Abstract
Background:
From 2012 to 2014, rates of congenital syphilis increased in Louisiana and Florida. We evaluated the effectiveness of early (first or second) and third trimester syphilis screening for the prevention of congenital syphilis in these high-morbidity states.
Methods:
Reported syphilis cases among pregnant women in Louisiana and Florida during January 1, 2013, to December 31, 2014, were reviewed for documented screening for syphilis in the first 2 trimesters and third trimester. Pregnant women with syphilis were linked to congenital syphilis records and stratified by whether the pregnancy led to a reported congenital syphilis case.
Results:
Seven hundred ten pregnant women with syphilis in Louisiana and Florida were linked to 155 congenital syphilis cases. Three hundred seventy (52%) pregnant women with syphilis were staged as early syphilis (n = 270) or high-titer late or unknown duration-latent syphilis (n = 100), and 109 (70% of the total) were linked to congenital syphilis cases. Screening in the first 2 trimesters identified 513 pregnant women who tested positive for syphilis, and 470 (92%) potential congenital syphilis were averted. One hundred nine pregnant women tested positive for syphilis in the third trimester, and 85 (78%) had babies without congenital syphilis. During their pregnancy, 85 (12%) women tested negative at least once, and 55 (65%) had babies with congenital syphilis. Thirty-nine women had no reported syphilis screening 30 days or longer before delivery.
Conclusions:
Screening for syphilis both early and in the third trimester prevented many pregnant women with syphilis from having a baby with congenital syphilis. Preventing all congenital syphilis would likely require preventing all syphilis among women.
Congenital syphilis (CS) is a sentinel event suggesting failure of the public health and health care systems. The consequences may be severe. Untreated syphilis during pregnancy can lead to fetal or infant death in up to 40% of cases.1,2 Rates of CS had been declining for most of the 1990s and 2000s, but began to increase after 2012, reaching 11.6 reported cases per 100,000 live births in 2014, the highest rate since 2001.2–3 Between 2012 and 2014, rates of CS increased in Louisiana (LA) (from 52.7 to 73.4 cases per 100,000 live births) and Florida (FL) (from 17.4 to 22.1 cases per 100,000 live births).3,4
The United States Preventative Services Task Force and the Centers for Disease Control and Prevention (CDC) recommend screening pregnant women for syphilis during their first prenatal visit. Screening again in the third trimester is promoted for women at increased risk for acquiring syphilis.5,6 Florida Administrative Code states that practitioners should test pregnant women for syphilis at initial examination for each pregnancy and at 28 to 32 weeks gestation.7 Louisiana passed similar rules and regulations for syphilis testing among pregnant women in June 2014.8
Despite United States Preventative Services Task Force and CDC recommendations and state-level legislation, failure to screen at first visit and failure to rescreen early in the third trimester of pregnancy are major contributors to the rising rates of CS in the United States.9–11 The benefit of third-trimester screening is highly dependent on the local incidence of syphilis among women.12,13 Even in areas where third-trimester screening is recommended it has been often been implemented at low rates. One study in Miami found that only 11% of women were being rescreened in the third trimester and another study from Texas found only 5 of 31 providers were routinely screening twice during pregnancy.14,15
Many studies of CS focus on describing pregnancies that led to CS, and do not describe pregnancies where screening and treatment prevented CS.9–11 One study among pregnant women with reactive nontreponemal tests (including those who were previously treated) found that earlier access to prenatal care and increasing prenatal visits decreased the odds that the pregnancy would result in a CS case.16 Another study compared infected pregnant women who did or did not complete treatment, but it did not report on success preventing CS.17 Appropriate treatment of pregnant women with syphilis has been found to be 98% effective in preventing CS.18,19 Assessing maternal syphilis cases that did and did not lead to CS can help determine the impact of screening and appropriate timely treatment on preventing cases of CS.
The aims of this investigation were to describe maternal and CS in 2 high-morbidity state programs, elucidate the effects of interventions, and identify opportunities for prevention of CS.
MATERIALS AND METHODS
In LA and FL, all women of child-bearing age who have syphilis are assigned for further investigation to determine if the women are pregnant. Pregnancy can be determined by reviewing laboratory reports, provider reports, but was most often identified during interviews by disease intervention specialists. Women were classified as pregnant, not pregnant, or unknown pregnancy status.
We reviewed records from all women classified as pregnant who were reported to have syphilis in LA and FL between January 1, 2013, and December 31,2014. Deidentified data were extracted from each state’s sexually transmitted disease (STD) surveillance system, Patient Reporting Investigation Surveillance Manager (PRISM). All data submitted to PRISM are part of routine STD surveillance activities. The CDC determined this project was research that does not involve identifiable human subjects.
Birth outcomes for the women were determined by linking to records of their infants who had been assessed for possible CS as defined by the Council of State and Territorial Epidemiologists (CSTE).20 Pregnant women diagnosed with syphilis were stratified into 2 groups: the CS group and the non-CS group, based on whether or not their infants met the CSTE surveillance case definition for CS. Three pregnant women and their infants from LA were excluded because there was conflicting information related to the case definition. Maternal-to-CS case ratios were calculated using the total number of maternal cases in a given category divided by the number of CS cases in the same category.
Case management and disease investigation records within PRISM from each pregnant woman with syphilis were examined to determine the stage of syphilis.20 Primary, secondary, and early-latent syphilis cases were considered to be “early syphilis” infections that were likely to have been acquired within the preceding year. Late or unknown duration-latent syphilis was a latent infection without sufficient information to be staged as early syphilis, so it was considered likely to have been acquired more than 1 year before diagnosis.
Additional variables extracted for each maternal syphilis case included: mother’s age in years, race and ethnicity, maximum rapid plasma reagin (RPR) titer associated with the reported case, human immunodeficiency virus status, self-reported drug use, syphilis screening history, treatment status of the mother (for her stage of syphilis), and self-reported prior history of STDs. Race and ethnicity were extracted directly from each state’s PRISM system, and categorized in 4 groups: white non-Hispanic, black non-Hispanic, Hispanic or Latino, and other or unknown. The maximum RPR titer for each woman for the current episode of syphilis was categorized as high titer (≥1:32), medium titer (from 1:4 through 1:16), or low titer (≤1:2). Records in FL were reviewed to identify women born outside of the United States (this variable was not captured in LA). Screening history was based on syphilis test results reported within PRISM. To determine when in the course of the pregnancy screening occurred, sample collection dates were compared with the estimated due dates (EDD), or delivery date when the EDD was not available. Screening was considered to be in the first 2 trimesters if the mother was tested in the first 27 weeks of pregnancy (≥91 days from EDD). Third-trimester screening was after 27 weeks of pregnancy (<91 days from EDD) but also 30 days or longer before delivery. Testing less than 30 days before delivery was not considered to be third-trimester screening because treatment less than 30 days before delivery is not be considered sufficient to prevent all cases of CS and their infants would meet the CSTE case definition.
RESULTS
From January 1, 2013, to December 31, 2014, there were 562,569 live births (127,470 in LA and 435,099 in FL).21,22 A total of 3,497 syphilis cases among women (LA 1,558 and FL 1,939) were reported during January 1, 2013, to December 31, 2014. Pregnancy status was reported for 2621 (75%) female syphilis cases (LA, 870 of 1558 [56%] and FL, 1751 of 1939 [90%]), and 710 syphilis infections during pregnancy were reported (LA, 304 and FL, 406) (Table 1). Two women were infected twice and were each counted twice. Among women with syphilis, 20.3% were known to be pregnant (LA, 19.5% and FL, 20.9%). One hundred fifty-five (22%) of them were linked to CS cases, with 72 reported in LA and 83 reported in FL, including 5 stillbirths (1 in LA and 4 in FL) and 5 infants that were born alive and then died (2 in LA and 3 in FL). Thus, for every 4.6 pregnant women with syphilis, there was 1 case of CS (4.2 for LA and 4.8 for FL).
TABLE 1.
Characteristic of Maternal Syphilis Cases Reported in LA and FL, 2013–2014
| Early Syphilis | Late Latent | All Syphilis | |||||
|---|---|---|---|---|---|---|---|
| Characteristics | CS* (%) | Non-CS* (%) | CS* (%) | Non CS* (%) | CS* (%) | Non CS* (%) | All (%) |
| State of residence | |||||||
| FL | 47 (60) | 115 (60) | 36 (47) | 208 (57) | 83† (54) | 323 (58) | 406 (57) |
| LA | 31 (40) | 77 (40) | 41 (53) | 155 (43) | 72† (46) | 232 (42) | 304 (43) |
| Race/ethnicity | |||||||
| White non-Hispanic | 16 (20) | 28 (15) | 10 (13) | 36 (10) | 26 (17) | 64 (12) | 90 (13) |
| Black non-Hispanic | 54 (69) | 137 (71) | 57 (74) | 235 (65) | 111 (72) | 372 (67) | 484 (68) |
| Hispanic/Latino | 6 (8) | 19 (10) | 7 (9) | 59 (16) | 13 (8) | 78 (14) | 91 (13) |
| Other/unknown | 2 (3) | 8 (4) | 3 (4) | 33 (9) | 5 (3) | 41 (7) | 46 (6) |
| US Territory/Foreign Born‡ | |||||||
| Yes | 10 (21) | 22 (19) | 11 (31) | 87 (42) | 21 (25) | 109 (34) | 130 (32) |
| No | 37 (79) | 93 (81) | 25 (69) | 121 (58) | 62 (75) | 214 (66) | 276 (68) |
| Max titer§ | |||||||
| High (≥1:32) | 38 (49) | 98 (51) | 31 (40) | 69 (19) | 69 (45) | 167 (31) | 236 (34) |
| Medium (1:4–1:16) | 26 (34) | 67 (35) | 30 (39) | 147 (41) | 56 (37) | 214 (39) | 270 (38) |
| Low (≤1:2) | 13 (17) | 26 (14) | 15 (20) | 140 (39) | 28 (18) | 166 (30) | 194 (28) |
| History of prior STD | |||||||
| Yes | 44 (56) | 102 (53) | 32 (42) | 130 (36) | 76 (49) | 232 (42) | 308 (43) |
| No | 26 (33) | 74 (39) | 37 (48) | 199 (55) | 63 (41) | 273 (49) | 336 (48) |
| Unknown | 8 (10) | 16 (8) | 8 (10) | 34 (9) | 16 (10) | 50 (9) | 66 (9) |
| Total | 78 (100) | 192 (100) | 77 (100) | 363 (100) | 155 (100) | 555 (100) | 710 (100) |
CS = maternal case linked to a CS case. Non-CS = maternal case not linked to a CS case.
In LA and FL, 1 maternal syphilis infection was linked to 2 CS cases (multiple birth).
This variable was not captured in LA; numbers are presented for FL only.
In FL, 1 titer was missing for an early maternal syphilis case linked to a CS case. In LA, 1 titer was missing for a late-latent maternal syphilis case linked to a CS case and 8 titers were missing for maternal syphilis case linked to non-CS cases (1 early syphilis and 7 late-latent syphilis).
In both jurisdictions, African Americans accounted for the majority of maternal syphilis infections (68%) and maternal syphilis cases that resulted in CS (72%). These percentages were higher in LA at 88% for both maternal infections and for maternal cases that resulted in a congenital case. A higher percentage of pregnant women with syphilis were Hispanic in FL (20%) compared to LA (3%). Thirty percent of births in Florida are to foreign-born women23 and nearly one third of all pregnant women with syphilis in FL were foreign-born (a variable not collected in LA’s PRISM system). About 38% (n = 270) of pregnant women with syphilis had early syphilis (8 had primary, 54 had secondary, and 208 had early latent). Half (n = 79) of the CS cases were linked to women with early syphilis. Another 20% (n = 31) of CS cases were linked to pregnant women with high-titer late latent syphilis (RPR titer ≥ 1:32) which suggests that the women were recently infected. The remaining 30% (n = 45) of CS cases were linked to pregnant women with medium- or low-titer late latent syphilis. Babies were more likely to have CS iftheir mothers had high titers (69 of 167, 41.3%) than if they had medium or low titers (84 of 380 [22.1%], P = 0.001.
During 2013 to 2014, 555 potential CS cases were prevented (78% of potential cases which could have resulted from 710 syphilis infections among pregnant women) by appropriately treating pregnant women who had syphilis (232, 76% in LA and 323, 80% in FL) (Fig. 1).
Figure 1.
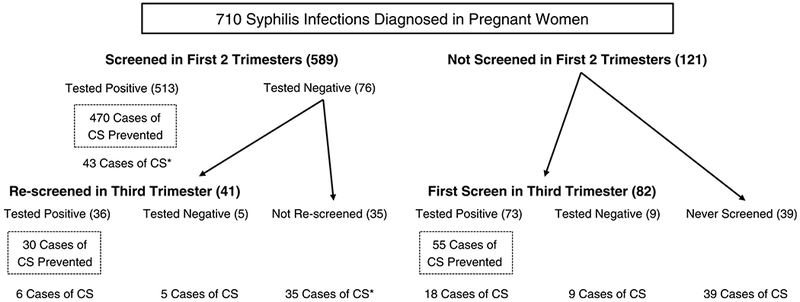
Documented syphilis screening during pregnancy for 710 syphilis infections among pregnant women in Louisiana and Florida, 2013–2014 and whether the case resulted in a CS case.
Early screening for syphilis in the first 2 trimesters occurred for 589 (83%) of all maternal syphilis cases. Of these, 513 (87%) tested positive for syphilis at this screening, and after timely and appropriate treatment, 470 (92% of those testing positive in the first 2 trimesters) avoided CS. Treatment of syphilis detected during the first 2 trimesters was equally effective in preventing CS for women with early syphilis (140 of 152,92%) and women with late or unknown duration syphilis (310 of 343, 90%).
Third-trimester screening for syphilis was reported for 41 (33%) women who had tested negative in the first 2 trimesters and 82 (67%) who did not have a prior reported syphilis test for a total of 123 tests. Of those 123 tests, 109 (89%) tested positive at the third trimester screen and 85 (78%) of them delivered babies who did not have CS. Of 710 maternal syphilis cases 39 (5%) had no reported syphilis testing during pregnancy that was at least 30 days before delivery. Eighty-five women tested negative at least once during pregnancy, and 55 (65%) of them had babies with CS (6 + 5 + 35 + 9 in Fig. 1).
One difference between LA and FL was the success in preventing CS cases by screening for the first time in the third trimester; medical providers in LA prevented 64% (27 of 42) and FL prevented 90% (28 of 31). Many of the cases in LA had been tested at the end of the third trimester and were not treated 30 days or longer before delivery.
In total, 41 (26%) infants with CS were reported as having one or more of the following outcomes: laboratory confirmation of Treponema pallidum by dark field microscopy (n = 1), stillbirth (n = 5), signs and symptoms consistent with CS (n = 4), abnormal long-bone x-rays (n = 11), or abnormal cerebral spinal fluid (CSF) findings (n = 26) including elevated protein (n = 19) or pleocytosis, greater than 15 white blood cells per mm3 (n = 9).
Nearly 30% of all CS cases were among pregnant women who tested positive in the first 2 trimesters. These cases were not prevented for a variety of reasons including: pregnant women who refused treatment (n = 4), had insufficient treatment for late or unknown duration syphilis (n = 13), were reinfected during pregnancy (n = 13), or infants who met the CS surveillance case definition despite appropriate treatment of their mother (n = 8). Nearly 50% of the reported CS cases were the result of 1 of 1 scenarios: (1) pregnant women who had no recorded syphilis testing (usually they had no prenatal care) [n = 39] and (2) pregnant women that tested negative for syphilis in the first 2 trimesters, and were not rescreened early in the third trimester (n = 35) (Table 2). Lastly, 27 cases of CS were identified among pregnant women screened for the first time in the third trimester. Most of these were either mothers who tested negative and then seroconverted at or around delivery (n = 9) or pregnant women who were not treated at least 30 days before delivery (n = 9). Among the 14 women who tested negative in the third trimester and then seroconverted at or around delivery, none had a previous history of syphilis.
TABLE 2.
Criteria for CS Cases in LA and FL, 2013–2014
| Criteria for Meeting the CS Case Definition | Total (%) |
|---|---|
| Screened during first 2 trimesters | 89 (57) |
| Tested positive for syphilis | 43 (28) |
| Mother was reinfected (4-fold titer increase) after initial treatment | 13 (8) |
| Insufficient treatment for stage of disease | 13 (8) |
| Treated appropriately infant met surveillance case definition | 8 (5) |
| Patient refused treatment | 4 (3) |
| Premature birth screened < 30 d before delivery* | 3 (2) |
| Mother treated <30 d before delivery | 2 (1) |
| Tested negative for syphilis | 46 (30) |
| Not rescreened >30 d before delivery, (1 was born before third trimester)* | 35 (23) |
| Negative third-trimester screening | 5 (3) |
| Third-trimester screen positive, treated < 30 d before delivery | 4 (3) |
| Third-trimester screen positive, four-fold titer increase at delivery | 2 (1) |
| Screened after the first 2 trimesters, but > 30 d before delivery | 27 (17) |
| Tested positive for syphilis | 18 (12) |
| Treated <30 d before delivery | 9 (6) |
| Mother not treated | 4 (3) |
| Born prematurely, treatment <30 d before delivery | 4 (3) |
| Treated appropriately infant met surveillance case definition | 1 (1) |
| Tested negative for syphilis | 9 (6) |
| No recorded syphilis testing more than 30 d before delivery | 39 (25) |
| Total | 155 (100) |
For pregnant women diagnosed with syphilis that delivered twins, only 1 case of CS was included.
Ultimately, 579 (82%) pregnant women with syphilis received sufficient treatment at least once during their pregnancy. Of these, 555 (96%) did not result in a case of CS. Among the 24 (4%) women who were sufficiently treated and still had a baby with CS, 15 had serologic test results that suggested reinfection during pregnancy and 9 were adequately treated and still had infants that met the case definition. Among these 9 women: 6 had late or unknown duration syphilis and 3 had early latent syphilis; 8 had nontreponemal titers of 1:32 or greater and one had a titer of 1:16; the first positive test for syphilis was in the second trimester or later for 7; and their infants met the case definition by having either elevated CSF white blood cells or protein without another known cause (n = 6), abnormal long bone x-rays consistent with CS (n = 2), or a reactive CSF Venereal Disease Research Laboratory test (n = 1).
DISCUSSION
Most potential cases of CS were prevented in LA and FL by prenatal screening, case management, and timely treatment. The majority of pregnant women with syphilis had early or late or unknown duration-latent syphilis with a high titer (≥ 1:32 RPR), suggesting that without treatment their newborns would be infected. The likelihood of vertical transmission in early syphilis is nearly 100%.10,24 Early screening, rescreening, and timely appropriate treatment of maternal syphilis cases is instrumental in preventing CS9,15,17,25
Our results demonstrate that CS cases were prevented chiefly by screening pregnant women during the first 2 trimesters and effectively treating women who tested positive. It is clear that appropriate intervention in the first 2 trimesters of pregnancy can prevent most cases of CS in infants in LA and FL. Other studies have shown that screening and timely treatment for maternal syphilis not only prevents CS cases but also represents a positive return on investment from a cost or benefit perspective.26–29
Screening for syphilis among women in the third trimester prevented fewer CS cases, but is worthwhile in these high-morbidity areas. Moreover, it was still fairly effective because most of the infected pregnant women that were screened and treated early in the third trimester had babies that did not have CS. Models suggest universal third-trimester screening for syphilis in the United States would not be economically beneficial in areas with low morbidity.12 However, in high-morbidity areas where third-trimester testing is cost-effective and required by law, it is often underused.14,16,28 Given the high levels of morbidity, continuing to recommend and promote third-trimester screening in LA and FL could prevent additional CS cases and be economically viable.12,25
Some pregnant women with syphilis delivered babies with CS despite screening regulations requiring early and third-trimester screening for pregnant women. Small numbers of women were: never screened for syphilis at least 30 days before delivery; tested negative in the first 2 trimesters and were not rescreened; or developed syphilis after testing negative in the third trimester. As we demonstrate here, prior studies have consistently found some CS cases related to lack of prenatal care, imperfect screening or treatment, and infections that occur near delivery.9–11,14,15,29 Eliminating CS requires timely detection and treatment of syphilis in pregnant women, prevention of unintended pregnancies in women at risk of syphilis and, ultimately, the prevention of syphilis among women and their partners.25,30
Although timely treatment for syphilis in pregnancy is highly effective for preventing CS, this study identified 9 potential treatment failures. Previous studies found treatment failure was more likely when women had secondary syphilis, high-titer nontreponemal tests, or a short interval from treatment to delivery.18,19,31 Our small number of potential treatment failures were identified among pregnant women with early latent and late or unknown duration syphilis and nearly all had high-titer RPRs. Additional studies with larger numbers are needed to further elucidate the possible causes of treatment failures.
Our analysis suffers from many of the same difficulties that accompany studies using passive public health surveillance, including potential missing or incomplete data from patients or providers on some reported cases.3,10,14,27 Our data did not include sufficient detail to allow us to identify among women with no reported syphilis if they had received no prenatal care or were not screened despite prenatal visits. Differences in prevalence of syphilis, access to health care, public health services, and other social determinants of health that impact CS may limit the generalizability of this analysis to other areas. In addition, changes to LA rules and regulations regarding testing of pregnant women for syphilis throughout the course of their pregnancy were implemented during the study period. This may be why some mothers with syphilis were not being rescreened in the third trimester, but the data from FL and other studies also demonstrate missed opportunities for third-trimester screening among providers.11,14,15
Pregnancy status ascertainment for women with syphilis enables appropriate public health action to prevent CS and was missing for many women in LA. However, each state had a similar proportion of female syphilis cases that were identified as pregnant, so it is likely that pregnancy status was reported more often when women were pregnant than when they were not. An improvement in pregnancy status ascertainment by these programs could assess the validity of this assumption. When looking at the most severe outcome of CS, stillbirths and miscarriages, we do not expect to have underreporting of these outcomes among pregnant women diagnosed with syphilis during their pregnancy. However, among pregnant women with stillbirths, testing for syphilis may be underused and therefore, CS stillbirths may be underreported. Throughout most of the analysis, LA and FL were very similar. However, 1 major difference between programs was in the racial and ethnic demographics of maternal syphilis cases. Much of this difference is likely due to difference in each state’s demographics, but foreign-born pregnant women diagnosed with syphilis, especially those arriving in FL during their pregnancy, may provide additional challenges in CS case prevention. Thus, understanding which populations within an area are at greatest risk for acquiring syphilis can aid in developing and implementing interventions.11,15,16
This analysis highlights the ability to prevent many cases of CS and the difficulty in preventing all of them. Most CS can be prevented by the coordinated efforts of clinicians and public health programs to ensure appropriate screening, timely treatment, partner treatment, and appropriate evaluation and treatment for the infants.3,9,10,14,24,27–31 Eliminating all CS will require prevention of syphilis in all women.
Acknowledgments:
The authors would like to acknowledge all of the disease intervention specialists and staff who completed these maternal and congenital syphilis investigations in LA and FL. Without their effort and follow-up this analysis would not have been possible. In addition, we acknowledge Gayle Keller, Florida Department of Health, in assisting with data extraction for FL.
Footnotes
Publisher's Disclaimer: Disclaimer: The findings, opinions, and conclusions expressed by authors contributing to this journal do not necessarily reflect the official position of the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
Conflicts of interest and source of funding: None declared.
REFERENCES
- 1.Beltrami J, Berman S. Congenital syphilis: A persisting sentinel public health event. Sex Transm Dis 2006; 33:675–676. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Syphilis among infants down more than half in three years. Available at: http://www.cdc.gov/stopsyphilis/media/presscsyph7-2001.htm. Retrieved August 23, 2016.
- 3.Bowen V, Su J, Torrone E, et al. Increases in incidence of congenital syphilis—United States, 2012–2014. MMWR Morb Mortal Wkly Rep 2015; 64:1241–1245. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2014. Atlanta: U.S.: Department of Health and Human Services; 2015. [Google Scholar]
- 5.U.S. Preventive Services Task Force. Screening for syphilis infection in pregnancy: U.S. Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med 2009; 150:705–709. [DOI] [PubMed] [Google Scholar]
- 6.Workowski KA, Bolan GA, Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015; 64(RR-03):34–51. [PMC free article] [PubMed] [Google Scholar]
- 7.64D Florida Adm. Code 3.042. 2006.
- 8.Louisiana Acts 2014, No. 459, eff. June 4, 2014.
- 9.Warner L, Rochat RW, Fichtner RR, et al. Missed opportunities for congenital syphilis prevention in an urban southeastern hospital. Sex Transm Dis 2001; 28:92–98. [DOI] [PubMed] [Google Scholar]
- 10.Patel SJ, Klinger EJ, OʼToole D, et al. Missed opportunities for preventing congenital syphilis infection in New York City. Obstet Gynecol 2012; 120:882–888. [DOI] [PubMed] [Google Scholar]
- 11.Taylor MM, Mickey T, Browne K, et al. Opportunities for the prevention of congenital syphilis in Maricopa County, Arizona. Sex Transm Dis 2008; 35:341–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Albright CM, Emerson JB, Werner EF, et al. Third trimester prenatal syphilis screening: A cost-effectiveness analysis. Obstet Gynecol 2015; 126:479–485. [DOI] [PubMed] [Google Scholar]
- 13.Shiber L, Todia WJ. Cost and clinical utility of repeated syphilis screening in the third trimester in a high-risk population. Am J Obstet Gynecol 2014; 210:e1–e5. [DOI] [PubMed] [Google Scholar]
- 14.Trepka MJ, Bloom SA, Zhang G, et al. Inadequate syphilis screening among women with prenatal care in a community with a high syphilis incidence. Sex Transm Dis 2006; 33:670–674. [DOI] [PubMed] [Google Scholar]
- 15.Southwick KL, Guidry HM, Weldon MM, et al. An epidemic of congenital syphilis in Jefferson County, Texas, 1994–1995: Inadequate prenatal syphilis testing after an outbreak in adults. AmJ Public Health 1999; 89:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mobley JA, McKeown RE, Jackson KL, et al. Risk factors for congenital syphilis in infants of women with syphilis in South Carolina. Am J Public Health 1998; 88:597–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhu L, Qin M, Du L, et al. Maternal and congenital syphilis in Shanghai, China, 2002 to 2006. Int J Infect Dis 2010; 14(Suppl 3): e45–e48. [DOI] [PubMed] [Google Scholar]
- 18.Alexander JM, Sheffield JS, Sanchez PJ, et al. Efficacy of treatment for syphilis in pregnancy. Obstet Gynecol 1999; 93:5–8. [DOI] [PubMed] [Google Scholar]
- 19.Wendel GD Jr, Sheffield JS, Hollier LM, et al. Treatment of syphilis in pregnancy and prevention of congenital syphilis. Clin Infect Dis 2002; 35(Suppl 2):S200–S209. [DOI] [PubMed] [Google Scholar]
- 20.Council of State and Territorial Epidemiologists. Update to public health reporting and national notification for syphilis. Available at: http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PS/13-ID-04.pdf. Retrieved October 3, 2016.
- 21.Louisiana Department of Health. State registrar & vital records: Birth data. Available at: http://new.dhh.louisiana.gov/index.cfm/page/704. Retrieved January 31, 2017.
- 22.Florida Department of Health. Florida vital statistics annual report 2015. Tallahassee, FL: Florida Department of Health; 2016. [Google Scholar]
- 23.Florida Department of Health. Florida Birth Query System. Available at: http://www.flhealthcharts.com/FLQUERY/Birth/BirthRpt.aspx. Retrieved March 23, 2017.
- 24.Berman S Maternal syphilis: pathophysiology and treatment. Bull World Health Organ 2004; 82:433–438. [PMC free article] [PubMed] [Google Scholar]
- 25.Hong FC, Liu JB, Feng TJ, et al. Congenital syphilis: an economic evaluation of a prevention program in China. Sex Transm Dis 2010; 37:26–31. [DOI] [PubMed] [Google Scholar]
- 26.Schmid G Economic and programmatic aspects of congenital syphilis prevention. Bull World Health Organ 2004; 82:402–409. [PMC free article] [PubMed] [Google Scholar]
- 27.Stray-Pedersen B Economic evaluation of maternal screening to prevent congenital syphilis. Sex Transm Dis 1983; 10:167–172. [DOI] [PubMed] [Google Scholar]
- 28.Desenclos JC, Scaggs M, Wroten JE. Characteristics of mothers of live infants with congenital syphilis in Florida, 1987–1989. Am J Epidemiol 1992; 136:657–661. [DOI] [PubMed] [Google Scholar]
- 29.Schrag SJ, Arnold KE,Mohle-Boetani JC, et al. Prenatal screening for infectious diseases and opportunities for prevention. Obstet Gynecol 2003; 102:753–760. [DOI] [PubMed] [Google Scholar]
- 30.Gust DA, Levine WC, St Louis ME, et al. Mortality associated with congenital syphilis in the United States, 1992–1998. Pediatrics 2002; 109:e79. [DOI] [PubMed] [Google Scholar]
- 31.Sheffield JS, Sanchez PJ,Morris G, et al. Congenital syphilis after maternal treatment for syphilis during pregnancy. Am J Obstet Gynecol 2002; 186:569–573. [DOI] [PubMed] [Google Scholar]


