Abstract
The role of chorioamnionitis (CA) in the development of retinopathy of prematurity (ROP) is difficult to establish, because CA-exposed and CA-unexposed infants frequently present different baseline characteristics. We performed an updated systematic review and meta-analysis of studies reporting on the association between CA and ROP. We searched PubMed and EMBASE for relevant articles. Studies were included if they examined preterm or very low birth weight (VLBW, <1500g) infants and reported primary data that could be used to measure the association between exposure to CA and the presence of ROP. Of 748 potentially relevant studies, 50 studies met the inclusion criteria (38,986 infants, 9,258 CA cases). Meta-analysis showed a significant positive association between CA and any stage ROP (odds ratio [OR] 1.39, 95% confidence interval [CI] 1.11 to 1.74). CA was also associated with severe (stage ≥3) ROP (OR 1.63, 95% CI 1.41 to 1.89). Exposure to funisitis was associated with a higher risk of ROP than exposure to CA in the absence of funisitis. Additional meta-analyses showed that infants exposed to CA had lower gestational age (GA) and lower birth weight (BW). Meta-regression showed that lower GA and BW in the CA-exposed group was significantly associated with a higher risk of ROP. Meta-analyses of studies with data adjusted for confounders could not find a significant association between CA and ROP. In conclusion, our study confirms that CA is a risk factor for developing ROP. However, part of the effects of CA on the pathogenesis of ROP may be mediated by the role of CA as an etiological factor for very preterm birth.
Introduction
Chorioamnionitis (CA) is a major risk factor for preterm birth, especially at earlier gestational age (GA), and a major contributor to prematurity-associated morbidity and mortality [1–6]. The pathogenetic role of CA in the development of adverse outcomes of prematurity, such as bronchopulmonary dysplasia (BPD) [6–8], necrotizing enterocolitis (NEC) [9], patent ductus arteriosus (PDA) [10, 11], neonatal brain injury [12], or cerebral palsy [13], has been addressed in a number of cohort and case-control studies, which have been summarized in systematic reviews. Nevertheless, it is still controversial whether the effects of CA on neonatal mortality and morbidity are related to infection/inflammation or to the role of CA as an etiological factor for very preterm birth [1–6].
Retinopathy of prematurity (ROP) is a vasoproliferative disorder of the developing retina and a leading cause of childhood blindness around the world [14–20]. Prematurity and postnatal oxygen therapy have consistently been associated with ROP [14–21]. However, ROP is a multifactorial disease, and multiple other modifiable clinical factors have been associated with an increased risk of ROP. These include, among others, hypoxia, hypercapnia, hyperglycemia, exposure to blood transfusions, or poor postnatal weight gain [14–19, 22–27]. In addition, recent experimental and clinical data support the hypothesis that multiple hits of antenatal and postnatal infection/inflammation are involved in ROP etiology and progression [16, 28].
The role of CA as a potential pathogenic factor for ROP has already been the subject of a systematic review and meta-analysis [29]. Mitra et al. [29] included 27 studies (10,590 preterm infants) in their review. They found, in unadjusted analyses, that CA was significantly associated with ROP (any stage, summary risk ratio 1.33, 95% confidence interval [CI] 1.14 to 1.55), but that CA was not significantly associated with severe ROP (stage ≥3, summary risk ratio 1.27, 95% CI 0.99 to 1.63) [29]. They also carried out subgroup analysis of studies which did not show a significant difference in GA between the CA-exposed and CA-unexposed groups. In this analysis they could not find a significant association between CA and ROP (risk ratio 0.98, 95% CI 0.77 to 1.26). They concluded that CA could not definitively be considered a risk factor for ROP, and that further studies that adjust for potential confounding factors were required [29].
After the publication of the meta-analysis by Mitra et al. [29], more studies assessing the relationship between CA and ROP have been published. Some of these studies are of high methodological quality and included large infant populations. Therefore, in the present study, we aimed to update the meta-analysis of Mitra et al. [29]. We used an extensive search strategy, which included not only studies describing ROP as an outcome after exposure to CA, but also studies that assessed CA as potential risk factor for ROP. In addition, we analyzed the magnitude of the differences in potential confounders, such as GA, birth weight (BW), rate of sepsis, or exposure to antenatal corticosteroids between the infants of the CA and the control group. Finally, we performed a meta-regression in order to investigate the effect of confounders on the association between CA and ROP.
Methods
The methodology of this study was based on an earlier meta-analysis on the association of CA and PDA [11], and on another meta-analysis on probiotics and ROP [30]. The study was conducted according to the Guidelines for Meta-Analyses and Systematic Reviews of Observational Studies (MOOSE) [31] and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [32]. The study is reported according to the PRISMA checklist (S1 File).
Sources and search strategy
A comprehensive literature search was undertaken using the PubMed/MEDLINE and EMBASE databases from their inception to July 1, 2017. The search terms involved various combinations of the following keywords: “chorioamnionitis”, “intrauterine infection” “intrauterine inflammation”, “antenatal infection” “antenatal inflammation”, “retinopathy of prematurity”, “risk factors”, “outcome”, “cohort”, and “case-control”. The search strategy for PubMed/MEDLINE is described in detail in S1 Table. No language limit was applied. Additional strategies to identify studies included manual review of reference lists from key articles that fulfilled our eligibility criteria and other systematic reviews on CA, use of “related articles” feature in PubMed, and use of the “cited by” tool in Web of Sciences and Google scholar.
Study selection
Studies were included if they examined preterm or very low birth weight (VLBW, <1500g) infants and reported primary data that could be used to measure the association between exposure to CA and the presence of ROP. Therefore, we selected studies describing ROP as outcome after exposure to CA, and studies that assessed CA as a potential risk factor for ROP. Studies were considered for inclusion if they were cohort studies, case control studies or randomized controlled trials with a control arm which met the inclusion criteria. To identify relevant studies, two reviewers (E.V., G.C.) independently screened the results of the searches and applied inclusion criteria using a structured form. Discrepancies were resolved through discussion or consultation with a third reviewer (P.D.).
Data extraction
A team of three investigators (G.C., S.G., G.R.) extracted data from relevant studies using a predetermined data extraction form, and a second team of four investigators (E.V.-M., A.G., O.R., P.D.) checked data extraction for accuracy and completeness. Discrepancies were resolved by consulting the primary report. Data extracted from each study included citation information, language of publication, location where research was conducted, time period of the study, study objectives, study design, definitions of CA and ROP, inclusion/exclusion criteria, patient characteristics, and results (including raw numbers, summary statistics and adjusted analyses on CA and ROP where available). Severe ROP was defined as ROP stage ≥ 3.
Quality assessment
Methodological quality was assessed using the Newcastle-Ottawa Scale for cohort or case-control studies [33]. This scale uses a rating system (range: 0–9 points) that scores three aspects of a study: selection (0–4 points), comparability (0–2 points) and exposure/outcome (0–3 points). Studies were evaluated as though the association between CA and ROP was the primary outcome. Two reviewers (E.V.-M. and E.V.) independently assessed the methodological quality of each study. Discrepancies were resolved through discussion.
Statistical analysis
Studies were combined and analyzed using comprehensive meta-analysis V3.0 software (Biostat Inc., Englewood, NJ, USA). For dichotomous outcomes, the odds ratio (OR) with 95% confidence interval (CI) was calculated from the data provided in the studies. ORs adjusted for potential confounders were extracted from the studies reporting these data. For continuous outcomes, the mean difference (MD) with 95% CI was calculated. When studies reported continuous variables as median and range or interquartile range, we estimated the mean and standard deviation using the method of Wan et al. [34].
Due to anticipated heterogeneity, summary statistics were calculated with a random-effects model. This model accounts for variability between studies as well as within studies. Subgroup analyses were conducted according to the mixed-effects model [35]. In this model, a random-effects model is used to combine studies within each subgroup, and a fixed-effect model is used to combine subgroups and yield the overall effect. The study-to-study variance (tau-squared) is not assumed to be the same for all subgroups. This value is computed within subgroups and not pooled across subgroups. Statistical heterogeneity was assessed by Cochran’s Q statistic and by the I2 statistic, which is derived from Q and describes the proportion of total variation that is due to heterogeneity beyond chance [36]. We used the Egger’s regression test [37] and funnel plots to assess publication bias. To explore differences between studies that might be expected to influence the effect size, we performed univariate random-effects meta-regression (method of moments) [38]. The potential sources of variability defined a priori were: CA type (clinical or histological), differences in GA and BW between the infants with and without CA, use of antenatal corticosteroids, mode of delivery, rate of small for gestational age (SGA), rate of premature rupture of membranes (PROM), rate of preeclampsia, rate of early-onset sepsis (EOS), rate of late-onset sepsis (LOS), and mortality. Additional sensitivity analyses were performed excluding studies that included infants with GA >32 weeks. A probability value of less than 0.05 (0.10 for heterogeneity) was considered statistically significant.
Results
Description of studies
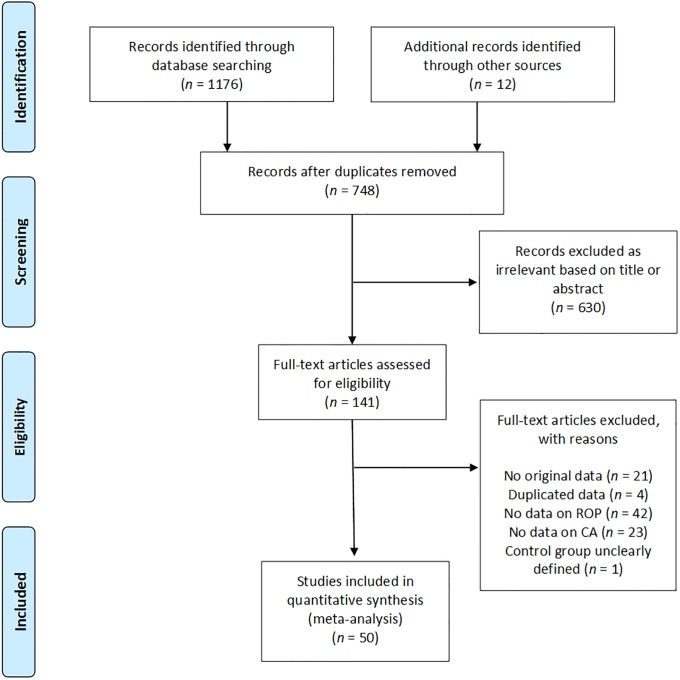
Of 748 potentially relevant studies, 50 met the inclusion criteria [12, 39–87]. The PRISMA flow diagram of the search process is shown in Fig 1. The included studies evaluated 38,956 infants, and included 9258 CA cases, 3251 cases of all stages ROP, and 2720 cases of severe ROP. The included studies and their characteristics are summarized in S2 Table. None of the studies were designed to primarily examine the association between CA and ROP. In 35 studies, the aim was to examine the outcomes, including ROP, of preterm infants with and without maternal CA. Fifteen studies examined the risk factors for ROP, including maternal CA. Nineteen studies used a clinical definition of CA and 26 studies used a histological definition. In two studies [57, 87], ROP was associated with clinical CA and with histological CA separately. In two studies [55, 65], infants were considered to have CA if they had both clinical and histological CA. In the study of Gray et al. [47] infants were assigned to the CA group if they had clinical or histological CA. Finally, 43 of the 50 studies included infants who were at least <32 weeks GA or had a BW <1500g. One study included infants of <33 weeks [68], five studies included infants up to GA 34 weeks [40, 52, 54, 55, 63], and one study included infants of GA <37 weeks [70].
Fig 1. PRISMA flow diagram of search process.
CA: Chorioamnionitis; ROP: retinopathy of prematurity.
Quality assessment
The quality of each study according to the Newcastle-Ottawa Scale is summarized in S2 Table. Most (k = 40) studies received a quality score of 6 or 7 points. Studies were downgraded in quality most frequently for not adjusting the risk of ROP for confounders (k = 42), for not defining ROP clearly (k = 24), and for not defining CA clearly (k = 16).
Analysis based on unadjusted data
As shown in Fig 2, meta-analysis showed a significant positive association between all types CA and any stage ROP. The association remained significant for histological, but not for clinical CA. Excluding studies [40, 54, 63, 70] that included older premature infants (GA 32–37 weeks) did not significantly affect the association between CA and any stage ROP (OR 1.34, 95% CI 1.05 to 1.71). Moreover, as shown in Fig 3, meta-analysis showed a significant positive association between all types CA and severe ROP. The association remained significant for both histological and clinical CA. The study of Soraisham et al. [68] included older infants (up to 33 weeks GA) and its exclusion did not significantly affect the association between CA and severe ROP (OR 1.62, 95% CI 1.39 to 1.89). Three studies reported on ROP stage ≥1, and meta-analysis demonstrated a significant positive association with CA (S1 Fig). This association became non-significant when a study which included infants up to 34 weeks GA [52] was removed from the analysis (OR 1.89, CI 1.06 to 3.29). Finally, as shown in Fig 4, ROP stage 1–2 was not significantly associated with all types CA, clinical CA, or histological CA. Neither visual inspection of the funnel plot nor the regression test of Egger revealed evidence of publication bias in the analyses of all stages ROP, severe ROP, or stage 1–2 ROP (S2 Fig). There were too few studies (k = 3) reporting on stages ≥1 ROP to test for publication bias.
Fig 2. Meta-analysis of chorioamnionitis and risk of any stage ROP.
CA: chorioamnionitis; ROP: retinopathy of prematurity; (c): clinical chorioamnionitis; (h): histological chorioamnionitis.
Fig 3. Meta-analysis of chorioamnionitis and risk of severe ROP (stage ≥3).
CA: chorioamnionitis; ROP: retinopathy of prematurity; (c): clinical chorioamnionitis; (h): histological chorioamnionitis.
Fig 4. Meta-analysis of chorioamnionitis and risk of stage 1–2 ROP.
CA: chorioamnionitis; ROP: retinopathy of prematurity; (c): clinical chorioamnionitis; (h): histological chorioamnionitis.
To explore the possible differences in baseline characteristics between the groups exposed and non-exposed to CA, we performed several additional meta-analyses. As summarized in Tables 1 and 2, infants exposed to CA showed significantly lower GA and BW, significantly lower rates of birth by cesarean delivery, significantly lower rates of SGA, significantly lower rates of preeclampsia, and significantly lower rates of maternal diabetes. Moreover, infants exposed to CA showed significantly higher rates of exposure to antenatal corticosteroids, significantly higher rates of PROM, significantly higher rates of EOS, significantly higher rates of LOS, and significantly higher mortality.
Table 1. Meta-analysis of chorioamnionitis and continuous variables.
| Meta-analysis | CA type | k | Mean difference | 95% CI | Z | p | Heterogeneity | ||
|---|---|---|---|---|---|---|---|---|---|
| Q | p | I2 (%) | |||||||
| Gestational age (weeks) | Clinical | 7 | -0.94 | -1.44 to -0.43 | -3.60 | <0.001 | 158.7 | <0.001 | 96.2 |
| Histological | 9 | -1.42 | -1.85 to -0.99 | -6.53 | <0.001 | 118.6 | <0.001 | 93.3 | |
| Any type | 18 | -1.15 | -1.44 to -0.85 | -7.61 | <0.001 | 312.5 | <0.001 | 94.6 | |
| Birth weight (g) | Clinical | 8 | -19 | -72 to 34 | -0.71 | 0.480 | 127.1 | <0.001 | 94.5 |
| Histological | 19 | -49 | -86 to -11 | 2.57 | 0.010 | 155.5 | <0.001 | 88.4 | |
| Any type | 29 | -34 | -62 to -6 | -2.38 | 0.017 | 294.1 | <0.001 | 90.5 | |
| Maternal age (years) | Any type | 5 | -0.31 | -1.61 to 0.99 | -0.47 | 0.639 | 37.2 | <0.001 | 89.3 |
CA: chorioamnionitis; k: number of included studies. Mean differences represent the mean of the CA-exposed group minus the mean of the CA-unexposed group. Statistically significant mean differences are marked in bold.
Table 2. Meta-analysis of chorioamnionitis and dichotomous variables.
| Meta-analysis | CA type | k | OR | 95% CI | Z | p | Heterogeneity | ||
|---|---|---|---|---|---|---|---|---|---|
| Q | p | I2 (%) | |||||||
| Antenatal Corticosteroids (any dosage) | Clinical | 6 | 1.19 | 0.79 to 1.79 | 0.84 | 0.402 | 73.5 | <0.001 | 93.2 |
| Histological | 18 | 1.28 | 1.00 to 1.64 | 1.96 | 0.050 | 85.3 | <0.001 | 80.1 | |
| Any type | 25 | 1.25 | 1.03 to 1.52 | 2.21 | 0.027 | 162.0 | <0.001 | 85.2 | |
| Cesarean section | Clinical | 7 | 0.33 | 0.19 to 0.57 | -3.93 | <0.001 | 278.3 | <0.001 | 97.8 |
| Histological | 14 | 0.34 | 0.23 to 0.49 | -5.52 | <0.001 | 86.8 | <0.001 | 85.0 | |
| Any type | 22 | 0.34 | 0.26 to 0.45 | -7.33 | <0.001 | 368.3 | <0.001 | 94.3 | |
| Maternal diabetes | Any type | 2 | 0.71 | 0.53 to 0.95 | -2.29 | 0.022 | 0.1 | 0.775 | 0.0 |
| Preeclampsia | Histological | 5 | 0.20 | 0.16 to 0.25 | -13.20 | <0.001 | 1.4 | 0.844 | 0.0 |
| PROM | Clinical | 2 | 5.99 | 2.52 to 14.26 | 4.05 | <0.001 | 5.0 | 0.025 | 80.0 |
| Histological | 9 | 3.37 | 2.21 to 5.16 | 5.61 | <0.001 | 87.6 | <0.001 | 90.9 | |
| Any type | 11 | 3.78 | 2.61 to 5.47 | 7.04 | <0.001 | 99.0 | <0.001 | 89.9 | |
| Small for gestational age | Clinical | 2 | 0.48 | 0.16 to 1.49 | -1.47 | 0.204 | 0.01 | 0.925 | 0.0 |
| Histological | 9 | 0.32 | 0.18 to 0.56 | -4.04 | <0.001 | 90.0 | <0.001 | 91.1 | |
| Any type | 11 | 0.35 | 0.22 to 0.55 | -4.44 | <0.001 | 90.1 | <0.001 | 88.9 | |
| Early onset sepsis | Clinical | 7 | 4.51 | 3.29 to 6.19 | 9.36 | <0.001 | 6.1 | 0.409 | 2.1 |
| Histological | 10 | 3.68 | 2.53 to 5.36 | 6.81 | <0.001 | 21.2 | 0.012 | 57.6 | |
| Any type | 17 | 4.15 | 3.26 to 5.28 | 11.55 | <0.001 | 27.5 | 0.036 | 41.9 | |
| Late onset sepsis | Clinical | 4 | 1.30 | 0.86 to 1.98 | 1.23 | 0.219 | 12.4 | 0.006 | 75.9 |
| Histological | 11 | 1.40 | 1.05 to 1.86 | 2.31 | 0.021 | 75.5 | <0.001 | 86.8 | |
| Any type | 16 | 1.35 | 1.09 to 1.67 | 2.78 | 0.005 | 89.1 | <0.001 | 83.2 | |
| Mortality | Clinical | 7 | 1.66 | 1.26 to 2.18 | 3.65 | <0.001 | 17.1 | 0.009 | 64.9 |
| Histological | 13 | 1.47 | 1.15 to 1.87 | 3.17 | 0.002 | 37.3 | <0.001 | 67.9 | |
| Any type | 21 | 1.52 | 1.25 to 1.85 | 4.15 | <0.001 | 81.1 | <0.001 | 75.3 | |
CA: chorioamnionitis; k: number of included studies; OR: odds ratio; PROM: premature rupture of membranes; SGA: small for gestational age. An OR higher than 1 indicates that CA is a risk factor for the outcome, an OR below one indicates that CA is a protective factor for the outcome. Statistically significant odds ratios are marked in bold.
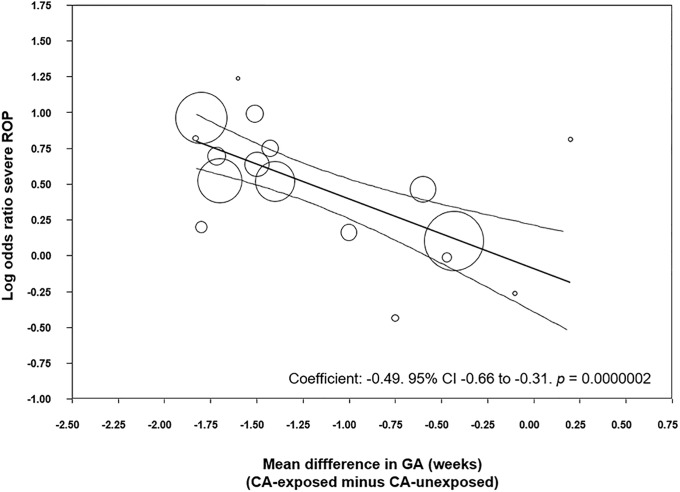
To analyze the possible influence of the GA and BW on the unadjusted association between CA and ROP, we performed meta-regression analyses. These analyses showed that the differences in GA or BW between the CA exposed and non-exposed groups were significantly correlated with the risk of ROP in the CA-exposed group (Table 3). Specifically, we found a significant correlation between an increasing mean difference in GA and a higher CA-associated risk of all stages ROP (Fig 5), stages 1–2 ROP (S3 Fig) and severe ROP (Fig 6). Moreover, we found a significant correlation between an increasing mean difference in BW and a higher CA-associated risk of all stages ROP (S4 Fig), and stages 1–2 ROP (S5 Fig). In contrast, meta-regression could not demonstrate a significant correlation between an increasing MD in BW and a higher CA-associated risk of severe ROP (Table 3).
Table 3. Meta-regression of difference in gestational age and difference in birth weight and risk of ROP.
| ROP stage | Meta-regression | k | Coefficient | 95% CI | Z | p |
|---|---|---|---|---|---|---|
| All stages ROP | Difference in mean GA (per week) |
19 | -0.52 | -0.99 to -0.06 | -2.21 | 0.027 |
| Difference in mean BW (per 100 g) |
19 | -0.34 | -0.68 to -0.01 | -2.04 | 0.042 | |
| Stages 1–2 ROP | Difference in mean GA (per week) |
7 | -0.58 | -0.96 to -0.21 | -3.06 | 0.002 |
| Difference in mean BW (per 100 g) |
7 | -0.36 | -0.57 to -0.15 | -3.39 | 0.001 | |
| Severe ROP (stage ≥3) | Difference in mean GA (per week) |
17 | -0.49 | -0.66 to -0.31 | -5.30 | <0.001 |
| Difference in mean BW (per 100 g) |
16 | -0.03 | -0.22 to 0.16 | -0.29 | 0.774 |
ROP: retinopathy of prematurity; GA: gestational age; BW: birth weight; k: number of included studies; CI: confidence interval
Fig 5. Meta-regression plot of association between chorioamnionitis and all stages ROP controlling for difference in GA between exposed and non-exposed groups.
CA: chorioamnionitis; ROP: retinopathy of prematurity; GA: gestational age.
Fig 6. Meta-regression plot of association between chorioamnionitis and severe ROP (stage ≥3) controlling for difference in GA between exposed and non-exposed groups.
CA: chorioamnionitis; ROP: retinopathy of prematurity; GA: gestational age.
To eliminate the effect of prematurity as a confounding factor, we carried out a meta-analysis of studies where the mean difference in GA was non-significant (p > 0.05). Ten studies met this criterion. As shown in S6 Fig, we could not find a significant association between any type CA and all stages ROP, or any type CA and severe ROP.
In addition, we carried out meta-regression analyses to examine the effect of other covariates on the risk of ROP (S3 Table). We examined the effect of the covariates we predefined on the risk of ROP in the CA-exposed group. We found that an increased risk of EOS in the CA-group significantly correlated with an increased risk of all grades ROP. Moreover, an increased risk of SGA in the CA-group significantly correlated with an increased risk of all grades ROP. Finally, an increased risk of mortality in the CA-group correlated with an increased risk of severe ROP. Other meta-regression analyses of confounders did not show significant associations.
We performed additional analyses aimed at evaluating the role of the presence of fetal inflammatory response (i.e., funisitis) on the development of ROP (S7 Fig). Two studies reported on all grades ROP in infants with histological CA, with or without funisitis. Meta-analysis showed a significant increase in risk of all stages ROP in infants who had funisitis, compared to infants who had CA without funisitis. Two studies reported on severe ROP in infants with funisitis. Meta-analysis showed a significant increase in severe ROP risk in funisitis-positive infants, compared to infants who were only CA-positive (S7 Fig). Finally, when considering any stage ROP and severe ROP together, we observed an increase in risk of ROP in the funisitis-exposed group (S7 Fig). However, additional meta-analysis showed the groups also differed in degree of prematurity. Funisitis-positive infants had significantly lower GA (MD -1.30 weeks, 95% CI -1.37 to -1.23, p < 0.0001) than the CA-exposed infants without funisitis.
Analysis based on adjusted data
Eight studies reported adjusted data on CA-exposure and ROP risk. As described in S4 and S5 Tables, studies adjusted for different covariates. Meta-analysis of unadjusted data in these studies showed that CA-infants were at a significant risk of all stages ROP (OR 1.73, 95% CI 1.33 to 2.25, S4 Table). Similarly, unadjusted data from these studies showed a significant risk of severe ROP in the CA-group (OR 2.00, 95% CI 1.46 to 2.74, S5 Table). We compared the results of the unadjusted analyses to the adjusted ORs reported in these 8 studies. When using adjusted data, meta-analysis could no longer find a significant association between CA (histological, clinical and any type) and ROP (all stages ROP: OR 1.29, 95% CI 0.87 to 1.91, S4 Table; severe ROP: OR 1.17, 95% CI 0.88 to 1.56, S5 Table).
Discussion
Our updated meta-analysis included a greater pool of studies (50 vs. 27) and a larger number of infants (38,956 vs. 10,590) than the meta-analysis of Mitra et al. [29], but further confirmed their results. We observed a significant positive association between any CA and all stages of ROP. This association was significant for histological but not for clinical CA. In contrast, both clinical and histological CA were associated with severe ROP. Exposure to funisitis was associated with a higher risk of ROP than exposure to CA in the absence of funisitis. Additional meta-analyses showed that infants exposed to CA had significantly lower GA and lower BW than the infants not exposed to CA. Meta-regression showed that these differences in GA and BW were significantly correlated with a higher risk of ROP in the CA-exposed group. Meta-regression also showed that higher rates of EOS, SGA, and mortality in the CA-exposed group correlated significantly with a higher risk of ROP. Meta-analyses of studies with adjusted data could not find an association between CA and ROP. In summary, our study confirms that CA is a risk factor for developing ROP. However, part of the effects of CA on the pathogenesis of ROP may be mediated by the role of CA as an etiological factor for very preterm birth.
Assessment of CA as a risk factor for adverse outcomes in (very) preterm infants is hampered by the lack of a ‘normal’ control group. Two broad pathological conditions have been identified to lead to very preterm birth: (i) infection/inflammation and (ii) placental dysfunction resulting from vascular malfunction [88, 89]. As discussed elsewhere [11, 90], in addition to distinct pathophysiological pathways, baseline and clinical characteristics are different between these two groups [88, 91]. Accordingly, our analyses showed that the infants exposed to CA were born significantly earlier (~1.15 weeks), were lighter (~35 g), had a higher rate of exposure to antenatal corticosteroids, had a lower rate of cesarean section, were less often SGA, had a higher rate of PROM, had a higher rate of EOS and LOS, and had a higher mortality. Some of these differences may have had a direct or indirect influence on the development of ROP.
We performed meta-regression analyses to evaluate the potential impact of confounders on the risk of ROP. Meta-regression is a statistical technique which examines the relationship between continuous or categorical moderators and the size of effects observed in the studies [38, 92]. Thus, meta-regression allows for the exploration of more complex questions than traditional meta-analysis. The present meta-regression demonstrated that the studies with higher differences in GA and BW between the CA-exposed and CA-unexposed group were also the studies where infants with CA had a greater risk of ROP. Previous meta-regression analyses found a similar correlation between the differences in GA and BW and the CA-associated risk of BPD [8] and PDA [11].
Additionally, we observed that when the few studies that corrected for GA, BW, and other confounding factors were pooled, they did not show a significant increase in the risk of ROP (S4 and S5 Tables). This supports the idea that GA, BW and other confounders significantly modify the association between CA and ROP. Previous meta-analyses on the relationship between CA and BPD [8], or cerebral palsy [13], showed that the positive association observed with unadjusted data was significantly reduced, or became non-significant, when adjusted data were pooled. Moreover, in another meta-analysis, the significant positive association between CA and PDA became a significant negative association when only adjusted data were taken into consideration [11]. As mentioned in the introduction, in their meta-analysis on CA and ROP, Mitra et al. [29] did not pool the studies with adjusted results but performed a subgroup analysis of studies which did not show a significant difference in GA between the CA-exposed and CA-unexposed group. In this subgroup of studies, CA was not significantly associated with ROP. This finding is confirmed in the present meta-analysis, underlining the idea that the effects of CA on ROP development are, at least in part, related to its ability to induce (very) preterm birth.
That the fetal inflammatory response induced by CA might specifically influence the development of the fetal retina is a biologically plausible hypothesis. It has been suggested that multiple hits of antenatal and postnatal infection/inflammation are involved in ROP etiology and progression [16, 28, 93, 94]. Proinflammatory cytokines may exert a direct effect on retinal angiogenesis or sensitize the developing retina to the effects of postnatal oxygen, or other stressors. [16, 94]. After birth, the circulatory instability and fluctuation of oxygen saturation following infection/inflammation may affect the retinal perfusion and lead to increased retinal injury. Our meta-analysis shows that CA is not only a risk factor for ROP but also a risk factor for EOS and LOS. Moreover, meta-regression showed a correlation between the effect size of the CA-ROP association and the CA-EOS association. In addition, the meta-analysis of Been et al. [9] demonstrated that CA was a risk factor for NEC, a complication of prematurity in which inflammation plays an important pathogenic role. Altogether, these data suggest that CA-exposed infants are more prone to be exposed to postnatal infection/inflammation and that this propensity makes these infants more vulnerable to ROP.
CA will not always lead to an inflammatory process extending to the fetal component [95]. Funisitis is considered the histologic counterpart of the fetal inflammatory response syndrome [5, 95]. Our analysis showed that the presence of funisitis increased the risk of developing ROP when compared with CA in the absence of funisitis (S8 Fig). These data support the role of the fetal inflammatory response as etiopathogenic factor for ROP. Nevertheless, the number of studies including data on funisitis was rather limited. In addition, infants with funisitis also presented a significantly lower GA when compared with infants with CA without funisitis. Therefore, as in the case of CA, the effects of funisitis on ROP may be related to mechanisms that involve fetal inflammation but also to mechanisms that induce earlier birth.
A further point of interest is that, as assessed by Dammann et al. [77], risk factor patterns for ROP occurrence and progression might differ. A large proportion of very preterm infants will develop low-grade ROP, while in a small proportion it will progress to high-grade disease [77]. Of note, our meta-analysis could not demonstrate that CA was a significant risk factor for ROP stage 1–2 (Fig 4). Recent clinical data suggest that infection/inflammation mechanisms are mainly related to the more advanced stages of ROP, particularly the so-termed aggressive posterior ROP (APROP) [28, 93].
As mentioned above, the two main etiological groups for very preterm birth are infection/inflammation and placental vascular dysfunction [88, 89]. Two recent meta-analyses have studied the risk of ROP of conditions related to the vascular dysfunction group. Neither Chan et al. [27] nor Zhu et al. [96] could demonstrate that maternal or gestational hypertensive disorders affected the risk of developing ROP. However, they did not analyze the differences in basal characteristics between the group of infants exposed and unexposed to maternal/gestational hypertensive disorders. We speculate that the exposed infants probably had a higher GA than the ‘control’ infants and that this difference may have influenced the risk of ROP.
Limitations of the literature and our systematic review and meta-analysis deserve comment. First, the published literature showed great heterogeneity in definition of CA, and in assessment of confounders. Particularly, criteria for the use of the term clinical CA are highly variable, and recent recommendations propose to restrict the term CA to pathologic diagnosis [97]. Second, none of the included studies evaluated the association between CA and ROP as their main objective. Third, adjusted data were available only from 8 of the 50 studies included in the meta-analysis. In addition, we had to rely on the adjusted analyses as presented in the published reports and the variables for which they adjusted, which were not consistent across studies. Finally, meta-regression uses summary data at the study level, meaning we cannot comment on data of individual infants within a study and there is a risk of ecological bias [98]. On the other hand, the main strengths of the present study are the large number of included studies and the use of rigorous methods, including an extensive and comprehensive search; duplicate screening, inclusion, and data extraction to reduce bias; meta-analysis of baseline and secondary characteristics; and the use of meta-regression to control for potential confounders.
Conclusions
ROP is a multifactorial disease that occurs in the youngest and sickest preterm infants [14–20, 99]. Our data show that CA, particularly when accompanied by funisitis, is a risk factor for ROP, but also a risk factor for being a younger and sicker preterm infant. Clinical and experimental evidence suggests that low GA, oxygen stress, as well as ante- and postnatal infection/inflammation are not only independent risk factors for ROP but also interact beyond additive and even multiplicative patterns [16, 22, 100]. Future preventive and therapeutic strategies aimed to reduce ROP, as well as other complications of prematurity, should be tailored, as much as possible, to the particular pathogenic pathway leading to very preterm birth.
Supporting information
CA: chorioamnionitis; ROP: retinopathy of prematurity.
(TIF)
CA: chorioamnionitis; ROP: retinopathy of prematurity.
(TIF)
CA: chorioamnionitis; ROP: retinopathy of prematurity; GA: gestational age.
(TIF)
CA: chorioamnionitis; ROP: retinopathy of prematurity.
(TIF)
CA: chorioamnionitis; BW: birth weight; ROP: retinopathy of prematurity.
(TIF)
GA: gestational age; CA: chorioamnionitis; ROP: retinopathy of prematurity.
(TIF)
CA: chorioamnionitis; ROP: retinopathy of prematurity.
(TIF)
(DOCX)
GA: gestational age; BW: birth weight; ACS: antenatal steroids.
(DOCX)
Log: logarithm; OR: odds ratio; ROP: retinopathy of prematurity; k: number of studies included; CI: confidence interval.
(DOCX)
BW: birth weight; GA: gestational age; Histol.: histological; OR: odds ratio; ROP: retinopathy of prematurity.
(DOCX)
BW: birth weight; GA: gestational age; Histol.: histological; OR: odds ratio; ROP: retinopathy of prematurity.
(DOCX)
(DOC)
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Cornette L. Fetal and neonatal inflammatory response and adverse outcome. Semin Fetal Neonatal Med. 2004;9(6):459–70. 10.1016/j.siny.2004.08.004 [DOI] [PubMed] [Google Scholar]
- 2.Thomas W, Speer CP. Chorioamnionitis: important risk factor or innocent bystander for neonatal outcome? Neonatology. 2011;99(3):177–87. 10.1159/000320170 [DOI] [PubMed] [Google Scholar]
- 3.Tita AT, Andrews WW. Diagnosis and management of clinical chorioamnionitis. Clin Perinatol. 2010;37(2):339–54. 10.1016/j.clp.2010.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pugni L, Pietrasanta C, Acaia B, Merlo D, Ronchi A, Ossola MW, et al. Chorioamnionitis and neonatal outcome in preterm infants: a clinical overview. J Matern Fetal Neonatal Med. 2015:1–5. 10.3109/14767058.2015.1053862 . [DOI] [PubMed] [Google Scholar]
- 5.Gantert M, Been JV, Gavilanes AW, Garnier Y, Zimmermann LJ, Kramer BW. Chorioamnionitis: a multiorgan disease of the fetus? J Perinatol. 2010;30 Suppl:S21–30. 10.1038/jp.2010.96 . [DOI] [PubMed] [Google Scholar]
- 6.Rocha G. Chorioamnionitis and lung injury in preterm newborns. Crit Care Res Pract. 2013;2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Watterberg KL, Demers LM, Scott SM, Murphy S. Chorioamnionitis and early lung inflammation in infants in whom bronchopulmonary dysplasia develops. Pediatrics. 1996;97(2):210–5. . [PubMed] [Google Scholar]
- 8.Hartling L, Liang Y, Lacaze-Masmonteil T. Chorioamnionitis as a risk factor for bronchopulmonary dysplasia: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2012;97(1):F8–F17. 10.1136/adc.2010.210187 . [DOI] [PubMed] [Google Scholar]
- 9.Been JV, Lievense S, Zimmermann LJ, Kramer BW, Wolfs TG. Chorioamnionitis as a risk factor for necrotizing enterocolitis: a systematic review and meta-analysis. J Pediatr. 2013;162(2):236–42 e2. 10.1016/j.jpeds.2012.07.012 . [DOI] [PubMed] [Google Scholar]
- 10.Park HW, Choi YS, Kim KS, Kim SN. Chorioamnionitis and Patent Ductus Arteriosus: A Systematic Review and Meta-Analysis. PLoS One. 2015;10(9):e0138114 10.1371/journal.pone.0138114 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Behbodi E, Villamor-Martínez E, Degraeuwe PL, Villamor E. Chorioamnionitis appears not to be a Risk Factor for Patent Ductus Arteriosus in Preterm Infants: A Systematic Review and Meta-Analysis. Sci Rep. 2016;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Felice C, Toti P, Laurini RN, Stumpo M, Picciolini E, Todros T, et al. Early neonatal brain injury in histologic chorioamnionitis. J Pediatr. 2001;138(1):101–4. . [DOI] [PubMed] [Google Scholar]
- 13.Wu YW, Colford JM Jr. Chorioamnionitis as a risk factor for cerebral palsy: A meta-analysis. JAMA. 2000;284(11):1417–24. . [DOI] [PubMed] [Google Scholar]
- 14.Fang JL, Sorita A, Carey WA, Colby CE, Murad MH, Alahdab F. Interventions To Prevent Retinopathy of Prematurity: A Meta-analysis. Pediatrics. 2016;137(4). 10.1542/peds.2015-3387 . [DOI] [PubMed] [Google Scholar]
- 15.Cavallaro G, Filippi L, Bagnoli P, La Marca G, Cristofori G, Raffaeli G, et al. The pathophysiology of retinopathy of prematurity: an update of previous and recent knowledge. Acta Ophthalmol. 2014;92(1):2–20. 10.1111/aos.12049 . [DOI] [PubMed] [Google Scholar]
- 16.Lee J, Dammann O. Perinatal infection, inflammation, and retinopathy of prematurity. Semin Fetal Neonatal Med. 2012;17(1):26–9. 10.1016/j.siny.2011.08.007 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hartnett ME, Penn JS. Mechanisms and management of retinopathy of prematurity. N Engl J Med. 2012;367(26):2515–26. 10.1056/NEJMra1208129 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartnett ME, Lane RH. Effects of oxygen on the development and severity of retinopathy of prematurity. J AAPOS. 2013;17(3):229–34. 10.1016/j.jaapos.2012.12.155 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hartnett ME. Pathophysiology and mechanisms of severe retinopathy of prematurity. Ophthalmology. 2015;122(1):200–10. 10.1016/j.ophtha.2014.07.050 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Soetikno BT, Yi J, Shah R, Liu W, Purta P, Zhang HF, et al. Inner retinal oxygen metabolism in the 50/10 oxygen-induced retinopathy model. Sci Rep. 2015;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holmström G, Tornqvist K, Al‐Hawasi A, Nilsson Å, Wallin A, Hellström A. Increased frequency of retinopathy of prematurity over the last decade and significant regional differences. Acta Ophthalmol (Copenh). 2017. [DOI] [PubMed] [Google Scholar]
- 22.Chen M, Citil A, McCabe F, Leicht KM, Fiascone J, Dammann CE, et al. Infection, oxygen, and immaturity: interacting risk factors for retinopathy of prematurity. Neonatology. 2011;99(2):125–32. 10.1159/000312821 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hauspurg AK, Allred EN, Vanderveen DK, Chen M, Bednarek FJ, Cole C, et al. Blood gases and retinopathy of prematurity: the ELGAN Study. Neonatology. 2011;99(2):104–11. 10.1159/000308454 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hellstrom A, Hard AL, Engstrom E, Niklasson A, Andersson E, Smith L, et al. Early weight gain predicts retinopathy in preterm infants: new, simple, efficient approach to screening. Pediatrics. 2009;123(4):e638–45. 10.1542/peds.2008-2697 . [DOI] [PubMed] [Google Scholar]
- 25.Au SC, Tang SM, Rong SS, Chen LJ, Yam JC. Association between hyperglycemia and retinopathy of prematurity: a systemic review and meta-analysis. Sci Rep. 2015;5:9091 10.1038/srep09091 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uddin MI, Evans SM, Craft JR, Capozzi ME, McCollum GW, Yang R, et al. In Vivo Imaging of Retinal Hypoxia in a Model of Oxygen-Induced Retinopathy. Sci Rep. 2016;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chan PYL, Tang S-M, Au SCL, Rong S-S, Lau HHW, Ko STC, et al. Association of Gestational Hypertensive Disorders with Retinopathy of prematurity: A Systematic Review and Meta-analysis. Sci Rep. 2016;6:30732 10.1038/srep30732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lundgren P, Lundberg L, Hellgren G, Holmström G, Hård A-L, Smith LE, et al. Aggressive posterior retinopathy of prematurity is associated with multiple infectious episodes and thrombocytopenia. Neonatology. 2017;111(1):79–85. 10.1159/000448161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mitra S, Aune D, Speer CP, Saugstad OD. Chorioamnionitis as a risk factor for retinopathy of prematurity: a systematic review and meta-analysis. Neonatology. 2014;105(3):189–99. 10.1159/000357556 . [DOI] [PubMed] [Google Scholar]
- 30.Cavallaro G, Villamor-Martínez E, Filippi L, Mosca F, Villamor E. Probiotic supplementation in preterm infants does not affect the risk of retinopathy of prematurity: A meta-analysis of randomized controlled trials. Sci Rep. 2017;7(1):13014 10.1038/s41598-017-13465-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–12. [DOI] [PubMed] [Google Scholar]
- 32.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. [cited 2016 December 1]. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm
- 34.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Borenstein M, Hedges LV, Higgins J, Rothstein HR. Subgroup analyses Introduction to Meta-analysis 2009. p. 149–86. [Google Scholar]
- 36.Borenstein M, Hedges LV, Higgins J, Rothstein HR. Identifying and quantifying heterogeneity Introduction to Meta-Analysis 2009. p. 107–26. [Google Scholar]
- 37.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Borenstein M, Hedges LV, Higgins J, Rothstein HR. Meta‐Regression Introduction to Meta-Analysis 2009. p. 187–203. [Google Scholar]
- 39.Austeng D, Blennow M, Ewald U, Fellman V, Fritz T, Hellstrom-Westas L, et al. Incidence of and risk factors for neonatal morbidity after active perinatal care: extremely preterm infants study in Sweden (EXPRESS). Acta Paediatr. 2010;99(7):978–92. 10.1111/j.1651-2227.2010.01846.x [DOI] [PubMed] [Google Scholar]
- 40.Barrera-Reyes RH, Ruiz-Macías H, Segura-Cervantes E. Neurodesarrollo al año de edad en recién nacidos pretérmino con antecedente de corioamnionitis materna. Ginecol Obstet Mex. 2011;79(1):31–7. [PubMed] [Google Scholar]
- 41.Bordigato MA, Piva D, Di Gangi IM, Giordano G, Chiandetti L, Filippone M. Asymmetric dimethylarginine in ELBW newborns exposed to chorioamnionitis. Early Hum Dev. 2011;87(2):143–5. 10.1016/j.earlhumdev.2010.11.004 [DOI] [PubMed] [Google Scholar]
- 42.Botet F, Figueras J, Carbonell-Estrany X, Arca G, Group CS. Effect of maternal clinical chorioamnionitis on neonatal morbidity in very-low birthweight infants: a case-control study. J Perinat Med. 2010;38(3):269–73. 10.1515/JPM.2010.029 [DOI] [PubMed] [Google Scholar]
- 43.Fung G, Bawden K, Chow P, Yu V. Long-term Outcome of Extremely Preterm Infants Following Chorioamnionitis 絨毛膜羊膜炎對極早早產兒的長遠影響. HK J Paediatr (new series). 2003;8(2):87–92. [Google Scholar]
- 44.Gagliardi L, Rusconi F, Bellù R, Zanini R, Network IN. Association of maternal hypertension and chorioamnionitis with preterm outcomes. Pediatrics. 2014;134(1):e154–e61. 10.1542/peds.2013-3898 [DOI] [PubMed] [Google Scholar]
- 45.Garcia-Munoz Rodrigo F, Galan Henriquez G, Figueras Aloy J, Garcia-Alix Perez A, Network S. Outcomes of very-low-birth-weight infants exposed to maternal clinical chorioamnionitis: a multicentre study. Neonatology. 2014;106(3):229–34. 10.1159/000363127 [DOI] [PubMed] [Google Scholar]
- 46.González-Luis G, García IJ, Rodríguez-Miguélez J, Mussons FB, Aloy JF. Patología neonatal en los menores de 1.500 gramos con relación al antecedente de corioamnionitis. An Pediatr (Barc). 2002;56(6):551–5. [PubMed] [Google Scholar]
- 47.Gray PH, Hurley TM, Rogers YM, O’Callaghan MJ, Tudehope DI, Burns YR, et al. Survival and neonatal and neurodevelopmental outcome of 24–29 week gestation infants according to primary cause of preterm delivery. Aust N Z J Obstet Gynaecol. 1997;37(2):161–8. [DOI] [PubMed] [Google Scholar]
- 48.Hendson L, Russell L, Robertson CM, Liang Y, Chen Y, Abdalla A, et al. Neonatal and neurodevelopmental outcomes of very low birth weight infants with histologic chorioamnionitis. J, Pediatr. 2011;158(3):397–402. [DOI] [PubMed] [Google Scholar]
- 49.Kim SY, Choi CW, Jung E, Lee J, Lee JA, Kim H, et al. Neonatal Morbidities Associated with Histologic Chorioamnionitis Defined Based on the Site and Extent of Inflammation in Very Low Birth Weight Infants. J Korean Med Sci. 2015;30(10):1476–82. 10.3346/jkms.2015.30.10.1476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lau J, Magee F, Qiu Z, Houbé J, Von Dadelszen P, Lee SK. Chorioamnionitis with a fetal inflammatory response is associated with higher neonatal mortality, morbidity, and resource use than chorioamnionitis displaying a maternal inflammatory response only. Am J Obstet Gynecol. 2005;193(3):708–13. [DOI] [PubMed] [Google Scholar]
- 51.Lee HJ, Kim E-K, Kim H-S, Choi CW, Kim BI, Choi J-H. Chorioamnionitis, respiratory distress syndrome and bronchopulmonary dysplasia in extremely low birth weight infants. J Perinatol. 2011;31(3):166–70. 10.1038/jp.2010.113 [DOI] [PubMed] [Google Scholar]
- 52.Lee Y, Kim H-J, Choi S-J, Oh S-y, Kim J-S, Roh C-R, et al. Is there a stepwise increase in neonatal morbidities according to histological stage (or grade) of acute chorioamnionitis and funisitis?: effect of gestational age at delivery. J Perinat Med. 2015;43(2):259–67. 10.1515/jpm-2014-0035 [DOI] [PubMed] [Google Scholar]
- 53.Liu Z, Tang Z, Li J, Yang Y. Effects of placental inflammation on neonatal outcome in preterm infants. Pediatr Neonatol. 2014;55(1):35–40. 10.1016/j.pedneo.2013.05.007 [DOI] [PubMed] [Google Scholar]
- 54.Mehta R, Nanjundaswamy S, Shen-Schwarz S, Petrova A. Neonatal morbidity and placental pathology. Indian J Pediatr. 2006;73(1):25–8. [DOI] [PubMed] [Google Scholar]
- 55.Morales WJ. The effect of chorioamnionitis on the developmental outcome of preterm infants at one year. Obstet Gynecol. 1987;70(2):183–6. [PubMed] [Google Scholar]
- 56.Mu S-C, Lin C-H, Chen Y-L, Ma H-J, Lee J-S, Lin M-I, et al. Impact on neonatal outcome and anthropometric growth in very low birth weight infants with histological chorioamnionitis. J Formos Med Assoc. 2008;107(4):304–10. 10.1016/S0929-6646(08)60091-1 [DOI] [PubMed] [Google Scholar]
- 57.Nasef N, Shabaan AE, Schurr P, Iaboni D, Choudhury J, Church P, et al. Effect of clinical and histological chorioamnionitis on the outcome of preterm infants. Am J Perinatol. 2013;30(01):059–68. [DOI] [PubMed] [Google Scholar]
- 58.Ogunyemi D, Murillo M, Jackson U, Hunter N, Alperson B. The relationship between placental histopathology findings and perinatal outcome in preterm infants. J Matern Fetal Neonatal Med. 2003;13(2):102–9. 10.1080/jmf.13.2.102.109 [DOI] [PubMed] [Google Scholar]
- 59.Ohyama M, Itani Y, Yamanaka M, Goto A, Kato K, Ijiri R, et al. Re-evaluation of chorioamnionitis and funisitis with a special reference to subacute chorioamnionitis. Hum Pathol. 2002;33(2):183–90. [DOI] [PubMed] [Google Scholar]
- 60.Pappas A, Kendrick DE, Shankaran S, Stoll BJ, Bell EF, Laptook AR, et al. Chorioamnionitis and early childhood outcomes among extremely low-gestational-age neonates. JAMA pediatrics. 2014;168(2):137–47. 10.1001/jamapediatrics.2013.4248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Perrone S, Toti P, Toti MS, Badii S, Becucci E, Gatti MG, et al. Perinatal outcome and placental histological characteristics: a single-center study. J Matern Fetal Neonatal Med. 2012;25(sup1):110–3. [DOI] [PubMed] [Google Scholar]
- 62.Polam S, Koons A, Anwar M, Shen-Schwarz S, Hegyi T. Effect of chorioamnionitis on neurodevelopmental outcome in preterm infants. Arch Pediatr Adolesc Med. 2005;159(11):1032–5. 10.1001/archpedi.159.11.1032 [DOI] [PubMed] [Google Scholar]
- 63.Rocha G, Proença E, Quintas C, Rodrigues T, Guimarães H. Chorioamnionitis and neonatal morbidity. Acta Med Port. 2006;19(3):207–12. [PubMed] [Google Scholar]
- 64.Sato M, Nishimaki S, Yokota S, Seki K, Horiguchi H, An H, et al. Severity of chorioamnionitis and neonatal outcome. J Obstet Gynaecol Res. 2011;37(10):1313–9. 10.1111/j.1447-0756.2010.01519.x [DOI] [PubMed] [Google Scholar]
- 65.Schlapbach LJ, Ersch J, Adams M, Bernet V, Bucher HU, Latal B. Impact of chorioamnionitis and preeclampsia on neurodevelopmental outcome in preterm infants below 32 weeks gestational age. Acta Paediatr. 2010;99(10):1504–9. 10.1111/j.1651-2227.2010.01861.x [DOI] [PubMed] [Google Scholar]
- 66.Seliga-Siwecka JP, Kornacka MK. Neonatal outcome of preterm infants born to mothers with abnormal genital tract colonisation and chorioamnionitis: a cohort study. Early Hum Dev. 2013;89(5):271–5. 10.1016/j.earlhumdev.2012.10.003 [DOI] [PubMed] [Google Scholar]
- 67.Soraisham A, Trevenen C, Wood S, Singhal N, Sauve R. Histological chorioamnionitis and neurodevelopmental outcome in preterm infants. J Perinatol. 2013;33(1):70–5. 10.1038/jp.2012.49 [DOI] [PubMed] [Google Scholar]
- 68.Soraisham AS, Singhal N, McMillan DD, Sauve RS, Lee SK, Network CN. A multicenter study on the clinical outcome of chorioamnionitis in preterm infants. Am J Obstet Gynecol. 2009;200(4):372.e1–e6. [DOI] [PubMed] [Google Scholar]
- 69.Suppiej A, Franzoi M, Vedovato S, Marucco A, Chiarelli S, Zanardo V. Neurodevelopmental outcome in preterm histological chorioamnionitis. Early Hum Dev. 2009;85(3):187–9. 10.1016/j.earlhumdev.2008.09.410 [DOI] [PubMed] [Google Scholar]
- 70.Tsiartas P, Kacerovsky M, Musilova I, Hornychova H, Cobo T, Sävman K, et al. The association between histological chorioamnionitis, funisitis and neonatal outcome in women with preterm prelabor rupture of membranes. J Matern Fetal Neonatal Med. 2013;26(13):1332–6. 10.3109/14767058.2013.784741 [DOI] [PubMed] [Google Scholar]
- 71.van Vliet EO, de Kieviet JF, van der Voorn JP, Been JV, Oosterlaan J, van Elburg RM. Placental pathology and long-term neurodevelopment of very preterm infants. Am J Obstet Gynecol. 2012;206(6):489.e1–e7. [DOI] [PubMed] [Google Scholar]
- 72.Wirbelauer J, Thomas W, Speer CP. Response of leukocytes and nucleated red blood cells in very low-birth weight preterm infants after exposure to intrauterine inflammation. J Matern Fetal Neonatal Med. 2011;24(2):348–53. 10.3109/14767058.2010.497568 [DOI] [PubMed] [Google Scholar]
- 73.Al-Essa M, Azad R, Rashwan N. Threshold stage of retinopathy of prematurity: maternal and neonatal risk factors. Ann Saudi Med. 2000;20(2):129–31. [DOI] [PubMed] [Google Scholar]
- 74.Allegaert K, Verdonck N, Vanhole C, de Halleux V, Naulaers G, Cossey V, et al. Incidence, perinatal risk factors, visual outcome and management of threshold retinopathy. Bull Soc Belge Ophtalmol. 2003;287:37–44. [PubMed] [Google Scholar]
- 75.Borroni C, Carlevaro C, Morzenti S, De Ponti E, Bozzetti V, Console V, et al. Survey on retinopathy of prematurity (ROP) in Italy. Ital J Pediatr. 2013;39(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen ML, Allred EN, Hecht JL, Onderdonk A, VanderVeen D, Wallace DK, et al. Placenta microbiology and histology and the risk for severe retinopathy of prematurity. Invest Ophthalmol Vis Sci. 2011;52(10):7052–8. 10.1167/iovs.11-7380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dammann O, Brinkhaus M-J, Bartels DB, Dördelmann M, Dressler F, Kerk J, et al. Immaturity, perinatal inflammation, and retinopathy of prematurity: a multi-hit hypothesis. Early Hum Dev. 2009;85(5):325–9. 10.1016/j.earlhumdev.2008.12.010 [DOI] [PubMed] [Google Scholar]
- 78.Gaugler C, Beladdale J, Astruc D, Schaeffer D, Donato L, Speeg-Schatz C, et al. Retinopathie du premature: Etude retrospective sur une periode de dix ans au CHU de Strasbourg. Arch Pediatr. 2002;9(4):350–7. [DOI] [PubMed] [Google Scholar]
- 79.Giapros V, Drougia A, Asproudis I, Theocharis P, Andronikou S. Low gestational age and chronic lung disease are synergistic risk factors for retinopathy of prematurity. Early Hum Dev. 2011;87(10):653–7. 10.1016/j.earlhumdev.2011.05.003 [DOI] [PubMed] [Google Scholar]
- 80.Holmström G, Thomassen P, Broberger U. Maternal risk factors for retinopathy of prematurity—a population‐based study. Acta Obstet Gynecol Scand. 1996;75(7):628–35. [DOI] [PubMed] [Google Scholar]
- 81.Hwang JH, Lee EH, Kim EA-R. Retinopathy of prematurity among very-low-birth-weight infants in Korea: incidence, treatment, and risk factors. J Korean Med Sci. 2015;30(Suppl 1):S88–S94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kavurt S, Özcan B, Aydemir O, Bas AY, Demirel N. Risk of retinopathy of prematurity in small for gestational age premature infants. Indian Pediatr. 2014;51(10):804–6. [DOI] [PubMed] [Google Scholar]
- 83.Martínez-Cruz CF, Salgado-Valladares M, Poblano A, Trinidad-Pérez MC. Risk factors associated with retinopathy of prematurity and visual alterations in infants with extremely low birth weight. Rev Invest Clin. 2012;64(2):136–43. [PubMed] [Google Scholar]
- 84.Park SH, Yum HR, Kim S, Lee YC. Retinopathy of prematurity in Korean infants with birthweight greater than 1500 g. Br J Ophthalmol. 2015:bjophthalmol-2015-306960. [DOI] [PubMed] [Google Scholar]
- 85.Serenius F, Ewald U, Farooqi A, Holmgren PÅ, Håkansson S, Sedin G. Short‐term outcome after active perinatal management at 23–25 weeks of gestation. A study from two Swedish tertiary care centres. Part 2: infant survival. Acta Paediatr. 2004;93(8):1081–9. [PubMed] [Google Scholar]
- 86.Slidsborg C, Jensen A, Forman JL, Rasmussen S, Bangsgaard R, Fledelius HC, et al. Neonatal risk factors for treatment-demanding retinopathy of prematurity: a Danish national study. Ophthalmology. 2016;123(4):796–803. 10.1016/j.ophtha.2015.12.019 [DOI] [PubMed] [Google Scholar]
- 87.Woo SJ, Park KH, Jung HJ, nae Kim S, Choe G, Ahn J, et al. Effects of maternal and placental inflammation on retinopathy of prematurity. Graefe’s Arch Clin Exp Ophthalmol. 2012;250(6):915–23. [DOI] [PubMed] [Google Scholar]
- 88.McElrath TF, Hecht JL, Dammann O, Boggess K, Onderdonk A, Markenson G, et al. Pregnancy disorders that lead to delivery before the 28th week of gestation: an epidemiologic approach to classification. Am J Epidemiol. 2008;168(9):980–9. 10.1093/aje/kwn202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gagliardi L, Rusconi F, Da Frè M, Mello G, Carnielli V, Di Lallo D, et al. Pregnancy disorders leading to very preterm birth influence neonatal outcomes: results of the population-based ACTION cohort study. Pediatr Res. 2013;73(6):794–801. 10.1038/pr.2013.52 [DOI] [PubMed] [Google Scholar]
- 90.Villamor-Martinez E, Fumagalli M, Rahim OMM, Passera S, Cavallaro G, Degraeuwe P, et al. Chorioamnionitis Is a Risk Factor for Intraventricular Hemorrhage in Preterm Infants: A Systematic Review and Meta-Analysis. bioRxiv. 2018:334375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Durrmeyer X, Kayem G, Sinico M, Dassieu G, Danan C, Decobert F. Perinatal risk factors for bronchopulmonary dysplasia in extremely low gestational age infants: a pregnancy disorder—based approach. J Pediatr. 2012;160(4):578–83.e2. 10.1016/j.jpeds.2011.09.025 [DOI] [PubMed] [Google Scholar]
- 92.Simon SR, van Zogchel L, Bas-Suarez MP, Cavallaro G, Clyman RI, Villamor E. Platelet Counts and Patent Ductus Arteriosus in Preterm Infants: A Systematic Review and Meta-Analysis. Neonatology. 2015;108(2):143–51. 10.1159/000431281 . [DOI] [PubMed] [Google Scholar]
- 93.Ahn Y, Hong K, Yum H, Lee J, Kim K, Youn Y, et al. Characteristic clinical features associated with aggressive posterior retinopathy of prematurity. Eye. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Friddle K. Pathogenesis of Retinopathy of Prematurity: Does Inflammation Play a Role? Newborn Infant Nurs Rev. 2013;13(4):161–5. [Google Scholar]
- 95.Revello R, Alcaide MJ, Dudzik D, Abehsera D, Bartha JL. Differential amniotic fluid cytokine profile in women with chorioamnionitis with and without funisitis. J Matern Fetal Neonatal Med. 2015:1–5. [DOI] [PubMed] [Google Scholar]
- 96.Zhu T, Zhang L, Zhao F, Qu Y, Mu D. Association of maternal hypertensive disorders with retinopathy of prematurity: A systematic review and meta-analysis. PLoS One. 2017;12(4):e0175374 10.1371/journal.pone.0175374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Higgins RD, Saade G, Polin RA, Grobman WA, Buhimschi IA, Watterberg K, et al. Evaluation and management of women and newborns with a maternal diagnosis of chorioamnionitis: summary of a workshop. Obstet Gynecol. 2016;127(3):426–36. 10.1097/AOG.0000000000001246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Thompson SG, Higgins JP. How should meta‐regression analyses be undertaken and interpreted? Stat Med. 2002;21(11):1559–73. 10.1002/sim.1187 [DOI] [PubMed] [Google Scholar]
- 99.Piermarocchi S, Bini S, Martini F, Berton M, Lavini A, Gusson E, et al. Predictive algorithms for early detection of retinopathy of prematurity. Acta Ophthalmol (Copenh). 2017;95(2):158–64. [DOI] [PubMed] [Google Scholar]
- 100.Lee JW, McElrath T, Chen M, Wallace DK, Allred EN, Leviton A, et al. Pregnancy disorders appear to modify the risk for retinopathy of prematurity associated with neonatal hyperoxemia and bacteremia. J Matern Fetal Neonatal Med. 2013;26(8):811–8. 10.3109/14767058.2013.764407 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CA: chorioamnionitis; ROP: retinopathy of prematurity.
(TIF)
CA: chorioamnionitis; ROP: retinopathy of prematurity.
(TIF)
CA: chorioamnionitis; ROP: retinopathy of prematurity; GA: gestational age.
(TIF)
CA: chorioamnionitis; ROP: retinopathy of prematurity.
(TIF)
CA: chorioamnionitis; BW: birth weight; ROP: retinopathy of prematurity.
(TIF)
GA: gestational age; CA: chorioamnionitis; ROP: retinopathy of prematurity.
(TIF)
CA: chorioamnionitis; ROP: retinopathy of prematurity.
(TIF)
(DOCX)
GA: gestational age; BW: birth weight; ACS: antenatal steroids.
(DOCX)
Log: logarithm; OR: odds ratio; ROP: retinopathy of prematurity; k: number of studies included; CI: confidence interval.
(DOCX)
BW: birth weight; GA: gestational age; Histol.: histological; OR: odds ratio; ROP: retinopathy of prematurity.
(DOCX)
BW: birth weight; GA: gestational age; Histol.: histological; OR: odds ratio; ROP: retinopathy of prematurity.
(DOCX)
(DOC)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.