Abstract
Background
Bipolar disorder (BD) is characterized by recurrent (hypo)manic and depressive episodes, alternating with euthymic states in which patients are relatively symptom free. Besides clinical recovery, it is important to also strive for improvement of mental well-being and personal recovery. One prominent field focussing on the improvement of well-being is positive psychology. However, studies assessing the effects of positive psychology or personal recovery interventions for people with BD are scarce and have used weak methodological designs. The study described in this protocol article aims to assess the effectiveness of a multicomponent positive psychology intervention (“Living well with bipolar disorder”) adjusted for people with BD in the euthymic phase to improve well-being and personal recovery.
Method
The study concerns a pragmatic randomized multicenter trial. The principle objective of the study is to assess whether the positive psychology intervention offered to BD patients in remission in addition to usual care (CAU) is more effective than CAU. The study will include 112 participants randomized to either the experimental condition receiving the intervention in addition to CAU or the control condition receiving CAU. The study population are patients with BD I or II in the euthymic phase.
The inclusion criteria are 1) diagnosis of BD I or BD II, 2) between the ages of 18–65, 3) four or more supportive sessions in the last year, and 4) only residual depressive or manic symptoms. Patients are excluded if they are in a depressive or manic episode, have current addiction problems or have optimal levels of well-being. Measurements take place at baseline, post-intervention and follow-up 6 and 12 months from baseline. Outcomes of measures include positive well-being, personal recovery, psychopathology, self-compassion, positive relationships, dampening of positive affect and relapse.
Discussion
The outlined study will be the first RCT examining the effects of a multicomponent positive psychology intervention for patients with bipolar disorder. Several limitations, including generalizability of the results and possible attrition issues, are discussed in advance.
Trial registration
This study has been registered in the Netherlands Trial Register (NTR6729) on 12 October 2017.
Electronic supplementary material
The online version of this article (10.1186/s12888-018-1916-3) contains supplementary material, which is available to authorized users.
Keywords: Positive psychology, Well-being, Flourishing, Personal recovery, Bipolar disorder, Intervention, Randomized controlled trial, RCT, Effect, Effectiveness
Background
Bipolar disorder (BD) is a severe mood disorder and is characterized by recurrent (hypo)manic and depressive episodes, alternating with euthymic phases in which patients are relatively symptom free [1, 2]. BD is subclassified as bipolar I and bipolar II disorder. In the latter, patients solely experience hypomanic episodes but never a full manic episode [3, 4]. Prevalence estimates from the Netherlands reveal a lifetime prevalence of 1.3% and 12-month prevalence of 0.8% for BD I and II [5]. The economic burden in 2009 was estimated at 151 billion dollars per year in the United States [6]. BD is associated with decreased quality of life [7], negative social consequences, such as a disturbed social life and disrupted family interactions [8], issues related to work-performance and productivity [9, 10] and high caregiver burden [11, 12]. Current treatment for euthymic BD patients in the Netherlands includes pharmacotherapy, supportive treatment, psycho education and enhancement of self-management skills, and psychotherapy if indicated [13, 14].
In addition to current symptom-focused treatment, it becomes increasingly important to also focus on personal recovery [15–17]. Leamy, Bird, Le Boutillier, Williams and Slade [18] created a conceptual framework for personal recovery in mental health, containing five processes of personal recovery: connectedness, hope and optimism about the future, identity, meaning in life and empowerment (giving the acronym CHIME) as important factors for personal recovery [18]. Anthony (1993) operationalizes personal recovery in the context of psychopathology and describes it as the ability to live a meaningful, hopeful and contributing life, even in the presence of mental illness [19]. Similarly, Keyes [20] defines mental health recovery as the presence of well-being and not merely the absence of mental illness. Well-being, in turn, includes subjective well-being (i.e. positive affect and life-satisfaction), psychological well-being (i.e. meaning, goals in life, mastery, positive relationships) and social well-being (i.e. contributing to society) [20].
Personal recovery and well-being are particularly important in BD for several reasons. Residual subthreshold symptoms often persist in the interval between mood episodes [21–23]. Moreover, up to 35% of BD patients do not completely recover from a depressive or manic episode [24], which is an important risk factor for relapse [17]. Research also indicates that improvement of well-being protects against the recurrence of mental illness [25–27]. Patients with serious mental illness, such as BD also express dissatisfaction with current primary targets of treatment and instead argue for the importance of personal recovery outcomes [28, 29].
One prominent field of psychology focussing on the improvement of well-being and positive capacities is positive psychology [30]. Positive psychology interventions focus on the enhancement of positive feelings, behaviours, or cognitions and aim to improve well-being [31]. The key processes and goals of positive psychology are similar and central to personal recovery [15, 32] making positive psychology interventions potentially useful for improving both well-being and personal recovery in people with mental illness. The effect of positive psychology interventions has been shown in meta-analyses for both general and clinical populations [31, 33].
To date, however, no study has been conducted assessing the effect of positive psychology interventions for the treatment of people with BD and only a few studies investigated the effect of interventions focussing on the improvement of personal recovery. Deckersbach, Hölzel, Eisner, Stange, Peckham, Dougherty, Rauch, Lazar and Nierenberg [34] report on a small uncontrolled clinical trial with 12 euthymic participants diagnosed with BD using Mindfulness-Based Cognitive Therapy (CBT). Analysis from pre- to follow-up indicated significant moderate to large improvements in outcomes of depressive symptoms (Cohen’s d = .75), positive affect and aspects of well-being. Eisner, Eddie, Harley, Jacobo, Nierenberg and Deckersbach [35] conducted a proof-of-concept pilot study with 37 participants with BD who did not have a current major depressive, manic or mixed episode. Significant large improvements were obtained from baseline to post-treatment in psychological well-being, emotion regulation, and emotion reactivity. Finally, Jones, Smith, Mulligan, Lobban, Law, Dunn, Welford, Kelly, Mulligan and Morrison [36] investigated the effectiveness of recovery-focused CBT in a randomized controlled pilot trial (n = 67) with care as usual as control. Personal recovery significantly improved from baseline to 6 and 12 months follow-up (d = .62) in comparison with a control group receiving treatment as usual. Although no significant effects were obtained in average mood symptoms, patients in the recovery-focused CBT group showed significantly longer time to relapse into depression or mania over a 15-month period compared to patients only receiving care as usual. For example, 32 patients relapsed to either depression or mania (20 CAU v. 12 recovery-focused CBT) and median survival times were longer for recovery-focused CBT (56 weeks) compared to CAU (18 weeks).
In summary, no studies exist investigating the effectiveness of positive psychology interventions for BD patients. Furthermore, studies examining the effect of interventions aimed to enhance personal recovery or well-being for patients with BD are scarce and mostly used underpowered and weak methodological designs. For this reason, we aim to develop, implement and thoroughly investigate the effects of a multicomponent positive psychology intervention for the improvement of well-being and personal recovery for people with BD in an adequately powered randomized controlled trial. This will be the first study specifically evaluating a positive psychology intervention for patients with BD and will use a more sophisticated methodological design than studies before.
The primary objective is to evaluate the effectiveness of an eight-week multicomponent intervention “Living well with bipolar disorder” added to usual care (CAU) in BD patients in the euthymic phase. Primary outcome is the short and long term improvement of well-being and personal recovery. Secondly, the study aims to investigate whether the intervention in addition to CAU is more effective in improving social participation, and in improving depressive, manic, and anxiety symptoms. Thirdly, we will explore possible working mechanisms for intervention effects, including positive emotions, self-compassion, positive relationships and dampening of positive affect. Fourthly, the study aims to assess whether the intervention combined with CAU is more effective than CAU in reducing recurrence of depressive and (hypo)manic episodes in patients with BD in the long term. Finally, we aim to evaluate the cost-effectiveness of the intervention in addition to CAU for the treatment of euthymic patients with BD compared to CAU.
Method
Study design
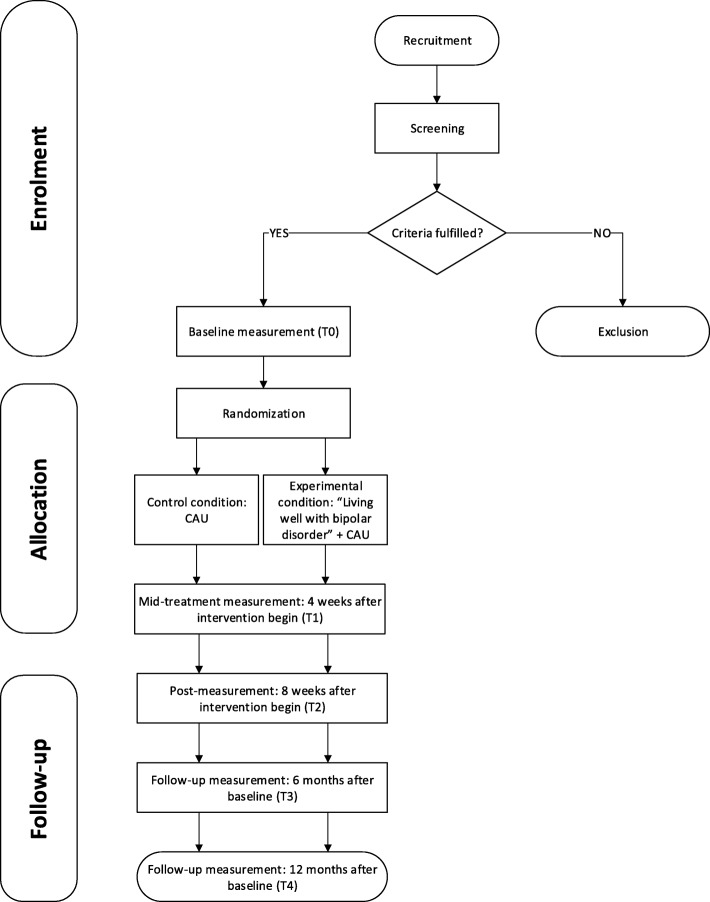
A pragmatic, parallel-group randomized non-blinded multicenter trial is used to investigate the effectiveness of a multicomponent positive psychology intervention to improve well-being and personal recovery in patients with BD. Since the outcome in BD I and BD II disorder may be different, the sample will be stratified accordingly. Patients in the experimental condition receive “Living well with bipolar disorder” in addition to CAU. Participants in the control condition receive CAU only. Both participants in the control and experimental condition receive CAU according to the Dutch multidisciplinary guideline for BD [13], consisting mainly of self-monitoring of mood and supportive group sessions focusing on functional problems, and psychopharmacotherapy. The study duration is 12 months for each individual and includes five measurement points. Immediately prior to the start of the intervention a baseline measurement is completed (T0), 4 weeks after the start of the intervention a mid-treatment measurement takes place (T1) and immediately following the intervention a post measurement will be conducted (T2). In addition, two follow-up measures will be conducted, 6 months (T3) and 12 months after baseline (T4). Figure 1 shows the intended flow of participants (Additional file 1).
Fig. 1.
Participant timeline
Participants, eligibility and screening
In order to be eligible to participate in this study, participants must meet the following inclusion criteria: (1) diagnosis of BD I or BD II (assessed using the MINI-international neuropsychiatric interview [37]); (2) between the ages of 18–65; (3) four or more supportive sessions in the previous year with a psychiatrist or psychologist; and (4) presence of residual subsyndromal symptoms. Participants are included if they score between 2 (minimal symptoms) and 4 (moderate symptoms) for depressive symptoms and between 2 (minimal symptoms) and 3 (mild symptoms) for manic symptoms on the Clinical Global Impression Scale – Bipolar (CGI-BP). Exclusion criteria are: (1) currently in a depressive or (hypo)manic episode; (2) currently in treatment for addiction problems, or (3) having already optimal levels of well-being. Participants are assumed to have an optimal level of well-being if they score 4 or 5 on at least one item of the emotional well-being subscale together with a score of 4 or 5 on at least 6 of the 11 remaining items of the Mental Health Continuum-Short Form (MHC-SF; [20]).
Randomization and treatment allocation
Randomization will be centrally conducted by the principal investigator using stratified (by center) block randomisation. For this purpose, randomization lists will be generated beforehand (one list for each participating treatment center) with an online tool (https://sealedenvelope.com/). The lists contain a random sequence of treatment allocations (i.e., participants are either allocated to the intervention or control condition according to the corresponding record) and are divided in blocks of allocations (20 allocations per block). By using blocks of allocations, 20 participants can be allocated to either the intervention or control condition after which the following block is used. This ensures that the group sessions in each center can start as soon as sufficient participants are randomized. The first participant included in the study is allocated according to the first record on the list, the second participant according to the second record on the list and so forth.
Recruitment
Participants will be recruited from at least four mental health centers with six locations in the east and west of the Netherlands and will start in September 2018. Possible participants are informed by means of flyers and posters distributed in these centers. In order to include sufficient participants, mental health professionals will play an active role, by informing potentially eligible patients about the study and handing out information folders.
Intervention
We will adapt the positive psychology intervention “This is your life” [38, 39] for patients with BD in the euthymic phase aiming to enhance personal recovery and well-being. Originally developed as a self-help book, the intervention is primarily based on the well-being theory of Seligman [40] and Ryff’s theory of psychological well-being [41] and comprises different modules focusing on six key components: positive emotions; discovering and using strengths; optimism and hope; self-compassion; resilience and post-traumatic growth and positive relations. Each module contains psycho-education and a range of different positive psychology exercises, such as the “three good things exercise” [33] or the “best possible self” [42]. All modules include proven strategies for improving well-being. In a recent randomized controlled trial, the intervention as guided self-help with email support revealed moderate to large effects on well-being (d = 0.66) and effectively reduced subclinical symptoms of anxiety (d = 0.63) and depression (d = 0.43) in a non-clinical sample [39].
Intervention adjustments for euthymic BD patients
Since “This is your life” was not specifically developed for individuals with BD, we decided to customize the intervention content and delivery to the needs of this target group. The adjusted intervention is called “Living well with bipolar disorder”. We changed the mode of treatment delivery from individual self-help to group meetings (8–10 people per group), including eight sessions of 2 h conducted by a specially trained therapist. This setup is believed to give participants the possibility to share experiences with fellow patients and benefit from the presence of other group members.
Each week, a key positive psychology component will be covered and corresponding exercises will be introduced. Participants are also encouraged to keep training with those exercises at home (for 15–30 min per day). All intervention participants receive the self-help book “This is your life” [43], since several parts of the modules refer to chapters or exercises in the book. The adapted intervention consists of eight different modules covering different topics, such as positive emotions, positive relationships or personal goals. Homework differs depending on the module, but every week participants are encouraged to keep training with the exercises at home. Experiences with the homework is discussed at the beginning of each next session and possible obstacles or other benefits can be shared with the therapist and other group members. In case the module contains a collective exercise, a short debriefing session will take place immediately after the exercise, to discuss experienced benefits or difficulties. Every module contains a short break of 15 min. Every session is finished by a short conclusion in which the therapist summarizes the session and where uncertainties can be broached and questions can be asked.
In spring 2017, a formative user evaluation of “This is your life” was carried out to evaluate the original intervention contents. Five individuals with BD read and practiced a selection of the original exercises and rated them on a scale from 1 (not at all) to 5 (extremely), representing the relevance and usability of the exercises. Results of this group were used to further adapt and tailor the intervention to the needs of individuals with BD by taking into account the ratings of exercises, preferences of the patients and also their critical responses.
For several reasons, we decided to put additional emphasis on fostering self-compassion skills by including two sessions of self-compassion. Research on emotion regulation [44–46] emphasizes the importance of disturbed positive emotion regulation (i.e., how an individual reacts to positive emotions) for the onset, maintenance and illness course of BD [47]. Suppression of positive emotions is heightened among BD patients and predicts depressive and also manic symptoms [48, 49]. Additionally, negative thinking about high moods (e.g. “I will lose control if I get excited”) is also elevated in individuals with BD, compared with nonclinical controls [50–52], individuals with remitted unipolar depression [50, 52] and individuals who have had hypomanic experiences, but no psychological disorder [50] and predicts mood symptoms in BD over the period of 1 month [53] and 6 months [49]. Studies show that self-compassion is positively related with adaptive emotion regulation processes, including acceptance and positive reappraisal and negatively correlated with maladaptive strategies, such as thought suppression and rumination [54–56]. An overview of the intervention contents can be found in Table 1.
Table 1.
Content of “Living well with bipolar disorder” and corresponding example exercises adapted for euthymic BD patients
| Module | Contents | Example (home) exercises |
|---|---|---|
| 1. Introduction & compassion | ▪ Participants are welcomed and become familiar with each other ▪ Psychoeducation about personal recovery and compassion ▪ Collective compassion exercise ▪ Homework: Fill in handout about personal goals and optimism |
▪ Wish yourself something good: be mindful and identify needs and use your inner voice to repeat your compassionate wish [86]. ▪ Common humanity: Realize that negative feelings and experiences are universal [87, 88]. |
| 2. Personal goals & optimism | ▪ Based on the handouts, participants talk about personal goals and wishes and specify personal goals in the group ▪ Individually adjusting personal goals ▪ Collective optimism exercise ▪ Reading and discussing letter from an experienced person with BD ▪ Homework: Working on personal goals, writing a letter from the future |
▪ Imagine your best possible self: Visualize yourself in a future where everything has turned out in the most optimal way [42, 89]. ▪ Letter from the future: write yourself a letter from a future perspective |
| 3. Positive emotions | ▪ Read out letter from the future ▪ Psychoeducation about positive emotions ▪ Collective positive emotions exercises ▪ Homework: Taking a photo of a positive moment or experience, working on personal goals |
▪ Three good things: Think about three good things that went well today and savor these moments [90]. ▪ Expressing gratitude: identify what you are grateful for in the context of your illness and share those experiences [91]. |
| 4. Coping with fear of relapse | ▪ Sharing photos of positive experiences and talking about the photos ▪ Talking about participant’s fears, how fear is experienced and internal barriers ▪ Psychoeducation about fear and (un)healthy emotion regulation strategies ▪ Collective exercises on how to efficiently cope with fear ▪ Homework: Do something you find exciting, perform personal strengths exercise, completing mid-treatment measurement |
▪ Learn to tolerate and accept fear as important part of life and learn to regulate positive mood and gain a more open view towards them [43]. ▪ Compassionate coping with inner fear: learn to be compassionate towards yourself, your emotions and your negative experiences [86]. |
| 5. Personal strengths | ▪ Identifying strengths ▪ Psychoeducation about personal strengths ▪ Personal goals and strengths: which strengths can be used to achieve personal goals? ▪ Homework: Keep training with exercises, record possible benefits and barriers while performing the exercises |
▪ Identifying strengths: Describe an activity you enjoy to someone else and he/she names strengths deriving from this activity. ▪ Top 5 strengths: Choose your top 5 strengths that give you energy and pleasure [92, 93]. |
| 6. Positive relationships | ▪ Participants name skills they gathered in the course of the intervention so far and described one example from the last week ▪ Psychoeducation about positive relationships ▪ Participants describe a relationship they want to reinforce positively ▪ Collective positive relationship exercises ▪ Homework: Keep training with positive relationship exercises |
▪ Acts of kindness: Performing unexpected acts of kindness for someone else [94]. ▪ Active-constructive responding: Respond positively to good news shared by someone else. Use active communication skills [95, 96]. ▪ Expressing gratitude [91]. |
| 7. Compassion | ▪ Psychoeducation about emotional systems and evolutionary background ▪ Collective exercises mindfulness and compassion ▪ Coping with thoughts of inferiority and self-critique ▪ Homework: Writing a response to the letter from the second session, fill in questionnaires for post-measurement |
▪ Develop a compassionate inner voice: Write about situation in the past week where you showed self-compassion [86]. ▪ Grandma exercise: Imagine a person you feel comfortable with. Concentrate on how it feels to be together with this person and savor this moment [43]. |
| 8. Conclusion | ▪ Talking about results of the questionnaires and figuring out which aspects are going well and which should receive some extra attention in the next weeks ▪ Read out response to the letter from the second sessions ▪ Participants thank each other |
▪ Not applicable. |
Control group
Participants in the comparison group will receive CAU for BD as described in the Dutch multi-disciplinary guideline for bipolar disorder [13] which comprises supportive sessions with a psychologist or psychiatric nurse and maintenance pharmacological treatment by a psychiatrist. Most patients receive 2–12 supportive sessions per year. CAU includes many psychoeducational elements that have the following aims: to give patients information about the illness in the context of the patients’ life-history, to learn to identify early warning signals and prodromal symptoms, to develop and implement strategies to cope with prodromal symptoms, and to develop plans for acute crisis and stabilizing one’s mood. For some patients, CAU may additionally include psychotherapeutic treatments such as cognitive behavioral therapy and interpersonal therapy. For all patients, current CAU does not primarily focus on personal recovery in terms of emotional and psychological well-being (i.e. meaning, purpose in life, positive relationships).
Therapists training and treatment manual
Therapists carrying out the intervention will receive a one-day workshop covering the central ideas of “Living well with bipolar disorder”, including background, goals and possible exercises of the intervention. A treatment manual will be prepared to guarantee a standardized execution of the intervention. The manual includes explanations on each module and also on corresponding exercises. Short session handouts (1–2 pages) will be developed for patients participating in the intervention, explaining and summarizing the topics of each module and will include affiliated exercises and can be used to further exercise at home.
Study procedure
Initial screening for participation will be performed by therapists working at the treatment centers. To assess symptom severity of possible participants, the Clinical Global Impression Scale – Bipolar (CGI-BP) is used. After possible participants sign the informed consent, the principal investigator contacts the patient and agrees on a time and date to conduct the additional screening. To verify the diagnosis of BD, the MINI international neuropsychiatric interview [37, 57] is used and to assess well-being, participants are asked to complete the Mental Health Continuum – Short Form (MHC-SF) [58]. Eligible participants are then asked to complete the first test battery at baseline. Since the MHC-SF has already been completed for screening reasons before, participants are not asked to complete it again at baseline. Baseline measurements should take approximately 40 min to complete. Afterwards, allocation of participants to the intervention or control group takes place.
The first intervention group will start approximately in fall 2018 and the last group will finish in fall 2019. Four weeks after the intervention begins (T1) and after the intervention has finished (T2), participants in the intervention and control condition are asked to fill out a test battery again. Six (T3) and 12 (T4) months after baseline, participants in the experimental and control group will be asked to complete the follow-up measures. We assume that completing the test battery takes approximately 35 min on average at each measurement point. At T4, participants will be approached for a semi-structured telephone interview with the goal to retrospectively assess relapse into mood episodes in the past 9 months. To perform the interviews, a guideline will be prepared and the interviews will be conducted by student assistants according to a fixed scheme. The trained student assistants are blind to the treatment condition of the participants. One interview will take approximately 30 min.
Study measures
Almost all data being gathered during the trial are self-reported data that will be collected via an online survey program (https://www.qualtrics.com). In addition, one semi-structured telephone interview will be conducted 12 months after baseline to assess relapse. Participants will be asked to report demographical data including gender, age, marital and employment status, ethnicity and education, as well as the information about the past course of BD, at baseline. The primary outcome is well-being and secondary outcomes include personal recovery, social role participation and symptoms of depression, mania and anxiety. Additionally, processes of positive emotions, self-compassion and positive relationships are assessed and economic outcomes are used to calculate the cost-effectivness. An overview of the study measures at the different time points can be found in Table 2.
Table 2.
Overview of study parameters and measurement points
| Questionnaire | Outcome | Screening | T0 | T1 | T2 | T3 | T4 |
|---|---|---|---|---|---|---|---|
| Pre-test | Mid-treatmenta | Post-test | Follow-upb | Follow-upc | |||
| CGI-BPd | Global illness severity | X | |||||
| MINI | Diagnosis BD | X | |||||
| MHC-SF | Well-being | X | X | X | X | X | X |
| QPR | Personal recovery | X | X | X | X | ||
| s-SRPQ | Social participation | X | X | X | X | ||
| QIDS-SR | Depressive symptoms | X | X | X | X | ||
| ASRM | Manic symptoms | X | X | X | X | ||
| HADS-A | Anxiety symptoms | X | X | X | X | ||
| PANAS | Positive emotions | X | X | X | |||
| SCS-SF | Self-compassion | X | X | X | |||
| SPWB | Positive relationships | X | X | X | |||
| RPA | Dampening of positive affect | X | X | X | |||
| Telephone interviews | Relapse | X | |||||
| EQ-5D-5 L | Quality of Life | X | X | ||||
| TiC-P | Costs associated with psychiatric illness | X | X | ||||
| Socio- demographics | Gender, age, education, marital status, living situation, ethnicity | X |
a4 weeks after intervention begin
b6 months after baseline
c12 months after baseline
dclinician reported
Global illness severity
To screen for the presence of depressive and (hypo)manic symptoms and determine eligibility of possible participants, the Clinical Global Impression – Bipolar (CGI-BP; [59]) scale will be used. This scale comprises three different measures, including severity of depressive and (hypo)manic symptoms, change from preceding phases and change from worst phase of illness. For this study, only the measure assessing the severity of symptoms will be used ranging from 1 (normal, not ill) to 7 (very severely ill). The CGI-BP showed excellent interrater reliability in prior studies [59].
Well-being
The Mental Health Continuum – Short Form (MHC-SF) is a comprehensive well-validated measure of well-being [58]. The MHC-SF measures three dimensions of well-being: 1) emotional well-being (three items), defined in terms of the presence of positive feelings, the absence of negative feelings and satisfaction with life; 2) psychological well-being (six items), defined in terms of positive functioning in individual life in terms of e.g. self-acceptance, personal goals, positive relationships, and environmental mastery; 3) social well-being (five items), defined in terms of positive functioning in social life in terms of e.g. social integration and social contribution. Participants rate the frequency of feelings in the last week. A total score can be created by summing all 14 items, where higher scores indicate better positive well-being. The Dutch version of the MHC-SF showed high internal consistency for total scores (α = 0.89) and for the subscales emotional (α = 0.83) and psychological well-being (α = 0.83) and adequate reliability for the subscale social well-being (α = 0.74) and correlates well with corresponding aspects of well-being and functioning, showing convergent validity [58].
Personal recovery
To comprehensively assess personal recovery, the 15-item version of the Questionnaire about the Process of Recovery is used (QPR; [60, 61]).The scale aims to assess personal recovery in the last 7 days (e.g. “I feel better about myself” or “I can actively engage with life”), with items being scored on a 5-point Likert scale, ranging from 0 to (disagree strongly) to 4 (agree strongly) and higher scores being indicative of recovery. The internal consistency of the 15-item version has been found to be high (α = 0.89) in a sample of psychotic patients [62] and in a group of individuals with a schizophrenia spectrum diagnosis (α = 0.93) [61]. For this study, the QPR has been translated into Dutch via forward and backward translation.
Social role participation
The Social Role Participation Questionnaire (SRPQ; [63]) assesses social role participation. For this study, the short version of the questionnaire (s-SRPQ; [64]) will be used, which consists of 12 items, measuring the influence of (psychological) health in the past on six social roles (e.g. intimate relationship or employment) along two dimensions: (1) satisfaction with role performance and (2) experienced physical / psychological difficulty. Items are scored on a 5-point Likert Scale, reaching from 0 (not satisfied at all / no difficulties at all) to 4 (very much satisfied / not possible), with higher scores indicating more satisfaction respectively more experienced difficulties with a social role. The psychometric qualities of the Dutch s-SRPQ were found to be good for both subscales (α = 0.86) [64].
Depressive symptoms
The self-report version of the Quick Inventory of Depressive Symptomatology (QIDS-SR) [65, 66] assesses depressive symptoms in the past on 16 items. The scale requires individuals to rate different depression symptoms, such as sad mood, concentration, suicidal ideation, general interest, energy/fatigue, sleep, appetite and weight. Items are scored on a 4-point Likert Scale with different answering categories. A total score can be obtained by summing all items, with higher scores indicating more depressive symptomatology. The QIDS-SR has shown to be internally consistent (α = 0.86) [65].
Manic symptoms
Current manic symptoms are measured using the Altman Self-Rating Mania Scale (ASRM) [67]. The scale consists of five statements that represent different manic symptoms, including feeling happier, self-confident and talkative than normal. All five items are rated on a 5-point Likert scale with different answering categories. A total score can be obtained by summing all items, with higher scores indicating more manic symptomatology. The ASRM has high test-retest reliability [67], has been shown to be sensitive to changes of clinical states [68] and to predict related measures in non-clinical student samples [69].
Anxiety symptoms
The anxiety subscale of the Hospital Anxiety and Depression Scale (HADS-A; [70]) is used to assess anxious symptomatology. The HADS-A aims to measure anxiety symptoms in 7 items. Participants rate the frequency of symptoms (e.g. “Worrying thoughts go through my mind”) on a scale ranging from 0 (“not at all”) to 3 (“very often”) and higher scores indicate higher anxiety symptoms. The Dutch version of the HADS-A [71] has been shown good internal consistency in a sample from the general population (α = 0.84) and in a sample of psychiatric outpatients (α = 0.81).
Positive emotions
The Positive and Negative Affect Schedule (PANAS) [72] measures current emotions on two different dimensions: (1) positive and (2) negative affect and includes 20 items describing emotional states (e.g. “active” or “anxious”). Participants can score those states on a 5-point Likert scale, representing the extent to which they experience an affect at this moment or have experienced in the past week, reaching from 1 (very slightly or not at all) to 5 (extremely). The scores can be summed up to gain scores for positive and negative affect respectively, with higher scores indicating higher affectivity. For this study, the Dutch version of the PANAS and only the positive affect subscale will be used, which showed acceptable reliability (α = .79) [73].
Self-compassion
The Self-Compassion Scale – Short Form (SCS-SF) [74, 75] measures the process of self-compassion on six dimensions: (1) self-kindness, (2) self-judgment, (3) common humanity, (4) isolation, (5) mindfulness and (6) over-identification and contains 12 items (e.g., “When I fail at something important to me I become consumed by feelings of inadequacy”). Each dimension is assessed by two items, which are scored on a 7-point response scale ranging from 1 (almost never) to 7 (almost always), representing the extent to which an individual experiences certain aspects of self-compassion. Higher scores indicate an increased degree of self-compassion. Reliability of the total Dutch SCS-SF was shown to be good (α = .87). Solely total scores of the SCS-SF will be used for further analyses, since the psychometric properties of the subscales were questionable [74].
Positive relationships
The process of positive relationships is assessed using the Scales of Psychological Well-Being (SPWB; [76]), which assesses psychological well-being on six different dimensions (e.g. environmental mastery, self-acceptance). For this study, the subscale positive relations will be used measuring the extent to which an individual experiences meaningful intrapersonal relationships with other people (e.g. “People would describe me as a giving person, willing to share my time with others”). Items are scored on a scale ranging from 1 (strongly disagree) to 6 (strongly agree) with higher scores indicating more positive relations with others. Different versions of the SPWB exist within literature, differing in number of items per subscale (reaching from 3 items to 20 items per subscale). For feasibility reasons and since the short version of this subscale (3-items) showed unacceptable internal consistency (α = .44–.52), we decided to use the 9-item version of the positive relationship subscale, which showed acceptable internal consistency in two previous studies (α = .77) in samples of psychology students and professionals from a divers occupation background [77].
Dampening of positive affect
To assess the process of dampening the Responses to Positive Affect Questionnaire (RPA; [78, 79]) is used, which consists of 17 items and measures cognitive responses to positive affective states. Respondents rate the items on a 4-point Likert scale, ranging from 1 (almost never) to 4 (almost always). For this study, only the subscale dampening is used (e.g., “I don’t deserve this”), which assesses the tendency to cognitively avoid or suppress positive emotions (eight items). Scores of the scales are calculated by summing up the scores on the items. The Dutch version, which is used in this study, showed satisfactory internal consistency (α = 0.80) for the dampening subscale [78].
Relapse
Semi-structured telephone interviews will be performed with people of both the intervention and control group. Goal of the interviews is to retrospectively illustrate the mood development in the time after the intervention and to capture depressive or manic mood swings with the Life Chart Method [80]. The interviews allow to graphically score severity of mood swings, the time they appeared (i.e., in which month) and which type of mood swings appeared (e.g., rapid cycling). The interview has been applied successfully in a previous study to measure relapse [14].
Economic measures
Quality of life
The EQ-5D-5 L [81] is a quality of life measure consisting of five items representing five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/ depression). For each dimension/item, individuals rate the extent of problems ranging from ‘no problems’ to ‘extreme problems’.
Costs associated with psychiatric illness
The Trimbos and iMTA questionnaire on costs associated with psychiatric illness (TiC-P) [82] is a measure of health care utilization and production loss in patients with psychiatric disorders. Items are generic and not related to a specific psychiatric disease. A first part of the TiC-P includes 9 structured no/yes items on medical consumption (e.g. contact with specific mental health care providers). A second part (13 items) consists of the Short Form-Health and Labour Questionnaire, a generic instrument to collect data on productivity losses due to health problems (e.g. absence from work).
Data collection, management and storage
Data will be handled confidentially in accordance with the Dutch Personal Data Protection Act. For the purpose of this study, a data management plan has been created with DMPonline (https://dmponline.dcc.ac.uk). Details of data management procedures can be requested from the first author of this manuscript. Quality checks, including double data entry and range check for data values will be performed by the first author (JK) and an additional researcher. Personal data will be coded with an individual ID-code, which is not relatable to the participant. All collected data will be stored in a file containing only the identification code. The coded research data will be stored at the BMS Datalab of the University of Twente for a period of 15 years. In this time period, data is accessible to other researchers. After the period of 15 years, data will be stored in long time storage at Data Archiving and Networked Service by the Royal Dutch Academy of Sciences. Participants who want to be informed about their personal data or who want their data deleted can send a request to the principal investigator.
Study integrity
The study protocol has been designed in accordance with the SPIRIT STATEMENT [83] and the study has been approved by the Medical Ethical Committee Twente (Proposal No: NL62997.044.17). The study will be carried out according to the principles of the Declaration of Helsinki (64th WMA General Assembly, Fortaleza, Brazil, October 2013) and the Medical Research Involving Human Subjects Act (WMO).
Statistical methods
Power calculation
The sample size calculation for this trial is conservatively based on the ability to detect at least a moderate effect of Cohen’s d = 0.60 in the post-hoc tests on the primary outcome (well-being) at post-intervention (T1). For a two-sided independent t-test with 80% power and α = 0.05, this requires 45 patients for both treatment groups. Taking a maximum drop-out rate of 20% into account, a total of 112 patients will need to be included for the per-protocol analysis.
Statistical analyses
Analyses will be done on both intention to treat (ITT) and per-protocol basis. The primary ITT analyses will be performed using linear mixed modelling (LMM) that adequately deals with missing at random data and the nested structure of repeated-measures data. LMMs with time, treatment and time-by-treatment interactions will be performed to test the effectiveness of the intervention in improving continuous primary and secondary outcomes of well-being, personal recovery, psychopathology, sef-compassion, positive relationships and dampening. Post-hoc independent t-tests with Holm-Bonferroni correction will be performed to test for significant between-group differences at all time-points. Based on estimated marginal means and corresponding standard errors from the LMM models, between-group standardized effect sizes will additionally be expressed as Cohen’s d with 95% confidence intervals (CI). Binary relapse data from the interviews will be analyzed with Kaplan Meyer survival estimates to compare the time to relapse and relapse rates between the intervention and control group. Differences in the proportion of relapsed patients and predictors of relapse will be additionally examined using generalized (binary) LMMs with post-hoc chi-square tests and relative risks (RR) with 95% CI to examine the significance and magnitude of differences at each follow-up point. Moderation and mediation analyses will be conducted to explore possible working mechanisms of the interventions. To calculate the cost-effectiveness of the intervention, quality adjusted life years (QALYs) will be taken into account as primary utility measure. QALYs will be calculated from the EQ-5D-5 L. The incremental cost-utility ratio (ICUR) will be calculated by dividing the difference in costs calculated from the TiC-P by the difference in the QALYs produced by the two groups. The ICUR is expressed as costs per QALY gained.
Discussion
The presented study aims to examine the short- and long term effectiveness of the multicomponent positive psychology intervention “Living well with bipolar disorder” for euthymic BD patients to enhance personal recovery and well-being. In the present article, we described the intervention development process and several adaptations made to the original program to tailor the intervention for the target group. The study will be conducted in at least four different outpatient treatment centers in the Netherlands, all specialized in the treatment of BD. The intervention group will receive the intervention program in addition to CAU and the control group will receive CAU only.
Several potential limitations of the study have to be considered in advance. Firstly, since participants in this intervention are euthymic (i.e. not in a syndromal depressive, hypomanic or manic episode), results of the trial cannot be generalized to the entire patient group in all phases of BD. Secondly, the study will not be able to determine which specific elements of the interventions lead to possible effects of the intervention. Non-specific factors (e.g. social contact during group lessons or placebo effect) can thus not be ruled out as possible confounding variables. However, since we mainly aim to investigate the effect of the intervention in real-life clinical practice and our study concerns a pragmatic randomized trial, this limitation is not considered to impair the value of our study [84]. Further research could investigate the effectiveness of the intervention to determine whether the intervention is equally effective when taking non-specific factors into account. Thirdly, non-adherence to the intervention or dropout from the assessment might occur. Both types of attrition are likely to bias the results [85].
Our study will be the first to explore the effectiveness of a positive psychology intervention for the treatment of people with BD. In addition, it will be the first study to be implemented that focusses on the improvement of primarily personal recovery and well-being and uses a more sound design than existing pilot studies. The results of the study are expected to broaden the evidence base of clinical positive psychology and personal recovery and potentially generate novel treatment methods for people suffering from BD.
Additional file
Participant timeline. Participant activity throughout the trial. (PDF 122 kb)
Funding
This study is funded by a grant from the Netherlands Organsiation for Health Research and Development (Grant No: 80-84300-98-81007) within the Efficiency Studies program.
Abbreviations
- ASRM
Altman self-rating mania scale
- BD
Bipolar disorder
- CAU
Care as usual
- CI
Confidence intervals
- GLMM
Generalized linear mixed modelling
- HADS-A
Hospital anxiety and depression scale - anxiety
- ITT
Intention-to-treat
- MHC-SF
Mental health continuum – Short form
- PANAS
Positive and negative affect schedule
- QALYs
Quality adjusted life years
- QIDS-SR
Quick inventory of depressive symptomatology – Self-report
- QPR
Questionnaire about the process of recovery
- RPA
Responses to positive affect questionnaire
- RR
Relative risks
- SCS-SF
Self-compassion scale – Short form
- SPWB
Scales of psychological wellbeing
- SRPQ
Social Role participation questionnaire
Authors’ contributions
MC, AWMMS, RWK. ETB and EN developed the original research design and developed the grant proposal in cooperation with PMtK and HRT. JTK coordinates the trial and drafted this manuscript. The manuscript was critically reviewed and modified by all authors and all authors read and approved the final manuscript.
Ethics approval and consent to participate
The current study has been approved by the Medical Ethical Committee Twente (Proposal No: NL62997.044.17). All participants will give written informed consent prior to taking part in the baseline assessment.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jannis T. Kraiss, Phone: + 31 (0) 53 489 4470, Email: j.t.kraiss@utwente.nl
Peter M. ten Klooster, Email: p.m.tenklooster@utwente.nl
Melissa Chrispijn, Email: m.chrispijn@dimence.nl.
Hester R. Trompetter, Email: h.r.trompetter@uvt.nl
Anja W.M.M. Stevens, Email: a.stevens@dimence.nl
Erica Neutel, Email: ericaneutel@gmail.com.
Ralph W. Kupka, Email: r.kupka@ggzingeest.nl
Ernst T. Bohlmeijer, Email: e.t.bohlmeijer@utwente.nl
References
- 1.Grande I, Berk M, Birmaher B, Vieta E. Bipolar disorder. Lancet. 2015;387(10027):1561–1572. doi: 10.1016/S0140-6736(15)00241-X. [DOI] [PubMed] [Google Scholar]
- 2.Kupka R, Knoppert E, Nolen W. Handboek bipolaire stoornissen. Utrecht: De Tijdstroom; 2008. [Google Scholar]
- 3.Berk M, Dodd S. Bipolar II disorder: a review. Bipolar Disord. 2005;7(1):11–21. doi: 10.1111/j.1399-5618.2004.00152.x. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association . Diagnostic and statistical manual of mental disorders (DSM-5®) Arlington: American Psychiatric Pub; 2013. [Google Scholar]
- 5.de Graaf R, ten Have M, van Dorsselaer S. Nemesis-2: Opzet en eerste resultaten. Utrecht: Trimbos-instituut; 2010. De psychische gezondheid van de Nederlandse bevolking. [Google Scholar]
- 6.Dilsaver SC. An estimate of the minimum economic burden of bipolar I and II disorders in the United States: 2009. J Affect Disord. 2011;129(1):79–83. doi: 10.1016/j.jad.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 7.Dean BB, Gerner D, Gerner RH. A systematic review evaluating health-related quality of life, work impairment, and healthcare costs and utilization in bipolar disorder. Curr Med Res Opin. 2004;20(2):139–154. doi: 10.1185/030079903125002801. [DOI] [PubMed] [Google Scholar]
- 8.Calabrese JR, Hirschfeld RMA, Reed M, Davies MA, Frye MA, Keck PE, Lewis L, McElroy SL, McNulty JP, Wagner KD. Impact of bipolar disorder on a U.S. community sample. J Clin Psychiatry. 2003;64(4):425–432. doi: 10.4088/JCP.v64n0412. [DOI] [PubMed] [Google Scholar]
- 9.Laxman KE, Lovibond KS, Hassan MK. Impact of bipolar disorder in employed populations. Am J Manag Care. 2008;14(11):757–764. [PubMed] [Google Scholar]
- 10.Fajutrao L, Locklear J, Priaulx J, Heyes A. A systematic review of the evidence of the burden of bipolar disorder in Europe. Clin Pract Epidemiol Ment Health. 2009;5:3. doi: 10.1186/1745-0179-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reinares M, Vieta E, Colom F, Martinez-Aran A, Torrent C, Comes M, Goikolea JM, Benabarre A, Daban C, Sanchez-Moreno J. What really matters to bipolar patients’ caregivers: sources of family burden. J Affect Disord. 2006;94(1–3):157–163. doi: 10.1016/j.jad.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 12.Miller S, Dell'Osso B, Ketter TA. The prevalence and burden of bipolar depression. J Affect Disord. 2014;169(Supplement 1):S3–S11. doi: 10.1016/S0165-0327(14)70003-5. [DOI] [PubMed] [Google Scholar]
- 13.Kupka R, Goossens P, van Bendegem M, Daemen P, Daggenvoorde T, Daniels M, Dols A, Hillegers MHJ, Hoogelander A, ter Kulve E. Edited by Trimbos-instituut. Utrecht: De Tijdstroom; 2015. Multidisciplinaire richtlijn bipolaire stoornissen. [Google Scholar]
- 14.van der Voort TY, van Meijel B, Goossens PJ, Renes J, Beekman AT, Kupka RW. Collaborative care for patients with bipolar disorder: a randomised controlled trial. BMC Psychiatry. 2011;11(1):133. doi: 10.1186/1471-244X-11-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Slade M. Mental illness and well-being: the central importance of positive psychology and recovery approaches. BMC Health Serv Res. 2010;10(1):26. doi: 10.1186/1472-6963-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones S, Mulligan LD, Higginson S, Dunn G, Morrison AP. The bipolar recovery questionnaire: psychometric properties of a quantitative measure of recovery experiences in bipolar disorder. J Affect Disord. 2013;147(1):34–43. doi: 10.1016/j.jad.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 17.Fava GA, Ruini C, Belaise C. The concept of recovery in major depression. Psychol Med. 2007;37(3):307–317. doi: 10.1017/S0033291706008981. [DOI] [PubMed] [Google Scholar]
- 18.Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry. 2011;199(6):445–452. doi: 10.1192/bjp.bp.110.083733. [DOI] [PubMed] [Google Scholar]
- 19.Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychiatr Rehabil J. 1993;16(4):11. [Google Scholar]
- 20.Keyes CL. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002;43(2):207–222. doi: 10.2307/3090197. [DOI] [PubMed] [Google Scholar]
- 21.Fagiolini A, Kupfer DJ, Masalehdan A, Scott JA, Houck PR, Frank E. Functional impairment in the remission phase of bipolar disorder. Bipolar Disord. 2005;7(3):281–285. doi: 10.1111/j.1399-5618.2005.00207.x. [DOI] [PubMed] [Google Scholar]
- 22.Judd LL, Schettler PJ, Akiskal HS, et al. Residual symptom recovery from major affective episodes in bipolar disorders and rapid episode relapse/recurrence. Arch Gen Psychiatry. 2008;65(4):386–394. doi: 10.1001/archpsyc.65.4.386. [DOI] [PubMed] [Google Scholar]
- 23.Kaya E, Aydemir Ö, Selcuki D. Residual symptoms in bipolar disorder: the effect of the last episode after remission. Prog Neuro-Psychopharmacol Biol Psychiatry. 2007;31(7):1387–1392. doi: 10.1016/j.pnpbp.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Fagiolini A, Forgione R, Maccari M, Cuomo A, Morana B, Dell'Osso MC, Pellegrini F, Rossi A. Prevalence, chronicity, burden and borders of bipolar disorder. J Affect Disord. 2013;148(2–3):161–169. doi: 10.1016/j.jad.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 25.Keyes CL, Dhingra SS, Simoes EJ. Change in level of positive mental health as a predictor of future risk of mental illness. Am J Public Health. 2010;100:2366–2371. doi: 10.2105/AJPH.2010.192245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lamers SMA, Westerhof GJ, Glas CAW, Bohlmeijer ET. The bidirectional relation between positive mental health and psychopathology in a longitudinal representative panel study. J Posit Psychol. 2015;10(6):553–560. doi: 10.1080/17439760.2015.1015156. [DOI] [Google Scholar]
- 27.Trompetter HR, de Kleine E, Bohlmeijer ET. Why does positive mental health buffer against psychopathology? An exploratory study on self-compassion as a resilience mechanism and adaptive emotion regulation strategy. Cogn Ther Res. 2017;41(3):459–468. doi: 10.1007/s10608-016-9774-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jones S, Higginson S, Murray C, Morrison AP. Britisch association for behavioural and cognitive psychotherapy annual conference. Manchester, UK. 2010. Recovery experiences in bipolar disorder. [Google Scholar]
- 29.Mead S, Copeland ME. What recovery means to us: consumers’ perspectives. Community Ment Health J. 2000;36(3):315–328. doi: 10.1023/A:1001917516869. [DOI] [PubMed] [Google Scholar]
- 30.Seligman CM. Positive psychology: an introduction. In: Csikszentmihalyi M, editor. Flow and the foundations of positive psychology: the collected works of Mihaly Csikszentmihalyi. edn. Dordrecht: Springer Netherlands; 2014. pp. 279–298. [Google Scholar]
- 31.Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol. 2009;65(5):467–487. doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- 32.Resnick SG, Rosenheck RA. Recovery and positive psychology: parallel themes and potential synergies. Psychiatr Serv. 2006;57(1):120–122. doi: 10.1176/appi.ps.57.1.120. [DOI] [PubMed] [Google Scholar]
- 33.Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health. 2013;13(1):119. doi: 10.1186/1471-2458-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deckersbach T, Hölzel BK, Eisner LR, Stange JP, Peckham AD, Dougherty DD, Rauch SL, Lazar S, Nierenberg AA. Mindfulness-based cognitive therapy for nonremitted patients with bipolar disorder. CNS Neurosci Ther. 2012;18(2):133–141. doi: 10.1111/j.1755-5949.2011.00236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eisner L, Eddie D, Harley R, Jacobo M, Nierenberg AA, Deckersbach T. Dialectical behavior therapy group skills training for bipolar disorder. Behav Ther. 2017;48(4):557–566. doi: 10.1016/j.beth.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jones S, Smith G, Mulligan LD, Lobban F, Law H, Dunn G, Welford M, Kelly J, Mulligan J, Morrison AP. Recovery-focused cognitive–behavioural therapy for recent-onset bipolar disorder: randomised controlled pilot trial. Br J Psychiatry. 2015;206(1):58–66. doi: 10.1192/bjp.bp.113.141259. [DOI] [PubMed] [Google Scholar]
- 37.Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IVand ICD-10. J Clin Psychiatry. 1998;59(20):2233. [PubMed] [Google Scholar]
- 38.Schotanus-Dijkstra M, Drossaert CH, Pieterse ME, Walburg JA, Bohlmeijer ET. Efficacy of a multicomponent positive psychology self-help intervention: study protocol of a randomized controlled trial. JMIR Res Protoc. 2015;4(3):e105. doi: 10.2196/resprot.4162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schotanus-Dijkstra M, Drossaert CHC, Pieterse ME, Boon B, Walburg JA, Bohlmeijer ET. An early intervention to promote well-being and flourishing and reduce anxiety and depression: a randomized controlled trial. Internet Interv. 2017;9(Supplement C):15–24. doi: 10.1016/j.invent.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Seligman . Flourishing. A new understanding of happiness and well-being–and how to achieve them Boston: Nicholas Brealey. 2011. [Google Scholar]
- 41.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57(6):1069. doi: 10.1037/0022-3514.57.6.1069. [DOI] [Google Scholar]
- 42.Meevissen YM, Peters ML, Alberts HJ. Become more optimistic by imagining a best possible self: effects of a two week intervention. J Behav Ther Exp Psychiatry. 2011;42(3):371–378. doi: 10.1016/j.jbtep.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 43.Bohlmeijer E, Hulsbergen M. Dit is jouw leven: ervaar de effecten van de positieve psychologie: UItgeverij Boom. 2013. [Google Scholar]
- 44.Gruber J. Can feeling too good be bad? Curr Dir Psychol Sci. 2011;20(4):217–221. doi: 10.1177/0963721411414632. [DOI] [Google Scholar]
- 45.Gruber J, Harvey AG, Gross JJ. When trying is not enough: emotion regulation and the effort-success gap in bipolar disorder. Emotion. 2012;12(5):997–1003. doi: 10.1037/a0026822. [DOI] [PubMed] [Google Scholar]
- 46.Phillips ML, Vieta E. Identifying functional neuroimaging biomarkers of bipolar disorder: toward DSM-V. Schizophr Bull. 2007;33(4):893–904. doi: 10.1093/schbul/sbm060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carl JR, Soskin DP, Kerns C, Barlow DH. Positive emotion regulation in emotional disorders: a theoretical review. Clin Psychol Rev. 2013;33(3):343–360. doi: 10.1016/j.cpr.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 48.Edge MD, Miller CJ, Muhtadie L, Johnson SL, Carver CS, Marquinez N, Gotlib IH. People with bipolar I disorder report avoiding rewarding activities and dampening positive emotion. J Affect Disord. 2013;146(3):407–413. doi: 10.1016/j.jad.2012.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gilbert KE, Nolen-Hoeksema S, Gruber J. Positive emotion dysregulation across mood disorders: how amplifying versus dampening predicts emotional reactivity and illness course. Behav Res Ther. 2013;51(11):736–741. doi: 10.1016/j.brat.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 50.Mansell W, Paszek G, Seal K, Pedley R, Jones S, Thomas N, Mannion H, Saatsi S, Dodd A. Extreme appraisals of internal states in bipolar I disorder: a multiple control group study. Cogn Ther Res. 2011;35(1):87–97. doi: 10.1007/s10608-009-9287-1. [DOI] [Google Scholar]
- 51.Mansell W, Powell S, Pedley R, Thomas N, Jones SA. The process of recovery from bipolar I disorder: a qualitative analysis of personal accounts in relation to an integrative cognitive model. Br J Clin Psychol. 2010;49(Pt 2):193–215. doi: 10.1348/014466509X451447. [DOI] [PubMed] [Google Scholar]
- 52.Alatiq Y, Crane C, Williams J, Goodwin G. Dysfunctional beliefs in bipolar disorder: hypomanic vs. depressive attitudes. J Affect Disord. 2010;122(3):294–300. doi: 10.1016/j.jad.2009.08.021. [DOI] [PubMed] [Google Scholar]
- 53.Dodd AL, Mansell W, Morrison AP, Tai S. Extreme appraisals of internal states and bipolar symptoms: the hypomanic attitudes and positive predictions inventory. Psychol Assess. 2011;23(3):635. doi: 10.1037/a0022972. [DOI] [PubMed] [Google Scholar]
- 54.Allen AB, Leary MR. Self-compassion, stress, and coping. Soc Personal Psychol Compass. 2010;4(2):107–118. doi: 10.1111/j.1751-9004.2009.00246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leary MR, Tate EB, Adams CE, Batts Allen A, Hancock J. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Pers Soc Psychol. 2007;92(5):887–904. doi: 10.1037/0022-3514.92.5.887. [DOI] [PubMed] [Google Scholar]
- 56.Barnard LK, Curry JF. Self-compassion: conceptualizations, correlates, & interventions. Rev Gen Psychol. 2011;15(4):289–303. doi: 10.1037/a0025754. [DOI] [Google Scholar]
- 57.Hergueta T, Weiller E. Evaluating depressive symptoms in hypomanic and manic episodes using a structured diagnostic tool: validation of a new Mini International Neuropsychiatric Interview (MINI) module for the DSM-5′With mixed features’ specifier. Int J Bipolar Disord. 2013;1(1):21. doi: 10.1186/2194-7511-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lamers SMA, Westerhof GJ, Bohlmeijer ET, ten Klooster PM, Keyes CL. Evaluating the psychometric properties of the mental health continuum-short form (MHC-SF) J Clin Psychol. 2011;67(1):99–110. doi: 10.1002/jclp.20741. [DOI] [PubMed] [Google Scholar]
- 59.Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W. Modification of the Clinical Global Impressions (CGI) scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res. 1997;73(3):159–171. doi: 10.1016/S0165-1781(97)00123-6. [DOI] [PubMed] [Google Scholar]
- 60.Neil ST, Kilbride M, Pitt L, Nothard S, Welford M, Sellwood W, Morrison AP. The questionnaire about the process of recovery (QPR): a measurement tool developed in collaboration with service users. Psychosis. 2009;1(2):145–155. doi: 10.1080/17522430902913450. [DOI] [Google Scholar]
- 61.Law H, Neil ST, Dunn G, Morrison AP. Psychometric properties of the questionnaire about the process of recovery (QPR) Schizophr Res. 2014;156(2–3):184–189. doi: 10.1016/j.schres.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 62.Williams J, Leamy M, Pesola F, Bird V, Le Boutillier C, Slade M. Psychometric evaluation of the Questionnaire about the Process of Recovery (QPR) Br J Psychiatry. 2015;207(6):551. doi: 10.1192/bjp.bp.114.161695. [DOI] [PubMed] [Google Scholar]
- 63.Davis AM, Palaganas MP, Badley EM, Gladman DD, Inman RD, Gignac MA. Measuring participation in people with spondyloarthritis using the social role participation questionnaire. Ann Rheum Dis. 2011;70(10):1765–1769. doi: 10.1136/ard.2010.149211. [DOI] [PubMed] [Google Scholar]
- 64.Oude Voshaar M, van Onna M, van Genderen S, van de Laar M, van der Heijde D, Heuft L, Spoorenberg A, Luime J, Gignac M, Boonen A. Development and validation of a short form of the social role participation questionnaire in patients with ankylosing spondylitis. J Rheumatol. 2016;43(7):1386–1392. doi: 10.3899/jrheum.151013. [DOI] [PubMed] [Google Scholar]
- 65.Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Markowitz JC, Ninan PT, Kornstein S, Manber R, et al. The 16-item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–583. doi: 10.1016/S0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 66.Wardenaar KJ, van Veen T, Giltay EJ, den Hollander-Gijsman M, Penninx BWJH, Zitman FG. The structure and dimensionality of the Inventory of Depressive Symptomatology Self Report (IDS-SR) in patients with depressive disorders and healthy controls. J Affect Disord. 2010;125(1):146–154. doi: 10.1016/j.jad.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 67.Altman EG, Hedeker D, Peterson JL, Davis JM. The Altman self-rating mania scale. Biol Psychiatry. 1997;42(10):948–955. doi: 10.1016/S0006-3223(96)00548-3. [DOI] [PubMed] [Google Scholar]
- 68.Altman E, Hedeker D, Peterson JL, Davis JM. A comparative evaluation of three self-rating scales for acute mania. Biol Psychiatry. 2001;50(6):468–471. doi: 10.1016/S0006-3223(01)01065-4. [DOI] [PubMed] [Google Scholar]
- 69.Meyer B, Beevers CG, Johnson SL. Goal appraisals and vulnerability to bipolar disorder: a personal projects analysis. Cogn Ther Res. 2004;28(2):173–182. doi: 10.1023/B:COTR.0000021538.34160.52. [DOI] [Google Scholar]
- 70.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 71.Spinhoven P, Ormel J, Sloekers P, Kempen G, Speckens A, Van Hemert A. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27(2):363–370. doi: 10.1017/S0033291796004382. [DOI] [PubMed] [Google Scholar]
- 72.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063. doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 73.Engelen U, De Peuter S, Victoir A, Van Diest I, Van den Bergh O. Verdere validering van de Positive and Negative Affect Schedule (PANAS) en vergelijking van twee Nederlandstalige versies. Gedrag en gezondheid. 2006;34(2):61–70. [Google Scholar]
- 74.Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the self-compassion scale. Clin Psychol Psychother. 2011;18(3):250–255. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- 75.Neff KD. The development and validation of a scale to measure self-compassion. Self Identity. 2003;2(3):223–250. doi: 10.1080/15298860309027. [DOI] [Google Scholar]
- 76.Ryff CD, Keyes CLM. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69(4):719. doi: 10.1037/0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- 77.Van Dierendonck D. The construct validity of Ryff's scales of psychological well-being and its extension with spiritual well-being. Personal Individ Differ. 2004;36(3):629–643. doi: 10.1016/S0191-8869(03)00122-3. [DOI] [Google Scholar]
- 78.Raes F, Daems K, Feldman G, Johnson S, Van Gucht D. A psychometric evaluation of the Dutch version of the responses to positive affect questionnaire. Psychologica Belgica. 2010;49(4):293–310. doi: 10.5334/pb-49-4-293. [DOI] [Google Scholar]
- 79.Feldman G, Joormann J, Johnson S. Responses to positive affect: a self-report measure of rumination and dampening. Cogn Ther Res. 2008;32(4):507. doi: 10.1007/s10608-006-9083-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Denicoff KD, Leverich GS, Nolen WA, Rush AJ, McElroy SL, Keck PE, Suppes T, Altshuler LL, Kupka R, Frye MA, et al. Validation of the prospective NIMH-Life-Chart Method (NIMH-LCM-p) for longitudinal assessment of bipolar illness. Psychol Med. 2000;30(6):1391–1397. doi: 10.1017/S0033291799002810. [DOI] [PubMed] [Google Scholar]
- 81.Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual Life Res. 2011;20(10):1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bouwmans C, De Jong K, Timman R, Zijlstra-Vlasveld M, Van der Feltz-Cornelis C, Tan SS, Hakkaart-van Roijen L. Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P) BMC Health Serv Res. 2013;13(1):217. doi: 10.1186/1472-6963-13-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chan A-W, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, Dickersin K, Hróbjartsson A, Schulz KF, Parulekar WR, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586. doi: 10.1136/bmj.e7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chalkidou K, Tunis S, Whicher D, Fowler R, Zwarenstein M. The role for pragmatic randomized controlled trials (pRCTs) in comparative effectiveness research. Clin Trials. 2012;9(4):436–446. doi: 10.1177/1740774512450097. [DOI] [PubMed] [Google Scholar]
- 85.Eysenbach G. The law of attrition. J Med Internet Res. 2005;7(1):e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gilbert P. An introduction to compassion focused therapy in cognitive behavior therapy. Int J Cognit Ther. 2010;3(2):97–112. doi: 10.1521/ijct.2010.3.2.97. [DOI] [Google Scholar]
- 87.Neff K. Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Identity. 2003;2(2):85–101. doi: 10.1080/15298860309032. [DOI] [Google Scholar]
- 88.Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol. 2013;69(1):28–44. doi: 10.1002/jclp.21923. [DOI] [PubMed] [Google Scholar]
- 89.Peters ML, Flink IK, Boersma K, Linton SJ. Manipulating optimism: can imagining a best possible self be used to increase positive future expectancies? J Posit Psychol. 2010;5(3):204–211. doi: 10.1080/17439761003790963. [DOI] [Google Scholar]
- 90.Fredrickson BL. Positive emotions broaden and build. Adv Exp Soc Psychol. 2013;47(1):53. [Google Scholar]
- 91.Lyubomirsky S, Layous K. How do simple positive activities increase well-being? Curr Dir Psychol Sci. 2013;22(1):57–62. doi: 10.1177/0963721412469809. [DOI] [Google Scholar]
- 92.Linley PA, Nielsen KM, Gillett R, Biswas-Diener R. Using signature strengths in pursuit of goals: effects on goal progress, need satisfaction, and well-being, and implications for coaching psychologists. Int Coach Psychol Rev. 2010;5(1):6–15. [Google Scholar]
- 93.Wood AM, Linley PA, Maltby J, Kashdan TB, Hurling R. Using personal and psychological strengths leads to increases in well-being over time: a longitudinal study and the development of the strengths use questionnaire. Personal Individ Differ. 2011;50(1):15–19. doi: 10.1016/j.paid.2010.08.004. [DOI] [Google Scholar]
- 94.Otake K, Shimai S, Tanaka-Matsumi J, Otsui K, Fredrickson BL. Happy people become happier through kindness: a counting kindnesses intervention. J Happiness Stud. 2006;7(3):361–375. doi: 10.1007/s10902-005-3650-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Reis HT, Gable SL. Toward a positive psychology of relationships. 2003. [Google Scholar]
- 96.Reis HT, Smith SM, Carmichael CL, Caprariello PA, Tsai F-F, Rodrigues A, Maniaci MR. Are you happy for me? How sharing positive events with others provides personal and interpersonal benefits. J Pers Soc Psychol. 2010;99(2):311. doi: 10.1037/a0018344. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Participant timeline. Participant activity throughout the trial. (PDF 122 kb)