Abstract
Introduction
The global burden of disease (GBD) studies have derived detailed and comparable epidemiological and burden of disease estimates for schizophrenia. We report GBD 2016 estimates of schizophrenia prevalence and burden of disease with disaggregation by age, sex, year, and for all countries.
Method
We conducted a systematic review to identify studies reporting the prevalence, incidence, remission, and/or excess mortality associated with schizophrenia. Reported estimates which met our inclusion criteria were entered into a Bayesian meta-regression tool used in GBD 2016 to derive prevalence for 20 age groups, 7 super-regions, 21 regions, and 195 countries and territories. Burden of disease estimates were derived for acute and residual states of schizophrenia by multiplying the age-, sex-, year-, and location-specific prevalence by 2 disability weights representative of the disability experienced during these states.
Findings
The systematic review found a total of 129 individual data sources. The global age-standardized point prevalence of schizophrenia in 2016 was estimated to be 0.28% (95% uncertainty interval [UI]: 0.24–0.31). No sex differences were observed in prevalence. Age-standardized point prevalence rates did not vary widely across countries or regions. Globally, prevalent cases rose from 13.1 (95% UI: 11.6–14.8) million in 1990 to 20.9 (95% UI: 18.5–23.4) million cases in 2016. Schizophrenia contributes 13.4 (95% UI: 9.9–16.7) million years of life lived with disability to burden of disease globally.
Conclusion
Although schizophrenia is a low prevalence disorder, the burden of disease is substantial. Our modeling suggests that significant population growth and aging has led to a large and increasing disease burden attributable to schizophrenia, particularly for middle income countries.
Keywords: mental health, schizophrenia, epidemiology, burden of disease
Introduction
Schizophrenia is a complex mental disorder, with typical onset in late adolescence or early adulthood. Despite intensive and ongoing research, outcomes from best-practice treatment are often suboptimal. A systematic review based on 50 outcome studies reported that the median proportion of people with schizophrenia who met clinical and social recovery criteria was only 13.5%.1
In addition to poor recovery outcomes, those living with schizophrenia have a significantly reduced life expectancy.2 High excess mortality is found across all age groups3 and this differential mortality gap between those with and without schizophrenia may have increased in recent decades.4 Schizophrenia has also been linked to higher rates of comorbid illnesses and most excess deaths are due to underlying physical illnesses, especially chronic diseases such as coronary heart disease, stroke, type II diabetes, respiratory diseases, and some cancers.2 Unnatural causes, including suicide, account for less than 15% of excess deaths.3
Schizophrenia is a disorder with a relatively low prevalence. A systematic review conducted by Saha et al5 demonstrated a median population period prevalence of 3.3 per 1000. Developing health services for schizophrenia will require robust and informative epidemiological estimates, including estimates of the number of people living with schizophrenia in a given population and how these have changed over time—estimates that are currently unavailable for schizophrenia. Recent innovations in statistical modeling, as part of the global burden of disease (GBD) studies, have allowed for the derivation of detailed and comparable epidemiological estimates for schizophrenia by age, sex, geography, and year.
Quantification of the burden of disease attributable to schizophrenia was first undertaken in the GBD Study carried out by the World Health Organization in 1990,6 with an update in 2004.7 Recent iterations of the GBD Study, conducted by the Institute for Health Metrics and Evaluation at the University of Washington, have expanded the number of included disorders and made significant methodological improvements. The most recent iteration is GBD 2016.8
The core metric used to measure disease burden in GBD is the disability adjusted life year (DALY). One DALY is equivalent to 1 healthy year of life lost to a disease. The DALY is calculated by summing the years of life lived with disability (YLDs) and years of life lost (YLLs) to premature mortality for a given disease. This inclusion of disability when measuring disease burden has been particularly influential in highlighting schizophrenia as a leading contributor to disease burden. Despite being a low prevalence disorder, schizophrenia ranked the 12th most disabling disorder among 310 diseases and injuries globally in 2016.9
The GBD 2016 study provides an overview of the epidemiology and burden of disease attributable to 333 diseases and injuries; however, detailed findings for schizophrenia have not been previously published. We report GBD 2016 estimates of schizophrenia prevalence and burden of disease with disaggregation by age, sex, year, and country. Additionally, we will explore how changes in population growth and ageing have impacted on the epidemiology of schizophrenia over time, and how burden of disease varies by geography and development status. The availability of global epidemiological data on schizophrenia, which underpins this work, will also be presented in detail.
Methods
In GBD 2016, schizophrenia was defined according to diagnostic criteria proposed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR: 295.10–295.30, 295.60, 295.90)10 or the International Classification of Diseases (ICD-10: F20.0-F20.3 F20.5-F20.9).11 Other psychotic disorders, including those due to a general medical condition or substance induced cases, were not included.
Estimation of Years Lived With Disability
Identifying Available Data.
We conducted a systematic review of the literature to identify studies reporting the prevalence, incidence, remission, and/or excess mortality associated with schizophrenia. Comprehensive literature reviews have been conducted for studies reporting on the incidence,12 prevalence,5 remission,1 and excess mortality4 of schizophrenia published between 1965 and 2002. These existing reviews formed the starting point of our search. All included studies were reviewed for eligibility and the systematic literature searches were replicated to identify any subsequent data published up to 2016. Electronic databases (Medline, PsycInfo, and EMBASE) were searched using the following search string: (Schizophrenia[Title]) AND (((((epidemiology) OR epidemiology[MeSH Terms]) OR prevalence[Title/Abstract]) OR incidence[Title/Abstract]) OR mortality[Title/Abstract]) OR remission[Title/Abstract])). A secondary manual search of review articles, texts, and key documents was conducted to identify any additional studies not found in the database search. The final stage was to email experts in the field seeking information on any further data, including that not yet published. The search methodology adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.13 All GBD 2016 analyses adhered to the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER).14
Studies found in both the previous reviews and the current search were evaluated against a set of inclusion criteria. To be included in our GBD 2016 analysis, studies needed to: (1) make use of a cross-sectional or longitudinal design, the latter with a minimum follow up period of two years to allow sufficient time for observation of outcomes; (2) report estimates of prevalence, incidence, remission, and/or excess mortality for schizophrenia; or provide sufficient data for these to be estimated; (3) utilize the DSM or ICD diagnostic criteria; (4) report estimates of point (current/past month) or past year prevalence (lifetime estimates were excluded as these are at an increased risk of recall bias15–18); (5) report estimates of incidence in the form of hazard rates with person years of follow up as the denominator; (6) report estimates of excess mortality in the form of relative risks or standardized mortality ratio; and (7) make use of a sample which could be considered representative of the community, region, or country under study (inpatient and clinical samples were excluded, except for estimates of mortality). Publications were restricted to those published from 1980 onwards. A list of epidemiological data sources by type and country can be found in the online supplementary material. Additionally, a suite of visualization tools is available to explore GBD data inputs and outputs (http://www.healthdata.org/gbd/data-visualizations).
Modeling Prevalence.
Reported estimates of prevalence, incidence, remission, and excess mortality were entered in DisMod-MR 2.1 for analysis. DisMod-MR 2.1 is a Bayesian meta-regression tool used in GBD 2016 to meta-analyze prevalence.19,20 It is an updated version of DisMod MR 1.0 used in GBD 201021 and makes use of an established incidence–prevalence–mortality mathematical model as well as a log rate model to estimate prevalence. DisMod-MR 2.1 estimated prevalence globally for 23 age groups, 6 time points, 7 super-regions, 21 regions, and 195 countries and territories. This includes subnational locations in the United Kingdom, China, Mexico, Indonesia, Brazil, India, Japan, Kenya, Sweden, South Africa, Saudi Arabia, and the United States. If no raw epidemiological data were available for a particular location, data from surrounding locations were used to estimate prevalence. Within DisMod-MR 2.1, regions and super-regions were defined according to GBD 2016’s classification of broad geographic regions or continents. Each region was made up of 2 or more countries, grouped according to child/adult mortality rates and major causes of death. The estimation of prevalence was conducted as a full “cascade” ie, in sequence from global, to super-regional, to regional, and finally, country-level and where relevant sub-national-level estimations. This approach ensured that the modeled prevalence output was consistent at all levels of the cascade. At the global level, reported estimates of prevalence, incidence, remission, and excess-mortality were used to estimate super-regions priors using a mixed effects nonlinear regression model. The super-region modeled output was generated using these priors passed down from the global fit. These were used to generate regional-level estimates which in turn informed country- and subnational-level estimates. Additional information on DisMod-MR 2.1 can be accessed elsewhere.19,20
In order to facilitate modeling, a range of simplifying assumptions was used to guide the DisMod-MR 2.1 analysis for schizophrenia. We assumed zero incidence before age 10 and after age 80. These age limits were corroborated with expert feedback as well as the age range of the incidence data obtained from our systematic review. Remission was defined as complete clinical remission and was restricted to a maximum annualized remission rate of 0.04 as guided by the raw data.
Covariates.
We identified sources of variability in the raw data and used covariates during the modeling process to test whether these sources of variability were being driven by measurement error; however, none of the study-level covariates had a statistically significant effect on the prevalence model. Examples of variables tested in DisMod modeling include diagnostic type (designed to create a crosswalk between prevalence based on unknown diagnostic criteria to prevalence based on the ICD/DSM criteria), and sample coverage (designed to create a crosswalk between prevalence derived from samples with community coverage and prevalence from samples with more representative regional/national coverage).
Disability Weights.
YLDs were estimated for schizophrenia by multiplying the DisMod MR 2.1 age-, sex-, year-, and location-specific prevalence by 2 disability weights representative of the disability experienced during acute and residual states of schizophrenia. An acute state predominantly involved the presentation of positive symptoms of schizophrenia (eg, delusions, hallucinations, and thought disorder). A residual state predominantly involved negative symptoms (eg, flat affect, loss of interest, and emotional withdrawal).22 These 2 health states were selected to capture differences in disability caused by changes in the severity of symptoms of schizophrenia. They were defined according to the DSM-IV-TR description of this disorder.10 Disability weights were estimated using community-based surveys in Bangladesh, Indonesia, Peru, the United Republic of Tanzania, and the United States of America (conducted for GBD 2010), and Hungary, Italy, Sweden, and the Netherlands (conducted for GBD 2013), as well as an open-access internet survey available in English, Spanish, and Mandarin.20,23–26 Overall, disability weight surveys included lay descriptions representing all nonfatal outcomes from the diseases and injuries in GBD. Lay descriptions were presented to participants in a pair-wise comparison method, ie, participants were provided with random pairings of lay descriptions and asked to nominate which lay description they considered the healthier. Their responses were anchored on a scale of 0 (healthy) to 1 (death) using additional questions comparing the benefits of lifesaving and disease prevention programs for a selection of health states.20 The estimated disability weights for acute and residual states of schizophrenia were 0.778 (0.606–0.900) and 0.588 (0.411–0.754), respectively. Acute schizophrenia carries the highest disability weight of all disorders in GBD.25
Severity Splits.
To capture differences in disability caused by changes in the severity of symptoms of schizophrenia, disability weights were determined for 2 health states (acute and residual states) defined according to the DSM-IV-TR10 description of this disorder.9 We conducted a separate systematic literature review to identify survey data reporting on the proportion of schizophrenia cases in an acute and residual state, respectively.22 Meta-Xl 1.2, a Microsoft Excel add in for meta-analysis was used to pool data from 6 studies into the total proportion of schizophrenia cases experiencing acute and residual states.22 Pooled health state-specific proportions were used to distribute total schizophrenia prevalent cases (estimated by Dismod MR 2.1) across each health-state specific disability weight. Overall, 62.7% (28.8%–91.4%) of schizophrenia cases fell within an acute state and 37.3% (8.6%–71.2%) fell within a residual state. More information on the meta-analysis of health-state specific proportions is presented in the online supplementary material.
Comorbidity Adjustments.
An adjustment for comorbidity was necessary due to the fact that the burden attributable to GBD causes was estimated separately. The co-occurrence of different diseases and injuries was simulated in populations of 40000 within each stratification of location, age, sex, and year. The individuals within each population were hypothetically exposed to the independent probability of having any combination of sequelae included in GBD 2016. The comorbidity adjustment estimated the difference between the average disability weight of individuals experiencing one sequela and the multiplicatively combined disability weight of those experiencing multiple sequelae. The average comorbidity correction estimated for each sequela was applied to the respective location-, age-, sex-, and year-specific YLD. Further information is available elsewhere.9
Estimation of DALYs
DALYS are estimated by the sum of YLDs and YLLs for an overall measure of disease burden. Although it is widely acknowledged that schizophrenia is associated with premature mortality, GBD 2016 did not attribute any cause-specific deaths to schizophrenia per se, thus there were no YLLs estimated and DALYs were equivalent to YLDs.
95% uncertainty intervals (UI) were propagated from all levels of the burden estimation methodology based on the 25th and 75th ordered draw of the modeling process. Age-standardized rates were computed using the world standard population developed for the GBD study.27
Results
Data Availability
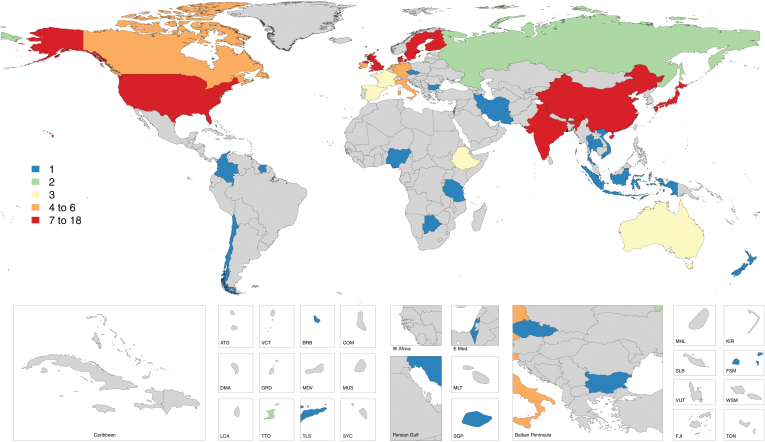
The systematic review found a total of 129 individual data sources which could be included in the DisMod modeling for GBD 2016. These included 64 prevalence, 37 mortality, 5 remission, and 30 incidence studies from 106 geographical locations (including both national and subnational locations) giving a total of 756 individual data points (supplementary table S1). Much of epidemiological data came from high income countries—notably, Denmark, Japan, and Sweden (figure 1). China and India also had a relatively high amount of epidemiological data representative at the provincial-level; however, data from other low- and middle-income countries was very sparse (figure 1). Further details of input data sources can be found online at http://ghdx.healthdata.org/gbd-2016/data-input-sources.
Fig. 1.
Map of epidemiological data points by global burden of disease region.
Prevalence
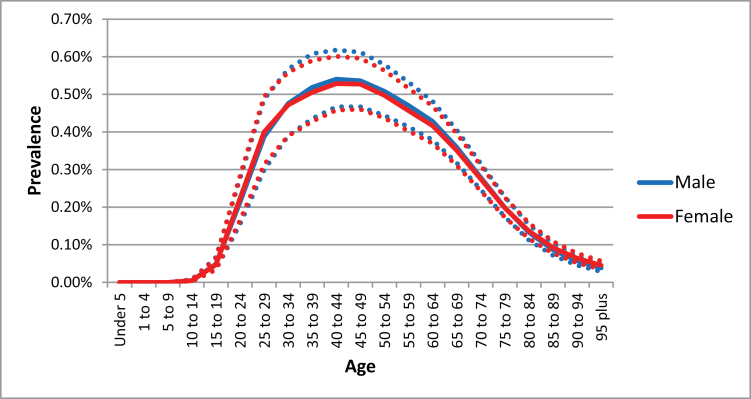
The global age-standardized point prevalence of schizophrenia in 2016 was estimated to be 0.28% (95% UI: 0.24–0.31). Figure 2 demonstrates an onset of schizophrenia in adolescence and young adulthood with prevalence peaking at around 40 years of age with a decline in the older age groups. No sex differences were observed in prevalence.
Fig. 2.
Global mean prevalence rates (with 95% uncertainty interval) by age and sex, 2016.
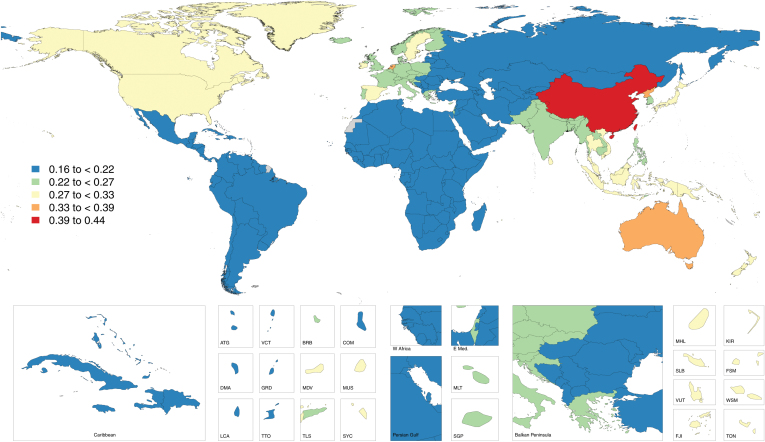
Age-standardized point prevalence rates to do not vary widely across countries or regions (figure 3 and supplementary table S2); however, data sources from several subnational surveys in China have resulted in consistently higher modeled estimates for China, which showed the highest age-standardized prevalence of schizophrenia (0.42% [95% UI: 0.38–0.48]; figure 3). The prevalence of schizophrenia in the Netherlands was higher than that of other countries within Western Europe (0.36% [95% UI: 0.32–0.40]). Some of the lowest mean prevalence rates were found in the sub-Saharan Africa and North Africa/Middle East regions.
Fig. 3.
Map of age-standardized prevalence by country, 2016.
Globally, prevalent cases rose from 13.1 (95% UI: 11.6–14.8) million in 1990 to 20.9 (95% UI: 18.5–23.4) million cases in 2016. An estimated 70.8% (or 14.8 million) of these cases occurred in the 25–54 years age group.
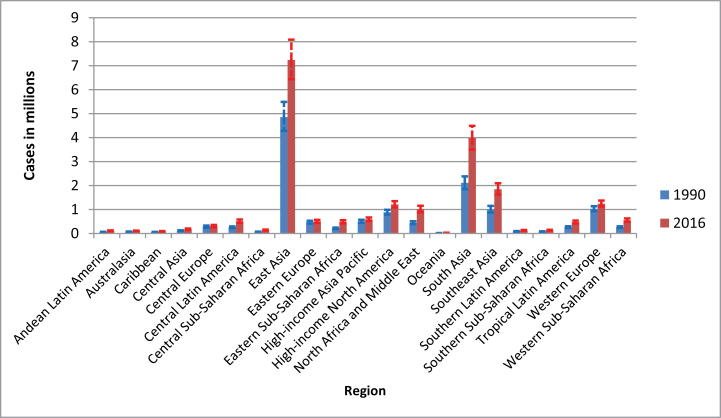
Incorporating regional population sizes to estimate prevalent cases shows that East Asia and South Asia carry the largest number of cases, approximately 7.2 (95% UI: 6.4–8.1) million and 4.0 (95% UI: 3.5–4.5) million, respectively in 2016 (figure 4). Oceania had the lowest number of cases, around 28000 (95% UI: 24000–32000), and the combined sub-Saharan African regions experienced approximately 1.3 (95% UI: 1.1–1.5) million cases in 2016.
Fig. 4.
Prevalent schizophrenia cases by year and region, 1990 and 2016.
East Asia experienced the largest absolute increase in prevalent cases from approximately 4.9 million cases in 1990 to 7.2 million cases in 2016. However, the largest percentage increases over the 1990 to 2016 period took place in Eastern sub-Saharan Africa (126%) and North Africa/Middle East (128%). These increases were attributable to the significant population growth during this period. Prevalent cases by country and year can be found in supplementary table S2).
Burden of Disease Estimates
The schizophrenia burden, as estimated by GBD 2016, is attributed to a disability-associated burden (ie, YLDs). Schizophrenia contributes 13.4 (95% UI: 9.9–16.7) million YLDs to burden of disease globally, equivalent to 1.7% of total YLDs globally in 2016.
As with prevalence, the peak disease burden is observed at around 30–40 years of age. A comparable burden is seen in males and females. DALYs by country and region for 2016 can be found in the supplementary table S3.
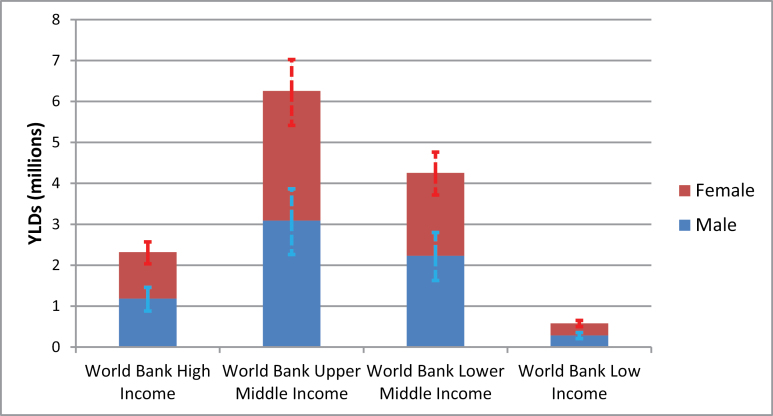
Observing differences in DALYs according to income status demonstrates that the large burden of schizophrenia experienced in lower- and upper-middle income countries is around 4 times the burden experienced by high-income countries (figure 5). This is largely attributable to the burgeoning populations of low- and middle-income countries.
Fig. 5.
Absolute years of life lived with disability (with 95% uncertainty interval) for schizophrenia by World Bank income group, 2016.
Discussion
This study estimates that 21 million people are living with schizophrenia, globally, and this figure is set to continue to rise with population ageing and growth. The majority of these people live in low- and middle-income countries, coinciding with the highest treatment gaps of around 90% in most low- and middle-income countries.28
Saha et al5 found 132 prevalence studies that met their inclusion criteria. Our study had more stringent inclusion criteria (eg, prevalence estimates were required to be representative of the general population, rather than from clinical samples) but included the full range of epidemiological parameters (prevalence, incidence, remission, and mortality) and found 129 studies, 64 of which were studies reporting prevalence. Saha et al5 found a pooled mean point prevalence of 0.60% (SD 0.6); our study estimates were significantly lower at 0.28% but with narrow uncertainty (95% UI: 0.24–0.31); however, comparisons with our findings are difficult due to methodological differences.
Our study draws attention to the lack of high quality, representative data available on the epidemiology of schizophrenia. Very limited data meeting our inclusion criteria were found in low- and middle-income countries. High-quality studies of low prevalence disorders are very challenging to conduct, particularly in resource constrained settings. DisMod-MR 2.1 is able to impute estimates for countries with missing data until such a time countries are able to conduct prevalence surveys. Although schizophrenia is a low prevalence disorder, the burden of disease is undeniably substantial. Our modeling shows that age-specific prevalence remains largely consistent over time and across countries, and significant population growth and ageing has led to a large and increasing disease burden attributable to schizophrenia, particularly for middle income countries. The early onset of the disorder, the low remission rates and the high disability weights all contribute to excessive burden associated with this disorder.
A few countries demonstrated notable differences. Age-standardized prevalence and YLD rates attributable to schizophrenia were significantly higher in China than the global average. Earlier iterations of GBD,29 and community-based surveys30–32 have also estimated higher prevalence and burden of schizophrenia in China, suggesting this finding may not be driven by variation in study methodology by location. Within the European region, The Netherlands demonstrated higher prevalence, a finding supported by both prevalence and incidence studies within our dataset. Like Saha et al,5 we also found lower prevalence estimates from the least developed countries.
Consistent with the systematic review by Saha et al,5 we also found no apparent sex difference in prevalence. One notable exception of this is the lower prevalence of schizophrenia among males compared to females in China. The higher suicide rate among males with schizophrenia in China may partially contribute to the reversed sex effect seen in China relative to other global regions.33 Previous research suggests that women develop schizophrenia later than men34; however, this was not observed in our models. The availability of more age- and sex-specific data points is needed to inform these patterns. The disability measured in GBD captures the morbidity attributable to schizophrenia. Schizophrenia is also associated with significant impairments in psychosocial function; people with schizophrenia are more likely to be unemployed, homeless, living in poverty, having difficulties keeping up with household and self-care tasks, and relying on ongoing support from family carers and available mental health services. The largest burden from schizophrenia is in the 25–54 year age group, where individuals are most likely to be economically productive. This results in significant economic deficits due to losses in productivity by individuals and their families, out-of-pocket costs for treatment, and considerable burdens on health and welfare systems.35
Limitations
The most significant limitation in this study was the sparsity of data, particularly in low- and middle-income countries. There may have been insufficient data to capture true variations across geography, sex, and time. There is a need for more epidemiological research on schizophrenia to inform and improve future burden of disease estimates, including more data to inform the disability weights and health states for schizophrenia. Further limitations related to the GBD studies have been discussed elsewhere.8
A limitation of GBD 2016 is that it did not attribute any cause-specific deaths to, and thus no YLLs were estimated for, schizophrenia. This is due to the relative absence of schizophrenia being coded as the primary cause of death on medical certificates within vital registration systems. The causes of premature mortality of those suffering from schizophrenia are typically coded to injuries (eg, suicide) or other health conditions (eg, cardiovascular disease). However, it is well established that there is a substantial life expectancy gap between people living with schizophrenia and the general population, and it would be wrong to interpret GBD findings as suggesting the absence of premature mortality due to schizophrenia and its comorbidities. The majority of the premature mortality is due to higher rates of comorbid physical health conditions, such as heart disease and respiratory disease.36 As discussed earlier, the psychosocial and economic burdens of schizophrenia are also not captured in the disability weights used in GBD.
Implications
Improved nutrition, reproductive health, and control of communicable disease have resulted in significant demographic changes, causing an increase in the relative contribution of noncommunicable disease to the global disease burden.9 This is leading to an increase in the burden from mental disorders, including schizophrenia. Health systems in low- and middle-income countries need to prepare for this increase but existing evidence-based interventions have been poorly implemented, with only 31% of people with schizophrenia accessing treatment in low- and middle-income countries, where the overall mental disorders treatment gap is as high as 89%.37 This calls for an urgent scaling up of services to respond to serious mental disorders such as schizophrenia.
Conclusion
The burden of schizophrenia is increasing globally. Most of the burden is in low- and middle-income countries where infant and childhood mortality has declined, resulting in a greater proportion of the population living to the age group where the risk of schizophrenia is greatest. Health systems in most countries are unprepared for this escalating burden and without action to scale-up services, a lack of effective treatment for this debilitating mental disorder will critically impact individuals and their families.
Supplementary Material
Supplementary data are available at Schizophrenia Bulletin online.
Funding
F.J.C. is supported by an Australian National Health and Medical Research Council (NHMRC) Early Career Fellowship (APP1138488). A.F. is supported by an Australian National Health and Medical Research Council (NHMRC) Early Career Fellowship (APP1121516). E.S. is supported by an Australian National Health and Medical Research Council (NHMRC) Early Career Fellowship (APP1104600). Prof. McGrath received a John Cade Fellowship APP1056929 from the National Health and Medical Research Council and Niels Bohr Professorship from the Danish National Research Foundation. JGS is supported by a National Health and Medical Research Council Practitioner Fellowship Grant APP1105807.
References
- 1. Jääskeläinen E, Juola P, Hirvonen N et al. . A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull. 2012;39:1296–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014;10:425–448. [DOI] [PubMed] [Google Scholar]
- 3. Charlson FJ, Baxter AJ, Dua T, Degenhardt L, Whiteford HA, Vos T. Excess mortality from mental, neurological and substance use disorders in the Global Burden of Disease Study 2010. Epidemiol Psychiatr Sci. 2015;24:121–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time?Arch Gen Psychiatry. 2007;64:1123–1131. [DOI] [PubMed] [Google Scholar]
- 5. Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2:e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Murray C, Lopez AD, Jamison DT. The global burden of disease in 1990: summary results, sensitivity analysis and future directions. Bull World Health Organ. 1994;72:495. [PMC free article] [PubMed] [Google Scholar]
- 7. Mathers C, Fat DM, Boerma JT.. The Global Burden of Disease: 2004 Update. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 8. Hay SI, Abajobir AA, Abate KH et al. . Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1260–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vos T, Abajobir AA, Abate KH et al. . Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). 4th ed., revised. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 11. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders. Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
- 12. McGrath J, Saha S, Welham J, El Saadi O, MacCauley C, Chant D. A systematic review of the incidence of schizophrenia: the distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Med. 2004;2:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stevens GA, Alkema L, Black RE et al. ; GATHER Working Group. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. PLoS Med. 2016;13:e1002056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kruijshaar ME, Barendregt J, Vos T, de Graaf R, Spijker J, Andrews G. Lifetime prevalence estimates of major depression: an indirect estimation method and a quantification of recall bias. Eur J Epidemiol. 2005;20:103–111. [DOI] [PubMed] [Google Scholar]
- 16. Moffitt TE, Caspi A, Taylor A et al. . How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med. 2010;40:899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Simon GE, VonKorff M. Recall of psychiatric history in cross-sectional surveys: implications for epidemiologic research. Epidemiol Rev. 1995;17:221–227. [DOI] [PubMed] [Google Scholar]
- 18. Susser E, Shrout PE. Two plus two equals three? Do we need to rethink lifetime prevalence? A commentary on ‘How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment’ by Moffitt et al. (2009). Psychol Med. 2010;40:895–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Flaxman A, Murray C, Vos T, eds. Integrated Meta-Regression Framework for Descriptive Epidemiology. Seattle, WA: University of Washington Press; 2015. [Google Scholar]
- 20. Global Burden of Disease Study Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vos T, Flaxman AD, Naghavi M et al. . Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ferrari AJ, Saha S, McGrath JJ et al. . Health states for schizophrenia and bipolar disorder within the Global Burden of Disease 2010 Study. Popul Health Metr. 2012;10:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Salomon JA, Vos T, Hogan DR et al. . Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2012;380:2129–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Haagsma JA, Maertens de Noordhout C, Polinder S et al. . Assessing disability weights based on the responses of 30,660 people from four European countries. Popul Health Metr. 2015;13:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Salomon JA, Haagsma JA, Davis A et al. . Disability weights for the Global Burden of Disease 2013 study. Lancet Glob Health. 2015;3:e712–e723. [DOI] [PubMed] [Google Scholar]
- 26. Burstein R, Fleming T, Haagsma J, Salomon JA, Vos T, Murray CJ. Estimating distributions of health state severity for the global burden of disease study. Popul Health Metr. 2015;13:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wang H, Naghavi M, Allen C et al. . Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Demyttenaere K, Bruffaerts R, Posada-Villa J et al. ; WHO World Mental Health Survey Consortium. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–2590. [DOI] [PubMed] [Google Scholar]
- 29. Murray C, Lopez AD.. Global Health Statistics: A Compendium of Incidence, Prevalence, and Mortality Estimates for over 200 Conditions. Cambridge: Harvard University Press; 1996. [Google Scholar]
- 30. Cooper J, Sartorius N. Mental disorders in China. Glasgow: Gaskell; 1996. [Google Scholar]
- 31. Liu T, Zhang L, Pang L, Li N, Chen G, Zheng X. Schizophrenia-related disability in China: prevalence, gender, and geographic location. Psychiatr Serv. 2015;66:249–257. [DOI] [PubMed] [Google Scholar]
- 32. Zhang W, Shen Y, Li S et al. . Epidemiological survey on mental disorders in 7 areas in China. Chin J Psychiatry. 1998;31:69–71. [Google Scholar]
- 33. Phillips MR, Yang G, Li S, Li Y. Suicide and the unique prevalence pattern of schizophrenia in mainland China: a retrospective observational study. Lancet. 2004;364:1062–1068. [DOI] [PubMed] [Google Scholar]
- 34. Mueser KT, McGurk SR. Schizophrenia. Lancet. 2004;363:2063–2072. [DOI] [PubMed] [Google Scholar]
- 35. Knapp M, Mangalore R, Simon J. The global costs of schizophrenia. Schizophr Bull. 2004;30:279–293. [DOI] [PubMed] [Google Scholar]
- 36. Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. Lancet Psychiatry. 2017;4:295–301. [DOI] [PubMed] [Google Scholar]
- 37. Lora A, Kohn R, Levav I, McBain R, Morris J, Saxena S. Service availability and utilization and treatment gap for schizophrenic disorders: a survey in 50 low- and middle-income countries. Bull World Health Organ. 2012;90:47–54, 54A. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The systematic review found a total of 129 individual data sources which could be included in the DisMod modeling for GBD 2016. These included 64 prevalence, 37 mortality, 5 remission, and 30 incidence studies from 106 geographical locations (including both national and subnational locations) giving a total of 756 individual data points (supplementary table S1). Much of epidemiological data came from high income countries—notably, Denmark, Japan, and Sweden (figure 1). China and India also had a relatively high amount of epidemiological data representative at the provincial-level; however, data from other low- and middle-income countries was very sparse (figure 1). Further details of input data sources can be found online at http://ghdx.healthdata.org/gbd-2016/data-input-sources.
Fig. 1.
Map of epidemiological data points by global burden of disease region.