Abstract
Impairments in social cognition are key determinants of poor functioning in psychosis and an important new target for treatment development. Initial studies support the feasibility and efficacy of training interventions for social cognition, but have been small and have had substantial methodological limitations. This report describes the largest rigorously controlled study of a social cognitive treatment to date. We evaluated the efficacy of a refined version of the 24-session Social Cognitive Skills Training (SCST) program, and whether adding in vivo training sessions in community settings would enhance generalization to functional improvements. One hundred thirty-nine outpatients with psychotic disorders were randomly assigned to one of 3 time- and format-matched conditions: (1) SCST plus in vivo community-based training, (2) SCST plus clinic-based training, or (3) Illness management control condition. SCST targeted the domains of emotion processing, social perception, attributional bias, empathy, and mentalizing. Assessments of social cognition, nonsocial cognition, symptoms, and functioning were completed at baseline, mid-treatment, posttreatment, and 3-month follow-up. On the primary social cognitive outcome measures, there was significant, durable SCST-related improvement in facial emotion identification. There was also a significant SCST benefit for emotional intelligence and an in vivo training effect for empathy, though these improvements were not durable. Further, there were no overall or in vivo-related changes in functioning. This study bolsters and extends support for the efficacy of SCST in a relatively large and rigorously controlled trial, although our effort to enhance generalization to functional improvements through in vivo community-based training was not successful.
Keywords: schizophrenia, psychosocial treatment, facial emotion identification, emotion processing
Introduction
Recovery-oriented treatments for schizophrenia and related psychotic disorders have increasingly focused on social cognition. Social cognition refers to mental operations that underlie social interactions, including perceiving, interpreting, managing, and generating responses to socially relevant stimuli.1 People with psychotic disorders show substantial impairments across the 4 social cognitive domains of emotion processing (particularly facial affect perception), social cue perception, attributional style, and mentalizing.2 More recent evidence indicates that these impairments extend to a fifth domain of empathy,3 which refers to the ability to share, understand, and respond to emotions of others. In relation to nonsocial neurocognitive deficits, social cognitive impairments are more strongly related to community functioning and appear to be more proximal (ie, act as a mediator) to functioning.4,5 These characteristics make social cognition a particularly attractive treatment target.
Several research groups have developed interventions specifically designed to improve multiple domains of social cognition. Kurtz et al6 reviewed 16 initial studies of such treatments and reported encouraging results. Most studies assessed affect perception and mentalizing, with large and medium treatment-related improvements, respectively. This review reinforced the importance of developing interventions for social cognition for psychosis, but it also demonstrated considerable variability in the methods and quality of the included studies. In particular, studies have been small (typically less than 20 per condition), several did not include randomized assignment and/or an active control comparison condition, few have examined durability of treatment benefits, and generalization to functioning was often not considered (see7 for further discussion of limitations).
We report here the largest well-controlled study of a comprehensive social cognitive intervention to date. Specifically, we evaluated the efficacy of a refined version of the Social Cognitive Skills Training (SCST) program we have developed,8–11 which includes separate modules targeting the 5 social cognitive domains described above. Primary outcome measures were selected to assess impact on each of these domains. Based on prior trials of SCST,8–11 we expected the strongest effects on emotion processing (particularly facial affect perception) but also evaluated whether benefits of the revised SCST program extended to the other domains. Secondary outcomes included neurocognition, symptoms, and functioning. Durability was assessed at 3-months posttreatment. In addition, we addressed the issue of generalizability by evaluating whether adding an in vivo training component to SCST led to additional improvements in functioning.
Methods
Subjects
One hundred thirty-nine participants were recruited from outpatient clinics at the VA Greater Los Angeles Healthcare Center and local community mental health facilities. All patients met DSM-IV criteria for schizophrenia (n = 108), schizoaffective disorder (n = 15), or psychosis NOS (n = 16) (not secondary to substance use disorder) as determined by medical records and consultation with treating psychiatrists. Subjects were clinically stable (no psychiatric hospitalizations in the past 2 mo, same antipsychotic medication for the past 6 wk). Exclusion criteria were evidence of current or past neurological disorder (eg, epilepsy), IQ < 70, or substance use disorder within the past month. Medication types and dosages were not controlled and were left to the discretion of subjects’ treating physicians.
Design
The 139 participants were recruited in groups of 6 to 8 and these groups were assigned to one of 3 twelve-week group-based interventions using a randomized permuted block design (see supplementary material for Consort diagram): “SCST-in vivo (n = 41); “SCST-Clinic” (n = 49); “Control” (n = 49). The groups did not differ in terms of diagnoses (X2 (4,139) = 1.81, P = .77). During the first 6 weeks all participants completed 2 one-hour sessions/wk and during the second 6 weeks all participants completed 3 one-hour sessions/wk. The curricula and location for the sessions for the 3 intervention groups were as follows: (1) SCST-in vivo = 24 SCST sessions in the clinic plus 6 sessions (1/wk during the second 6 wk) of training in the community, (2) SCST-Clinic = 24 SCST sessions plus 6 sessions (1/wk during the second 6 wk) of practice in the clinic, (3) Control = 30 sessions of Illness management training in the clinic (1 extra session/wk during the second 6 wk). All sessions were led by 2 co-facilitators, who were postdoctoral fellows in psychology or experienced bachelor’s-level clinicians.
Assessments of primary social cognitive outcome variables, and secondary measures of neurocognition, symptoms, and functioning were conducted at baseline (0 wk), mid-point (6 wk), end-point (12 wk), and follow-up (24 wk). Assessors were blind to treatment condition. The numbers of participants who completed assessments at each of the 4 time points were: SC-in vivo: 41, 41, 39, 38; SC-Clinic: 47, 47, 46, 41; Control: 47, 45, 45, 44. Written informed consent was obtained from all study participants. Participants received compensation after each session and assessment ($12/h).
Interventions
The intervention approaches (except for the in vivo component) have been presented elsewhere8–11 and are briefly described here (see supplementary material for further detail and fidelity monitoring procedures).
SCST Program.
The training approach incorporates several skill-building strategies that are widely used in psychiatric rehabilitation including: (1) breaking down complex social cognitive processes into their component skills, (2) initially teaching/training skills at the most fundamental level and gradually increasing complexity of skill acquisition, and (3) automating these skills through repetition and practice. All sessions are accompanied by slide presentations and structured to include a brief review of previously covered material, didactic presentation of new material, and interactive practice and training exercises. A partly new and expanded set of training stimuli were employed, including photos, audio clips, written vignettes, and a set of audio-visual training materials that we developed using professional actors. New interactive training activities and games were also included.
The program includes 5 modules: (1) Emotion processing: defining basic emotions, identifying them on the face, and identifying social situations/contexts in which they are commonly experienced; (2) Social perception: identifying vocal and bodily expressions of emotion, nonverbal gestures, and social norms; (3) How emotions color our social interpretations: this module draws heavily on the attributional bias curriculum from Penn et al12 and focuses on distinguishing between useful suspiciousness vs harmful suspiciousness, distinguishing among facts, guesses, and feelings, and avoiding “jumping to conclusions”; (4) Understanding others’ emotions: this new module focuses on emotional empathy and perspective taking, including understanding how others are feeling and using this understanding to communicate more effectively; and (5) Understanding others’ intentions: the final module integrates all of the social cues covered in the first 4 modules to help participants make better inferences about others’ beliefs. Training focuses on distinguishing among sincerity, sarcasm, and lying to be kind.
SCST in vivo.
During the second half of the SCST program, participants in this condition completed an additional 1 h/wk of training activities in community settings. We chose to initiate the community-based work during session 7 because the in vivo sessions build on skills gained in the SCST training, and participants had covered half of the curriculum by this point. Two sessions were held individually and 4 sessions were held in a small group of 3–4 participants. Building on an established in vivo amplified social skills training manual,13 the objective was to provide participants with the opportunity to practice social cognition in familiar community settings with a skillful trainer to guide them. The sessions occurred in pre-specified locations (eg, coffee shop, cafeteria, mall) and followed a structured set of activities with corresponding worksheets.
SCST Clinic.
During the second half of SCST, participants in this condition completed an additional 1 h/wk of activities in the clinic. These consisted of the same practice activities and interactive games used in the main SCST sessions, but the specific training stimuli differed. The sessions consisted of an equal amount of activities from each of the 5 SCST modules.
Control Condition.
Illness Management Skills Training exercises included selections from the UCLA Social and Independent Living Skills Program14 plus material on nutrition and relaxation. We excluded role-play and other exercises that directly target social skill building due to concerns that the nature of these exercises could influence social cognitive test performance. Patients in this condition completed a 34-item pre- and post-intervention knowledge quiz. Scores significantly improved from pre- (M = 23.8, SD = 5.8) to posttreatment (M = 27.4, SD = 5.4) (t[43] = 5.97, P < .001) suggesting that participants were engaged and learning.
Treatment Quality Control and Fidelity Monitoring.
The study trainers met with one of the PIs for bi-weekly supervision. In addition, 2 sessions for each cohort were attended by one of the PIs to assess fidelity to the treatment protocol. For each attended session, trainers were rated on the following 6 training components on a scale from 0 (not at all) to 4 (very much): introducing content material, participant involvement, use of educational materials, use of corrective feedback, breaking down exercises into simple components, and repetitive practice. The ratings were uniformly high with means greater than 3.56 across all 6 training components for each of the 3 treatment conditions, indicating good adherence to the protocols.
Assessments
The test battery and dependent variable for each task is presented in table 1. Primary social cognition outcomes included 2 measures for emotion processing and one for each of the 4 other domains. The stimuli in these tasks never appeared during the training sessions. Secondary outcome measures assessed neurocognition, symptoms, and functioning.
Table 1.
Summary of Primary and Secondary Outcome Measures
| Domain | Task | Task Description | Dependent Variable |
|---|---|---|---|
| Primary social cognition measures | |||
| Emotion processing | Facial Emotion Identification Task34 | Participants view a series of faces (not used in training) and select the label that matches from a list of 6 emotions (happy, sad, angry, afraid, disgust, surprise; the same 6 emotions targeted in the training). Eight digitized photos of facial expressions for each of the 6 emotions plus neutral expressions were included (total of 56 images). | Total correct |
| The Mayer-Salovey- Caruso Emotional Intelligence Test 2.035 | Consists of 141 items and 8 ability subscales, which assess 4 components (branches) of emotional processing that each includes 2 subscales: (1) Identifying Emotions, (2) Using Emotions (to facilitate cognition), (3) Understanding Emotions, and (4) Managing Emotions. Responses include 5-point Likert ratings with specific anchor points for some items and a 5-item multiple-choice format for others. MSCEIT total scores were derived using the general consensus approach based on a large community sample. | Total scaled score | |
| Social perception | Half-Profile of Nonverbal Sensitivity (PONS)36 | The 110 scenes in this videotape-based measure last 2 seconds each and contain facial expressions, voice intonations, and/or bodily gestures of a Caucasian female. After watching each scene, participants select which of 2 labels (eg, saying a prayer; talking to a lost child) better describes a situation that would generate the social cue(s). | Total correct |
| Attributional bias | Ambiguous Intentions Hostility Questionnaire (AIHQ)37 | Participants read a series of 5 vignettes describing ambiguous social situations and answer questions about the intentions of the characters and how subjects themselves would respond to the situation. The AIHQ contains Hostility and Aggression bias scores, which were independently scored by 2 blinded raters (intraclass correlation coefficient’s [ICC] for both bias scores were > .85), along with a composite “Blame” score (average of Intentionality, Anger, and Blame item ratings; higher scores reflect more bias). | Average score (of Hostility, Aggression, and Blame subscores) for 5 ambiguous vignettes. |
| Empathy | Empathic Accuracy test38 | Participants watch 9 video clips (2.0–2.5 min each) of people discussing positive or negative autobiographical events and provide continuous ratings (via button presses on a keyboard) of how positive or negative they believe the individual (“target”) is feeling throughout the clip using a 9-point scale from 1 (extremely negative) to 9 (extremely positive). For each clip the correlation between the participant’s ratings of the targets’ emotions and the targets’ ratings of their own emotions is computed (in 2-s segments). This measure was added after the study began and was completed by 98/135 participants. | Mean correlation across clips |
| Mentalizing | The Awareness of Social Inference Test (TASIT) – Parts 2 and 339 | Participants watch a series of videotaped vignettes that depict people interacting and answer 4 types of questions about what a person in the conversation: (1) believes or knows, (2) means, (3) intends; and (4) feels. Part 2 (social inference – minimal) assesses understanding using cues such as tone of voice and facial expression in 15 vignettes that involve sincere and sarcastic exchanges. Part 3 (social inference – enriched) assesses the ability to use contextual knowledge (visual and verbal), in addition to voice and face cues, to derive meaning from the conversation. It includes 16 vignettes and in each there is an untrue comment presented as either sarcasm or as a lie. | Average score from Parts 2 and 3 |
| Secondary outcome variables | |||
| Neurocognition | MATRICS Consensus Cognitive Battery (MCCB)40 | Assesses 6 domains of neurocognition: speed of processing, attention/vigilance, working memory, verbal learning, visual learning, reasoning and problem solving (social cognition domain was not included). | Composite score, based on the average of t-scores from the 6 domains. |
| Symptoms | Brief Psychiatric Rating Scale (BPRS)41 | 24-item structured interview that assesses a broad range of psychiatric symptoms on a scale from 1 to 7. We computed average scores for positive symptom, negative symptom, depression/anxiety, and agitation subscales, and the total score (sum of 24 items). | 4 subscale scores and total score |
| Functional capacity | UCSD Performance- based Skills Assessment (UPSA)42 | Role-play tests with props that are administered as simulations of events in the areas of general organization, finance, social/communications, transportation, and household chores. | Overall summary score |
| Maryland Assessment of Social Competence (MASC)43 | A measure of ability to solve common problems in an interpersonal context that consists of four 3-min role play scenarios. One scene involves initiating a conversation with a casual acquaintance, 2 involve negotiation and compromise, and one involves standing up for one’s rights. The interactions were videotaped and subsequently scored by specially trained raters who achieved reliability standards (ICC > .95) with a gold-standard rater. | Overall effectiveness rating | |
| Real-world functioning | Role Functioning Scale (RFS)44 | An interviewer-rated scale that measures 4 domains of functioning: work/school productivity, independent living, family contact, and social network. Ratings of 1 (severely limited functioning) to 7 (optimal functioning) for each domain are based on a comprehensive semi-structured interview. | Average of 4 subscales |
Tolerability Ratings
At study completion, participants provided ratings (1 [not at all] to 10 [very much]) of their perceptions of how much they enjoyed the treatment, how enthusiastic and knowledgeable they found the trainers, and how effective the training was in helping them deal with daily life and their symptoms.
Data Analysis
Preliminary analyses examined the 3 treatment groups for baseline differences on demographic characteristics and attendance levels to determine whether these factors needed to be included as covariates, as well as checking for baseline differences on the outcome measures. The primary analyses evaluated treatment effects for the 5 social cognitive outcome variables, which were selected to provide adequate coverage of the main domains targeted by SCST. While prior studies strongly suggested that the SCST effect would be largest for the domain of emotion processing, we designed the SCST-in vivo condition with the intention of obtaining stronger and broader treatment effects for the other targeted social cognitive domains. Given the novelty of the in vivo approach and our interest in each domain, we report the results with unadjusted P-values. We also report whether significant results survive correction for multiple comparisons across the 5 domains using a Bonferroni adjustment (P < .01), although Bonferroni correction is likely overly conservative because the social cognitive outcome variables are not independent of each other. Analyses of the secondary outcome variables were corrected for multiple comparisons using a Bonferonni adjustment (P < .006). Effect sizes are given using Cohen’s ƒ2 which indexes explained variability; values of 0.02, 0.15, and 0.35 are termed small, medium, and large, respectively.
We first examined efficacy by evaluating group differences in the longitudinal trajectories of the primary social cognitive outcomes over the intervention period using generalized linear mixed models (GLMMs). The GLMM provides a powerful approach to dealing with missing data as it allows unbiased parameter estimates even when including cases with incomplete data as long as the data are missing completely at random (MCAR15,16). Typically, evaluating group differences in longitudinal trajectories would include group (SCST-Clinic, SCST-in vivo, control) as the between-subjects factor, time (0, 6, 12 wk) as the within-subjects factor, and a group by time interaction, along with subject level random intercepts to account for the correlations induced by the repeated measurements. However, in our design the 2 SCST groups received the same curriculum over the first 6 weeks. To account for this overlap, we instead parameterized the model with only 2 levels for group (SCST or not) and a separate main-effect indicator for the “in vivo” component of the training which was active only at the week 12 time point. In this way, the group by time interaction evaluates whether SCST training improves performance relative to the control condition (ie, “SCST Effect”) over the full treatment period while the indicator term corresponds to the additional impact of community-based practice at 12 weeks (ie, “in vivo Effect”) and hence measures whether the outcomes for the 2 SCST groups diverge over the second half of the intervention. A significant result for either of these model components would indicate a differential treatment effect.
We next considered durability of treatment effects for those social cognition variables that showed significant SCST or in vivo effects. First, durability analyses examined the trajectories of change from 12 to 24 weeks and used the standard 3-group by time modeling structure since by follow-up the groups had all received separate curricula. Significant main effects of time or group by time interactions would indicate overall or relative lack of durability, respectively. Follow-up contrasts, corresponding to the average change from end-point to follow-up, were used to evaluate degree of maintenance for each treatment condition. Second, we evaluated the trajectories of change between 0 and 24 weeks using the same analytic approach. These analyses indicate whether scores remained significantly improved at follow-up relative to baseline levels.
Efficacy and durability of treatment for the secondary outcome measures, including the symptom, neurocognitive, and functioning measures, were assessed using the same analytic strategy outlined above for the primary outcomes. Finally, tolerability ratings were examined with 1-way ANOVAs.
Results
Preliminary Analyses
There were no significant differences between the groups on demographic characteristics with the exception of gender (table 2) for which there was a higher proportion of women in SC-Clinic compared to the other conditions. However, there were no baseline sex differences on any outcome measure, so we did not adjust for gender in subsequent models. The patients were generally chronically ill. There were no significant differences in attendance levels (average of about 24/30 sessions), nor were there significant group differences at baseline on any of the primary or secondary outcome variables.
Table 2.
Demographic and Attendance Data for Control (n = 47), SCST-Clinic (n = 47), and SCST-in vivo (n = 41) Groups
| Control | SCST-Clinic | SCST-in vivo | Statistic | |
|---|---|---|---|---|
| Age (y) | 46.7 (10.2) | 48.8 (9.09) | 46.3 (11.3) | F[1,134] = .79 |
| Education (y) | 12.7 (1.7) | 12.3 (2.1) | 12.3 (2.0) | F[1,134] = .92 |
| Age onset (y) | 22.8 (7.4) | 21.6 (7.7) | 20.5 (7.4) | F[1,134] = .96 |
| Sex | ||||
| Male | 36 | 26 | 32 | X2 [2,135] = 7.00* |
| Female | 11 | 21 | 9 | |
| Ethnicity | ||||
| Hispanic | 9 | 13 | 8 | X2 [2,135] = 1.24 |
| Not Hispanic | 38 | 34 | 33 | |
| Race | ||||
| Asian | 1 | 1 | 2 | X2 [8,135] = 2.70 |
| Hawaiian/Pacific Islander | 2 | 1 | 1 | |
| African American | 18 | 15 | 12 | |
| White | 24 | 29 | 25 | |
| More than 1 | 2 | 1 | 1 | |
| Sessions attended | 24.2 (3.4) | 25.0 (4.9) | 23.1 (5.1) | F [2,134] = 2.00 |
Note: SDs appear in parentheses.
P < .05.
Primary Social Cognition Variables
Treatment Effects.
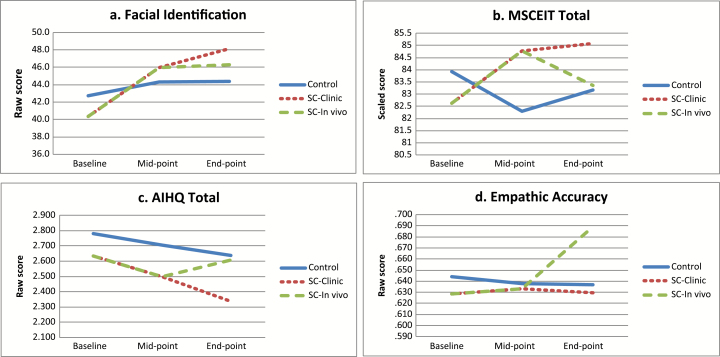
Estimated marginal means, results, and effect sizes are summarized in table 3 (see supplementary table 1 for raw means). For emotional processing, there were significant SCST effects on both outcome measures. As displayed in figure 1a, for facial affect perception, the combined SCST groups demonstrated significantly greater improvement over time than controls. This remained significant even after adjustment for multiple comparisons. There was also a trend-level in vivo effect, reflecting a tendency toward greater improvements in SCST-Clinic vs SCST-in vivo in the second half of the treatment period; this is the opposite of what would be expected although it did not rise to the level of statistical significance.
Table. 3.
Treatment Effects: Primary Social Cognition Measures Across Baseline, Mid-point, and End-point Assessments.

Fig. 1.
Treatment effects: estimated marginal means across baseline, mid-point, and end-point assessments for measures showing significant Social Cognitive Skills Training (SCST) or in vivo effects: (a) Facial identification: SCST effect; (b) Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT): in vivo effect; (c) Ambiguous Intentions Hostility Questionnaire (AIHQ): in vivo effect; (d) Empathic accuracy: in vivo effect.
Similarly, as displayed in figure 1b, the combined SCST groups demonstrated significantly greater improvement on Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT) Total scores over time than controls, though this did not survive correction for multiple comparisons. There was not a significant in vivo effect, although the means were more stable in the SCST-Clinic group than the SCST-in vivo which actually had a small decline during the second half of treatment.
For attributional bias, the results were also somewhat counter-intuitive. Across groups, total AIHQ scores significantly decreased (ie, improved). There was also a significant in vivo effect. However, as shown in figure 1c, scores in the second half of treatment continued to decrease in SCST-Clinic but got worse and returned to baseline levels in SCST-in vivo. The in vivo effect was not significant after multiple comparison correction.
For empathic accuracy, there was no SCST effect (group by time interaction) but there was a significant in vivo effect in the expected direction. As shown in figure 1d, scores for SCST-in vivo group improved but those for the SCST-Clinic group were relatively flat. The in vivo effect was not significant after multiple comparison correction.
Finally, there was a nonsignificant trend for the SCST effect for The Awareness of Social Inference Test (TASIT) Total, with scores tending to improve more in the combined SCST groups than controls. There were no significant treatment effects for the PONS.
Durability.
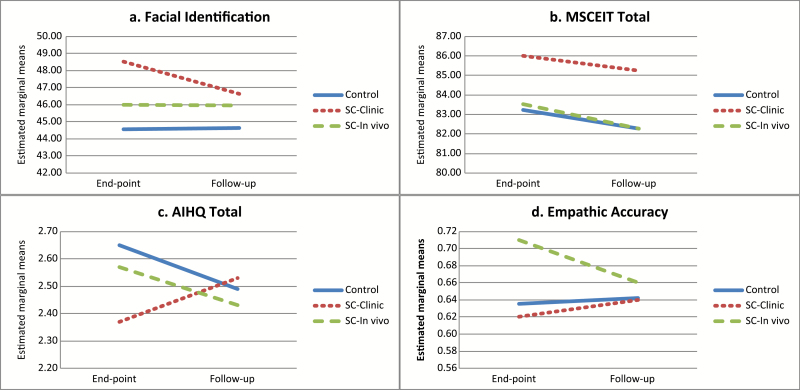
We next evaluated the durability for the 4 social cognitive variables that showed significant treatment effects. For the comparison of 12 to 24 weeks (see figure 2 and supplementary table 2 for full results), there were no overall significant time or group by time effects for posttreatment change, suggesting a general absence of change from end-point to follow-up, although trend-level effects were observed for facial affect identification (time) and AIHQ (interaction).
Fig. 2.
Durability: estimated marginal means across end-point and follow-up assessments for measures showing significant Social Cognitive Skills Training (SCST) or in vivo effects.
For the comparison of 0 to 24 weeks (see supplementary table 3 for full results), with regard to facial affect identification, there were significant time and group by time effects; post hoc analyses indicated that scores were significantly higher (ie, improved) at follow-up vs baseline for both the SCST-Clinic and in vivo groups but not for the Control group. Thus, the significant facial affect identification improvements associated with SCST were relatively durable.
With regard to AIHQ, there was a significant overall time effect indicating that scores were generally lower (ie, improved) at 24 than at 0 weeks across groups; post hoc analyses indicated this was primarily driven by improvement within the Control group. Thus, the overall results indicate that the SCST-Clinic and in vivo groups did not lead to durable improvements in attributional bias. Finally, with regard to the MSCEIT and empathic accuracy, there were no significant time or group by time effects when comparing 0- to 24-week scores. Thus, despite the improvements in these areas during treatment, the changes at follow-up were not significantly above baseline levels.
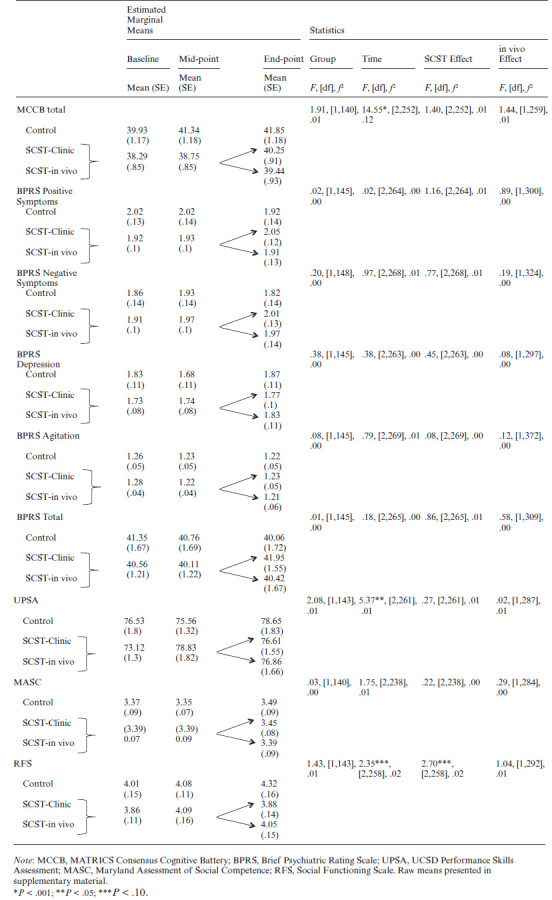
Secondary Outcome Measures
As shown in table 4 (see supplementary table 4 for raw means) there were no significant SCST or in vivo effects for the measures of neurocognition, symptoms, or functioning.
Table. 4.
Treatment effects: Secondary Neurocognition, Symptom, and Functioning Measures Across Baseline, Midpoint, and End-point Assessments.
Tolerability Ratings
Participants reported uniformly high tolerability ratings. Across groups, there were high mean (SD) ratings for how much they liked the groups (9.0 [1.6]), how enthusiastic they considered the trainers (8.9 [1.4]), how well trainers know the material (9.4 [1.1]), how much the treatment helped their daily lives (8.6 [1.7]), and how much the treatment helped with symptoms (8.6 [1.8]). There were no significant between-group differences (supplementary table 5).
Discussion
As in prior studies of SCST, the refined and expanded SCST program was well tolerated. Further, attrition rates were low and fidelity ratings were uniformly high. In this context, there was a robust and relatively durable overall SCST benefit for facial emotion identification. This improvement was not accompanied by any differential between-group changes in neurocognition or symptoms. There was also a significant SCST effect for emotional intelligence and a significant in vivo effect for empathy, though these improvements were less robust and were not durable. Furthermore, there were no overall SCST-related improvements for functioning, and the in vivo group did not show any relative functional improvements. Although this study bolsters and extends evidence for the efficacy of SCST in certain respects, our efforts to enhance functioning were not successful.
We replicated prior findings that SCST improves emotion processing.9–11 The improvement in facial affect perception converges with most prior social cognition treatment studies.6 Somewhat surprisingly, there was a nonsignificant trend for larger improvements for SCST-Clinic vs in vivo in the second half of treatment. The SCST-Clinic group received 6 additional practice sessions that included some exercises similar in content and format to the affect perception outcome measure, and this extra practice may have contributed to this finding.
SCST is the only targeted social cognition intervention to show broad improvement in the area of emotional intelligence.9,17 Notably, although the refined SCST program targets several aspects of emotion processing, the MSCEIT branches extend beyond these areas to processes such as using emotions to enhance cognition and regulating emotions. Thus, the benefits of SCST generalize to areas of emotion processing that are not directly targeted in this treatment.
A key expansion of the SCST program was the addition of a module to address empathy. There was an SCST-in vivo related improvement on an empathic accuracy task, and performance on this task is impaired in schizophrenia and linked to poor functioning.18,19 This improvement converges with a proof of concept study by our group which found that patients who received intra-nasal oxytocin (vs placebo) before each of 12 sessions (including 4 on empathy) of SCST differentially improved empathic accuracy.8 Speculatively, engaging in in vivo training exercises in real-world settings may have contributed to increased sensitivity to others’ emotions. This is consistent with a recent social cognition treatment study that engaged family members or close friends as “practice partners” and found improvement on a different empathy measure.20 Thus, empathy, particularly with adjunctive treatment elements to maximize benefits, is a modifiable treatment target.
This study is one of the few to examine the durability of treatment effects. The results were mixed. The SCST-related treatment effects for facial affect identification were relatively durable, with scores at the 3-month posttreatment follow-up assessment remaining above baseline levels. Notably, there was already some evidence of deterioration for the SCST-Clinic group over the relatively brief follow-up period, and it is unclear whether the apparent benefits would persist over longer intervals. The treatment related effects for emotional intelligence and empathy were not durable as significant improvements were not evident at follow-up compared to baseline scores. The few studies of other interventions have also been mixed, with one reporting retention of gains at a 6-month follow-up in an inpatient forensic sample21 and another reporting no social cognitive gains at either the end of treatment or 3-month follow-up in outpatients.22
Findings for the other 3 social cognitive domains were less clear-cut. For attributional bias, the findings were significant but not in line with our predictions. AIHQ scores improved in the combined study sample as a whole, but the significant in vivo effect reflected a worsening of AIHQ scores during the second half of treatment for SCST-in vivo. Although we have not found improvements on the AIHQ in our prior SCST studies, the recent Kurtz et al review reported an overall improvement in the small to moderate range. It is possible that engaging in real-life interactions in community-based exercises had the effect of confirming patients’ initial attributional biases and consequently moving their AIHQ scores closer to baseline levels. However, the numeric difference between SCST-in vivo vs –Clinic on the AIHQ at 12 weeks was small (.25 on a 5-point scale) and we are reluctant to over interpret this unexpected finding.
For mentalizing, we found only a nonsignificant trend toward SCST-related improvement. Although the Kurtz et al review reported medium-to-large improvements in mentalizing, no prior studies by our group and others that used the TASIT6,23 have reported significant improvements. Finally, for social perception, there were no SCST-related effects. Similar to mentalizing, we have found no improvement in this domain using PONS in our studies, although a few other groups have reported benefits using alternative tasks. These findings highlight the fact that there is currently no widely accepted battery of social cognitive tasks for use in clinical trials (see7 for further methodological critique). Indeed, it is known that many available tests have relatively poor psychometric properties.23–25 Notably, the MSCEIT and empathic accuracy tasks, which showed positive treatment effects, have relatively good psychometric properties,19,26 whereas the PONS, AIHQ, and TASIT have fared less well in psychometric studies.27,28 This key measurement issue is being addressed in the Social Cognition Psychometric Evaluation project.27,28
We did not find evidence for generalization of SCST benefits to improvements in functional capacity or community functioning. Functioning has typically not been a primary outcome in social cognition treatment research, although some smaller studies included various functional measures. Some reported benefits (eg, 20,29) while others reported mixed or null findings (eg, 22,30; see7 for review). Although in vivo community-based training exercises have been found to promote functional improvements in other psychosocial treatments,13 we found no such benefits. Two prior trials that included components designed to enhance generalization (ie, including family members or friends as practice partners) reported positive results for functional capacity31 and other measures of social functioning/quality of life.32 Although neither study was designed to test whether the bridging activities provided any benefit beyond regular treatment, the findings raise the question of optimal dosing. Both studies, as well as recent studies of cognitive remediation with bridging groups,33 devoted more time to these activities than we did. Aside from dosage, several other factors may have contributed to the lack of generalization. First, the content of the sessions may not have adequately matched the skills assessed on our functional outcome measures. For example, improvements in community functioning often require interactions with known (or increasingly familiar) others (eg, succeeding in a job, making and keeping friends), while our in vivo sessions were conducted in public settings with unknown others. Second, more focused assessments of functioning, such as the Ecological Momentary Assessment method, may be more sensitive to functional changes than our outcome measures. Third, in vivo training approaches may be more useful for only certain aspects of social cognition (eg, empathy).
This is the largest rigorously-controlled social cognitive treatment study to date and the results support the efficacy of the SCST approach for certain social cognitive domains. As mentioned above, study limitations include the relatively short follow-up period and the relatively low dose of in vivo sessions. It should be noted that only the SCST-related treatment benefit for facial affect identification survived a conservative Bonferroni correction. In addition, the content and structure of the 6 additional SCST-in vivo and –Clinic sessions differed in several respects, as the in vivo exercises were built around the specific community-based locations where they were held. Further, the generalizability of findings from this chronically ill, predominantly male sample to other populations (eg, recent-onset patients) is unclear. Although evidence for the efficacy of social cognitive interventions is growing and our results extend support in a few key ways, the ultimate goal of such programs is to achieve lasting improvements in functioning. Thus, a critical direction for future research is to develop more effective ways to achieve generalization to the community.
Supplementary Material
Supplementary data are available at Schizophrenia Bulletin online.
Funding
This project was funded by a VA Merit Award (to M.F.G.), the VA Research Enhancement Award Program (REAP) on Enhancing Community Integration for Homeless Veterans, and the Desert Pacific Mental Illness Research, Education, and Clinical Center (MIRECC).
Acknowledgments
M.F.G. has been a consultant to AbbVie, ACADIA, DSP, and Takeda, he is a member of the scientific board for Luc, and he received research funds from Forum. Clinical Trial Registration: www.clinicaltrials.gov; #NCT01267019.
References
- 1. Fiske ST, Taylor SE.. Social Cognition. 2nd ed. New York, NY: McGraw-Hill Book Company; 1991. [Google Scholar]
- 2. Savla GN, Vella L, Armstrong CC, Penn DL, Twamley EW. Deficits in domains of social cognition in schizophrenia: a meta-analysis of the empirical literature. Schizophr Bull. 2013;39:979–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Green MF, Horan WP, Lee J. Social cognition in schizophrenia. Nat Rev Neurosci. 2015;16:620–631. [DOI] [PubMed] [Google Scholar]
- 4. Fett AK, Viechtbauer W, Dominguez MD, Penn DL, van Os J, Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci Biobehav Rev. 2011;35:573–588. [DOI] [PubMed] [Google Scholar]
- 5. Schmidt SJ, Mueller DR, Roder V. Social cognition as a mediator variable between neurocognition and functional outcome in schizophrenia: empirical review and new results by structural equation modeling. Schizophr Bull. 2011;37(Suppl 2):S41–S54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kurtz MM, Gagen E, Rocha NB, Machado S, Penn DL. Comprehensive treatments for social cognitive deficits in schizophrenia: A critical review and effect-size analysis of controlled studies. Clin Psychol Rev. 2016;43:80–89. [DOI] [PubMed] [Google Scholar]
- 7. Horan WP, Green MF. Treatment of social cognition in schizophrenia: Current status and future directions. Schizophr Res. In press. [DOI] [PubMed] [Google Scholar]
- 8. Davis MC, Green MF, Lee J et al. Oxytocin-augmented social cognitive skills training in schizophrenia. Neuropsychopharmacology. 2014;39:2070–2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gohar SM, Hamdi E, El Ray LA, Horan WP, Green MF. Adapting and evaluating a social cognitive remediation program for schizophrenia in Arabic. Schizophr Res. 2013;148:12–17. [DOI] [PubMed] [Google Scholar]
- 10. Horan WP, Kern RS, Tripp C et al. Efficacy and specificity of social cognitive skills training for outpatients with psychotic disorders. J Psychiatr Res. 2011;45:1113–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Horan WP, Kern RS, Shokat-Fadai K, Sergi MJ, Wynn JK, Green MF. Social cognitive skills training in schizophrenia: an initial efficacy study of stabilized outpatients. Schizophr Res. 2009;107:47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Penn DL, Roberts DL, Combs D, Sterne A. Best practices: the development of the Social Cognition and Interaction Training program for schizophrenia spectrum disorders. Psychiatr Serv. 2007;58:449–451. [DOI] [PubMed] [Google Scholar]
- 13. Glynn SM, Marder SR, Liberman RP et al. Supplementing clinic-based skills training with manual-based community support sessions: effects on social adjustment of patients with schizophrenia. Am J Psychiatry. 2002;159:829–837. [DOI] [PubMed] [Google Scholar]
- 14. Liberman RP, Mueser KT, Wallace CJ, Jacobs HE, Eckman T, Massel HK. Training skills in the psychiatrically disabled: learning coping and competence. Schizophr Bull. 1986;12:631–647. [DOI] [PubMed] [Google Scholar]
- 15. Little RJA, Rubin DB.. Statistical Analysis With Missing Data. New York, NY: John Wiley & Sons; 1987. [Google Scholar]
- 16. Verbeke G, Molenberghs G.. Linear Mixed Models for Longitudinal Data. New York, NY: Springer; 2000. [Google Scholar]
- 17. Eack SM, Pogue-Geile MF, Greenwald DP, Hogarty SS, Keshavan MS. Mechanisms of functional improvement in a 2-year trial of cognitive enhancement therapy for early schizophrenia. Psychol Med. 2011;41:1253–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lee J, Zaki J, Harvey PO, Ochsner K, Green MF. Schizophrenia patients are impaired in empathic accuracy. Psychol Med. 2011;28:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Olbert CM, Penn DL, Kern RS et al. Adapting social neuroscience measures for schizophrenia clinical trials, part 3: fathoming external validity. Schizophr Bull. 2013;39:1211–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tas C, Danaci AE, Cubukcuoglu Z, Brüne M. Impact of family involvement on social cognition training in clinically stable outpatients with schizophrenia – a randomized pilot study. Psychiatry Res. 2012;195:32–38. [DOI] [PubMed] [Google Scholar]
- 21. Combs DR, Adams SD, Penn DL, Roberts D, Tiegreen J, Stem P. Social Cognition and Interaction Training (SCIT) for inpatients with schizophrenia spectrum disorders: preliminary findings. Schizophr Res. 2007;91:112–116. [DOI] [PubMed] [Google Scholar]
- 22. Roberts DL, Penn DL. Social cognition and interaction training (SCIT) for outpatients with schizophrenia: a preliminary study. Psychiatry Res. 2009;166:141–147. [DOI] [PubMed] [Google Scholar]
- 23. Fiszdon JM, Roberts DL, Penn DL et al. Understanding Social Situations (USS): a proof-of-concept social-cognitive intervention targeting theory of mind and attributional bias in individuals with psychosis. Psychiatr Rehabil J. 2017;40:12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Green MF, Penn DL, Bentall R et al. Social cognition in schizophrenia: an NIMH workshop on definitions, assessment, and research opportunities. Schizophr Bull. 2008;34:1211–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Davidson CA, Lesser R, Parente LT, Fiszdon JM. Psychometrics of social cognitive measures for psychosis treatment research. Schizophr Res. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Eack SM, Greeno CG, Pogue-Geile MF, Newhill CE, Hogarty GE, Keshavan MS. Assessing social-cognitive deficits in schizophrenia with the Mayer-Salovey-Caruso Emotional Intelligence Test. Schizophr Bull. 2010;36:370–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pinkham AE, Penn DL, Green MF, Buck B, Healey K, Harvey PD. The social cognition psychometric evaluation study: results of the expert survey and RAND panel. Schizophr Bull. 2014;40:813–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pinkham AE, Penn DL, Green MF, Harvey PD. Social cognition psychometric evaluation: results of the Initial Psychometric Study. Schizophr Bull. 2016;42:494–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mazza M, Lucci G, Pacitti F et al. Could schizophrenic subjects improve their social cognition abilities only with observation and imitation of social situations?Neuropsychol Rehabil. 2010;20:675–703. [DOI] [PubMed] [Google Scholar]
- 30. Hasson-Ohayon I, Mashiach-Eizenberg M, Avidan M, Roberts DL, Roe D. Social cognition and interaction training: preliminary results of an RCT in a community setting in Israel. Psychiatr Serv. 2014;65:555–558. [DOI] [PubMed] [Google Scholar]
- 31. Roberts DL, Combs DR, Willoughby M et al. A randomized, controlled trial of Social Cognition and Interaction Training (SCIT) for outpatients with schizophrenia spectrum disorders. Br J Clin Psychol. 2014;53:281–298. [DOI] [PubMed] [Google Scholar]
- 32. Tas C, Danaci AE, Cubukcuoglu Z, Brüne M. Impact of family involvement on social cognition training in clinically stable outpatients with schizophrenia – a randomized pilot study. Psychiatry Res. 2012;195:32–38. [DOI] [PubMed] [Google Scholar]
- 33. Reddy LF, Horan WP, Jahshan C, Green MF. Cognitive remediation for schizophrenia: a review of recent findings. Current Treatment Options in Psychiatry 2014;1:121–133. [Google Scholar]
- 34. Ekman P. Subtle Expression Training Tool (SETT) & Micro Expression Training Tool (METT). In: Paul Ekman, wpc, ed; 2004.
- 35. Mayer JD, Salovey P, Caruso DR, Sitarenios G. Measuring emotional intelligence with the MSCEIT V2.0. Emotion. 2003;3:97–105. [DOI] [PubMed] [Google Scholar]
- 36. Rosenthal R, Hall JA, DiMatteo MR, Rogers PL, Archer D.. Sensitivity to Nonverbal Communication: The PONS Test. Baltimore, MD: Johns Hopkins University Press; 1979. [Google Scholar]
- 37. Combs DR, Penn DL, Wicher M, Waldheter E. The Ambiguous Intentions Hostility Questionnaire (AIHQ): a new measure for evaluating hostile social-cognitive biases in paranoia. Cogn Neuropsychiatry. 2007;12:128–143. [DOI] [PubMed] [Google Scholar]
- 38. Kern RS, Penn DL, Lee J et al. Adapting social neuroscience measures for schizophrenia clinical trials, Part 2: trolling the depths of psychometric properties. Schizophr Bull. 2013;39:1201–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McDonald S, Flanagan S, Rollins J.. The Awareness of Social Inference Test. Suffolk, UK: Thames Valley Test Company, Ltd; 2002. [Google Scholar]
- 40. Nuechterlein KH, Green MF.. MATRICS Consensus Cogntive Battery. Los Angeles, CA: MATRICS Assessment, Inc; 2006. [Google Scholar]
- 41. Kopelowicz A, Ventura J, Liberman RP, Mintz J. Consistency of Brief Psychiatric Rating Scale factor structure across a broad spectrum of schizophrenia patients. Psychopathology. 2008;41:77–84. [DOI] [PubMed] [Google Scholar]
- 42. Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD Performance-Based Skills Assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull. 2001;27:235–245. [DOI] [PubMed] [Google Scholar]
- 43. Bellack AS, Sayers M, Mueser KT, Bennett M. Evaluation of social problem solving in schizophrenia. J Abnorm Psychol. 1994;103:371–378. [DOI] [PubMed] [Google Scholar]
- 44. McPheeters HL. Statewide mental health outcome evaluation: a perspective of two southern states. Community Ment Health J. 1984;20:44–55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.