design cannot rule out the possibility that some gains were simply due to therapist effects rather than to TMH-FCBT specifically. Further, the relatively poorer outcomes observed in the Miami sample may have been due, in part, to regional and/or cultural mismatches between the non-Hispanic therapist located in Boston and Hispanic families located in South Florida.
In addition, given the pilot nature of the present study, we opted for a somewhat abbreviated three-month follow-up period. Although three-month follow-up evaluations are certainly found throughout the child anxiety treatment literature (e.g., Flannery-Schroeder & Kendall, 2000; Hogendoorn et al., 2014; Khanna & Kendall, 2010), larger studies of TMH-FCBT need to evaluate outcomes over longer periods of time. Longer-term evaluations of clinic-based CBT for child anxiety suggest many treatment gains are maintained, whereas some gains dissipate with time and likely require booster treatment (Albano et al., 2018; Ginsburg et al., 2014; Kendall et al., 2008; Piacentini et al., 2014). Future work will be needed to clarify the extent to which gains in the context of videoconference-based treatment are maintained across time.
Moreover, both recruitment settings were located in urban areas and university settings. All families lived within an hour or so of Boston or Miami and were willing to come to the clinic for initial baseline assessment. Accordingly, it is unclear whether the present results generalize to families in more rural areas. As Chou and colleagues (2017) have noted, there is currently a relative mismatch in the TMH literature between the rhetoric that broadly characterizes the promise of technology to improve treatment accessibility and the reality of the samples in which TMH formats are being tested. Rural populations show relatively poorer rates of technological access. To poise TMH formats for success, more relevant sampling efforts are now needed to go beyond proof-of-concept studies conducted in metropolitan settings and to examine TMH formats in the very populations they might best serve. In addition, although the majority of U.S. families now have household Internet access, future TMH efforts might do well to also target non-household settings (e.g., schools, libraries, primary care offices) to overcome gaps in household technology access.
Although all participants met criteria at baseline for an anxiety disorder, and although baseline CBCL Anxiety Problem scores were in the clinically elevated range, baseline MASC scores were, on average, relatively low. This may reflect somewhat low correspondence between the MASC and the CBCL/ADIS, or may reflect that on some dimensions the present sample was not as severe as other samples of anxious youth. Moreover, we used the original MASC, rather than the less evaluated but more recent MASC 2. This potentially calls into question the full generalizability of the present findings to clinical and research settings that use the MASC 2 in their practices.
Finally, eligible primary diagnoses were restricted to GAD, SepAD, and SocAD for comparability with the Coping Cat treatment literature, which has restricted focus to these disorders (e.g., Kendall et al., 2008; Walkup et al., 2008). As such, our findings may not generalize to the treatment of other anxiety disorders, such as specific phobias, panic disorder, and selective mutism.
Clinical Implications and Future Directions
Despite limitations, the present findings are the first to provide evidence in support of the preliminary feasibility, acceptability, and efficacy of TMH-FCBT for children presenting with GAD, SocAD, and/or SepAD. Despite promising findings, some issues with engagement still arose and roughly 15% of enrolled families dropped out of treatment prematurely. Only 62.5% of sessions had zero interruptions. This raises the issue of what to do when elimination of traditional barriers (e.g., transportation, childcare) only yields new ones (technological complications) (Chou et al., 2017). Moreover, the two cases that dropped out of treatment were both Hispanic males with single mothers, whereas the other three Hispanic males that completed treatment had a two-parent household or other caregiver support. Theoretically, TMH offers improved flexibility for single parents lacking spare time to drive to appointments. However, these two families tended to become distracted by household chores during session, suggesting TMH flexibility may inadvertently allow for a less structured experience that interfered with parents truly being “present.” In addition, both mothers who dropped out of treatment reported they had never used videoconferencing prior to the study. There is still much to learn about which families are best suited for home-based TMH.
The field of TMH is still very new, and a number of critical issues still need to be resolved (Comer & Barlow, 2014; Doss et al., in press). First, although videoconferencing technology liberates therapists from the confines of geography, licensure regulations in most states do not allow therapists to cross state lines. TMH therapists may do well to seek out licensure in multiple states in order to reach as broad a population as possible. Second, cultural competency issues are particularly critical in TMH. Technology logistically enables therapists to reach new populations of varying cultures in regions far away from their office, but it is not necessarily the case that TMH therapists are adequately competent in working with regionally and culturally diverse populations. Third, TMH is still a relatively new mode of treatment delivery, and payer issues related to TMH are still not resolved (Comer & Barlow, 2014). Many private insurance companies will not yet reimburse for TMH services, although a number of federal and state insurance programs do.
Finally, as Comer and Barlow (2014) note, real-time TMH strategies hold great promise for expanding the geographic accessibility of quality care, but may nonetheless be restricted by workforce-power problems. High quality clinic-based treatment centers often cluster around academic and metropolitan hubs and already operate with sizable waitlists. Accordingly, even doubling the workforces at these clinics may not have a meaningful impact if such clinics are now delivering real-time TMH to entire statewide regions (Comer & Barlow, 2014). Consistent with Kazdin and Blase (2011), a broadened portfolio of treatment delivery models that do not rely on real-time provider-based care is needed. Specifically, research is needed to identify how lower intensity and largely self-administered behavioral intervention technologies (BITs; see Doss et al., in press) can be used to buttress real-time TMH efforts at earlier stages of stepped care efforts.
As the field of TMH advances, this study adds to a growing literature supporting TMH (e.g., Comer et al., 2017a, 2017b; Nelson et al., 2004; Sibley et al., 2017; Storch et al., 2011) by providing preliminary evidence of the feasibility, acceptability, and efficacy of TMH-FCBT for anxious youth. Future work with larger, controlled trials is needed to build on this pilot work to evaluate the full potential of TMH formats for the delivery of child anxiety treatment. Amidst a concerning backdrop of considerable barriers to traditional treatment services for a large proportion of the population in need, as well as indications that psychological treatments are playing a less prominent role in mental health care (Olfson & Marcus, 2010), the present findings underscore the promising role that TMH formats may offer for improving the reach of supported treatment for child anxiety.
Highlights.
Internet-delivered CBT for anxious youth is feasible and acceptable to families.
Internet-delivered CBT showed preliminary efficacy in reducing child anxiety symptoms in this pilot study.
Cross-site differences in engagement were found, suggesting need for further evaluation.
Acknowledgments
We wish to thank Drs. Marcy Thompson, Kristin Long, and Lisa Smith for their helpful comments on early versions of this work. We also acknowledge the contributions of Laura Nelson, B.A., Amanda Rodrigues, B.A., and Morgan Manning, for their efforts in fidelity coding and data entry, and the contributions of the independent evaluators in Boston (Caroline Kerns, Ph.D., R. Meredith Elkins, PhD., Allie Keller, M.A., and Lydia Chevalier, M.A.) and Miami (Tommy Chou, M.S., Amanda Sanchez, M.S., and Danielle Cornacchio, M.S.).
Funding: This work was supported by the American Psychological Association (Dissertation Research Award); Boston University (Clara Mayo Fellowship); and the National Institute of Health (K23 MH090247).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. Integrative guide for the 1991 CBCL/4-18, YSR, TRF profiles. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2000. [Google Scholar]
- Albano AM, Comer JS, Compton SN, Piacentini J, Kendall PC, Birmaher B, Walkup JT, Ginsburg GS, Rynn MA, McCracken J, Keeton C, Sakolsky DJ, Sherrill JT. Secondary outcomes from the Child/Adolescent Anxiety Multimodal Study (CAMS): Implications for clinical practice. Evidence-Based Practice in Child and Adolescent Mental Health. 2018 doi: 10.1080/23794925.2017.1399485. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association. Guidelines for the practice of telepsychology. Washington, D.C: 2013. [Google Scholar]
- Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning. 1982;5(3):233–237. doi: 10.1016/0149-7189(82)90074-X. [DOI] [PubMed] [Google Scholar]
- Balazs J, Miklosi M, Kereszteny A, Hoven CW, Carli V, Wasserman C, Wasserman D, et al. Adolescent subthreshold-depression and anxiety: psychopathology, functional impairment and increased suicide risk. Journal of Child Psychology and Psychiatry. 2013;54(6):670–677. doi: 10.1111/jcpp.12016. [DOI] [PubMed] [Google Scholar]
- Caporino NE, Read KL, Shiffrin B, Settipani C, Kendall PC, Compton SN, Albano AM, et al. Sleep-related problems and the effects of anxiety treatment in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2017;46(5):675–685. doi: 10.1080/15374416.2015.1063429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou T, Bry LJ, Comer JS. Overcoming traditional barriers only to encounter new ones: Doses of caution and direction as technology-enhanced treatments begin to “go live”. Clinical Psychology: Science and Practice. 2017;24(3):241–244. doi: 10.1111/cpsp.12196. [DOI] [Google Scholar]
- Chou T, Comer JS, Turvey CL, Karr A, Spargo G. Technological considerations for the delivery of real-time child telemental healthcare. Journal of Child and Adolescent Psychopharmacology. 2016;26(3):192–197. doi: 10.1089/cap.2015.0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu BC. Coping Cat Adherence & Extensiveness Coding Manual. 2011 Unpublished manuscript. [Google Scholar]
- Comer JS. Introduction to the special series: Applying new technologies to extend the scope and accessibility of mental health care. Cognitive and Behavioral Practice. 2016;22(3):253–257. doi: 10.1016/j.cbpra.2015.04.002. [DOI] [Google Scholar]
- Comer JS, Barlow DH. The occasional case against broad dissemination and implementation: Retaining a role for specialty care in the delivery of psychological treatments. American Psychologist. 2014;69:1–18. doi: 10.1037/a0033582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Elkins RM, Chan PT, Jones DJ. New methods of service delivery for children’s mental health care. In: Alfano CA, Beidel D, editors. Comprehensive evidence-based interventions for school-aged children and adolescents. New York: Wiley; 2014. [Google Scholar]
- Comer JS, Kendall PC. A symptom-level examination of parent-child agreement in the diagnosis of anxious youths. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:878–886. doi: 10.1097/01.chi.0000125092.35109.c5. [DOI] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Cooper-Vince C, Kerns C, Chan PT, Edson AL, Khanna M, Freeman JB. Internet-delivered treatment for early-onset OCD: A preliminary case series. Journal of Clinical Child and Adolescent Psychology. 2014;43:74–87. doi: 10.1080/15374416.2013.855127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Cooper-Vince C, Madigan RJ, Chow C, Chan PT, Idrobo F, Eyberg SM, et al. Rationale and considerations for the Internet-based delivery of Parent-Child Interaction Therapy. Cognitive and Behavioral Practice. 2015;22:302–316. doi: 10.1016/j.cbpra.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Kerns CE, Miguel E, Coxe S, Elkins RM, Freeman JB, et al. Internet-delivered, family-based treatment for early-onset OCD: A pilot randomized trial. Journal of Consulting and Clinical Psychology. 2017a;85:178–186. doi: 10.1037/ccp0000155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Miguel E, Cooper-Vince CE, Carpenter AL, Elkins RM, Chase R, et al. Remotely delivering real-time parent training to the home: An initial randomized trial of Internet-delivered Parent-Child Interaction Therapy (I-PCIT) Journal of Consulting and Clinical Psychology. 2017b;5(9):909–917. doi: 10.1037/ccp0000230. [DOI] [PubMed] [Google Scholar]
- Comer JS, Myers KM. Future directions in the use of telemental health to improve the accessibility and quality of children’s mental health services. Journal of Child and Adolescent Psychopharmacology. 2016;26:296–300. doi: 10.1089/cap.2015.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper-Vince C, Chou T, Furr JM, Puliafico AC, Comer JS. Videoteleconferencing early child anxiety treatment: A case study of the Internet-delivered CALM (I-CALM) Program. Evidence-Based Practice in Child and Adolescent Mental Health. 2016;1:24–39. doi: 10.1080/23794925.2016.1191976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Crum KI, Comer JS. Using synchronous videoconferencing to deliver family based mental health care. Journal of Child and Adolescent Psychopharmacology. 2016;26(3):229–234. doi: 10.1089/cap.2015.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan CL, March S. Online CBT for preschool anxiety disorders: A randomized control trial. Behaviour Research and Therapy. 2014;58:24–35. doi: 10.1016/j.brat.2014.05.001. [DOI] [PubMed] [Google Scholar]
- Doss BD, Feinberg LK, Rothman K, Roddy MK, Comer JS, et al. Using technology to enhance and expand interventions for couples and families: Conceptual and methodological considerations. Journal of Family Psychology. doi: 10.1037/fam0000349. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flannery-Schroeder EC, Kendall PC. Group and individual cognitive-behavioral treatments for youth with anxiety disorders: A randomized clinical trial. Cognitive Therapy and Research. 2000;24(3):251–278. doi: 10.1023/A:1005500219286. [DOI] [Google Scholar]
- Fung DS, Manassis K, Kenny A, Fiksenbaum L. Web-based CBT for selective mutism. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(2):112–113. doi: 10.1097/00004583-200202000-00003. [DOI] [PubMed] [Google Scholar]
- Gallo K, Comer JS, Barlow DH. Single case experimental designs and small pilot trial designs. In: Comer JS, Kendall PC, editors. The Oxford Handbook of Research Strategies for Clinical Psychology. New York, NY: Oxford University Press; 2013. [Google Scholar]
- Ginsburg GS, Becker EM, Keeton CP, Sakolsky D, Piacentini J, Albano AM, Compton SN, Iyengar S, Sullivan K, Caporino N, Peris T, Birmaher B, Rynn M, March J, Kendall PC. Naturalistic follow-up of youths treated for pediatric anxiety disorders. JAMA Psychiatry. 2014;71(3):310–318. doi: 10.1001/jamapsychiatry.2013.4186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green JG, Comer JS, Nadeau M, Donaldson A, Elkins RM, Reid G, Pincus DB. School functioning and use of school-based accommodations by treatment-seeking anxious children. Journal of Emotional and Behavioral Disorders. 2017;25(4):220–232. doi: 10.1177/1063426616664328. [DOI] [Google Scholar]
- Guy W, Bonato RR. Clinical Global Impressions. Chevy Chase, MD: National Institute of Mental Health; 1970. [Google Scholar]
- Higa-McMillan CK, Francis SE, Rith-Najarian L, Chorpita BF. Evidence base update: 50 years of research on treatment for child and adolescent anxiety. Journal of Clinical Child and Adolescent Psychology. 2016;45:91–113. doi: 10.1080/15374416.2015.1046177. [DOI] [PubMed] [Google Scholar]
- Hogendoorn SM, Prins PJ, Boer F, Vervoort L, Wolters LH, Moorlag H, Nauta MH, Hartman CA, de Haan E. Mediators of cognitive behavioral therapy for anxiety-disordered children and adolescents: Cognition, perceived control, and coping. Journal of Clinical Child and Adolescent Psychology. 2014;43(3):486–500. doi: 10.1080/15374416.2013.807736. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36:223–233. doi: 10.1037/0022-0167.36.2.223. [DOI] [Google Scholar]
- Howard B, Chu BC, Krain AL, Marrs-Garcia AL, Kendall PC. Cognitive Behavioral Family Therapy for Anxious Children: Therapist Manual. Second Edition. Workbook Publishing; 2000. [Google Scholar]
- Hughes AA, Lourea-Waddell B, Kendall PC. Somatic complaints in children with anxiety disorders and their unique prediction of poorer academic performance. Child Psychiatry and Human Development. 2008;39(2):211–220. doi: 10.1007/s10578-007-0082-5. [DOI] [PubMed] [Google Scholar]
- Jones DJ. Future directions in the design, development, and investigation of technology as a service delivery vehicle. Journal of Clinical Child and Adolescent Psychology. 2014;43:128–142. doi: 10.1080/15374416.2013.859082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JD, Forehand R, Cuellar J, Parent J, Honeycutt A, Khavjou O. Technology-enhanced program for child disruptive behavior disorders: Development and pilot randomized control trial. Journal of Clinical Child and Adolescent Psychology. 2014;43:88–101. doi: 10.1080/15374416.2013.822308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspectives on Psychological Science. 2011;6(1):21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, Crowley M, Breton S. Barriers to treatment participation scale: evaluation and validation in the context of child outpatient treatment. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 1997;38(8):1051–1062. doi: 10.1111/j.1469-7610.1997.tb01621.x. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology. 2008;76(2):282–297. doi: 10.1037/0022-006x.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Khanna MS, Edson A, Cummings C, Harris MS. Computers and psychosocial treatment for child anxiety: Recent advances and ongoing efforts. Depression and Anxiety. 2011;28:58–66. doi: 10.1002/da.20757. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Robin JA, Hedtke KA, Suveg C, Flannery-Schroeder E, Gosch E. Considering CBT with anxious youth? Think exposures. Cognitive and Behavioral Practice. 2005;12:136–150. doi: 10.1016/S1077-7229(05)80048-3. [DOI] [Google Scholar]
- Khanna MS, Kendall PC. Computer-assisted cognitive behavioral therapy for child anxiety: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2010;78(5):737–745. doi: 10.1037/a0019739. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry. 2006;63:484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- Langer DA, Wood JJ, Bergman RL, Piacentini JC. A multitrait-multimethod analysis of the construct validity of child anxiety disorders in a clinical sample. Child Psychiatry and Human Development. 2010;41(5):549–61. doi: 10.1007/s10578-010-0187-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(4):554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Barlow DH. The dissemination and implementation of evidence-based psychological treatments: A review of current efforts. American Psychologist. 2010;65:73–84. doi: 10.1037/a0018121. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Swendsen J, et al. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan AJ, Rapee RM, Salim A, Goharpey N, Tamir E, McLellan LF, Bayer JK. Internet-delivered parenting program for prevention and early intervention of anxiety problems in young children: Randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2017;56(5):417–425. doi: 10.1016/j.jaac.2017.02.010. [DOI] [PubMed] [Google Scholar]
- Myers K, Comer JS. Telemental health: Rectifying disparities in access to evidence-based mental health care. Journal of Child and Adolescent Psychopharmacology. 2016;26(3):186–191. doi: 10.1089/cap.2015.0055. [DOI] [PubMed] [Google Scholar]
- Myers KM, Nelson EL, Hilty DM, Rabinowitz T, Barwell SS, Bernard J, Boyce G, Cain S, Chui L, Comer JS, Cradock C, Varrell JR, Goldstein F, Johnston B, Krupinski EA, Lo K, Luxton D, McSwain D, McWilliams J, North S, Ostrowski J, Pignatiello A, Roth D, Turvey C, Wright S. American Telemedicine Association Practice Guidelines for Telemental Health with Children and Adolescents. Telemedicine and e-Health. 2017;23:779–804. doi: 10.1089/tmj.2017.0177. [DOI] [PubMed] [Google Scholar]
- Nelson EL, Barnard M, Cain S. Treating childhood depression over videoconferencing. Telemedicine Journal and e-Health. 2004;9(1):49–55. doi: 10.1089/153056203763317648. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus SC. National trends in outpatient psychoatherapy. American Journal of Psychiatry. 2010;167:1456–1463. doi: 10.1176/appi.ajp.2010.10040570. [DOI] [PubMed] [Google Scholar]
- Owens PL, Hoagwood K, Horwitz SM, Leaf PJ, Poduska JM, Kellam SG, Ialongo NS. Barriers to children’s mental health services. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(6):731–738. doi: 10.1097/00004583-200206000-00013. [DOI] [PubMed] [Google Scholar]
- Piacentini J, Bennett S, Compton SN, Kendall PC, Birmaher B, Albano AM, March J, Sherrill J, Sakolsky D, Ginsburg G, Rynn M, Bergman RL, Gosch E, Waslick B, Iyengar S, McCracken J, Walkup J. 24- and 36-week outcomes for the Child/Adolescent Anxiety Multimodal Study (CAMS) Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53(3):297–310. doi: 10.1016/j.jaac.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsawh HJ, Weisberg RB, Dyck I, Stout R, Keller MB. Age of onset, clinical characteristics, and 15-year course of anxiety disorders in a prospective, longitudinal, observational study. Journal of Affective Disorders. 2011;132(1-2):260–264. doi: 10.1016/j.jad.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A children’s global assessment scale (CGAS) Archives of General Psychiatry. 1983;40:1228–31. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Comer JS, Gonzalez J. Delivering parent-teen therapy for ADHD through videoconference: A preliminary investigation. Journal of Psychopathology and Behavioral Assessment. 2017;39(3):467–485. doi: 10.1007/s10862-017-9598-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for Children for DSM-IV: Child and parent versions. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Silverman WK, Ollendick TH. Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34:380–411. doi: 10.1207/s15374424jccp3403_2. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(8):937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Spence SH, Donovan CL, March S, Gamble A, Anderson RE, Prosser S, Kenardy J. A randomized controlled tial of online versus clinic-based CBT for adolescent anxiety. Journal of Consulting and Clinical Psychology. 2011;79(5):629–642. doi: 10.1037/a0024512. [DOI] [PubMed] [Google Scholar]
- Storch EA, Caporino NE, Morgan JR, Lewin AB, Rojas A, Brauer L, Murphy TK, et al. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Research. 2011;189(3):407–412. doi: 10.1016/j.psychres.2011.05.047. [DOI] [PubMed] [Google Scholar]
- Thompson-Hollands J, Kerns CE, Pincus DB, Comer JS. Parental accommodation of child anxiety and related symptoms: Range and impact. Journal of Anxiety Disorders. 2014;28(8):765–763. doi: 10.1016/j.anxdis.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigerland S, Lenhard F, Bonnert M, Lalouni M, Hedman E, Olén O, Ljótsson B, et al. Internet-delivered cognitive behavior therapy for children and adolescents: A systematic review and meta-analysis. Clinical Psychology Review. 2016;50:1–10. doi: 10.1016/j.cpr.2016.09.005. [DOI] [PubMed] [Google Scholar]
- Vigerland S, Serlachius E, Thulin U, Andersson G, Larsson JO, Ljotsson B. Long-term outcomes and predictors of internet-delivered cognitive behavioral therapy for childhood anxiety disorders. Behaviour Research and Therapy. 2017;90:67–75. doi: 10.1016/j.brat.2016.12.008. [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, Ivengar S, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359(26):2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner CL, Elkins RM, Pincus DB, Comer JS. Anxiety sensitivity and sleep-related problems in anxious youth. Journal of Anxiety Disorders. 2015;32:66–72. doi: 10.1016/j.janxdis.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood KK, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. Journal of Clinical Child and Adolescent Psychology. 2002;31(3):335–42. doi: 10.1207/153744202760082595. [DOI] [PubMed] [Google Scholar]
- Wu P, Goodwin R, Comer JS, Hoven C, Cohen P. The relationship between anxiety disorders and substance use among adolescents in the community: Specificity and gender differences. Journal of Youth and Adolescence. 2010;39:177–188. doi: 10.1007/s10964-008-9385-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


