Abstract
Bertolotti’s syndrome refers to the presence of pain associated to the anatomical variant of sacralization of the last lumbar vertebra. It is often a factor that is not addressed in the evaluation and treatment of lower back pain. The presence of a lumbosacral transitional vertebra is a common finding among general population with a prevalence that ranges between 4 and 30%, however, this finding is rarely associated to the cause of lower back pain and thus, the prevalence of Bertolotti’s syndrome in general population is unknown doe to underdiagnosis. The sacralization of the fifth lumbar vertebra has been related to changes in the anatomy and biomechanics of the spine with no general agreement to its clinical significance, however Bertolotti’s syndrome should be considered as a differential diagnosis for lower back pain, therefore, its pathophysiology, epidemiology and treatment must be a topic of general knowledge to physicians that often treat this condition.
INTRODUCTION
Bertolotti’s syndrome (BS) refers to the presence of pain associated to the anatomical variant of the presence of a lumbosacral transitional vertebra (LSTV). It is recognized when an elongated transverse process of the last lumbar vertebra fuses with the first sacral segment in variable degrees and this anomaly is recognized as a mechanical cause for lower back pain [1].
The assimilation of the fifth lumbar vertebra by the sacrum was first described by Bertolotti in the year of 1917. He was the first author to relate this finding to low back pain. LSTV are congenital anomalies defined as either sacralization of the lowest lumbar segment or lumbarization of the highest sacral segment [1]. Castelvi’s divides the pathology in four groups according to the development of the transverse process [2] (Table 1). We present a patient with this condition that had persistent pain that only resolved after injection with local corticosteroids.
Table 1.
Castellvi’s classification for lumbosacral transitional vertebrae.
| Castellvi’s classification | |||
|---|---|---|---|
| Type | Description | Anatomic features | Example |
| Type I | Displastic transverse process | Unilateral (a)or bilateral (b) large transverse process (>19 mm wide). |
 Type 1a Type 1a |
| Type II | Incomplete lumbarization/sacralization | Enlarged transverse process, with unilateral (a)or bilateral(b) pseudoarthrosis wit the sacral ala. |
 Type IIa Type IIa |
| Type III | Complete lumbarization/sacralization | Enlarged transverse process, with unilateral (a) or bilateral (b) complete fusion with the sacral ala. |
 Type IIIa Type IIIa |
| Type IV | Mixed | Type IIa on one side and type IIIa on the other |
 Type IV Type IV |
CASE REPORT
A 42-year-old female presented to the clinic with a history of chronic low back pain. She reported no relevant medical history. She had already been treated in the last 4 years by general practitioners with analgesics and home based physiotherapy with no satisfactory results. She had two previous admissions to the emergency department where morphine was prescribed to control the pain on her lower back. She was under ambulatory treatment with diclofenac, and tizanidine with partial relief of symptoms. Her main complaint was pain on the lower lumbar back with no radiation to the lower extremities. In her physical evaluation she presented limitation to full rotation and bending of the lumbar spine due to pain. Lasegue sign was negative, sensitivity, reflexes, sagittal balance, distal muscular strength and pulses were normal. Radiographs showed an overdeveloped left transverse process of the fifth lumbar vertebra which contacts with the sacrum at the left sacral wing with signs of degeneration at the same site (Fig. 1). Magnetic resonance imaging (MRI) studies were obtained (Figs 2–5). The patient was taken to the operating room where infiltration with 1 mL of lidocaine and 40 mg of Triamcinolone was performed in the pseudoarticulation between the left transverse process and the sacrum under fluoroscopic guidance. She reported a complete relief of pain after the procedure. At three months follow-up she was managed with strengthening and stabilizing exercises for the lumbar spine and postural education was initiated. She remains asymptomatic at her 12 months follow up.
Figure 1:
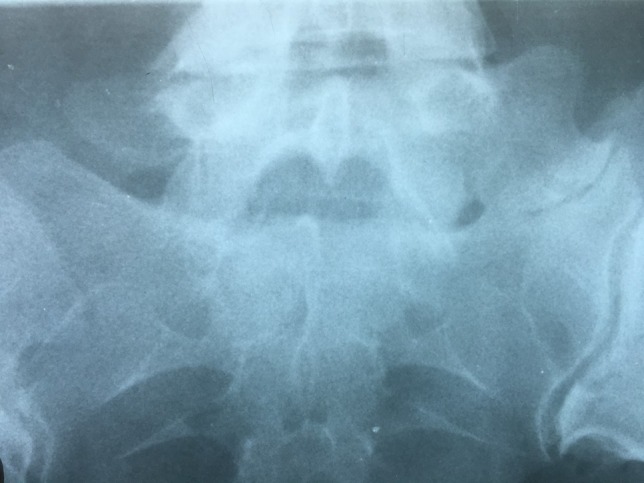
Radiographs showing an overdeveloped left transverse process, which contacts with the sacrum left sacral wing (Castelvi’s Type IIa).
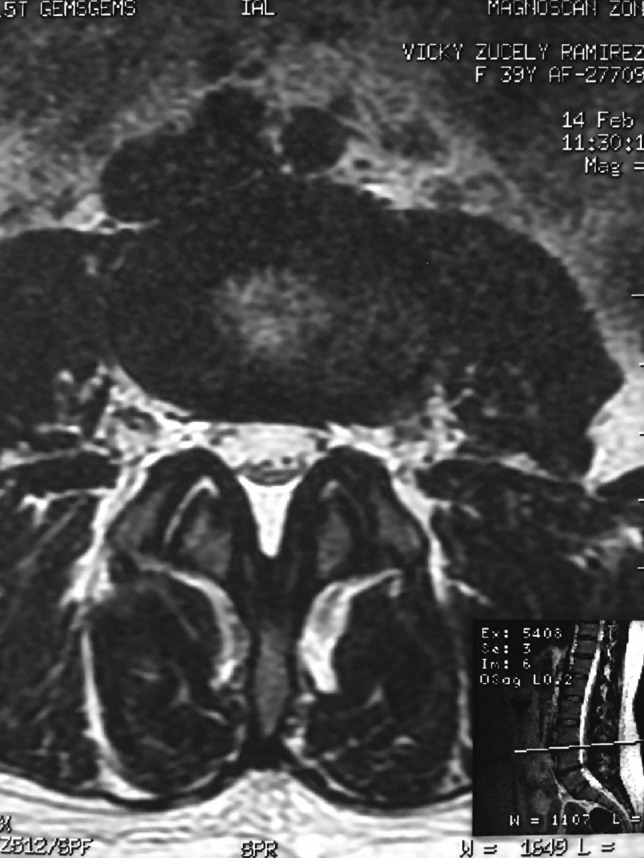
Figure 2:

RMN of the patient showing smaller facets in the anomalous articulation and healthy disc compared to the supradjacent one (next figure).
Figure 5:

Showing the protective effect of the limitation of the motion in the distal disc to the anomaly.
Figure 3:
Degenerative changes at the facets and disc in the adjacent segment.
Figure 4:

Showing the protective effect of the limitation of the motion in the distal disc to the anomaly.
DISCUSSION
Fusion of the fifth vertebra to the sacrum is a common finding. Its prevalence has been reported in between 4 and 30% of the general population. Overall, 13% of the patients with a LSTV are asymptomatic but BS is diagnosed in only in 4–8% patients with low back pain, 18.5% of these patients are under 30 years of age [3].
Physical examination of patients with BS is often non-specific presenting with tenderness in the lower back and limitation to the ranges of motion, signs of radiculopathy can be present, the contact between bones at the pseudoarticulation has been speculated as a source of pain which can be manifested as sacroiliac, hip, groin or even imitating an L5 radicular pain (pseudo-radiculopathy) [4].
Plain radiographs of the lumbosacral spine demonstrate 76–84% effectiveness to detect LSTV. Ferguson radiographs of the lumbosacral spine (AP radiograph with a 30° cranial angulation) presents with a higher sensitivity in detecting LSTV. Mid-sagittal T2-weighted MRI presents with 80% sensitivity and specificity for the diagnosis, with bone marrow edema as one of the most common findings [5]. CT scan is a complimentary imaging resource that helps defining bone structures, osteophytes and the state of the pseudoarticulation of the fifth transverse process [6].
The partial fusion at the lower part of the lumbosacral transition produces important alterations in normal biomechanics at the levels immediately above and below the LSTV. Changes such as hypermobility and abnormal torque moments are present at the level above the LSTV, predisposing it to early degeneration (early disc pathology and facet joint degenerative disease). Restricted movement below the LSTV produces a protective effect against degeneration of disc and facets and is related to changes (facets are smaller and coronally oriented) in the dimensions of the lower level facet joints [7]. These alterations can be verified in the adjacent levels of the LSTV in our patient.
The cause of our patient’s pain could be related to the presence of the pseudoarticulation between the sacrum and the fifth lumbar vertebra (that already showed signs of arthrosis) or the degenerative changes in the disc and facets of the level above the LSTV.
Infiltration with local steroids and anesthetics is a useful diagnostic tool to study BS. It is used to determine which patients have pain originated exclusively at the pseudoarticulation (complete relief of pain after the injection of the pseudoarticulation) and which patients have additional pain doe to the irritation of the L4 or L5 nerve root. Patients with poor response to the intra-articular/periarticular and transforaminal injection are candidates to more complex surgeries such as resection of the transverse process of the fifth lumbar vertebra and decompression, but this is rarely needed [4, 8, 9].
Kongsted was not able to determine which procedure (injection alone or extended surgical intervention) presented with the best clinical outcomes considering the heterogenicity and low level of evidence of the current available literature [10]. We believe that the best approach is to perform a local steroid injection at the point of the pseudoarticulation in patients with no radicular pain and an additional transforaminal injection in patients with radicular involvement. An extended surgical approach will be necessary in patients with persistent pain. New techniques such as 3D guided surgery and minimally invasive procedures can be applied to this pathology with good results [8–10].
CONCLUSION
Bertolotti’s syndrome is a frequent anomaly which can be related to lower back pain. It should be considered as a differential diagnosis when confronting a patient with compatible radiographic findings and persistent back pain. Confirmation of pain originating from the pseudoarticulation can be made with steroid injections.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Jancuska J, Spivak J, Bendo J. A review of symptomatic lumbosacral transitional vertebrae: Bertolotti’s syndrome. Int J Spine Surg 2015;9:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Castellvi A, Goldstein L, Chan D. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine 1984;9:493–5. [DOI] [PubMed] [Google Scholar]
- 3. Kapetanakis S, Chaniotakis C, Paraskevopoulos C, Pavlidis P. An unusual case report of Bertolotti’s syndrome: extraforaminal stenosis and L5 unilateral root compression (Castellvi Type III an LSTV). J Orthop Case Rep 2017;7:9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Adams R, Herrera-Nicol S, Jenkins A. Surgical treatment of a rare presentation of Bertolotti’s syndrome from Castellvi Type IV lumbosacral transitional vertebra: case report and review of the literature. J Neurol Surg Rep 2018;79:e70–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Neelakantan S, Anandarajan R, Shyam K, Philip B. Multimodality imaging in Bertolotti’s syndrome: an important cause of low back pain in young adults. BMJ Case Rep 2016;2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Benvenuto P, Benvenuto N. Bertolotti’s syndrome: a transitional anatomic cause of low back pain. Intern Emerg Med 2018. https://www.ncbi.nlm.nih.gov/pubmed/30022398. [DOI] [PubMed] [Google Scholar]
- 7. Kundi M, Habib M, Babar S, Kundi A, Assad S, Sheikh A. Transitional vertebra and spina bifida occulta related with chronic low back pain in a young patient. Cureus 2016;8:e837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chang I, Won Kim S, Gyue Kim J, Myung Lee S, Shin H, Young Lee H. Decompressive L5 transverse processectomy for Bertolotti’s syndrome: a preliminary study. Pain Physician 2017;20:E923–32. [PubMed] [Google Scholar]
- 9. Babu H, Lagman C, Kim T, Grode M, Johnson P, Drazin D. Intraoperative navigation guided resection of anomalous transverse process in patients with Bertolotti’s syndrome. Surg Neurol Int 2017;8:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kongsted E, Bunger C, Bindzus C. Symptomatic lumbosacral transitional vertebra: a review of the current literature and clinical outcomes following steroid injection or surgical intervention. SICOT J 2017;3:71. [DOI] [PMC free article] [PubMed] [Google Scholar]


