Abstract
OBJECTIVE:
Technological advances have allowed cardiac implantable electronic devices (CIEDs) to detect, analyze, and store atrial high-rate episodes (AHREs), which are surrogate for the term silent atrial fibrillation (AF). The association of AHREs with adverse clinical events has been demonstrated in several recent studies, implying that morbidity and mortality can be significantly prevented by prompt recognition and intervention. Inflammation and oxidative stress are among several mechanisms that contribute to the pathogenesis of AF. The monocyte-to-high-density lipoprotein ratio (M/H ratio) is a novel indicator of both inflammation and oxidative stress. In this study, we aimed to investigate the value of the M/H ratio for predicting AHREs detected by CIEDs.
METHODS:
A total of 203 patients (mean age: 57.5+9.1 years, 60.1% male) implanted with a dual pacemaker because of sick sinus syndrome were included. Blood samples were obtained from the patients after 12 h of fasting for the analysis of routine biochemistry tests and the lipid panel in the morning of device implantation. At a clinical visit 6 months after CIED implantation, the devices were interrogated to detect the occurrence of AHREs. AHREs were defined as atrial episodes faster than 220 bpm and lasting longer than 5 min. The patients were divided into two groups depending on the presence of AHREs during pacemaker interrogation: Group 1 (AHRE present) and Group 2 (AHRE absent).
RESULTS:
At the clinical visit 6 months after CIED implantation, 51 (25.1%) patients had at least one AHRE. The M/H ratio was significantly higher in patients in Group 1 (11.41±1.24) than in those in Group 2 (8.17±1.02) (p<0.01). On performing multivariate Cox regression analysis, the M/H ratio was found to be associated with the occurrence of AHREs in patients with CIEDs (OR: 22.813, 95% CI: 6.852–75.953, p<0.01).
CONCLUSION:
The M/H ratio is an indicator of inflammation and oxidative stress, both of which play an important role in the pathogenesis of AF. This ratio was found to be statically higher in patients with AHREs detected by CIEDs than in those without AHREs.
Keywords: Atrial high-rate episodes, cardiac implantable electronic devices, monocyte-to-high-density lipoprotein ratio, inflammation, oxidative stress
Atrial fibrillation (AF) is the most common cardiac rhythm disturbance in the adult population. The prevalence of AF has reached up to 10% in people over 80 years old 1. AF is associated with a 5-fold increase in the stroke risk and 2-fold increase in the mortality rate 2, which has necessitated prompt diagnosis and intervention to prevent significant morbidity and mortality. In recent years, several studies have demonstrated the poor correlation between AF and symptoms 3. Until recently, difficulties in the diagnosis of asymptomatic AF have resulted in its importance to be unknown. Technological advances have allowed cardiac implantable electronic devices (CIEDs) to detect, analyze, and store atrial high-rate episodes (AHREs) with high sensitivity and specificity 4, which led to emergence of the term “silent AF.” Subsequent studies have demonstrated that silent AF is not only a harbinger of the development of clinical AF but also increases the risk of ischemic stroke and death 5. The prediction of AHREs detected by CIEDs and the necessity of anticoagulation therapy for silent AF remain as some of the most controversial issues at present.
Inflammation and oxidative stress are among several mechanisms contributing to the pathogenesis of AF. The activation of leukocytes and subsequent release of various pro-inflammatory and pro-oxidant cytokines and chemokines have led to pathological structural and electrical remodeling in the left atrium; this remodeling is considered to be an important prerequisite for the development of AF 6.
High-density lipoprotein (HDL) exhibits anti-inflammatory and anti-oxidant properties by several pathways; these include inhibition of the transmigration of monocytes in response to oxidized low-density lipoprotein (LDL), expression of endothelial adhesion proteins, and promotion of the reverse transport of oxidized molecules 7. Due to these protective effects, a low HDL level is associated with more frequent AF occurrence 8.
Recently, several studies have demonstrated the importance of the serum monocyte count-to-HDL ratio (M/H ratio) as a reliable predictor of AF recurrence after catheter ablation 9 and a prognostic marker in chronic kidney disease 10. To best of our knowledge, to date, no study has evaluated the role of the M/H ratio as a predictor of AHREs using CIEDs. Therefore, the aim of the present study was to investigate the use of the M/H ratio as a predictor of AHREs in patients with CIEDs.
MATERIALS AND METHODS
We prospectively enrolled 210 patients who were implanted with a dual chamber pacemaker because of sinus node dysfunction between January 2014 and December 2014. In all patients, the choice of device manufacturer was left to the discretion of the attending physician. Patients with a previous history of atrial arrhythmias, renal failure, valvular heart disease, valvuloplasty, or valve replacement procedure and patients on pacemaker rhythm were excluded. The final study population was 203 patients. All patients participating in the study provided written consent and signed the consent form. The study was approved by the Institutional Ethical Committee.
Baseline demographic characteristics and relevant clinical information of each patient were recorded at the time of implantation. All patients were implanted with a dual-chamber pacemaker, which was programmed to the DDDR mode. The atrial tachycardia detection mode was enabled, and the AF suppression feature was programmed off by performing atrial overdrive pacing. Bipolar atrial leads sensitivity and post-ventricular atrial blanking period was interrogated properly to reduce P-wave sensitivity and far-field R-wave over-sensing to identify atrial activities during AHREs.
At a clinical visit 1 month later, the patients underwent transthoracic echocardiographic (TTE) by an expert in the field of cardiovascular imaging; 6 months after CIED implantation, the devices were interrogated to detect and classify the patients on the basis of the occurrence of AHREs. AHREs were defined as episodes faster that 220 bpm and lasting longer than 5 minutes on the basis of a previous study that demonstrated their significance via an increased rate of stroke and thromboembolic events and the exclusion of R-wave over-sensing episodes that were frequently found at periods of less than 5 min 11. The termination of AF was defined as the occurrence of 20 beats below the AHRE detection rate to ensure the exclusion of short episodes of atrial premature beats. The patients were divided into two groups on the basis of the presence of AHRE (Group 1) or absence (Group 2) of AHREs at the time of device interrogation.
Blood samples were obtained from the patients after 12 h of fasting for the analysis of routine biochemistry tests and the lipid panel in the morning of device implantation. At the same time, samples for complete blood count analysis were collected in ethylene-diamine-tetraacetic acid-anticoagulated tubes. The reference value for monocyte count in our laboratory was 2–10% of the total white blood cell count.
All data were evaluated using IBM SPSS 22 (IBM SPSS, USA). Mean and standard deviation were used for quantitative variables; Student’s t-test was used for normally distributed variables in both groups, and the Mann–Whitney U test was used for variables that were not normally distributed. Qualitative variables were evaluated by Pearson’s chi-squared test and Yates’ correction for continuity. The logistic regression model was used in multivariate analysis to identify risk factors related to mortality. A p-value of <0.05 was considered to be statistically significant.
RESULTS
Between January 2014 and December 2014, 203 patients (mean age: 57.5+9.1 years, 60.1% male) with a dual pacemaker were included in the study. They were divided into two groups on the basis of presence of AHRE in their pacemaker interrogation at a clinical visit 6 months after device implantation. Fifty one (25.1%) patients with AHRE were in Group 1 and 152 (74.1%) patients without AHRE were in Group 2.
Both groups were similar in terms of baseline characteristics and demographic features (Table 1). Echocardiographic and laboratory data of the study population are given in Table 2. As shown in Table-2, serum sodium levels were statistically higher in Group 1 (p<0.01). Serum potassium and serum calcium levels were similar in both groups. Although the total white blood cell count was similar in both groups, serum monocyte levels were significantly higher in Group 1 (p<0.01). Serum high density lipoprotein levels were significantly lower in Group 1 (p<0.01). When comparing the M/H ratio in both groups, Group 1 showed significantly higher M/H values (11.41±1.24) than Group 2 (8.17±1.02) (p<0.01) (Fig. 1). TTE findings including left atrial diameter, left ventricular end-diastolic and systolic diameters, and ejection fraction were similar in both groups.
Table 1.
Demographic features of the study population
| Parameters | Total (n:203) | AHRE (-) (n:152) | AHRE (+) (n:51) | P |
|---|---|---|---|---|
| Age (years) | 67.51±9.17 | 67.24±9.09 | 68.31±9.43 | 0.751 |
| Women | 81 (39.9%) | 57 (37.5%) | 24 (47.1%) | 0.250 |
| Body Mass Index (kg/m2) | 26.03±2.90 | 25.98±2.90 | 26.19±2.92 | 0.896 |
| Coronary Artery Disease | 23 (11.3%) | 17 (11.2%) | 6 (11.8%) | 0.910 |
| Diabetes Mellitus | 85 (41.9%) | 63 (41.7%) | 22 (44%) | 0.869 |
| Hypertension | 86 (42.3%) | 63 (41.7%) | 23 (45.1%) | 0.744 |
| Dyslipidemia | 41 (20.2%) | 30 (19.7%) | 11 (21.6%) | 0.778 |
| Alcohol intake | 19 (8.8%) | 14 (9.2%) | 5 (9.8%) | 0.900 |
| Current smoker | 59 (29.1%) | 43 (28.3%) | 16 (31.4%) | 0.675 |
AHREs: Atrial high-rate episodes
Table 2.
Echocardiographic and laboratory parameters
| Parameters | Total (n:203) | AHRE (-) (n:152) | AHRE (+) (n:51) | P |
|---|---|---|---|---|
| Ejection Fraction (%) | 60.64±4.98 | 60.63±4.99 | 60.69±5.00 | 0.949 |
| Left Atrial Diameter (cm) | 3.86±0.26 | 3.86±0.27 | 3.87±0.25 | 0.565 |
| Left ventricle end-diastolic diameter (cm) | 4.5±0.3 | 4.5±0.3 | 4.5±0.3 | 0.621 |
| Left ventricle end-systolic diameter (cm) | 2.65±0.39 | 2.64±0.34 | 2.67±0.48 | 0.106 |
| Hemoglobin (g/dl) | 13.51±1.76 | 13.65±1.74 | 13.10±1.75 | 0.750 |
| Creatinine (mg/dl) | 0.95±0.25 | 0.93±0.23 | 0.99±0.27 | 0.797 |
| Na(mEq/L) | 138.30±3.04 | 138.2±3.03 | 139.32±2.12 | <0.001 |
| K (mEq/L) | 4.16±0.56 | 4.11±0.53 | 4.31±0.60 | 0.094 |
| White Blood Cell Count (x109/L) | 7375±1.57 | 7344±1.35 | 7469±2.10 | 0.623 |
| Monocyte (x109/L) | 365.8±50.32 | 344.2±34.07 | 430.1±32.95 | <0.001 |
| LDL Cholesterol (mg/dl) | 112.97±26.8 | 111.53±25.6 | 117.23±30.14 | 0.191 |
| HDL Cholesterol (mg/dl) | 41.18±3.86 | 42.28±3.39 | 37.92±3.21 | <0.001 |
| Monocyte/HDL ratio | 8.98±1.77 | 8.17±1.02 | 11.41±1.24 | <0.001 |
AHREs: Atrial high-rate episodes, HDL: High-density lipoprotein cholesterol, LDL: Low-density lipoprotein cholesterol, Na: Sodium, K: Potassium
Figure 1.
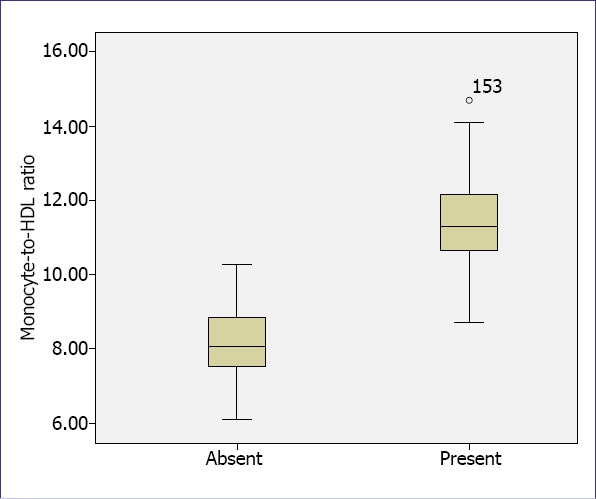
Atrial High Rate Episode
According to univariate Cox proportional hazard regression analysis, serum monocyte count, HDL level, and M/H ratio were significantly associated with AHRE (p<0.01) (Table 3). Multivariate Cox proportional hazard regression analysis revealed that the M/H ratio (OR=3.768, 95% CI=0.123–0.392, p<0.01) and serum HDL level (OR=2.601, 95% CI=0.01–0.07, p<0.01) were independent predictors of AHRE in patients with CIEDs (Table 3).
Table 3.
Univariate and multivariate Cox proportional Hazard modeling results of the occurrence of AHREs in patients with CIED
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| P value | OR | %95CI | P value | OR | %95CI | |
| Monocyte/HDL ratio | <0.01 | 22.813 | 6.852-75.953 | <0.01 | 3.768 | 0.123-0.392 |
| LDL | 0.899 | 1.001 | 0.986-1.016 | |||
| WBC | 0.702 | 0.946 | 0.711-1.259 | |||
| Monocyte | <0.01 | 1.079 | 1.051-1.108 | |||
| HDL | <0.01 | 0.617 | 0.521-0.730 | <0.01 | 2.601 | 0.010-0.070 |
| Hemoglobin level | 0.265 | 0.863 | 0.667-1.118 | |||
HDL: High-density lipoprotein cholesterol, LDL: Low-density lipoprotein cholesterol, WBC: White blood cell count
DISCUSSION
In this prospective study, we aimed to focus on the association between the M/H ratio and AHRE occurrence in patients with CIEDs. After the follow-up visit, we demonstrated that patients with a high M/H ratio before the procedure were more likely to develop AHREs. To the best of our knowledge, this is the first study reporting the value of the M/H ratio in predicting the occurrence of AHREs in this population.
Electrical and structural remodeling is a complex mechanism underlying the pathogenesis of AF. Electrical remodeling includes an increased atrial refractory period and atrial conductivity prolongation, whereas structural remodeling includes left atrial dilation and increased connective tissue deposition within the atrial wall, leading to atrial fibrosis. Functional changes within the atria occurring after the development of AF perpetuate the arrhythmia via these complex mechanisms (AF begets AF). Over the past years, electrical remodeling has been considered to be the main pathway leading to the occurrence and persistence of AF. However, recent reports, including studies on atrial biopsies of patients with AF, have demonstrated that structural remodeling caused by inflammation and oxidative damage occurs in parallel with electrical remodeling 12.
There is strong evidence on the association of inflammation with various cardiovascular conditions including coronary artery disease, diabetes mellitus and hypertension. Similarly, recent studies have demonstrated that inflammatory processes are involved in the pathogenesis of AF 13.
C-reactive protein (CRP) is a highly specific biomarker of systemic inflammation. AF incidence is higher in post-operative patients. The peak incidence of AF occurs during the second and third day postoperatively, which is similar to the time when the CRP level peaks 14. Inflammatory markers, including IL-6, IL-8, IL-10, VEGF, and CRP, levels were found to be higher in patients with AF than in those with sinus rhythm 15.
The activation of leukocytes is considered to be the key initiating step that leads to various inflammatory cascades. Leukocytes are the main source of inflammatory cytokines, including TNF-α, IL-6, and IL-8, which are found to be present in higher levels in the blood samples of patients with AF than in the samples of those with sinus rhythm 16.
Yamashita et al. studied the left atrial appendage specimens of patients with AF undergoing the maze procedure and repair of non-rheumatic mitral valve regurgitation or atrial septal defect 16. Immunohistochemistry of specimens revealed more prominent leucocyte infiltration in the endo/sub-endocardium in patients with AF. Leucocytes were positive for CD45 and CD68, which are specific for monocytes and macrophages. In addition, leucocytes were activated during their transmigration from the endo/sub-endocardium to the mid-myocardium. The adhesion and transmigration of immune cells were regulated by various adhesion molecules and chemokines. Immunohistochemical analysis revealed that the expression of adhesion molecules, including ICAM-1 and VCAM-1, was high in the endocardium of patients with AF; however, the expression of these molecule was low in patients with sinus rhythm. Monocyte chemotactic protein-1 (MCP-1) is known to be a chemotactic molecule that regulates the transmigration of immune cells following activation and adhesion. MCP-1 expression was higher in patients with AF than in those with sinus rhythm. Locally expressed IL-6 and TGF-ß propagate inflammation and increase extracellular matrix deposition and fibrosis. Yamashita et al. demonstrated that monocytes and macrophages within atrial specimens of patients with AF highly expressed these cytokines, leading to electrical and structural remodeling. These observations suggested the presence of “occult myocarditis” within atrial layers with the recruitment of immune cells predominantly monocytes/macrophages 16.
Dyslipidemia is associated with atherosclerosis and a risk factor for various cardiovascular conditions including coronary artery disease and stroke. However, there are conflicting results on the role of dyslipidemia in the occurrence of AF 17.
Reverse cholesterol transport is the best recognized mechanism by which HDLs exert their anti-atherogenic function. However, recent studies have revealed other functions of HDLs, including anti-inflammatory and anti-oxidant functions, which can guide its association with AF 18.
HDLs exert anti-oxidant functions via various mechanisms. They bind and transport oxidant molecules such as lipid hydroperoxides in different cell types 18. In addition, HDLs possess several enzymes that degrade lipid hydroperoxides, which oxidize the cell membrane components of LDL.
HDL exhibits anti-inflammatory effects on several steps in the inflammation process. HDL inhibits the adhesion of immune cells via reduced expression of activated endothelial adhesion molecules including VCAM-1, ICAM-1, and E-selectin 19. In addition, HDLs inhibit MCP-1, which is a chemokine for monocytes/macrophages, in response to LDL oxidation 19.
These observations led researchers to investigate the possible association of HDL with AF occurrence. Watanabe et al. investigated the association of lipid profile and new-onset AF in the general population. According to the result of that study, a lower HDL plasma level is a risk factor for AF occurrence, particularly in women 8.
Recently, Canpolat et al. investigated the impact of the M/H ratio before the procedure in predicting AF recurrence after successful cryoballoon-based catheter ablation. They demonstrated that an increased M/H ratio is an independent and strong predictor of AF recurrence after successful cryoablation 9. A cut-off M/H ratio of >11.48, which is slightly higher than ours (>9.48), has been established for the prediction of AF recurrence. In addition, Kanbay et al. reported that higher M/H ratios are associated with poorer cardiovascular outcome in patients with chronic kidney diseases 10.
The term “silent AF” has emerged in accordance with advances in CIED technology. In several studies, researchers have concluded that AHREs are harbingers of mortality and morbidity, particularly in terms of stroke and future AF 20. In light of these data, patients with AHREs constitute an important group of patients for anti-coagulants to prevent fatal and non-fatal thromboembolic complications. To date, a screening method to predict AHRE in patients with CIEDs is absent. In our study, the M/H ratio predicted AHREs with high sensitivity and specificity. However, prospective double-blind studies are needed to confirm this prediction.
Our study should be evaluated with its inherent limitations. Firstly, this was a single-center study with a limited number of patients. Secondly, measuring of the serum HDL level and monocyte count once may not be sufficient for use as a parameter. Thirdly, we defined AHRE as episodes faster than 220 bpm and longer than 5 min; different definitions of AHREs in terms of atrial rate and duration are present in the literature. Using other AHRE definitions would lead to results that are different from those in our present study.
CONCLUSION
AHREs detected by CIEDs are harbingers of ischemic stroke and future AF. The M/H ratio is a novel biomarker representing both inflammation and oxidative stress. Our results indicate that an elevated M/H ratio can predict AHREs in patients with CIEDs.
Footnotes
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 2.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–8. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 3.Page RL, Wilkinson WE, Clair WK, McCarthy EA, Pritchett EL. Asymptomatic arrhythmias in patients with symptomatic paroxysmal atrial fibrillation and paroxysmal supraventricular tachycardia. Circulation. 1994;89:224–7. doi: 10.1161/01.cir.89.1.224. [DOI] [PubMed] [Google Scholar]
- 4.Jędrzejczyk-Patej E, Lenarczyk R, Mazurek M, Liberska A, Przybylska-Siedlecka K, Podolecki T, et al. Can we rely on machines? Device-detected atrial high rates correspond well with atrial arrhythmias in cardiac resynchronization recipients. Europace. 2016;18:436–44. doi: 10.1093/europace/euv095. [DOI] [PubMed] [Google Scholar]
- 5.Glotzer TV, Hellkamp AS, Zimmerman J, Sweeney MO, Yee R, Marinchak R, et al. Atrial high rate episodes detected by pacemaker diagnostics predict death and stroke: report of the Atrial Diagnostics Ancillary Study of the MOde Selection Trial (MOST) Circulation. 2003;107:1614–9. doi: 10.1161/01.CIR.0000057981.70380.45. [DOI] [PubMed] [Google Scholar]
- 6.Psychari SN, Apostolou TS, Sinos L, Hamodraka E, Liakos G, Kremastinos DT. Relation of elevated C-reactive protein and interleukin-6 levels to left atrial size and duration of episodes in patients with atrial fibrillation. Am J Cardiol. 2005;95:764–7. doi: 10.1016/j.amjcard.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 7.Barter PJ, Baker PW, Rye KA. Effect of high-density lipoproteins on the expression of adhesion molecules in endothelial cells. Curr Opin Lipidol. 2002;13:285–8. doi: 10.1097/00041433-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Watanabe H, Tanabe N, Yagihara N, Watanabe T, Aizawa Y, Kodama M. Association between lipid profile and risk of atrial fibrillation. Circ J. 2011;75:2767–74. doi: 10.1253/circj.cj-11-0780. [DOI] [PubMed] [Google Scholar]
- 9.Canpolat U, Aytemir K, Yorgun H, Şahiner L, Kaya EB, Çay S, et al. The role of preprocedural monocyte-to-high-density lipoprotein ratio in prediction of atrial fibrillation recurrence after cryoballoon-based catheter ablation. Europace. 2015;17:1807–15. doi: 10.1093/europace/euu291. [DOI] [PubMed] [Google Scholar]
- 10.Kanbay M, Solak Y, Unal HU, Kurt YG, Gok M, Cetinkaya H, et al. Monocyte count/HDL cholesterol ratio and cardiovascular events in patients with chronic kidney disease. Int Urol Nephrol. 2014;46:1619–25. doi: 10.1007/s11255-014-0730-1. [DOI] [PubMed] [Google Scholar]
- 11.Pollak WM, Simmons JD, Interian A, Jr, Atapattu SA, Castellanos A, Myerburg RJ, et al. Clinical utility of intraatrial pacemaker stored electrograms to diagnose atrial fibrillation and flutter. Pacing Clin Electrophysiol. 2001;24:424–9. doi: 10.1046/j.1460-9592.2001.00424.x. [DOI] [PubMed] [Google Scholar]
- 12.Frustaci A, Chimenti C, Bellocci F, Morgante E, Russo MA, Maseri A. Histological substrate of atrial biopsies in patients with lone atrial fibrillation. Circulation. 1997;96:1180–4. doi: 10.1161/01.cir.96.4.1180. [DOI] [PubMed] [Google Scholar]
- 13.Boos CJ, Anderson RA, Lip GY. Is atrial fibrillation an inflammatory disorder? Eur Heart J. 2006;27:136–49. doi: 10.1093/eurheartj/ehi645. [DOI] [PubMed] [Google Scholar]
- 14.Guo Y, Lip GY, Apostolakis S. Inflammation in atrial fibrillation. J Am Coll Cardiol. 2012;60:2263–70. doi: 10.1016/j.jacc.2012.04.063. [DOI] [PubMed] [Google Scholar]
- 15.Li J, Solus J, Chen Q, Rho YH, Milne G, Stein CM, et al. Role of inflammation and oxidative stress in atrial fibrillation. Heart Rhythm. 2010;7:438–44. doi: 10.1016/j.hrthm.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamashita T, Sekiguchi A, Iwasaki YK, Date T, Sagara K, Tanabe H, et al. Recruitment of immune cells across atrial endocardium in human atrial fibrillation. Circ J. 2010;74:262–70. doi: 10.1253/circj.cj-09-0644. [DOI] [PubMed] [Google Scholar]
- 17.Annoura M, Ogawa M, Kumagai K, Zhang B, Saku K, Arakawa K. Cholesterol paradox in patients with paroxysmal atrial fibrillation. Cardiology. 1999;92:21–7. doi: 10.1159/000006942. [DOI] [PubMed] [Google Scholar]
- 18.Christison J, Karjalainen A, Brauman J, Bygrave F, Stocker R. Rapid reduction and removal of HDL- but not LDL-associated cholesteryl ester hydroperoxides by rat liver perfused in situ. Biochem J. 1996;314:739–42. doi: 10.1042/bj3140739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cockerill GW, Rye KA, Gamble JR, Vadas MA, Barter PJ. High-density lipoproteins inhibit cytokine-induced expression of endothelial cell adhesion molecules. Arterioscler Thromb Vasc Biol. 1995;15:1987–94. doi: 10.1161/01.atv.15.11.1987. [DOI] [PubMed] [Google Scholar]
- 20.Healey JS, Connolly SJ, Gold MR, Israel CW, Van Gelder IC, Capucci A, et al. ASSERT Investigators Subclinical atrial fibrillation and the risk of stroke. N Engl J Med. 2012;366:120–9. doi: 10.1056/NEJMoa1105575. [DOI] [PubMed] [Google Scholar]


