Abstract
A 52-year-old man with a history of hypertension was referred to our hospital due to persistent abdominal pain. Abdominal palpation revealed remarkable rigidity and rebound tenderness all over the abdomen. Enhanced computed tomography demonstrated the superior mesenteric artery (SMA) dissection with a complete obstruction at the middle part of the SMA. Intraoperative findings showed significant necrosis in the most small intestine and surgical resection was performed. Emergent operation is warranted once abdominal pain becomes uncontrollable or intestinal necrosis is suspected. Physicians should pay careful attention to patients' symptoms and repeatedly perfume physical examinations.
Keywords: superior mesenteric artery dissection, physical examinations, abdominal pain, atherosclerosis
Introduction
Spontaneous isolated visceral artery dissection (SIVAD) involving celiac artery and superior mesenteric artery (SMA) dissection is a relatively rare entity and causes various symptoms, including nausea, vomiting, abdominal pain, and back pain. SIVAD can be catastrophic if it is complicated with intestinal necrosis or arterial rupture secondary to aneurysm formation. In principle, the first-line therapy is conservative therapy, such as rest, blood pressure control, or anticoagulation therapy, since most patients recover from this disorder without any complications under conservative treatment (1-3). However, a few patients with SIVAD need surgical intervention due to uncontrollable pain, intestinal necrosis, or arterial rupture.
We herein report a case of isolated SMA dissection requiring emergent surgery.
Case Report
A 52-year-old man with a history of hypertension was referred to our hospital for the further investigation of severe abdominal pain. He was well until one day prior to admission, when he complained of severe abdominal pain during abdominal muscle exercise. The pain gradually worsened without remission, and he decided to visit the local hospital. Five hours later, he was transferred to our clinic for a further investigation and treatment. There was no significant family history other than hypertension.
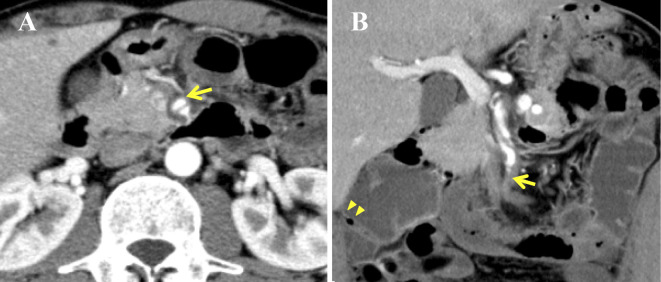
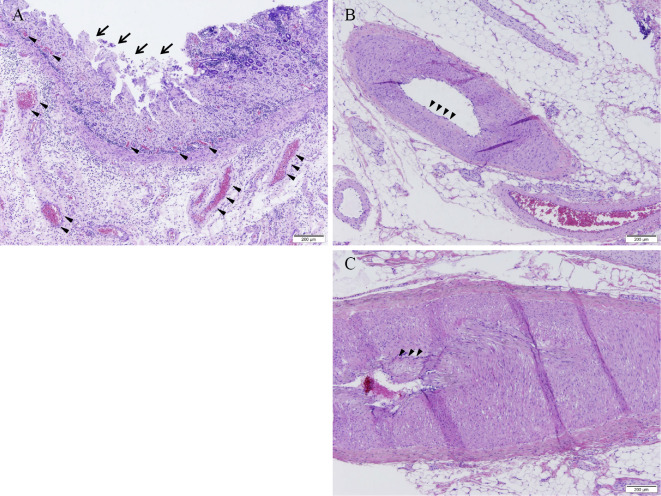
On admission, he was alert and had non-acute distress. His blood pressure was 140/72 mmHg, and his heart rate was 110 beats per minute. However, abdominal palpation revealed remarkable rigidity and rebound tenderness all over the abdomen. No bowel sounds were audible on auscultation. There were no specific findings on chest X-ray, and atrial fibrillation was not observed on 12-lead electrocardiography. A blood test demonstrated a significant elevation of the white blood cell count (17,200/μL), creatine phosphokinase (1,621 IU/L), and C reactive protein (11.7 mg/dL), with slight escalation of lactate dehydrogenase (349 IU/L). Thus, intestinal necrosis was suspected, and enhanced CT was performed. Enhanced CT revealed SMA dissection (Fig. 1A, large arrow), with the SMA dissected spirally with thrombus formation in the false lumen (Fig. 1B, large arrow). No abnormal findings were observed in the aorta, including intimal flap and aneurysm formation. Notably, the true lumen was compressed by a false lumen at the proximal portion of the SMA, and complete obstruction was detected at the middle part of the SMA, complicated with intestinal edema and emphysema (Fig. 1B, small arrow). According to Yun's categorization, the present case was classified as type III, SMA dissection with occlusion of SMA (4). We chose surgical treatment, since the pain was not under control and intestinal necrosis was strongly suspected based on the findings of a physical examination and enhanced CT. The intraoperative findings revealed significant necrosis in the most small intestine 30 cm from the anal side of the ligament of Treitz as well as the ascending colon (Fig. 2). Therefore, the surgeons decided to perform extensive small intestinal resection and ascending colon resection, despite the risk that short-bowel syndrome may sometimes occur after such an operation. The histopathological findings of the intestine demonstrated that the structure of intestinal villi (Fig. 3A, large arrow) had been destroyed by severe edema, vessel dilatation (Fig. 3A, small arrow), and lymphocyte infiltration, all of which were compatible with acute malperfusion of the small intestine. Notably, atherosclerotic changes, such as thickening of the intima and fat deposition, were also observed within the small vessels of the intestinal tissue (Fig. 3B and C, small arrow).
Figure 1.
Axial and coronary views of the dissecting superior mesenteric artery on enhanced computed tomography. Dissecting superior mesenteric artery (SMA) was clearly observed, and the false lumen was enhanced at the proximal SMA (A, large arrow). The SMA was dissected spirally and was occluded at the middle portion due to thrombus formation (B, large arrow). Intestinal edema and emphysema (B, small arrow) were observed, suggesting intestinal necrosis.
Figure 2.
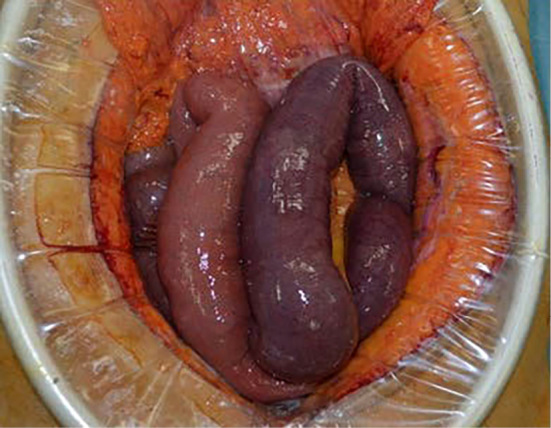
Intraoperative findings of the small intestine complicated with necrosis. An intraoperative observation revealed extensive necrosis of the small intestine and the ascending colon.
Figure 3.
Histopathological findings of the small intestine. Hematoxylin and Eosin staining were performed. The structure of the intestinal villi (A, large arrow) had been destroyed by edema, vessel dilatation (A, small arrow), and lymphocyte infiltration. These findings were compatible with congestion, increased permeability of the vessels, edema, and inflammation, suggesting acute malperfusion of the small intestine. Thickening of the intima and fat deposition were observed within the small vessels of the small intestinal tissue (B and C, small arrow). Foam cells were not observed in the present specimen.
After the operation, the patient suffered from malnutrition and diarrhea due to short bowel syndrome, and total parenteral nutrition was introduced. He was discharged home on the 99th day after surgery.
Discussion
SIVAD mainly including celiac artery and SMA dissection is reportedly observed in middle-aged men with a history of hypertension and smoking, suggesting that SIVAD might be related to atherosclerosis (5). In the current case, the patient had some risk factors associated with atherosclerosis, such as hypertension and smoking. Furthermore, the histopathological findings revealed intimal thickening in the SMA branches, which was compatible with atherosclerotic changes in the vessels. We therefore speculate that such changes might be observed in the dissected SMA as well. This is the first case report to describe the histopathological changes in the affected vessels in a case of spontaneous isolated SMA dissection. Of note, the occult atherosclerotic changes could not be identified by conventional methods, such as enhanced CT. Patients with SIVAD might seem healthy despite being complicated with the progression of atherosclerosis in the visceral arteries. Of course, this finding should be verified in autopsy cases or patients who undergo intestinal resection for SIVAD.
How SIVAD is triggered remains unclear. Park et al. investigated the possible mechanism of SIVAD using a computer simulation and highlighted the importance of hemodynamic forces generated by the convex curvature of the SMA as a possible cause of shear stress (6). Although they did not evaluate the correlation between SIVAD and atherosclerotic changes, mechanical stress caused by sit-ups might have contributed to SMA dissection in the present case.
Although treatment options vary, ranging from conservative therapy to surgery, depending on the patient's situation, conservative treatment is considered the first-line therapy, showing acceptable results in patients with SIVAD. However, open surgery is indicated in patients who experience uncontrollable abdominal pain or who show signs of intestinal necrosis or rupture. In the current case, abdominal pain persisted despite optimum conservative therapies and became complicated with signs of intestinal necrosis. Therefore, surgical treatment was considered the best option in the present case. Recently, endovascular treatment (EVT), such as stenting or coiling, has been introduced, and the number of reports concerning EVT is increasing. However, intestinal necrosis was evident in the present case, so EVT was considered to be contraindicated.
The present case highlights two important clinical messages. First, emergent operation is warranted once abdominal pain becomes uncontrollable or intestinal necrosis is suspected. Physicians should pay careful attention to patients' symptoms and repeatedly perform physical examinations. Follow-up with repetitive blood tests might be useful for avoiding missing intestinal necrosis. Second, patients with SMA dissection may seem healthy even as occult atherosclerotic changes progress in their vessels.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Tanaka Y, Yoshimuta T, Kimura K, et al. . Clinical characteristics of spontaneous isolated visceral artery dissection. J Vasc Surg 67: 1127-1133, 2018. [DOI] [PubMed] [Google Scholar]
- 2. Zettervall SL, Karthaus EG, Soden PA, et al. . Clinical presentation, management, follow-up, and outcomes of isolated celiac and superior mesenteric artery dissections. J Vasc Surg 65: 91-97, 2017. [DOI] [PubMed] [Google Scholar]
- 3. Cavalcante RN, Motta-Leal-Filho JM, De Fina B, et al. . Systematic literature review on evaluation and management of isolated spontaneous celiac trunk dissection. Ann Vasc Surg 34: 274-279, 2016. [DOI] [PubMed] [Google Scholar]
- 4. Yun WS, Kim YW, Park KB, et al. . Clinical and angiographic follow-up of spontaneous isolated superior mesenteric artery dissection. Eur J Vasc Endovasc Surg 37: 572-577, 2009. [DOI] [PubMed] [Google Scholar]
- 5. Naganuma M, Matsui H, Fushimi K, Yasunaga H. Clinical features of isolated dissections of abdominal aortic branches. Heart Vessels 31: 1006-1009, 2016. [DOI] [PubMed] [Google Scholar]
- 6. Park YJ, Park CW, Park KB, Roh YN, Kim DI, Kim YW. Inference from clinical and fluid dynamic studies about underlying cause of spontaneous isolated superior mesenteric artery dissection. J Vasc Surg 53: 80-86, 2011. [DOI] [PubMed] [Google Scholar]