Abstract
Introduction:
It is well established that socially marginalized groups experience worse health than dominant groups. However, many questions remain about the health of members of multiple marginalized groups, such as black sexual minority women. The purpose of this study was to examine the relationship between health-related quality of life (HRQOL), race, and sexual orientation identity among a general population sample of black and white women and to assess additive interaction between sexual orientation identity and race.
Methods:
This study used cross-sectional 2014 and 2015 Behavioral Risk Factor Surveillance System data from 154,995 women residing in 20 U.S. states. G-computation was used to estimate age-adjusted prevalence differences for nine dichotomized measures of HRQOL. The HRQOL of black sexual minority women was compared with the HRQOL of black heterosexual women, white sexual minority women, and white heterosexual women. Analyses were conducted in 2017.
Results:
Age-adjusted prevalence differences for all measures suggested worse HRQOL among black sexual minority women, compared with most of the other groups (e.g., frequent poor mental health comparing black lesbian and heterosexual women: 0.083, 95% CI= –0.017, 0.183); HRQOL among black bisexual women was often similar to or worse than white bisexual women. Most prevalence differences comparing black sexual minority women with white heterosexual women suggested additive interaction that led to stronger or weaker associations than expected. Although many point estimates suggested meaningful differences, many 95% CIs for prevalence differences, and when assessing for interaction, included 0.
Conclusions:
Having two marginalized identities, compared with one, is often associated with worse HRQOL. In addition, race and sexual orientation identity may interact in their relationship to HRQOL, such that black sexual minority women have worse or better HRQOL than expected.
INTRODUCTION
It is well established that socially marginalized groups, such as, sexual minorities (non-heterosexual people) and black people in the U.S., generally experience worse health than dominant groups.1,2 Research focused on members of multiple marginalized groups, such as black sexual minority women (SMW), is growing, but many questions remain.
Among women, sexual minority status and black race are each associated with negative health behaviors and outcomes. For example, cardiovascular disease risk, fair or poor health, and poor mental health, are more common among SMW than heterosexual women.3–6 Compared with white women, black women have higher diabetes incidence, higher obesity prevalence, higher rates of HIV diagnosis, and worse self-rated health and health-related quality of life (HRQOL).2,7 Some explanations for these health inequities incorporate the psychosocial stress, discrimination, and limited access to health-promoting resources experienced by marginalized groups.8–11
Intersectionality acknowledges that people occupy unique social spaces at the intersection of their particular combination of privileged and marginalized identities that cannot be accurately characterized by “adding up” the identities, or the corresponding social structures.12 For example, Crenshaw13(p140) articulates how the effects of multiple systems of oppression are not merely additive: “Because the intersectional experience is greater than the sum of racism and sexism, any analysis that does not take intersectionality into account cannot sufficiently address the particular manner in which black women are subordinated.” As intersectionality relates to public health, Bowleg14 describes how individual social identities and corresponding structural factors intersect to create health inequities. Thus, intersecting systems of oppression may influence the health of black SMW, and outcomes may be better than or worse than predicted based solely on an additive model.15 Intersectionality acknowledges this non-additivity, or qualitative concept of “multiplicativity” of social identities. Existing research documents quantitative statistical interactions between social groupings and their relationship to health, which have been analyzed on additive and multiplicative statistical scales, related to but distinct from the more conceptual meaning of multiplicative as it relates to intersectionality.12,15–17 Therefore, individual associations between race and health among women, and sexual orientation and health among women cannot necessarily be “summed” to predict the health of black SMW.
Research on the health of black SMW exists (e.g., smoking, reproductive health, and others), but gaps remain, including HRQOL.18–22 HRQOL is associated with behavioral risk factors and chronic illness and provides information about a population’s “burden of preventable disease, injuries, and disabilities.”23(p7) Furthermore, research on the health of black SMW has not quantitatively characterized the relationship between the intersection of race and sexual orientation and health by comparing health among black SMW with health among white heterosexual women.18,19,21 In addition, few studies have used probability samples.19
The objectives of this study are twofold. First, this study used probability samples from 20 states to examine the relationship between HRQOL and race among black and white SWM, and the relationship between HRQOL and sexual orientation identity (SOI) among black women. Second, this study examines whether there is evidence of interaction in the relationship between the intersection of race and SOI and HRQOL among black and white women, which provides quantitative support for the concept of intersectional multiplicativity. The authors expect that HRQOL among black SMW is worse than each of the comparison groups and that race and SOI interact in their relationship to HRQOL.
METHODS
Study Sample
The U.S.’s Behavioral Risk Factor Surveillance System (BRFSS) is a nationally representative phone survey of non-institutionalized English- or Spanish-speaking adults ages ≥18 years conducted annually by states and some territories, in partnership with the U.S. Centers for Disease Control and Prevention (CDC). The present study included the 20 states (Appendix) that asked participants’ SOI in both 2014 and 2015, and made data publicly available by December 2016. BRFSS included 446,421 non-Hispanic black and white women in 2014 and 2015; a total of 183,867 of those women resided in the included states. The median survey response rate for all states, territories, and Washington, DC, in 2014 was 47.0% (range, 25.1%–60.1%); the median response rate for 2015 was 47.2% (range, 33.9%–61.1%).24,25 For 2014 and 2015 combined, the median response rate for states included in this study was 45.5% (range, 33.0%– 57.6%).
Analyses included participants with non-missing values for all predictor (race and SOI) and outcome variables; age group was available for all participants. Ninety percent (n=166,256) of black and white women in included states were asked to select their SOI. The present study excluded women who chose other or something else (n=578, 0.31%), don’t know/not sure (n=1,072, 0.58%), or who refused to answer the question (n=3,097, 1.68%).26 Of the 161,509 black and white women who reported a SOI of heterosexual, lesbian, or bisexual, 6,512 (4%) were excluded due to missing at least one of the HRQOL measures. This resulted in losing between 2.2% and 4.9% of each race and SOI combination. Excluded participants tended to be older and have lower educational attainment, and a higher proportion were widowed, were black, and had fair or poor health compared with included participants. Two white heterosexual women were also excluded because they were the only participants within their strata, for a total sample size of 154,995. This study does not constitute human subjects research, per the University of California, Berkeley Committee for Protection of Human Subjects.
Measures
The CDC optional module asks: Do you consider yourself to be: 1 Straight, 2 Lesbian or gay, 3 Bisexual? Some state-added questions explained the identity options by referencing sexual behavior and attraction (behavior and attraction were not collected), and presented the options in a different order. The study included non-Hispanic black and non-Hispanic white women.
HRQOL captures perceptions of physical or mental health, and CDC recommends the validated Healthy Days Measures, which are in the BRFSS core module.23,27 In addition to self-rated general health, a useful predictor of mortality and morbidity, the Healthy Days Measures capture the number of days in the past 30 days that participants’ physical health was not good, mental health was not good, and poor physical or mental health limited their usual activities.28
Per the CDC’s recommendation, the number of days of poor physical health and poor mental health were summed.23 Based on suggestions in CDC documentation, and for comparability with existing research, outcomes were dichotomized.23,29 Self-rated health was dichotomized as excellent, very good, or good versus fair or poor; days measures were dichotomized as both ≥14 days (“frequent”) and ≥7 days.
Six age categories provided by the CDC were used: 18 to 24, 25 to 34, 35 to 44, 45 to 54, 55 to 64, and ≥65 years. Analyses did not adjust for other common control variables (e.g., educational attainment, marital status, income) or health behaviors (e.g., smoking) because they are likely mediators of the relationship between race and SOI and HRQOL.11,30,31
Statistical Analysis
Data weighting in BRFSS accounts for the sampling design, noncoverage and nonresponse, and makes each state’s data representative for that state. Analyses incorporated the BRFSS sample design stratification variable and raked weights using the survey package in Stata SE, version 14.2. Weighted proportions of each HRQOL measure and select demographics were estimated for each SOI and race combination. Crude and age-adjusted prevalence differences (PDs) comparing each HRQOL measure among black SMW with the HRQOL of: (1) black heterosexual women, (2) white SMW, and (3) white heterosexual women were estimated. These comparisons show differences in prevalence associated with: (1) SOI within black women, (2) black race within SMW, and (3) the intersection of SOI and race among black and white women; that is, having both marginalized social identities compared with having neither. Lesbian and bisexual women were analyzed separately.3,6,26,29 For outcomes in which age-adjusted PDs for lesbian and bisexual women were both non-zero, in the same direction, and not statistically different at α=0.05, lesbian and bisexual women were also combined to increase sample size. No adjustments were made for multiple comparisons. In brief, Rothman32(p44) argues that in most contexts, adjusting for multiple comparisons inaccurately presumes a “universal null hypothesis.” CIs for each comparison are provided for the reader to critically examine.
Interaction on the additive scale is relevant to potential underlying causal interaction, and the presence of interaction on the additive scale is consistent with the concept of intersectional multiplicativity.12 To assess additive interaction, the expected PD comparing black SMW with white heterosexual women was subtracted from the observed PD. The expected PD, assuming no additive interaction, was calculated by summing the PD associated with race among heterosexual women and the PD associated with SOI minority status among white women. In the absence of additive interaction, the observed PD was equal to the expected PD.
Age-adjusted PDs were estimated using g-computation, which standardizes each group’s marginal prevalence to the age distribution of the corresponding sample.33 For example, age-adjusted prevalences comparing black bisexual women and black heterosexual women were standardized to the combined age distribution of black bisexual women and black heterosexual women. For interaction analyses, age-adjusted prevalences were standardized to the combined age distribution of all heterosexual women and either all lesbians or all bisexual women. The underlying logistic regression allowed age to interact with SOI and race. Bootstrapping with 1,000 repetitions provided 95% CIs for age-adjusted PDs; both 95% CIs and 80% CIs were calculated for differences between expected and observed PDs.34 Bootstrap sampling was stratified by the BRFSS sample design stratification variable. Analyses were conducted in 2017.
RESULTS
In general, black bisexual or lesbian women reported the worst HRQOL, at times matched or exceeded by white bisexual women (Table 1). White heterosexual women tended to report the best HRQOL. For example, black bisexual women reported fair or poor health more frequently than other women (29.2%); white lesbians and white heterosexual women least frequently reported fair or poor health (13% and 14%, respectively).
Table 1.
Number and Weighted Proportions: Age and HRQOL – BRFSS, Selected U.S. States, 2014 and 2015
| Variable | Black | White | ||||
|---|---|---|---|---|---|---|
| Lesbian n=150 n (%) |
Bisexual n=213 n (%) |
Heterosexual n=12,464 n (%) |
Lesbian n=1,598 n (%) |
Bisexual n=1,969 n (%) |
Heterosexual n=138,601 n (%) |
|
| Age, years | ||||||
| 18–24 | 18 (29.4) |
50 (39.7) |
639 (13.1) | 110 (18.8) |
358 (34.9) |
4,194 (9.1) |
| 25–34 | 39 (29.3) |
60 (32.7) |
1,309 (17.0) | 133 (15.0) |
437 (30.4) |
9,352 (12.8) |
| 35–44 | 26 (11.3) |
39 (14.8) |
1,737 (18.1) | 182 (16.6) |
316 (14.0) |
14,387 (14.5) |
| 45–54 | 33 (17.8) |
23 (5.0) | 2,419 (18.4) | 383 (22.4) |
272 (8.9) | 22,937 (19.0) |
| 55–64 | 23 (8.4) | 20 (3.1) | 3,040 (17.3) | 467 (17.1) |
278 (6.1) | 33,818 (19.4) |
| >65 | 11 (3.7) | 21 (4.7) | 3,320 (16.2) | 323 (10.1) |
308 (5.8) | 53,913 (25.3) |
| HRQOL measures | ||||||
| Fair or poor self-rated health |
36 (22.9) |
59 (29.2) |
2,901 (20.7) | 243 (13.0) |
397 (21.1) |
20,365 (14) |
| Frequent poor physical health |
23 (16.6) |
35 (21.1) |
1,781 (12.1) | 233 (11.6) |
348 (18.0) |
17,845 (12.4) |
| Frequent poor mental health |
30 (21.3) |
51 (27.8) |
1,497 (13.7) | 234 (17.6) |
475 (28.4) |
14,230 (12.2) |
| Frequent unhealthy days |
39 (28.3) |
75 (41.5) |
2,776 (22.2) | 402 (26.1) |
679 (40.3) |
27,563 (21.1) |
| Frequent activity limitation |
25 (19.7) |
22 (14.7) |
1,223 (9.0) | 185 (11.1) |
264 (15.1) |
11,328 (8.2) |
| 7+ days poor physical health |
34 (31.9) |
51 (28.9) |
2,512 (18.2) | 317 (17.3) |
478 (26.3) |
24,464 (17.3) |
| 7+ days poor mental health |
39 (27.3) |
73 (36.5) |
2,183 (19.9) | 330 (24.9) |
677 (42.1) |
20,716 (17.7) |
| 7+ unhealthy days |
52 (45.0) |
97 (51.5) |
3,903 (31.9) | 559 (38.0) |
918 (53.1) |
38,390 (29.9) |
| 7+ days activity limitation |
32 (24.2) |
38 (20.9) |
1,685 (13.0) | 257 (15.1) |
382 (20.7) |
15,685 (11.5) |
BRFSS, Behavioral Risk Factor Surveillance System; HRQOL, health-related quality of life
Age-adjusted PDs for most measures and comparisons showed worse HRQOL among black SMW; comparisons between black bisexual women and white bisexual women were an exception with mixed associations (Table 2 and Figure 1). Frequent days measures, which exhibit a similar pattern of results, are included in Appendix Table 2. Age-adjusted PDs tended to be larger (indicating worse health among black SMW) for measures dichotomized at ≥7 days than at ≥14 days. When analyzing bisexual and lesbian women separately, most 95% CIs included 0. When analyzing bisexual and lesbian women together, estimates were more precise.
Table 2.
Select Age-adjusted HRQOL Prevalence Differences – BRFSS, Selected U.S. States, 2014 and 2015
| HRQOL measure | PD (95% CI) | PD (95% CI) | PD (95% CI) |
|---|---|---|---|
| Black lesbian women compared to |
Black heterosexual | White lesbian | White heterosexual |
| Fair or poor self-rated health |
0.142 (–0.016, 0.299) |
0.227 (0.104, 0.351) |
0.273 (0.073, 0.472) |
| 7+ days poor physical health |
0.165 (0.001, 0.328) |
0.166 (0.038, 0.294) |
0.220 (0.008, 0.432) |
| 7+ days poor mental health |
0.042 (–0.059, 0.142) |
0.034 (–0.056, 0.124) |
0.047 (–0.068, 0.163) |
| 7+ unhealthy days | 0.129 (–0.030, 0.288) |
0.088 (–0.040, 0.215) |
0.183 (–0.023, 0.389) |
| 7+ days activity limitation |
0.132 (–0.008, 0.271) |
0.133 (0.024, 0.241) |
0.152 (–0.022, 0.326) |
| Black bisexual women compared to |
Black heterosexual | White bisexual | White heterosexual |
| Fair or poor self-rated health |
0.035 (–0.071, 0.142) |
0.070 (–0.017, 0.157) |
0.095 (–0.014, 0.204) |
| 7+ days poor physical health |
0.081 (–0.028, 0.190) |
0.020 (–0.065, 0.106) |
0.11 (–0.015, 0.234) |
| 7+ days poor mental health |
0.107 (0.008, 0.206) | –0.036 (–0.120, 0.047) |
0.116 (0.006, 0.227) |
| 7+ unhealthy days | 0.054 (–0.059, 0.167) |
–0.041 (–0.129, 0.047) |
0.077 (–0.050, 0.203) |
| 7+ days activity limitation |
0.092 (–0.020, 0.203) |
0.030 (–0.053, 0.113) |
0.113 (–0.013, 0.239) |
| Black sexual minority women (combined lesbian and bisexual; SMW) compared to |
Black heterosexual | White SMW | White heterosexual |
| Fair or poor self-rated health |
0.067 (–0.022, 0.155) |
0.122 (0.046, 0.198) |
0.145 (0.035, 0.255) |
| 7+ days poor physical health |
0.101 (0.009, 0.193) |
0.078 (0.000, 0.155) |
0.134 (0.018, 0.251) |
| 7+ days poor mental health |
0.085 (0.008, 0.162) | N/Aa | 0.091 (0.008, 0.173) |
| 7+ unhealthy days | 0.080 (–0.013, 0.172) |
N/Aa | 0.107 (–0.011, 0.224) |
| 7+ days activity limitation |
0.118 (0.036, 0.201) |
0.079 (0.012, 0.145) |
0.136 (0.041, 0.231) |
Estimates for lesbian and bisexual women were in different directions. Boldface indicates statistical significance (p<0.05). Age-adjusted using age categories: 18–24, 25–34, 35–44, 45– 54, 55–64, >65 years.
BRFSS, Behavioral Risk Factor Surveillance System; HRQOL, health-related quality of life; PD, prevalence difference
Figure 1.
HRQOL among black sexual minority women – BRFSS, selected U.S. states, 2014 and 2015.
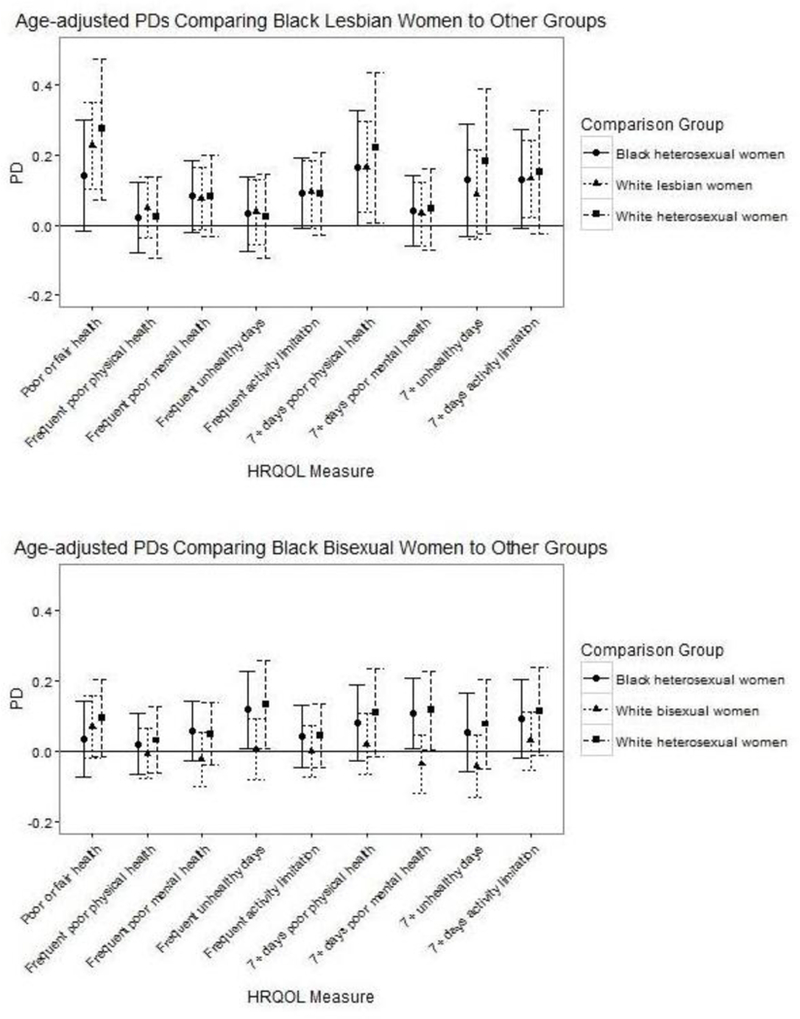
Notes: Age-adjusted using age categories: 18–24, 25–34, 35–44, 45–54, 55–64, >65 years.
BRFSS, Behavioral Risk Factor Surveillance System; HRQOL, Health-related quality of life; PDs, prevalence differences.
PD point estimates varied by measure and by comparison group. Across comparisons, the largest PDs tended to be for fair or poor self-rated general health (e.g., age-adjusted PD=0.273, 95% CI=0.073, 0.472 comparing black lesbian women and white heterosexual women) and the smallest PDs tended to be for frequent poor physical health (e.g., age-adjusted PD=0.024, 95% CI= –0.091, 0.140 comparing black lesbian women and white heterosexual women; Appendix Table 2). Across measures, comparisons that included white heterosexual women, in particular black lesbians compared with white heterosexual women, tended to have the largest PDs; comparisons between black and white bisexual women tended to have the smallest PDs.
Many comparisons between black SMW and white heterosexual women suggested additive interaction between race and SOI. Age-adjusted PDs comparing black lesbian women and white heterosexual women were larger in magnitude than expected in the absence of additive interaction, with the exception of frequent unhealthy days (Table 3). Age-adjusted PDs comparing black bisexual women and white heterosexual women tended to be weaker than, or the same as, expected. All 95% CIs, and most 80% CIs, comparing observed and expected age-adjusted PDs included 0.
Table 3.
Age-adjusted Excess HRQOL Prevalencea Due to Interaction - BRFSS, Selected U.S. States, 2014 and 2015
| HRQOL | Black lesbian women | Black bisexual women | ||||||
|---|---|---|---|---|---|---|---|---|
| measure | Expected PDa |
Excess prevalencea due to interaction |
Expected PDa |
Excess prevalencea due to interaction |
||||
| Excess | 95% CI | 80% CI |
Excess | 95% CI | 80% CI |
|||
| Fair or poor self- rated health |
0.073 | 0.199 | −0.004, 0.402 |
0.067, 0.331 |
0.172 | –0.077 | −0.192, 0.038 | −0.152, –0.002 |
| Frequent poor physical health |
0.014 | 0.011 | −0.109, 0.130 | − 0.067, 0.089 |
0.072 | −0.041 | −0.140, 0.058 | −0.106, 0.024 |
| Frequent poor mental health |
0.017 | 0.067 | −0.049, 0.183 | − 0.009, 0.143 |
0.093 | −0.043 | −0.135, 0.049 | −0.103, 0.017 |
| Frequent unhealthy days |
0.036 | −0.008 | −0.129, 0.113 | − 0.087, 0.071 |
0.129 | 0.004 | −0.129, 0.138 | −0.083, 0.091 |
| Frequent activity limitation |
0.029 | 0.061 | −0.059, 0.180 | − 0.017, 0.139 |
0.06 | −0.016 | −0.109, 0.078 | −0.077, 0.045 |
| 7+ days poor physical health |
0.040 | 0.18 | −0.036, 0.396 |
0.039, 0.321 |
0.095 | 0.015 | −0.117, 0.147 | −0.071, 0.101 |
| 7+ days poor mental health |
0.035 | 0.013 | −0.104, 0.130 | − 0.063, 0.089 |
0.115 | 0.002 | −0.113, 0.116 | −0.072, 0.076 |
| 7+ unhealthy days |
0.080 | 0.103 | −0.108, 0.313 | − 0.034, 0.240 |
0.135 | −0.058 | −0.192, 0.076 | −0.146, 0.030 |
| 7+ days activity limitation |
0.040 | 0.112 | −0.064, 0.288 | − 0.003, 0.227 |
0.070 | 0.043 | −0.086, 0.172 | −0.041, 0.127 |
Compared to white heterosexual women. Boldface indicates statistical significance (p<0.20, customary for interaction analyses, see Jewell [2004]). Age-adjusted using age categories: 18– 24, 25–34, 35–44, 45–54, 55–64, >65 years.
BRFSS, Behavioral Risk Factor Surveillance System; HRQOL, Health-related quality of life; PD, prevalence difference
DISCUSSION
Consistent with the hypothesis, this study found that black SMW generally reported worse HRQOL than black heterosexual women, white SMW, and white heterosexual women. Comparisons between black and white bisexual women were a notable exception; the poor HRQOL of black bisexual women was sometimes matched or exceeded by the poor HRQOL of white bisexual women. The largest associations were found for comparisons between black SMW and white heterosexual women. To the authors’ best knowledge, this is the first published research to compare these HRQOL measures between these groups using the same probability samples.
Some studies have investigated self-rated health among black SMW using different methods. In contrast to the present study, researchers found no difference in age-standardized prevalence of fair or poor self-rated health when comparing combined black lesbian (82%), bisexual (9%), and other sexual minority (9%) women with black heterosexual women from another survey.35 However, this sample was limited to Los Angeles County, and the authors used a different standardization method.35 Compared with the present study, Hsieh and Ruther15 found both similar and contrasting results in their investigation of race, SOI, and self-rated health. However, they used different methodology than the present study, including combining non-Hispanic black and Hispanic women.
Previous research on the mental health of black SMW used different methods than the present study, and reported partially consistent results. The present study found worse mental health-related HRQOL among combined black lesbian and bisexual women than among black heterosexual women, which is consistent with research on past indicators of psychological distress in two metropolitan nonprobability samples of black lesbian and heterosexual women.22 In the present study, black lesbians had worse mental health-related HRQOL than white lesbians, whereas black bisexual women had better mental health-related HRQOL than white bisexual women, although 95% CIs included 0 for all comparisons. These results are partially consistent with results from a New York City-based nonprobability sample, which analyzed lesbian and bisexual women together.36
Consistent with the multiplicative intersectionality-informed hypothesis of non-additivity, the present study found that sexual orientation and race may interact in their relationship to HRQOL. Most PDs comparing black SWM with white heterosexual women implied interaction that led to either stronger or weaker associations than expected. However, all 95% CIs and most 80% CIs comparing observed and expected PDs included 0. Though not investigating the health of black SMW specifically, some results from Hsieh and Ruther15 supported a non-additive relationship between SOI and race and self-rated health, whereas other results did not. However, the study by Hsieh and Ruther15 controlled for additional demographic variables and investigated a different measure of self-rated health than the present study. The findings from the study by Veenstra16 are also consistent with the theory of intersectionality’s application to health, though analyses did not test the intersection of SOI and race, specifically.
Although patterns of association magnitude differed for black lesbian and black bisexual women, the wide CIs suggest that further research with larger sample sizes would improve confidence that these patterns reflect real phenomena. The small number of black SMW in the present study and the underrepresentation of some U.S. regions, highlight the need for large national surveys that collect sexual orientation information, especially in geographic regions where more black women live. The contrast in the associations between race and HRQOL within lesbian women and within bisexual women may partially reflect the elevated prevalence of poor HRQOL among white bisexual women in this study sample. This is consistent with previous research that found worse HRQOL among bisexual women compared with lesbian women in a sample that was 80% non-Hispanic white.29 In the present study, the racial disparity in college completion was larger between black and white lesbian women than between black and white bisexual women, which may contribute to the finding of stronger inequities in HRQOL between black and white lesbian women than between black and white bisexual women. Health-related behaviors, experiences of stigma and support, and other determinants of health may vary between lesbian and bisexual women and explain the different patterns of association between these SOI groups; future research will investigate health-related behavior among black SMW within the present sample.29,37
Limitations
Twenty states were eligible for inclusion, therefore, results of the present study may not generalize to the U.S. as a whole. A small percentage of women were excluded due to missing outcome variables; results may have varied slightly if they had been included. The present study may not represent the HRQOL of SMW who self-identify using a term other than lesbian or bisexual (e.g., same gender loving or queer) and therefore selected other or something else, or women who have same-sex attractions or sexual interactions but do not identify as a sexual minority.26 Furthermore, the concept of intersectionality encompasses all social identities and the present study included only two, SOI and race, among an already disadvantaged group—women—future work should address heterogeneity within black SMW. Finally, this study focused on black SMW, but the health of other SMW of color is also understudied. Nevertheless, the patterns in direction and magnitude of PDs suggest the importance of further investigation of the health of black SMW.
CONCLUSIONS
This study addresses an important knowledge gap by using a probability sample to investigate HRQOL and its relationship to race, SOI, and the intersection of race and SOI among black and white women using a quantitative interaction analysis that aligns with concepts of intersectional multiplicativity.12 The present study identified a pattern of health inequities experienced by black SMW that, for the most part, aligns with theory and existing research. These patterns highlight the importance of further research about the health of black SMW, such as investigating specific health conditions and health-related behaviors, to inform prevention and intervention efforts. Some research using nonprobability samples has identified potential differences in health-related behaviors between black and white SMW.18,21 Future work should explore determinants of health and specific points of prevention or intervention, including those in the clinical setting, that may be unique to or more nuanced among black SMW, and should include building from black SMW’s strengths.36,38 In addition, longitudinal studies with diverse participants would add a life course perspective to the health of black SMW. Finally, to the degree that societal structures and power differentials contribute to the patterns of health inequities in the present study, multilevel interventions and social change are crucial to addressing these patterns.11,39
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank Stephanie Leonard, Amelia Wallace, Alison Cohen, Monika Izano, and Ellicott Matthay for providing feedback on earlier drafts, as well as Alan Hubbard for statistical analysis guidance. Karen Trocki and Tonda Hughes provided consultation regarding prior research among sexual minority women. The authors would also like to thank three anonymous reviewers for their constructive feedback. In addition, the authors acknowledge the state Behavioral Risk Factor Surveillance Survey programs and coordinators in Alaska, Colorado, Massachusetts, Michigan, New Mexico, North Carolina, and Washington for providing data that were not available through the Centers for Disease Control and Prevention. Finally, this work would not have been possible without the Behavioral Risk Factor Surveillance Survey participants.
The research reported here does not represent the official views of the funding sources.
Emily M. Yette was supported by the National Institute on Alcohol Abuse and Alcoholism: Graduate Research Training on Alcohol Problems, award number T32AA007240 and Center grant P50AA005595; the Hellman Graduate Award; and the Philip Brett LGBT Studies Award. She is affiliated with the Division of Epidemiology at the School of Public Health at University of California, Berkeley. The funding sources had no role in study design; collection, analysis, or interpretation of data; writing the manuscript; or the decision to submit the manuscript for publication.
EY worked on the study conception and design; obtaining, analyzing, and interpreting data; drafting and revising manuscript, and approved the final version. JA worked on the study design, data interpretation, critical revisions of manuscript, and approved the final version.
Contents of this article were presented at The 145th Annual American Public Health Association Meeting and Exposition, November 7, 2017 in Atlanta, Georgia.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Institute of Medicine (U.S.) Committee on Lesbian, Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding Washington, DC: National Academies Press (U.S.); 2011. www.ncbi.nlm.nih.gov/books/NBK64806/. Accessed September 8, 2017. [PubMed] [Google Scholar]
- 2.CDC. CDC health disparities and inequalities report – United States, 2013. MMWR Morb Mortal Wkly Rep 2013;62(suppl 3):1–189. [PubMed] [Google Scholar]
- 3.Fredriksen-Goldsen KI, Kim H-J, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health 2013;103(10):1802–1809. 10.2105/AJPH.2012.301110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blosnich JR, Farmer GW, Lee JGL, Silenzio VMB, Bowen DJ. Health inequalities among sexual minority adults: evidence from ten U.S. states, 2010. Am J Prev Med 2014;46(4):337–349. 10.1016/j.amepre.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matthews DD, Lee JGL. A profile of North Carolina lesbian, gay, and bisexual health disparities, 2011. Am J Public Health 2014;104(6):e98–e105. 10.2105/AJPH.2013.301751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health 2010;100(10):1953– 1960. 10.2105/AJPH.2009.174169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pereira CCA, Palta M, Mullahy J, Fryback DG. Race and preference-based health-related quality of life measures in the United States. Qual Life Res Int J Qual Life Asp Treat Care Rehabil 2011;20(6):969–978. 10.1007/s11136-010-9813-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 2003;129(5):674– 697. 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eliason MJ, Fogel SC. An ecological framework for sexual minority women’s health: factors associated with greater body mass. J Homosex 2015;62(7):845–882. 10.1080/00918369.2014.1003007. [DOI] [PubMed] [Google Scholar]
- 10.Lick DJ, Durso LE, Johnson KL. Minority stress and physical health among sexual minorities. Perspect Psychol Sci J Assoc Psychol Sci 2013;8(5):521–548. 10.1177/1745691613497965. [DOI] [PubMed] [Google Scholar]
- 11.Phelan J, Link B. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol 2015;41:311–330. 10.1146/annurev-soc-073014-112305. [DOI] [Google Scholar]
- 12.Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med 2014;110:10–17. 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 13.Crenshaw KW. Demarginalizing the intersection of race and sex: a black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ Chic Leg Forum 1989;1989:139–167. [Google Scholar]
- 14.Bowleg L The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health 2012;102(7):1267–1273. 10.2105/AJPH.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsieh N, Ruther M. Sexual minority health and health risk factors: Intersection effects of gender, race, and sexual identity. Am J Prev Med 2016;50(6):746–755. 10.1016/j.amepre.2015.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Veenstra G. Race, gender, class, and sexual orientation: intersecting axes of inequality and self-rated health in Canada. Int J Equity Health 2011;10:3 10.1186/1475-9276-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Veenstra G. Race, gender, class, sexuality (RGCS) and hypertension. Soc Sci Med 2013;89:16–24. 10.1016/j.socscimed.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 18.Ortiz KS, Duncan DT, Blosnich JR, Salloum RG, Battle J. Smoking among sexual minorities: Are there racial differences? Nicotine Tob Res 2015;17(11):1362–1368. 10.1093/ntr/ntv001. [DOI] [PubMed] [Google Scholar]
- 19.Agénor M, Krieger N, Austin SB, Haneuse S, Gottlieb BR. At the intersection of sexual orientation, race/ethnicity, and cervical cancer screening: assessing Pap test use disparities by sex of sexual partners among black, Latina, and white U.S. women. Soc Sci Med 2014;116:110–118. 10.1016/j.socscimed.2014.06.039. [DOI] [PubMed] [Google Scholar]
- 20.Agénor M, Austin SB, Kort D, Austin EL, Muzny CA. Sexual orientation and sexual and reproductive health among African American sexual minority women in the U.S. South. Womens Health Issues 2016;26(6):612–621. 10.1016/j.whi.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Molina Y, Lehavot K, Beadnell B, Simoni J. Racial disparities in health behaviors and conditions among lesbian and bisexual women: The role of internalized stigma. LGBT Health 2014;1(2):131–139. 10.1089/lgbt.2013.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hughes TL, Matthews AK, Razzano L, Aranda F. Psychological distress in African American lesbian and heterosexual women. J Lesbian Stud 2003;7(1):51–68. 10.1300/J155v07n01_04. [DOI] [PubMed] [Google Scholar]
- 23.Measuring Healthy Days Atlanta, GA: Centers for Disease Control and Prevention; 2000. [Google Scholar]
- 24.Behavioral Risk Factor Surveillance System 2014 Summary Data Quality Report Atlanta, GA: CDC; 2015. www.cdc.gov/brfss/annual_data/2014/pdf/2014_dqr.pdf. [Google Scholar]
- 25.Behavioral Risk Factor Surveillance System 2015 Summary Data Quality Report Atlanta, GA: CDC; 2016. www.cdc.gov/brfss/annual_data/2015/pdf/2015-sdqr.pdf. [Google Scholar]
- 26.Badgett L, Goldberg N. Best practices for asking questions about sexual orientation on surveys The Williams Institute; 2009. https://williamsinstitute.law.ucla.edu/wp-content/uploads/SMART-FINAL-Nov-2009.pdf. Accessed April 9, 2018. [Google Scholar]
- 27.Moriarty DG, Zack MM, Kobau R. The Centers for Disease Control and Prevention’s Healthy Days Measures - population tracking of perceived physical and mental health over time. Health Qual Life Outcomes 2003;1:37 10.1186/1477-7525-1-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jylhä M What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med 2009;69(3):307–316. 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 29.Fredriksen-Goldsen KI, Kim H-J, Barkan SE, Balsam KF, Mincer SL. Disparities in health-related quality of life: a comparison of lesbians and bisexual women. Am J Public Health 2010;100(11):2255–2261. 10.2105/AJPH.2009.177329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mollborn S, Everett B. Understanding the educational attainment of sexual minority women and men. Res Soc Stratif Mobil 2015;41:40–55. 10.1016/j.rssm.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Badgett MVL, Lau H, Sears B, Ho D. Bias in the workplace: Consistent evidence of sexual orientation and gender identity discrimination The Williams Institute; 2007. https://williamsinstitute.law.ucla.edu/wp-content/uploads/Badgett-Sears-Lau-Ho-Bias-in-the-Workplace-Jun-2007.pdf. Accessed April 9, 2018. [Google Scholar]
- 32.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiol Camb Mass 1990;1(1):43–46. 10.1097/00001648-199001000-00010. [DOI] [PubMed] [Google Scholar]
- 33.Ahern J, Hubbard A, Galea S. Estimating the effects of potential public health interventions on population disease burden: a step-by-step illustration of causal inference methods. Am J Epidemiol 2009;169(9):1140–1147. 10.1093/aje/kwp015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jewell NP. Statistics for Epidemiology Boca Raton, FL: CRC Press LLC; 2004. [Google Scholar]
- 35.Mays VM, Yancey AK, Cochran SD, Weber M, Fielding JE. Heterogeneity of health disparities among African American, Hispanic, and Asian American women: unrecognized influences of sexual orientation. Am J Public Health 2002;92(4):632–639. 10.2105/AJPH.92.4.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Calabrese SK, Meyer IH, Overstreet NM, Haile R, Hansen NB. Exploring discrimination and mental health disparities faced by black sexual minority women using a minority stress framework. Psychol Women Q 2015;39(3):287–304. 10.1177/0361684314560730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Israel T, Mohr JJ. Attitudes toward bisexual women and men. J Bisexuality 2004;4(1– 2):117–134. 10.1300/J159v04n01_09. [DOI] [Google Scholar]
- 38.Agénor M, Bailey Z, Krieger N, Austin SB, Gottlieb BR. Exploring the cervical cancer screening experiences of black lesbian, bisexual, and queer women: the role of patient-provider communication. Women Health 2015;55(6):717–736. 10.1080/03630242.2015.1039182. [DOI] [PubMed] [Google Scholar]
- 39.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol 2001;27:363–385. 10.1146/annurev.soc.27.1.363. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


