Abstract
To control movement, the brain has to integrate proprioceptive information from a variety of mechanoreceptors. The role of proprioception in daily activities, exercise, and sports has been extensively investigated, using different techniques, yet the proprioceptive mechanisms underlying human movement control are still unclear. In the current work we have reviewed understanding of proprioception and the three testing methods: threshold to detection of passive motion, joint position reproduction, and active movement extent discrimination, all of which have been used for assessing proprioception. The origin of the methods, the different testing apparatus, and the procedures and protocols used in each approach are compared and discussed. Recommendations are made for choosing an appropriate technique when assessing proprioceptive mechanisms in different contexts.
Keywords: Joint motion sense, Joint position sense, Kinaesthesia, Movement discrimination, Proprioception
1. Updated understanding of proprioception
Body movement is a fundamental and essential component of human life. In daily activities, most of what a human does in their interaction with the environment is associated with the generation of movement. Further, in competitive sports, precise and coordinated body movement is critical for success. A fundamental shift in the research field of human movement control has occurred in recent decades, largely due to a growing understanding of the role that sensory information plays in neuroplasticity through use-dependent mechanisms.1 The most important source for the promotion of task-specific neural development is argued to be proprioception.1, 2, 3, 4, 5
The question “What is proprioception?” has often been asked in the literature.6 Different conceptualizations of “proprioception” by researchers have led to different definitions, and consideration of their historical emergence is relevant here.
The fundamental anatomical basis for the connection between the brain and limbs was first identified in 1826 by a Scottish physiologist, Charles Bell. Bell wrote that “between the brain and the muscles there is a circle of nerve; one nerve (ventral roots) conveys the influence from the brain to the muscle, another (dorsal roots) gives the sense of the condition of the muscle to the brain”.7 In Bell's view, “muscular sense” refers to a closed-loop system between the brain and the muscles: the afferent pathway from the muscles to the brain and the efferent pathway from the brain to the muscles.
Sixty years later, the English anatomist and pathologist Henry Bastian introduced the term “kinaethesia”, derived from two Greek words “kinein” (move) and “aisthesis” (sensation):“I refer to the body of sensation which results from or is directly occasioned by movements … kinaesthesis. By means of this complex of sensory impression we are made acquainted with the position and movements of our limbs … by means of it the brain also derives much unconscious guidance in the performance of movement generally”.8
Subsequently, in 1906, the English neurophysiologist Sir Charles Sherrington coined “proprioception”, from a combination of the Latin “proprius” (one's own) and “perception”, to give a term for the sensory information derived from (neural) receptors embedded in joints, muscles and tendons that enable a person to know where parts of the body are located at any time. He referred to proprioception as “the perception of joint and body movement as well as position of the body, or body segments, in space”.9
Currently, both “proprioception” and “kinaesthesis (kinaesthesia)” continue to be used as terms in the published literature. However, specialists from fields such as neurology, neurophysiology, neuropsychology, sports and exercise medicine, and orthopaedic surgery have different interpretations of the two terms. Some researchers define proprioception as joint position sense only, and kinaesthesia as the conscious awareness of joint motion;10, 11 while others consider that kinaesthesia is one of the submodalities of proprioception, and that proprioception as a construct contains both joint position sense and the sensation of joint movement (kinaesthesia).12, 13, 14, 15, 16, 17, 18, 19 Proprioception defined in this way accords with Bastian's conceptualization of kinaesthesis (kinaesthesia), each including both position and movement senses. Although joint position and movement have been considered as two separate sensory entities,20, 21 any movement is accompanied by changes in information regarding both position and movement senses.22, 23, 24, 25 That is, the senses of joint movement and joint position are always associated with each other in daily activities.26 Consequently, it has been argued that it is appropriate to interpret “proprioception” and “kinaesthesis (kinaesthesia)” as being synonymous.26, 27, 28, 29
The original definition of proprioception, given by Charles Sherrington when he first used the term, was that proprioception is “… the perception of joint and body movement as well as position of the body, or body segments, in space”, and the “perceptions of the relative flexions and extensions of our limbs”.9 Here Sherrington refers to proprioception as “perception” of body position and movement. Perception, from the Latin “percepio” (perceive), is the identification, organization, and interpretation of sensory information, in order for humans to internally represent and understand the environment.30 All perceptions require signals within the nervous system, which derive from physical stimulation of various sense organs.31 For instance, hearing involves sound waves impacting the eardrum, and vision includes light impinging the retina of the eye and the transduction of these different forms of energy into electrical energy within neurons. Likewise, proprioception requires the stimulation of mechanoreceptors to threshold via body movements (changes of body position). However, a characteristic of perception is that it is not simply the passive receipt of a sensory signal, but rather, perception is shaped by memory and learning.32
In this understanding, proprioception can be defined as an individual's ability to integrate the sensory signals from mechanoreceptors to thereby determine body segment positions and movements in space.1, 33, 34, 35, 36, 37 In other words, proprioception is not merely a physiological property, but rather, it has both physiological (hardware) and psychological (software) aspects.37, 38 To be specific, proprioception is the perception of body position and movements in three-dimensional space, and overall proprioceptive performance is determined by the quality of both the available proprioceptive information and an individual's proprioceptive ability. Thus, the hardware (peripheral mechanoreceptors) provides proprioceptive information to the brain for the software (central processing) to integrate and use.39
More specifically, Ashton-Miller et al.40 have argued that if proprioception is only the afferent (hardware) part of the system, proprioception cannot be trained because there is no capacity to train a signal. In contrast, a recent systematic review by Witchalls et al.41 has demonstrated that proprioception as a measure of the neuromuscular response to a stimulus must involve sensory input, central processing, and motor output in a closed loop. In light of this latter view, it is insufficient to consider proprioception just as a cumulative neural input to the central nervous system (CNS) from the mechanoreceptors located in muscles, joints and the skin,42, 43, 44, 45 and it is inappropriate to interpret either passive movement detection without muscle activation or a measure of reflex muscle activation46 as overall proprioceptive ability.
In the past century, (neuro)physiologists have had a strong interest in investigating the roles of peripheral mechanoreceptors in determining proprioception, and have used different techniques, such as vibration or anaesthesia, to differentiate the functional roles of the different mechanoreceptor types.47, 48, 49 However, to execute functional movements in daily activities, exercise, and sports, proprioceptive information from a variety of mechanoreceptors is available for central processing. Therefore a complex array of different sources is utilized, although muscles spindles are seen as the main transducers used to gather proprioceptive information.21, 50 Further, an increasing number of researchers, especially those in exercise and sports, now recognize the importance of central processing in proprioception, when attempting to understand human movement.
For instance, evidence has suggested that central processing in proprioception may play a role in sport performance. Although most body movements in daily activities are automated, conscious attention is required to learn complex skills in sports and exercise, such as when using the foot to control a ball, performing a variety of arm movements in ice skating, or executing Tai Chi movements in a coordinated pattern. Learning movement skills means developing new patterns of movement by processing proprioceptive information appropriately. New neural programs are developed, refined by repetition and transferred to the more fundamental regions of the brain, from where they are executed with less effort and relayed much faster.51 It has been argued that a novice athlete spends time consciously mastering new movements using a closed-loop system of control, whereas skilled athletes only occasionally use sensory checking for successful execution of relevant movements.52, 53 Han et al.53, 54 found that ankle proprioception scores were significantly and positively correlated with sport performance level in soccer. They argued that elite soccer players allocate less central capacity to processing proprioceptive information for movement control, thereby devoting more attention to tasks such as locating team mates and opponents, and determining the best opportunity to pass or shoot.53, 55 In addition, recent evidence suggests that when attentional demands are increased, this has a detrimental impact on ankle joint proprioceptive performance in young adults.56 A recent brain imaging study also found that in addition to peripheral reflex mechanisms, central processing of proprioceptive information from the foot was essential for balance control.57
To date, the peripheral and central mechanisms underlying proprioceptive control are still unclear. In exercise and sport, it is unknown if proprioceptive improvement associated with exercise58, 59, 60 is a result of peripheral adaptation, or neural plasticity, or both;33, 61 and if superior proprioceptive ability in athletes53, 54, 62, 63, 64 is due to intensive training or determined by selection for genetic factors.53, 54, 65 Nevertheless, the importance of proprioception has been well established in sports injury prevention and rehabilitation, sports performance selection and talent identification, and for falls prediction and intervention.54, 59, 66, 67
To examine proprioceptive mechanisms, different techniques have been reported in the literature. There are three main testing techniques for assessing proprioception – threshold to detection of passive motion (TTDPM),68 joint position reproduction (JPR), also known as joint position matching,69 and active movement extent discrimination assessment (AMEDA).70 These tests have been developed from different concepts, are conducted under different testing conditions, and arguably assess different aspects of proprioceptive modalities.71, 72 In this paper, the three techniques are reviewed systematically to compare the origin of the methods, the different apparatus used for testing, the procedures and the protocols used in each approach.
2. Origin of proprioception assessment techniques
Testing an individual's sensory acuity is the primary aim of psychophysics, and the standard measures used to do so were described as early as 1860 by Fechner.73 Psychophysics refers to quantitative investigation of the relationship between an objective physical stimulus and the subjective perceptions it causes.28 In 1860, Gustav Theodor Fechner published the Elemente der Psychophysik in which he reported the first experiments on the psychophysics of active movement.74 In his study, Fechner assessed perception of differences in the amount of force required for the upper limb to overcome gravity for lifting weights. Following this classic work, in the 1880s, James McKeen Cattell and Hugo Munsterberg were the pioneer researchers who first used comparison of the extent of pairs of movements made to physical stops, without visual cues, as an experimental psychophysical method for studying human movement.75 In fact, this work constituted the earliest study of proprioception, because to compare the extent of pairs of active arm movements, without visual cues, one has to use proprioceptive information to determine limb position. Although this psychophysical study was conducted 2 decades before the English physiologist Charles Sherrington proposed his “proprioception” concept, Munsterberg and Cattell's apparatus and methodology was not recognized as a method for conducting proprioceptive assessment for over 100 years.
There are three classical methods used in psychophysical experiments: the method of adjustment, the method of limits and the method of constant stimuli.76 In the method of adjustment, also known as the method of average error,76 the participant is required to control the level of the stimulus, starting with a level that is clearly less or greater than a reference stimulus, and then to adjust the level until they feel that the level of the stimulus is the same as the level of the reference stimulus. The difference between the adjustable stimulus and the reference one is recorded as the participant's error, and the average error is calculated as the measure of sensitivity. The current JPR proprioception test protocol is one form of the method of adjustment, where participants are usually asked to match or reproduce the previously experienced reference joint positions, using their ipsilateral or the contralateral limb.1
The method of limits can be conducted in either an ascending or descending fashion. In the ascending method of limits, the experimenter begins the stimulus at such a low level that it cannot be detected by the participant. The level of stimulus is then gradually increased until the participant reports that they can just perceive it. In the descending method of limits, the procedure is reversed.76 These two methods are usually used alternately in experiments and the thresholds are averaged. A limitation of the ascending and descending methods is that the participant may anticipate that the stimulus is about to become noticeable or unnoticeable and, consequently, make a premature judgement. Conversely, the participants may also become conditioned to report that they detect a stimulus and continue to report the same way. In this sense, the TTDPM proprioception technique is one form of the method of limits, where participants are required to detect joint movement under different velocities.69
In contrast, in the method of constant stimuli (originally, right and wrong cases), the levels of stimulus intensity are not presented in a sequential order, but rather, in pairings with the standard stimulus, presented randomly. Therefore, the method of constant stimuli prevents the participant from predicting the level of the next stimulus, and thus reduces errors of expectation and habituation. To obtain an “absolute threshold”, the participant is required to report whether they are able to detect the stimulus; whereas to obtain “difference thresholds”, the participant makes a comparison between the constant stimulus and stimuli at each of the different levels presented. Thus, unlike the method of adjustment, with the method of constant stimuli participants compare two movements, both of which have clearly defined start and end positions, to determine which stimulus is greater. The method of constant stimulus has been thought to be the most accurate of Fechner's methods for studying the psychophysics of movement.77 From Fullerton and Cattell's work77 onwards, the method of constant stimuli has been widely used for assessing an individual's sensitivity to upper78, 79, 80, 81, 82, 83 and lower70, 84, 85 limb movements. Some of these studies have employed just noticeable difference (JND) as a measure for discrimination threshold in proprioception.70, 83, 84, 85 However, The JND discrimination measure method is based on a curve-fitting procedure which means that outliers exert a distorting effect,86 and that it is better suited to data sets based on several hundred trials. Fullerton and Cattell77 suggested that as a measure, “the probable error that is the difference with which an observer is right 75% of the time, is the most convenient measure of discrimination”, and they also noted that the method of constant stimuli “requires a large number of trials, which is not practical for clinical, anthropometric or provisional purposes”.
The number of trials can be reduced when only the variable stimuli are presented and the standard movement is eliminated, as in the method of single stimuli.87, 88 If the same number of responses and stimuli are used, this becomes the method of absolute judgement.89 Using the absolute judgement method, Waddington and Adams38 developed the AMEDA to test participants' ability to use proprioceptive information to differentiate between ankle inversion angles. In recent years, the AMEDA technique has been developed and validated for testing proprioception at the knee,90, 91, 92 hip,66, 93 lumbar spine,94, 95 cervical spine,96 shoulder,97, 98 and hand.37, 99, 100 The same technique has been termed “interdental dimension discrimination” when used for assessing proprioception at the jaw in dentistry and oral rehabilitation.101, 102
3. Apparatus for proprioception tests
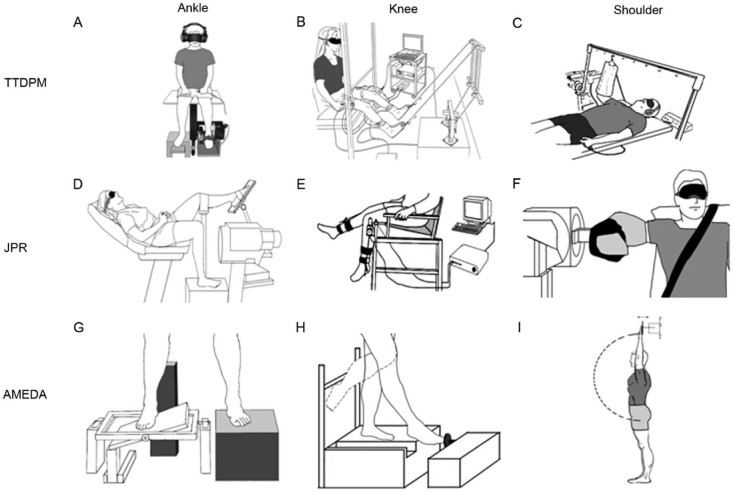
Ankle, knee, and shoulder proprioception have been extensively investigated by sports science and medical researchers. The three different approaches to test proprioceptive acuity at the ankle, knee and shoulder are presented in Fig. 1 for comparison. Each technique uses a different physical setup and explores different aspects of proprioceptive functioning (Table 1).
Fig. 1.
Comparison of different apparatus employed in threshold to detection of passive motion (TTDPM), joint position reproduction (JPR), and active movement extent discrimination apparatus (AMEDA) proprioception tests, at the ankle, knee, and shoulder. (A) Adapted from Yasuda et al.;56 (B) adapted from Beynnon et al.;131 (C) adapted from Lephart et al.;132 (D) adapted from Willems et al.;133 (E) adapted from Larsen et al.;134 (F) adapted from Janwantanakul et al.;135 (G) adapted from Symes et al.;136 (H) adapted from Cameron and Adams;90 (I) adapted from Han et al.54
Table 1.
Comparison of protocols used in TTDPM, JPR, and AMEDA proprioception tests.
| Variable | TTDPM | JPR | AMEDA |
|---|---|---|---|
| Movement type | Passive | Passive/active | Active |
| Movement velocity | Very slow | Slow/normal | Normal |
| Practice/familiarization trial number | Unfixed | Unfixed | Fixed, 15 trials |
| Testing trial number | 3–5 correct answers | Usually 3–5, up to 10 trials | 50 |
| Movement difference between familiarization and testing | No | Depends on the types of movement used in target joint position establishment and reproduction | No |
| Proprioceptive information | Largely movement information | Depends on whether a physical stop is used during target joint position establishment | Both movement and position information |
| General vision | Blocked | Blocked | Available |
| Audio | Blocked | Available | Available |
| Posture | Usually lying or sitting | Usually lying or sitting | Standing |
| Constrain | Usually constrained | Usually constrained | No constrains |
| Weight-bearing | Usually none or partial weight-bearing | None, partial or normal weight-bearing | Normal weight-bearing |
| Attention requirement | Very high | High | Medium-high |
| Memory requirement | Very low | High | Low (recall) |
| Measurement | Difference between the start position and responded position | Error between the target position and performed position | AUC score |
| Unit | Degree | Degree | AUC score |
| Testing duration | Up to 6 h | Depends on the number of trials used | 10 min |
Abbreviations: TTDPM = threshold to detection of passive motion; JPR = joint position reproduction; AMEDA = active movement extent discrimination apparatus; AUC = area under the curve.
With respect to ease of applicability of the three testing methods, it is clear from Fig. 1 and Table 1 that the experimental setups differ in complexity, due to the necessity of having motors apply forces to slowly move body segments for some proprioception tests. In addition, the lack of portability of the testing apparatus and the prolonged testing sessions have been highlighted as problematic for particular testing methods, particularly when attempting to obtain large sample numbers.103
4. Testing procedures for each of the proprioception testing method
The TTDPM method has been employed at various joints across the body (Fig. 1A–C), with the investigator-controlled machine moving an isolated body segment in a predetermined direction, using different speeds.104, 105 Velocity-dependent differences have been detected, with individuals typically demonstrating higher thresholds for detecting the applied force at slower speeds.104 A number of researchers have selected very slow speeds in their experiments, such as 0.25°/s, for example, generated by the Biodex System.106 During a TTDPM test, participants are seated or lying down. The body site being tested is isolated by strapping the adjacent body segments, such as the upper body. Other peripheral information, such as tactile, visual, and aural information, is usually occluded by using air cushions, blindfolds, and headphones. With all these variables controlled, the body segment under investigation is passively moved in a predetermined direction. Participants are instructed to press a stop-button as soon as they perceive the movement and direction. They then report the perceived direction of movement of their limb. If the reported direction is wrong, the trial is discarded, and testing proceeds until three to five correct judgements are achieved.106 Gibson107 classifies the proprioception arising when an external device passively moves a body part, as occurs in TTDPM, as “imposed proprioception”, which he contrasts with the “obtained proprioception” that arises from active, voluntary movements.
In contrast to the TTDPM method where passive movement is used, the JPR testing method is conducted under either passive or active conditions for criterion and reproduction movements, and may involve either ipsilateral or contralateral limb movements1 (Fig. 1D–F). There are three types of JPR tasks described in the assessment of proprioception: ipsilateral JPR (IJPR); and two contralateral JPR (CJPR) approaches. For IJPR testing, a predetermined target joint position is passively or actively presented to the participant for a few seconds. Thereafter, the joint is returned to the initial start position, either passively by the experimenter or actively by the participant. Participants are then required to reproduce the target joint position previously experienced by either indicating the target position by pressing a stop-button when the joint is passively moved into the same range, or by actively moving the joint to the target position. That is, participants need to remember the target position and reproduce the position using the same limb. Of the two CJPR tests, one procedure is identical to the method for IJPR testing in terms of experiencing the target joint position, but differs in that the participant is asked to reproduce the joint position by using the contralateral limb. That is, participants need to remember the target joint position and use the opposite limb to reproduce the position. The second CJPR test differs in that once one joint is moved to the target position, it remains in that position and the contralateral limb is required to reproduce the target joint position. That is, the test does not require a memory of the target position, but rather, participants can use this “online” information in the position task to help them to replicate the position on the contralateral side.
AMEDA tests (Fig. 1G–I) are conducted using active movements.70 Each participant is given a familiarization session using an AMEDA apparatus before data collection commences, during which they are informed that they will experience, for example, five movement displacement distances, in order, from the smallest (moving to position 1) to the largest (moving to position 5), three times: 15 movements in total. Participants thereafter (typically) undertake 50 trials of testing, in which all five positions are presented 10 times, in a random order. On each trial in the AMEDA test protocol, only one movement out to the stop at a steady pace is allowed, followed by return to the start position. After experiencing a position and returning to the start position, participants are asked to make a judgement as to the position number (1, 2, 3, 4, or 5) of each test movement, without feedback being given as to the correctness to the judgement they make for each trial. That is, participants must use their memory of the five movement extents from the familiarization trials to enable them to identify each stimulus and thus make a numerical judgement (1, 2, 3, 4, or 5) identifying each perceived stimulus after it is presented. This task is thus a single stimulus or absolute judgement task, wherein a single stimulus is presented and single response is made on each trial. The time required to undertake one joint proprioception test is approximately 10 min.
5. Testing protocols for each of the proprioceptive methods
Details of the protocols for each of the proprioceptive methods are listed and compared in Table 1. The different attributes of the three protocols are listed. The ecological validity, testing validity, and data validity of each technique varies between the different methods.
Both the TTDPM and JPR techniques seek to minimize extraneous variables and reduce factors thought to be confounders, in order to explore proprioceptive sense in isolation. In contrast, the AMEDA approach seeks to examine how proprioception functions under natural conditions using test conditions that are more analogous to normal function. Some researchers have argued that both the TTDPM and JPR tests of proprioception lack ecological validity108, 109 because the testing conditions are so different from normal function that they can contribute little to understanding the role proprioception plays in daily and sporting activities. In addition, performances obtained at different TTDPM test speeds may not be correlated.71
A number of the variables listed in Table 1 are employed to minimize other inputs and thus ensure test purity, but they may also diminish ecological validity. Examples of this are protocols that use very slow movement velocities, passive movements, non-weight bearing conditions and isolation of the joint under investigation. That is to say, few everyday movement patterns involve passively imposed movements, delivered at very slow velocities.110 In contrast, most daily activities require active movements at normal, functional speeds.40 Although the isolation of inputs with a proprioceptive testing protocol may be achieved when participants are strapped in a machine (usually lying or sitting and non-weight-bearing) with vision and audition blocked out, the cost of this is that the testing does not reflect normal performance of the proprioceptive system in the real world, where individuals move freely in normal weight-bearing condition, with both visual and auditory information available. In contrast, ecological validity is enhanced by having these latter conditions available.111
Rather than focussing on a single joint to detect whether the relevant segment has been moved, the role of proprioceptive ability in real world activities is to enable the performer to accurately judge limb movements when interacting with the environment, such as making an immediate, and likely implicit, judgement as to the degree of ankle inversion when stepping on an uneven surface in order to keep one's balance. Because most upper and lower limb functional movements are terminated with physical stops, such as the sides of a drinking glass or the slope of the ground, testing methods that encompass movement extent and limb endpoint position information can be argued to be more realistic and ecologically valid.79 Testing methods that allow not only different submodalities of the proprioceptive senses, but which do not entirely eliminate other sense information such as that of texture, vision and hearing, are more likely to characterize normal function. Therefore, if ecological validity is a research goal, the AMEDA testing method is more suitable than either the TTDPM or the JPR protocols.
The validity of the testing protocol is another important consideration when determining which procedure to use for testing proprioception. It has been argued that JPR tests for proprioception have low testing validity, because the proprioceptive information available during target position generation and the proprioceptive information available during target position reproduction are not the same.108, 109 The first difference between target position establishment and reproduction is the type of movement undertaken. It has been suggested that in passive movement, since muscles are not active, fusimotor activity and the sensory feedback from muscle spindles are diminished. Thus, input from cutaneous receptors appears to play a greater role in sensory feedback. In contrast, in active movement control, fusimotor drive and muscle spindle feedback are both involved, although input from muscle spindles is considered to play a more dominant role.112, 113 As a result, when a target joint position is passively generated for active matching, or vice versa, the brain may rely on different information from different receptors in the two phases, and the results may even reflect hemispheric specialization in the use of particular proprioceptive information at that joint.36 Another difference between the first or criterion movement and the second reproduction movement in JPR tests is that there is usually a physical stop at the end of the criterion movement for defining the target position, while the physical stop is removed during position reproduction. That is, during target position generation, information about movement extent and end position are both available, whereas only movement extent information is available in position reproduction. Although a movement extent/displacement matching strategy has been thought to be less effective than target position matching,33 information about both limb movement extent and end position are needed for the most accurate judgement of limb movements.79 Finally, because JPR tests are highly dependent on memory, particularly CJPR tests where participants need to remember a previously experienced joint position of one limb and use the contralateral limb to reproduce the target position, JPR tests are less appropriate when participants have cognitive or memory deficits.1
The validity of data generated from the different protocols is another issue when determining which form of testing to employ. Issues may arise from both data acquisition and data analysis processes adopted. During data acquisition, proprioceptive tests usually involve a practice or familiarization session. However, the number of practice/familiarization trials varies between testing protocols. For example, some studies report using three practice trials before data collection,106 while others collect the test data only when participants are satisfied with the amount of practice.114 Different numbers of practice/familiarization trials may lead to learning or fatigue effects and consequently affect data accuracy. In addition, TTDPM tests record only “correct” answers and discard the trials if participants make wrong judgements.106 Thus, it is possible that relatively low threshold data may be obtained from a higher proportion of wrong decisions and relatively high threshold data arise from a lower wrong judgement ratio. That is, a better result may be the outcome of chance responding. However, few studies have reported the percentage of the incorrect trials in their results; therefore it is unknown whether there is a relationship between correctness of responses and accuracy of results. Similarly, in most JPR tests, attention is seldom paid to the number of movements that participants use in position reproduction, and information is rarely given as to exactly how participants adjust the limb to reproduce the previously experienced target position.1 Further, the number of sampling movements has been shown to have an impact on judgement accuracy,115 suggesting that failure to control number of movements in JPR tests could confound the results. Moreover, most TTDPM and JPR assessment protocols usually use only 3–5 trials during the test.106, 113, 116, 117 This number may be insufficient to accurately determine participant ability parameters in proprioceptive tests, as noted by Ashton-Miller.109 A recent study estimated that 20% of post-stroke patients with proprioceptive deficits would be unidentified if only three trials were used rather than 10 trials; however when 10 trials were used, not all patients with proprioceptive deficits were identified, suggesting that even 10 trials to obtain a proprioceptive sensitivity measure is insufficient to set as the “gold standard” for a JPR protocol.118 Of the three proprioceptive techniques, only AMEDA testing requires more than 10 trials.
In terms of data analysis, the usefulness of the accuracy metric derived in both TTDPM and JPR procedures has also been questioned.27, 119 The mean value of the differences between the start and perceived positions in TTDPM tests, or between the target and reproduced positions in the JPR tests, has been interpreted as an assessment of accuracy, and the error variance an assessment of consistency. However, the mean value of the difference alone is unlikely to adequately convey proprioceptive information, because data can present as either a small mean difference with a large error variance or as a large mean difference with a small error variance. That is, participants can be very accurate, on average with a large trial variation, or have a high level of inaccuracy with excellent performance consistency. When processing proprioceptive information, the brain has to deal with noise in the CNS arising from spontaneous or background neural activity120 that results in uncertainty in making a decision about a joint's position in space. The AMEDA proprioception measurement was developed based on the signal detection theory121, 122 to provide a means of analysing response data collected in the presence of uncertainty, such that sensitivity to a stimulus can be evaluated regardless of response bias.123 Using the receiver operating characteristic (ROC) analysis, participants' ability to use a continuous response scale to discriminate between the two states of a binary variable can be measured, representing how certain participants are when they make judgements on joint movements against noise. The area under the ROC curve (AUC) represents the participant's ability to discriminate between two joint movements, which can be calculated by geometric means.124 If the participant is unable to discriminate between the two movements, the ROC curve would cut off half of the area and giving an AUC value of 0.5, equivalent to chance responding. In contrast, if the participant is able to perfectly discriminate two movements, the corresponding AUC would include all area below the ROC curve, and give a perfect AUC value of 1.0.121, 122, 124
In summary, signal detection theory offers a means to take a participant's uncertainty into account and produce an unbiased estimate of a participant's proprioceptive performance. This method requires many more trials to more closely reflect the actual distribution of proprioceptive signal presentation in the brain than are currently used in TTDPM and JPS methodologies. While it is intuitively easier to understand more direct measures than the theoretical underpinnings of signal detection analysis, it does not necessarily mean that the former are more accurate. On the contrary, it is likely that signal detection theory methods capture and reflect more accurately the neural mechanisms underlying proprioceptive performance, which include proprioceptive signal collecting and processing against noise in the CNS, and decision making as to a joint's position in space, than do the other methods.
6. Scope of review
The current review has considered kinematic aspects of proprioception. The senses of effort, force, and heaviness are also considered by some researchers to be components of proprioception.50, 125 However, the relationships between movement-related and force-related aspects of proprioception are still unclear. Early studies suggested that the extent to which somatosensory information is used for effort perception is associated with the amplitude of movements.126 Contrary to this notion, Han et al.100 recently found finger pinch movement discrimination accuracy was not affected by the presence of elastic resistance, indicating that movement-related and force-related aspects of proprioception are separate entities and may have different neural mechanisms. In line with this argument, a recent study found that sense of effort was processed centrally, with little or even no contribution from peripheral sensory information,127 contrary to the current understanding of movement-related proprioception, which requires both peripheral and central processing mechanisms.
7. Conclusion
Proprioception plays a crucial role in human movement control, which is fundamental for daily activities, exercise, and sports. The importance of central processing in understanding proprioception has been recognized in recent years. However, the peripheral and central mechanisms underlying proprioceptive control are still unclear. To explore proprioceptive mechanisms, three techniques have been widely used in the literature, but their applicability, ecological validity, test validity, and data validity differ. The TTDPM method has less relative ecological validity, but has high conceptual purity,72 given the prior relaxation of the stimulated musculature, and the control of other information sources. This method has been widely used in neurophysiology studies,105, 128, 129 when differentiating between the contribution of different mechanoreceptors to proprioception.112 Although JPR tests may have less relative test validity, the method is efficient and enables exploration of hemispheric asymmetries in sensorimotor abilities.1 The AMEDA method appears to have better ecological validity and relatively better test validity and data validity. However, as a proprioceptive sensitivity measure, the AUC score is not as intuitively accessible as the average error measure given by JPR methods, or the threshold in degrees given by TTDPM methods. Nevertheless, it can be argued that the AMEDA test method is an effective method for assessing the performance of proprioceptive system during active, functional body movements that occur in most daily activities, exercise, and sports.
In addition to the current theoretical comparisons between the three methods, any data obtained from a proprioception testing method should have relevance and predictive validity in sport performance or clinical contexts. To date, only a few studies have investigated associations between proprioception and sport performance,54 and proprioception and injury,41, 66, 130 and no empirical comparison between the three methods with regards to their predictive validity has been undertaken.
Authors' contributions
All authors conceived of the study. JH reviewed the literature and drafted the manuscript. GW participated in the study design and helped to draft the manuscript. RA participated in the study design and helped to draft the manuscript. JA participated in the study design and helped to draft the manuscript. YL made edits and comments to the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order and presentation of the authors.
Competing interests
None of the authors declare competing financial or other sorts of interests.
Acknowledgments
The authors would like to thank the University of Canberra, Key Laboratory of Exercise and Health Sciences of Ministry of Education, Shanghai University of Sport and Shanghai Municipal Science and Technology Commission (No. 13490503800) for funding the research. This paper was also supported by Shanghai Pujiang Program (No. 15PJ1407600). The funding source had no involvement in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. None of the authors have any relevant conflicts of interest.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.Goble D.J. Proprioceptive acuity assessment via joint position matching: from basic science to general practice. Phys Ther. 2010;90:1176–1184. doi: 10.2522/ptj.20090399. [DOI] [PubMed] [Google Scholar]
- 2.Xerri C. Plasticity of cortical maps: multiple triggers for adaptive reorganization following brain damage and spinal cord injury. Neuroscientist. 2012;18:133–148. doi: 10.1177/1073858410397894. [DOI] [PubMed] [Google Scholar]
- 3.Xerri C., Merzenich M.M., Peterson B.E., Jenkins W. Plasticity of primary somatosensory cortex paralleling sensorimotor skill recovery from stroke in adult monkeys. J Neurophysiol. 1998;79:2119–2148. doi: 10.1152/jn.1998.79.4.2119. [DOI] [PubMed] [Google Scholar]
- 4.Pleger B., Schwenkreis P., Dinse H.R., Ragert P., Höffken O., Malin J.P. Pharmacological suppression of plastic changes in human primary somatosensory cortex after motor learning. Exp Brain Res. 2003;148:525–532. doi: 10.1007/s00221-002-1324-1. [DOI] [PubMed] [Google Scholar]
- 5.Schwenkreis P., Pleger B., Höffken O., Malin J.P., Tegenthoff M. Repetitive training of a synchronised movement induces short-term plastic changes in the human primary somatosensory cortex. Neurosci Lett. 2001;312:99–102. doi: 10.1016/s0304-3940(01)02196-6. [DOI] [PubMed] [Google Scholar]
- 6.Ogard W.K. Proprioception in sports medicine and athletic conditioning. Strength Cond J. 2011;33:111–118. [Google Scholar]
- 7.Bell C. On the nervous circle which connects the voluntary muscles with the brain. Philosophi Trans Royal Soc. 1826;116:163–173. [PMC free article] [PubMed] [Google Scholar]
- 8.Bastian H.C. The “muscular sense”: its nature and cortical localisation. Brain. 1887;10:1–88. [Google Scholar]
- 9.Sherrington C.S., editor. The integrative action of the nervous system. Cambridge University Press; Cambridge: 1906. [Google Scholar]
- 10.Swanik C.B., Lephart S.M., Rubash H.E. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Jt Surg. 2004;86:328–334. doi: 10.2106/00004623-200402000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Swanik K.A., Lephart S.M., Swanik C.B., Lephart S.P., Stone D.A., Fu F.H. The effects of shoulder plyometric training on proprioception and selected muscle performance characteristics. J Shoulder Elbow Surg. 2002;11:579–586. doi: 10.1067/mse.2002.127303. [DOI] [PubMed] [Google Scholar]
- 12.Safran M.R., Borsa P.A., Lephart S.M., Fu F.H., Warner J.J. Shoulder proprioception in baseball pitchers. J Shoulder Elbow Surg. 2001;10:438–444. doi: 10.1067/mse.2001.118004. [DOI] [PubMed] [Google Scholar]
- 13.Lephart S.M., Pincivero D.M., Giraldo J.L., Fu F.H. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25:130–137. doi: 10.1177/036354659702500126. [DOI] [PubMed] [Google Scholar]
- 14.Myers J.B., Guskiewicz K.M., Schneider R.A., Prentice W.E. Proprioception and neuromuscular control of the shoulder after muscle fatigue. J Athl Train. 1999;34:362–367. [PMC free article] [PubMed] [Google Scholar]
- 15.Ergen E., Ulkar B. Proprioception and ankle injuries in soccer. Clin Sports Med. 2008;27:195–217. doi: 10.1016/j.csm.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 16.Wingert J.R., Burton H., Sinclair R.J., Brunstrom J.E., Damiano D.L. Joint position sense and kinesthesia in cerebral palsy. Arch Phys Med Rehabil. 2009;90:447–453. doi: 10.1016/j.apmr.2008.08.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duzgun I., Kanbur N.O., Baltaci G., Aydin T. Effect of tanner stage on proprioception accuracy. J Foot Ankle Surg. 2011;50:11–15. doi: 10.1053/j.jfas.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 18.Maier M., Niklasch M., Dreher T., Wolf S.I., Zeifang F., Loew M. Proprioception 3 years after shoulder arthroplasty in 3D motion analysis: a prospective study. Arch Orthop Trauma Surg. 2012;132:1003–1010. doi: 10.1007/s00402-012-1495-6. [DOI] [PubMed] [Google Scholar]
- 19.Lephart S.M., Fu F.H. The role of proprioception in the treatment of sports injuries. Sports Exerc Inj. 1995;1:96–102. [Google Scholar]
- 20.McCloskey D.I. Differences between the senses of movement and position shown by the effects of loading and vibration of muscles in man. Brain Res. 1973;61:119–131. doi: 10.1016/0006-8993(73)90521-0. [DOI] [PubMed] [Google Scholar]
- 21.Proske U., Gandevia S.C. The kinaesthetic senses. J Physiol London. 2009;587:4139–4146. doi: 10.1113/jphysiol.2009.175372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCloskey D.I. Kinesthetic sensibility. Physiol Rev. 1978;58:763–820. doi: 10.1152/physrev.1978.58.4.763. [DOI] [PubMed] [Google Scholar]
- 23.Clark F.J., Burgess R.C., Chapin J.W., Lipscomb W.T. Role of intramuscular receptors in the awareness of limb position. J Neurophysiol. 1985;54:1529–1540. doi: 10.1152/jn.1985.54.6.1529. [DOI] [PubMed] [Google Scholar]
- 24.Taylor J.L., McCloskey D.I. Ability to detect angular displacements of the fingers made at an imperceptibly slow speed. Brain. 1990;113:157–166. doi: 10.1093/brain/113.1.157. [DOI] [PubMed] [Google Scholar]
- 25.Gregory J.E., Morgan D.L., Proske U. After effects in the responses of cat muscle spindles and errors of limb position sense in man. J Neurophysiol. 1988;59:1220–1230. doi: 10.1152/jn.1988.59.4.1220. [DOI] [PubMed] [Google Scholar]
- 26.Stillman B.C. Making sense of proprioception: the meaning of proprioception, kinaesthesia and related terms. Physiotherapy. 2002;88:667–676. [Google Scholar]
- 27.Clark F.J., Horch K.W. Kinesthesia. In: Boff K.R., Kaufman L., Thomas J.P., editors. Handbook of perception and human performance. Wiley; New York, NY: 1986. pp. 11–62. [Google Scholar]
- 28.Schmidt R.A. Human Kinetics; Champaign, IL: 1991. Motor learning and performance: from principles to practice. [Google Scholar]
- 29.Steinicke F., Whitton M.C., Lecuyer A., Mohler B. China; Hong Kong: 2011. Perceptually inspired methods for naturally navigating virtual worlds. SIGGRAPH Asia 2011 Courses. [Google Scholar]
- 30.Schacter D.L., Gilbert D.T., Wegner D.M. Worth Publishers; New York, NY: 2010. Introducing psychology. [Google Scholar]
- 31.Goldstein E.B. 8th ed. Wadswooth; Pacific Grove, CA: 2009. Sensation and perception. [Google Scholar]
- 32.Bernstein D., Nash P. 4th ed. Houghton-Mifflin; Boston, MA: 2008. Essentials of psychology. [Google Scholar]
- 33.Goble D.J., Noble B.C., Brown S.H. Proprioceptive target matching asymmetries in left-handed individuals. Exp Brain Res. 2009;197:403–408. doi: 10.1007/s00221-009-1922-2. [DOI] [PubMed] [Google Scholar]
- 34.Goble D.J., Noble B.C., Brown S.H. Proprioceptive target matching asymmetries in left-handed individuals. Exp Brain Res. 2009;197:403–408. doi: 10.1007/s00221-009-1922-2. [DOI] [PubMed] [Google Scholar]
- 35.Suprak D.N. Shoulder joint position sense is not enhanced at end range in an unconstrained task. Hum Move Sci. 2011;30:424–435. doi: 10.1016/j.humov.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 36.Han J. University of Canberra; Canberra: 2013. Multiple joint proprioception in movement discrimination. Dissertation. [Google Scholar]
- 37.Han J., Anson J., Waddington G., Adams R. Proprioceptive performance of bilateral upper and lower limb joints: side-general and site-specific effects. Exp Brain Res. 2013;226:313–323. doi: 10.1007/s00221-013-3437-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Waddington G., Adams R. Ability to discriminate movements at the ankle and knee is joint specific. Percept Mot Skills. 1999;89:1037–1041. doi: 10.2466/pms.1999.89.3.1037. [DOI] [PubMed] [Google Scholar]
- 39.Han J., Waddington G., Adams R., Anson J. A proprioceptive ability underlying all proprioception tests? Response to tremblay. Percept Mot Skills. 2014;119:301–304. doi: 10.2466/10.23.24.PMS.119c16z2. [DOI] [PubMed] [Google Scholar]
- 40.Ashton-Miller J.A., Wojtys E.M., Huston L.J., Fry-Welch D. Can proprioception really be improved by exercises? Knee Surg Sports Traumatol Arthrosc. 2001;9:128–136. doi: 10.1007/s001670100208. [DOI] [PubMed] [Google Scholar]
- 41.Witchalls J., Blanch P., Waddington G., Adams R. Intrinsic functional deficits associated with increased risk of ankle injuries: a systematic review with meta-analysis. Br J Sports Med. 2012;46:515–523. doi: 10.1136/bjsports-2011-090137. [DOI] [PubMed] [Google Scholar]
- 42.Lee H.M., Liau J.J., Cheng C.K., Tan C.M., Shih J.T. Evaluation of shoulder proprioception following muscle fatigue. Clin Biomech. 2003;18:843–847. doi: 10.1016/s0268-0033(03)00151-7. [DOI] [PubMed] [Google Scholar]
- 43.Carpenter J.E., Blasier R.B., Pellizzon G.G. The effects of muscle fatigue on shoulder joint position sense. Am J Sports Med. 1998;26:262–265. doi: 10.1177/03635465980260021701. [DOI] [PubMed] [Google Scholar]
- 44.Ribeiro F., Oliveira J. Aging effects on joint proprioception: the role of physical activity in proprioception preservation. Eur Rev Aging Phys Act. 2007;4:71–76. [Google Scholar]
- 45.Ribeiro F., Oliveira J. Factors influencing proprioception: what do they reveal? In: Klika V., editor. Biomechanics in applications. InTech; Rijeka: 2011. [Google Scholar]
- 46.Willems T.M., Witvrouw E., Delbaere K., Mahieu N., De Bourdeaudhuij I., De Clercq D. Intrinsic risk factors for inversion ankle sprains in male subjects — a prospective study. Am J Sports Med. 2005;33:415–423. doi: 10.1177/0363546504268137. [DOI] [PubMed] [Google Scholar]
- 47.Burke D., Hagbarth K.E., Lofstedt L., Wallin B.G. The responses of human muscle spindle endings to vibration of non-contracting muscles. J Physiol. 1976;261:673–693. doi: 10.1113/jphysiol.1976.sp011580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Barrack R.L., Skinner H.B., Brunet M.E., Haddad R.J., Jr Functional performance of the knee after intraarticular anesthesia. Am J Sports Med. 1983;11:258–261. doi: 10.1177/036354658301100414. [DOI] [PubMed] [Google Scholar]
- 49.Clark F.J., Grigg P., Chapin J.W. The contribution of articular receptors to proprioception with the fingers in humans. J Neurophysiol. 1989;61:186–193. doi: 10.1152/jn.1989.61.1.186. [DOI] [PubMed] [Google Scholar]
- 50.Proske U., Gandevia S.C. The proprioceptive senses: their roles in signalling body shape, body position and movement, and muscle force. Physiol Rev. 2012;92:1651–1697. doi: 10.1152/physrev.00048.2011. [DOI] [PubMed] [Google Scholar]
- 51.Smetacek V., Mechsner F. Making sense. Nature. 2004;432:21. doi: 10.1038/432021a. [DOI] [PubMed] [Google Scholar]
- 52.Provins K.A. The specificity of motor skill and manual asymmetry: a review of the evidence and its implications. J Mot Behav. 1997;29:183–192. doi: 10.1080/00222899709600832. [DOI] [PubMed] [Google Scholar]
- 53.Han J., Anson J., Waddington G., Adams R. Sport attainment and proprioception. Int J Sports Sci Coach. 2014;9:159–170. [Google Scholar]
- 54.Han J., Waddington G., Anson J., Adams R. Level of competitive success achieved by elite athletes and multi-joint proprioceptive ability. J Sci Med Sport. 2015;18:77–81. doi: 10.1016/j.jsams.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 55.Yogev-Seligmann G., Hausdorff J.M., Giladi N. The role of executive function and attention in gait. Mov Disord. 2008;23:329–342. doi: 10.1002/mds.21720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yasuda K., Sato Y., Iimura N., Iwata H. Allocation of attentional resources toward a secondary cognitive task leads to compromised ankle proprioceptive performance in healthy young adults. Rehabil Res Prac. 2014;2014:7. doi: 10.1155/2014/170304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Goble D.J., Coxon J.P., Van Impe A., Geurts M., Doumas M., Wenderoth N. Brain activity during ankle proprioceptive stimulation predicts balance performance in young and older adults. J Neurosci. 2011;31:16344–16352. doi: 10.1523/JNEUROSCI.4159-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liu J., Wang X.Q., Zheng J.J., Pan Y.J., Hua Y.H., Zhao S.M. Effects of Tai Chi versus proprioception exercise program on neuromuscular function of the ankle in elderly people: a randomized controlled trial. Evid Based Complement Altern Med. 2012;2012:265486. doi: 10.1155/2012/265486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guo L.Y., Yang C.P., You Y.L., Chen S.K., Yang C.H., Hou Y.Y. Underlying mechanisms of Tai-Chi-Chuan training for improving balance ability in the elders. Chin J Integr Med. 2014;20:409–415. doi: 10.1007/s11655-013-1533-4. [DOI] [PubMed] [Google Scholar]
- 60.Waddington G., Adams R.D. The effect of a 5-week wobble-board exercise intervention on ability to discriminate different degrees of ankle inversion, barefoot and wearing shoes: a study in healthy elderly. J Am Geriatr Soc. 2004;52:573–576. doi: 10.1111/j.1532-5415.2004.52164.x. [DOI] [PubMed] [Google Scholar]
- 61.Nodehi-Moghadam A., Nasrin N., Kharazmi A., Eskandari Z. A comparative study on shoulder rotational strength, range of motion and proprioception between the throwing athletes and non-athletic persons. Asian J Sports Med. 2013;4:34–40. doi: 10.5812/asjsm.34528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lin C.H., Lien Y.H., Wang S.F., Tsauo J.Y. Hip and knee proprioception in elite, amateur, and novice tennis players. Am J Phys Med Rehabil. 2006;85:216–221. doi: 10.1097/01.phm.0000200376.12974.41. [DOI] [PubMed] [Google Scholar]
- 63.Muaidi Q.I., Nicholson L.L., Refshauge K.M. Do elite athletes exhibit enhanced proprioceptive acuity, range and strength of knee rotation compared with non-athletes? Scand J Med Sci Sports. 2009;19:103–112. doi: 10.1111/j.1600-0838.2008.00783.x. [DOI] [PubMed] [Google Scholar]
- 64.Courtney C.A., Rine R., Jenk D.T., Collier P.D., Waters A. Enhanced proprioceptive acuity at the knee in the competitive athlete. J Orthop Sports Phys Ther. 2013;43:422–426. doi: 10.2519/jospt.2013.4403. [DOI] [PubMed] [Google Scholar]
- 65.Baker J., Horton S., Robertson-Wilson J., Wall M. Nurturing sport expertise: factors influencing the development of elite athlete. J Sports Sci Med. 2003;2:1–9. [PMC free article] [PubMed] [Google Scholar]
- 66.Cameron M., Adams R., Maher C. Motor control and strength as predictors of hamstring injury in elite players of Australian football. Phys Ther Sport. 2003;4:159–166. [Google Scholar]
- 67.Lephart S.M., Fu F.H., editors. Proprioception and neuromuscular control in joint stability. Human Kinetics; Champaign, IL: 2000. [Google Scholar]
- 68.Weerakkody N.S., Blouin J.S., Taylor J.L., Gandevia S.C. Local subcutaneous and muscle pain impairs detection of passive movements at the human thumb. J Physiol (London) 2008;586:3183–3193. doi: 10.1113/jphysiol.2008.152942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lephart S.M., Myers J.B., Bradley J.P., Fu F.H. Shoulder proprioception and function following thermal capsulorraphy. Arthroscopy. 2002;18:770–778. doi: 10.1053/jars.2002.32843. [DOI] [PubMed] [Google Scholar]
- 70.Waddington G., Adams R. Discrimination of active plantarflexion and inversion movements after ankle injury. Aust J Physiother. 1999;45:7–13. doi: 10.1016/s0004-9514(14)60335-4. [DOI] [PubMed] [Google Scholar]
- 71.de Jong A., Kilbreath S.L., Refshauge K.M., Adams R. Performance in different proprioceptive tests does not correlate in ankles with recurrent sprain. Arch Phys Med Rehabil. 2005;86:2101–2105. doi: 10.1016/j.apmr.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 72.Elangovan N., Herrmann A., Konczak J. Assessing proprioceptive function: evaluating joint position matching methods against psychophysical thresholds. Phys Ther. 2014;94:553–561. doi: 10.2522/ptj.20130103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Blake R., Sekuler R. 5th ed. McGraw-Hill; New York, NY: 2005. Perception. [Google Scholar]
- 74.Fechner G.T. Breitkopf und Härtel; Leipzig: 1860. Elemente der Psychophysik. [Google Scholar]
- 75.Adams R., Lee K.Y., Waddington G., Lee H.J. James McKeen Cattell and the method of constant stimuli in the psychophysics of movement. Proc Fechner Day. 2012;28:18–23. [Google Scholar]
- 76.Gescheider G.A. Lawrence Erlbaum Associates; Mahwah, NJ: 1997. Psychophysics: the fundamentals. [Google Scholar]
- 77.Fullerton G.S., Cattell J.M. University of Pennsylvania Press; Philadelphia, PA: 1892. On the perception of small differences: with special reference to the extent, force and time of movement. [Google Scholar]
- 78.Woodworth R.S. The accuracy of voluntary movement. Psychol Rev. 1899;3:1–14. [Google Scholar]
- 79.Magill R.A., Parks P.F. The psychophysics of kinesthesis for positioning responses: the physical stimulus-psychological response relationship. Res Q Exerc Sport. 1983;54:346–351. [Google Scholar]
- 80.Woodworth R.S., Schlosberg H. Holt, Rinehart & Winston; New York, NY: 1965. Experimental psychology. [Google Scholar]
- 81.Maher C., Adams R. A psychophysical evaluation of manual stiffness discrimination. Aust J Physiother. 1995;41:161–167. doi: 10.1016/S0004-9514(14)60426-8. [DOI] [PubMed] [Google Scholar]
- 82.Anderson D.I. The discrimination, acquisition, and retention of aiming movements made with and without elastic resistance. Hum Factor. 1999;41:129–138. doi: 10.1518/001872099779577291. [DOI] [PubMed] [Google Scholar]
- 83.Tan H.Z., Srinivasan M.A., Reed C.M., Durlach N.I. Discrimination and identification of finger joint-angle position using active motion. ACM Trans Appl Percept. 2007;4:1–4. [Google Scholar]
- 84.Pacey V., Adams R., Tofts L., Munns C., Nicholson L. Proprioceptive acuity into knee hypermobile range in children with joint hypermobility syndrome. Pediatr Rheumatol. 2014 doi: 10.1186/1546-0096-12-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Waddington G., Adams R., Jones A. Wobble board (ankle disc) training effects on the discrimination of inversion movements. Aust J Physiother. 1999;45:95–101. doi: 10.1016/s0004-9514(14)60341-x. [DOI] [PubMed] [Google Scholar]
- 86.Lee K.Y., Adams R., Lee H.J., Waddington G. Comparisons of indices of movement discrimination: psychometric function, information theory, and signal detection analysis. In: Leth-Steensen C., Schoenherr J.R., editors. Fechner Day 2012. The International Society of Psychophysics; Ottawa, ON: 2012. [Google Scholar]
- 87.Morgan M.J., Watamaniuk S.N.J., McKee S.P. The use of an implicit standard for measuring discrimination thresholds. Vision Res. 2000;40:2341–2349. doi: 10.1016/s0042-6989(00)00093-6. [DOI] [PubMed] [Google Scholar]
- 88.Woodworth R.S., Schlosberg H. Oxford and IBH Publishing; Oxford: 1954. Experimental psychology. [Google Scholar]
- 89.Miller G.A. The magical number seven, plus or minus two: some limits on our capacity for processing information. Psychol Rev. 1956;63:81–97. [PubMed] [Google Scholar]
- 90.Cameron M., Adams R. Kicking footedness and movement discrimination by elite Australian Rules footballers. J Sci Med Sport. 2003;6:266–274. doi: 10.1016/s1440-2440(03)80020-8. [DOI] [PubMed] [Google Scholar]
- 91.Waddington G., Seward H., Wrigley T., Lacey N., Adams R. Comparing wobble board and jump-landing training effects on knee and ankle movement discrimination. J Sci Med Sport. 2000;3:449–459. doi: 10.1016/s1440-2440(00)80010-9. [DOI] [PubMed] [Google Scholar]
- 92.Muaidi Q.L., Nicholson L.L., Refshauge K.M. Proprioceptive acuity in active rotation movements in healthy knees. Arch Phys Med Rehabil. 2008;89:371–376. doi: 10.1016/j.apmr.2007.08.154. [DOI] [PubMed] [Google Scholar]
- 93.Cameron M., Adams R.D., Maher C.G. The effect of neoprene shorts on leg proprioception in Australian football players. J Sci Med Sport. 2008;11:345–352. doi: 10.1016/j.jsams.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 94.Hobbs A.J., Adams R.D., Shirley D., Hillier T.M. Comparison of lumbar proprioception as measured in unrestrained standing in individuals with disc replacement, with low back pain and without low back pain. J Orthop Sports Phys Ther. 2010;40:439–446. doi: 10.2519/jospt.2010.40.7.439. [DOI] [PubMed] [Google Scholar]
- 95.Han J., Waddington G., Adams R., Anson J. Ability to discriminate movements at multiple joints around the body: global or site-specific. Percept Mot Skills. 2013;116:59–68. doi: 10.2466/24.10.23.PMS.116.1.59-68. [DOI] [PubMed] [Google Scholar]
- 96.Lee H., Nicholson L., Adams R., Bae S.S. Proprioception and rotation range sensitization associated with subclinical neck pain. Spine. 2005;30:E60–7. doi: 10.1097/01.brs.0000152160.28052.a2. [DOI] [PubMed] [Google Scholar]
- 97.Naughton J., Adams R.D., Maher C.G. Contacting points overhead with and without a tennis racquet. Percept Mot Skills. 2003;96:1323–1329. doi: 10.2466/pms.2003.96.3c.1323. [DOI] [PubMed] [Google Scholar]
- 98.Whiteley R.J., Adams R.D., Nicholson L.L., Ginn K.A. Shoulder proprioception is associated with humeral torsion in adolescent baseball players. Phys Ther Sport. 2008;9:177–184. doi: 10.1016/j.ptsp.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 99.Han J., Waddington G., Adams R., Anson J. Bimanual proprioceptive performance differs for right- and left-handed individuals. Neurosci Lett. 2013;542:37–41. doi: 10.1016/j.neulet.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 100.Han J., Waddington G., Anson J., Adams R. Does elastic resistance affect finger pinch discrimination? Hum Factor. 2013;55:976–984. doi: 10.1177/0018720813481620. [DOI] [PubMed] [Google Scholar]
- 101.Morimoto T., Hamada T., Kawamura Y. Alteration in directional specificity of interdental dimension discrimination with the degree of mouth opening. J Oral Rehabil. 1983;10:335–342. doi: 10.1111/j.1365-2842.1983.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 102.Morneburg T., Dohla S., Wichmann M., Proschel P. Afferent sensory mechanisms involved in jaw gape-related muscle activation in unilateral biting. Clin Oral Investig. 2014;18:883–890. doi: 10.1007/s00784-013-1024-1. [DOI] [PubMed] [Google Scholar]
- 103.Wycherley A.S., Helliwell P.S., Bird H.A. A novel device for the measurement of proprioception in the hand. Rheumatology. 2005;44:638–641. doi: 10.1093/rheumatology/keh568. [DOI] [PubMed] [Google Scholar]
- 104.Refshauge K.M., Chan R., Taylor J.L., McCloskey D.I. Detection of movements imposed on human hip, knee, ankle and toe joints. J Physiol (London) 1995;488:231–241. doi: 10.1113/jphysiol.1995.sp020961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cordo P.J., Horn J.L., Küenster D., Cherry A., Bratt A., Gurfinkel V. Contributions of skin and muscle afferent input to movement sense in the human hand. J Neurophysiol. 2011;105:1879–1888. doi: 10.1152/jn.00201.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Nagai T., Sell T.C., Abt J.P., Lephart S.M. Reliability, precision, and gender differences in knee internal/external rotation proprioception measurements. Phys Ther Sport. 2012;13:233–237. doi: 10.1016/j.ptsp.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 107.Gibson J.J. George Allen & Unwin Ltd.; London: 1966. The senses considered as perceptual systems. [Google Scholar]
- 108.Laszlo J.I. Motor control and learning: how far do the experimental tasks restrict our theoretical insight? In: Summers J.J., editor. Approaches to the study of motor control and learning. Elsevier; Amsterdam: 1992. pp. 47–79. [Google Scholar]
- 109.Ashton-Miller J.A. Proprioceptive thresholds at the ankle: implications for the prevention of ligament injury. In: Lephart S.M., Fu F.H., editors. Proprioception and neuromuscular control in joint stability. Human Kinetics; Champaign, IL: 2000. pp. 279–289. [Google Scholar]
- 110.Taylor A., Sluckin W., Davies D.R., Reason J.T., Thomson R., Colman A.M. Penguin Books; Harmondsworth: 1982. Introducing psychology. [Google Scholar]
- 111.Gibson J.J. Lawrence Erlbaum Associates; New Jersey, NJ: 1979. The ecological approach to visual perception. [Google Scholar]
- 112.Gandevia S.C., McCloskey D.I., Burke D. Kinaesthetic signals and muscle contraction. Trends Neurosci. 1992;15:62–65. doi: 10.1016/0166-2236(92)90028-7. [DOI] [PubMed] [Google Scholar]
- 113.Zazulak B.T., Hewett T.E., Reeves N.P., Goldberg B., Cholewicki J. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med. 2007;35:368–373. doi: 10.1177/0363546506297909. [DOI] [PubMed] [Google Scholar]
- 114.Kurian G., Sharma N.K., Santhakumari K. Left-arm dominance in active positioning. Percept Mot Skills. 1989;68:1312–1314. doi: 10.2466/pms.1989.68.3c.1312. [DOI] [PubMed] [Google Scholar]
- 115.Macfadyen N., Maher C.G., Adams R. Number of sampling movements and manual stiffness judgments. J Manipulative Physiol Ther. 1998;21:604–610. [PubMed] [Google Scholar]
- 116.Bullock-Saxton J.E., Wong W.J., Hogan N. The influence of age on weight-bearing joint reposition sense of the knee. Exp Brain Res. 2001;136:400–406. doi: 10.1007/s002210000595. [DOI] [PubMed] [Google Scholar]
- 117.Adamo D.E., Alexander N.B., Brown S.H. The influence of age and physical activity on upper limb proprioceptive ability. J Aging Phys Act. 2009;17:272–293. doi: 10.1123/japa.17.3.272. [DOI] [PubMed] [Google Scholar]
- 118.Piriyaprasarth P., Morris M.E., Delany C., Winter A., Finch S. Trials needed to assess knee proprioception following stroke. Physiother Res Int. 2009;14:6–16. doi: 10.1002/pri.405. [DOI] [PubMed] [Google Scholar]
- 119.Clark F.J., Larwood K.J., Davis M.E., Deffenbacher K.A. A metric for assessing acuity in positioning joints and limbs. Exp Brain Res. 1995;107:73–79. doi: 10.1007/BF00228018. [DOI] [PubMed] [Google Scholar]
- 120.Faisal A.A., Selen L.P.J., Wolpert D.M. Noise in the nervous system. Nat Rev Neurosci. 2008;9:292–303. doi: 10.1038/nrn2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Swets J.A., Dawes R.M., Monahan J. Better decisions through science. Sci Am. 2000;283:82–87. doi: 10.1038/scientificamerican1000-82. [DOI] [PubMed] [Google Scholar]
- 122.Swets J.A. Lawrence Erlbaum Associates, Inc.; Hillsdale, NJ: 1996. Signal detection theory and ROC analysis in psychology and diagnostics: collected papers. [Google Scholar]
- 123.Swets J.A., editor. Tulips to thresholds: counterpart careers of the author and signal detection theory. Peninsula Publishing; Los Altos Hills, CA: 2010. [Google Scholar]
- 124.McNicol D. Routledge; New York, NY: 2004. A primer of signal detection theory; pp. 24–105. [Google Scholar]
- 125.Rosker J.S. Kinaesthesia and methods for its assessment. Sport Sci Rev. 2010;19:165–208. [Google Scholar]
- 126.Sanes J.N., Shadmehr R. Sense of muscular effort and somesthetic afferent information in humans. Can J Physiol Pharmacol. 1995;73:223–233. doi: 10.1139/y95-033. [DOI] [PubMed] [Google Scholar]
- 127.Smirmaul Bde. P. Sense of effort and other unpleasant sensations during exercise: clarifying concepts and mechanisms. Br J Sports Med. 2012;46:308–311. doi: 10.1136/bjsm.2010.071407. [DOI] [PubMed] [Google Scholar]
- 128.Lowrey C.R., Strzalkowski N.D., Bent L.R. Skin sensory information from the dorsum of the foot and ankle is necessary for kinesthesia at the ankle joint. Neurosci Lett. 2010;485:6–10. doi: 10.1016/j.neulet.2010.08.033. [DOI] [PubMed] [Google Scholar]
- 129.Weerakkody N.S., Mahns D.A., Taylor J.L., Gandevia S.C. Impairment of human proprioception by high-frequency cutaneous vibration. J Physiol (London) 2007;581:971–980. doi: 10.1113/jphysiol.2006.126854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Willems T.M., Witvrouw E., Delbaere K., Philippaerts R., De Bourdeaudhuij I., De Clercq D. Intrinsic risk factors for inversion ankle sprains in females: a prospective study. Scand J Med Sci Sports. 2005;15:336–345. doi: 10.1111/j.1600-0838.2004.00428.x. [DOI] [PubMed] [Google Scholar]
- 131.Beynnon B.D., Ryder S.H., Konradsen L., Johnson R.J., Johnson K., Renstrom P.A. The effect of anterior cruciate ligament trauma and bracing on knee proprioception. Am J Sports Med. 1999;27:150–155. doi: 10.1177/03635465990270020601. [DOI] [PubMed] [Google Scholar]
- 132.Lephart S.M., Warner J.J., Borsa P.A., Fu F.H. Proprioception of the shoulder joint in healthy, unstable, and surgically repaired shoulders. J Shoulder Elbow Surg. 1994;3:371–380. doi: 10.1016/S1058-2746(09)80022-0. [DOI] [PubMed] [Google Scholar]
- 133.Willems T., Witvrouw E., Verstuyft J., Vaes P., De Clercq D. Proprioception and muscle strength in subjects with a history of ankle sprains and chronic instability. J Athl Train. 2002;37:487–493. [PMC free article] [PubMed] [Google Scholar]
- 134.Larsen R., Lund H., Christensen R., Rogind H., Danneskiold-Samsoe B., Bliddal H. Effect of static stretching of quadriceps and hamstring muscles on knee joint position sense. Br J Sports Med. 2005;39:43–46. doi: 10.1136/bjsm.2003.011056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Janwantanakul P., Magarey M.E., Jones M.A., Dansie B.R. Variation in shoulder position sense at mid and extreme range of motion. Arch Phys Med Rehabil. 2001;82:840–844. doi: 10.1053/apmr.2001.21865. [DOI] [PubMed] [Google Scholar]
- 136.Symes M., Waddington G., Adams R. Depth of ankle inversion and discrimination of foot positions. Percept Mot Skills. 2010;111:475–484. doi: 10.2466/06.25.26.PMS.111.5.475-484. [DOI] [PubMed] [Google Scholar]