Abstract
Lichen planopilaris (LPP) is an inflammatory hair disorder that is characterized by scarring hair loss, mostly affecting the vertex and parietal areas of the scalp. Frontal fibrosing alopecia (FFA) is considered a particular form of LPP, primarily affecting the hair follicles in the frontotemporal area of the scalp, with the hairline recession and eyebrow loss. There are case reports of FFA with concomitant involvement of facial vellus, characterized by roughening of the facial skin. We report five cases of facial vellus hair involvement in LPP, in the absence of other sites of disease activity. To the best of our knowledge, ours is the first report of LPP affecting the facial vellus hairs in the absence of FFA.
Key words: Lichen planopilaris, facial vellus hairs, facial papules
INTRODUCTION
Lichen planopilaris (LPP) is an uncommon inflammatory hair disorder that is clinically characterized by perifollicular erythema, follicular hyperkeratosis, and scarring hair loss, mostly affecting the vertex and parietal areas of the scalp. Frontal fibrosing alopecia (FFA) is considered a clinical subtype of LPP, first described by Kossard[1] in 1994. It mainly occurs in postmenopausal women, and primarily affects the hair follicles in the frontotemporal area of the scalp, with the hairline recession and eyebrow loss.
Abbas et al.[2] were the first to report a case of FFA with concomitant follicular lichen planus-like lesions of the face in a 37-year-old premenopausal woman. More recently, other cases of involvement of facial vellus hairs have been reported in FFA, characterized by the appearance of facial papules and roughening of the facial skin.[3,4,5,6] We report five cases of facial LPP, in the absence of other sites of disease activity.
CLINICAL CASES
Five Caucasian women presented at our clinic because of roughening of the facial skin surface, caused by the appearance of small skin-colored papules [Table 1]. All of them were premenopausal, with ages ranging from 30 to 44 years old. None of the patients had a history of autoimmune diseases, hormonal disorders, or other comorbidities. On clinical examination, they all presented with fine, skin-colored, follicular papules spread over the temples, the cheeks and mandibular area, and the forehead and the chin [Figure 1]. Facial vellus hairs were reduced. There were neither clinical nor dermoscopical signs of hairline recession or eyebrow alopecia. A total body examination was performed in all of the five patients, and did not show any alterations regarding body hair. There was no involvement of mucous membranes or nails. In some of these patients, their skin condition was misdiagnosed and treated, even for several years, as acne vulgaris, rosacea or Demodex folliculitis, although inflammatory papules or pustules were absent.
Table 1.
Clinical cases
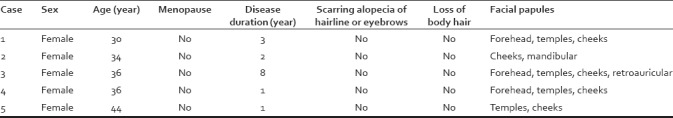
Figure 1.
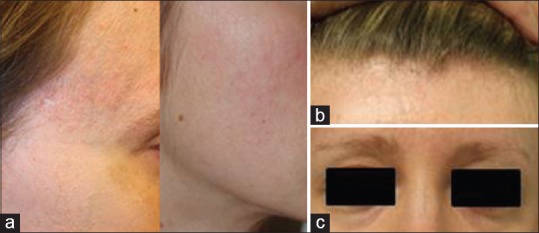
Clinical presentation. (a) Characteristic pinpoint papules over the left temporal region. (b and c) normal frontal hairline and eyebrows with no signs of scarring alopecia
A skin biopsy was performed in all five patients. Histologic evaluation of these five specimens showed a similar image of disruption and destruction of the follicular unit architecture, with a chronic lymphocytic inflammation surrounding the follicle. There were fibrous tract formation and perifollicular fibrosis, compatible with the histological features of lichen planopilaris [Figure 2].
Figure 2.
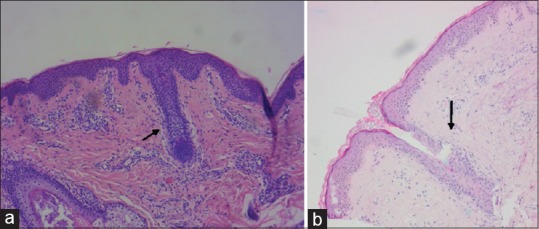
Histopathological evaluation of skin biopsy. (a) Case 3: Perifollicular lymphocytic infiltrate. (b) Case 1: Perifollicular fibrosis and fibrous tract formation
DISCUSSION
Lichen planopilaris is typically characterized by perifollicular erythema, follicular hyperkeratosis, and scarring hair loss, mostly affecting the vertex and parietal areas of the scalp. The involvement of facial vellus hairs, clinically presenting as pinpoint, skin-colored papules and a decrease or absence of vellus hairs has been reported, but always in concomitance with FFA.[3,4,5,6] Vañó-Galván et al. reported a series of 355 patients with FFA, of which 49 (14%) presented with facial papules.[4] These authors state that the involvement of facial vellus hairs in FFA is thought to be associated with a more severe form of FFA and higher disease activity.[4] In that case, it would be advisable to monitor patients with facial vellus involvement more closely, to detect any alterations in scalp or eyebrow hair early, and evaluate the need for systemic treatment. In the follow-up period of our patients, however (1–8 years), there was no sign of evolving FFA.
To our knowledge, ours is the first report on LPP affecting the facial vellus hairs in the absence of FFA. Due to the subtle clinical changes, especially in the early phase of the disease, recognition of these papules can be difficult and subjective. Especially, in younger patients, they are often mistaken for comedones or small papules of acne or rosacea. In older patients, photoaging may hamper the diagnosis, as solar elastosis and wrinkles may complicate the recognition of these small papules. Involvement of inframandibular and retroauricular areas may help to differentiate from solar elastosis. A skin biopsy is often needed to establish this diagnosis; however even then it remains difficult, due to the subtle histological changes. A clinicopathological correlation is of great importance. Dermoscopy can be of diagnostic help. The damage of the facial vellus hair can manifest as white-blurred dots, with a decrease or lack in vellus hairs and follicular orifices.[6]
We believe that this diagnosis is often missed and may be more prevalent then it appears from the literature. Since this is the first report on LPP affecting the facial vellus hairs in the absence of FFA, still a lot of questions remain. We are not convinced that, as previously reported in the literature,[3] the facial vellus hair involvement is always part of the clinical spectrum of FFA. The young age of the patients and the absence of any other involvement of the skin even lead us to think this might be a separate entity, although presenting with similar histopathology. We as dermatologists have to be aware of this entity and learn to recognize these subtle clinical changes. This together with further follow-up of the patients may contribute to clarify this entity in the near future.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kossard S. Postmenopausal frontal fibrosing alopecia. Scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130:770–4. [PubMed] [Google Scholar]
- 2.Abbas O, Chedraoui A, Ghosn S. Frontal fibrosing alopecia presenting with components of piccardi-lassueur-graham-little syndrome. J Am Acad Dermatol. 2007;57:S15–8. doi: 10.1016/j.jaad.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 3.Donati A, Molina L, Doche I, Valente NS, Romiti R. Facial papules in frontal fibrosing alopecia: Evidence of vellus follicle involvement. Arch Dermatol. 2011;147:1424–7. doi: 10.1001/archdermatol.2011.321. [DOI] [PubMed] [Google Scholar]
- 4.Vañó-Galván S, Molina-Ruiz AM, Serrano-Falcón C, Arias-Santiago S, Rodrigues-Barata AR, Garnacho-Saucedo G, et al. Frontal fibrosing alopecia: A multicenter review of 355 patients. J Am Acad Dermatol. 2014;70:670–8. doi: 10.1016/j.jaad.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Ramanauskaite A, Trueb R. Facial papules in frontal fibrosing alopecia in a pattern distribution (cicatricial pattern hari loss) Int J Trichology. 2015;7:119–22. doi: 10.4103/0974-7753.167463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.López-Pestaña A, Tuneu A, Lobo C, Ormaechea N, Zubizarreta J, Vildosola S, et al. Facial lesions in frontal fibrosing alopecia (FFA): Clinicopathological features in a series of 12 cases. J Am Acad Dermatol. 2015;73:987.e1–6. doi: 10.1016/j.jaad.2015.08.020. [DOI] [PubMed] [Google Scholar]


