Abstract
Background:
Surgical revision rate of rhinoplasty is from 5% to 15% in literature. The aims of our study were to define the rate and the predictive factors for surgical revision of rhinoplasty.
Methods:
We have realized a single-center case/control study including 62 patients who underwent surgical revision among 732 patients who underwent closed rhinoplasty between 2005 and 2015. Data of each rhinoplasty were collected from medical records and photographs. Statistical analyses were used.
Results:
The surgical revision rate was 8.6%. After multivariate analysis, 4 factors were statistically significant and independently associated with surgical revision: “preexisting respiratory functional disorder” [odds ratio OR = 3.30; 95% CI (1.47–7.76); P = 0.004], “wide nasal bone and side walls” [OR = 3.94; 95% CI (1.49–11.25); P = 0.007], “deviated nasal bone and side walls” [OR = 2.68; 95% CI [1.14–6.58]; P = 0.02] and the use of camouflage grafts [OR = 0.26; 95% CI [0.07–0.89]; P = 0.04].
Conclusions:
Closed rhinoplasties have similar revision rate to open techniques. Revision surgeries are justified by functional or aesthetic disorders. The interests of this study are to better inform patients and to adapt operative management. We provide here some recommendations with focus on the keys to successful rhinoplasty surgery.
INTRODUCTION
Rhinoplasties are surgical procedures aiming to correct deformities of the different structures of the nose and the nasal septum. This surgery is commonly practiced, and its various techniques are widely described.1 The experienced surgeon should identify requests of patients to manage them during the procedure. However, despite all these precautions, rhinoplasties have bad reputation for surgeons because they are difficult to achieve with sometimes disappointing results for the patient. Thus, surgical revisions, also called “secondary rhinoplasties,” can be performed to manage the request of patients. Their satisfactions should be at the center of the concerns. Surgical revisions are not so rare as attested by several studies with surgical revision rates of 5–15%.2–5 Given the widespread practice of rhinoplasties and the increasing requests of patients, it becomes necessary for surgeons, to identify the noses at risk for surgical revision. This will allow to better inform patients and to modify the surgical management. The aims of our study are to define the rate and the predictive factors for surgical revision of rhinoplasty.
METHODS
We have realized a single-center retrospective case/control study. Among patients who underwent closed rhinoplasty from 2005 to 2015, we have determined 2 groups of patients. Inclusion criteria for the “revision” group were consecutive patients, operated for revision rhinoplasty by the senior surgeon (J. B. B.), with available data and who were followed up at least 6 months after the surgery. The “control” group was determined by random selection of patients operated by the same surgeon (J. B. B.) with the same surgical technique (closed approach), during the same period but who did not require revision. We have chosen a ratio of at least 1:1 for statistical comparison.
For each patient, after precise examinations of medical records (medical history, physical examination) and photographs (double-blind reading, J. B. B. and J. B.), we have extracted data of the first rhinoplasty, also called “primary rhinoplasty.” The following information were saved origin and context of requests (functional disorders, posttraumatic disorders), results of the preoperative physical examination, detailed operative management, significant postoperative complications (fatal or leading to longer length of hospital stay) and aesthetic or functional postoperative disorders. The evaluation of the nasal function and the research of preexisting respiratory disorders was based on clinical examination. We have considered the nasal obstruction whose importance was characterized by the medical history (unilateral or asymmetrical, permanent or not, tilting, nocturnal) and the presence or not of chronic rhinitis. The nasosinuendoscopy and computed tomography scan were usually not performed since only anterior septal deviations are obstructive. For each patient, an exhaustive anterior rhinoscopy with examination of the nasal septum, the inferior turbinates and the valve nasal was performed. The functional validated surveys such as the NOSE questionnaire6,7 were not used. The modified Cottle maneuver was performed in case of suspected nasal valve collapse.8,9 The noses were defined as “wide noses” when the nasal bones base projects out of the internal canthi.
The study population was described by statistical mean and SDs for the quantitative variables and by effectives and percentages for the qualitative variables. The personal and operative characteristics of the “revision” and “control” groups were compared by univariate analysis to determine the factors associated with surgical revision. The group (case and control) differences were examined by using independent t tests for continuous variables and by using chi-square test or Fisher’s exact test when the validity conditions were not respected, for discrete variables. In case of statistical significance between a factor and the revision surgery, the link was quantified by odds ratio (OR) calculated by the conditional maximum likelihood method.
A logistic regression was performed. The variables included in the model are those that were significant at the 20% threshold in the bi-varied analysis. Then a selection by automatic backward procedure was carried out. The adjusted OR and their 95% confidence interval (95% CI) were calculated. All analyses were carried out using software R version 3.1.1 (ref: https://cran.r-project.org/R Foundation for Statistical Computing/Vienna/Austria/2017). The file has been declared to the National Commission of Informatics and Liberties.
This study was approved by ethics committee and institutional review board. The written informed consents were obtained from study participants before surgery.
RESULTS
From 2005 to 2015, we have performed 732 rhinoplasties including 75 secondary rhinoplasties (revision rhinoplasty). Among the latter, n = 13 patients underwent primary surgery by another surgeon in another center and were excluded to homogenize the groups. Thus, there was n = 62 patients included in the “revision group.” After random selection, we have included n = 77 patients in the “control” group. Both groups were homogeneous and comparable. The most frequently represented ethnic groups were quoted in the order of largest prevalence: Turkish/Kurds, Maghreb origin, White and others. The mean age was 27.5 years (range, 15–54) with a sex ratio male/female of 1/3. No craniofacial disorder was found. All revision surgeries were performed using closed approaches. The rhinoplasty revision rate of the surgeon was 8.6%. No significant perioperative or postoperative surgical complication was found (infection, hemorrhage, empty nose syndrome).
Comparing data of primary rhinoplasties in the 2 groups, 3 factors were statistically relevant.
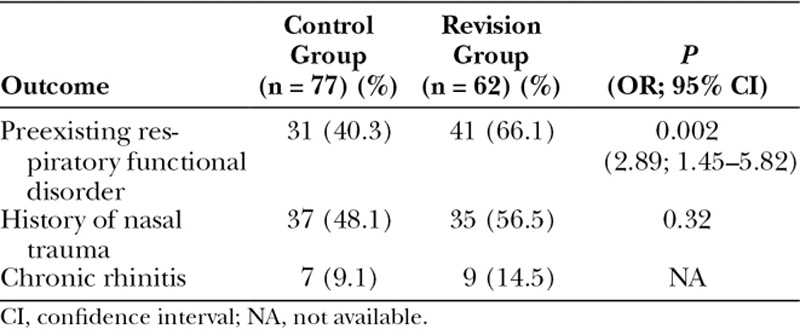
First of all, data of the primary rhinoplasties (Table 1) have revealed that there was requests for correction of preexisting respiratory functional disorder for n = 41 (66.1%) patients in the revision group and n = 31 (40.3%) patients in the control group [OR = 2.89; 95% CI (1.45–5.82)].
Table 1.
Outcome in the Control and Revision Groups before the Primary Rhinoplasty
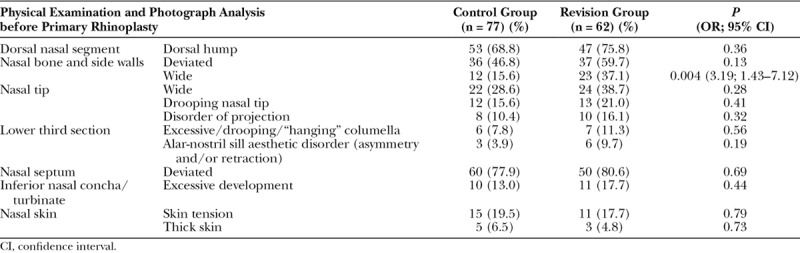
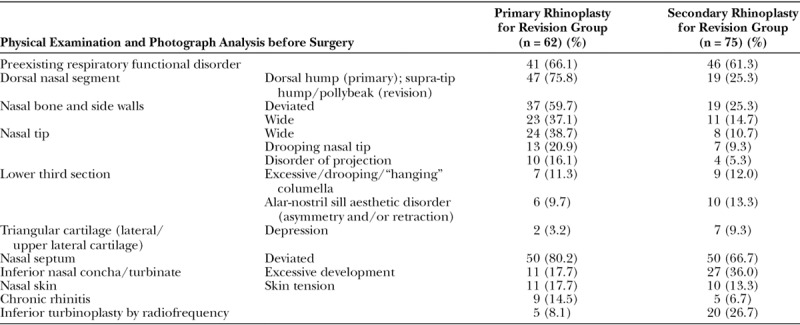
Second, data of the physical examination and the photographs before primary rhinoplasties have shown nasal bones resulting in wide aspects of the noses for n = 23 (37.1%) patients in the revision group and n = 12 (15.6%) patients in the control group [OR = 3.19; 95% CI (1.43–7.12)]. In addition, in the revision group, more deviated nasal bones and sidewall (P = 0.13) and more alar-nostril sill aesthetic disorder (P = 0.19) were observed (Table 2).
Table 2.
Physical Examination and Photograph Analysis before Primary Rhinoplasty in the 2 Groups of Patients, Defining the Surgical Context
Regarding perioperative data of the primary rhinoplasties (Table 3), internal silicone splints restraining the nasal septum were statistically more used for the revision group compared with the control group, n = 36 (58.1%) and n = 33 [42.9%; OR = 2.09; 95% CI (1.05–4.17)], respectively.
Table 3.
Surgical Management during Primary Rhinoplasty
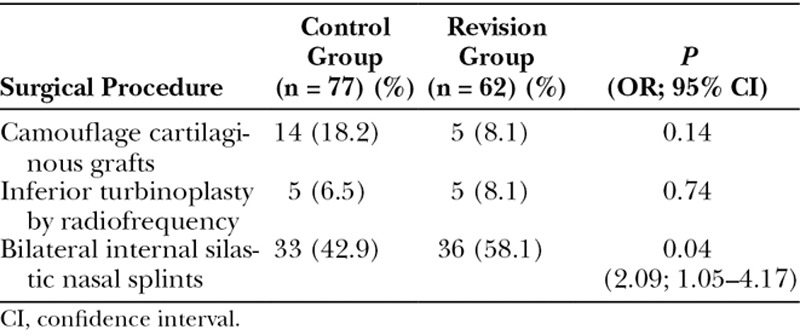
We also have noted that “camouflage” cartilaginous grafts to correct aesthetic defects were more used for patients of the control group compared with the revision group, n = 14 (18.2%) and n = 5 (8.1%; P = 0.14), respectively.
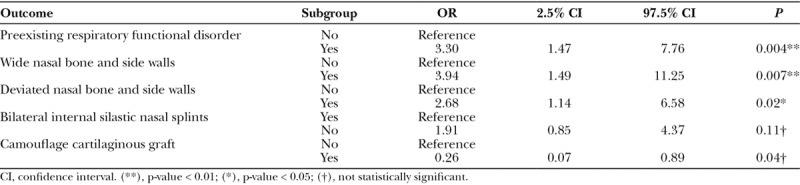
For these 3 statistically significant factors and the 2 other factors for which there was a statistical trend, a multivariate analysis was realized (Table 4). Four factors were independently and statistically associated with revision rhinoplasties: the “preexisting respiratory functional disorders” [OR = 3.30; 95% CI (1.47–7.76); P = 0.004], the “wide nasal bones and side walls” [OR = 3.94; 95% CI (1.49–11.25); P = 0.007], the “deviated nasal bones and side walls” [OR = 2.68; 95% CI (1.14–6.58); P = 0.02] and the use of “camouflage cartilaginous grafts” [OR = 0.26; 95% CI (0.07–0.89); P = 0.04].
Table 4.
Multivariate Analysis
By comparing the characteristics of patients in the revision group for both primary and revision rhinoplasties (Table 5), we have found similar frequencies of functional disorders (66.1% versus 61.3%). Regarding the aesthetic disorders that motivated revision surgeries, the supra-tip humps « pollybeak » were the most frequent and were observed for n = 19 (25.3%) patients. Among the lower section of the nose, the excessive/drooping/“hanging” columellas and/or the alar-nostril sill aesthetic disorders were frequently associated with requests of surgical revision and had similar preoperative frequencies for both primary and secondary rhinoplasties.
Table 5.
Characteristics of Patients of the Revision Group during the Primary and the Revision Rhinoplasties
DISCUSSION
To our best knowledge, we present the first study of both primary and secondary closed rhinoplasty. The revision rate of the main operator was 8.6%. No significant perioperative or postoperative surgical complication was found. We have found 4 factors independently and statistically associated with revision rhinoplasties: (1) the preoperative respiratory functional disorder; (2) the wide; or (3) the deviated aspect of the nose due to nasal bones and sidewalls; and (4) the use of camouflage cartilaginous grafts. After multivariate analyses, the postoperative use of internal silicone splints restraining the nasal septum was not significant.
Revision rates after primary rhinoplasty have been reported as reaching between 5% and 15%.3,4,10–15 Regarding studies in which primary rhinoplasties were mainly performed by open approach,2,4,5 the revision rates were approximately 10%. The revision rate of closed rhinoplasty in our study was similar to that in these studies. As supporting by large literature review, there is no difference between primary open or closed rhinoplasty techniques in relation to revision.16 Despite studied factors could be specific to the surgeon and/or the population studied,17 our results allow us to express several advices.
First, the “preexisting respiratory functional disorders” are predictive factors for surgical revision.18,19 Rhinoplasties cause major changes in the airways.20
Given the previous results, and the similar preoperative frequencies of functional disorders observed for patients of the revision group (Table 5), surgeons should research nasal respiratory functional disorders and especially pay attention to their determinants and impacts before each intervention.
Reviewing primary surgeries, we have found that cartilaginous septum deviations of the revision group differed from the control group. This is supported by the higher frequency of using internal silicone splints in the revision group. In our experience, internal silicone splints were only used for severe septal deviations.
Moreover, we believe that postoperative respiratory functional disorders are multifactorial implicating moderate and residual cartilaginous septum deviation, nasal turbinate hypertrophy, and nasal valve compromise.21 In fact, although the septum nasal deviation represents a key problem area in more than one-third of revision rhinoplasties,22 it does not fully explain the persistence of the functional disorders for our patients. In most cases (91.5%), after the sufficient resection of septal cartilage with preservation of an anterior lower support, the septum was weakened, refocused and formal fixed to nasal spine. Despite these surgical strategies, respiratory functional disorders have persisted. Thus, the systematic resection of the nasal septum was insufficient to correct the preoperative functional disorders.
Surgeons should manage the other determinants of the respiratory function,12 such as correcting the size and volume of the inferior nasal turbinates. In our series, the inferior nasal turbinates hypertrophy was not a statistical predictive factor of revision rhinoplasty. Nevertheless, we have observed their excessive size in more than one-third of patient before revision surgeries. Thus, the inferior turbinates should be considered since they participle to the postoperative the nasal obstruction.21 We made our practice evolved in this field. We increasingly realize inferior turbinoplasties by radiofrequency.
In our study, nasal valve collapse was not significantly associated with revision surgeries. The refinements of the nasal tip by cephalic trim were limited to maintain resistance to contractile forces.17 On the other hand, sections of the lateral crus were rare, and we do not practice sections of the cartilaginous domes. Thus, we aimed to maintain sufficient cartilaginous structures to support collapse forces.23 These cartilaginous surgical procedures could have important consequences.24 Rare and objective nasal valve collapses were managed during secondary rhinoplasties by supporting the airway with alar batten grafts for the lateral wall.25–31
The second and the third predictive factors for revision rhinoplasties were the “wide” and “deviated” nasal bone and sidewalls. Nasal dorsum deformities are the first key problems area for revision rhinoplasty.22 Furthermore, these results are supported by the anatomical features of Turkish/Kurdish patients, which were the most numerous ethnic group of our series.32 They often had very large dorsal humps, thick skins, and under-projected nasal tips. These large dorsal humps spread nasal bones and make them difficult to position on the median line despite the resection of the bone corners.
Regarding the other aesthetic disorders, about a quarter of patients presented and required the correction of supra-tip humps “pollybeak.” Postoperative pollybeaks are known to be significant causes of revision rhinoplasty.33,34 In some cases, pollybeak deformities are due to postoperative loss of nasal tip projection.35 To avoid it, we have systematically anticipated postoperative loss of nasal tip projection by informatics projects and by the importance of the anterior septum resection. In our series, these features were most often related to (i) the thick skin of the nose in tension (“wrestling skin”), very common in this population36; and (2) the postoperative hypertrophic scarring, which one feels perfectly by pinching the skin of the supra-tip called “soft tissue polly-beak.”33 These 2 points explain our results despite the satisfactory resection of the anterior septum and upper lateral cartilages. The management of the skin envelop was sometimes difficult, and good results could be challenging,22,37 requiring various methods and the local steroid injection, retinoic acid, or other systemic or topical agents.38
In our study, aesthetic disorders of the tip were not significantly associated with surgical revisions. However, tip deformities (deprojection, malrotation, abnormal curvature, asymmetry, bulbosity) are mainly associated revision rhinoplasties.3,22,33,39,40 We explain this difference with literature because no interruption of alar cartilage has been performed. On the other hand, we systematically inform patients with thick/tension skins that results of the tip deformities correction are limited. Although the nasal tips could be imperfect, the respect of the natural appearance was in accordance with the expectations of patients. Furthermore, the closed approach offers the advantage to respect more major and minor tip supporting mechanism and avoid unexpected additional deformities.22 In our experience, we preferred:
1) to complete modest computer projects with a relatively short noses,
2) to perform adequate resections of the anterior septum and the upper lateral cartilages and
3) to realize columella-septal sutures to secure the tip cartilages to the caudal septum to effect both tip projection and rotation.41,42
The columella importantly influenced the aesthetic balances of the nose and particularly the tip.43 In our series, the “hanging” columellas were related to the insufficient resection of the caudal septum or to the convex shape of the mesial crus or to soft-tissue deformities. Since the systematic practice of columella-septal suture, the “hanging” columella have almost disappeared.41
Some alar-nostril sill aesthetic disorders (malpositioned lateral crura, short medial crura ...) were noted. These disorders were not related to unfavorable healing of alar base reductions but rather to the insufficient practice of nostril-plasties. The alar-nostril sill aesthetic disorders were more frequently observed in the revision group, but not significantly. Hence, we have decided to perform more frequently these plasties, which improve the nasal harmony.44,45
As a reminder, we have used 2 types of cartilaginous grafts. During primary rhinoplasties, to correct aesthetic disorders such as residual pyramid asymmetry, saddle nose deformity, supratip depression, instability or « low » dorsum, we have used “camouflage” grafts.22 The use of these camouflage grafts was statistically and independently associated with surgical revision. Thus, the use of camouflage grafts during primary rhinoplasty is protective from surgical revision.
During revision surgeries, Spreader grafts were useful for patients with bad septum deviation that required reconstruction.46,47
Interestingly, certain disorders observed by the surgeon differed from the patient’s requests. However, these revision requests were legitimate and once they were corrected, patient satisfaction was obtained.48
Some limitations are due to our retrospective data collection. First of all, some confounding factors may not have been identified. In addition, the revision rate may be underestimated by the relatively limited long-term follow-up. After all these inherent limitations due to our retrospective design, our study includes some relatively large groups of patients with available data blinded analyzed. Moreover, the revision rate of our study was concordant with those observed on several other series, performed by other surgeons, with open approach, for different populations.3–5,16 The incision technique in closed approach does not require supplementary external incisions and allows access to all parts of the nose. On the other hand, it requires more experience for the surgeon due to the reduced intra-operative view.49
This study has changed our managing of rhinoplasties and allows us to propose some advice.
First of all, surgeons should identify what are the patient requests and how to respond to each situation. Preoperative clinical examination should be standardized, with focus on both functional and aesthetic disorders. This assessment remains one of the keys to successful rhinoplasty surgery.50 Regarding functional disorders, the preestablished and validated surveys and the NOSE questionnaire should be used.6,7
In case of functional trouble, even if limited, the surgeon should manage it to reduce the risk of revision.51 Different techniques could be used such as the correction of deviated anterior nasal spine with sufficient resection of the anterior septum,21,22 the alar batten grafts for the lateral wall to support the airway from nasal valve collapse,25–31 and the realization of a lower turbinoplasty by radiofrequency.
Regarding aesthetic disorders, especially for the dorsum and the supra-tip, camouflage cartilaginous grafts should be considered.3,22,33,39,40 We recommend integrating preoperative computer project to better objectify with patients the aesthetic disorders and to predict more realistic results.2
Finally, communication with patients is of fundamental importance for a successful surgery.52 Surgeons should inform their patients that surgical revisions could be necessary after the healing phase. Satisfaction of the patients is obtained only if they are informed and aware of the surgical challenge of their noses.53,54
CONCLUSIONS
Closed rhinoplasty remains a valid technique for experienced surgeons and has a revision rate (8.8%) similar to open approaches. In addition to systematic sufficient resection of the nasal septum, the correction of functional disorders frequently requires inferior turbinoplasties by radiofrequency. Regarding aesthetic predictive factors, patients with wide or deviated noses have an increased risk for surgical revision. In case of aesthetic defects or irregularities, using camouflage cartilaginous grafts seems to be protector from revision surgery. The interests of this study are to better inform patients and to adapt operative management. Prospective studies with more objective data may teach us more about predictive factors of revision rhinoplasty.
Footnotes
Published online 5 September 2018.
Presented at the ENT world congress (IFOS) meeting 2017 in Paris, France.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Rudy SF, Most SP. Rhinoplasty. JAMA. 2017;318:1406. [DOI] [PubMed] [Google Scholar]
- 2.Neaman KC, Boettcher AK, Do VH, et al. Cosmetic rhinoplasty: revision rates revisited. Aesthet Surg J. 2013;33:31. [DOI] [PubMed] [Google Scholar]
- 3.Parkes ML, Kanodia R, Machida BK. Revision rhinoplasty. An analysis of aesthetic deformities. Arch Otolaryngol Head Neck Surg. 1992;118:695. [DOI] [PubMed] [Google Scholar]
- 4.Kamer FM, McQuown SA. Revision rhinoplasty. Analysis and treatment. Arch Otolaryngol Head Neck Surg. 1988;114:257. [DOI] [PubMed] [Google Scholar]
- 5.Bagheri SC, Khan HA, Jahangirnia A, et al. An analysis of 101 primary cosmetic rhinoplasties. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2012;70:902. doi:10.1016/j.joms.2011.02.075. [DOI] [PubMed] [Google Scholar]
- 6.Rhee JS, Sullivan CD, Frank DO, et al. A systematic review of patient-reported nasal obstruction scores: defining normative and symptomatic ranges in surgical patients. JAMA Facial Plast Surg. 2014;16:219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stewart MG, Witsell DL, Smith TL, et al. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg. 2004;130:157. [DOI] [PubMed] [Google Scholar]
- 8.Fung E, Hong P, Moore C, et al. The effectiveness of modified cottle maneuver in predicting outcomes in functional rhinoplasty. Plast Surg Int. 2014;2014:618313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rhee JS, Weaver EM, Park SS, et al. Clinical consensus statement: diagnosis and management of nasal valve compromise. Otolaryngol Head Neck Surg. 2010;143:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dziewulski P, Dujon D, Spyriounis P, et al. A retrospective analysis of the results of 218 consecutive rhinoplasties. Br J Plast Surg. 1995;48:451. [DOI] [PubMed] [Google Scholar]
- 11.Goudakos JK, Daskalakis D, Patel K. Revision rhinoplasty: retrospective chart review analysis of deformities and surgical maneuvers in patients with nasal airway obstruction—five years of experience. Facial Plast Surg. 2017;33:334. [DOI] [PubMed] [Google Scholar]
- 12.Lee M, Zwiebel S, Guyuron B. Frequency of the preoperative flaws and commonly required maneuvers to correct them: a guide to reducing the revision rhinoplasty rate. Plast Reconstr Surg. 2013;132:769. doi:10.1097/PRS.0b013e3182a01457. [DOI] [PubMed] [Google Scholar]
- 13.Pearlman SJ, Talei BA. An anatomic basis for revision rhinoplasty. Facial Plast Surg. 2012;28:390. [DOI] [PubMed] [Google Scholar]
- 14.Cvjetković N, Lustica I. [Secondary rhinoplasty (analysis of failures over a 5-year period)]. Lijec Vjesn. 1997;119:68. [PubMed] [Google Scholar]
- 15.Byrd HS, Hobar PC. Rhinoplasty: a practical guide for surgical planning. Plast Reconstr Surg. 1993;91:642. [PubMed] [Google Scholar]
- 16.Crosara PF, Nunes FB, Rodrigues DS, et al. Rhinoplasty complications and reoperations: systematic review. Int Arch Otorhinolaryngol. 2017;21:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pawar SS, Garcia GJ, Rhee JS. Advances in technology for functional rhinoplasty: the next frontier. Facial Plast Surg Clin North Am. 2017;25:263. [DOI] [PubMed] [Google Scholar]
- 18.Toriumi DM. Discussion: frequency of the preoperative flaws and commonly required maneuvers to correct them: a guide to reducing the revision rhinoplasty rate. Plast Reconstr Surg. 2013;132:777. [DOI] [PubMed] [Google Scholar]
- 19.Thomson C, Mendelsohn M. Reducing the incidence of revision rhinoplasty. J Otolaryngol. 2007;36:130. [DOI] [PubMed] [Google Scholar]
- 20.Guyuron B. Nasal osteotomy and airway changes. Plast Reconstr Surg. 1998;102:856. [PubMed] [Google Scholar]
- 21.Garcia GJM, Rhee JS, Senior BA, et al. Septal deviation and nasal resistance: an investigation using virtual surgery and computational fluid dynamics. Am J Rhinol Allergy. 2010;24:46. [DOI] [PubMed] [Google Scholar]
- 22.East C, Kwame I, Hannan SA. Revision rhinoplasty: what can we learn from error patterns? An analysis of revision surgery. Facial Plast Surg. 2016;32:409. [DOI] [PubMed] [Google Scholar]
- 23.Oliaei S, Manuel C, Protsenko D, et al. Mechanical analysis of the effects of cephalic trim on lower lateral cartilage stability. Arch Facial Plast Surg. 2012;14:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ishii LE, Rhee JS. Are diagnostic tests useful for nasal valve compromise? Laryngoscope. 2013;123:7. [DOI] [PubMed] [Google Scholar]
- 25.Chua DY, Park SS. Alar batten grafts. JAMA Facial Plast Surg. 2014;16:377. [DOI] [PubMed] [Google Scholar]
- 26.Xavier R. Nasal valve collapse treatment. JAMA Facial Plast Surg. 2014;16:66. [DOI] [PubMed] [Google Scholar]
- 27.Sufyan AS, Hrisomalos E, Kokoska MS, et al. The effects of alar batten grafts on nasal airway obstruction and nasal steroid use in patients with nasal valve collapse and nasal allergic symptoms: a prospective study. JAMA Facial Plast Surg. 2013;15:182. [DOI] [PubMed] [Google Scholar]
- 28.Bewick JC, Buchanan MA, Frosh AC. Internal nasal valve incompetence is effectively treated using batten graft functional rhinoplasty. Int J Otolaryngol. 2013;2013:734795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cervelli V, Spallone D, Bottini JD, et al. Alar batten cartilage graft: treatment of internal and external nasal valve collapse. Aesthetic Plast Surg. 2009;33:625. doi:10.1007/s00266-009-9349-5. [DOI] [PubMed] [Google Scholar]
- 30.Becker DG, Becker SS. Treatment of nasal obstruction from nasal valve collapse with alar batten grafts. J Long Term Eff Med Implants. 2003;13:259. [DOI] [PubMed] [Google Scholar]
- 31.Toriumi DM, Josen J, Weinberger M, et al. Use of alar batten grafts for correction of nasal valve collapse. Arch Otolaryngol Head Neck Surg. 1997;123:802. [DOI] [PubMed] [Google Scholar]
- 32.Niechajev I. Noses of the middle east: variety of phenotypes and surgical approaches. J Craniofac Surg. 2016;27:1700. [DOI] [PubMed] [Google Scholar]
- 33.Rettinger G. Risks and complications in rhinoplasty. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2008;6 Available at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3199839/. Accessed July 22, 2017. [PMC free article] [PubMed] [Google Scholar]
- 34.Holt GR, Garner ET, McLarey D. Postoperative sequelae and complications of rhinoplasty. Otolaryngol Clin North Am. 1987;20:853. [PubMed] [Google Scholar]
- 35.Moubayed SP, Most SP. Revision of the nasal dorsum. Facial Plast Surg FPS. 2017;33:202. doi:10.1055/s-0036-1598017. [DOI] [PubMed] [Google Scholar]
- 36.Erol OO. Tip rhinoplasty in broad noses in a Turkish population: Eurasian noses. Plast Reconstr Surg. 2012;130:185. [DOI] [PubMed] [Google Scholar]
- 37.Adamson PA, Warner J, Becker D, et al. Revision rhinoplasty: panel discussion, controversies, and techniques. Facial Plast Surg Clin North Am. 2014;22:57. [DOI] [PubMed] [Google Scholar]
- 38.Hussein WKA, Foda HMT. Pollybeak deformity in middle eastern rhinoplasty: prevention and treatment. Facial Plast Surg FPS. 2016;32:398. doi:10.1055/s-0036-1585571. [DOI] [PubMed] [Google Scholar]
- 39.Bracaglia R, Fortunato R, Gentileschi S. Secondary rhinoplasty. Aesthetic Plast Surg. 2005;29:230. [DOI] [PubMed] [Google Scholar]
- 40.Kridel RW, Soliemanzadeh P. Tip grafts in revision rhinoplasty. Facial Plast Surg Clin North Am. 2006;14:331. [DOI] [PubMed] [Google Scholar]
- 41.Gruber RP, Weintraub J, Pomerantz J. Suture techniques for the nasal tip. Aesthet Surg J. 2008;28:92. [DOI] [PubMed] [Google Scholar]
- 42.Harrison DH. Reflections on the open and closed rhinoplasty. J Plast Reconstr Aesthet Surg. 2013;66:1356. [DOI] [PubMed] [Google Scholar]
- 43.Rohrich RJ, Afrooz PN. Components of the hanging columella: strategies for refinement. Plast Reconstr Surg. 2018;141(1):46e. [DOI] [PubMed] [Google Scholar]
- 44.Rosenberger ES, Toriumi DM. Controversies in revision rhinoplasty. Facial Plast Surg Clin North Am. 2016;24:337. [DOI] [PubMed] [Google Scholar]
- 45.Totonchi A, Guyuron B. Alar rim deformities. Clin Plast Surg. 2016;43:127. [DOI] [PubMed] [Google Scholar]
- 46.Wee JH, Lee JE, Cho SW, et al. Septal batten graft to correct cartilaginous deformities in endonasal septoplasty. Arch Otolaryngol Head Neck Surg. 2012;138:457. [DOI] [PubMed] [Google Scholar]
- 47.Matthias C. Surgery of the nasal septum and turbinates. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2007;6:Doc10 Available at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3199838/. Accessed July 22, 2017. [PMC free article] [PubMed] [Google Scholar]
- 48.Constantian MB. What motivates secondary rhinoplasty? A study of 150 consecutive patients. Plast Reconstr Surg. 2012;130:667. [DOI] [PubMed] [Google Scholar]
- 49.Berghaus A. Modern rhinoplasty: is there a place for the closed approach? Facial Plast Surg. 2016;32:402. [DOI] [PubMed] [Google Scholar]
- 50.Paun SH, Nolst Trenité GJ. Revision rhinoplasty: an overview of deformities and techniques. Facial Plast Surg. 2008;24:271. [DOI] [PubMed] [Google Scholar]
- 51.Spataro E, Piccirillo JF, Kallogjeri D, et al. Revision rates and risk factors of 175 842 patients undergoing septorhinoplasty. JAMA Facial Plast Surg. 2016;18:212. doi:10.1001/jamafacial.2015.2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Loyo M, Wang TD. Revision rhinoplasty. Clin Plast Surg. 2016;43:177. [DOI] [PubMed] [Google Scholar]
- 53.Abbas OL. Revision rhinoplasty: measurement of patient-reported outcomes and analysis of predictive factors. Springerplus. 2016;5:1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khansa I, Khansa L, Pearson GD. Patient satisfaction after rhinoplasty: a social media analysis. Aesthet Surg J. 2016;36:NP1. [DOI] [PubMed] [Google Scholar]


