Abstract
Objective:
This secondary analysis of the Child/Adolescent Anxiety Multimodal Study (CAMS) used baseline patient characteristics to identify prognostic subgroups of children based on likelihood of remission. We also investigated predictors and moderators of outcome.
Method:
CAMS randomized 488 youths with generalized, social and separation anxiety disorders to cognitive behavioral therapy (CBT), sertraline, both or pill placebo. Outcomes were week-12 child, parent and independent evaluator (IE) ratings of child anxiety. We used receiver operating characteristics analysis and stepwise regression to identify predictors and moderators of outcome.
Results:
Severe anxiety, lower socioeconomic status and comorbid obsessive-compulsive disorder (OCD) predicted higher IE-rated anxiety posttreatment; child-rated social anxiety predicted poorer outcomes reported by all informants. Regarding moderators, Hispanic ethnicity predicted higher IE-rated anxiety after CBT and higher parent-rated anxiety after sertraline. In youths with severe anxiety (Pediatric Anxiety Rating Scale ≥ 20, n=220), combination treatment increased remission (relative risk (RR) 2.93, 95CI 1.41–3.91, p=0.001), while CBT (RR 1.59, 95CI 0.79–3.19, p=0.19) and sertraline (1.34, 95CI 0.79–3.19, p=0.46) did not significantly increase remission relative to placebo.
Conclusions:
These are the first findings demonstrating a combination of CBT and a selective serotonin reuptake inhibitor, not monotherapy, is likely key for achieving remission in severe anxiety. CAMS was not powered to detect treatment efficacy after stratification by anxiety severity, so further research is needed regarding effective treatments in severe anxiety. Our main effect findings suggest youth with severe anxiety (especially social phobia), low socioeconomic status and OCD benefit less from current first-line treatments relative to other anxious youth.
Keywords: predictors, children, anxiety disorders, clinical trial, pediatric
INTRODUCTION
Anxiety disorders are among the most common mental health problems in children (Costello, Egger, & Angold, 2005) and when not treated successfully are associated with significant short and long term impairment and tremendous societal cost (Greenberg et al., 1999; Higa-McMillan, Francis, Rith-Najarian, & Chorpita, 2016; Taylor et al., 2016). The largest randomized controlled trial for childhood anxiety disorders to date is the Child/Adolescent Anxiety Multimodal Study (CAMS) (Piacentini et al., 2014; Rynn et al., 2015; Walkup et al., 2008). CAMS randomized 488 children and adolescents (henceforth referred to as children) aged 7–17 years with generalized anxiety disorder (GAD), social phobia (SOP) or separation anxiety disorder (SAD) to treatment with sertraline, cognitive behavior therapy (CBT), both (COMB) or pill placebo (PBO). CAMS made an important contribution to the field by providing empirical support for the efficacy of both CBT and sertraline, with the combined treatment showing the best outcomes, and monotherapy with CBT or sertraline having better outcomes than PBO. The CAMS investigative team concluded that all three treatment options could be recommended (Walkup et al., 2008, first paragraph of Discussion).
The CAMS investigative team also called for further analysis to identify predictors and moderators of outcome to assist clinicians with accurately prescribing particular interventions based on patient characteristics (predictors are factors that impact outcomes for all treatments, and moderators are treatment-specific predictors) (Walkup et al., 2008). Several studies have found that greater anxiety severity predicts poorer treatment outcomes in pediatric anxiety, but other predictor findings are inconsistent and there are no consistent moderator findings underscoring the need for further research ((Nilsen, Eisemann, & Kvernmo, 2013); Compton et al., 2014 Introduction for review). Previous studies have identified the following variables as predictors of poorer CBT outcomes in youth with GAD, SAD and SOP: mother and teacher ratings of child internalizing symptoms, maternal self-reported depression and older age (Southam-Gerow, Kendall, & Weersing, 2001b); depression, trait anxiety and parental psychopathology (Berman, Weems, Silverman, & Kurtines, 2000); and SOP, comorbid mood and externalizing disorders and parental psychopathology (Hudson et al., 2015). Studies examining age as a predictor of CBT outcome have varied, but a meta-analysis found there was no association between age and CBT outcome in anxious youth (Bennett et al., 2013). Predictors of poorer SSRI anxiety outcomes include: more severe baseline anxiety, SAD and family history of anxiety (Birmaher et al., 2003b); and more severe anxiety, SOP and parent rated child depression (Walkup et al., 2003). Previous studies have not identified moderators of GAD, SAD and SOP treatment outcome when comparing CBT and SSRI aside from the CAMS analyses discussed next.
Since the original CAMS results, there have been two studies focusing on predictors and moderators (Compton et al., 2014; Ginsburg et al., 2011). Ginsburg et al. (2011) investigated ten potential predictors including demographic, clinical child variables and parent psychopathology measures. When investigated in a combined regression model, minority status, baseline anxiety severity, and SOP significantly predicted lower remission rates; moderators were not investigated. Compton et al. (2014) focused on predictors and moderators of response to treatment (as opposed to remission) and found greater caregiver strain predicted poorer treatment response. Regarding moderators, Compton et al. (2014) found participants with a principal diagnosis of SAD responded to COMB and the other treatment arms did not differ significantly. For participants with a principal diagnosis of SOP, response was greatest when treatment included sertraline (i.e., sertraline or combined), and for participants with a principal diagnosis of GAD response was greatest when treatment included CBT. A third manuscript found parental anxiety moderated outcomes such that greater parental anxiety predicted better outcomes with sertraline (Gonzalez et al., 2015).
The current study significantly extends prior analyses of CAMS outcomes by changing the methodology in three ways: 1) integrating receiver operating characteristics (ROC) analysis into the analytic approach, 2) examining baseline anxiety using dimensional measures (i.e., ratings that include subscales for each specific anxiety disorders) as opposed to only global measures of anxiety, and 3) investigating predictors and moderators of parent and child ratings of child anxiety outcomes. Our analytic approach moved beyond regression employed in prior studies. We used receiver operating characteristics (ROC) to identify prognostic subgroups with similar probability of symptom remission in addition to stepwise regression. ROC is a non-parametric statistical technique that quantifies the discriminative power (i.e. sensitivity and specificity) of various thresholds of a predictor variable; the threshold that maximizes sensitivity and specificity can be used to divide a population into two prognostic subgroups. There are advantages and disadvantages to both ROC and regression in predictor and moderator analysis. For linear regression, an advantage is that it can evaluate predictors of continuous outcomes, while ROC requires a binary outcome. Advantages of ROC are that it is sensitive to high-order interactions, is hypothesis-independent, and can identify distinct prognostic subgroups (Kiernan, Kraemer, Winkleby, King, & Taylor, 2001). Both ROC analysis and our stepwise regression approach are designed to minimize Type I (false positive) error (Fournier et al., 2009). The current study’s integration of both of these methodologies allowed us to generate meaningful novel information to help move toward a more nuanced evidence based approach to treatment practice.
In the current study, we also examined baseline anxiety using dimensional measures to complement the analyses in Ginsburg et al. (2011) and Compton et al. (2014), which used global ratings of baseline anxiety – the Clinical Global Impression-Severity (CGI-S) and a global severity index for child, parent and independent evaluator (IE) ratings based on a principal component analysis, respectively. Our analysis measured anxiety using the Pediatric Anxiety Rating Scale (PARS) (RUPP, 2002) and child and parent disorder-specific subscales on the Screen for Child Anxiety-Related Emotional Disorders (SCARED) (Birmaher et al., 1999a; Silverman & Ollendick, 2005; Van Meter et al., 2016).
Additionally, previous investigations of predictors and moderators of outcomes in CAMS have primarily focused on IE rated response and/or remission as opposed to child and parent rated outcomes. A 2015 meta-analysis found low-to-moderate agreement between informants on psychological symptoms and that agreement was poorer for internalizing disorders relative to externalizing disorders (De Los Reyes et al., 2015). Such research demonstrating significant informant discrepancies in childhood psychological disorders motivated our decision to examine outcomes from the child, parent and IE perspectives. Identifying predictors of self-ratings and parent ratings of anxiety outcomes will help clinicians predict how children and parents will experience the therapeutic effects of treatment. Understanding child and parent experience has practical implications for enhancing patient and parent engagement. For instance, predictors of parent and child perspectives on outcomes are important because child and parent perspectives have direct bearing on adherence to treatment recommendations and how children and parents decide to utilize mental health services (Hoffman & Chu, 2015; Kendall & Sugarman, 1997). The exception of CAMS analyses focusing primarily on IE outcomes is a 2015 CAMS analysis by Schleider et al. that found families with greater parental psychopathology at baseline had greater improvements in family functioning and reductions caregiver strain, which in turn predicted lower posttreatment parent rated child anxiety (Schleider et al., 2015). An important caveat to using self and parent ratings is that research staff in CAMS were trained to rate anxiety, and research staff ratings of child anxiety may reflect a more objective measure of functional impairment due to anxiety. Still, the CAMS dataset represents a unique opportunity to conduct integrated predictor and moderator analyses because of the detailed and structured assessment of baseline characteristics and outcome measures collected on complementary informants (child, parent, independent evaluator) on all participants enrolled in the trial. We therefore took advantage of the rich and detailed multi-informant assessment procedures used in CAMS in our analyses to understand child and parent perspectives on CAMS outcomes (De Los Reyes, Thomas, Goodman, & Kundey, 2013; Silverman & Ollendick, 2005).
METHOD
Participants
Participant characteristics, inclusion criteria, methods of recruitment, enrollment and randomization have been detailed previously (Walkup et al., 2008). Participating children had to: 1) be 7–17 years-old and 2) meet criteria for a primary DSM-IV-TR diagnosis of generalized anxiety disorder (GAD), social phobia (SoP) or separation anxiety disorder (SAD) based on the Anxiety Disorder Interview Schedule for Children for DSM-IV-TR (Child and Parent Versions) (ADIS-C/P) (Silverman & Albano, 1996; Silverman & Nelles, 1988). Children who had not responded to previous treatment (i.e., two trials of selective serotonin reuptake inhibitors (SSRI) or a completed course of CBT) were excluded. Youths with current major depression or a lifetime history of autism spectrum, bipolar or psychotic disorders were excluded. Parents provided informed consent and children provided assent. No significant differences were found between the study arms in terms of baseline clinical, parent or demographic variables.
The 488 children enrolled in CAMS were randomized in a 2:2:2:1 ratio to sertraline only, CBT only, COMB or PBO. Children met criteria for at least one of the following diagnoses: SoP (337; 82%), GAD (324; 79%), SAD (72; 17%). 42 children (9%) had comorbid obsessive-compulsive disorder (OCD). 308 children (75%) were between the ages of 7–12, 325 (79%) were White, 37 (9%) were Black, 11 (3%) were Asian, 39 (9%) were other races and 52 children (13%) were Hispanic. Ninety percent completed week 12 outcomes (127 sertraline, 114 CBT, 133 COMB, 65 PBO), and those with missing outcome data were excluded from the current analysis.
Procedures
Full details of intervention and assessment also have been published previously (Walkup et al., 2008). CAMS was conducted at six university sites (University of California in Los Angeles, Johns Hopkins, Columbia, Duke, Temple and the University of Pittsburgh) in the United States, and procedures were approved by each site’s Institutional Review Board. CBT involved 14 60-minute sessions using the Coping Cat program (Kendall & Hedtke, 2006). Pharmacotherapy involved eight 30–60 minute sessions, with sertraline titrating up from 25mg per day at week 1 to 200mg per day by week 8, based on response and side effects. This secondary analysis focuses on the assessments conducted at baseline and at week 12 posttreatment. Assessments were conducted by trained IE, blind to treatment condition.
Assessments
Binary Outcome Variables
ROC analyses require a binary outcome, and our primary ROC outcome was anxiety remission at week 12. Because diagnosis is based on clinician assessment rather than child- or parent-ratings, we based remission on IE ratings. We used the same definitions of remission as those found in past studies (Caporino et al., 2013; Ginsburg et al., 2011): (1) No longer met DSM-IV diagnostic criteria for GAD, SoP, or SAD on ADIS-C/P, (2) Pediatric Anxiety Rating Scale (PARS) < 10, and (3) Clinical Global Impression-Severity of Illness (CGI-S) of 1 (“not at all ill”) or 2 (“borderline ill”). IEs rated child anxiety on the PARS 0–30 based on symptoms during the prior week, and scores > 13 typically indicate moderate anxiety that is clinically significant (Walkup et al., 2008).
Continuous Outcome Variables
The continuous outcome variables of interest in this analysis were post-treatment, week-12 ratings of child anxiety severity completed by each of the three informants: IE (PARS), child and parent. Children and parents rated the child anxiety during the prior two weeks on respective versions of the Screen for Childhood Anxiety Related Emotional Disorders (SCARED-C for children and SCARED-P for parents). Mothers completed the parent ratings in 87% of cases (Compton et al., 2014).
Potential Predictors and Moderators
All variables investigated as potential predictors and moderators in the analysis were assessed prior to random treatment assignment. In terms of selecting potential predictor and moderator variables, due to the inconsistent predictor and moderator findings (Compton et al., 2014; Nilsen et al., 2013), we chose variables that had previously been shown to predict or moderate outcomes, even if findings regarding the variable differed between studies (Bennett et al., 2013; Berman et al., 2000; Birmaher et al., 2003a; Compton et al., 2014; Ginsburg et al., 2011; Gonzalez et al., 2015; Hudson et al., 2015; Pina, Silverman, Fuentes, Kurtines, & Weems, 2003; Walkup et al., 2008; Walkup et al., 2003). We also included socioeconomic status, sex and treatment expectancy based on findings in the adult anxiety literature (Kelly, Jakubovski, & Bloch, 2014; Taylor, Jakubovski, & Bloch, 2015); coping skills based on findings that coping skills mediated improvements in CAMS (Philip C Kendall et al., 2016); family functioning and family burden related to anxiety based on findings that augmenting CBT with family management improves anxiety outcomes (Barrett, Dadds, & Rapee, 1996); IQ based on findings in the autism literature that higher IQ may be associated with more severe anxiety (White, Oswald, Ollendick, & Scahill, 2009); and bias to threat based on the potentially bidirectional relationship between bias to threat and anxiety (Van Bockstaele et al., 2014). The following 68 variables were included in the ROC analysis, 52 of which were included in the regression analysis as described in Supplemental Table 1A (available online) and the Statistical Analyses section below:
Treatment Assignment.
COMB, sertraline, CBT, placebo.
Demographic Variables.
Child sex, Ethnicity (Hispanic vs not Hispanic), Socioeconomic Status (SES; Hollingshead Two Factor Scale (Hollingshead, 1957) summary score), Race (White vs non-White), Age, Full Scale IQ (Tellegen and Briggs Formula).
Child Rated Variables.
Anxiety symptoms (SCARED-C (Birmaher et al., 1999b) total score and subscales for Panic, Generalized Anxiety, Separation Anxiety, Social Phobia and School Anxiety); bias to threat (child rated Ambiguous Situations Questionnaire (Bergman & Piacentini, 2001), ASQ-C); child coping ability (child rated Coping Questionnaire (Kendall, 1994), CQ-C); depressive symptoms (child rated Mood and Feelings Questionnaire, MFQ-C); anxiety impact (child rated Child Anxiety Impact Scale (Langley et al., 2014), CAIS-C); family functioning (child rated Brief Family Assessment Measure (BFAM-C); child treatment expectancies.
Parent Rated Variables.
SCARED-P total score and subscales; child bias to threat (ASQ-P); child coping ability (CQ-P); child depressive symptoms (MFQ-P); child anxiety impact (CAIS-P); child behavioral problems (Child Behavior Checklist (CBCL) for ages 6–18 with subscales for Anxious/Depressed, Withdrawn/Depressed, Somatic Complaints, Social Problems, Thought Problems, Attention Problems, Rule-Breaking Behavior, Aggressive Behavior, Internalizing, Externalizing); parent psychopathology (parent rated Brief Symptom Inventory (BSI) Global Severity and subscales for Somatization, Depression, Phobic Anxiety, Obsessive-Compulsive, Anxiety, Interpersonal Sensitivity, Paranoid Ideation, Hostility, Psychoticism); family burden related to the child’s anxiety (parent rated Family Burden Assessment Scale (FBAS); family functioning (BFAM-P); parent treatment expectancies.
Independent Evaluator Assessed Variables.
Child psychiatric diagnoses based on the ADIS-C/P; total number of psychiatric diagnoses (excluding GAD, SOP, SAD); PARS; child global functioning (Children’s Global Assessment Scale (CGAS)).
Statistical Analyses
We analyzed CAMS Data Version 4.1 from the NIMH database using SAS 9.3 (SAS Institute Inc., Cary, North Carolina) for regression analysis and software made available by Professor Ruth O’Hara, PhD at http://www.stanford.edu/~yesavage/ROC.html for ROC analysis. ROC analysis is non-parametric and uses recursive partitioning. ROC seeks to distinguish subgroups of individuals who have different likelihoods of achieving a particular dichotomous outcome (Gabriel, Jakubovski, Taylor, Artukoglu, & Bloch, 2017; Jakubovski & Bloch, 2015; Kiernan et al., 2001; Taylor et al., 2015). We conducted ROC analyses based on 3 outcomes: remission defined using the (1) ADIS-C/P, (2) PARS and (3) CGI-S. Across all predictor variables, the cut-off point that produces the best prediction is then used to divide the total sample into two subsamples. This procedure repeats within each subsample, and this iterative process continues until a subgroup contains less than 10 individuals or the group difference is not significant at the chi-square p < 0.05 threshold. We also stopped the analysis at the 3-way interaction level. Based on the ROC analysis results, we divided youths into those with lower baseline anxiety (PARS < 20) and higher baseline anxiety (PARS ≥ 20), determined remission rates and calculated the risk ratios (RR) and number needed to treat (NNT). NNT is the number of patients who need to be treated on average before one patient benefits from a particular treatment relative to placebo. A high NNT indicates few children benefit from the treatment relative to placebo.
To examine predictors and moderators of treatment outcome per each informant and complement the ROC analysis, we implemented a linear regression technique developed by Fournier and colleagues (Fournier et al., 2009; Gabriel et al., 2017). The 3 outcome variables were (1) SCARED-C, (2) SCARED-P and (3) PARS ratings at week 12. For each domain (demographic, child rated, parent rated and IE assessed variables) the subsequent stepwise algorithm proceeds along the following: Step 1) Test a full model including all variables and their interactions with treatment. Step 2) Repeat the analysis retaining predictors with p < 0.20 from step 1. Step 3) Repeat the analysis retaining predictors with p < 0.10 from step 2. Step 4) Repeat the analysis retaining predictors with p < 0.05 from step 3. Step 4 is repeated until only variables with p < 0.05 remain in the model. Finally, all predictors significant at p < 0.05 in Step 4 across all domains are included in a combined model. All 4 steps are applied to the combined model. To determine moderators, we identified variables that significantly interacted with treatment arm. If at any step an interaction term was significant (indicating a potential moderation effect), but not the corresponding main effect, the main effect was still retained. Continuous predictors were centered at the grand mean and dichotomous predictors were coded as – 0.5 and 0.5 (Kraemer, Wilson, Fairburn, & Agras, 2002).
For ROC analyses, there were a total of 68 independent variables. The ROC analytic approach minimizes multicollinearity by empirically choosing the most discriminative variable among similar variables hierarchically and choosing a maximum of three variables to characterize each subgroup. To address multicollinearity in regression models, we first manually excluded redundant variables: we removed SCARED and CBCL total scores and included only subscales and we removed BSI subscales and included only the global score. For the CBCL, we also removed the Anxious/Depressed, Withdrawn/Depressed, Somatic and Internalizing subscales which overlap in content with SCARED-P subscales and MFQ-P. We also removed the CBCL Externalizing subscale which overlaps in content with the Rule-breaking and Aggressive Behavior subscales. Next, we excluded variables with variable inflation factors (VIF) > 2.5 within each domain and then within the combined model. For regression analyses, there were a total of 52 independent variables, which are listed in Supplemental Table 1A, available online. To examine agreement between informants with regards to anxiety outcomes, we computed inter-informant Pearson correlations. To examine whether age affected inter-informant agreement as demonstrated in a prior CAMS analysis (Becker, Jensen-Doss, Kendall, Birmaher, & Ginsburg, 2016), we determined agreement for younger children (children up to age 12) and adolescents (age 13 and older) to see if correlations differed significantly.
RESULTS
ROC Results: Prognostic Subgroups
Figures 1A, 1B and 1C display ROC results with baseline prognostic subgroups in a hierarchy based on likelihood of IE rated remission on the ADIS-C/P, PARS and CGI-S at week 12. Figure 1A shows ADIS-C/P remission rates for the most discriminative prognostic subgroups were 20% (baseline PARS ≥ 20, did not receive COMB, CBCL Social Problems t-score ≥ 58) and 79% (baseline PARS < 20, higher functioning (CGAS ≥ 51), CBCL Rule-breaking Behavior t-score < 57). Figure 1B shows PARS remission rates ranged from 22% (baseline PARS ≥ 20, did not receive COMB, SCARED-P Social Phobia ≥ 10) to 83% (baseline PARS < 20, CBCL Somatic Complaints t-score ≥ 56, SCARED-P Social Phobia < 10). Figure 1C shows CGI-S remission rates ranged from 17% (baseline PARS ≥ 20, did not receive COMB, youth’s Pre-treatment Expectancy was lower (score ≥ 2)) to 85% (baseline PARS < 20, better family functioning (BFAM-C t-score < 46), lower baseline functional impairment due to anxiety (CAIS-P < 25)).
FIGURE 1A.
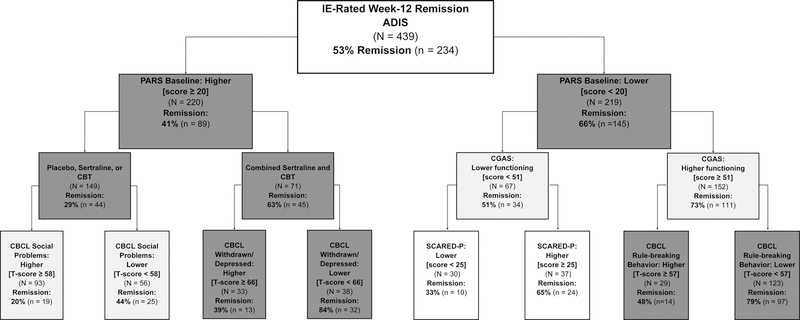
Receiver operating characteristics analysis with baseline prognostic subgroups in a hierarchy based on likelihood of week-12 anxiety remission on the ADIS-C/P.
ADIS-C/P = Anxiety Disorder Interview Schedule-Child/Parent Version; CBCL = Child Behavior Checklist; CBT = cognitive behavioral therapy; CGAS = Children’s Global Assessment Scale (scored 0–100); IE = independent evaluator; PARS = Pediatric Anxiety Rating Scale (scored 0–30, PARS scores > 13 typically indicate clinically significant moderate anxiety); SCARED-P = Screen for Child Anxiety Related Disorders-Parent Version (scored 0–82).
Chart color indicates significance of the difference between subgroups: dark grey: p<0.001; light grey: p<0.01; white: p<0.05.
FIGURE 1B.
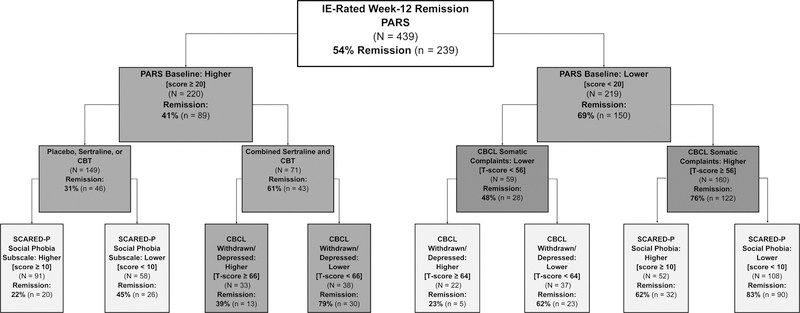
Receiver operating characteristics analysis with baseline prognostic subgroups in a hierarchy based on likelihood of week-12 anxiety remission on the PARS.
CBCL = Child Behavior Checklist; CBT = cognitive behavioral therapy; IE = independent evaluator; PARS = Pediatric Anxiety Rating Scale (scored 0–30); SCARED-P = Screen for Child Anxiety Related Disorders-Parent Version (Social Phobia Subscale scored 0–14).
Chart color indicates significance of the difference between subgroups: dark grey: p<0.001; light grey: p<0.01.
FIGURE 1C.
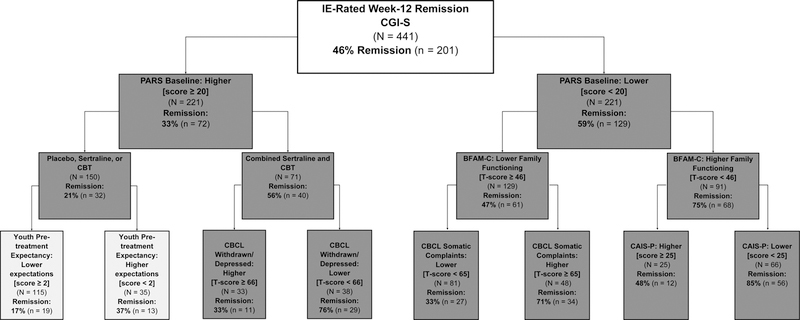
Receiver operating characteristics analysis with baseline prognostic subgroups in a hierarchy based on likelihood of week-12 anxiety remission on the CGI-S.
BFAM-C = Brief Family Assessment Measure-Child Version; CAIS-P = Child Anxiety Impact Scale-Parent Version (scored 0–81); CBCL = Child Behavior Checklist; CBT = cognitive behavioral therapy; CGI-S = Clinical Global Impression-Severity of Illness (scored 1–7); IE = independent evaluator; PARS = Pediatric Anxiety Rating Scale (scored 0–30); Pre-treatment Expectancy scored 1–7.
Chart color indicates significance of the difference between subgroups: dark grey: p<0.001; light grey: p<0.01.
The baseline anxiety severity cut-off of PARS < 20 was identified as the most discriminative predictor of IE-rated remission in the ADIS-C/P, PARS and CGI-S ROC analyses (χ2 (df = 1) = 29.25, 34.79 and 31.18; p < 0.00001) (Figures 1, 2). For youths with high baseline anxiety (baseline PARS ≥ 20), randomization to treatment with COMB was the most discriminative predictor of remission on the ADIS-C/P, PARS and CGI-S (χ2 (df = 1) = 22.87, 17.60 and 26.88; p < 0.00003). This result suggests an interaction between COMB and baseline anxiety severity such that COMB may be particularly beneficial towards inducing remission in youths with high baseline anxiety. The importance of COMB for remission in youths with high anxiety was consistent when all four treatment arms (i.e. including placebo) were included in ROC analyses (Figures 1A, 1B, 1C) and also when only the active treatment arms were included (Supplemental Figures 1A, 1B, 1C, available online).
FIGURE 2.
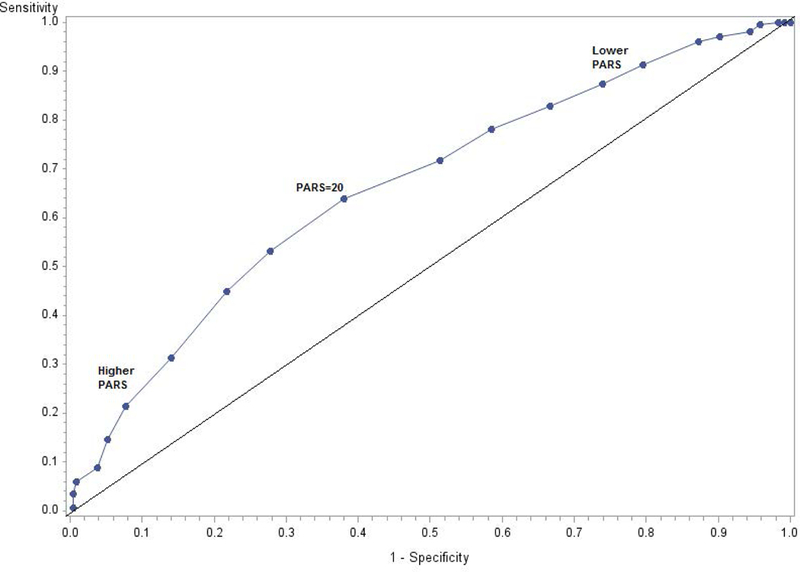
Receiver operating characteristics curve illustrating the optimal cut-off point of baseline PARS for predicting non-remission on the ADIS-C/P was baseline PARS ≥ 20.
Week-12 Anxiety Remission Stratified By Baseline Anxiety Severity
Table 1 displays the remission rates, relative risks (RR) and NNT for each treatment modality stratified by baseline anxiety severity on the PARS. COMB was more efficacious than monotherapy across all levels of anxiety for all treatment outcomes. However, COMB especially benefited youths with high baseline anxiety (PARS ≥ 20). The relative risks for remission show that high anxiety youths benefitted most from COMB. Higher relative risks quantify how superior treatment is relative to placebo in terms of remission, and the highest relative risk for all remission outcomes was COMB in higher anxiety youths; furthermore, COMB was the only treatment that significantly increased probability of remission relative to placebo in high anxiety youths (ADIS-C/P remission RR: COMB 2.93, 95% CI 1.55–5.55, p=0.001; sertraline 1.34, 95% CI 0.62‐2.87, p=0.46; CBT 1.59, 95% CI 0.79‐3.19, p=0.19). It is important to note that while sertraline and CBT did not demonstrate significant superiority over placebo, CAMS was not powered to detect treatment effects after stratification by anxiety severity. The NNT also demonstrate that COMB’s advantage over monotherapy (particularly sertraline) was more pronounced in high-anxiety youths than in low-anxiety youths. A clinician would on average have to treat 14 severely anxious children with sertraline only (NNTsertraline=14) or 8 children with CBT only (NNTCBT=8) for one child to benefit relative to placebo. In stark contrast, a clinician would only have to treat 3 severely anxious children with COMB (NNTCOMB=3) for one child to benefit more from treatment compared to placebo. The same did not hold for children with lower baseline anxiety; all therapies had fairly low NNT to achieve remission compared to placebo: NNTCOMB=3, NNTsertraline=3 and NNTCBT=5. Furthermore, the ROC results presented in Figure 1A, 1B and 1C demonstrate the importance of COMB for children with severe anxiety; the most discriminative predictor of remission for higher-anxiety children was randomization to COMB. In contrast, treatment modality was not the most discriminative predictor of remission in lower-anxiety children in ROC analyses.
TABLE 1.
Remission Rates in Youths Stratified by Baseline Anxiety Treated With Combined Sertraline and CBT, Sertraline Only, CBT Only or Placebo.
| Remission Outcome Stratified by Baseline Anxiety Severity |
Remission Rates by Treatment Arm | Relative Risk for Remission | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| COMB | SRT | CBT | PBO | COMB:PBO | SRT:PBO | CBT:PBO | |||||||
| Nlow=56 Nhigh=71 |
Nlow=69 Nhigh=45 |
Nlow=66 Nhigh=67 |
Nlow=28 Nhigh=37 |
Nlow=84 Nhigh=108 |
Nlow=97 Nhigh=82 |
Nlow=94 Nhigh=104 |
|||||||
| % (95 CI) | % (95 CI) | % (95 CI) | % (95 CI) | Ratio (95 CI) | p | NNT | Ratio (95 CI) | p | NNT | Ratio (95 CI) | p | NNT | |
| ADIS-C/P | |||||||||||||
| Lower Anxiety | 84 (72‒92) | 70 (57‒80) | 60 (47‒72) | 36 (19‒58) | 2.35 (1.41‒3.91) | 0.001 | 3 | 1.94 (1.16‒3.28) | 0.01 | 3 | 1.70 (1.00‒2.89) | 0.05 | 5 |
| High Anxiety | 63 (51‒75) | 28 (16‒43) | 34 (23‒46) | 22 (10‒39) | 2.93 (1.55‒5.55) | 0.001 | 3 | 1.34 (0.62‒2.87) | 0.46 | 14 | 1.59 (0.79‒3.19) | 0.19 | 8 |
| PARS | |||||||||||||
| Lower Anxiety | 86 (74‒94) | 71 (59‒81) | 64 (51‒75) | 39 (22‒59) | 2.18 (1.36‒3.50) | 0.001 | 3 | 1.81 (1.11‒2.93) | 0.02 | 4 | 1.62 (0.99‒2.66) | 0.06 | 5 |
| High Anxiety | 61 (49‒73) | 33 (20‒49) | 36 (24‒48) | 19 (8‒35) | 3.20 (1.60‒6.40) | 0.001 | 3 | 1.76 (0.80‒3.86) | 0.16 | 7 | 1.89 (0.90‒3.97) | 0.09 | 6 |
| CGI-S | |||||||||||||
| Lower Anxiety | 79 (66‒88) | 65 (53‒76) | 50 (37‒62) | 25 (11‒45) | 3.14 (1.63‒6.06) | <0.001 | 2 | 2.61 (1.34‒5.07) | 0.005 | 3 | 1.94 (0.97‒3.86) | 0.06 | 5 |
| High Anxiety | 56 (44‒68) | 24 (13‒39) | 24 (14‒36) | 14 (5‒30) | 4.17 (1.80‒9.66) | <0.001 | 3 | 1.81 (0.69‒4.74) | 0.23 | 10 | 1.77 (0.70‒4.44) | 0.23 | 10 |
Lower baseline anxiety defined as PARS < 20; high baseline anxiety defined as PARS ≥ 20. PARS scores > 13 typically indicate clinically significant moderate anxiety. NNT = number needed treat, which is the number of youths who need to be treated on average before one youth benefits from treatment over placebo. A high NNT indicates few children benefit from the treatment relative to placebo. 95 CI = 95% confidence interval; ADIS-C/P = Anxiety Disorder Interview Schedule-Child/Parent Version; COMB=combined, SRT=sertraline, CBT=Cognitive Behavioral Therapy; PBO=placebo, CGI-S=Clinical Global Impression-Severity of Illness; PARS = Pediatric Anxiety Rating Scale.
Informant Agreement Results
Correlations between child rated, parent rated and IE rated anxiety measures was moderate (r = 0.52–0.60). Correlations of child rated anxiety with parent and IE rated child anxiety were significantly lower when children were 12 years-old or younger. For instance, the correlation between parent and child ratings for youth under 12 years was 0.46, while the parent-child ratings correlation for children at least 12 years was 0.64 (p < 0.05). Supplemental Table 2 presents Pearson correlations between continuous outcome variables and is available online. Because of the low to moderate correlations found, we next examined anxiety outcomes as rated by each informant.
Regression Results: Predictors and Moderators of Anxiety Treatment Outcome
In the regression analysis, baseline predictors explained a substantial portion of variance in anxiety outcomes, regardless of informant. When comparing the predictive value of baseline data from each informant (child, parent or IE), baseline IE ratings were most informative in predicting IE rated anxiety outcomes (R2=28%). Linear regression model results for child, parent and IE outcomes by domain (demographic, child, parent and IE rated variables) are in Supplemental Table 1B, available online. Table 2 presents results from the combined best-fitting models.
TABLE 2.
Combined Best Fitting Model of Significant Pretreatment Predictors and Moderators of Child Anxiety Severity after 12 Weeks of Treatment in Stepwise Multiple Linear Regression Analysis Stratified by Informant.
| Child Informant Outcome (SCARED-C) | Parent Informant Outcome (SCARED-P) | Independent Evaluator Outcome (PARS) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PE | SE | t | p | PE | SE | t | p | PE | SE | t | p | |||
| SCARED-C SOP | 0.61 | 0.14 | 4.44 | <0.001 | SCARED-C SOP | 0.43 | 0.14 | 3.14 | 0.002 | SCARED-C SOP | 0.21 | 0.07 | 3.20 | 0.002 |
| SCARED-C SEP | 0.51 | 0.14 | 3.52 | <0.001 | SCARED-P SOP | 0.43 | 0.14 | 3.12 | 0.002 | SES | −0.59 | 0.29 | −2.02 | 0.04 |
| SCARED-P PAN | CBCL TP | 0.24 | 0.06 | 3.80 | <0.001 | OCD DX | 2.39 | 0.96 | 2.49 | 0.01 | ||||
| COMB | −0.93 | 0.39 | −2.41 | 0.02 | CBCL RULE X TX | SCARED-C SEP X TX | ||||||||
| MFQ-C X TX | CBT | 0.88 | 0.29 | 3.07 | 0.002 | COMB | −0.49 | 0.22 | −2.26 | 0.02 | ||||
| CBT | −0.36 | 0.15 | −2.46 | 0.01 | SCARED-P PAN X TX | HISPANIC X TX | ||||||||
| COMB | −0.48 | 0.15 | −3.24 | 0.001 | CBT | 1.11 | 0.38 | 2.91 | 0.004 | CBT | 7.86 | 2.71 | 2.90 | 0.004 |
| CQ-C X TX | SCARED-P SCH X TX | BSI GSI X TX | ||||||||||||
| CBT | −2.93 | 1.34 | −2.19 | 0.03 | CBT | −1.74 | 0.70 | −2.50 | 0.01 | CBT | 4.71 | 2.02 | 2.33 | 0.02 |
| CBCL TP X TX | SRT | 2.55 | 0.72 | 3.55 | <0.001 | SRT | −5.20 | 2.28 | −2.28 | 0.02 | ||||
| SRT | −0.46 | 0.23 | −2.02 | 0.04 | SCARED-C SEP X TX | SELECTIVE MUT DX X TX | ||||||||
| BSI GSI X TX | SRT | 1.02 | 0.47 | 2.20 | 0.03 | COMB | 12.65 | 5.48 | 2.31 | 0.02 | ||||
| SRT | −9.97 | 4.51 | −2.21 | 0.03 | COMB | −0.91 | 0.39 | −2.32 | 0.02 | |||||
| BSI GSI X TX | ||||||||||||||
| SRT | −14.51 | 4.16 | −3.48 | <0.001 | ||||||||||
| COMB | −8.98 | 4.08 | −2.20 | 0.03 | ||||||||||
| HISPANIC X TX | ||||||||||||||
| SRT | 20.01 | 6.06 | 3.30 | 0.001 | ||||||||||
| SELECTIVE MUT DX X TX | ||||||||||||||
| CBT | 37.78 | 11.64 | 3.25 | 0.001 | ||||||||||
| R2 | 0.40 | R2 | 0.50 | R2 | 0.33 | |||||||||
Note: PE = parameter estimate; SE = standard error; CBT = Cognitive Behavior Therapy; SRT = Sertraline; COMB = Combined CBT and SRT; X TX denotes an interaction with treatment arm assignment; Variables with –C are child rated and variables with –P are parent rated; HISPANIC= child of Hispanic ethnicity; SES = socioeconomic status (Hollingshead Two Factor Scale); SCARED = Screen for Childhood Anxiety Related Emotional Disorders [Includes the following subscale abbreviations: SEP=Separation Anxiety, SOP=Social Phobia, GAD=Generalized Anxiety, SCH=School Anxiety; PAN=Panic Disorder]; MFQ = Mood and Feelings Questionnaire; CQ = Coping Questionnaire; CBCL = Child Behavior Checklist [Includes the following subscales abbreviations: ANX/DEP=Anxious Depressed, RULE=Rule Breaking, TP=thought problems]; SELECT MUT DX = Met criteria for Selective Mutism; BSI GSI = Brief Symptom Inventory Global Severity Index.
Independent Evaluator Rated Anxiety Outcomes
In the regression analysis, the combined (best-fitting) model explained 33% of variance in IE rated PARS scores at week 12. In the best fitting combined model, several predictors of anxiety outcome were identified. Higher PARS score at week 12 was associated with meeting criteria for an OCD diagnosis at baseline, lower socioeconomic status and higher score on the Social Phobia subscale of SCARED-C. Additionally, several moderators of treatment effects were identified. Hispanic ethnicity was associated with higher PARS score after CBT. Higher global parental psychopathology predicted lower PARS score after sertraline and higher PARS score after CBT. Higher SCARED-C Separation Anxiety subscale score predicted lower PARS score after COMB and selective mutism comorbidity predicted higher PARS score after COMB
Child Rated Anxiety Outcomes
In the regression analysis, the combined (best-fitting) model explained 40% of variance in child rated SCARED-C score at 12 weeks. The best-fitting model found that higher scores on the Separation Anxiety and Social Phobia subscales of SCARED-C predicted higher child rated anxiety on SCARED-C at week 12.
Several moderator variables were also identified. Higher score on the child rated MFQ predicted lower SCARED-C after CBT and COMB. Better coping skills (higher baseline scores on the child rated Child Coping Questionnaire) predicted lower SCARED-C after CBT. Higher score on the SCARED-P Panic subscale predicted lower SCARED-C after COMB. Higher CBCL Thought Problem subscale score and more severe global parental psychopathology on the BSI predicted lower SCARED-C after sertraline.
Parent Rated Anxiety Outcomes
In the regression analysis, the combined (best-fitting) model explained 50% of variance in parent rated SCARED-P scores. In the best-fitting combined model, several predictors of anxiety outcome were identified. Higher score on the Thought Problems subscale of the CBCL, as well as both child and parent rated Social Phobia subscales of SCARED, predicted higher week 12 child anxiety ratings on the SCARED-P.
Several moderator variables were also identified. Meeting criteria for a diagnosis of selective mutism was associated with higher SCARED-P scores after CBT, as were higher scores on the Rule Breaking subscale of CBCL and the Panic subscale of SCARED-P. Higher Separation Anxiety subscale score on the SCARED-C predicted lower SCARED-P scores after COMB but higher SCARED-P score after sertraline. Higher score on the School Phobia subscale of SCARED-P predicted higher week-12 SCARED-P scores after sertraline but lower SCARED-P score after CBT. Greater global parent psychopathology predicted lower SCARED-P scores after sertraline and COMB but not after CBT. Hispanic ethnicity predicted higher SCARED-P score after sertraline.
DISCUSSION
Primary analysis of CAMS demonstrated that combined treatment was superior to sertraline alone and CBT alone, both of which outperformed placebo (Walkup et al., 2008). The current analysis provides several important new findings with direct implications for clinical practice including that combined treatment was paramount for achieving remission in children with high anxiety, while less anxious children were likely to remit with any active treatment. The CAMS investigative group concluded that all three treatments could be recommended to patients (Walkup et al., 2008). Our study found that this is true for children with mild-moderate anxiety but not with severe anxiety. Our methodological approach using ROC further allowed us to identify the interaction between high anxiety and combination treatment as the most discriminative predictor of clinical outcome compared with all other baseline demographic and clinical characteristics. Moreover, our analysis of CAMS is the first to demonstrate that in CAMS: 1) low socioeconomic status predicted poorer IE rated outcomes, 2) OCD comorbidity predicted poorer IE rated outcomes, 3) more severe child rated social anxiety is an important predictor of poorer outcomes across informants and 4) Hispanic ethnicity moderated outcomes such that IE rated anxiety was higher after CBT and parent rated anxiety was higher after sertraline for Hispanics. Our finding that parental psychopathology moderated outcomes such that greater global parental psychopathology predicted better IE and parent rated outcomes after sertraline-containing treatments but not CBT is in line with a prior CAMS analysis that found greater parental anxiety predicted better outcomes with sertraline (Gonzalez et al., 2015). Additionally, our ROC analysis was able to identify empirically derived prognostic subgroups with probabilities of remission as determined by an independent evaluator that ranged from 17% to 85%.
Our study is the first study to demonstrate that randomization to COMB was key to achieving remission in children with high baseline anxiety (Walkup et al., 2008). We found children with lower baseline anxiety usually achieved remission with any active treatment, but children with high baseline anxiety usually achieved remission only if they were treated with COMB. Our findings contrast with the original CAMS report which concluded, “Our findings indicate that all three of the treatment options may be recommended, taking into consideration the family’s treatment preferences, treatment availability, cost, and time burden.” (Walkup et al., 2008, first paragraph of Discussion). Prior work determined COMB was particularly effective for youth with separation and generalized anxiety disorder, underscoring the importance of primary diagnosis when selecting a treatment (Compton et al., 2014). Our findings highlight that anxiety severity is also important to consider when choosing treatment modality. When children are acutely and severely impaired due to anxiety, there is increased urgency to effectively treat symptoms (Connolly, Bernstein, & Work Group on Quality, 2007). Given the low remission rates with SSRI alone or CBT alone, clinicians should strongly consider combined treatment as first-line for severe childhood anxiety.
These findings have potentially important clinical practice implications. Oftentimes, descriptions of the CAMS results emphasize that all three treatments (CBT only, sertraline only, or combined treatment) are effective and can be considered first-line treatments (Walkup et al., 2008). Some guidelines, in fact, recommend monotherapy (psychotherapy only) as the first-line treatment in pediatric anxiety. For instance, the National Institute for Health and Care Excellence (NICE) guidelines state, “Do not routinely offer drug interventions to treat social anxiety disorder in children and young people (NICE, 2013).” Our study clarifies that severity plays a key role in determining appropriate treatment.
One main difference between current results and those from prior predictor and moderator CAMS analyses is that the current analysis found that child rated SoP at baseline was an important predictor of child, parent and IE rated outcomes (Compton et al., 2014). Specifically, we found more severe self-ratings of SoP predicted more severe anxiety after treatment. Prior CAMS analyses have not identified child rated SoP as a predictor of outcome because prior analyses aggregated scales completed by children into a global anxiety index as opposed to our analytic approach which examined domains of anxiety as predictors (Compton et al., 2014). The current work confirms earlier reports indicating that more severe baseline anxiety levels, and in particular SoP, portend poorer anxiety treatment outcomes and extends prior findings by identifying that self-ratings (as opposed to clinician ratings) of SoP strongly predict outcome (Compton et al., 2014; Ginsburg et al., 2011; Hudson et al., 2015; Jakubovski & Bloch, 2015; Liber et al., 2010; Southam-Gerow, Kendall, & Weersing, 2001a).
Similar to findings in the adult anxiety literature (Jakubovski & Bloch, 2015; Taylor et al., 2015), we found that low socioeconomic status predicted poorer IE rated outcomes. Our findings differ from a prior CAMS analysis that found SES does not predict outcome, and the difference may be due to how the SES variable was coded (Compton et al., 2014). CAMS measured SES using the Hollingshead Two Factor Index, which uses occupational prestige and education level to rank SES into a five class system (1= low SES, 5= high SES). While we used the ordinal five class system to measure SES, the Compton et al. 2014 CAMS analysis dichotomized this variable into low SES (scores 1–3) and high SES (scores 4–5). Additionally, we found that comorbidity with OCD predicted poorer IE rated outcomes. Prior studies have inconsistently found links between poorer treatment outcomes and comorbidity (Nilsen et al., 2013).
Several variables emerged as moderators of child anxiety outcomes. We found children who reported more depressive symptoms at baseline reported less anxiety after treatment if they were assigned to CBT-containing treatments (CBT or COMB). Ginsburg and colleagues investigated depression as a comorbid internalizing diagnosis (along with other non-primary anxiety disorders) and found an association between comorbid internalizing diagnoses and lower rates of remission, but did not examine the unique impact of depressive symptoms on outcome (Ginsburg et al., 2011). Similarly, coping skills were not investigated as potential predictors of outcome in prior predictor and moderator analysis of CAMS (Compton et al., 2014; Ginsburg et al., 2011). Current results indicate self-rated child coping skills at baseline predicted better child rated outcomes in children treated with CBT. This finding suggests children who have better coping skills before treatment may particularly benefit from CBT which seeks to bolster coping capability. The importance of coping skills in anxiety treatment in CAMS is also seen in prior work which found improvements in coping skills mediated improvements in anxiety in CBT, sertraline and combination treatment (Kendall et al., 2016).
Hispanic ethnicity was another significant moderator and was associated with poorer IE rated outcomes after CBT monotherapy and poorer parent rated outcomes after sertraline monotherapy. Research regarding the impact of minority status on treatment outcomes for childhood anxiety has been mixed (Pina et al., 2003). A previous secondary analysis of IE rated outcomes from CAMS reported that minority status predicted lower likelihood of remission (Ginsburg et al., 2011), while other studies have reported non-significant results (Berman et al., 2000; Southam-Gerow et al., 2001a). Our analysis differs from prior CAMS analyses in that we investigated race and ethnicity as distinct, while Ginsburg et al. (2011) grouped all racial and ethnic minorities and compared their outcomes to non-Hispanic White outcomes. The Ginsburg approach does not account for the fact that the Hispanic ethnicity includes people of multiple races (i.e. there are Black Hispanics, White Hispanics and Hispanics who classify their race as “Other”). That is, race is a social construct based on biological characteristics like skin color, hair texture and facial morphology, while ethnicity is based on a common cultural background. Although the current analysis suggests Hispanic ethnicity predicts poorer outcomes after monotherapy, it should be noted that prior research has found similar CBT outcomes for Hispanics and European-American youths when therapist training included cultural components, such as education about culturally-appropriate expressions of anxiety and coping strategies ((Pina, Little, Knight, & Silverman, 2009; Pina et al., 2003; Pina, Zerr, Villalta, & Gonzales, 2012)). Culturally-sensitive approaches were not explicitly discussed in the CAMS Protocol (Version 1.4), which may have contributed to the poorer outcomes for Hispanic youths receiving monotherapy.
Among the anxiety disorders, only the presence of selective mutism significantly moderated outcomes; selective mutism predicted more severe IE rated anxiety after combined treatment and more severe parent rated anxiety after treatment with CBT only. Clinical trials for selective mutism are scarce and most lack adequate control conditions, making it difficult to draw confident conclusions about CBT efficacy (Viana, Beidel, & Rabian, 2009). However, CBT requires active patient participation and can be difficult in cases of selective mutism, and addressing selective mutism before implementing CBT-containing treatment strategies for comorbid anxiety disorders may be advisable.
We also found parent ratings of their own psychological difficulties significantly moderated treatment outcomes, such that more severe global ratings of psychopathology on the BSI predicted lower IE ratings of child anxiety when the child received medication. Our findings fit with prior CAMS results that more severe parental anxiety predicted better outcomes for children who received sertraline (Gonzalez et al., 2015). It is possible that parental psychopathology suggests genetic underpinnings of child anxiety variants especially amenable to pharmacological treatment.
Externalizing symptoms, specifically rule breaking behaviors, moderated only the parent rated child anxiety, predicting more severe anxiety following CBT but did not significantly affect child or IE rated outcomes. Previous investigations of child externalizing comorbidity as a predictor of child anxiety outcomes did not report significant findings (Kendall, Brady, & Verduin, 2001; Manassis et al., 2002; Southam-Gerow et al., 2001a), and the clinical presentation of externalizing symptoms in children with anxiety disorders is quite heterogeneous (Williams, Dahan, Silverman, & Pettit, 2013). The present findings, showing a moderator role for externalizing symptoms, highlight the importance of assessing externalizing symptoms prior to CBT. It also is plausible that some parents may have difficulty in distinguishing anxious symptoms from externalizing symptoms. Children with high anxiety and related disorders rely heavily on family accommodation of their symptoms to avoid distress (Lebowitz, Scharfstein, & Jones, 2014; Lebowitz et al., 2013), and frequently forcefully impose accommodation on family members or react with rage or aggression when not accommodated (Lebowitz, Omer, & Leckman, 2011; Storch et al., 2012).
Additionally, examination of outcomes according to each informant allowed us to identify a weaker correlation between parent and child ratings for younger children compared to adolescents 13 years-old and up, highlighting the particular importance of a multi-informant assessment for younger children with anxiety (De Los Reyes, 2011; De Los Reyes et al., 2015; De Los Reyes et al., 2013). Becker et al. 2016 also analyzed CAMS data and found older age was associated with greater parent-child agreement on anxiety symptoms (Becker et al., 2016); however, a 2015 meta-analysis found that there was not a significant relationship between age and inter-informant agreement when looking at childhood mental health outcomes (De Los Reyes et al., 2015). More research is needed on the relationship between patient age and inter-informant agreement on childhood anxiety outcomes. Becker and colleagues (2016) also found that agreement was higher in separation anxiety relative to other anxiety disorders. Appreciating informant discrepancies is also important because mental health service discontinuation against clinician recommendations can occur when parents feel their child is no longer symptomatic (Philip C Kendall & Sugarman, 1997; Pina, Silverman, Weems, Kurtines, & Goldman, 2003). The importance of evaluating information from multiple informants is further underscored by recent research indicating that child rated anxiety is a better predictor of objectively measured avoidant behavior, compared to parent ratings of the child’s anxiety (Lebowitz, 2017).
Our study has several important strengths. Our use of ROC and examination of hierarchical interactions allowed us to stratify children by baseline anxiety and identify the importance of combined treatment for remission in youths with high baseline anxiety. Also, our consistent ROC findings across three different IE-based definitions of remission suggest strong internal validity. Additional methodological strengths stem directly from the original rigorous and well conducted CAMS study.
This research needs to be interpreted in light of certain limitations. First, the analysis was empirical, not hypothesis-driven. We conducted a large number of statistical tests without statistical correction for multiple hypothesis testing. Examination of multiple dimensions of anxiety and patient baseline characteristics increases type I error and can result in false-positive results. However, we used exploratory analysis approaches such as ROC analysis and Fournier regression techniques that are designed to minimize the problems with multiple hypothesis testing. Nonetheless, significant findings in our manuscript are subject to possible false-positive error and vulnerable to overfitting the models to this specific group of children, and thus require replication in future studies.
Another potential limitation is that the algorithmic statistical approach can have the effect of mechanically choosing between variables based on sometimes small differences in explanatory power without the benefit of clinically informed judgment. Therefore, these statistical techniques are also prone to false-negative error (type II error). Some of the potential explanatory variables included in these models may be significantly predictive of outcome if investigated individually but may not have been selected in our models because there are other variables included that are more discriminative of outcome (in ROC analysis) or their effects are diminished by other information provided by the same informant (in regression analysis). Our techniques use data-driven approaches designed not to identify every potentially predictive variable but to balance type I and type II error. Additionally, while CAMS is the largest study of its kind, it was not powered to detect differences between treatments after stratification by pretreatment severity, thus the finding that monotherapy did not significantly increase remission in severe anxiety requires further investigation. More research regarding effective treatments for severe anxiety is warranted.
Despite these limitations, this investigation contributes to understanding how anxiety severity affects treatment outcome. We found that for youths with severe baseline anxiety in CAMS, a combined treatment approach with both CBT and a SSRI (as compared to monotherapies) was especially important for achieving remission. Given the differences in the literature regarding which youth should receive combined CBT and SSRI treatment instead of CBT alone (Connolly, Bernstein, & Work Group on Quality, 2007; NICE, 2013; Wehry, Beesdo-Baum, Hennelly, Connolly, & Strawn, 2015), our results are particularly relevant to current clinical practice. In addition to anxiety severity, other factors like urgency (e.g. school refusal), resource availability and family and patient preferences and expectancies are key to creating an effective treatment plan. Additionally, we found that children with more severe self-rated social anxiety were more likely to have poor outcomes, and future research should consider how to augment available first-line treatments to improve outcomes in social anxiety disorder.
Supplementary Material
Acknowledgments:
Data used in the preparation of this article were obtained from the limited access datasets distributed from the NIH-supported “Child and Adolescent Anxiety Disorders” (CAMS). This is a multisite, clinical trial of children and adolescents with anxiety disorders comparing the effectiveness of the medication sertraline (Zoloft®), cognitive-behavioral therapy, the combination of these treatments, and placebo for youths with anxiety disorders. The study was supported by NIMH Grant # U01 MH64089 to Johns Hopkins University. The ClinicalTrials.gov identifier is NCT00052078. This manuscript reflects the views of the authors and may not reflect the opinions or views of the CAMS Study Investigators or the NIH.
The authors gratefully acknowledge support from the National Institutes of Health/National Institute of Mental Health (NIH/NIMH, 5T32MH018268 and 5T32MH019112, J.H.T.; 1K23MH103555 E.R.L.; 1K23MH091240, M.H.B.), NARSAD (E.R.L; M.H.B.), Patterson Trust (J.H.T., M.H.B.), the American Psychiatric Association/Substance Abuse and Mental Health Services Administration Minority Fellowship Program (J.H.T.). Dr. Silverman receives royalties for the Anxiety Disorders Interview Schedule for Children and Parents.
Footnotes
Disclosures: The authors have no conflicts of interest to disclose.
Contributor Information
Jerome H. Taylor, University of Pennsylvania, Department of Psychiatry, 3400 Spruce St, Gates Pavilion 10th Floor, Philadelphia, PA 19104.
Eli R. Lebowitz, Yale University Child Study Center, 230 S Frontage Rd, New Haven, CT 06520.
Ewgeni Jakubovski, Yale University Child Study Center, 230 S Frontage Rd, New Haven, CT 06520.
Catherine G. Coughlin, Yale University Child Study Center, 230 S Frontage Rd, New Haven, CT 06520.
Wendy K. Silverman, Yale University Child Study Center, 230 S Frontage Rd, New Haven, CT 06520.
Michael H. Bloch, Yale University Child Study Center and Yale University Department of Psychiatry, 230 S Frontage Rd, New Haven, CT 06520.
REFERENCES
- Barrett PM, Dadds MR, & Rapee RM (1996). Family treatment of childhood anxiety: a controlled trial. Journal of Consulting and Clinical Psychology, 64(2), 333–342. doi: 10.1037/0022-006X.64.2.333 [DOI] [PubMed] [Google Scholar]
- Becker EM, Jensen-Doss A, Kendall PC, Birmaher B, & Ginsburg GS (2016). All Anxiety is not Created Equal: Correlates of Parent/Youth Agreement Vary Across Subtypes of Anxiety. Journal of Psychopathology and Behavioral Assessment, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett K, Manassis K, Walter SD, Cheung A, Wilansky‐Traynor P, Diaz‐Granados N, . . . Barrett P (2013). Cognitive behavioral therapy age effects in child and adolescent anxiety: An individual patient data metaanalysis. Depression and Anxiety, 30(9), 829–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman RL, & Piacentini J (2001). The Ambiguous Situations Questionnaire: UCLA, Department of Psychiatry [Google Scholar]
- Berman S, Weems C, Silverman W, & Kurtines W (2000). Predictors of outcome in exposure-based cognitive and behavioral treatments for phobic and anxiety disorders in children. Behavior Therapy, 31(4), 713–731. doi: 10.1016/s0005-7894 [DOI] [Google Scholar]
- Birmaher B, Axelson DA, Monk K, Kalas C, Clark DB, Ehmann M, . . . Brent DA (2003a). Fluoxetine for the treatment of childhood anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 42(4), 415–423. doi: 10.1097/01.CHI.0000037049.04952.9F [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson DA, Monk K, Kalas C, Clark DB, Ehmann M, . . . Brent DA (2003b). Fluoxetine for the treatment of childhood anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 42(4), 415–423. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, & Baugher M (1999a). Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. Journal of the American Academy of Child and Adolescent Psychiatry, 38(10), 1230–1236. doi: 10.1097/00004583-199910000-00011 [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, & Baugher M (1999b). Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. Journal of the American Academy of Child and Adolescent Psychiatry, 38(10), 1230–1236. doi: 10.1097/00004583-199910000-00011 [DOI] [PubMed] [Google Scholar]
- Caporino NE, Brodman DM, Kendall PC, Albano AM, Sherrill J, Piacentini J, . . . Walkup JT (2013). Defining Treatment Response and Remission in Child Anxiety: Signal Detection Analysis Using the Pediatric Anxiety Rating Scale. Journal of the American Academy of Child and Adolescent Psychiatry, 52(1), 57–67. doi: 10.1016/j.jaac.2012.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton SN, Peris TS, Almirall D, Birmaher B, Sherrill J, Kendall PC, . . . Albano AM (2014). Predictors and moderators of treatment response in childhood anxiety disorders: results from the CAMS trial. Journal of Consulting and Clinical Psychology, 82(2), 212–224. doi: 10.1037/a0035458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly SD, Bernstein GA, & Work Group on Quality, I. (2007). Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 46(2), 267–283. doi: 10.1097/01.chi.0000246070.23695.06 [DOI] [PubMed] [Google Scholar]
- Costello EJ, Egger HL, & Angold A (2005). The developmental epidemiology of anxiety disorders: phenomenology, prevalence, and comorbidity. Child and Adolescent Psychiatric Clinics of North America, 14(4), 631–648, vii. doi: 10.1016/j.chc.2005.06.003 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Augenstein TM, Wang M, Thomas SA, Drabick DA, Burgers DE, & Rabinowitz J (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141(4), 858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, Thomas SA, Goodman KL, & Kundey SM (2013). Principles underlying the use of multiple informants’ reports. Annual Review of Clinical Psychology, 9, 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier JC, DeRubeis RJ, Shelton RC, Hollon SD, Amsterdam JD, & Gallop R (2009). Prediction of response to medication and cognitive therapy in the treatment of moderate to severe depression. Journal of Consulting and Clinical Psychology, 77(4), 775–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabriel D, Jakubovski E, Taylor JH, Artukoglu BB, & Bloch MH (2017). Predictors of Treatment Response and Drop Out in the Treatment of Early-Onset Schizophrenia Spectrum Disorders (TEOSS) Study. Psychiatry Research [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Kendall PC, Sakolsky D, Compton SN, Piacentini J, Albano AM, . . . March J (2011). Remission after acute treatment in children and adolescents with anxiety disorders: findings from the CAMS. Journal of Consulting and Clinical Psychology, 79(6), 806–813. doi: 10.1037/a0025933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez A, Peris TS, Vreeland A, Kiff CJ, Kendall PC, Compton SN, . . . Keeton CP (2015). Parental anxiety as a predictor of medication and CBT response for anxious youth. Child Psychiatry and Human Development, 46(1), 84–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg PE, Sisitsky T, Kessler RC, Finkelstein SN, Berndt ER, Davidson JR, . . . Fyer AJ (1999). The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatry, 60(7), 427–435. [DOI] [PubMed] [Google Scholar]
- Higa-McMillan CK, Francis SE, Rith-Najarian L, & Chorpita BF (2016). Evidence base update: 50 years of research on treatment for child and adolescent anxiety. Journal of Clinical Child and Adolescent Psychology, 45(2), 91–113. [DOI] [PubMed] [Google Scholar]
- Hollingshead A (1957). Hollingshead two factor index of social position. Handbook of Research Design and Social Measurement, 5th ed. Newbury Park, CA: Sage Publications, 351–359. [Google Scholar]
- Hudson JL, Keers R, Roberts S, Coleman JR, Breen G, Arendt K, . . . Eley TC (2015). Clinical Predictors of Response to Cognitive-Behavioral Therapy in Pediatric Anxiety Disorders: The Genes for Treatment (GxT) Study. Journal of the American Academy of Child and Adolescent Psychiatry, 54(6), 454–463. doi: 10.1016/j.jaac.2015.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakubovski E, & Bloch MH (2015). Anxiety Disorder-Specific Predictors of Treatment Outcome in the Coordinated Anxiety Learning and Management (CALM) Trial. Psychiatric Quarterly, 1–20. [DOI] [PubMed] [Google Scholar]
- Kelly J, Jakubovski E, & Bloch M (2014). Prognostic subgroups for remission and response in the Coordinated Anxiety Learning and Management (CALM) trial. The Journal of clinical psychiatry [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC (1994). Treating anxiety disorders in children: results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 62(1), 100–110. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Brady EU, & Verduin TL (2001). Comorbidity in childhood anxiety disorders and treatment outcome. Journal of the American Academy of Child and Adolescent Psychiatry, 40(7), 787–794. doi: 10.1097/00004583-200107000-00013 [DOI] [PubMed] [Google Scholar]
- Kendall PC, Cummings CM, Villabø MA, Narayanan MK, Treadwell K, Birmaher B, . . . Walkup J (2016). Mediators of change in the Child/Adolescent Anxiety Multimodal Treatment Study. Journal of Consulting and Clinical Psychology, 84(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, & Hedtke KA (2006). Cognitive-behavioral therapy for anxious children: therapist manual (3rd ed.). Ardmore, PA: Workbook Publishing. [Google Scholar]
- Kiernan M, Kraemer HC, Winkleby MA, King AC, & Taylor CB (2001). Do logistic regression and signal detection identify different subgroups at risk? Implications for the design of tailored interventions. Psychological Methods, 6(1), 35. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, & Agras WS (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59(10), 877–883. [DOI] [PubMed] [Google Scholar]
- Langley AK, Falk A, Peris T, Wiley JF, Kendall PC, Ginsburg G, . . . Piacentini J (2014). The child anxiety impact scale: examining parent-and child-reported impairment in child anxiety disorders. Journal of Clinical Child and Adolescent Psychology, 43(4), 579–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz ER (2017). Mother and Child Ratings of Child Anxiety: Associations With Behavioral Avoidance and the Role of Family Accommodation. Parenting, 17(2), 124–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz ER, Omer H, & Leckman JF (2011). Coercive and disruptive behaviors in pediatric obsessive–compulsive disorder. Depression and Anxiety, 28(10), 899–905. doi: 10.1002/da.20858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz ER, Scharfstein LA, & Jones J (2014). Comparing family accommodation in pediatric obsessive-compulsive disorder, anxiety disorders, and nonanxious children. Depression and Anxiety, 31(12), 1018–1025. doi: 10.1002/da.22251 [DOI] [PubMed] [Google Scholar]
- Lebowitz ER, Woolston J, Bar-Haim Y, Calvocoressi L, Dauser C, Warnick E, . . . Leckman JF (2013). Family accommodation in pediatric anxiety disorders. Depression and Anxiety, 30(1), 47–54. doi: 10.1002/da.21998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liber JM, van Widenfelt BM, van der Leeden AJ, Goedhart AW, Utens EM, & Treffers PD (2010). The relation of severity and comorbidity to treatment outcome with Cognitive Behavioral Therapy for childhood anxiety disorders. Journal of Abnormal Child Psychology, 38(5), 683–694. doi: 10.1007/s10802-010-9394-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manassis K, Mendlowitz SL, Scapillato D, Avery D, Fiksenbaum L, Freire M, . . . Owens M (2002). Group and individual cognitive-behavioral therapy for childhood anxiety disorders. A randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry, 41(12), 1423–1430. doi: 10.1097/00004583-200212000-00013 [DOI] [PubMed] [Google Scholar]
- NICE. (2013). Department of Health, United Kingdom. National Institute for Health and Care Excellence (NICE). Social anxiety disorder: recognition, assessment and treatment [PubMed] [Google Scholar]
- Nilsen TS, Eisemann M, & Kvernmo S (2013). Predictors and moderators of outcome in child and adolescent anxiety and depression: a systematic review of psychological treatment studies. European Child and Adolescent Psychiatry, 22(2), 69–87. [DOI] [PubMed] [Google Scholar]
- Piacentini J, Bennett S, Compton SN, Kendall PC, Birmaher B, Albano AM, . . . Walkup J (2014). 24- and 36-week outcomes for the Child/Adolescent Anxiety Multimodal Study (CAMS). Journal of the American Academy of Child and Adolescent Psychiatry, 53(3), 297–310. doi: 10.1016/j.jaac.2013.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pina AA, Little M, Knight GP, & Silverman WK (2009). Cross-ethnic measurement equivalence of the RCMAS in Latino and White youth with anxiety disorders. Journal of Personality Assessment, 91(1), 58–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pina AA, Silverman WK, Fuentes RM, Kurtines WM, & Weems CF (2003). Exposure-based cognitive-behavioral treatment for phobic and anxiety disorders: treatment effects and maintenance for Hispanic/Latino relative to European-American youths. Journal of the American Academy of Child and Adolescent Psychiatry, 42(10), 1179–1187. [DOI] [PubMed] [Google Scholar]
- Pina AA, Zerr AA, Villalta IK, & Gonzales NA (2012). Indicated prevention and early intervention for childhood anxiety: A randomized trial with Caucasian and Hispanic/Latino youth. Journal of Consulting and Clinical Psychology, 80(5), 940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RUPP. (2002). Research Units on Pediatric Psychopharmacology Anxiety Study Group. The pediatric anxiety rating scale (PARS): Development and psychometric properties. Journal of the American Academy of Child and Adolescent Psychiatry, 41(9), 1061–1069. [DOI] [PubMed] [Google Scholar]
- Rynn MA, Walkup JT, Compton SN, Sakolsky DJ, Sherrill JT, Shen S, . . . Birmaher B (2015). Child/Adolescent anxiety multimodal study: evaluating safety. Journal of the American Academy of Child and Adolescent Psychiatry, 54(3), 180–190. doi: 10.1016/j.jaac.2014.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider JL, Ginsburg GS, Keeton CP, Weisz JR, Birmaher B, Kendall PC, . . . Walkup JT (2015). Parental psychopathology and treatment outcome for anxious youth: Roles of family functioning and caregiver strain. Journal of Consulting and Clinical Psychology, 83(1), 213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, & Albano AM (1996). Anxiety Disorders Interview Schedule for DSM-IV.: Child and Parent Interview Schedules (Vol. 1): Oxford University Press. [Google Scholar]
- Silverman WK, & Nelles WB (1988). The Anxiety Disorders Interview Schedule for Children. Journal of the American Academy of Child and Adolescent Psychiatry, 27(6), 772–778. doi: 10.1097/00004583-198811000-00019 [DOI] [PubMed] [Google Scholar]
- Silverman WK, & Ollendick TH (2005). Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34(3), 380–411. [DOI] [PubMed] [Google Scholar]
- Southam-Gerow MA, Kendall PC, & Weersing VR (2001a). Examining outcome variability: correlates of treatment response in a child and adolescent anxiety clinic. Journal of Clinical Child Psychology, 30(3), 422–436. doi: 10.1207/S15374424JCCP3003_13 [DOI] [PubMed] [Google Scholar]
- Southam-Gerow MA, Kendall PC, & Weersing VR (2001b). Examining outcome variability: correlates of treatment response in a child and adolescent anxiety clinic. Journal of Clinical Child Psychology, 30(3), 422–436. doi: 10.1207/S15374424JCCP3003_13 [DOI] [PubMed] [Google Scholar]
- Storch EA, Jones AM, Lack CW, Ale CM, Sulkowski ML, Lewin AB, . . . Murphy TK (2012). Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. Journal of the American Academy of Child and Adolescent Psychiatry, 51(6), 582–592. doi: 10.1016/j.jaac.2012.02.016 [DOI] [PubMed] [Google Scholar]
- Taylor J, Xu Y, Li F, Shaw M, Dziura J, Caprio S, . . . Savoye M (2016). Psychosocial predictors and moderators of weight management programme outcomes in ethnically diverse obese youth. Pediatric Obesity [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JH, Jakubovski E, & Bloch MH (2015). Predictors of anxiety recurrence in the Coordinated Anxiety Learning and Management (CALM) trial. Journal of Psychiatric Research, 65, 154–165. doi: 10.1016/j.jpsychires.2015.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bockstaele B, Verschuere B, Tibboel H, De Houwer J, Crombez G, & Koster EH (2014). A review of current evidence for the causal impact of attentional bias on fear and anxiety. Psychological Bulletin, 140(3), 682. [DOI] [PubMed] [Google Scholar]
- Van Meter AR, You DS, Halverson T, Youngstrom EA, Birmaher B, Fristad MA, . . . Frazier TW (2016). Diagnostic efficiency of caregiver report on the SCARED for identifying youth anxiety disorders in outpatient settings. Journal of Clinical Child and Adolescent Psychology, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viana AG, Beidel DC, & Rabian B (2009). Selective mutism: A review and integration of the last 15 years. Clinical Psychology Review, 29(1), 57–67. doi: 10.1016/j.cpr.2008.09.009 [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, . . . Kendall PC (2008). Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine, 359(26), 2753–2766. doi: 10.1056/NEJMoa0804633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup JT, Labellarte MJ, Riddle MA, Pine D, Greenhill L, Klein R, . . . Psychopharmacolog, R. U. P. (2003). Searching for moderators and mediators of pharmacological treatment effects in children and adolescents with anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 42(1), 13–21. doi: 10.1097/01.Chi.0000024906.60748.A8 [DOI] [PubMed] [Google Scholar]
- Wehry AM, Beesdo-Baum K, Hennelly MM, Connolly SD, & Strawn JR (2015). Assessment and Treatment of Anxiety Disorders in Children and Adolescents. Current psychiatry reports, 17(7), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Oswald D, Ollendick T, & Scahill L (2009). Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review, 29(3), 216–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams S, Dahan J, Silverman WK, & Pettit JW (2013). Heterogeneous classes of co-occurring externalizing symptoms in a sample of youth referred for anxiety disorders. Journal of Anxiety Disorders, 27(3), 340–346. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


