Abstract
AIM
To determine the prevalence of vision impairment (VI) and refractive error in first year university students at the Tianjin Medical University.
METHODS
This is a cross-sectional observational cohort study of VI and refractive error among first year university students at the Tianjin Medical University. The first year university students were involved in this study and were given a detailed questionnaire including age, birth date, and spectacle wearing history. A standardized ophthalmologic examination including visual acuity (VA), slit-lamp examination, non-cycloplegic auto-refraction, objective refraction, fundus photography, and examination of their spectacles were recorded.
RESULTS
A total of 3654 participants were included in this study. Totally 3436 (94.03%) individuals had VI in this population. Totally 150 (4.10%) individuals had VI due to ocular disease, including amblyopia, congenital cataract, retinal atrophy or degeneration, strabismus, congenital nystagmus, refractive surgery orthokeratology. Totally 3286 (89.93%) subjects had VI due to refractive error. Only 218 (5.97%) students were emmetropia. Moreover, refractive error was the main cause for the VI (95.63%). Totally 3242 (92.52%) students were myopia and the prevalence of mild, moderate, and high myopia subgroup was 27.05%, 44.35%, and 21.26% respectively. Totally 44 (1.29%) subjects were hyperopic. The rates of uncorrected visual acuity (UCVA), presenting visual acuity (PVA) and best corrected visual acuity (BCVA) which better than 20/20 in both eyes were 5.65%, 22.32% and 82.13% respectively. The rates of correction, under correction and well correction in myopia subjects were 82.73%, 84.39% and 15.61%, respectively.
CONCLUSION
We present a high prevalence of refractive errors and high rates of under correction refractive error among first year university students. These results may help to promote vision protection work in young adults.
Keywords: vision impairment, refractive error, corrective status, myopia, first year university students
INTRODUCTION
Vision impairment (VI) is the main factor that hampers people's daily activities and quality of life. According to the World Health Organization (WHO), an estimated 253 million people live with VI and 217 million have moderate to severe VI. Uncorrected or under-corrected refractive error is the leading causes (53%) of VI and the second cause (21%) of blindness globally[1]. Moreover, approximately 19 million children and adolescents 5 to 15y of age suffer from VI, and approximately 12 million children have a VI due to refractive error, especially myopia[2]. VI due to refractive error has become a common social and public health problem in young people globally.
Recently, some studies reported the prevalence of myopia surpassed 90% in university students[3] in China compared with 60% among 12-year-old after primary school[4], 80% at 16-year-old after junior high school[5]. The high prevalence of myopia in university students attracted our sight. As far as we know, over 72% of myopia aged over 18 years old in East Asians lived in China[6]. The prevalence of myopia was high in Chinese adolescents and increased as age increased[7]. This adolescent myopia not only is simply refractive error but also can progress to high myopia and pathologic myopia[8], which finally leads to irreversible vision loss[9]. Adolescent myopia has become a remarkable public health problem in Chinese young people, especially in university students[3],[10]–[11].
Previous studies on VI are mostly focused on children below age 15, little is known about VI in university students (age 18 and over). The survey of VI and refractive error in this population is limited. Our study presented detailed analysis on the prevalence of VI and refractive error in a specific population of first year university students at Tianjin Medical University (TMU). These results may help to promote vision protection work in young adults.
SUBJECTS AND METHODS
This study was approved by the Ethics Committee of Tianjin Medical University Eye Hospital, and adhered to the tenets of the Declaration of Helsinki. Informed written consent was obtained from at least one parent of 71 students whose age was less than 18y old.
Study Population
Totally 3754 students from TMU were registered for this study and 3654 students were finished all examinations in this study from October 2016 to October 2017 (response rates 97.34%). Eventually, 3654 students were involved in this study.
Examinations
This study was done by a team consisting of one qualified ophthalmologist, two optometrists, and five optometry assistants. A training course was conducted to ensure all questions would be asked under the same criteria and a standard procedure was made for the whole outcome recording during the study.
All participants were required to complete a questionnaire which contained personal information and spectacle wearing habits. A regular ocular examination was performed using a slit-lamp and fundus ophthalmoscope (66 Vision Tech Co., Ltd., Suzhou, China) to check ocular abnormalities.
Visual acuity (VA) was measured using a standard logarithmic VA chart with Tumbling-E optotypes and the uncorrected visual acuity (UCVA) was recorded. Best corrected visual acuity (BCVA) and presenting visual acuity (PVA) was measured in all students. PVA refers to the daily present vision for student, PVA was recorded as follows: 1) if a person usually does not wear spectacles, then it takes naked eye vision as PVA; 2) if a person usually wears spectacles where the spectacles are appropriate, it takes the vision wearing the spectacles as PVA; 3) if a person has spectacles barely wearing it, it takes naked eye vision as PVA.
An automatic refractometer (model KR 8900; Topcon, Tokyo, Japan) and a photometer (VT10; Topcon, Tokyo, Japan) was used to measure the degree of the refractive error. Refractive errors [spherical (S), cylinder (C), axis (α)] were recorded after three repetitions.
Spherical equivalent (SE) was calculated according to the following formula: SE=S+C/2. Refractive errors were classified according to SE. Emmetropia was defined as refractive error less than 0.50 diopter (D). Myopia was the SE degree <-0.50 D, Hyperopia was the SE degree >0.50 D. Astigmatism was defined as a cylinder more than 0.50 D. Myopia was also classified into mild, moderate, and high myopia as an SE of -0.50 to -3.00 D, -3.00 to -6.00 D, and more than -6.00 D, respectively.
Statistical Analysis
The statistical analysis were performed using SPSS statistical package version 23.0 (IBM Corporation, Armonk, NY, USA). All numerical data were given as the mean±SD. The prevalence of refractive error between males and females were compared using the Chi-square statistic. P value was two-side and considered significantly when P<0.05.
RESULTS
The Prevalence of Vision Impairment
Totally 3654 participants were involved in this study. Totally 3436 (94.03%) subjects had VI in this population (Table 1). Totally 150 (4.10%) individuals had VI due to ocular disease, including amblyopia, congenital cataract, retinal atrophy or degeneration, strabismus, congenital nystagmus, refractive surgery or orthokeratology. Totally 3286 (89.93%) subjects had VI due to refractive error. Only 218 (5.97%) students were emmetropia. Moreover, refractive error was the main cause for the VI (95.63%).
Table 1. Causes of visual impairment.
| Causes of VI | Students with VI (one or both eyes) | Prevalence in the population n=3654 (%) |
| Refractive error | 3286 (95.63) | 89.92 |
| Amblyopia | 36 (1.05) | 0.99 |
| Congenital cataract | 20 (0.58) | 0.55 |
| Retinal atrophy or degeneration | 24 (0.70) | 0.66 |
| Strabismus | 10 (0.29) | 0.27 |
| Congenital nystagmus | 6 (0.17) | 0.16 |
| Surgery and orthokeratology | 54 (1.57) | 1.48 |
| Total | 3436 (100) | 94.03 |
n (%)
The Prevalence of Refractive Errors
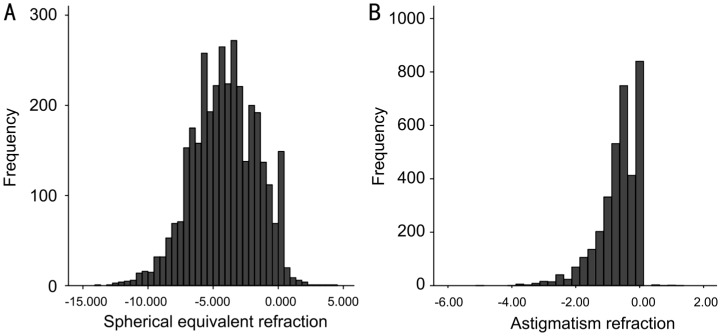
Totally 3504 individuals were involved in the refractive error analysis after eliminating participants of ocular disease. This population included 1330 (37.96%) males and 2174 (62.04%) females. The mean age was 18.83±0.92y. In total 7008 eyes, the mean SE was -4.11±2.49 D (Figure 1A) and the mean diopter of astigmatism was -0.66±0.64 D (Figure 1B). Table 2 showed the prevalence of different type of refractive errors. Totally 218 subjects (6.22%) were emmetropia and it was significantly higher in males (7.97%) than females (5.15%) (Chi-square=6.616, P=0.018). Totally 44 subjects (1.26%) were hyperopia and there was no remarkably difference in males (1.80%) and females (0.92%) (Chi-square=2.604, P=0.107). Totally 3242 (92.52%) individuals were myopia. Moreover, the number of students who had mild myopia, moderate and high myopia were 948 (27.05%), 1554 (44.35%) and 740 (21.12%), respectively. Female students had a higher prevalence in the myopia group (Chi-square=4.556, P=0.004) and the mild myopia subgroup (Chi-square=4.871, P=0.027) comparing with male students. The prevalence of astigmatism was 64.16% and indicated no remarkable difference with gender (Chi-square=0.304, P=0.582).
Figure 1. The distribution of refractive errors in the 3504 subjects.
A: The distribution of SE refraction (mean SE=-4.11±2.49 DS); B: The distribution of astigmatism (mean astigmatism diopter =-0.66±0.64 DC).
Table 2. The prevalence of refractive error in this study.
| Groups | Total | Male | Female | P |
| Emmetropia | 218 (6.22) | 106 (7.97) | 112 (5.15) | 0.018 |
| Hyperopia | 44 (1.26) | 24 (1.80) | 20 (0.92) | 0.107 |
| Myopia | 3242 (92.52) | 1200 (90.23) | 2042 (93.93) | 0.004 |
| Mild myopia | 948 (27.05) | 320 (24.06) | 628 (28.89) | 0.027 |
| Moderate myopia | 1554 (44.35) | 612 (46.02) | 942 (43.33) | 0.272 |
| High myopia | 740 (21.12) | 268 (20.15) | 472 (27.71) | 0.437 |
| Astigmatism | 2248 (64.16) | 864 (64.96) | 1384 (63.66) | 0.582 |
n (%)
Visual Acuity
Totally 198 (5.65%) students had a UCVA better than 20/20 in both eyes and 2394 (68.32%) students less than 20/63 in the better eye. A total of 2678 students (76.43%) wore spectacles for vision correction. There were 782 (22.32%) individuals who had PVA better than 20/20 in both eyes and 746 (21.29%) students had PVA better than 20/20 in one eye only, while the PVA of 1168 (33.33%) students were between 20/25 and 20/20. The PVA of 112 (3.20%) students were worse than 20/63 in the better eye. After vision correction, 2878 (82.13%) students can achieve BCVA better than 20/20 in both eyes in 3504 subjects (Table 3).
Table 3. Distribution of first year university students in UCVA, PVA, and BCVA.
| VA category | UCVA | Wearing spectacles | PVA | BCVA |
| ≥ 20/20 both eyes | 198 (5.65) | 4 (2.02) | 782 (22.32) | 2878 (82.13) |
| ≥ 20/20 one eye only | 246 (7.02) | 32 (13.01) | 746 (21.29) | 358 (10.22) |
| <20/20 to ≥20/25 better eye | 152 (4.34) | 34 (22.37) | 1168 (33.33) | 268 (7.65) |
| <20/25 to ≥ 20/40 better eye | 306 (8.73) | 166 (54.25) | 438 (12.50) | 0 (0.00) |
| <20/40 to ≥ 20/63 better eye | 208 (5.94) | 128 (61.54) | 258 (7.36) | 0 (0.00) |
| < 20/63 better eye | 2394 (68.32) | 2314 (96.66) | 112 (3.20) | 0 (0.00) |
| All | 3504 (100.00) | 2678 (76.43) | 3504 (100.00) | 3504 (100.00) |
n (%)
Habits of Spectacle Wearing
Spectacles is one of the approaches for correction of refractive error. Table 4 showed habits of spectacle wearing in the students of our study. Among the 2678 participants who wore spectacles, 1712 (63.93%) subjects wore spectacles constantly, 966 (36.07%) students wore spectacles when necessary such as driving, reading and studying. The number of students changing spectacles every year was 436 (32.57%), the number of students for changing spectacles every 2, 3y and more than 3y were 1276 (47.65%), 332 (12.42%) and 198 (7.36%) respectively. Totally 228 (6.51%) students worn spectacles less than 1y. The numbers of students wearing spectacles with 1-3y, 3-5y 5-8y, 8-10y were 562 (16.04%), 808 (23.06%), 912 (26.03%), 122 (3.48%), 46 (1.31%) respectively.
Table 4. Habits of spectacle wearing.
| Characteristic | n (%) |
| The frequency of changing spectacles | |
| ≤1y | 872 (32.57) |
| 1-2y | 1276 (47.65) |
| 2-3y | 332 (12.42) |
| >3y | 198 (7.36) |
| Habits of wearing spectacles | |
| Wearing when need | 966 (36.07) |
| Wearing constantly | 1712 (63.93) |
| Duration of wearing spectacles | |
| <1y | 228 (6.51) |
| 1-3y | 562 (16.04) |
| 3-5y | 808 (23.06) |
| 5-8y | 912 (26.03) |
| 8-10y | 122 (3.48) |
| >10y | 46 (1.31) |
Correction of Myopia
In this survey, the definition of under corrective myopia is that PVA could be improved by at least 2 lines with subjective refraction compared with baseline. Table 5 showed the correction status in 3242 myopia subjects in which 2682 (82.73%) individuals had corrected whereas 560 (17.27%) without corrected, while 2736 (84.39%) students were under correction, only 506 (15.61%) students were well corrected. The ratio of correction of mild, moderate and high myopia were 49.58%, 95.62% and 98.11%, respectively. While the ratio of under correction in mild, moderate and high myopia were 82.70%, 83.40% and 90.54%, respectively. The ratio of well correction in mild, moderate and high myopia were 17.30%, 16.60% and 9.46%, respectively.
Table 5. Correction status of students of myopia subjects.
| Groups | Total | Corrected | Under correction | Well corrected |
| Myopia | 3242 (92.52) | 2682 (82.73) | 2736 (84.39) | 506 (15.61) |
| Mild myopia | 948 (27.05) | 470 (49.58) | 784 (82.70) | 164 (17.30) |
| Moderate myopia | 1554 (44.35) | 1486 (95.62) | 1296 (83.40) | 258 (16.60) |
| High myopia | 740 (21.12) | 726 (98.11) | 670 (90.54) | 70 (9.46) |
n (%)
DISCUSSION
Our study showed that the VI rate before vision correction among first year university students was 94.03%, but about with 95.63% of VI was attributable to refractive error and mostly myopia. Refractive errors, especially myopia, had become a major public health problem worldwide, especially in Asia[12]–[13]. This study demonstrated high prevalence of refractive errors and high myopia in young adults exposed to high educational demands, though the sample investigated was not representative of the young adult population as a whole. University students comprised a specific academic excellent population. Therefore, the prevalence of myopia and high myopia were probably high. This opinion was verified by our study. In our study, myopia was found in 92.52% of all participants, with high myopia occurring in 22.26% of all participants. First year university students with emmetropia were very rare (6.22%). Other studies also found a high prevalence of myopia and high myopia in Chinese university students. Sun et al[3] reported that 95.5% first year university students and postgraduates from Donghua University were myopia in Shanghai and 19.5% of them were high myopia. Wu et al[14] reported that the prevalence of about 80% for myopia and 10% for high myopia in students aged 16 to 18y. These results supported our discovery. University students had remarkably myopia prevalence; it might be associated with education levels[15]. Previous study[16] showed that higher levels of school and post-school professional education were associated with myopic refraction. University first year university students were a special population which just underwent a high-intensity of prolonged near work and less outdoor activities. Recent studies supported the association of time spent outdoors with the incidence of myopia[17]–[18]. It has been reported for years that near work can be associated with myopia, though recent studies raised some doubts about this association[19]–[20]. Therefore, prolonged near work and less outdoor activities may be the main risk factors that leads to myopia in young university students.
We also found a slightly higher prevalence of myopia in female first year university students. Some studies presented high prevalence of myopia in female subjects. Females students spent more time on reading, doing near work[21]. The Shunyi Study conducted a semirural area in northern China, 36.7% male and 55% female subjects were myopic at the age of 15[22]. Nevertheless, other study[23] did not find any significant difference for the prevalence of myopia on gender. Large-scale studies need to confirm this result.
Astigmatism, another major cause of correctable VI in the world, is divided into refractive astigmatism (RA) and corneal astigmatism[24] that can be independently measured. The etiology of astigmatism is complex with gene[25] and environmental[26] risk factors. Astigmatism is highly prevalent in school-age children and aged 21 to 30y old[27]. A study in Singapore[13] showed that the prevalence of refractive astigmatism increased significantly from 41.4% of 15 085 young subjects aged around 19y old in 1996-1997 to 50.9% of 28 908 young subjects aged around 19y old in 2009-2010. NHANES Study analyzed 12 010 participants aged 20y and over, it presented the prevalence of astigmatism was 36.2% in USA[28]. While our study showed a higher prevalence (61.16%) of refractive astigmatism in university first year university students comparing with Singapore (50.9%) and the USA (36.2%). This difference may be caused by the different aged population in each study.
The refractive error is an avoidable VI. PVA is a crucial factor that affect the vision quality. As shown in Table 5, our study found that the PVA of most students was worse which was eventually affect their daily life. The under correction ratio was remarkable in myopia subjects indicating a poor corrective status of university first year university students. Some worse corrected students did not realize their poor corrected VA can be further improved, that would make them feel frustrated and affect their daily activities, such as job hunting, marriage and specializations. Some studies in different age support this result. Wang et al[11] reported that among urban migrant children aged around 11y old in eastern China, there was a high ratio of needing for spectacles (55.80%) and a very low ratio of spectacle ownership (12.82%). He et al[29] showed that the rate of wearing spectacles was low and the percentage of inaccurate prescriptions, among those who wore spectacles, was high in schools for children in Shanghai, China. This increasing high ratio of under correction was a crucial public social issue in young adult. However, this kind of PVA was easy to be well corrected. In our study, all under correction myopia students could achieve BCVA to a normal level except for students with ocular disease.
The reasons of high ratio of under correction in university students was not clear. Previous studies reported poor spectacle compliance was due to heavy spectacles, poor cosmetic appearance with spectacles, peer pressure and embarrassment of wearing spectacles[30]. In our study, high ratio of under correction was considered as follow. On the one hand, some students refused to check their VA, especially high myopia students. The spectacles were not appropriate prepared for vision correction including in accurate spectacles prescription and poor quality of spectacles. On the other hand, the habit of wearing spectacles is not proper. In our study, 36.07% students wear spectacles only when they need in the specific circumstance such as examination, driving and studying, so that they had a poor VA in most time of their daily life. There is also a misunderstanding in spectacle wearing. A commonly-held opinion is that wearing spectacles may be harmful to our eyes leading rapidly increasing of refractive error. This attitude prevents wearing spectacles in myopia students, even if they had medium or high myopia. This baseless opinion is refuted by some literatures. Under correction or full correction of myopia by wearing spectacles did not show any association with myopia progression or axial elongation[31]. Under correction or poor correction was not a beneficial therapeutic modality in early-onset myopia. While full correction should be adopted during the whole early-onset myopia[32]. This result indicated that under correction status and poor PVA were main reason for correction error in young university students. Full correction with spectacles should be adopted in myopia.
The limitations of this study were attributable to small population size. The characteristics of only first year university students subjects in one university also biased the results in this population. Large-scale study and wide age range will contribute to more accurate results.
Our study demonstrated high prevalence of refractive error and high ratio of under correction in university first year university students. This study offered evidence on worse PVA of university students in TMU affected by refractive error. This result may help to promote vision protection work in young adults.
Acknowledgments
Foundations: Supported by National Natural Science Foundation of China (No.81500745; No.81670875); the Natural Science Foundation of Tianjin (No.16JCQNJC12700; No.15JCZDJC34500).
Conflicts of Interest: Shi XY, None; Ke YF, None; Jin N, None; Zhang HM, None; Wei RH, None; Li XR, None.
REFERENCES
- 1.Bourne RRA, Flaxman SR, Braithwaite T, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(9):e888–e897. doi: 10.1016/S2214-109X(17)30293-0. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Visual Impairment and Blindness (2014) [Accessed on February 3, 2016]. Available at: http://www.who.int/mediacentre/factsheets/fs282/en/.
- 3.Sun J, Zhou J, Zhao P, et al. High prevalence of myopia and high myopia in 5060 Chinese university students in Shanghai. Invest Ophthalmol Vis Sci. 2012;53(12):7504–7509. doi: 10.1167/iovs.11-8343. [DOI] [PubMed] [Google Scholar]
- 4.Li SM, Liu LR, Li SY, et al. Design, methodology and baseline data of a school-based cohort study in Central China: the Anyang Childhood Eye Study. Ophthalmic Epidemiol. 2013;20(6):348–359. doi: 10.3109/09286586.2013.842596. [DOI] [PubMed] [Google Scholar]
- 5.Wu JF, Bi HS, Wang SM, Hu YY, Wu H, Sun W, Lu TL, Wang XR, Jonas JB. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong Children Eye Study. PLoS One. 2013;8(12):e82763. doi: 10.1371/journal.pone.0082763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rudnicka AR, Kapetanakis VV, Wathern AK, Logan NS, Gilmartin B, Whincup PH, Cook DG, Owen CG. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016;100(7):882–890. doi: 10.1136/bjophthalmol-2015-307724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castagno VD, Fassa AG, Carret ML, Vilela MA, Meucci RD. Hyperopia: a meta-analysis of prevalence and a review of associated factors among school-aged children. BMC Ophthalmol. 2014;14:163. doi: 10.1186/1471-2415-14-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379(9827):1739–1748. doi: 10.1016/S0140-6736(12)60272-4. [DOI] [PubMed] [Google Scholar]
- 9.Wong TY, Ferreira A, Hughes R, Carter G, Mitchell P. Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. Am J Ophthalmol. 2014;157(1):9–25.e12. doi: 10.1016/j.ajo.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 10.Zhu M, Tong X, Zhao R, He X, Zhao H, Liu M, Zhu J. Visual impairment and spectacle coverage rate in Baoshan district, China: population-based study. BMC Public Health. 2013;13:311. doi: 10.1186/1471-2458-13-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang X, Yi H, Lu L, Zhang L, Ma X, Jin L, Zhang H, Naidoo KS, Minto H, Zou H, Rozelle S, Congdon N. Population prevalence of need for spectacles and spectacle ownership among urban migrant children in eastern China. JAMA Ophthalmol. 2015;133(12):1399–1406. doi: 10.1001/jamaophthalmol.2015.3513. [DOI] [PubMed] [Google Scholar]
- 12.Pan CW, Ramamurthy D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012;32(1):3–16. doi: 10.1111/j.1475-1313.2011.00884.x. [DOI] [PubMed] [Google Scholar]
- 13.Koh V, Yang A, Saw SM, Chan YH, Lin ST, Tan MM, Tey F, Nah G, Ikram MK. Differences in prevalence of refractive errors in young Asian males in Singapore between 1996-1997 and 2009-2010. Ophthalmic Epidemiol. 2014;21(4):247–255. doi: 10.3109/09286586.2014.928824. [DOI] [PubMed] [Google Scholar]
- 14.Wu LJ, You QS, Duan JL, Luo YX, Liu LJ, Li X, Gao Q, Zhu HP, He Y, Xu L, Jonas JB, Wang W, Guo XH. Prevalence and associated factors of myopia in high-school students in Beijing. PLoS One. 2015;10(3):e0120764. doi: 10.1371/journal.pone.0120764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldschmidt E, Jacobsen N. Genetic and environmental effects on myopia development and progression. Eye (Lond) 2014;28(2):126–133. doi: 10.1038/eye.2013.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mirshahi A, Ponto KA, Hoehn R, Zwiener I, Zeller T, Lackner K, Beutel ME, Pfeiffer N. Myopia and level of education: results from the Gutenberg Health Study. Ophthalmology. 2014;121(10):2047–2052. doi: 10.1016/j.ophtha.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 17.Guggenheim JA, Northstone K, McMahon G, Ness AR, Deere K, Mattocks C, Pourcain BS, Williams C. Time outdoors and physical activity as predictors of incident myopia in childhood: a prospective cohort study. Invest Ophthalmol Vis Sci. 2012;53(6):2856–2865. doi: 10.1167/iovs.11-9091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, Mitchell P. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115(8):1279–1285. doi: 10.1016/j.ophtha.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 19.Lu B, Congdon N, Liu X, Choi K, Lam DS, Zhang M, Zheng M, Zhou Z, Li L, Liu X, Sharma A, Song Y. Associations between near work, outdoor activity, and myopia among adolescent students in rural China: the Xichang Pediatric Refractive Error Study report no. 2. Arch Ophthalmol. 2009;127(6):769–775. doi: 10.1001/archophthalmol.2009.105. [DOI] [PubMed] [Google Scholar]
- 20.Ip JM, Saw SM, Rose KA, Morgan IG, Kifley A, Wang JJ, Mitchell P. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. 2008;49(7):2903–2910. doi: 10.1167/iovs.07-0804. [DOI] [PubMed] [Google Scholar]
- 21.Guo L, Yang J, Mai J, Du X, Guo Y, Li P, Yue Y, Tang D, Lu C, Zhang WH. Prevalence and associated factors of myopia among primary and middle school-aged students: a school-based study in Guangzhou. Eye (Lond) 2016;30(6):796–804. doi: 10.1038/eye.2016.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao J, Mao J, Luo R, Li F, Munoz SR, Ellwein LB. The progression of refractive error in school-age children: Shunyi district, China. Am J Ophthalmol. 2002;134(5):735–743. doi: 10.1016/s0002-9394(02)01689-6. [DOI] [PubMed] [Google Scholar]
- 23.Pan CW, Dirani M, Cheng CY, Wong TY, Saw SM. The age-specific prevalence of myopia in Asia: a meta-analysis. Optom Vis Sci. 2015;92(3):258–266. doi: 10.1097/OPX.0000000000000516. [DOI] [PubMed] [Google Scholar]
- 24.Young TL, Metlapally R, Shay AE. Complex trait genetics of refractive error. Arch Ophthalmol. 2007;125(1):38–48. doi: 10.1001/archopht.125.1.38. [DOI] [PubMed] [Google Scholar]
- 25.Lopes MC, Hysi PG, Verhoeven VJ, et al. Identification of a candidate gene for astigmatism. Invest Ophthalmol Vis Sci. 2013;54(2):1260–1267. doi: 10.1167/iovs.12-10463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tong L, Saw SM, Carkeet A, Chan WY, Wu HM, Tan D. Prevalence rates and epidemiological risk factors for astigmatism in Singapore school children. Optom Vis Sci. 2002;79(9):606–613. doi: 10.1097/00006324-200209000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Leung TW, Lam AK, Deng L, Kee CS. Characteristics of astigmatism as a function of age in a Hong Kong clinical population. Optom Vis Sci. 2012;89(7):984–992. doi: 10.1097/OPX.0b013e31825da156. [DOI] [PubMed] [Google Scholar]
- 28.Vitale S, Ellwein L, Cotch MF, Ferris FL, 3rd, Sperduto R. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008;126(8):1111–1119. doi: 10.1001/archopht.126.8.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.He J, Lu L, Zou H, He X, Li Q, Wang W, Zhu J. Prevalence and causes of visual impairment and rate of wearing spectacles in schools for children of migrant workers in Shanghai, China. BMC Public Health. 2014;14:1312. doi: 10.1186/1471-2458-14-1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kumaran SE, Balasubramaniam SM, Kumar DS, Ramani KK. Refractive error and vision-related quality of life in South Indian children. Optom Vis Sci. 2015;92(3):272–278. doi: 10.1097/OPX.0000000000000494. [DOI] [PubMed] [Google Scholar]
- 31.Li SY, Li SM, Zhou YH, Liu LR, Li H, Kang MT, Zhan SY, Wang N, Millodot M. Effect of undercorrection on myopia progression in 12-year-old children. Graefes Archiv Clin Exp Ophthalmol. 2015;253(8):1363–1368. doi: 10.1007/s00417-015-3053-8. [DOI] [PubMed] [Google Scholar]
- 32.Adler D, Millodot M. The possible effect of undercorrection on myopic progression in children. Clin Exp Optom. 2006;89(5):315–321. doi: 10.1111/j.1444-0938.2006.00055.x. [DOI] [PubMed] [Google Scholar]