Abstract
Objective:
Although family-based therapy (FBT) is a well-established treatment for anorexia nervosa, its implementation and effectiveness in clinical settings has been neglected.
Method:
Seven therapists at a community-based eating disorders clinic were trained in skills-enhanced FBT and provided treatment to 11 youth with anorexia nervosa. Family-based skills training, which borrowed heavily from dialectical behavior therapy, was introduced in four additional sessions and then integrated throughout the remainder of FBT.
Results:
FBT was perceived as “appropriate” and “acceptable” by all participants. Therapists reported high treatment fidelity. There was a large improvement in weight and moderate improvement in caregiver-reported eating disorder psychopathology but no clinically significant change by youth report.
Conclusions:
This study provides preliminary data on the implementation and effectiveness of FBT in the community.
Keywords: implementation, family-based treatment, dialectical behavior therapy, anorexia nervosa, youth
Although evidence-based psychosocial treatments are available for various childhood psychiatric disorders (David-Ferdon & Kaslow, 2008; Higa-McMillan, Francis, Rith-Najarian, & Chorpita, 2016; Hogue, Henderson, Ozechowski, & Robbins, 2014; McCart & Sheidow, 2016), they are not routinely implemented in clinical settings (Garland et al., 2010; Mitchell, 2011; Weisz, Ng, & Bearman, 2014). One avenue for bridging the research-practice gap is through implementation research, which seeks to generate new knowledge to understand the adoption, implementation, and sustainment of evidence-based treatments in community practice. Dissemination and implementation models have focused largely on higher prevalence disorders, such as mood, anxiety, and disruptive behavior disorders. While these efforts serve the largest number of youth, they neglect several high risk disorders, including eating disorders.
Eating disorders, such as anorexia nervosa (AN) and bulimia nervosa, are associated with high suicide risk (Crow, Swanson, Le Grange, Feig, & Merikangas, 2014) as well as numerous medical complications, including loss of muscle mass, cardiac muscle complications, amenorrhea, electrolyte abnormalities, and seizures (Andersen & Yager, 2009), resulting in the highest mortality rate (4–5%; Crow et al., 2009) of any psychiatric disorder (Arcelus, Mitchell, Wales, & Nielsen, 2011). AN in particular is associated with high rates of hospitalization (20%) and rehospitalization (40%) within one year of the original hospitalization (Steinhausen, Grigoroiu-Serbanescu, Boyadjieva, Neumärker, & Metzke, 2008), with annual costs per patient that are on par with those for schizophrenia (Striegel-Moore, Leslie, Petrill, Garvin, & Rosenheck, 2000). Consequently, there is an urgent need to develop and test implementation models for low base-rate disorders like AN in “real world” settings in order to increase the availability of effective psychosocial treatment. Given low prevalence rates, specialty clinics may be the most appropriate settings for implementation efforts (Comer & Barlow, 2014).
Family-based treatment (FBT) is a well-established therapy for youth with AN (Lock, 2015), with approximately one-third of youth achieving 95% of median body mass index and eating disorder psychopathology scores within 1 SD of a normal range at the end of treatment (Le Grange et al., 2016; Lock et al., 2010), and four-year follow-up (Le Grange et al., 2014). Preliminary research also suggests that focused adaptations may enhance remission rates in FBT for early non-responders (Lock et al., 2015). However, anecdotal data suggest that FBT is rarely utilized outside of academic settings. There are multiple barriers to the implementation of FBT, including treatment-specific barriers (e.g., high demands on therapists and families, inadequate attention to co-occurring symptoms), organizational barriers (e.g., physical space, time constraints, and lack of support for training/implementation), interpersonal barriers (e.g., disliking one-size-fits-all model of treatment), and familial barriers (e.g., parental willingness and ability to participate in FBT) (Couturier et al., 2013). Furthermore, clinicians who are implementing FBT report “drift” from the manual by excluding core treatment components (e.g., weighing the patient) (Couturier et al., 2013), while adding new ones (e.g., mindfulness techniques) (Kosmerly, Waller, & Robinson, 2015).
The few existing effectiveness or implementation studies of FBT for AN are limited due to having provided treatment at no cost (Couturier, Isserlin, & Lock, 2010; Hughes et al., 2014; Loeb et al., 2007; Turkiewicz, Pinzon, Lock, & Fleitlich-Bilyk, 2010) and being conducted in academic settings by researchers embedded in those settings (Hughes et al., 2014; Loeb et al., 2007; Turkiewicz et al., 2010), rather than implementing FBT in the community (Goldstein et al., 2016). Building on the existing literature, the present study examined the implementation of FBT for youth with AN within a fee-for-service community-based specialty clinic. The aims of this study were 1) to determine the appropriateness, acceptability, feasibility, fidelity, and sustainability (Proctor et al., 2009) of implementing FBT in a specialty eating disorders setting, and 2) to examine its initial effect size for patients in this setting.
Methods
Setting
This study was conducted at a fee-for-service non-academic specialty program consisting of three sites that provided intensive outpatient and partial hospitalization programs in a large Midwestern city. Its specializations were eating disorders, obesity, and mood and anxiety disorders. The institutional review boards at The University of Chicago and the University of California, San Francisco approved all procedures.
Treatment and training
Therapists and researchers initiated a dialogue about the feasibility of FBT within their program following a one-day introductory training by the senior author (XXX). Through collaborative discussions, researchers worked with clinic staff to improve the “fit” of FBT within their context. The resulting adaptation included 19 sessions—a course of standard FBT (15 sessions) plus four skills-focused sessions that borrowed heavily from skills taught in dialectical behavior therapy (DBT) (Linehan, 1993) (see Table 1 for list of FBT versus adapted elements). Sessions were held twice weekly in weeks 3 through 6 to accommodate the skills-focused family sessions. These sessions sequentially covered four key DBT skills. First, for mindfulness (states of mind, including how eating disorder thoughts tend to reside in emotion mind under the guise of reasonable mind), the family learned that what makes one vulnerable to listening to and acting on emotion mind, also makes us vulnerable to listening to and acting on ones eating disorder (like being hungry, tired, or sick for example). They also learned the “what” skills, and “how” skills of mindfulness (mindfulness activity: counting breaths). Second, validation (principles of avoidance and reinforcement, both positive and negative) - particularly as they relate to food choices and distress in the refeeding process; how and when to validate, including a discussion of effective ways for caregivers to validate their child engaging in the difficult task of eating; (mindfulness activity: scratch the upper lip). Third, distress tolerance (four options when in distress, distraction, self soothing with the five senses, radical acceptance, and their applications for youth and caregivers during meal times and other distressing events; mindfulness activity: just this one moment). Fourth, emotion regulation (evolutionary purpose of emotions, “PLEASE MASTER”—reducing vulnerability to negative emotions through improved self-care, including a discussion of balanced eating and exercise, letting go of emotional suffering; mindfulness activity: urge surfing tickles and itches) (see Linehan, 1993 for skill descriptions). Therapists were trained by the primary author (YYY) in a two-day workshop that addressed key FBT interventions through instruction, modeling, and role-play, and discussed how to integrate the skills within the FBT model. Therapists were also provided with the original (non-adapted) FBT manual (Lock & Le Grange, 2013). Weekly one-hour group supervision was provided by the primary and senior authors (YYY and XXX).
Table 1.
Therapist fidelity to the treatment components of skills-enhanced FBT.
| Treatment Components | Occurrence | M | SD | Range |
|---|---|---|---|---|
| Orchestrate intense scene | 100.0% | 3.38 | 0.52 | [3,4] |
| Charge parents with task of refeeding | 100.0% | 4.13 | 0.64 | [3,5] |
| One more mouthful | 100.0% | 4.38 | 0.74 | [3,5] |
| Take patient’s weight | 100.0% | 4.12 | 0.82 | [3,5] |
| Provide feedback on patient’s weight | 100.0% | 4.45 | 0.67 | [3,5] |
| Externalize the illness | 100.0% | 4.06 | 0.87 | [2,5] |
| Remain agnostic | 96.4% | 2.97 | 1.04 | [1,5] |
| Reduce family guilt/blame | 93.6% | 2.80 | 1.03 | [1,5] |
| Modify parent/sibling criticism of patient | 99.0% | 3.11 | 1.39 | [1,5] |
| Align parents; support refeeding plans/efforts | 95.1% | 3.40 | 1.08 | [1,5] |
| Focus on eating disorder behaviors until eating disorder concerns are relieved | 100.0% | 4.10 | 0.91 | [2,5] |
| Facilitate transfer of independence to patient | 66.0% | 3.45 | 1.18 | [1,5] |
| Address issues related to adolescent development | 87.5% | 3.71 | 0.99 | [3,5] |
| Discuss use of validation* | 97.9% | 3.59 | 0.93 | [1,5] |
| Discuss use of mindfulness skills* | 85.1% | 2.32 | 1.07 | [1,5] |
| Discuss use of distress tolerance skills* | 83.6% | 2.89 | 1.02 | [1,5] |
| Discuss use of emotion regulation skills* | 71.2% | 2.19 | 1.11 | [1,5] |
| Overall | 92.7% | 3.47 | 0.94 |
Note: Adapted components are denoted with an asterisk ().
Participants
Therapists (N = 7) who participated in the “skills-enhanced” FBT training included four licensed clinical social workers (LCSW), one unlicensed social worker (MSW), one licensed professional counselor (LPC), and one licensed psychologist (PsyD), four of whom were allocated by the clinic director to see patients in this study (two at the main site and one at each satellite site). Upon initial contact, the intake coordinator informed caregivers of youth ages 11–18 years with possible AN about the option of participating in a research assessment to determine their eligibility for receiving FBT through a research study. Their alternative was to engage in standard treatment (i.e., intensive outpatient program or partial hospitalization program). Families who agreed to participate were evaluated by an independent research assistant at baseline and end of treatment (EOT) using structured interviews and questionnaires. Participants were eligible if they were between the ages of 11 and 18 years, met DSM-5 criteria for AN, and had a percent median body mass index (%mBMI) ≥75, calculated using the 50th percentile of BMI-for-age based on CDC growth charts (Centers for Disease Control and Prevention, 2002).
Measures
The main implementation outcomes were 1) appropriateness (i.e., the degree of fit, relevance, or compatibility of the intervention to address AN within this three-site clinical setting), 2) acceptability (i.e., the degree to which the intervention was perceived by therapists, patients, and caregivers as palatable or satisfactory), 3) feasibility (i.e., the extent to which the intervention was successfully implemented within this clinical setting, safety), 4) fidelity (i.e., the degree to which the intervention was implemented as intended by the treatment developers), and 5) sustainability (i.e., the extent to which the intervention is maintained or “institutionalized” within this clinical setting) (Proctor et al., 2009). Patient outcomes (i.e., symptomatology, satisfaction) were also examined.
Implementation outcomes.
The 22-item TCU Workshop Evaluation form (TCU WEVAL; Institute of Behavioral Research, 2002) was administered at the end of training and evaluated clinician ratings on (1) relevance of the training and intended utilization, (2) program resources supporting the training and implementation, (3) desire to obtain more training, and (4) organizational support. Higher scores indicate more positive perceptions and greater programmatic/organizational support (range: [10,50]). The Family-Based Treatment Attitude Scale (FBT-AS) is a 20-item measure that assesses clinician attitudes towards FBT for AN, adapted to assess skills-enhanced FBT in this study. Total scores range from −40 to 40, with higher scores indicating more favorable attitudes towards FBT. It demonstrated good internal reliability in this sample (Cronbach’s alpha = .87). The Therapeutic Technique Scale assessed implementation of 17 therapeutic techniques following each session, as a therapist self-report measure of treatment fidelity. Ratings included 0 = did not use, 1 = minimal, 2 = minimal to moderate, 3 = moderate, 4 = moderate to advanced, and 5 = advanced. The Abbreviated Acceptability Rating Profile (AARP; Tarnowski & Simonian, 1992) is an 8-item measure of treatment acceptability completed by youth and caregivers at session 4a that has good reliability and validity. Higher scores indicate greater treatment acceptability (range: [8,48]). The Therapy Suitability and Patient Expectancy (TSPE) was used to assess patients’ and caregivers’ perceptions of treatment suitability and expected improvement with the treatment from 0 (“not at all”) to 10 (“extremely”) at session 4a. This measure is frequently used to assess treatment acceptability in eating disorders treatment (Le Grange et al., 2016; Lock et al., 2015).
Patient and caregiver outcomes.
Participants were weighed by their therapist at each session wearing light, indoor clothing. Height was measured approximately monthly, and height and weight measurements were used to calculate body mass index (BMI = kg/m2) and %mBMI. The Eating Disorder Examination, version 14.3 (EDE; Cooper & Fairburn, 1987) is a semi-structured interview used to measure the global severity of eating disorder symptomatology at baseline and EOT, with higher scores indicating more severe eating psychopathology. The EDE has well-established reliability and validity (Berg, Peterson, Frazier, & Crow, 2012). The Parent Eating Disorder Examination – Questionnaire, version 1.4 (PEDE-Q; Loeb, 2007) is a caregiver-report measure of eating disorder psychopathology focused on caregiver observations of their child’s behaviors and attitudes since youth commonly underreport eating disorder symptoms. The 36-item Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) was administered to patients and caregivers to assess difficulties in emotion regulation at baseline and EOT, with higher scores indicating greater difficulties in regulating emotional states. The measure has been found to have good reliability and validity (Gratz & Roemer, 2004). The Distress Tolerance Scale (DTS; Simons & Gaher, 2005) is a 15-item measure of emotional distress tolerance administered to patients and caregivers at baseline and EOT, with higher scores representing greater tolerance of emotional distress. The DTS has good reliability and validity (Simons & Gaher, 2005). The Client Satisfaction Questionnaire (CSQ-8; Attkisson & Zwick, 1982) is an 8-item measure of patient satisfaction with mental health services completed by youth and caregivers at EOT that has good reliability and validity, with higher scores indicating greater satisfaction (range: [8,32]). The 11-item Helping Alliance Questionnaire (HAq; Luborsky, McLellan, Woody, O’Brien, & Auerbach, 1985) was used to assess patient-therapist therapeutic alliance at session 4a, with higher scores indicating greater alliance (range: [−33,33]). The HAq has good reliability and validity (Luborsky et al., 1985; Martin, Garske, & Davis, 2000). The 12-item Therapeutic Alliance Scale for Caregivers and Parents (TASCP; Accurso, Hawley, & Garland, 2012) was used to assess caregiver-therapist alliance at session 4a that has good reliability and validity, with higher scores indicating greater alliance (range: [12,48]).
Co-occurring psychiatric diagnosis.
The Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID, version 5.0; Sheehan et al., 2010)—a structured diagnostic interview used to assess DSM-IV psychiatric disorders and suicidality in children and adolescents—was administered to youth at baseline. Co-occurring psychiatric diagnoses from the MINI-KID were reviewed by two supervising clinical psychologists.
Analysis
SPSS 23 was used for all analyses. Given the small sample size and problems with significance-testing (Carver, 1993), patient outcomes were evaluated using effect sizes. Cohen’s d effect sizes were calculated as the difference between baseline and end-of-treatment outcomes, divided by the standard deviation of the change score (Feingold, 2009).
Results
Participant Characteristics
On average, therapist participants (N = 7) had 7.4 years (SD = 6.7) of therapy experience and 4.6 years (SD = 6.9) of experience treating adolescents with eating disorders. Youth participants (N = 11) were non-Hispanic Caucasian females ages 11 to 18 years (M = 15.47, SD = 1.78) with DSM-5 AN, restricting type. Mean %mBMI was 81.38 (SD = 4.20, range: [75.54, 86.65]). Mean duration of illness was 6.43 months (SD = 3.38). Three (27%) had previously received eating disorder psychotherapy, but not FBT, and two (18%) had been previously hospitalized for their eating disorder. At baseline, two (18%) were taking psychotropic medication (stable dose for past two months). Almost half of the sample met criteria for at least one co-occurring psychiatric disorder (n = 5, 45%), including major depressive disorder (n = 4, 36%) or an anxiety disorder (n = 3, 27%). The primary caregivers were mostly mothers (n = 10, 91%) who were predominantly married (n = 9, 82%), with one single parent who never married (adopted child) (9%), and one set of divorced parents who were not re-partnered (9%). Four families (36%) reported a familial history of an eating disorder.
Implementation outcomes
Appropriateness and acceptability.
The collaborative decision to adapt FBT (i.e., increasing intensity and adding skill-building sessions) intended to address concerns about FBT’s appropriateness for the complexity of cases presenting to this specialty clinic. After training in skills-enhanced FBT for AN and prior to delivering FBT, therapists reported moderately positive attitudes about the appropriateness and acceptability of this modified treatment (M = 15.57, SD = 8.66). Relevance (M = 38.81, SD = 2.49), program support (M = 38.07, SD = 1.84), and training engagement (M = 42.24, SD = 5.52) were all rated relatively highly by therapists post-training. Acceptability was also good as rated by patients (M = 33.67, SD = 10.19) and caregivers (M = 37.78, SD = 7.55). Patients and caregivers rated skills-enhanced FBT as moderately suitable (youth: M = 6.00, SD = 2.12; caregivers: M = 7.89, SD = 2.26) and expected it to be moderately successful (youth: M = 7.22, SD = 2.05; caregivers: M = 8.00, SD = 1.87). At termination, 5 participants planned to continue FBT, which suggests that families generally perceived therapy as acceptable. Continuation of FBT past EOT as designated by this study is not surprising given that families only received 15 FBT sessions, even though the dose recommended in the manual is 20 sessions (Lock & Le Grange, 2015).
Feasibility.
Eleven of fourteen (78.6%) families who preliminarily qualified for the study agreed to schedule an initial research assessment, all of whom met inclusion criteria and consented (100%) to the research study. Most patients (72.7%, n = 8) completed treatment (i.e., attended ≥80% of prescribed treatment sessions). Treatment non-completion was due to an inpatient medical hospitalization (session 2, alternative treatment recommended at discharge), family perceiving recovery (session 7), and family disliking treatment (session 10). With respect to safety, one youth (9.1%) was hospitalized due to medical instability (%mBMI <75 by losing 1.2 pounds from intake).
Fidelity.
Therapists reported implementing essential treatment components in 92.7% of applicable sessions, indicating high levels of treatment adherence to the modified FBT protocol. Only three treatment components were delivered less than 85% of the time, which included facilitating transfer of independence to patient (66.0%), discussing use of emotion regulation skills (71.2%), and discussing use of distress tolerance skills (83.6%) (see Table 1). Of note, two of these were specific to the skills-based modifications. Therapists also delivered FBT with greater initial frequency that tapered over time, as prescribed. Average time to complete therapy was 19.3 weeks. The first ten sessions (phase I) were completed in 6.0 weeks (SD = 1.7) (expectation: 5–6 weeks), and the next 9 sessions (phases II and III) were scheduled every 1.4 weeks (SD = 0.6) on average, indicating that therapists tapered down frequency in phases II and III.
Sustainability.
Following this study, therapists and leadership collaborated on developing a handbook for their intensive outpatient and partial hospitalization programs that integrated FBT principles into these levels of care, including weekly FBT sessions and daily parent participation at meals (i.e., parents prepare, bring, provide, and monitor meal with their child, with therapists providing parents with empowerment and coaching as indicated, as an extension of the “family meal”). The integration of FBT principles into existing services through the creation of this “FBT track” is evidence of good sustainability within a program that typically only provides higher levels of care.
Patient and caregiver outcomes
EDE interviews at EOT were completed by 8 (72.7%) of 11 participants; weight data were available for all participants.
Symptomatology.
Four participants (36.4%) achieved weight restoration at or above 95% mBMI, while six (54.5%) achieved an EDE Global score within 1 SD of community norms. Two participants (18.2%) achieved both weight restoration and EDE Global scores within community norms. Of those with secondary amenorrhea (n = 5), all (100%) achieved resumption of menses during the course of treatment, although one had started oral contraceptives. Cohen’s d effect sizes were large for change in %mBMI (d = 1.39) and moderate for caregiver-reported eating disorder psychopathology (d = 0.55) but not clinically significant by youth report (d = 0.08) (see Table 2). Figure 1 provides individual weight gain trajectories by participant.
Table 2.
Change in symptomatology.
| BL | EOT | ||||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Cohen’s d | |
| Primary outcomes | |||||
| %mBMI | 81.38 | 4.20 | 89.71 | 8.98 | 1.39 |
| EDE Global | 1.96 | 1.19 | 1.82 | 1.85 | 0.08 |
| PEDE-Q Global | 3.59 | 1.74 | 2.20 | 1.59 | 0.55 |
| Secondary outcomes | |||||
| DERS (youth) | 78.74 | 21.80 | 75.71 | 27.19 | 0.10 |
| DTS (youth) | 55.82 | 8.06 | 57.86 | 9.46 | 0.14 |
| DERS (caregiver) | 65.46 | 16.75 | 52.00 | 11.80 | 0.62 |
| DTS (caregiver) | 59.82 | 9.25 | 67.43 | 4.76 | 0.44 |
Note: BL = baseline, EOT = end of treatment, %mBMI = percent of median body mass index, EDE = Eating Disorder Examination, PEDE-Q = Parent Eating Disorder Examination Questionnaire, DERS = Difficulties in Emotion Regulation Scale, DTS = Distress Tolerance Scale.
Figure 1.
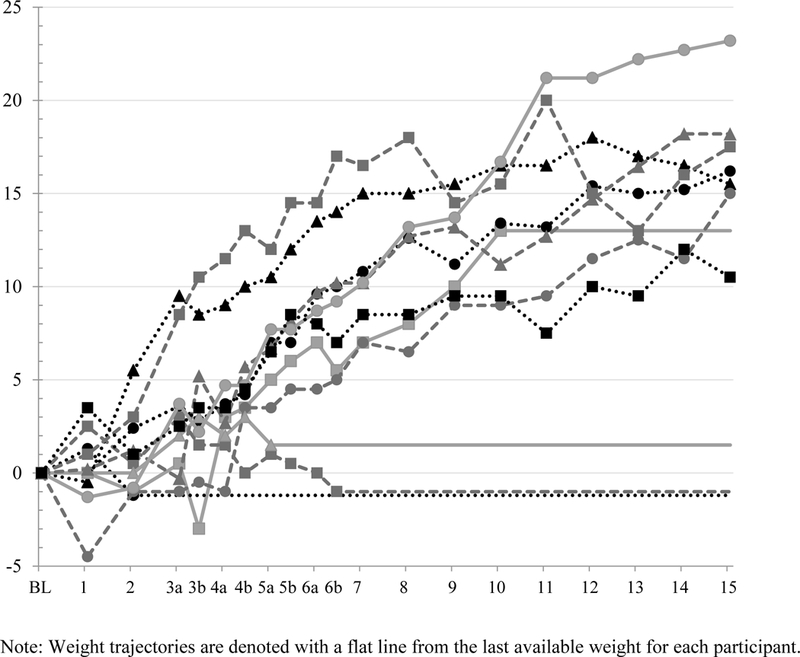
Individual weight gain trajectories by participant. Note: Weight trajectories are denoted with a flat line from the last available weight for each participant.
Satisfaction.
Youth (M = 26.3, SD = 4.3) and caregivers (M = 26.6, SD = 5.3) reported good satisfaction (i.e., on average, slightly more than “mostly satisfied”). In addition, patients rated therapeutic alliance as moderate (M = 14.1, SD = 13.3) while caregivers rated it highly (M =39.3, SD = 9.5).
Discussion
This case series supports the preliminary effectiveness of FBT when implemented outside of the “ivory tower.” Despite initial concerns about appropriateness and acceptability, the skills-enhanced adaptation was perceived positively by therapists and implemented with high fidelity. Interestingly, therapists reported higher fidelity to core components of FBT than to DBT skills, possibly due to difficulty integrating DBT skills into the newly learned FBT. FBT was viewed as acceptable and appropriate by youth and caregivers who presented to a program where they expected a higher level of care (i.e., intensive outpatient or day treatment). Also, FBT demonstrated feasibility and effectiveness in this context. Finally, FBT was sustained beyond the study period by incorporating its principles into the intensive outpatient and partial hospitalization programs, and by adding weekly FBT sessions for youth with AN in these levels of care at the study sites.
In addition to promising implementation outcomes, patients exhibited a large increase in %mBMI overall, which is an excellent predictor of subsequent improvement in eating disorder symptoms (Accurso, Ciao, Fitzsimmons-Craft, Lock, & Le Grange, 2014). Caregivers also reported moderate improvement in eating disorder psychopathology. Although youth reported relatively little change in eating disorder psychopathology, this is not necessarily surprising given that youth reported relatively low levels of eating disorder psychopathology, in contrast to high levels of eating disorder psychopathology as reported by caregivers. Full remission—achieving 95% mBMI and EDE scores within 1 SD of community norms—was achieved by 18% of patients by EOT (15 FBT + 4 skills sessions provided in under 5 months), compared with 22% in the most recent randomized clinical trial of FBT (18 sessions over 6 months; Le Grange et al., 2016), 23% in a randomized clinical trial following medical stabilization in hospital (20 sessions over 12 months; Madden et al., 2015), and 42% in the first randomized clinical trial to define remission in this way (24 sessions over 12 months; Lock et al., 2010). Further, the rate of early hospitalization was comparable to that for youth with AN receiving family therapy (17%; Lock et al., 2016). Caregivers also reported moderate increases in distress tolerance and large reductions in emotion dysregulation, suggesting that skills-enhanced FBT may help parents bolster their own emotional resilience. Given the distress that youth experience during the early phase of treatment, these skills may help caregivers tolerate their child’s distress while continuing with renourishment and managing eating disorder behaviors, despite no direct effect on youth’s distress tolerance or emotion dysregulation. Finally, patient satisfaction with treatment was good and comparable to that of another sample of youth with AN (Mountford et al., 2015).
This is one of the first studies to examine the implementation of an evidence-based treatment for youth with AN in a new service setting. Its strengths include implementation within a “usual care” specialty context (i.e., clinically-referred patients, community clinicians, three-site fee-for-service community program) with stakeholder involvement in designing the treatment adaptation, representative patients and caregivers, numerous implementation outcomes from therapist, patient, and caregiver perspectives, and its preliminary evaluation of treatment effectiveness. Certainly, this pilot study is limited by its size, moderate participant retention (≈70%), lack of comparison group, and therapist-report (i.e., subjective) measurement of fidelity. In addition, these findings would not likely generalize to non-specialist or publicly-funded settings. Despite shortcomings, this study adds to the limited literature on the implementation of FBT in community settings and provides preliminary data on the implementation of a skills-enhanced version of FBT and its effectiveness in a community-based specialist setting.
These findings suggest that FBT can be implemented with fidelity, is acceptable to community clinicians with the addition of DBT skills, and is associated with good patient outcomes. Findings from this pilot study should encourage clinicians and researchers alike to continue attempts at bridging the gap between the “ivory tower” and “real world” practice of evidence-based treatments for eating disorders. Future research examining factors related to implementation (e.g., youth/family characteristics, therapist attitudes) will be essential as dissemination and implementation efforts advance.
Acknowledgements
Funding for this study was provided by Insight Behavioral Health Center, Chicago, Illinois (PI: Le Grange). Dr. Le Grange also receives royalties from Guilford Press and Routledge and is Co-Director of the Training Institute for Child and Adolescent Eating Disorders, LLC. During the time of this study, Dr. Accurso was supported by grant T32-MH082761 from NIMH. The remaining authors declare that they have no conflict of interest.
References
- Accurso EC, Ciao AC, Fitzsimmons-Craft EE, Lock JD, & Le Grange D (2014). Is weight gain really a catalyst for broader recovery?: The impact of weight gain on psychological symptoms in the treatment of adolescent anorexia nervosa. Behaviour Research and Therapy, 56(1), 1–6. 10.1016/j.brat.2014.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Accurso EC, Hawley KM, & Garland AF (2012). Psychometric properties of the Therapeutic Alliance Scale for Caregivers and Parents. Psychological Assessment, 25(1), 244–252. 10.1037/a0030551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen AE, & Yager J (2009). Eating disorders In Sadock BJ, Sadock VA, & Ruiz P (Eds.), Kaplan & Sadock’s Comprehensive Textbook of Psychiatry, volume I, ninth edition (pp. 2128–2149). Philadelphia, PA: Lippincott Williams & Wilkins. [Google Scholar]
- Arcelus J, Mitchell AJ, Wales J, & Nielsen S (2011). Mortality rates in patients with anorexia nervosa and other eating disorders. Archives of General Psychiatry, 68(7), 724–731. [DOI] [PubMed] [Google Scholar]
- Attkisson CC, & Zwick R (1982). The Client Satisfaction Questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning, 5(3), 233–237. 10.1016/0149-7189(82)90074-X [DOI] [PubMed] [Google Scholar]
- Berg KC, Peterson CB, Frazier P, & Crow SJ (2012). Psychometric evaluation of the Eating Disorder Examination and Eating Disorder Examination-Questionnaire : A systematic review of the literature. International Journal of Eating Disorders, 45, 428–438. 10.1002/eat.20931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver RP (1993). The case against statistical significance testing. Journal of Experimental Education, 61(4), 287–292. 10.2307/20152382 [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. (2002). CDC growth charts for the United States: Development and methods. Atlanta, GA: Centers for Disease Control and Prevention. [Google Scholar]
- Comer JS, & Barlow DH (2014). The occaional case against broad dissemination and implementation: Retaining a role for specialty care in the delivery of psychological treatments. American Psychologist, 69(1), 1–18. 10.1037/a0033582.The [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper Z, & Fairburn C (1987). The eating disorder examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. International Journal of Eating Disorders, 6(1), 1–8. 10.1002/1098-108X [DOI] [Google Scholar]
- Couturier J, Isserlin L, & Lock J (2010). Family-based treatment for adolescents with anorexia nervosa: A dissemination study. Eating Disorders, 18(3), 199–209. 10.1080/10640261003719443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couturier J, Kimber M, Jack S, Niccols A, Van Blyderveen S, & McVey G (2013). Understanding the uptake of family-based treatment for adolescents with anorexia nervosa: Therapist perspectives. International Journal of Eating Disorders, 46(2), 177–188. 10.1002/eat.22049 [DOI] [PubMed] [Google Scholar]
- Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, & Mitchell JE (2009). Increased mortality in bulimia nervosa and other eating disorders. The American Journal of Psychiatry, 166(12), 1342–1346. 10.1176/appi.ajp.2009.09020247 [DOI] [PubMed] [Google Scholar]
- Crow SJ, Swanson SA, Le Grange D, Feig EH, & Merikangas KR (2014). Suicidal behavior in adolescents and adults with bulimia nervosa. Comprehensive Psychiatry, 55(7), 1534–1539. 10.1016/j.comppsych.2014.05.021 [DOI] [PubMed] [Google Scholar]
- David-Ferdon C, & Kaslow NJ (2008). Evidence-based psychosocial treatments for child and adolescent depression. Journal of Clinical Child & Adolescent Psychology, 37(1), 62–104. 10.1080/15374410701817865 [DOI] [PubMed] [Google Scholar]
- Feingold A (2009). Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric for classical analysis. Psychological Methods, 14(1), 43–53. 10.1037/a0014699.Effect [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland AF, Brookman-Frazee L, Hurlburt MS, Accurso EC, Zoffness RJ, Haine-Schlagel R, & Ganger W (2010). Mental health care for children with disruptive behavior problems: A view inside therapists’ offices. Psychiatric Services, 61(8), 788–795. 10.1176/appi.ps.61.8.788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein M, Murray SB, Griffiths S, Rayner K, Podkowka J, Bateman JE, … Thornton CE(2016). The effectiveness of family-based treatment for full and partial adolescent anorexia nervosa in an independent private practice setting: Clinical outcomes. International Journal of Eating Disorders, 0(0), 1–4. 10.1002/eat.22568 [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Higa-McMillan CK, Francis SE, Rith-Najarian L, & Chorpita BF (2016). Evidence base update: 50 years of research on treatment for child and adolescent anxiety. Journal of Clinical Child & Adolescent Psychology, 45(2), 91–113. 10.1080/15374416.2015.1046177 [DOI] [PubMed] [Google Scholar]
- Hogue A, Henderson CE, Ozechowski TJ, & Robbins MS (2014). Evidence base on outpatient behavioral treatments for adolescent substance use: Updates and recommendations 2007–2013. Journal of Clinical Child & Adolescent Psychology, 43(5), 695–720. 10.1080/15374416.2014.915550 [DOI] [PubMed] [Google Scholar]
- Hughes EK, Le Grange D, Court A, Yeo M, Campbell S, Whitelaw M, … Sawyer SM(2014). Implementation of family-based treatment for adolescents with anorexia nervosa. Journal of Pediatric Health Care, 28(4), 322–330. 10.1016/j.pedhc.2013.07.012 [DOI] [PubMed] [Google Scholar]
- Institute of Behavioral Research. (2002). TCU Workshop Evaluation Form (TCU WEVAL). Fort Worth: Texas Christian University; Retrieved from ibr.tcu.edu [Google Scholar]
- Kosmerly S, Waller G, & Robinson AL (2015). Clinician adherence to guidelines in the delivery of family-based therapy for eating disorders. International Journal of Eating Disorders, 48(2), 223–229. 10.1002/eat.22276 [DOI] [PubMed] [Google Scholar]
- Le Grange D, Hughes EK, Court A, Yeo M, Crosby RD, & Sawyer SM (2016). Randomized clinical trial of parent-focused treatment and family-based treatment for adolescent anorexia nervosa. Journal of the American Academy of Child & Adolescent Psychiatry, 55(8), 683–692. 10.1016/j.jaac.2016.05.007 [DOI] [PubMed] [Google Scholar]
- Le Grange D, Lock J, Accurso EC, Agras WS, Darcy A, Forsberg S, et al. (2014). Relapse from remission at two- to four-year follow-up in two treatments for adolescent anorexia nervosa. Journal of the American Academy of Child & Adolescent Psychiatry, 53(11):1162–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM (1993). Skills training manual for treating borderline personality disorder. New York, NY: Guilford Press. [Google Scholar]
- Lock J (2015). An update on evidence-based psychosocial treatments for eating disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 44(5), 707–21. 10.1080/15374416.2014.971458 [DOI] [PubMed] [Google Scholar]
- Lock J, Agras WS, Bryson SW, Brandt H, Halmi KA, Kaye W, … Jo B (2016). Does family-based treatment reduce the need for hospitalization in adolescent anorexia nervosa? International Journal of Eating Disorders, 49(9), 891–894. 10.1002/eat.22536 [DOI] [PubMed] [Google Scholar]
- Lock J, & Le Grange D (2013). Treatment manual for anorexia nervosa, second edition: A family-based approach. New York, NY: The Guilford Press. [Google Scholar]
- Lock J, Le Grange D, Agras WS, Fitzpatrick KK, Jo B, Accurso E, … Sztainer M(2015). Can adaptive treatment improve outcomes in family-based therapy for adolescents with anorexia nervosa? Feasibility and treatment effects of a multi-site treatment study. Behaviour Research and Therapy, 73, 90–95. 10.1016/j.brat.2015.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, & Jo B (2010). Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Archives of General Psychiatry, 67(10), 1025–32. 10.1001/archgenpsychiatry.2010.128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb KL (2007). Eating Disorder Examination Questionnaire - Parent Version (PEDE-Q), Version 1.4.
- Loeb KL, Walsh BT, Lock J, Le Grange D, Jones J, Marcus S, … Dobrow I(2007). Open trial of family-based treatment for full and partial anorexia nervosa in adolescence: Evidence of successful dissemination. Journal of the American Academy of Child & Adolescent Psychiatry, 46(7), 792–800. 10.1097/chi.0b013e318058a98e [DOI] [PubMed] [Google Scholar]
- Luborsky L, McLellan AT, Woody GE, O’Brien CP, & Auerbach A (1985). Therapist success and its determinants. Archives of General Psychiatry, 42(6), 602–611. 10.1001/archpsyc.1985.01790290084010 [DOI] [PubMed] [Google Scholar]
- Madden S, Miskovic-Wheatley J, Wallis A, Kohn M, Lock J, Le Grange D, … Touyz(2015). A randomized controlled trial of in-patient treatment for anorexia nervosa in medically unstable adolescents. Psychological Medicine, 45(2), 415–427. 10.1017/S0033291714001573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin DJ, Garske JP, & Davis MK (2000). Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. Journal of Consulting and Clinical Psychology, 68(3), 438–450. [PubMed] [Google Scholar]
- McCart MR, & Sheidow AJ (2016). Evidence-based psychosocial treatments for adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology, 45(5), 529–563. 10.1080/15374416.2016.1146990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell PF (2011). Evidence-based practice in real-world services for young people with complex needs: New opportunities suggested by recent implementation science. Children and Youth Services Review, 33(2), 207–216. 10.1016/j.childyouth.2010.10.003 [DOI] [Google Scholar]
- Mountford VA, Brown A, Bamford B, Saeidi S, Morgan JF, & Lacey H (2015). BodyWise: Evaluating a pilot body image group for patients with anorexia nervosa. European Eating Disorders Review, 23(1), 62–67. 10.1002/erv.2332 [DOI] [PubMed] [Google Scholar]
- Proctor EK, Landsverk J, Aarons G, Chambers D, Glisson C, & Mittman B (2009). Implementation research in mental health services: An emerging science with conceptual, methodological, and training challenges. Administration and Policy in Mental Health and Mental Health Services Research, 36(1), 24–34. 10.1007/s10488-008-0197-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, … Wilkinson B(2010). Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). Journal of Clinical Psychiatry, 71(3), 313–326. 10.4088/JCP.09m05305whi [DOI] [PubMed] [Google Scholar]
- Simons JS, & Gaher RM (2005). The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion, 29(2), 83–102. 10.1007/s11031-005-7955-3 [DOI] [Google Scholar]
- Steinhausen HC, Grigoroiu-Serbanescu M, Boyadjieva S, Neumärker KJ, & Metzke CW (2008). Course and predictors of rehospitalization in adolescent anorexia nervosa in a multisite study. International Journal of Eating Disorders, 41(1), 29–36. 10.1002/eat.20414 [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Leslie D, Petrill SA, Garvin V, & Rosenheck RA (2000). One-year use and cost of inpatient and outpatient services among female and male patients with an eating disorder: Evidence from a national database of health insurance claims. International Journal of Eating Disorders, 27(4), 381–389. [DOI] [PubMed] [Google Scholar]
- Tarnowski KJ, & Simonian SJ (1992). Assessing treatment acceptance: The Abbreviated Acceptability Rating Profile. Journal of Behavior Therapy and Experimental Psychiatry, 23(2), 101–106. [DOI] [PubMed] [Google Scholar]
- Turkiewicz G, Pinzon V, Lock J, & Fleitlich-Bilyk B (2010). Feasibility, acceptivility, and affectiveness of family-based treatment for adolescent anorexia nervosa: An observational study conducted in Brazil. Revista Brasileira de Psiquiatria, 32(2), 169–172. [DOI] [PubMed] [Google Scholar]
- Weisz J, Ng M, & Bearman S (2014). Odd couple? Reenvisioning the relation between science and practice in the dissemination-implementation era. Clinical Psychological Science, 2(1), 58–74. 10.1177/2167702613501307 [DOI] [Google Scholar]


