Abstract
Objective:
To examine the difference between outcomes in the administration of concurrent endoscopic sinus surgery (ESS), septoplasty (SP), and rhinoplasty (RP) and concurrent ESS and SP in 1 single surgical session.
Methods:
Patients who underwent concurrent ESS and SP from September 2004 to July 2015 were identified. Furthermore, patients among them who underwent functional primary RP were selected. Subjects who had been administered concurrent ESS, SP, and RP (primary RP) were matched for sex, age, sinonasal surgical procedures for treatment of chronic rhinosinusitis with patients underwent concurrent ESS and SP, used as control subjects. A literature review was performed to find previous articles describing results of concurrent procedures among ESS, SP, and RP.
Results:
Twenty subjects, who underwent concurrent ESS, SP, and RP, were compared with a matched control group made of 20 patients who underwent concurrent ESS and SP, evaluating different postoperative outcomes (postoperative complications, postoperative improvement of respiratory symptoms, persistence of chronic rhinosinusitis symptoms 6 months to 1 year postoperative, need of revision surgery, satisfaction of the patient). Obtained P values showed that there was no statistically significant difference (P > 0.05) as regards the different outcomes, except for postoperative complications, increased because of the invasiveness proper of RP (P < 0.05).
Conclusions:
Therefore, execution of concurrent ESS, SP, and RP seems to be safe and effective, and additional RP does not modify postoperative outcomes of concurrent ESS and SP except for a little increase of postoperative complications, even if most of them had low impact on result of procedures.
INTRODUCTION
Procedures of endoscopic sinus surgery (ESS), septoplasty (SP), and rhinoplasty (RP) were originally conceived with a functional aim to which today it is added an aesthetic target, and all these procedures contribute to safeguard and restore the binomium “shape and function” in a morphodynamic perspective. The functional aim stands in the recover of normal sinonasal physiology and ventilatory function, if impaired by different noxae resulting in chronic rhinosinusitis (CRS), and by primary (congenital defects) or secondary (trauma, etc.) causes with consequent septal alterations or external nose deformity.1 All these conditions can coexist in a single subject and need to be solved.
Traditionally, concurrent ESS and RP, with or without SP, was considered a high risk association because of postoperative complications, due to infections, prolonged bleeding and swelling and impairment of morphofunctional result of RP.2,3 But several authors considered the possibility of coupling and combining ESS, SP, and RP, because this association offers advantages like solving all at once the pathologies above, single general anesthetic and recovery period, reduced expenses for the structure, at the price of increasing the risk of postoperative complications and obviously operative time.4–10 Due to a wide international literature that conduced several surveys (retrospective series, case report, case-control studies) evaluating different combinations of procedures, we tried to take stock of the topic with a case–control study comparing a study group who underwent to concurrent ESS, SP, and RP with a control group of selected and matched subjects who underwent to ESS and SP only. Moreover, our research attempted to answer the question about the benefits of concurrent ESS, SP, and RP instead of defer the procedures in different surgical session and tried to close the cycle of surveys in which were previously involved authors such as Sclafani and Schaefer,11 Shafik and Youssef,12 and Kim et al.13 as well, who verified, through case–control studies, the effectiveness and safeness of ESS, SP, and RP differently combined. Specifically, in previous studies Sclafani and Schaefer11 considered SP and rhinoplasty with or without ESS, Shafik and Youssef12 considered endoscopic SP with or without rhinoseptoplasty and Kim et al.13 analyzed effect of open rhinoplasty with or without ESS and SP.
MATERIALS AND METHODS
Between September 2004 and July 2015, a total amount of 385 patients received in Universitary Hospital Policlinico “P. Giaccone”, Palermo, Italy, concurrent ESS and SP and, among them, 28 subjects underwent concurrent ESS, SP, and RP. Our institutional review board approved the present study, and all patient signed an informed consent.
We managed to contact and enroll them in our retrospective review consisting in the evaluation of clinical charts data and the submission of a questionnaire, based on the model of questionnaire by Bhattacharyya, 2005, Rhinosinusitis Symptom Inventory,14 about postoperative results to characterize 5 different outcomes: postoperative complications, postoperative improvement of respiratory symptoms, persistence of CRS symptoms (to each symptoms a score from 0 to 5 was ascribed), need of revision surgery, patient’s satisfaction. Eight of them refused to be included in this survey; hence, we considered only 20 patients as a study group that underwent concurrent ESS, SP, and RP and agreed to take part in this project. Moreover, we matched them with other 20 subjects among the remaining 357 patients that underwent concurrent ESS and SP only using matching criteria of sex (male or female), age (± 11 years), and sinonasal surgical procedures (paranasal sinuses underwent to surgery, even if a perfect overlapping between the 2 groups was not possible due to broad variability of extension of sinonasal pathology and related surgical treatment. Turbinate reduction with radiofrequency (RF) that was considered as an additional procedure and not as a strictly necessary criterion to match patients). The same evaluation of clinical charts data was conduced and the same questionnaire was submitted to them to enable a comparison of obtained outcomes between the study group (concurrent ESS, SP, RP) and the control group (concurrent ESS and RP).
The average age was 36.2 ± 8.9 years (range, 23–48 years) in the group of study, 37.4 ± 8.3 years (range, 24–50 years) in the group of control, and there were 7 men and 13 women for each group.
Mean postoperative follow-up was 4.9 ± 2.9 years in study group and 3.3 ± 2.7 years in control group.
All patients underwent surgery after performing preoperative computed tomography scans of their paranasal sinuses, and all of them were no responsive to maximum medical therapy for CRS. In facts, they had been previously administered more than 1 month CRS therapy (antibiotics, topic and systemic steroids, nasal saline irrigation, etc.). Patients with severe CRS were not excluded from being candidate to rhinoplasty.
ESS was performed under general anesthesia with classic anterior to posterior technique, opening the sinuses and ethmoidal cells involved by inflammatory disease. SP was performed after ESS, with 38 patients who underwent complete SP with hemitransfix incision and mucoperichondrial-mucoperiosteal flap elevation and 2 patients received limited SP. The removed portion was used as graft, after remodeling and reshaping, to complete SP.
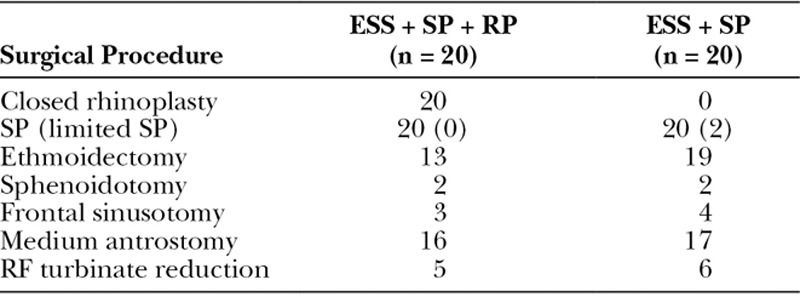
Turbinates were treated with RF turbinate reduction in 5 patients in study group (ESS + SP + RP) and in 6 patients in control group (ESS + SP).
Closed rhinoplasty was performed in the study group and was conduced with closed approach. Elevation of skin was conduced to identify a supraperichondral and supraperiosteal plane through which operations of osteotomy and remodeling of alar cartilages were performed. The alar cartilages were reshaped to improve the airflow and obtain an elevation of the tip of the nose. Where necessary, a cartilage autologous graft from the septum was placed in columellar site or in nasal dorsum site. A summary of surgical procedures can be observed in Table 1.
Table 1.
Summary of Surgical Procedures Performed in Study Group (ESS + SP + RP) and Control Group (ESS + SP)
All patient received postoperative antibiotics (cephalosporins), and packing was made with povidone-iodine soaked cotton lint, Merocel (Medtronic Xomed, Jacksonville, Fla.) and Silastic (Dow Corning Corporation, Midland, Mich.) for 72 hours. Gelita-Cel (GELITA MEDICAL GmbH, Eberbach, Del.) was used to obtain hemostasis in involved sinuses. Rhinoplasty group had also placed a nasal metal band and Steri-Strip to immobilize the bones and teguments for a period of 2 weeks postoperative. All patient had 1 night of hospitalization.
Statistical evaluation was based on analysis of odds ratio (OR) and 2-tailed McNemar exact test for each considered outcomes. A value of P < 0.05 was regarded as statistically significant. Both the evaluations were obtained with MS Office Excel 2015.
RESULTS
The obtained results from clinical charts data evaluation and questionnaire can be observed in Table 2. Statistical evaluations are reported in Table 3.
Table 2.
Obtained Results from Clinical Charts Data Evaluation and Questionnaire
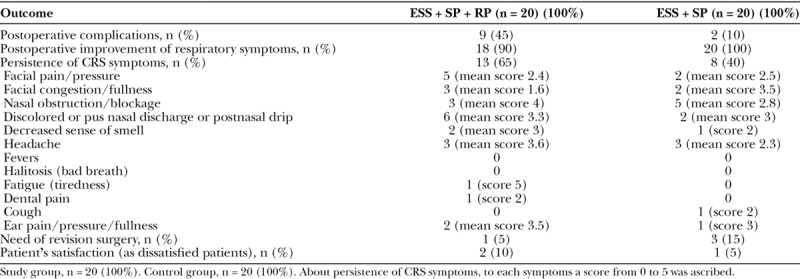
Table 3.
Statistical Evaluations about Outcomes, Based on Analysis of OR and 2-tailed McNemar Exact Test
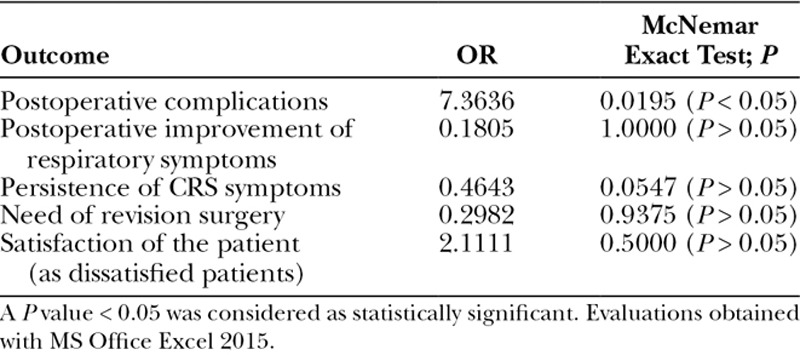
Postoperative complications verified in 45% (9) of patients in study group (ESS + SP + RP), but most of them had little significant impact on surgery result. Two patients had periorbital ecchymosis and major epistaxis that prolonged hospitalization, 1 patient had nasal dorsum depression, 2 patients had periorbital ecchymosis and minor epistaxis, 1 patient had periorbital ecchymosis and transient hyposmia, 1 patient had periorbital ecchymosis, minor epistaxis and transient hyposmia, 2 patients had periorbital ecchymosis only. In control group (ESS + SP) postoperative complications rate was 10% (2 patients) in which 1 patient had transient hyposmia and 1 had minor epistaxis. The OR was 7.3636 with a 95% confidence interval, extending from 1.3372 to 40.5492 and P value obtained was 0.0195 (P < 0.05). The OR > 1 confirms that concurrent ESS, SP, and RP could be implicated in increasing of postoperative complications and also the small P value suggests that there is an association between concurrent ESS, SP, and RP and postoperative complications, due to proper invasiveness of RP.
Postoperative improvement of nasal obstruction had been a success in both groups, with a rate of 90% in the study group (18 patients) and a rate of 100% (20 patients) in the control group. OR was 0.1805 and its confidence interval was 95%, extending from 0.0081 to 4.0096. McNemar exact test obtained a P value of 1.0000 (P > 0.05), and the difference between study group and control group was not statistically significant. Moreover, there was no association between concurrent ESS, SP, and RP, and postoperative improvement of nasal obstruction that was similar in both groups.
Persistence of CRS symptoms in the follow-up after surgical treatment was different between the 2 groups: 13 patients (65%) had persisting symptoms in the study group, 8 patients (40%) in the control group, with a OR of 0.4643, with a 95% confidence interval extending from 0.0766 to 2.8129, and a P value of 0.0547 (P > 0.05). The obtained difference was not statistically significant enough; therefore, there was no association between concurrent ESS, SP, and RP and persistence of CRS symptoms.
The most persisting symptoms, evaluated with a modification of Rhinosinusitis Symptom Inventory questionnaire were anterior rhinorrhea and/or postnasal drip (6 patients) and facial pain/pressure (5 patients) in the study group, and nasal obstruction/blockage (5 patients) and headache (3 patients) in the control group. Arithmetic mean was calculated only among patients presenting the symptoms, not considering patients who gave score 0 to the different symptoms.
The need of revision surgery showed a rate of 5% in study group (1 patient required a revision of SP to reposition of septal cartilage graft) and a rate of 15% in the control group (3 patients required revision of ESS because of an inadequate correction of sinus disease), with an OR of 0.2982, with a 95% confidence interval extending from 0.0283 to 3.1458 and a P value of 0.9375 (P > 0.05). There was no statistically significant difference between the 2 groups, and no association between concurrent ESS, SP, and RP and needs of revision surgery was found.
Patients’ satisfaction was considered as patients unsatisfied about received treatment. Dissatisfaction rate in the study group was 10% (2 patients) and 5% (1 patient) in the control group. Obtained OR was 2.1111 with a 95% confidence interval extending from 0.1758 to 25.3499 and obtained P value was 0.5000. No statistically significant difference was found between the 2 groups, suggesting there was no association between concurrent ESS, SP, and RP and patients’ dissatisfaction.
DISCUSSION
This study shows that there is no significant difference between patients who underwent concurrent ESS, SP, and RP and patients who underwent concurrent ESS and SP only, as regards outcomes like postoperative improvement of respiratory symptoms, persistence of CRS symptoms in the follow-up, need of revision surgery, patient’s satisfaction, but presents a statistically significant difference as regards the postoperative complications. The ESS done for tumor lesions, being generally more extensive, should be considered separately for high risk of complication rate.15
The postoperative improvement of respiratory symptoms shows an OR < 1 and P > 0.05. Symptoms, indeed, seem to improve the same way in both groups of patients and additional RP does not nullify the effect of CRS and septal deformity treatment.
Moreover, even the persistence of CRS symptoms does not experience any negative change in patients who underwent concurrent triple surgery (ESS, SP, RP) compared with subjects who underwent ESS and SP only, as confirmed by OR < 1 and P value (> 0.05). Besides the not statistically significant difference that may be attributable to the small sample, it can be assumed that the trend of major rate of persistence of CRS symptoms in the study group could be due to a more severe CRS in the study group. Therefore, the result related to the persistence of CRS symptoms could also be the result of chance. A larger study, with larger cohorts, could suggest the less favorable outcome of RP in addition to ESS and SP or completely disprove it.
The need of revision surgery does not show statistically significant differences between the 2 groups (P > 0.05) and compared with which obtained by Kim et al.13 (ESS + SP + OR group 8.8%) and Shafik and Youssef12 (ESS + SP + RP group 10%), our patients had less postoperative complications (study group ESS, SP, RP 5%), and we should consider that even if our statistic sample was not large; however, it was comparable to them as well (57 versus 57 patients in the study by Kim et al.13, 20 versus 20 patients in the study by Shafik and Youssef12).
Patients with severe CRS were not excluded from both groups. This could explain the higher rate of revision in the control group and the observed trend of persistence of CRS symptoms in study group as mentioned above.
The rate of patients’ satisfaction is similar in the 2 groups, with a major percentage in the control one, an OR > 1 and a P value > 0.05. In study group, 2 patients were dissatisfied about surgery and reason was the aesthetic result. They did not mention problems related to respiratory function. In control group, just 1 patient was dissatisfied about the functional result. Compared with Kim’s experience where the successful outcome related to ESS + SP + OR group was 82.5% with an unsuccessful outcome of 17.5%,13 our result appears to be the better in our study group (concurrent ESS, SP, RP) with a satisfaction rate of 90% and a dissatisfaction rate of 10%.
An ostensible negative but predictable result regards postoperative complications. Obtained P value (P < 0.05) and OR (OR > 1) seem to be directed toward a contraindication of additional RP to concurrent ESS and SP surgery. This result could seem alarming. Nevertheless, if we consider that RP is an invasive procedure, which brings an increase of postoperative time, risk of infections, bleeding and ecchymosis, when we analyze the reported complications above, we can see that most of them are minor complications that do not have negative effects on the results of the surgery.
If complications are considered divided between major5,16 and minor,17,18 it is obtained that patients with major complications in study group were 3 with a rate of 15% (2 patients with periorbital ecchymosis and major epistaxis that prolonged hospitalization and 1 patient with nasal dorsum depression), whereas in control group, no patient reported major complication (0%), with a not statistically significant difference (P > 0.05). As regards minor complications, in study group 6 patients were involved, with a rate of 30% (2 patients with periorbital ecchymosis and minor epistaxis, 1 patient with periorbital ecchymosis and transient hyposmia, 1 patient with periorbital ecchymosis, minor epistaxis and transient hyposmia, and 2 patients with periorbital ecchymosis), whereas in control group, only 2 patient had minor complications with a rate of 10% (1 with minor epistaxis and 1 with transient hyposmia) and with a not statistically significant difference (P > 0.05). Hence, the difference that is obtained is not statistically significant if major complications and minor complication are considered separately and minor complications have not a high impact on the outcome of the surgery and on the patient’s quality of life. If considering that, in study group where an extra surgical procedure is performed (rhinoplasty), in our opinion, it is acceptable an increasing of minor complications, even performing a closed rhinoplasty.
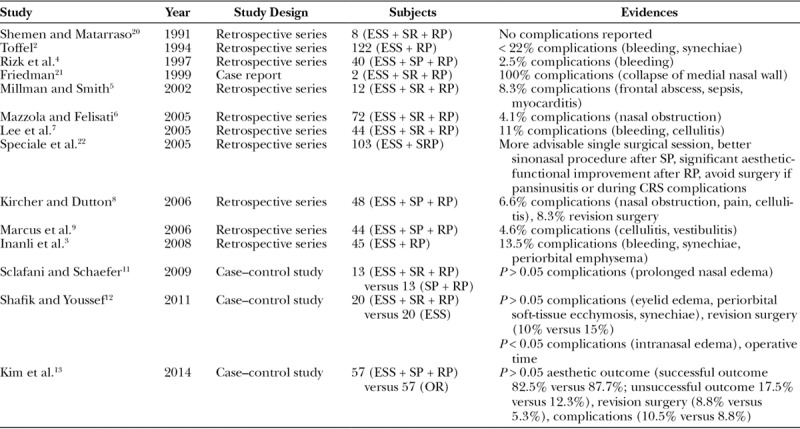
A summary of the previous literature can be observed in Table 4, modified from Patel et al.19
Table 4.
Summary of the Previous Literature about ESS Combined with SP and RP, Modified from Patel et al.,19 from 1991 to 2014
CONCLUSIONS
Therefore, we can assume that concurrent ESS, SP, and RP could be considered, in the light of all previous literature and relying on our results, an affordable, reliable, and safe association that can be used to reduce operative time, general anesthetic, and recovery period, stress of patients who undergoing a single surgical session.
The additional RP leads to an increase in postoperative complications when globally considered, but if analyzed separately, many of these are considered minor from literature.17,18 Hence, the result of surgery and the patient’s quality of life are not excessively compromised and in our opinion they could be considered acceptable.
Our statistic sample was not so large, but it was comparable to other authors’ samples. A future study with a larger sample, however, could better define a stronger evidence of how RP affects outcomes of concurrent ESS and SP.
Footnotes
Published online 14 September 2018.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the University of Padua.
REFERENCES
- 1.Dispenza F, Saraniti C, Sciandra D, et al. Management of naso-septal deformity in childhood: long-term results. Auris Nasus Larynx. 2009;36:665. [DOI] [PubMed] [Google Scholar]
- 2.Toffel PH. Simultaneous secure endoscopic sinus surgery and rhinoplasty. Ear Nose Throat J. 1994;73:554. [PubMed] [Google Scholar]
- 3.Inanli S, Sari M, Yazici MZ. The results of concurrent functional endoscopic sinus surgery and rhinoplasty. J Craniofac Surg. 2008;19:701. [DOI] [PubMed] [Google Scholar]
- 4.Rizk SS, Edelstein DR, Matarasso A. Concurrent functional endoscopic sinus surgery and rhinoplasty. Ann Plast Surg. 1997;38:323. [DOI] [PubMed] [Google Scholar]
- 5.Millman B, Smith R. The potential pitfalls of concurrent rhinoplasty and endoscopic sinus surgery. Laryngoscope. 2002;112:1193. [DOI] [PubMed] [Google Scholar]
- 6.Mazzola RF, Felisati G. Rhinoplasty and endoscopic surgery for functional and inflammatory nasal/sinus disorders. Plast Reconstr Surg. 2005;115:705. [DOI] [PubMed] [Google Scholar]
- 7.Lee JH, Sherris DA, Moore EJ. Combined open septorhinoplasty and functional endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2005;133:436. [DOI] [PubMed] [Google Scholar]
- 8.Kircher ML, Dutton JM. Concurrent endoscopic sinus surgery and rhinoplasty. Am J Rhinol. 2006;20:485. [DOI] [PubMed] [Google Scholar]
- 9.Marcus B, Patel Z, Busquets J, et al. The utility of concurrent rhinoplasty and sinus surgery: a 2-team approach. Arch Facial Plast Surg. 2006;8:260. [DOI] [PubMed] [Google Scholar]
- 10.Dispenza F, Gallina S, Mathur N, et al. Endoscopic septoplasty in combination with functional endoscopic sinus surgery: our indications. Otorinolaringologia. 2010;60:7. [Google Scholar]
- 11.Sclafani AP, Schaefer SD. Triological thesis: concurrent endoscopic sinus surgery and cosmetic rhinoplasty: rationale, risks, rewards, and reality. Laryngoscope. 2009;119:778. [DOI] [PubMed] [Google Scholar]
- 12.Shafik AG, Youssef TA. Benefit of combined endoscopic sinus surgery and aesthetic rhinoplasty. Auris Nasus Larynx. 2013;40:71. [DOI] [PubMed] [Google Scholar]
- 13.Kim JH, Cho GS, Cheang PP, et al. The effects of endoscopic sinus surgery on the postoperative outcomes of open rhinoplasty. Ann Otol Rhinol Laryngol. 2014;123:240. [DOI] [PubMed] [Google Scholar]
- 14.Bhattacharyya N, Lee KH. Chronic recurrent rhinosinusitis: disease severity and clinical characterization. Laryngoscope. 2005;115:306. [DOI] [PubMed] [Google Scholar]
- 15.Marchese D, Aleo G, Gallina S, et al. Personal experience on inverted papilloma surgical treatment. EuroMediterranean Biomed J. 2013;8:85. [Google Scholar]
- 16.Hosemann WG, Weber RK, Keerl RE, et al. Minimally Invasive Endonasal Sinus Surgery. 2000, Stuttgart, N.Y.: Thieme; 84. [Google Scholar]
- 17.Terrel JE. Cummings CW, Friedrickson JM, Harker LA, et al. Primary sinus surgery. In: Otolaryngology-Head & Neck Surgery. Vol 1998: 2 3rd ed St. Louis: Mosby; 1160. [Google Scholar]
- 18.Levine HL, May M. Endoscopic Sinus Surgery. 1993New York, N.Y.: Thieme Medical Publishers Inc.; [Google Scholar]
- 19.Patel ZM, Setzen M, Sclafani AP, et al. Concurrent functional endoscopic sinus surgery and septorhinoplasty: using evidence to make clinical decisions. Int Forum Allergy Rhinol. 2013;3:488. [DOI] [PubMed] [Google Scholar]
- 20.Shemen LJ, Matarraso A. Combined endoscopic sinus surgery and aesthetic rhinoplasty: a pilot study. Am J Rhinol. 1991;5:131. [Google Scholar]
- 21.Friedman WH. Endorhinoplasty: simultaneous rhinoplasty and endoscopic ethmoidectomy. Facial Plast Surg Clin North Am. 1999;7:357. [Google Scholar]
- 22.Speciale R, Gargano R, Poma S, et al. Staffieri A. Combinare F.E.S.S. e settorinoplastica. Perché, quando e come. La Chirurgia estetica facciale nella prospettiva ORL: oltre la rinoplastica. 2005;Torino: Edizioni Minerva Medica; 1. [Google Scholar]


