Abstract
Warfarin has been the cornerstone therapy for stroke prevention in non-valvular atrial fibrillation (NVAF), particularly in patients at high risk of ischemic stroke or thromboembolism. Warfarin use in NVAF results in a 64% relative reduction in the incidence of ischemic stroke and several trials have demonstrated warfarin to be superior to aspirin alone (relative risk reduction-22%)1. However, anticoagulation with warfarin is associated with increased bleeding, especially in the elderly population 1. Anticoagaulation with warfarin requires close monitoring of the international standardized ratio (INR), which can be inconvenient to patients. Additionally, large numbers of patients on coumadin have a subtherapeutic INR level, which increases the risk of thromboembolic episodes 2. In part due to the above mentioned reasons, anticoagulation with warfarin is underutilized for stroke prevention 2–4.
Introduction
The efficacy of alternative thromboprophylatic agents and regimens, with potentially fewer adverse effects, has been evaluated for stroke prevention. In addition to hypercoagulability, increased platelet activation 5–7 is thought to play an important role in thrombus development in patients with atrial fibrillation. Therefore, antiplatelet agents like aspirin, clopidrogel and dipyrdamole are of special interest in stroke prevention. The role of these antiplatelet agents alone or in combination with aspirin for stoke prevention in non-valvular atrial fibrillation (NVAF) is not yet clearly defined. The scope of this article is to review the studies that have looked at anti-platelet agents for stroke prevention, with special focus on dual antiplatelet therapy comprising of aspirin plus clopidogrel.
Platelet Activation and Atrial Fibrillation
Thrombogenesis in the left atrial appendage after onset of atrial fibrillation likely involves platelet activation, platelet aggregation, and increased thrombogenesis. Patients with NVAF have increased levels of serum markers of platelet activation and endothelial dysfunction 6–8. Markers of platelet activation like beta thromboglobulin and platelet factor 4(PF4) are significantly elevated in patients with NVAF as compared to the healthy controls 8. Similarly, levels of D-dimer and beta thromboglobulin are significantly elevated in NVAF patients compared to controls, and elevation of these hemostatic markers is even higher in individuals over age of 75 years 9. The increase in markers of platelet activation is more pronounced after first 12 hours of atrial fibrillation 10. P-selectin, another marker of platelet activation is significantly higher in patient with presence of left atrial thrombus or spontaneous echo contrast seen during echocardiography11. Consistent with these findings, a larger, population based prospective study revealed that patients with higher levels of P-selectin and atrial fibrillation had increased cardiac mortality 11. However, there was no significant difference in the biomarker of endothelial dysfunction and clotting i.e., von Willebrand factor and fibrinogen respectively, in patients with atrial fibrillation and sinus rhythm. Interestingly, no increased risk of ischemic stroke was observed with any of these biomarkers in this study 11. These studies suggest that markers of coagulation are increased in patients with AF 9–13, but elevation of these markers does not necessarily indicate a poor prognosis.
Antiplatelet Monotherapy Therapy in Atrial Fibrillation
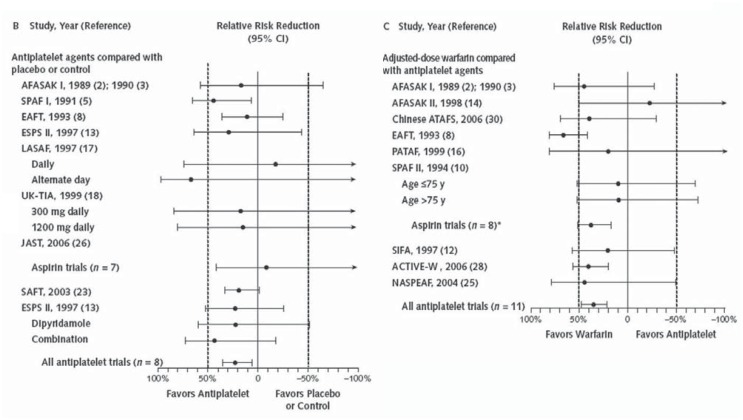
Antiplatelet agents are of interest as platelet activation seems to have some role in thrombogenesis in atrial fibrillation. Several studies have looked at the efficacy of aspirin monotherapy for stroke prevention in NVAF. The current ACC/AHA guidelines recommend aspirin 81 to 325 mg/day for patient with NVAF and no risk factors 12. For patient with NVAF and one moderate risk factor (CHADS2=1), either aspirin 81 to 325mg/day or warfarin can be used for stroke prophylaxis. However, in high risk patients (CHADS2≥1) warfarin is favored over aspirin for stroke prevention in the NVAF population. Eight randomized trials have studied the efficacy of aspirin against placebo in total of 4976 patient with for stroke prevention in NVAF. A meta-analysis of these studies (mean follow up 1.7 years) showed that aspirin alone is modestly effective for preventing stroke in NVAF, with a 22% relative reduction of stroke compared with placebo 1 [figure 1A]. The absolute reduction of stroke with aspirin monotherapy was 0.8% per year for primary prevention and 2.5% per year for secondary prevention. The dose of aspirin varied from 25mg twice daily to 1300mg daily. No significant benefit in stroke prevention was noted with high dose compared to low dose of aspirin (25mg/day). Of note, the point estimate in the studies comparing aspirin and placebo varied widely, suggesting that evidence supporting the use aspirin for stroke prophylaxis is weak and controversial. However, the point estimate of the studies comparing warfarin and placebo were similar, suggesting a clear benefit of warfarin in stroke prophylaxis.
Figures 1A & 1B.
Relative effects of antithrombotic therapies on all stroke from randomized trials in patients with atrial fibrillation1.
1A. Antiplatelet agents compared with placebo or no treatment in 8 randomized trials.
1B. Adjusted-dose warfarin compared with antiplatelet agents in 11 randomized trials.
Moreover, the studies that compared aspirin monotherapy with warfarin monotherapy showed a 40% greater relative reduction with warfarin, suggesting that aspirin is clearly inferior to warfarin in stroke prophylaxis in the high risk patient (figure 1b) 1. Collectively these data suggest that evidence of stroke prophylaxis with aspirin is rather weak as compared to warfarin.
Rationale of Dual Anti-Platelet Therapy in Atrial Fibrillation
Aspirin and clopidogrel inhibit platelet activation by two distinct mechanisms. Aspirin 13 inhibits platelet activation by irreversible inhibition of cycloxygenase and synthesis of thromboxane A2, where as clopidogrel irreversibly inhibits P2Y12, one of the ADP receptors16. Aspirin monotherapy therapy resulted in a reduction in p-selectin in a group of 35 hypertensive patients compared with controls but not in NVAF 14. However, in a clinical trial of twenty patients with NVAF, the use of aspirin plus clopidogrel therapy resulted in significant inhibition of markers of platelet activation i.e, p-selectin. Additionally, dual anti-platelet therapy consisting of aspirin plus clopidrogel resulted in greater inhibition of platelet aggregation, fibrinogen receptor activation and prolongation of in vitro bleeding time with no significant effect on coagulation parameters 15. This dual therapy was noted to cause significant inhibition of platelet aggregation in response to ADP and epinephrine. However, the reduction in markers of platelet activation like Beta-TG and P-selectin was predominately seen with warfarin and not clopidogrel plus aspirin16. Similarly, Lorenzoni et. al. showed that administration of dual anti-platelet therapy (aspirin plus clopidogrel) in non-high risk atrial fibrillation patients results in prolongation of bleeding time 17. On the other hand, warfarin has a more potent effect on coagulation parameters18, and this is also supported by the clinical studies showing significantly greater reduction incidence of stroke with use of warfarin in NVAF. Thus the data available suggests that dual antiplatelet therapy (aspirin and clopidrogel) modestly inhibits thrombogenesis by inhibition of platelet activation and has more effect on platelet aggregation, but the clinical utility of dual antiplatelet therapy in NVAF is not firmly established.
Role of Dual Therapy in Atrial Fibrillation
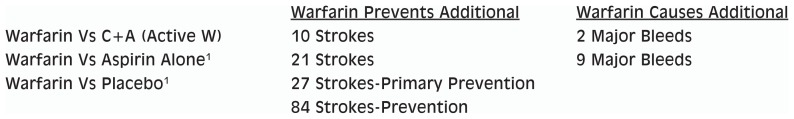
Clopidrogel plus aspirin has been shown to be inferior to warfarin for preventing stroke in patients with NVAF at increased risk for stroke in a recently published randomized clinical trial (Active W) 18. In this randomized trial, 6706 patients with NVAF and one or more risk factors for stroke were randomly assigned to either oral anticoagulation with warfarin or dual antiplatelet therapy clopidrogel (75mg/day) plus aspirin (75–100mg/day). These patients were followed for a median of 1.28 years. Oral anticoagulation therapy was noted to be superior to aspirin plus clopidrogel [annual risk 3.93% vs 5.60%, RR-1.44, 95% CI-1.18–1.76; p-0.0003] for the primary end point, a composite of myocardial infarction, stroke, vascular death, and non central nervous system embolism or stroke. Furthermore, the study was stopped early due clear evidence in favor of warfarin. The annual risk of a primary event with warfarin was 3.93%, compared to an annual risk of 5.6% with in aspirin plus clopidrogel. The comparison of risk benefit per 1000 patients with warfarin in comparison to aspirin, aspirin plus clopidrogel and placebo is shown in figure 2.
Figure 2.
Risk Benefit per 1,000 Patients with Warfarin in Comparison to Aspirin, Aspirin plus Clopidrogel and Placebo
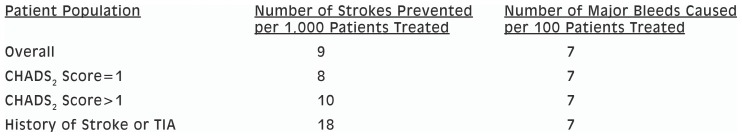
Patients either ineligible for or unwilling to take warfarin were offered entry into the Active A trial19, which compared clopidrogel (75mg/day) plus aspirin (75–100mg/day) versus placebo plus aspirin (75–100mg/day). The patients in ACTIVE A trial were followed for a median of 3.6 years to compare effectiveness of addition of clopidogrel to aspirin for stroke prevention in NVAF. Clopidogrel plus aspirin therapy was superior to aspirin alone for the primary end point of major vascular events with an 11% relative risk reduction. In patients on clopidogrel plus aspirin the event rate for ischemic stroke was 2.4% compared to an event rate of 3.3% per year in patients on placebo plus aspirin (p=0.001, RR 0.72, 95% CI, 0.62–0.83). The use of clopidogrel plus aspirin therapy showed a significant reduction in incidence of both disabling stroke (1.6% vs 2.1%, p=0.0041) and non-disabling stroke (0.9% vs 1.2%, p=0.004) (figure 3). Dual antiplatelet therapy (clopidogrel plus aspirin) resulted in a higher incidence of major bleeding (mostly gastrointestinal) as compared to the aspirin only group (2.0% vs 1.3%, p<0.001, RR-1.57; 95%CI 1.29–1.92). However, the incidence of hemorrhagic stroke was similar in both the study groups. These data support the use of combination of clopidrogel and aspirin in patients at increased risk for stroke who are ineligible for warfarin.
Figure 3.
Risk and Benefit of Dual Aspirin and Clopidogrel Therapy in the ACTIVE-A Trial
Conclusion
From the data available so far, we conclude that for patients with NVAF and high risk for stroke (defined by CHADS2 score ≥2), warfarin is the treatment of choice. Patients with NVAF who do not qualify for warfarin for various reasons can be treated with clopidogrel plus aspirin, as dual antiplatelet therapy results in relative risk reduction in stroke of 28% compared aspirin alone. Future research is required to define the utility of this dual antiplatelet therapy in NVAF.
Biography
Nadish Garg, MD, Arun Kumar, MD, Greg C. Flaker, MD, are at the University of Missouri Hospital and Clinics, Division of Cardiovascular Medicine.
Contact: gargn@health.missouri.edu

Footnotes
Disclosure
None reported.
References
- 1.Hart RG, Pearce LA, Aguilar MI. Meta-analysis: Antithrombotic Therapy to Prevent Stroke in Patients Who Have Nonvalvular Atrial Fibrillation. Ann Intern Med. 2007 Jun 19;146(12):857–67. doi: 10.7326/0003-4819-146-12-200706190-00007. [DOI] [PubMed] [Google Scholar]
- 2.Waldo AL, Becker RC, Tapson VF, Colgan KJ for the NABOR Steering Committee. Hospitalized Patients With Atrial Fibrillation and a High Risk of Stroke Are Not Being Provided With Adequate Anticoagulation. J Am Coll Cardiol. 2005 Nov 1;46(9):1729–36. doi: 10.1016/j.jacc.2005.06.077. [DOI] [PubMed] [Google Scholar]
- 3.Bungard TJ, Ghali WA, Teo KK, McAlister FA, Tsuyuki RT. Why Do Patients With Atrial Fibrillation Not Receive Warfarin? Arch Intern Med. 2000 Jan 10;160(1):41–6. doi: 10.1001/archinte.160.1.41. [DOI] [PubMed] [Google Scholar]
- 4.Hylek EM, D’Antonio J, Evans-Molina C, Shea C, Henault LE, Regan S. Translating the Results of Randomized Trials into Clinical Practice: The Challenge of Warfarin Candidacy Among Hospitalized Elderly Patients With Atrial Fibrillation. Stroke. 2006 Apr 1;37(4):1075–80. doi: 10.1161/01.STR.0000209239.71702.ce. [DOI] [PubMed] [Google Scholar]
- 5.Grau AJ, Ruf A, Vogt A, Lichy C, Buggle F, Patscheke H, Hacke W. Increased fraction of circulating activated platelets in acute and previous cerebrovascular ischemia. Thromb Haemost. 1998;80(2):298–301. [PubMed] [Google Scholar]
- 6.Minamino T, Kitakaze M, Sato H, Asanuma H, Funaya H, Koretsune Y, Hori M. Plasma Levels of Nitrite/Nitrate and Platelet cGMP Levels Are Decreased in Patients With Atrial Fibrillation. Arterioscler Thromb Vasc Biol. 1997 Nov 1;17(11):3191–5. doi: 10.1161/01.atv.17.11.3191. [DOI] [PubMed] [Google Scholar]
- 7.Atalar Enver, Haznedaroglu Ibrahim C, Acil Tayfun, Ozer Necla, Kilic Harun, Ovunc Kenan, Aksoyek Serdar, Nazl Nash, Kes Sirri, Kabak Giray, Kirazl Serafettin, Ozmen Ferhan. Patients with paroxysmal atrial fibrillation but not paroxysmal supraventricular tachycardia display evidence of platelet activation during arrhythmia. Platelets. 2003;14(7):407–11. doi: 10.1080/09537100310001638814. [DOI] [PubMed] [Google Scholar]
- 8.Gustafsson C, Blomback M, Britton M, Hamsten A, Svensson J. Coagulation factors and the increased risk of stroke in nonvalvular atrial fibrillation. Stroke. 1990 Jan 1;21(1):47–51. doi: 10.1161/01.str.21.1.47. [DOI] [PubMed] [Google Scholar]
- 9.Inoue H, Nozawa T, Okumura K, Jong-Dae L, Shimizu A, Yano K. Prothrombotic Activity Is Increased in Patients With Nonvalvular Atrial Fibrillation and Risk Factors for Embolism*. Chest. 2004 Sep;126(3):687–92. doi: 10.1378/chest.126.3.687. [DOI] [PubMed] [Google Scholar]
- 10.Sohara MD, Amitani MD, Kurose MD, Miyahara MD. Atrial Fibrillation Activates Platelets and Coagulation in a Time-Dependent Manner: A Study in Patients With Paroxysmal Atrial Fibrillation. J Am Coll Cardiol. 1997 Jan;29(1):106–12. doi: 10.1016/s0735-1097(96)00427-5. [DOI] [PubMed] [Google Scholar]
- 11.Heeringa J, Conway DS, Van der Kuip DA, Hofman A, Breteler MM, Lip GY, Witteman JC. A longitudinal population-based study of prothrombotic factors in elderly subjects with atrial fibrillation: the Rotterdam Study 1990–1999. J Thromb Haemost. 2006;4(9):1944–9. 1949. doi: 10.1111/j.1538-7836.2006.02115.x. [DOI] [PubMed] [Google Scholar]
- 12.Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S. ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation--Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation) Developed in Collaboration With the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2006 Aug 15;48(4):854–906. doi: 10.1016/j.jacc.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 13.Nadar S, Blann AD, Lip GYH. Effects of Aspirin on Intra-Platelet Vascular Endothelial Growth Factor, Angiopoietin-1, and P-Selectin Levels in Hypertensive Patients[ast] Am J Hypertens. 2006 Sep;19(9):970–7. doi: 10.1016/j.amjhyper.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 14.Storey RF, Judge HM, Wilcox RG, Heptinstall S. Inhibition of ADP-induced P-selectin expression and platelet-leukocyte conjugate formation by clopidogrel and the P2Y12 receptor antagonist AR-C69931MX but not aspirin. Thromb Haemost. 2002;88(3):488–94. [PubMed] [Google Scholar]
- 15.Müller I, Massberg S, Zierhut W, Binz C, Schuster A, Rüdiger-von Hoch S, Braun S, Gawaz M. Effects of aspirin and clopidogrel versus oral anticoagulation on platelet function and on coagulation in patients with nonvalvular atrial fibrillation (CLAFIB) Pathophysiol Haemost Thromb. 2002;32:16–24. doi: 10.1159/000057284. [DOI] [PubMed] [Google Scholar]
- 16.Kamath S, Blann AD, Chin BSP, Lip GYH. A prospective randomized trial of aspirin-clopidogrel combination therapy and dose-adjusted warfarin on indices of thrombogenesis and platelet activation in atrial fibrillation. J Am Coll Cardiol. 2002 Aug 7;40(3):484–90. doi: 10.1016/s0735-1097(02)01984-8. [DOI] [PubMed] [Google Scholar]
- 17.Lorenzoni R, Lazzerini G, Cocci F, De Caterina R. Short-term prevention of thromboembolic complications in patients with atrial fibrillation with aspirin plus clopidogrel: the Clopidogrel-Aspirin Atrial Fibrillation (CLAAF) Pilot Study. American Heart Journal. 2004 Jul;148(1):180. doi: 10.1016/j.ahj.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 18.ACTIVE Writing Group of the ACTIVE Investigators. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomized controlled trial. Lancet. 2006;(367):1903–12. doi: 10.1016/S0140-6736(06)68845-4. [DOI] [PubMed] [Google Scholar]
- 19.Effect of Clopidogrel Added to Aspirin in Patients with Atrial Fibrillation. The ACTIVE Investigators. NEJM. 2009;(360):2066–2078. doi: 10.1056/NEJMoa0901301. [DOI] [PubMed] [Google Scholar]