Abstract
Background and Objectives:
Laparoscopic hysterectomy poses the risk of lower urinary tract injury, and intraoperative recognition of urinary tract injury is often difficult. We sought to evaluate sodium fluorescein coloration of ureteral jets during cystoscopy after laparoscopic hysterectomy and to evaluate surgeons' satisfaction with this method of injury detection.
Methods:
This was an observational study, in which data were collected prospectively. A total of 30 women who underwent laparoscopic hysterectomy from August 2016 to February 2017 at the Centre Hospitalier de l'Université Laval (CHUL) de Québec. Twenty-five milligrams of 10% intravenous sodium fluorescein was administered after vaginal cuff closure. Cystoscopy was then systematically performed, and the time to visualization (time from injection to coloration of ureteral jet), the quality of coloration, and the duration of cystoscopy were recorded. Side effects were systematically recorded and rigorously analyzed.
Results:
Most frequent indications for hysterectomy were fibroids and endometriosis with uterine weight from 76 to 885 g. Ninety-three percent of patients (n = 28) had bilateral ureteral jet coloration, whereas 1 patient had no coloration bilaterally, and another patient had a complete unilateral obstruction immediately diagnosed and resolved intraoperatively after removal of the vaginal sutures. In 90% of cases (n = 27), surgeons were highly satisfied with the use of sodium fluorescein. The average time between visualization of both left and right ureteral jets was 1 minute. Side effects included hypotension (n = 3) and yellow coloration of urine (n = 15).
Conclusion:
Our study suggests that sodium fluorescein is an effective dye for documenting ureteral patency and improving visualization of ureteral jets during cystoscopy upon completion of laparoscopic hysterectomy.
Keywords: Cystoscopy, Laparoscopic hysterectomy, Sodium fluorescein, Ureteral jets
INTRODUCTION
Lower urinary tract injuries are serious potential complications of laparoscopic hysterectomy. Gynecological surgery is responsible for 75% of iatrogenic trauma of the ureter.1 When these complications occur, they may lead to hospitalization, additional surgical interventions, long-term sequelae, and deterioration of quality of life, and such occurrences may have medicolegal implications.2,3
Intraoperative recognition of urinary tract injury is often difficult, with only 10 to 15% of ureteral injuries detected.1,2,4 Performing a systematic diagnostic cystoscopy at the end of the intervention improves timely diagnosis and treatment of ureteral injury; however, up to 10% of ureteral injuries remain unidentified.3 Intraoperative management of urinary tract injury often consists of simple removal and replacement of sutures used for vaginal cuff closure.3 Several professional associations recommend systematic cystoscopy after pelvic surgery to improve timely diagnosis of ureteral injuries.4,5
Intraoperative cystoscopy is a simple technique that allows diagnosis of most urinary tract injuries.2–4,6 During cystoscopy, ureteral patency and absence of bladder trauma are evaluated. Nevertheless, visual assessment of ureteral jet can be challenging, and intravenous dye can improve detection2,7 by allowing diagnosis of complete (absence of coloration) or partial (delayed coloration) ureteral obstruction.6,7 Indigo carmine was commonly used8 until a shortage arose in June 2014, and it still remains unavailable in some countries, including Canada.9–11
As a result, different alternatives have been considered for the purpose of substitution. Sodium fluorescein, recently proposed by Doyle et al,12 is injected intravenously and is followed by visualization of brilliant yellow ureteral jets. Sodium fluorescein is frequently used in other disciplines such as ophthalmology and neurosurgery and appears to be well tolerated.13–18
The primary objective of our study was to assess the quality of ureteral jet visualization during cystoscopy after laparoscopic hysterectomy with the use of sodium fluorescein. Secondary objectives included assessment of surgeons' satisfaction and the overall safety of the drug.
METHODS
The Ethics Research Committee of the CHU de Québec–Université Laval (2016-2869) and Health Canada (HC6-24-c191987) approved the study protocol. Our study was registered on ClinicalTrials.gov (NCT02971800). This prospective, observational, single-center study was conducted August 2016 to February 2017. During the study period, we recruited women who underwent laparoscopic hysterectomy for benign conditions.
To be included in the study, patients had to be 18 years of age and older with normal kidney function (glomerular filtration rate >60 mL/min per 1.73m2) and had to provide informed consent. Patients with a diagnosis of cancer or sodium fluorescein hypersensibility or intolerance, who were breastfeeding, or who were taking probenecid, digoxin, quinidine, or β-blockers were excluded from study participation. Patients were enrolled during the preoperative consultation after signing the study consent.
Twenty-five milligrams of 10% intravenous sodium fluorescein (0.25 mL) was administered near the end of the laparoscopic hysterectomy, during suturing of the vaginal cuff. Doyle et al12 evaluated and demonstrated that the minimum dose of fluorescein sodium required for optimal visualization of the ureteral jet was 25 mg, and, at this dose, no side effects had been reported. After administration, the infusion lines were thoroughly flushed with 10 mL of saline solution, and the absence of sodium fluorescein extravasation at the injection site was verified. Cystoscopy was systematically performed within 5 minutes after injection of the dye. Three surgeons participated in the study.
The main outcome criteria were the coloration of the ureteral jets (very colored, somewhat colored, or not colored), and the satisfaction of the surgeons (highly satisfied, satisfied, or not satisfied). The time from injection to coloration, the time between appropriate visualization of the 2 colored jets (right and left), the turbulence of the jets, and the duration of the procedure were also recorded.
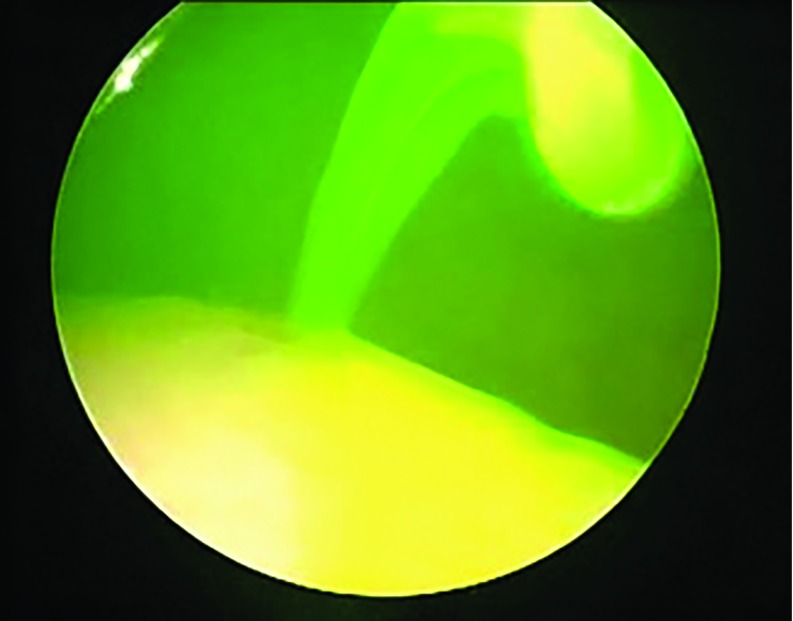
Figure 1 shows ureteral jet coloration during cystoscopy after injection of 25 mg 10% sodium fluorescein.
Figure 1.
Ureteral jet during cystoscopy after injection of 25 mg of 10% sodium fluorescein.
Side effects were systematically and rigorously recorded and analyzed up to 2 months after surgery. Early side effects were evaluated by the medical staff during the hospitalization, with particular attention to nausea and vomiting, hypersensibility, skin eruption, yellow skin coloration, pruritus, hypotension, and circulatory collapse. Short-term side effects were evaluated by a self-administered questionnaire during the first 48 h. Postoperative consultation at 2 months allowed review of any delayed side effects.
An interim analysis was performed early in the trial after 5 patients were enrolled, to ensure that the dose of 25 mg was sufficient to visualize the ureteral jets.
Statistical analyses were performed with Excel 9.0 (Microsoft, Redmond, Washington, USA). Population characteristics and outcomes were described as means ± SD and frequencies.
RESULTS
During the study period, 32 women who underwent a laparoscopic hysterectomy for benign conditions were identified, of which 30 were eligible. Two patients were excluded from study participation: 1 after surgery and cystoscopy with sodium fluorescein related to conversion to laparotomy in the context of voluminous fibroids and the other for taking a medication that was not permitted (ophthalmic β-blockers). Patient demographics and other patient-related relevant information are reflected in Table 1.
Table 1.
Clinical Characteristics
| Characteristic | Data |
|---|---|
| Age (yr) mean ± SD | 47 ± 5 |
| BMI (kg/m2) mean ± SD | 24.5 ± 4 |
| Caucasian, n (%) | 30 (100) |
| Indications n (%) | |
| Fibroids | 18 (60) |
| Chronic pelvic pain/endometriosis | 6 (20) |
| Abnormal uterine bleeding | 4 (13) |
| HSIL | 2 (7) |
| Duration of surgery (min) mean ± SD | 141 ± 47 |
| Bleeding (mL) mean ± SD | 83 ± 177 |
| Uterine weight (g) mean ± SD | 308 ± 212 |
N = 30. HSIL, high-grade squamous intraepithelial lesion.
Surgeons were highly satisfied with the use of sodium fluorescein in 90% of the procedures (n = 27), satisfied in 7% (n = 2), and not satisfied in 3% (n = 1). In 93% of cases (n = 29), ureteral jets were colored, with 83% having bilateral brightly colored jets (24/29).
The mean cystoscopy duration was 5 minutes (range: 1–13 ± 2 minutes). The average time between sodium fluorescein injection and visualization of colored ureteral jets was 7 minutes (range, 3–13 ± 2 minutes). Ninety-three percent (n = 28) of patients had bilateral ureteral jet coloration. Only 1 patient had no coloration of both right and left ureteral jets, and no coloration of her urine was observed after 48 h. The visualization of turbulence of uncolored jets, however, indicated the absence of ureteral obstruction.
Another patient had no coloration and no turbulence of the left ureteral jet allowing diagnosis of a complete unilateral obstruction. The obstruction was a consequence of vaginal cuff suturing, which was immediately corrected. The control cystoscopy was thereafter normal.
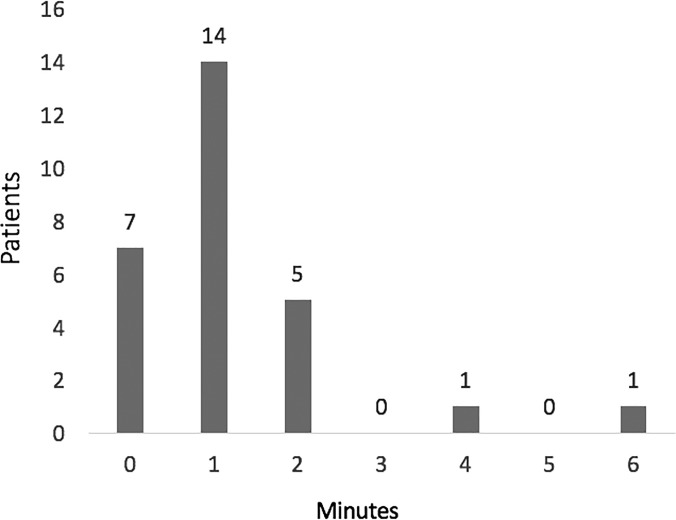
Figure 2 describes the distribution of patients according to the time gap between visualization of the 2 jets. The average time between visualization of the left and right jets was 1 minute with the longest delay being 6 minutes.
Figure 2.
Distribution of patients according to the time gap between visualization of right and left jets.
Three cases of hypotension requiring medical intervention with 10 mg of ephedrine, occurred within 5 minutes after injection (10%), with no adverse events reported in the recovery room. Fifty percent of patients (n = 15) disclosed yellow coloration of urine during the 48 hours after surgery and 10% of patient (n = 3) displayed itching. During the 2-month follow-up, no delayed adverse events related to the use of sodium fluorescein were reported. One patient presented with a delayed (13 days after surgery) moderate right hydronephrosis related to a partial obstruction of the ureter. This patient had normal intraoperative ureteral patency initially observed with fluorescein, but the time gap between the 2 jets was 6 minutes, the longest observed in our cohort, with the right side being delayed and less densely colored. The patient underwent right ureteral stenting and 6 weeks later was symptom free. Overall, the incidence of unrecognized ureteral injury recorded was 3% (1/30).
DISCUSSION
With these findings, the use of sodium fluorescein appears to be an effective and acceptable alternative to indigo carmine, allowing adequate documenting of ureteral patency and improving visualization of ureteral jets during cystoscopy at completion of laparoscopic hysterectomy.
The strength of this study is the prospective design, which allowed for rigorous follow-up and recording of any side effects and assessment of surgeons' satisfaction. The study was limited by the small sample size, although 30 patients was considered a sufficient sample by our team to describe an initial experience with fluorescein. The characteristics of the patients (age and body mass index [BMI]) and the procedure (time of surgery and uterus size) were comparable to those in a similar study.19
Our results confirm the data from a randomized control trial that compared saline distention (control) to 10% dextrose distention, oral phenazopyridine, and intravenous sodium fluorescein. In that study, the use of sodium fluorescein resulted in significantly improved visibility and physician satisfaction when compared with the control group (P = .004). No side effect was reported with 50 mg fluorescein.20
Recently, Grimes et al21 published a randomized control trial comparing 25 mg IV sodium fluorescein, oral phenazopyridine, mannitol bladder distention, and normal saline bladder distention. They found higher rates of surgeons' satisfaction with the use of mannitol, although total time of cystoscopy and time to confidently visualize ureteral efflux were not significantly different between mannitol and sodium fluorescein. Compared with mannitol, fluorescein also allowed direct visualization of ureters during laparoscopy in case of injury.
Visualization of ureteral jets without prior intravenous dye injection is often possible. However, to optimize visualization, urine coloration is paramount. As a result, the American Association of Gynecologic Laparoscopists (AAGL) recommends the use of dyes such as indigo carmine during cystoscopy.4 However, the use of dyes is not yet standard practice in laparoscopic hysterectomy. A 2009 survey found that only 19% of active members of the Society of Obstetricians and Gynaecologists of Canada (SOGC) had performed intraoperative cystoscopy after laparoscopic hysterectomy. Lack of training was the most common reason that cystoscopy was not performed (70/118, 59%).4,22
In addition to lack of formal training, many surgeons pointed out the inability of this technique to detect all ureteral injuries accurately as a reason that they did not perform intraoperative cystoscopy. Such a view is not entirely without merit. Delayed postoperative edema, secondary to inflammation caused by nearby sutures and thermal injuries that initially do not cause mechanical obstruction, can be missed during intraoperative cystoscopy.4 However, it is well established that the sensitivity and specificity of intraoperative cystoscopy remain high (80–90%) in diagnosing ureteral injuries.3,8
In our study, 1 case of immediate obstruction was diagnosed with cystoscopy. As mentioned in several studies, the obstruction was localized in the area of the vaginal cuff sutures.1 After removal of the sutures, ureteral patency was normal without the necessity for ureteral stenting.
In addition, 1 patient had partial right ureteral obstruction diagnosed 13 days after surgery. The cystoscopy during the intervention was suboptimal, which in retrospect should have been interpreted as a cautionary sign. Indeed, the coloration of the right jet was less intense. The time-gap between the 2 ureteral jets was the longest (6 minutes) when compared to the rest of the data points collected in this study. The measurement of this time gap could be a parameter to take into account in the assessment of ureteral patency. Finally, 1 patient had no coloration of ureteral jets, and it remains unknown whether the absence of the dye could have been related to altered metabolism or an error in the technique used to administer it.23
The AAGL Practice Committee recommends that surgeons and institutions consider routine implementation of cystoscopy at the time of laparoscopic total hysterectomy (level B).4 Furthermore, unrecognized urinary tract injury can lead to significant litigation. In its March 2015 report, the Canadian Medical Protective Association stated that ureteral injuries are the most common cause of litigation in gynecologic surgery. In some cases, experts concluded that it was difficult to defend surgeons who did not take all the necessary steps at their disposal to identify ureteral injury.5
The dose of sodium fluorescein used in our study (25 mg) appears sufficient to visualize ureteral jets. This dose is lower than those used in recent studies.20 Three cases of hypotension requiring medical treatment were observed. This side effect was not mentioned in a study in which this low dose was used.13 Although no other serious side effects were reported in our study at this concentration, this dye probably should not be used in patients with multiple allergies because of the risk of anaphylactic reaction.24
Sodium fluorescein is relatively inexpensive; it is marketed in 5-mL single-use vials of 100 mg/mL that cost approximately 37 CDN$ each. As only 1/20th of a vial is used to perform a cystoscopy, the rest of the dye can be used for other procedures.25
CONCLUSION
The use of low-dose sodium fluorescein appears to be an effective and accessible alternative for documenting ureteral patency and for improving visualization of ureteral jets during cystoscopy at the completion of laparoscopic hysterectomy.
Contributor Information
Lea Delbos, Département de gynécologie du CHU de Québec - Université Laval, Québec, QC, Canada..
Annie-Kim Gareau-Labelle, Département de gynécologie du CHU de Québec - Université Laval, Québec, QC, Canada..
Eve-Lyne Langlais, Département de gynécologie du CHU de Québec - Université Laval, Québec, QC, Canada..
Madeleine Lemyre, Département de gynécologie du CHU de Québec - Université Laval, Québec, QC, Canada..
Marianne Boutet, Département de gynécologie du CHU de Québec - Université Laval, Québec, QC, Canada..
Sarah Maheux-lacroix, Département de gynécologie du CHU de Québec - Université Laval, Québec, QC, Canada..
Lucie Dallaire, Département de pharmacie du CHU de Québec – Université Laval, Québec, QC, Canada..
Philippe Y Laberge, Département de gynécologie du CHU de Québec - Université Laval, Québec, QC, Canada..
References:
- 1. Chan JK, Morrow J, Manetta A. Prevention of ureteral injuries in gynecologic surgery. Am J Obstet Gynecol. 2003;188:1273–1277. [DOI] [PubMed] [Google Scholar]
- 2. Vakili B, Chesson RR, Kyle BL, et al. The incidence of urinary tract injury during hysterectomy: a prospective analysis based on universal cystoscopy. Am J Obstet Gynecol. 2005;192:1599–1604. [DOI] [PubMed] [Google Scholar]
- 3. Gilmour DT, Dwyer PL, Carey MP. Lower urinary tract injury during gynecologic surgery and its detection by intraoperative cystoscopy. Obstet Gynecol. 1999;94:883–889. [DOI] [PubMed] [Google Scholar]
- 4. AAGL Practice Report. Practice Guidelines for Intraoperative Cystoscopy in Laparoscopic Hysterectomy. J Minim Invasive Gynecol. 2012;19:407–411. [DOI] [PubMed] [Google Scholar]
- 5. L'association Canadienne de Protection Médicale (ACPM; Canadian Medical Protective Association): Obligations et responsabilités: reconnaître le risque de lésion urétérale au cours d'une chirurgie abdominale [Duties and responsibilities: recognizing the risk of ureteral injury during abdominal surgery]. Ottawa, Ontario, Canada: ACPM; March 2015. Available at: https://www.cmpa-acpm.ca/fr/advice-publications/browse-articles/2015/recognizing-the-risk-of-ureteric-injury-in-abdominal-surgery/ Accessed September 5, 2018. [Google Scholar]
- 6. Ibeanu OA, Chesson RR, Echols KT, Nieves M, Busangu F, Nolan TE. Urinary tract injury during hysterectomy based on universal cystoscopy. Obstet Gynecol. 2009;113:6–10. [DOI] [PubMed] [Google Scholar]
- 7. Indraratna PL, Walsh CA, Moore KH. Intra-operative cystoscopy in gynaecological surgery: a brief overview. Aust N Z J Obstet Gynaecol. 2011;51:272–275. [DOI] [PubMed] [Google Scholar]
- 8. Gustilo-Ashby AM, Jelovsek JE, Barber MD, Yoo E-H, Paraiso MFR, Walters MD. The incidence of ureteral obstruction and the value of intraoperative cystoscopy during vaginal surgery for pelvic organ prolapse. Am J Obstet Gynecol. 2006;194:1478–1485. [DOI] [PubMed] [Google Scholar]
- 9. Indigo carmine injection: current shortage. Bethesda, MD: American Society of Health System Pharmacists, Drug Shortage Resource Management Center, 2018. Available from: https://www.ashp.org/drug-shortages/current-shortages/Drug-Shortage-Detail.aspx?id=175 Accessed September 5, 2018. [Google Scholar]
- 10. Methylene blue injection shortage. Bethesda, MD: American Society of Health-System Pharmacists, Drug Shortage Resource Management Center, 2018. Available from: https://www.ashp.org/drug-shortages/current-shortages/Drug-Shortage-Detail.aspx?id=47 Accessed September 5, 2018. [Google Scholar]
- 11. Indocyanine green shortage. Bethesda, MD: American Society of Health System Pharmacists, Drug Shortage Resource Management Center, 2018. Available from: https://www.ashp.org/drug-shortages/current-shortages/Drug-Shortage-Detail.aspx?id=324 Accessed September 5, 2018. [Google Scholar]
- 12. Doyle PJ, Lipetskaia L, Duecy E, Buchsbaum G, Wood RW. Sodium fluorescein use during intraoperative cystoscopy. Obstet Gynecol. 2015;125:548–550. [DOI] [PubMed] [Google Scholar]
- 13. Ha SO, Kim DY, Sohn CH, Lim KS. Anaphylaxis caused by intravenous fluorescein: clinical characteristics and review of literature. Intern Emerg Med. 2014;9:325–330. [DOI] [PubMed] [Google Scholar]
- 14. Hara T, Inami M, Hara T. Efficacy and safety of fluorescein angiography with orally administered sodium fluorescein. Am J Ophthalmol. 1998;126:560–564. [DOI] [PubMed] [Google Scholar]
- 15. Okuda T, Yoshioka H, Kato A. Fluorescence-guided surgery for glioblastoma multiforme using high-dose fluorescein sodium with excitation and barrier filters. J Clin Neurosci Off J Neurosurg Soc Australas. 2012;19:1719–1722. [DOI] [PubMed] [Google Scholar]
- 16. Okuda T, Kataoka K, Yabuuchi T, Yugami H, Kato A. Fluorescence-guided surgery of metastatic brain tumors using fluorescein sodium. J Clin Neurosci Off J Neurosurg Soc Australas. 2010;17:118–121. [DOI] [PubMed] [Google Scholar]
- 17. Catapano G, Sgulò FG, Seneca V, Lepore G, Columbano L, di Nuzzo G. Fluorescein-guided surgery for high grade glioma resection: an intraoperative “contrast-enhancer.” World Neurosurg. 2017;104:239–247. [DOI] [PubMed] [Google Scholar]
- 18. Zhang J, Al-Nahari F, Wang Z-F, et al. Application of fluorescein sodium in the resection of vermis pilocytic astrocytomas. World J Surg Oncol. 2017;15:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lonky NM, Mohan Y, Chiu VY, et al. Hysterectomy for benign conditions: complications relative to surgical approach and other variables that lead to postoperative readmission within 90 days of surgery. Womens Health Lond Engl. 2017;13:17–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Espaillat-Rijo L, Siff L, Alas AN, et al. Intraoperative cystoscopic evaluation of ureteral patency: a randomized controlled trial. Obstet Gynecol. 2016;128:1378–1383. [DOI] [PubMed] [Google Scholar]
- 21. Grimes C, Patankar S, Ryntz T, et al. Evaluating ureteral patency in the post-indigo carmine era: a randomized controlled trial. Am J Obstet Gynecol. 2017;217:601.e1–601.e10. [DOI] [PubMed] [Google Scholar]
- 22. Farrell SA, Baskett TF, Baydock S. The use of intraoperative cystoscopy by general gynaecologists in Canada. Can J Obstet Gynaecol. 2009;31:48–53. [DOI] [PubMed] [Google Scholar]
- 23. Joel AB, Mueller MD, Pahira JJ, Mordkin RM. Nonvisualization of intravenous methylene blue in patients with clinically normal renal function. Urology. 2001;58:607. [DOI] [PubMed] [Google Scholar]
- 24. Lee T, Sanderson D, Doyle P, Buchsbaum G. Anaphylactic shock after intravenous fluorescein administration for intraoperative cystoscopy. Obstet Gynecol. 2018;131:727–729. [DOI] [PubMed] [Google Scholar]
- 25. Puertos E, Giles G. Potency and sterility of 10% sodium fluorescein injection, USP stored in sterile polypropylene syringes for use during cystoscopy. Hosp Pharm. 2016;51:778–781. [DOI] [PMC free article] [PubMed] [Google Scholar]