Abstract
This study evaluated the relationship between sleep quality and symptoms of depression and anxiety in women studied in pregnancy and postpartum. Scores on standardized measures of sleep (PSQI) at 6 months postpartum, and symptoms of anxiety and depression (OASIS, the PHQ9, and EPDS) were assessed by structured interviews in 116 women in pregnancy and/or postpartum. Poor sleep quality was significantly associated with greater symptoms of depression and anxiety. Women who had significantly higher OASIS (anxiety) scores (β = .530, p < .001), PHQ9 (depression) scores (β = .496, p < .001), and EPDS (postpartum depression and anxiety) scores (β = .585, p < .001) also had elevated total PSQI scores after adjustment for covariates, including prenatal depression and anxiety scores. Though inferences about causality are not feasible, these results support emerging research showing sleep quality is a risk factor for negative maternal affect in the postpartum period. Assessment of maternal sleep hygiene is worth consideration as a component of identifying women at risk for postpartum depression and anxiety.
Keywords: sleep quality, depression, anxiety, postpartum, PSQI, EPDS
Introduction
Symptoms of depression and anxiety are common in postpartum women, with prevalence rates of up to 13% (Gavin et al., 2005; Wisner et al., 2006) and 8–11% (Misri & Swift, 2015), respectively. Women who experience these symptoms are more likely to have difficulties establishing and sustaining strong maternal–infant interactions (Gavin et al., 2005; Moehler et al., 2006), difficulties adhering to recommended preventive health services for the infant (Logsdon et al., 2006), and diminished maternal role gratification (Logsdon et al., 2006). Depression and its consequences can have lasting effects including limitations in physical and psychological functioning even following recovery from depressive episodes (Kendler et al., 1993). While less frequently evaluated, anxiety can have similar consequences for maternal overall health and function and can increase postpartum parenting stress (Misri et al., 2010). Identifying the factors which put women at risk for postpartum depression and anxiety is essential to provide clinicians with strategies for mitigating these effects for mothers and infants.
Self-reported sleep disturbances are both common features of depression and anxiety and are used as diagnostic criteria for these disorders (American Psychiatric Association, 2013). Complaints of poor sleep are reported in up to 90% of people with diagnosed depression (Tsuno et al., 2005) and up to 70% of people with anxiety (Alvaro et al.,2013). There is also sufficient evidence to suggest that there is a bi-directional relationship between sleep and mood disturbance (Alvaro et al., 2013). In other words, sleep problems can precede a mood disorder or develop as a result of one; epidemiologic and clinical studies have shown that disturbed sleep is a prodromal symptom of both new and recurrent depressive episodes (Breslau et al., 1996; Ford & Cooper-Patrick, 2001; Perlis et al., 1997). However, there is limited empirical evidence regarding disturbed sleep and anxiety, and there is even less information about the relationship between disturbed sleep and anxiety during the postpartum period (Creti et al., 2017; Goyal et al., 2007; Okun et al., 2009; Okun et al., 2011; Tham et al., 2016; Wolfson et al., 2003).
Tham et al. recently assessed the Edinburgh Postnatal Depression Scale (EPDS) and the State-Trait Anxiety Inventory (STAI) (Spielberger et al., 1970) with the Pittsburgh Sleep Quality Index (PSQI) at 3 months postpartum and found that poor sleep quality was associated with only postnatal depression, not anxiety (Tham et al., 2009). Similarly, a recent paper by Creti et al. reported that poor sleep quality was associated with greater depressive and anxiety symptoms at 2 month postpartum (Creti et al., 2017). In another study, Lewis et al. assessed changes in sleep quality via the PSQI and depressive symptoms on the Patient Health Questionnaire (PHQ9), and found that greater increases on the PSQI from 6 weeks to 7 months postpartum predicted higher depressive symptoms at 7 months postpartum (Lewis et al., 2018). Saxbe and colleagues assessed causal pathways between sleep quality and postpartum depression in both new mothers and fathers (Saxbe et al., 2016). They utilized structural equation modeling to assess whether sleep quality mediated the associations between depressive symptoms measured shortly after birth (1-month) and at 6 and 12 months postpartum. They found that poor sleep quality, as assessed by a 3-item PSQI, was associated with greater depressive symptoms at both 6 months and 12 months postpartum. This association has also been observed among women with a history of postpartum depression as diagnosed by the Structured Clinical Interview for DSM-5 (SCID). Okun et al. examined PSQI scores among postpartum women collected eight times within the first 17 weeks postpartum. They found that PSQI scores were significantly related to recurrence of postpartum depression (SCID assessed) (Okun et al., 2011). Taken together, these findings argue that sleep and postpartum affect is an important research issue as it pertains to maternal and infant health.
Few studies have examined this association in women at 6 months postpartum. The current study provides new information about concurrent measures of sleep quality and maternal affect at this critical time point. Since postpartum depression can be diagnosed up to 1 year postpartum, these data will add to the current clinical understanding of the relationship between sleep quality and symptoms of depression and anxiety in women in the postpartum period. It was predicted that women who were categorized as having poor sleep quality (PSQI scores > 5) would report more symptoms of depression and anxiety at 6 months postpartum.
Methods
Participants
This is a preliminary evaluation of a subset of pregnant women (N = 116) enrolled in a longitudinal study, the Healthy Babies Before Birth study (HB3),which was designed to test the impact of antenatal maternal mood on pregnancy outcome and early infant development, and to examine the biological mechanisms underlying these relationships. Primi- and multiparous women who were 18 years of age or older, with singleton pregnancies and < 18 weeks gestation were eligible if they were able to complete their first visit no later than 16 weeks gestation. Participants were excluded if they had a current substance abuse diagnosis, HIV-positive status, were smokers, and/or had a multiple gestation pregnancy.
Procedures
The study was conducted at two sites with coordinated procedures and data collection. Human subjects research approval was obtained from both institutional review boards. In Los Angeles, participants were recruited for data collection at a west Los Angeles major medical center mainly through direct patient contact at prenatal clinics, but also via brochures in OB/GYN practices, and referral. In Denver, patients were recruited at a prenatal clinic affiliated with a major medical center serving a majority of low-income women. Patients were identified at prenatal appointments, and if eligible, approached to participate in the study. Written informed consent was obtained from all participants who expressed interest.
Upon enrollment, participants were screened for maternal affect with the PHQ-9 and the OASIS. If they scored greater than 10 on the PHQ-9 (excluding the item endorsing fatigue) or above 7 on the OASIS, then a trained researcher conducted the Structured Clinical Interview for DSM-V (SCID) (First MB et al., 1996) to determine lifetime or current Axis I or II diagnosis. In the parent study, participants were seen between 8–16 weeks (T1), 20–26 weeks (T2), 30–36 weeks (T3), and again 4–8 weeks postpartum (P1), approximately 6 months postpartum (P2), and 1-year postpartum (P3). Visits were scheduled either in conjunction with regularly scheduled health care visits or at a time that was convenient for the participant. For the current paper, associations between sleep quality and maternal affect were examined using data from second trimester (T2) and 6 months postpartum (P2) visits. Extensively trained interviewers administered structured interviews that contained the measures reported here. Data were entered directly into REDCAP, a HIPAA compliant database.
Measures
The Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989), an 18-item questionnaire, was used to measure habitual sleep quality over the previous month. It is comprised of 7 subscales assessing habitual duration of sleep, nocturnal sleep disturbances, sleep latency, sleep quality, daytime dysfunction, sleep medication usage, and sleep efficiency. Each subscale has a possible score of between 0–3, with an overall global score of 0–21. Higher scores reflect poorer sleep quality. In reports of various non-pregnant cohorts, a sensitivity of 89.6% and specificity of 86.5% and good internal consistency (Cronbach α = 0.80) are reported when using a cutoff ≤ 5. The PSQI and its psychometric properties have been validated in pregnant women (Qiu et al., 2016; Zhong et al.,2015). The present study used the established cutoff of a score of > 5 to depict poor sleep quality (Buysse et al., 1989). Participants were divided into two groups for analyses: good sleep quality (score ≤ 5) and poor sleep quality (score >5). Sleep quality scores at 6 months postpartum (P2) were used in these analyses.
The Patient Health Questionnaire (PHQ-9) (Kroenke et al., 2001) is a multipurpose instrument for screening, diagnosing, monitoring and measuring the severity of depression symptoms. The diagnostic validity of the PHQ-9 has been established in studies involving several primary care and obstetrical clinics. In previous studies, scores of ≥ 10 had a sensitivity of 88% and a specificity of 88% for major depression. Scores of 5, 10, 15 and 20 represent mild, moderate, moderately severe, and severe depression (Kroenke et al., 2001; Manea et al., 2012). For this study, a cutoff of ≥ 10 was used to define possible depression. The sleep question was removed from the total score in order to reduce collinearity with the PSQI scores. Scores from mid-pregnancy (T2: 20–26 weeks) were assessed as a covariate in the analyses, whereas scores from 6 months postpartum (P2) were the dependent variable of interest.
The Edinburgh Postnatal Depression Scale (EPDS) (Cox et al., 1987) is a 10-item questionnaire which is highly effective for assessing the unique features of depression in the perinatal period. Ratings of items are summed to provide information of the likelihood of a woman exhibiting clinical depression. Validation of the EPDS against a diagnostic clinical interview identified a specificity of 78%, a sensitivity of 86%, and a positive predictive value of 73% for women scoring >10 (Jomeen & Martin, 2007; Murray & Carothers, 1990). In the present study, women were categorized as having antenatal depression if they scored 11 or higher. The EPDS was administered at 6 months postpartum, P2, as used in the present analyses.
The Overall Anxiety Severity and Impairment Scale (OASIS) (Norman et al., 2006) was developed in an effort to fulfill the need for a self-report measure of anxiety that (1) assesses multiple domains of clinical severity including functional impairment; (2) effectively captures severity of any anxiety disorder as well as multiple anxiety disorders; and (3) is brief enough to be used in busy clinical settings such as primary care. The OASIS is a 5-item measure that assesses frequency of anxiety, intensity of anxiety symptoms, behavioral avoidance, and functional impairment associated with anxiety. The instructions for the OASIS ask the patient to consider a variety of experiences such as panic attacks, worries, and flashbacks and to consider all of their anxiety symptoms when answering the questions. The OASIS is therefore potentially applicable to any anxiety disorder and should be able to simultaneously assess severity and impairment associated with multiple anxiety disorders. Moreover, at five items it is one of the shortest anxiety scales available, which enhances its utility for many clinical settings (e.g., primary care) and research purposes (e.g., population-based surveys in which respondent burden is a concern). In this study, a score of 7 was used to indicate a probable anxiety disorder. Scores from second trimester (T2:20–26 weeks) were used as a covariate in the analyses, whereas scores from 6 months postpartum (P2) were the dependent variable of interest.
Other Covariates
All other covariates were assessed at the outset of the study (T1). Covariates assessed included maternal age, race/ethnicity (African-American or Other), marital status (single, living with partner or married), employment (yes or no), and education (college degree or no). BMI was assessed at each visit. The 6-month postpartum (P2) BMI value was used in analyses. Second trimester (T2) depressive (PHQ-9) and anxiety (OASIS) symptom scores were included as covariates in the relevant analyses consistent with previous studies that report that prenatal mood is correlated with postnatal mood symptoms (Okun et al., 2011; Tham et al., 2016).
Data Analysis
Analyses were conducted using SPSS 24.0 (IBM Analytics, New York). Demographic and clinical characteristics of the total cohort, as well as sleep quality group (good or poor), were examined with descriptive and inferential statistics (Table 1). Multivariate linear regression analyses were conducted to test whether sleep quality was associated with continuous measures of postpartum depressive or anxiety symptoms (P2). In Model 1, all the covariates were entered. In Model 2, sleep quality scores (PSQI split) were entered into the analysis. The EPDS was only given in the postpartum, so the regression model did not control for pregnancy scores in analyses. Statistical significance was set at p < .05.
Table 1.
Demographic Characteristics (N = 116)
| Total Cohort | Poor Sleep Quality PSQI >5 N= 57 |
Good Sleep Quality PSQI ≤ 5 N = 59 |
||
|---|---|---|---|---|
| Age | 31.4 ± 5.4 | 31.8 ± 5.15 | 31.2 ±5.65 | NS |
| BMI | 25.6 ± 5.9 | 26.1±5.56 | 24.9±6.19 | NS |
| Marital Status | NS | |||
| Single | 8 (14.3) | 13 (22.4) | ||
| Living with Partner | 5 (8.9) | 1 (1.7) | ||
| Married | 43 (76.8) | 44 (75.9) | ||
| Race | NS | |||
| Caucasian | 58 (47.5) | 27 (47.4) | 27 (45.8) | |
| African-American | 9 (7.4) | 2 (3.5) | 7 (11.9) | |
| Asian-American | 11 (9.0) | 5 (8.8) | 6 (10.2) | |
| Multi-racial | 13 (10.7) | 8 (14.0) | 5 (8.5) | |
| Hispanic origin/descent | 28 (23.0) | 13 (22.8) | 13 (22.0) | |
| Other/Refused | 2 (1.6) | 1 (1.8) | 1 (1.7) | |
| Employed | NS | |||
| Yes | 92 (75.4) | 46 (80.7) | 42 (71.2) | |
| No | 30 (24.6) | 11 (19.3) | 17 (28.8) | |
| College Degree | NS | |||
| Yes | 83 (68.0) | 42 (73.7) | 36 (61.0) | |
| No | 39 (32.0) | 15 (26.3) | 23 (39.0) |
Results
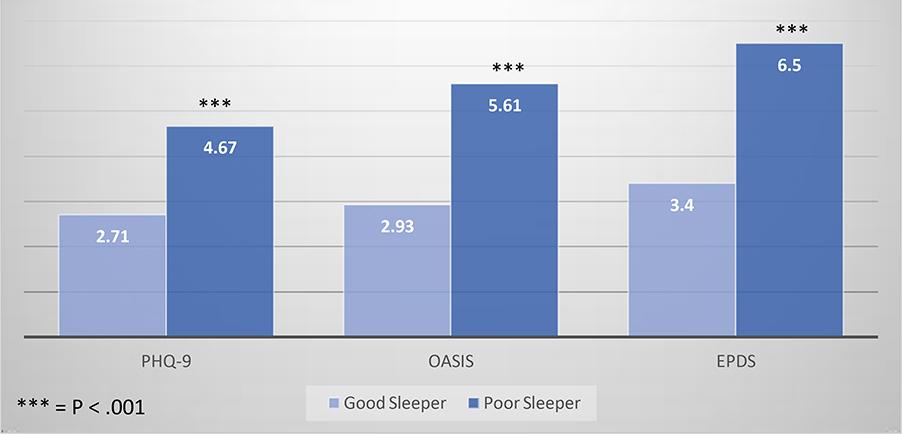
There were no differences between poor and good sleepers on any of the demographic variables (Table 1). There were significant differences between poor and good sleepers at 6 months postpartum on postnatal OASIS scores (4.67 ± 3.75 vs. 2.71± 2.53, t = −3.28, p = .001), the PHQ9 (5.61 ± 4.82 vs. 2.93 ± 2.63, t = −3.70, p < .001), and scores on the EPDS (6.5 ± 5.07 vs. 3.4 ± 3.36, t = −3.85, p < .001) (Figure 1). Although the average scores on the OASIS did not reach the identified threshold, twelve of the 116 (10.3%) scored ≥ 8 on the OASIS, suggesting the possible presence of an anxiety disorder. Average scores on the PHQ9 among those with poor sleep suggested mild depression (scores 5–9). However, upon closer examination, 35(30.2%) scored 5–9 (mild depressive symptoms), 5 (4.3%) scored 10–14 (moderate depressive symptoms), and 3(2.5%) scored ≥ 20 (severe depressive symptoms). Lastly, scores on the EPDS in this sample showed 11 women (9.5%) scored 11 or greater, which suggests possible postpartum depression or anxiety.
Figure 1.
Postpartum Women with poor sleep quality have greater depressive and anxiety symptoms
To assess the degree to which postpartum sleep quality was associated with each of the 3 postnatal mood measurements, multivariate linear regression analyses were conducted. Regression coefficients for sleep quality and maternal affect at 6 months postpartum, adjusted for age, employment, race/ethnicity, BMI, marital status, education, and PHQ-9 or OASIS scores (where appropriate) at mid-pregnancy are displayed in Tables 2–4. Women with poor sleep quality at 6 months postpartum had significantly higher postpartum PHQ9 (depression) scores (β = .191, p =.036) (Table 2), OASIS (anxiety) scores (β = .233, p = .012) (Table 3), and EPDS (postpartum depression and anxiety) scores (β = .369, p < .001) (Table 4) after adjustment for all covariates. As shown in Tables 2 & 3, prenatal depressive (β = .477, p < .001) and anxiety (β = .233, p < .001) symptoms significantly predicted higher depressive and anxiety symptom scores at 6 months postpartum.
Table 2.
Multivariate Linear Regression Models Testing Whether Poor Sleep Quality is Associated with Depressive Symptoms (PHQ9) (Full Model)
| Variable | B | SE β | β | Statistical Significance |
|---|---|---|---|---|
| Age | .103 | .064 | .152 | .1 |
| Employment | −.750 | .753 | −.086 | .322 |
| Current BMI | .010 | .054 | .017 | .851 |
| Race/Ethnicity (Black or other) | −.136 | 1.258 | −.009 | .914 |
| Marital Status | −.018 | .031 | −.057 | .568 |
| College Degree | −.340 | .614 | −.055 | .581 |
| Prenatal depression (PHQ9 at T2 (20–26 weeks) sleep variable removed | .704 | .130 | .477 | <.001 |
| PSQI split | 1.370 | .644 | .191 | .036 |
Table 4.
Multivariate Linear Regression Models Testing Whether Poor Sleep Quality is Associated with Postpartum Depression or Anxiety Symptoms (EPDS)
| Variable | B | SE β | β | Statistical Significance |
|---|---|---|---|---|
| Age | .150 | .091 | .172 | .101 |
| Employment | −2.633 | 1.063 | −.234 | .015 |
| Current BMI | .065 | .074 | .085 | .386 |
| Race/Ethnicity (Black or Other) |
−.916 | 1.787 | −.049 | .609 |
| Marital Status | −.076 | .043 | −.188 | .083 |
| College Degree | .032 | .850 | .004 | .970 |
| PSQI split | 3.419 | .877 | .369 | <.001 |
Table 3.
Multivariate Linear Regression Models Testing Whether Poor Sleep Quality is Associated with Anxiety Symptoms (OASIS) (Full Model)
| Variable | B | SE β | β | Statistical Significance |
|---|---|---|---|---|
| Age | .056 | .059 | .095 | .342 |
| Employment | −.968 | .687 | −.127 | .162 |
| Current BMI | −.134 | .050 | −.26 | .008 |
| Race/Ethnicity (Black or Other) |
.640 | 1.159 | .051 | .582 |
| Marital Status | −.023 | .028 | −.085 | .417 |
| College Degree | .058 | .564 | .011 | .918 |
|
Prenatal anxiety (OASIS at T2
(20–26 weeks) |
.436 | .096 | .414 | < .001 |
| PSQI split | 1.465 | .570 | .233 | .012 |
Discussion
In this preliminary test of the relationship between maternal sleep quality and affect at 6 months postpartum, poor sleep quality was found to be significantly associated with greater depressive and anxiety symptoms in women who had 6-month old infants. This association was significant even after controlling for prenatal depression or anxiety symptoms.
These findings are in line with much of the extant literature examining sleep quality and postpartum mood, although there are some notable differences. Specifically, in a study of similar design, Tham et al. found that poor sleep quality was associated with only postnatal depression, not anxiety at 3 months postpartum (Tham et al., 2009). However, Creti et al.’s (Creti et al., 2017) results are consistent with the present findings, regarding anxiety, suggesting these associations are reliable. Importantly, the present findings are consistent with several other studies that have reported cross-sectional or longitudinal data about pregnancy-assessed sleep quality or postpartum-assessed sleep quality, contributing to an overall understanding that these associations are meaningful. Yet, we contend that additional work remains to be done to fully elucidate their magnitude, impact, and the mechanisms which underlie them (Bei et al., 2010; Jomeen J & Martin C.R., 2007; Okun et al., 2009; Okun et al., 2011; Tham et al., 2016; Tomfohr et al., 2015). For instance, we found significant differences in BMI in the model assessing poor sleep quality and anxiety symptoms. The negative Beta suggests lower BMI might indirectly be associated with smoking or poor nutrition, all of which are associated with poor fetal growth (Abeysena & Jayawardana, 2011; Luke, 2005). Future studies need to examine mothers longitudinally after delivery and extend further through the postpartum period.
While it is accepted that sleep quality is often disturbed during pregnancy and the postpartum period, there is still a gap in the knowledge as to why this occurs. Commonly, poor sleep quality is attributed to physical discomfort, an increased need to urinate, lower back pain or restless legs syndrome, particularly in the third trimester. However, there is evidence that excessive inflammation (Blair et al., 2015; Okun & Coussons-Read, 2007; Okun et al., 2007; Okun et al., 2013) or hormonal dysregulation (Okun et al., 2011; Suzuki et al., 1993; TeranPerez et al., 2012) may contribute to poor sleep quality. Additional work is needed to determine whether these biological pathways mediate or moderate the association between sleep and maternal mood. Recently, some researchers have suggested that circadian rhythm disruptions may account for the increased risk in mood disorders. Patterns of fatigue were noted to vary by sleep patterns and sleep midpoints among postpartum women (Sharkey et al., 2013; WirzJustice, 2006). McBean and colleagues suggest that chronobiology plays a role in fatigue patterns during the postpartum period and that having a rhythmic pattern of fatigue (a statistically significant linear, cubic, or quadratic trend in fatigue over time) may be advantageous for mental health outcomes (Mcbean & Montgomery-Downs, 2015). Assessing sleep in the postpartum period and beyond is important due to robust associations with wake disturbance, fatigue, and depression/anxiety (Sharkey et al., 2013).
There are some limitations of this study. First, this is a preliminary report of sleep quality measured only once. Sleep is recognized to change, and often worsen, across the perinatal period, so a single determination only provides a snapshot of the relationships which are affecting mothers and infants during this critical period (Krawczak et al., 2016; Tomfohr et al., 2015). Future work will include repeated measures of sleep quality during pregnancy and through 1 year postpartum. Moreover, there is no objective measurement of sleep. Actigraphy was not feasible in the current study design. Future studies need to include this methodology. The ultimate goal of this work is to help determine the best methods of intervention to support better sleep quality in the perinatal period and the optimal duration for the implementation of such interventions. Second, we did not collect any data on daytime naps. Daytime naps can impact nocturnal sleep particularly among older adults (Dautovich et al., 2008; Hays et al., 1996), but this does not appear to apply to pregnant women, as it may be a good countermeasure to nocturnal sleep disruption (Ebert et al., 2015). As with all cross-sectional research designs, causal inference is not possible, but the connections illustrated in the present work and the work of others exploring this area continues to support the need to extend this research. Future studies should include additional measures and pursue deeper understanding of the relationships between maternal mood, sleep, and postpartum mother-infant interactions and mechanisms. For example, future studies should collect information on bedsharing with the infant and breastfeeding behavior as these could impact sleep quality.
In conclusion, the present data indicate a clear association between poor sleep quality and depression and anxiety symptoms in women at 6 months postpartum, and after adjusting for prenatal mood scores and many other variables. Not surprisingly, prenatal mood scores were strongly correlated with postpartum scores, but their inclusion did not diminish the impact of poor sleep quality on mood during the postpartum period. These findings support the need for clinicians to inquire about sleep quality during the perinatal period to more fully support mothers and infants during the critical first months of development. Future studies should also examine the efficacy and incorporation of behavioral interventions, such as cognitive behavioral therapy for insomnia (CBT-I), mindfulness meditation, and relaxation techniques, as there is growing evidence that behavioral interventions are helpful for both sleep issues as well as mood symptoms (Tomfohr-Madsen et al., 2016; Davidson, 2009; Taylor et al., 2007).
Acknowledgments
Funding Source: NIH (R01 HD073491: MPI Coussons-Read & Dunkel Schetter) Miriam Jacobs Chair Maternal Fetal Medicine: Calvin J. Hobel, MD
Index
- PSQI
Pittsburgh Sleep Quality Index
- PHQ9
Patient Health Questionnaire −9-item
- EPDS
Edinburgh Postnatal Depression Scale
- OASIS
Overall Anxiety Severity and Impairment Scale
- SCID
Structured Clinical Interview for DSM-5
Footnotes
Conflict of Interest: The authors declare that they have no conflicts of interest
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Reference List
- Abeysena C & Jayawardana P (2011). Sleep deprivation, physical activity and low income are risk factors for inadequate weight gain during pregnancy: a cohort study. Journal of Obstetrics and Gynaecology Research, 37, 734–740. [DOI] [PubMed] [Google Scholar]
- Alvaro PK, Roberts RM, & Harris JK (2013). A Systematic Review Assessing Bidirectionality between Sleep Disturbances, Anxiety, and Depression. Sleep, 36, 1059–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-V). (Fifth Edition, Text Revision ed.) Washington, DC: American Psychiatric Association. [Google Scholar]
- Blair LM, Porter K, Leblebicioglu B, & Christian LM (2015). Poor Sleep Quality and Associated Inflammation Predict Preterm Birth: Heightened Risk among African Americans. Sleep, 38, 1259–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Roth T, Rosenthal L, & Andreski P (1996). Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biological Psychiatry, 39, 411–418. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28, 193–213. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, & Sagovsky R (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry, 150, 782–786. [DOI] [PubMed] [Google Scholar]
- Creti L, Libman E, Rizzo D, Fichten CS, Bailes S, Tran DL et al. (2017). Sleep in the Postpartum: Characteristics of First-Time, Healthy Mothers. Sleep Disorders., 2017, 8520358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dautovich ND, McCrae CS, & Rowe M (2008). Subjective and Objective Napping and Sleep in Older Adults: Are Evening Naps “Bad” for Nighttime Sleep? Journal of the American Geriatrics Society. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson JR (2009). Insomnia treatment options for women. Obstetrics and Gynecology Clinics of North America, 36, 831–8xi. [DOI] [PubMed] [Google Scholar]
- Ebert RM, Wood A, & Okun ML (2015). Minimal Effect of Daytime Napping Behavior on Nocturnal Sleep in Pregnant Women. Journal of Clinical Sleep Medicine, 11, 635643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, & Williams JBW (1996). User’s Guide for the Structured Interview for DSM-IV Axis I Disorders - Research Version (SCID-1, version 2.0, February 1996 final version). In ( New York: Biometrics Research. [Google Scholar]
- Ford DE & Cooper-Patrick L (2001). Sleep disturbances and mood disorders: an epidemiologic perspective. Depression and Anxiety, 14, 3–6. [DOI] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, & Swinson T (2005). Perinatal depression: a systematic review of prevalence and incidence. Obstetrics and Gynecology, 106, 1071–1083. [DOI] [PubMed] [Google Scholar]
- Goyal D, Gay CL, & Lee KA (2007). Patterns of sleep disruption and depressive symptoms in new mothers. Journal of Perinatal and Neonatal Nursing, 21, 123–129. [DOI] [PubMed] [Google Scholar]
- Hays JC, Blazer DG, & Foley DJ (1996). Risk of napping: excessive daytime sleepiness and mortality in an older community population. Journal of the American Geriatrics Society, 44, 693–698. [DOI] [PubMed] [Google Scholar]
- Jomeen J & Martin CR (2007). Replicability and stability of the multidimensional model of the Edinburgh Postnatal Depression Scale in late pregnancy. Journal of Psychiatric and Mental Health Nursing, 14, 319–324. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, & Eaves LJ (1993). A longitudinal twin study of 1-year prevalence of major depression in women. Archives of General Psychiatry, 50, 843–852. [DOI] [PubMed] [Google Scholar]
- Krawczak EM, Minuzzi L, Hidalgo MP, & Frey BN (2016). Do changes in subjective sleep and biological rhythms predict worsening in postpartum depressive symptoms? A prospective study across the perinatal period. Archives of Womens Mental Health. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis BA, Gjerdingen D, Schuver K, Avery M, & Marcus BH (2018). The effect of sleep pattern changes on postpartum depressive symptoms. BioMed Central Womens Health, 18, 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logsdon MC, Wisner KL, & Pinto-Foltz MD (2006). The impact of postpartum depression on mothering. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 35, 652–658. [DOI] [PubMed] [Google Scholar]
- Luke B (2005). The evidence linking maternal nutrition and prematurity. Journal of Perinatal Medicine, 33, 500–505. [DOI] [PubMed] [Google Scholar]
- Manea L, Gilbody S, & McMillan D (2012). Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. Canadian Medical Association Journal, 184, E191–E196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcbean AL & Montgomery-Downs HE (2015). Diurnal fatigue patterns, sleep timing, and mental health outcomes among healthy postpartum women. Biological Research for Nursing, 17, 29–39. [DOI] [PubMed] [Google Scholar]
- Misri S, Kendrick K, Oberlander TF, Norris S, Tomfohr L, Zhang H et al. (2010). Antenatal depression and anxiety affect postpartum parenting stress: a longitudinal, prospective study. Canadian Journal of Psychiatry.Revue Canadienne de Psychiatrie, 55, 222–228. [DOI] [PubMed] [Google Scholar]
- Misri S & Swift E (2015). Generalized Anxiety Disorder and Major Depressive Disorder in Pregnant and Postpartum Women: Maternal Quality of Life and Treatment Outcomes. Journal of Obstetrics and Gynaecology Canada, 37, 798–803. [DOI] [PubMed] [Google Scholar]
- Moehler E, Brunner R, Wiebel A, Reck C, & Resch F (2006). Maternal depressive symptoms in the postnatal period are associated with long-term impairment of motherchild bonding. Archives of Womens Mental Health, 9, 273–278. [DOI] [PubMed] [Google Scholar]
- Murray L & Carothers AD (1990). The validation of the Edinburgh Post-natal Depression Scale on a community sample. British Journal of Psychiatry, 157, 288–290. [DOI] [PubMed] [Google Scholar]
- Norman SB, Cissell SH, Means-Christensen AJ, & Stein MB (2006). Development and validation of an Overall Anxiety Severity And Impairment Scale (OASIS). Depression and Anxiety, 23, 245–249. [DOI] [PubMed] [Google Scholar]
- Okun ML & Coussons-Read ME (2007). Sleep disruption during pregnancy: how does it influence serum cytokines? Journal of Reproductive Immunology, 73, 158–165. [DOI] [PubMed] [Google Scholar]
- Okun ML, Hall M, & Coussons-Read ME (2007). Sleep disturbances increase interleukin6 production during pregnancy: implications for pregnancy complications. Reproductive Science, 14, 560–567. [DOI] [PubMed] [Google Scholar]
- Okun ML, Hanusa BH, Hall M, & Wisner KL (2009). Sleep complaints in late pregnancy and the recurrence of postpartum depression. Behavioral Sleep Medicine, 7, 106–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okun ML, Luther J, Prather AA, Perel JM, Wisniewski S, & Wisner KL (2011). Changes in sleep quality, but not hormones predict time to postpartum depression recurrence. Journal of Affective Disorders, 130, 378–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okun ML, Luther JF, Wisniewski SR, & Wisner KL (2013). Disturbed sleep and inflammatory cytokines in depressed and nondepressed pregnant women: an exploratory analysis of pregnancy outcomes. Psychosomatic Medicine, 75, 670–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlis ML, Giles DE, Buysse DJ, Tu X, & Kupfer DJ (1997). Self-reported sleep disturbance as a prodromal symptom in recurrent depression. Journal of Affective Disorders, 42, 209–212. [DOI] [PubMed] [Google Scholar]
- Qiu C, Gelaye B, Zhong QY, Enquobahrie DA, Frederick IO, & Williams MA (2016). Construct validity and factor structure of the Pittsburgh Sleep Quality Index among pregnant women in a Pacific-Northwest cohort. Sleep and Breathing, 20, 293–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxbe DE, Schetter CD, Guardino CM, Ramey SL, Shalowitz MU, Thorp J et al. (2016). Sleep Quality Predicts Persistence of Parental Postpartum Depressive Symptoms and Transmission of Depressive Symptoms from Mothers to Fathers. Annals of Behavioral Medicine, 50, 862–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkey KM, Pearlstein TB, & Carskadon MA (2013). Circadian phase shifts and mood across the perinatal period in women with a history of major depressive disorder: a preliminary communication. Journal of Affective Disorders, 150, 1103–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, & Lushene RE. (1970). Manual for the State-Trait Anxiety Inventory (Form Y). Palo Alto, CA, Consulting Psychologists Press. [Google Scholar]
- Suzuki S, Dennerstein L, Greenwood KM, Armstrong SM, Sano T, & Satohisa E (1993). Melatonin and hormonal changes in disturbed sleep during late pregnancy. Journal of Pineal Research, 15, 191–198. [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Lichstein KL, Weinstock J, Sanford S, & Temple JR (2007). A pilot study of cognitive-behavioral therapy of insomnia in people with mild depression. Behavioral Therapy, 38, 49–57. [DOI] [PubMed] [Google Scholar]
- Teran-Perez G, Arana-Lechuga Y, Esqueda-Leon E, Santana-Miranda R, Rojas-Zamorano JA, & Velazquez MJ (2012). Steroid hormones and sleep regulation. Mini Reviews in Medicinal Chemistry, 12, 1040–1048. [DOI] [PubMed] [Google Scholar]
- Tham E, Liu J, Innis S, Thompson D, Gaylinn BD, Bogarin R et al. (2009). Acylated ghrelin concentrations are markedly decreased during pregnancy in mothers with and without gestational diabetes: relationship with cholinesterase. American Journal of Physiology, Endocrinology and Metabolism, 296, E1093–E1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tham EK, Tan J, Chong YS, Kwek K, Saw SM, Teoh OH et al. (2016). Associations between poor subjective prenatal sleep quality and postnatal depression and anxiety symptoms. Journal of Affective Disorders, 202, 91–94. [DOI] [PubMed] [Google Scholar]
- Tomfohr LM, Buliga E, Letourneau NL, Campbell TS, & Giesbrecht GF (2015). Trajectories of Sleep Quality and Associations with Mood during the Perinatal Period. Sleep, 38, 1237–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomfohr-Madsen LM, Clayborne ZM, Rouleau CR, & Campbell TS (2016). Sleeping for Two: An Open-Pilot Study of Cognitive Behavioral Therapy for Insomnia in Pregnancy. Behavioral Sleep Medicine, 1–17. [DOI] [PubMed] [Google Scholar]
- Tsuno N, Besset A, & Ritchie K (2005). Sleep and depression. Journal of Clinical Psychiatry, 66, 1254–1269. [DOI] [PubMed] [Google Scholar]
- Wirz-Justice A (2006). Biological rhythm disturbances in mood disorders. International Clinical Psychopharmacology, 21 Suppl 1, S11–S15. [DOI] [PubMed] [Google Scholar]
- Wisner KL, Chambers C, & Sit DK (2006). Postpartum depression: a major public health problem. Journal of the American Medical Association, 296, 2616–2618. [DOI] [PubMed] [Google Scholar]
- Wolfson AR, Crowley SJ, Anwer U, & Bassett JL (2003). Changes in sleep patterns and depressive symptoms in first-time mothers: last trimester to 1-year postpartum. Behavioral Sleep Medicine, 1, 54–67. [DOI] [PubMed] [Google Scholar]
- Zhong QY, Gelaye B, Sanchez SE, & Williams MA (2015). Psychometric Properties of the Pittsburgh Sleep Quality Index (PSQI) in a Cohort of Peruvian Pregnant Women. Journal of Clinical Sleep Medicine, 11, 869–877. [DOI] [PMC free article] [PubMed] [Google Scholar]