Abstract
Purpose:
While attentional function is an extremely important patient outcome for older adults, research on changes in function in this group is extremely limited. The purposes of this study were to: identify subgroups of older patients (i.e., latent growth classes) based on changes in their level of self-reported attentional function; determine which demographic and clinical characteristics were associated with subgroup membership; and determine if these subgroups differed on quality of life (QOL) outcomes.
Methods:
Older oncology outpatients (n=365) who were assessed for changes in attention and working memory using the Attentional Function Index a total of six times over two cycles of chemotherapy (CTX). QOL was assessed using the Medical Outcomes Study-Short Form 12 and the QOL-Patient Version Scale. Latent profile analysis (LPA) was used to identify subgroups of older adults with distinct attentional function profiles.
Results:
Three distinct attentional functional profiles were identified (i.e., low, moderate, and high attentional function). Compared to the high class, older adults in the low and moderate attentional function classes had lower functional status scores, a worse comorbidity profile and were more likely to be diagnosed with depression. In addition, QOL scores followed an expected pattern (low class < moderate class < high attentional function class).
Conclusions:
Three distinct attentional function profiles were identified among a relatively large sample of older adults undergoing CTX. The phenotypic characteristics associated with membership in the low and moderate latent classes can be used by clinicians to identify high risk patients.
Keywords: cognitive function, attentional function, older adults, chemotherapy, latent profile analysis
INTRODUCTION
The number of older adults diagnosed with cancer is expected to increase by 67% between 2010 and 2030 (Smith et al., 2009). However, older adults are less likely to receive the most effective cancer treatments (Extermann et al., 2005), and to complete a standard course of chemotherapy (CTX) (Fairfield et al., 2011). Because age is a well-established risk factor for cognitive decline, researchers have speculated that older adults may be more vulnerable to the adverse cognitive effects of cancer treatments (Ahles et al., 2012; Hurria et al., 2006b; Lange et al., 2014). However, only limited information is available on the impact of CTX on older oncology patients’ cognitive function (Joly et al., 2015).
In a longitudinal study of older women with breast cancer (Lange et al., 2016), 29% had a decline in working memory using the neuropsychological test Wechsler Adult Intelligence Scale-III (i.e., arithmetic, digit-span forward, digit-span backward, and letter-number sequencing) (Wechsler, 1997), from before to after the completion of CTX. In another study of older breast cancer patients (Hurria et al., 2006a), >60% perceived pre-existing working memory problems and were more likely to perceive worsening memory after CTX. In addition, older adults with comorbidities (e.g., diabetes) have poorer cognitive performance prior to cancer treatment (Mandelblatt et al., 2014b). None of these studies evaluated patients at multiple time points over two cycles CTX to assess for more acute changes in cognitive function. In addition, these studies were limited because the sample sizes were relatively small and assessed only older women with breast cancer. As noted in three reviews (Joly et al., 2015; Loh et al., 2016; Mandelblatt et al., 2014a), longitudinal studies of changes in and factors associated with decrements in cognitive function in older adults receiving CTX are urgently needed to inform clinical decisions and follow-up care.
A number of instruments can be used to assess changes in cognitive function (Andreis et al., 2013; Collins et al., 2013; Minisini et al., 2008). However, shorter instruments, that are focused on an evaluation of changes in attention and working memory (i.e., executive function), may be easier for older adults to complete and more reflective of changes in their ability to manage daily activities. In addition, attention and working memory are the two most common domains of cognitive function that are affected by CTX (Vannorsdall, 2017; Vitali et al., 2017; Yao et al., 2017). One such self-reported instrument is the Attentional Function Index (AFI) (Cimprich et al., 2011). This instrument has been used in several studies of oncology patients and can detect changes attentional function over time (Askren et al., 2014; Jung et al., 2017; Moon et al., 2011; Myers et al., 2015; Visovatti et al., 2016; Von Ah et al., 2009).
In most studies of changes in cognitive function in older oncology patients (Hurria et al., 2006a; Lange et al., 2016), mean scores were used to evaluate for between groups differences or changes over time. This approach does not allow for the identification of subgroups of patients with distinct cognitive function profiles. The use of statistical approaches, like latent profile analysis (LPA), allows for the identification of these subgroups. Once these subgroups are identified, the demographic and clinical characteristics associated with subgroup membership can be evaluated.
While attentional function is an important patient outcome for older adults, research on changes in function in this vulnerable group is extremely limited. Therefore, the purposes of this study, in a sample of older oncology outpatients (n=365) who were assessed for changes in attention and working memory using the AFI over two cycles of CTX were to: identify subgroups of older patients (i.e., latent growth classes) based on changes in their level of self-reported attentional function; determine which demographic and clinical characteristics were associated with subgroup membership; and determine if these subgroups differed on quality of life (QOL) outcomes.
METHODS
Patients and Settings
Details on the larger, longitudinal study are published elsewhere (Miaskowski et al., 2016; Miaskowski et al., 2014). In brief, for the larger study, eligible patients were ≥18 years of age; had a diagnosis of breast, gastrointestinal (GI), gynecological (GYN), or lung cancer; had received CTX within the preceding four weeks; were scheduled to receive at least two additional cycles of CTX; were able to read, write, and understand English; and gave written informed consent. Patients were recruited from two Comprehensive Cancer Centers, one Veteran’s Affairs hospital, and four community-based oncology programs. A total of 2234 patients were approached during their second or third cycle of CTX and 1343 consented to participate (60.1% response rate). The major reason for refusal was being overwhelmed with their cancer treatment. For this study, data from patients who were ≥65 years of age (n=365) were used in the analysis of changes in attentional function.
Instruments
A demographic questionnaire obtained information on age, gender, ethnicity, marital status, living arrangements, education, employment status, and income. The Karnofsky Performance Status (KPS) scale was used to assess patients’ overall performance status (Karnofsky et al., 1948). Patients rated their functional status using the KPS scale that ranged from 30 (I feel severely disabled and need to be hospitalized) to 100 (I feel normal; I have no complaints or symptoms) (Ando et al., 2001; Schnadig et al., 2008).
Self-Administered Comorbidity Questionnaire (SCQ) consists of thirteen common medical conditions simplified into language that can be understood without prior medical knowledge (Sangha et al., 2003). Patients indicated if they had the condition; if they received treatment for it (proxy for disease severity); and if it limited their activities (indication of functional limitations). Across the thirteen conditions, the total SCQ score can range from 0 to 39 with higher scores indicating a worse comorbidity profile. The SCQ has well established validity and reliability (Brunner et al., 2008; Cieza et al., 2006).
Alcohol Use Disorder Identification Test (AUDIT) is a 10-item questionnaire that assesses alcohol consumption, alcohol dependence, and consequences of alcohol abuse in the last 12 months. The AUDIT gives a total score that ranges between 0 and 40. Scores of ≥8 are defined as hazardous use and score of ≥16 are defined as use of alcohol that is likely to be harmful to health (Babor et al., 2001). The AUDIT has well-established validity and reliability (Berks and McCormick, 2008). The Cronbach’s alpha for the AUDIT was 0.63.
Changes in attentional function over two cycles of CTX were assessed using the AFI score (Cimprich et al., 2011). AFI consists of 16 questions about attentional function. A higher total mean score on a 0 to 10 numeric scale (NRS) indicates greater capacity to direct attention (Cimprich et al., 2011). Total scores are grouped into categories of attentional function (i.e., <5 low function, 5.0 to 7.5 moderate function, >7.5 high function) (Cimprich et al., 2005). The AFI has well-established validity and reliability (Cimprich et al., 2011). The Cronbach’s alpha for the AFI total score was 0.93.
Changes in QOL were assessed using the SF-12 (Ware et al., 1996). The SF-12 consists of 12 questions about physical and mental health as well as overall health status. The SF-12 was scored into two components that measure physical (i.e., PCS) and psychological (mental component summary (MCS)) function. These scores can range from 0 to 100. Higher PCS and MCS scores indicate better physical and psychological functioning, respectively. The PCS score includes the dimensions of physical functioning, role-physical, bodily pain, and general health perceptions. The MCS score includes the dimensions of mental functioning, emotional functioning, social functioning, and vitality. The SF-12 has well established validity and reliability (Ware et al., 1996).
Disease-specific QOL was evaluated using the Quality of Life Scale-Patient Version (QOL-PV)) (Padilla et al., 1990; Padilla et al., 1983). This 41-item instrument measures four domains of QOL (i.e., physical, psychological, social, and spiritual well-being) in oncology patients, as well as a total QOL score. Each item is rated on a 0 to 10 NRS with higher scores indicating a better QOL. The QOL-PV has well established validity and reliability (Ferrell, 1995; Ferrell et al., 1995; Padilla et al., 1990; Padilla et al., 1983). The Cronbach’s alpha for the QOLPV total score was 0.92.
Study Procedures
The study was approved by the Committee on Human Research at the University of California, San Francisco and by the Institutional Review Board at each of the study sites. Eligible patients were approached by a research staff member in the infusion unit to discuss participation in the study. Written informed consent was obtained from all patients. Depending on the length of their CTX cycles, patients completed questionnaires in their homes, a total of six times over two cycles of CTX (i.e., prior to their next cycle of CTX (assessment symptoms during the period of recovery from the previous CTX cycle, Assessments 1 and 4), approximately 1 week after CTX administration (assessment of acute symptoms following the administration of CTX, Assessments 2 and 5), and approximately 2 weeks after CTX administration (assessment of symptoms during the potential nadir, Assessments 3 and 6)).
Research nurses reviewed patients’ medical records for disease and treatment information. The toxicity of each patients’ CTX regimen was rated using the MAX2 index. Briefly, the MAX2 score is the average of the most frequent grade 4 hematologic toxicity and the most frequent grade 3 to 4 nonhematologic toxicity reported in publications of a regimen and correlates well with the average overall risk of severe toxicity for that regimen (Aapro et al., 2000; Extermann et al., 2004; Extermann et al., 2002; Extermann et al., 2015).
Data Analysis
Descriptive statistics–
Data were analyzed using SPSS version 23 (SPSS, 2015). Descriptive statistics and frequency distributions were calculated for demographic and clinical characteristics.
LPA of attentional function scores–
As was done for other symptoms (Alfaro et al., 2014; Doong et al., 2015; Dunn et al., 2011; Eshragh et al., 2017; Kober et al., 2016), unconditional LPA was used to identify the profiles of attentional function scores (i.e., AFI scores) that characterized unobserved subgroups of patients (i.e., latent classes) over the six assessments. Typically, latent class growth modeling would be used to identify latent classes of individuals who change differently over time. However, our data demonstrated a complex pattern of change because a pre-treatment assessment, an immediate post-treatment assessment, and a second posttreatment assessment were done over two cycles of CTX. Therefore, LPA is more appropriate for this type of change trajectory.
In order to incorporate expected correlations among the repeated measures, we included covariance parameters among measures that were one or two occasions apart (i.e., a covariance structure with a lag of two). In this way, we retained the within person correlation among the measures, at the same time that we focused on the patterns of means that distinguished among the latent classes. We limited the covariance structure to a lag of two to accommodate the expected reduction in the correlations that would be introduced by two treatments within each set of three measurement occasions and to reduce model complexity.
Estimation was carried out with full information maximum likelihood with standard errors and a Chi-square test that are robust to non-normality and non-independence of observations (“estimator=MLR”). Model fit was evaluated to identify the solution that best characterized the observed latent class structure with the Bayesian Information Criterion (BIC), Vuong-Lo-Mendell-Rubin likelihood ratio test (VLRM), entropy, and latent class percentages that were large enough to be reliable (i.e., likely to replicate in new samples) (Muthen and Muthen, 1998–2012; Nylund et al., 2007). Missing data were accommodated with the use of the Expectation-Maximization (EM) algorithm (Muthen and Shedden, 1999).
Mixture models, like LPA, are known to produce solutions at local maxima. Therefore, our models were fit with from 1,000 to 2,400 random starts. This approach ensured that the estimated model was replicated many times and was not due to a local maximum. Estimation was done with Mplus Version 7.4.(Muthen and Muthen, 1998–2017)
Evaluation of differences among the latent classes
Differences among the latent classes in relevant demographic and clinical characteristics (Ahles et al., 2012; Cimprich et al., 2005; Janelsins et al., 2014; Mandelblatt et al., 2014B; Myers et al., 2015) and QOL outcomes were evaluated using analysis of variance and Kruskal-Wallis or Chi Square tests with Bonferroni corrected post hoc contrasts. All calculations used actual values. A corrected p-value of <.0167 (i.e., .05/3) was considered statistically significant.
RESULTS
LCA of Attentional Function
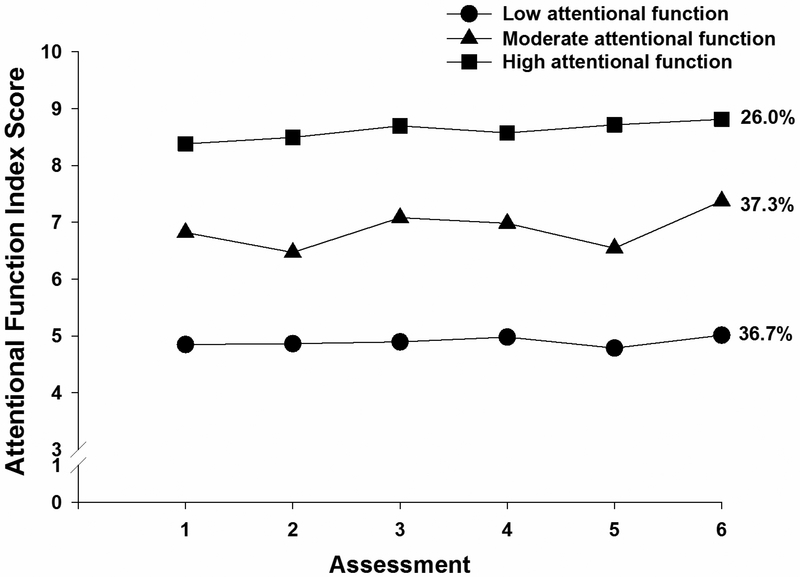
A three class solution was selected because the VLMR was significant, indicating that three classes fit the data better than two classes and the VLMR was not significant for the 4-class solution, indicating that too many classes had been extracted (Table 1). The classes were named based on the clinically meaningful cutpoints for the AFI reported in the literature (i.e., <5 low function, 5.0 to 7.5 moderate function, >7.5 high function) (Cimprich et al., 2005). As shown in Figure 1, at enrollment, 26.0% of the sample had high AFI scores. The largest class (37.3%) had moderate AFI scores and the third class (36.7%) had low AFI scores. The trajectories of attentional function differed among the latent classes. For both the low and the high attentional function classes, AFI scores remained relatively stable across the six assessments. For the moderate attentional function class, AFI scores varied over the two cycles of CTX, with slightly lower scores reported at assessments 2 and 5 (i.e., the week following the administration of CTX).
Table 1–
Latent Profile Analysis Solutions and Fit Indices for One- Through Four-Classes for Attentional Function Index Scores
| Model | LL | AIC | BIC | VLMR | Entropy |
|---|---|---|---|---|---|
| 1 Class | −3056.64 | 6155.28 | 6237.17 | n/a | n/a |
| 2 Class | −2905.26 | 5866.51 | 5975.71 | 302.76*** | .82 |
| 3 Classa | −2848.66 | 5767.33 | 5903.83 | 113.18* | .78 |
| 4 Class | −2811.97 | 5707.95 | 5871.74 | 73.38ns | .80 |
p < .05;
p < .001
The 3-class solution was selected because the VLMR was significant, indicating that three classes fit the data better than two classes. In addition, the VLMR was not significant for the 4-class solution, indicating that too many classes were extracted. In addition, one class in the 4-class solution was very small (18 cases or 5%) and unlikely to generalize to other samples.
Abbreviations: AIC = Akaike Information Criterion, BIC = Bayesian Information Criterion, LL = log-likelihood, n/a = not applicable, ns = not significant, VLMR = Vuong-Lo-Mendell-Rubin likelihood ratio test for the K vs. K-1 model
Figure 1–
Attentional Function Index trajectories for patients in each of the latent classes.
Demographic and Clinical Characteristics
As shown in Table 2, across the three latent classes, KPS scores (i.e., low < moderate < high) were in the expected direction. In addition, compared to the high class, patients in the moderate and low classes had higher SCQ scores and were more likely to be diagnosed with depression. Compared to the high class, patients in the low class were less likely to be married or partnered, less likely to be employed, more likely to report back pain and had a higher MAX2 score. Compared to the moderate and high classes, patients in the low class reported a lower annual household income. Finally, compared to the high class, patients in the moderate class were less likely to exercise on a regular basis and were less likely to not have received a previous cancer treatment.
Table 2–
Differences in Demographic and Clinical Characteristics Among the Attentional Function Latent Classes
| Characteristic | Low (0) 36.7% (n=134) |
Moderate (1) 37.3% (n=136) |
High (2) 26.0% (n=95) |
Statistics |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Age (years) | 71.8 (5.4) | 71.7 (5.9) | 70.2 (5.1) | F=2.91, p=.056 |
| Education (years) | 16.3 (3.0) | 16.7 (3.2) | 16.4 (3.0) | F=0.42, p=.658 |
| Body mass index (kg/m2) | 26.3 (5.4) | 26.2 (4.8) | 25.7 (6.0) | F=0.44, p=.646 |
| Karnofsky Performance Status score | 77.7 (13.2) | 83.8 (11.9) | 87.8 (10.0) | F=19.59, p<.001 0<1<2 |
| Number of comorbidities out of 16 | 3.7 (1.9) | 3.2 (1.6) | 2.8 (1.7) | F=6.39, p=.002 0>2 |
| SCQ score out of 16 conditions | 8.2 (4.3) | 7.0 (3.9) | 5.6 (3.3) | F=11.42, p<.001 0 and 1 > 2 |
| AUDIT score | 3.1 (3.0) | 3.1 (2.6) | 2.7 (1.5) | F=0.62, p=.539 |
| Hemoglobin | 11.3 (1.4) | 11.5 (1.5) | 11.7 (1.3) | F=1.86, p=.157 |
| Hematocrit | 33.9 (4.2) | 34.4 (4.5) | 35.1 (3.8) | F=2.25, p=.107 |
| Time since cancer diagnosis (years) | 2.4 (4.4) | 3.3 (5.9) | 3.1 (5.2) | KW, p=.355 |
| Time since cancer diagnosis (median) | 0.5 | 0.6 | 0.5 | |
| Number of prior cancer treatments | 1.8 (1.6) | 1.8 (1.4) | 1.6 (1.6) | F=0.79, p=.453 |
| Number of metastatic sites including lymph node involvement | 1.3 (1.3) | 1.4 (1.1) | 1.3 (1.2) | F=0.16, p=.850 |
| Number of metastatic sites excluding lymph node involvement | 0.9 (1.1) | 0.9 (1.0) | 0.9 (1.0) | F=0.03, p=.969 |
| MAX2 score | 0.17 (0.09) | 0.15 (0.08) | 0.14 (0.08) | F=4.51, p=.012 0>3 |
| % (n) | % (n) | % (n) | ||
| Gender | ||||
| Female | 73.5 (97) | 69.6 (94) | 60.0 (57) | X2=5.14, p=.077 |
| Male | 25.8 (34) | 30.4 (41) | 40.0 (38) | |
| Transgender* | 0.8 (1) | 0.0 (0) | 0.0 (0) | |
| Ethnicity | ||||
| White | 77.1 (101) | 84.3 (113) | 77.9 (74) | X2=6.67, p=.353 |
| Asian or Pacific Islander | 7.6 (10) | 5.2 (7) | 6.3 (6) | |
| Black | 7.6 (10) | 3.0 (4) | 10.5 (10) | |
| Hispanic, Mixed, or Other | 7.6 (10) | 7.5 (10) | 5.3 (5) | |
| Married or partnered (% yes) | 50.8 (66) | 59.7 (80) | 69.6 (64) | X2=7.91, p=.019 0<2 |
| Lives alone (% yes) | 36.2 (47) | 29.9 (40) | 20.9 (19) | X2=5.96, p=.051 |
| Child care responsibilities (% yes) | 3.9 (5) | 4.5 (6) | 6.4 (6) | X2=0.78, p=.678 |
| Care of adult responsibilities (% yes) | 6.2 (7) | 5.8 (7) | 2.3 (2) | X2=1.89, p=.390 |
| Currently employed (% yes) | 14.5 (19) | 23.1 (31) | 29.0 (27) | X2=7.14, p=.028 0<2 |
| Income | ||||
| < $30,000+ | 37.7 (43) | 16.9 (21) | 14.7 (11) | KW, p<.001 0 <1 and 2 |
| $30,000 to <$70,000 | 28.9 (33) | 29.8 (37) | 12.0 (9) | |
| $70,000 to < $100,000 | 9.6 (11) | 18.5 (23) | 28.0 (21) | |
| ≥ $100,000 | 23.7 (27) | 34.7 (43) | 45.3 (34) | |
| Specific comorbidities (% yes) | ||||
| Heart disease | 12.9 (17) | 13.3 (18) | 7.4 (7) | X2=2.27, p=.332 |
| High blood pressure | 43.2 (57) | 48.9 (66) | 46.3 (44) | X2=0.88, p=.645 |
| Lung disease | 23.5 (31) | 20.0 (27) | 15.8 (15) | X2=2.04, p=.361 |
| Diabetes | 15.9 (21) | 11.1 (15) | 16.8 (16) | X2=1.89, p=.388 |
| Ulcer or stomach disease | 6.1 (8) | 3.7 (5) | 3.2 (3) | X2=1.36, p=.506 |
| Kidney disease | 3.8 (5) | 1.5 (2) | 0.0 (0) | X2=4.41, p=.110 |
| Liver disease | 6.8 (9) | 8.9 (12) | 5.3 (5) | X2=1.14, p=.565 |
| Anemia or blood disease | 11.4 (15) | 8.9 (12) | 6.3 (6) | X2=1.71, p=.425 |
| Depression | 29.5 (39) | 17.0 (23) | 2.1 (2) | X2=28.64, p<.001 0 and 1 > 2 |
| Osteoarthritis | 25.0 (33) | 23.7 (32) | 21.1 (20) | X2=0.49, p=.785 |
| Back pain | 33.3 (44) | 25.2 (34) | 17.9 (17) | X2=6.93, p=.031 0>2 |
| Rheumatoid arthritis | 3.0 (4) | 4.4 (6) | 3.2 (3) | X2=0.46, p=.796 |
| Exercise on a regular basis (% yes) | 63.0 (80) | 61.4 (81) | 76.8 (73) | X2=6.76, p=.034 1<2 |
| Smoking, current or history of (% yes) | 48.8 (63) | 48.5 (64) | 44.7 (42) | X2=0.44, p=.802 |
| Cancer diagnosis | ||||
| Breast | 25.0 (33) | 24.4 (33) | 18.9 (18) | X2=7.46, p=.280 |
| Gastrointestinal | 28.0 (37) | 30.4 (41) | 42.1 (40) | |
| Gynecological | 20.5 (27) | 25.2 (34) | 18.9 (18) | |
| Lung | 26.5 (35) | 20.0 (27) | 20.0 (19) | |
| Type of prior cancer treatment | X2=15.42, p=.017 | |||
| No prior treatment | 22.5 (29) | 16.3 (21) | 36.2 (34) | 1<2 |
| Only surgery, CTX, or RT | 36.4 (47) | 40.3 (52) | 24.5 (23) | NS |
| Surgery & CTX, or Surgery & RT, or CTX & RT | 25.6 (33) | 31.8 (41) | 24.5 (23) | NS |
| Surgery & CTX & RT | 15.5 (20) | 11.6 (15) | 14.9 (14) | NS |
Abbreviations: AUDIT = Alcohol Use Disorders Identification Test, CTX = chemotherapy, kg = kilograms, KW = Kruskal Wallis; m2 = meter squared, RT = radiation therapy, SCQ = Self-Administered Comorbidity Questionnaire, SD = standard deviation
Chi Square analysis done without the transgender patient include in the analyses
No age, education, or gender differences were found among the latent classes. In addition, except for MAX 2 scores, none of the disease or treatment characteristics were associated with latent class membership.
Generic QOL Outcomes
For the SF-12 physical function, role physical, bodily pain, vitality, social functioning, role emotional, and mental health, as well as the PCS and MCS scores, the differences among the latent classes followed the same pattern (i.e., low < moderate < high). For the general health score, compared to patients in the moderate and high classes, patients in the low class reported lower scores (Table 3).
Table 3–
Differences in Quality of Life Scores at Enrollment Among the Attentional Function Latent Classes
| Characteristic | Low (0) 36.7% (n=134) |
Moderate (1) 37.3% (n=136) |
High (2) 26.0% (n=95) |
Statistics |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Medical Outcomes Study – Short Form-12 | ||||
| Physical functioning | 34.6 (30.7) | 50.8 (34.1) | 67.4 (34.2) | F=26.52, p<.001 0<1<2 |
| Role physical | 34.8 (22.3) | 53.7 (27.3) | 71.4 (24.9) | F=58.10, p<.001 0<1<2 |
| Bodily pain | 69.0 (31.1) | 80.7 (24.4) | 91.2 (19.5) | F=19.86, p<.001 0<1<2 |
| General health | 53.8 (29.1) | 65.5 (26.0) | 71.2 (25.7) | F=12.09, p<.001 0 < 1 and 2 |
| Vitality | 29.3 (22.8) | 46.2 (25.7) | 67.4 (20.2) | F=72.03, p<.001 0<1<2 |
| Social functioning | 50.8 (33.2) | 70.1 (31.4) | 85.9 (20.7) | F=38.41, p<.001 0<1<2 |
| Role emotional | 58.3 (29.8) | 82.1 (23.9) | 93.0 (12.4) | F=61.78, p<.001 0<1<2 |
| Mental health | 63.9 (22.4) | 78.0 (16.9) | 87.1 (12.6) | F=45.95, p<.001 0<1<2 |
| Physical component summary score | 36.9 (9.7) | 41.0 (10.9) | 45.7 (9.9) | F=18.58, p<.001 0<1<2 |
| Mental component summary score | 43.1 (11.6) | 52.2 (9.0) | 57.3 (5.3) | F=64.06, p<.001 0<1<2 |
| Multidimensional Quality of Life Scale – Cancer | ||||
| Physical well-being | 6.2 (1.6) | 7.2 (1.5) | 8.2 (1.3) | F=48.92, p<.001 0<1<2 |
| Psychological well-being | 4.8 (1.7) | 5.9 (1.6) | 7.4 (1.5) | F=66.82, p<.001 0<1<2 |
| Social well-being | 5.5 (2.0) | 6.7 (1.7) | 7.6 (1.3) | F=40.81, p<.001 0<1<2 |
| Spiritual well-being | 4.9 (2.2) | 4.8 (2.0) | 5.2 (2.1) | F=1.27, p=.283 |
| Total quality of life score | 5.2 (1.4) | 6.1 (1.2) | 7.2 (1.1) | F=66.42, p<.001 0<1<2 |
Disease-specific QOL Outcomes
For the QOL-PV physical well-being, psychological well-being, social well-being, and total QOL scores, the differences among the latent classes followed the same pattern (i.e., low < moderate < high). No differences were found among the latent classes in the spiritual wellbeing scores (Table 3).
DISCUSSION
This study is the first to use LPA to identify subgroups of older oncology patients with distinct attentional function profiles over two cycles of CTX. In this relatively large sample, with a mean age of 71.4 (±5.5), three groups of older adults with distinct attentional function profiles were identified. Of note, 74% of our older adults reported decrements in attentional function. The low and the high classes’ AFI scores remained relatively stable over the two cycles of CTX. However, the AFI scores for the moderate class decreased in the week following the administration of CTX (i.e., assessments 2 and 5, Figure 1). The exact reasons for these fluctuations in AFI scores in the moderate class are not readily apparent.
Our finding of three distinct attentional function profiles is consistent with our previous reports in two independent samples of patients who underwent radiation therapy and their family caregivers (Merriman et al., 2014b) and breast cancer patients who underwent surgery (Merriman et al., 2014a). While the range of AFI scores for the low, moderate, and high attentional function classes were relatively similar across our three studies, the distributions of class membership differed. In the study of patients and family caregivers (mean age = 62.1 years) who were assessed from prior to the initiation of radiation therapy through 4 months after its completion, 84.5% of the participants were in the low and moderate AFI classes. In the study of breast cancer patients (mean age = 54.8 years) who were assessed from prior to through 6 months after their surgery, 58.4% were in the low and moderate AFI classes. These differences in the distribution of attentional function profiles may be related to a number of sample characteristics (e.g., age, gender, receipt of previous cancer treatment).
Of note, in both of our previous studies (Merriman et al., 2014a; Merriman et al., 2014b), younger age was associated with membership in the low compared to the high attentional function class. While in general, older adults are at higher risk for cognitive impairments (Vega et al., 2017), it is possible that younger individuals may notice and report more subtle changes in their cognitive function. In contrast, older adults may have adjusted to their alterations in attentional function prior to the administration of CTX (Cimprich et al., 2011). An alternative explanation for the age differences across our studies may be the over-representation of females in our two previous studies (Merriman et al., 2014a; Merriman et al., 2014b). For example, in a study of patients receiving CTX for colorectal cancer (Vardy et al., 2015), after controlling for age, women had higher levels of cognitive impairment than men. Future studies need to evaluate for the effects of both age and gender on self-reported attentional function. That said, our findings suggest that decrements in attentional function are a significant problem for older oncology patients as well as for patients and their family caregivers during and following a variety of cancer treatments.
Our finding that 36.7% of our sample was in the low class is consistent with previous reports that found that between 29% (Lange et al., 2016) and 36% (Hshieh et al., 2018) of older patients had cognitive impairments prior to the initiation of cancer treatment. While we did not assess for cognitive impairments prior to the initiation of CTX, a growing body of evidence suggests that some older oncology patients have changes in cognition prior to the initiation of treatment (Loh et al., 2016). This vulnerable group of patients may have difficulties following simple directions and retaining educational information that is needed to care for themselves during outpatient CTX (Cimprich et al., 2011).
While a previous study found an association between poorer cognitive function and less education (Mandelblatt et al., 2014b), the demographic characteristics associated with membership in either the low and/or the moderate AFI classes in our study were: not being married/partnered, having a lower annual household income, and being unemployed. A plausible explanation for these associations may be the interaction between medical and social determinants of health. It is widely understood that health is determined not only by biological factors but by complex interactions between social, cultural, and economic factors; one’s physical environment; and individual behaviors (Solar and Irwin, 2010). In addition, as noted by Williams and colleagues (Williams et al., 2000) being employed may condition the mechanisms involved in directing attention to function more efficiently. Therefore, when patients are not working, they do not experience this routine conditioning. This deficit may contribute to the perception of decreases in attentional function. However, in other studies among younger patients and caregivers (Cimprich, 1999; Merriman et al., 2014b), no association was found between employment status and AFI scores. As noted in a recent review (Janelsins et al., 2014), socioeconomic status which is known to affect cognitive function in other medical conditions, warrants additional investigation in patients undergoing cancer treatment.
Consistent with our two previous reports (Merriman et al., 2014a; Merriman et al., 2014b), older adults in the low attentional function class had the worst comorbidity profile. As noted by Loh and colleagues (Loh et al., 2016), this relationship may be partially explained by the fact that CTX-related cognitive impairment may share common biological mechanisms (e.g., inflammation) with many comorbid conditions. In addition, they suggested that many of the medications that are used to treat common medical conditions may contribute to alterations in cognition in older adults receiving CTX.
As deficits in cognitive function are found in major depressive disorders (Lam et al., 2014), it is interesting to note that ~30% of the older adults in the low AFI class reported depression. In addition, over 30% of the patients in the low class reported back pain. Both of these conditions are treated with medications that can have deleterious effects on cognitive function (e.g., antidepressants, opioids). Future studies need to evaluate the impact of multiple medications on older adults cognitive function while they are undergoing cancer treatment.
Another plausible explanation for why the low attentional function class had the largest number of phenotypic characteristics associated with class membership is the complex interplay between multimorbidity in older adults and the broader social determinants of health (Northwood et al., 2018). For example, in one systematic review (Marengoni et al., 2011), significant associations were found between lower socioeconomic status and increased prevalence of multimorbidity in the elderly. In addition, in a cohort study of 2729 patients with multiple comorbidities (von dem Knesebeck et al., 2015), social inequalities was significantly associated with decrements in self-rated health, functional status, and QOL. Interestingly, these associations with income were stronger than with either education or occupational position. The authors suggested that a “double burden of disease” exists among older people with a lower socioeconomic status. While our findings support this hypothesis, additional research is warranted.
It is interesting to note that the only clinical characteristic associated with attentional function was the MAX2 score. As expected, compared to the high class, older adults in the low class had a higher MAX2 score which suggests that they were receiving a CTX regimen that was associated with a worse toxicity profile (Aapro et al., 2000; Extermann et al., 2004; Extermann et al., 2002; Extermann et al., 2015). Given that the first assessment in the current study took place after the patient had received their first or second cycle of CTX, it is not readily apparent if a 0.03 difference in MAX2 scores represents a clinically meaningful difference that could contribute to the decrements in attentional function found in the low AFI class.
Consistent with our hypothesis that differences would be found among the three attentional function classes, in both generic and disease specific measures of QOL, except for general health and spiritual well-being, statistically significant, as well as clinically meaningful differences were found among the low, moderate, and the high attentional function classes that followed the same pattern (i.e. low < moderate <high; Table 3). It is important to note that for all three classes of older adults, the PCS score for the SF-12 was below the normative score of 50 for the general United States population (Ware Jr et al., 1996). Of note, while significant differences were found among the three classes in the MCS score, only the low attentional function class had a score below 50 (Ware Jr et al., 1996). Taken together, these findings suggest that older adults who score less than 5 on the AFI warrant comprehensive geriatric assessments and careful monitoring not only for decrements in cognitive function but physical function as well.
Several study limitations warrant consideration. While a total of six assessments were done over two cycles of CTX, these older adults were not assessed prior to the initiation of CTX. Second, our assessment of cognitive function was limited to a self-report measure that primarily evaluates executive function. Therefore, additional research is warranted using objective measures of cognitive function to determine if latent class membership differs depending on the assessment method used (i.e., subjective or objective measures) and the domain of cognitive function that is evaluated (e.g., executive function, working memory). While some studies of cognitive function compare patients undergoing treatment to healthy controls (Cimprich et al., 2011; Piacentine et al., 2016), the goal of this study was to identify distinct subgroups of older adults within the context of CTX treatment.
Despite these limitations, this study is the first to identify subgroups of older adults with distinct attentional function profiles. The phenotypic characteristics associated with membership in the low and moderate AFI classes can be used to identify high risk patients. Future studies should evaluate the impact of multiple comorbidities on various domains of cognitive function, as well as the inter-relationships between physical and cognitive function in older patients receiving CTX. Additional research is warranted on longitudinal changes in cognitive function in older adults, as well as the impact of cognitive changes on the QOL of older adults using agespecific QOL measures.
Highlights.
Older adults vary in their levels of attentional function.
Decrements in attentional function are associated with higher levels of comorbidity.
Decrements in attentional function are associated with worse quality of life outcomes.
Acknowledgements:
This work was supported by the National Cancer Institute (R01CA134900 and K05CA168960), the National Institute on Aging (T32AG000212 and P30AG044281), and the National Center for Advancing Translational Sciences (KL2TR001870). Dr. Miaskowski is an American Cancer Society Clinical Research Professor.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Aapro M, Extermann M, Repetto L, 2000. Evaluation of the elderly with cancer. Ann Oncol 11 Suppl 3, 223–229. [DOI] [PubMed] [Google Scholar]
- Ahles TA, Root JC, Ryan EL, 2012. Cancer- and cancer treatment-associated cognitive change: an update on the state of the science. J Clin Oncol 30, 3675–3686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfaro E, Dhruva A, Langford DJ, Koetters T, Merriman JD, West C, Dunn LB, Paul SM, Cooper B, Cataldo J, Hamolsky D, Elboim C, Kober K, Aouizerat BE, Miaskowski C, 2014. Associations between cytokine gene variations and self-reported sleep disturbance in women following breast cancer surgery. Eur J Oncol Nurs 18, 85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ando M, Ando Y, Hasegawa Y, Shimokata K, Minami H, Wakai K, Ohno Y, Sakai S, 2001. Prognostic value of performance status assessed by patients themselves, nurses, and oncologists in advanced non-small cell lung cancer. Br J Cancer 85, 1634–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreis F, Ferri M, Mazzocchi M, Meriggi F, Rizzi A, Rota L, Di Biasi B, Abeni C, Codignola C, Rozzini R, Zaniboni A, 2013. Lack of a chemobrain effect for adjuvant FOLFOX chemotherapy in colon cancer patients. A pilot study. Support Care Cancer 21, 583–590. [DOI] [PubMed] [Google Scholar]
- Askren MK, Jung M, Berman MG, Zhang M, Therrien B, Peltier S, Ossher L, Hayes DF, Reuter-Lorenz PA, Cimprich B, 2014. Neuromarkers of fatigue and cognitive complaints following chemotherapy for breast cancer: a prospective fMRI investigation. Breast Cancer Res Treat 147, 445–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG, 2001. AUDIT: The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Care. World Health Organization, Geneva. [Google Scholar]
- Berks J, McCormick R, 2008. Screening for alcohol misuse in elderly primary care patients: a systematic literature review. Int Psychogeriatr 20, 1090–1103. [DOI] [PubMed] [Google Scholar]
- Brunner F, Bachmann LM, Weber U, Kessels AG, Perez RS, Marinus J, Kissling R, 2008. Complex regional pain syndrome 1--the Swiss cohort study. BMC Musculoskelet Disord 9, 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cieza A, Geyh S, Chatterji S, Kostanjsek N, Ustun BT, Stucki G, 2006. Identification of candidate categories of the International Classification of Functioning Disability and Health (ICF) for a Generic ICF Core Set based on regression modelling. BMC Med Res Methodol 6, 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cimprich B, 1999. Pretreatment symptom distress in women newly diagnosed with breast cancer. Cancer Nurs 22, 185–194. [DOI] [PubMed] [Google Scholar]
- Cimprich B, So H, Ronis DL, Trask C, 2005. Pre‐treatment factors related to cognitive functioning in women newly diagnosed with breast cancer. Psycho‐Oncology 14, 70–78. [DOI] [PubMed] [Google Scholar]
- Cimprich B, Visovatti M, Ronis DL, 2011. The Attentional Function Index--a self-report cognitive measure. Psychooncology 20, 194–202. [DOI] [PubMed] [Google Scholar]
- Collins B, MacKenzie J, Tasca GA, Scherling C, Smith A, 2013. Cognitive effects of chemotherapy in breast cancer patients: a dose-response study. Psycho-oncology 22, 1517–1527. [DOI] [PubMed] [Google Scholar]
- Doong SH, Dhruva A, Dunn LB, West C, Paul SM, Cooper BA, Elboim C, Abrams G, Merriman JD, Langford DJ, Leutwyler H, Baggott C, Kober K, Aouizerat BE, Miaskowski C, 2015. Associations between cytokine genes and a symptom cluster of pain, fatigue, sleep disturbance, and depression in patients prior to breast cancer surgery. Biol Res Nurs 17, 237–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn LB, Cooper BA, Neuhaus J, West C, Paul S, Aouizerat B, Abrams G, Edrington J, Hamolsky D, Miaskowski C, 2011. Identification of distinct depressive symptom trajectories in women following surgery for breast cancer. Health Psychol 30, 683–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eshragh J, Dhruva A, Paul SM, Cooper BA, Mastick J, Hamolsky D, Levine JD, Miaskowski C, Kober KM, 2017. Associations between neurotransmitter genes and fatigue and energy levels in women after breast cancer surgery. J Pain Symptom Manage 53, 67–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Extermann M, Aapro M, Bernabei R, Cohen HJ, Droz JP, Lichtman S, Mor V, Monfardini S, Repetto L, Sorbye L, Topinkova E, 2005. Use of comprehensive geriatric assessment in older cancer patients: recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG). Crit Rev Oncol Hematol 55, 241–252. [DOI] [PubMed] [Google Scholar]
- Extermann M, Bonetti M, Sledge GW, O’Dwyer PJ, Bonomi P, Benson AB 3rd, 2004. MAX2--a convenient index to estimate the average per patient risk for chemotherapy toxicity; validation in ECOG trials. Eur J Cancer 40, 1193–1198. [DOI] [PubMed] [Google Scholar]
- Extermann M, Chen H, Cantor AB, Corcoran MB, Meyer J, Grendys E, Cavanaugh D, Antonek S, Camarata A, Haley WE, Balducci L, 2002. Predictors of tolerance to chemotherapy in older cancer patients: a prospective pilot study. Eur J Cancer 38, 1466–1473. [DOI] [PubMed] [Google Scholar]
- Extermann M, Reich RR, Sehovic M, 2015. Chemotoxicity recurrence in older patients: Risk factors and effectiveness of preventive strategies-a prospective study. Cancer 121:2984–2992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairfield KM, Murray K, Lucas FL, Wierman HR, Earle CC, Trimble EL, Small L, Warren JL, 2011. Completion of adjuvant chemotherapy and use of health services for older women with epithelial ovarian cancer. J Clin Oncol 29, 3921–3926. [DOI] [PubMed] [Google Scholar]
- Ferrell BR, 1995. The impact of pain on quality of life. A decade of research. Nurs Clin North Am 30, 609–624. [PubMed] [Google Scholar]
- Ferrell BR, Dow KH, Grant M, 1995. Measurement of the quality of life in cancer survivors. Qual Life Res 4, 523–531. [DOI] [PubMed] [Google Scholar]
- Hshieh TT, Jung WF, Grande LJ, Chen J, Stone RM, Soiffer RJ, Driver JA, Abel GA, 2018. Prevalence of cognitive impairment and association with survival among older patients with hematologic cancers. JAMA Oncol Mar 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurria A, Goldfarb S, Rosen C, Holland J, Zuckerman E, Lachs MS, Witmer M, van Gorp WG, Fornier M, D’Andrea G, 2006a. Effect of adjuvant breast cancer chemotherapy on cognitive function from the older patient’s perspective. Breast Cancer Res Treat 98, 343–348. [DOI] [PubMed] [Google Scholar]
- Hurria A, Rosen C, Hudis C, Zuckerman E, Panageas KS, Lachs MS, Witmer M, van Gorp WG, Fornier M, D’Andrea G, Moasser M, Dang C, Van Poznak C, Hurria A, Holland J, 2006b. Cognitive function of older patients receiving adjuvant chemotherapy for breast cancer: a pilot prospective longitudinal study. J Am Geriatr Soc 54, 925–931. [DOI] [PubMed] [Google Scholar]
- Janelsins MC, Kesler SR, Ahles TA, Morrow GR, 2014. Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int Rev Psychiatry 26, 102–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joly F, Giffard B, Rigal O, De Ruiter MB, Small BJ, Dubois M, LeFel J, Schagen SB, Ahles TA, Wefel JS, Vardy JL, Pancre V, Lange M, Castel H, 2015. Impact of cancer and its treatments on cognitive function: Advances in research from the Paris International Cognition and Cancer Task Force Symposium and Update Since 2012. J Pain Symptom Manage 50, 830–841. [DOI] [PubMed] [Google Scholar]
- Jung MS, Zhang M, Askren MK, Berman MG, Peltier S, Hayes DF, Therrien B, Reuter-Lorenz PA, Cimprich B, 2017. Cognitive dysfunction and symptom burden in women treated for breast cancer: a prospective behavioral and fMRI analysis. Brain Image Behav 11, 86–97. [DOI] [PubMed] [Google Scholar]
- Karnofsky D, Abelmann WH, Craver LV, Burchenal JH, 1948. The use of nitrogen mustards in the palliative treatment of carcinoma. Cancer 1, 634–656. [Google Scholar]
- Kober KM, Cooper BA, Paul SM, Dunn LB, Levine JD, Wright F, Hammer MJ, Mastick J, Venook A, Aouizerat BE, Miaskowski C, 2016. Subgroups of chemotherapy patients with distinct morning and evening fatigue trajectories. Support Care Cancer 24, 1473–1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam RW, Kennedy SH, McIntyre RS, Khullar A, 2014. Cognitive dysfunction in major depressive disorder: effects on psychosocial functioning and implications for treatment. Can J Psychiatry 59, 649–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange M, Heutte N, Rigal O, Noal S, Kurtz JE, Levy C, Allouache D, Rieux C, Lefel J, Clarisse B, Veyret C, Barthelemy P, Longato N, Castel H, Eustache F, Giffard B, Joly F, 2016. Decline in cognitive function in older adults with early-stage breast cancer after adjuvant treatment. Oncologist July 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange M, Rigal O, Clarisse B, Giffard B, Sevin E, Barillet M, Eustache F, Joly F, 2014. Cognitive dysfunctions in elderly cancer patients: a new challenge for oncologists. Cancer Treat Rev 40, 810–817. [DOI] [PubMed] [Google Scholar]
- Loh KP, Janelsins MC, Mohile SG, Holmes HM, Hsu T, Inouye SK, Karuturi MS, Kimmick GG, Lichtman SM, Magnuson A, Whitehead MI, Wong ML, Ahles TA, 2016. Chemotherapy-related cognitive impairment in older patients with cancer. J Geriatr Oncol 7, 270–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandelblatt JS, Jacobsen PB, Ahles T, 2014a. Cognitive effects of cancer systemic therapy: implications for the care of older patients and survivors. J Clin Oncol 32, 2617–2626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandelblatt JS, Stern RA, Luta G, McGuckin M, Clapp JD, Hurria A, Jacobsen PB, Faul LA, Isaacs C, Denduluri N, Gavett B, Traina TA, Johnson P, Silliman RA, Turner RS, Howard D, Van Meter JW, Saykin A, Ahles T, 2014b. Cognitive impairment in older patients with breast cancer before systemic therapy: is there an interaction between cancer and comorbidity? J Clin Oncol 32, 1909–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, Meinow B, Fratiglioni L, 2011. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev 10, 430–439. [DOI] [PubMed] [Google Scholar]
- Merriman JD, Aouizerat BE, Cataldo JK, Dunn L, Cooper BA, West C, Paul SM, Baggott CR, Dhruva A, Kober K, Langford DJ, Leutwyler H, Ritchie CS, Abrams G, Dodd M, Elboim C, Hamolsky D, Melisko M, Miaskowski C, 2014a. Association between an interleukin 1 receptor, type I promoter polymorphism and self-reported attentional function in women with breast cancer. Cytokine 65, 192–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merriman JD, Aouizerat BE, Langford DJ, Cooper BA, Baggott CR, Cataldo JK, Dhruva A, Dunn L, West C, Paul SM, Ritchie CS, Swift PS, Miaskowski C, 2014b. Preliminary evidence of an association between an interleukin 6 promoter polymorphism and self-reported attentional function in oncology patients and their family caregivers. Biol Res Nurs 16, 152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miaskowski C, Cooper BA, Aouizerat B, Melisko M, Chen LM, Dunn L, Hu X, Kober KM, Mastick J, Levine JD, Hammer M, Wright F, Harris J, Armes J, Furlong E, Fox P, Ream E, Maguire R, Kearney N, 2017. The symptom phenotype of oncology outpatients remains relatively stable from prior to through 1 week following chemotherapy. Eur J Cancer Care 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miaskowski C, Cooper BA, Melisko M, Chen LM, Mastick J, West C, Paul SM, Dunn LB, Schmidt BL, Hammer M, Cartwright F, Wright F, Langford DJ, Lee K, Aouizerat BE, 2014. Disease and treatment characteristics do not predict symptom occurrence profiles in oncology outpatients receiving chemotherapy. Cancer 120, 2371–2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minisini AM, De Faccio S, Ermacora P, Andreetta C, Fantinel R, Balestrieri M, Piga A, Puglisi F, 2008. Cognitive functions and elderly cancer patients receiving anticancer treatment: a prospective study. Crit Rev Oncol Hematol 67, 71–79. [DOI] [PubMed] [Google Scholar]
- Moon S, Kim SH, Kim MJ, 2011. Perceived cognitive function and related factors in korean women with breast cancer. Asian Nurs Res 2, 141–150. [DOI] [PubMed] [Google Scholar]
- Muthen B, Shedden K, 1999. Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics 55, 463–469. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO, 1998–2012. Mplus User’s Guide, 7th ed. ed. Muthen & Muthen, Los Angeles, CA. [Google Scholar]
- Muthen LK, Muthen BO, 1998–2017. Mplus User’s Guide (8th ed.), 8th ed. Muthen & Muthen, Los Angeles, CA. [Google Scholar]
- Myers JS, Wick JA, Klemp J, 2015. Potential factors associated with perceived cognitive impairment in breast cancer survivors. Support Care Cancer 23, 3219–3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northwood M, Ploeg J, Markle-Reid M, Sherifali D, 2018. Integrative review of the social determinants of health in older adults with multimorbidity. J Adv Nurs 74, 45–60. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthen BO, 2007. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling 14, 535–569. [Google Scholar]
- Padilla GV, Ferrell B, Grant MM, Rhiner M, 1990. Defining the content domain of quality of life for cancer patients with pain. Cancer Nurs 13, 108–115. [PubMed] [Google Scholar]
- Padilla GV, Presant C, Grant MM, Metter G, Lipsett J, Heide F, 1983. Quality of life index for patients with cancer. Res Nurs Health 6, 117–126. [DOI] [PubMed] [Google Scholar]
- Piacentine LB, Miller JF, Haberlein S, Bloom AS, 2016. Perceived cognitive changes with chemotherapy for breast cancer: A pilot study. Appl Nurs Res 29, 9–11. [DOI] [PubMed] [Google Scholar]
- Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN, 2003. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum 49, 156–163. [DOI] [PubMed] [Google Scholar]
- Schnadig ID, Fromme EK, Loprinzi CL, Sloan JA, Mori M, Li H, Beer TM, 2008. Patient-physician disagreement regarding performance status is associated with worse survivorship in patients with advanced cancer. Cancer 113, 2205–2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA, 2009. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol 27, 2758–2765. [DOI] [PubMed] [Google Scholar]
- Solar O, Irwin A, 2010. A conceptual framework for action on the social determinants of health.
- SPSS, 2015. IBM SPSS for Windows (Version 23). SPSS, Inc., Armonk, NY. [Google Scholar]
- Vannorsdall TD, 2017. Cognitive Changes Related to Cancer Therapy. Med Clin North Am 101, 1115–1134. [DOI] [PubMed] [Google Scholar]
- Vardy JL, Dhillon HM, Pond GR, Rourke SB, Bekele T, Renton C, Dodd A, Zhang H, Beale P, Clarke S, Tannock IF, 2015. Cognitive function in patients with colorectal cancer who do and do not receive chemotherapy: A prospective, longitudinal, controlled study. J Clin Oncol 33, 4085–4092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega JN, Dumas J, Newhouse PA, 2017. Cognitive effects of chemotherapy and cancer-related treatments in older adults. Am J Geriatr Psychiatry 25, 1415–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visovatti MA, Reuter-Lorenz PA, Chang AE, Northouse L, Cimprich B, 2016. Assessment of cognitive impairment and complaints in individuals with colorectal cancer. Oncol Nurs Forum 43, 169–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitali M, Ripamonti CI, Roila F, Proto C, Signorelli D, Imbimbo M, Corrao G, Brissa A, Rosaria G, de Braud F, Garassino MC, Lo Russo G, 2017. Cognitive impairment and chemotherapy: a brief overview. Crit Rev Oncol Hematol 118, 7–14. [DOI] [PubMed] [Google Scholar]
- Von Ah D, Russell KM, Storniolo AM, Carpenter JS, 2009. Cognitive dysfunction and its relationship to quality of life in breast cancer survivors. Oncol Nurs Forum 36, 326–336. [DOI] [PubMed] [Google Scholar]
- von dem Knesebeck O, Bickel H, Fuchs A, Gensichen J, Hofels S, Riedel-Heller SG, Konig HH, Mergenthal K, Schon G, Wegscheider K, Weyerer S, Wiese B, Scherer M, van den Bussche H, Schafer I, 2015. Social inequalities in patient-reported outcomes among older multimorbid patients--results of the MultiCare cohort study. Int J Equity Health 14, 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware J Jr., Kosinski M, Keller SD, 1996. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34, 220–233. [DOI] [PubMed] [Google Scholar]
- Wechsler D, 1997. Wechsler Adult Intelligence Scale-III. The Psychological Corporation. [Google Scholar]
- Williams RA, Hagerty BM, Cimprich B, Therrien B, Bay E, Oe H, 2000. Changes in directed attention and short-term memory in depression. J Psychiatr Res 34, 227–238. [DOI] [PubMed] [Google Scholar]
- Yao C, Bernstein LJ, Rich JB, 2017. Executive functioning impairment in women treated with chemotherapy for breast cancer: a systematic review. Breast Cancer Res Treat 166, 15–28. [DOI] [PubMed] [Google Scholar]